Abstract
Background
There is a lack of research concerning health-related quality of life (HRQoL) in Saudi patients with sickle cell disease (SCD), particularly among adult populations. The aim of the current study was to describe the characteristics of SCD patients and their impact on their quality of life (QoL).
Methods
Six hundred twenty-nine adult SCD patients who attended King Fahad Hospital in Hofuf and King Fahad Central Hospital in Jazan were included in the analysis. Demographic/clinical data were collected and an Arabic version of the Medical Outcomes 36-Item Short-Form Health Survey (SF-36) questionnaire was used to assess QoL.
Results
SCD patients who hold a university degree reported positive impacts on the following domains of SF-36: physical role function, vitality, emotional well being, social function, pain reduction, and general health (P = .002, P = .001, P = .001, P = .003, P = .004, and P = .001, respectively). In general, patients with fever, skin redness, swelling, or history of blood transfusion tended to impair the health status of the SF-36. A multivariate analysis revealed that patients with a university degree tended to report high scores of physical role functions, emotional role function, and vitality. Patients with regular exercise tend to increase vitality, social function, general health, and reduce pain. Unemployment tends to lessen vitality and worsen pain. On average, pain, social function, and physical function scores tended to worsen in patients with swelling or history of blood transfusion.
Conclusions
This study highlighted that poor education, fever, skin redness, and swelling were negatively associated with specific components of SF-36. SCD patients with a history of blood transfusion found their QoL poorer, whereas regular exercise tended to improve QoL.
Keywords: Sickle cell disease, Quality of life, SF-36, Pain, Saudi Arabia
Background
Sickle cell disease (SCD) is a genetic disease that affects humans and is handed down from parents to children. Sickle cell patients report poorer quality of life (QoL) in comparison with the general population and other chronic non-communicable diseases [1–5]. Several international studies have been conducted to examine the QoL of children and adults with SCD [4–12]. There is a lack of research concerning health-related quality of life (HRQoL) in Saudi patients with SCD. A single study conducted in Saudi Arabia examined the QoL of adolescents with SCD [13]. This research has highlighted a number of important factors related to HRQoL. According to the authors, SCD-related complications and socio-demographics were shown to decrease QoL in Saudi adolescents [13]. The study revealed that age, gender, and education were associated with changes in QoL in Saudi adolescents with SCD [13]. However, no study has assessed HRQoL in adult patients with SCD in the entire Arabic world, particularly among Saudi adult populations. SCD is present throughout Saudi Arabia and is particularly common in the Eastern and Southern regions [13]. The frequency of the sickle cell gene in the Hofuf area ranges from 15–25 % of the population in Eastern province of Saudi Arabia [14]. The prevalence of sickle cell disease in Southern region of Saudi Arabia was 10.3 % [15]. Coping with this disease is a very challenging experience, especially for adolescents. Psychosocial problems are common in patients with SCD. Factors such as pain, apprehension, difficulty in fulfilling personal and family responsibility, financial burdens, and diminished cognition must also be encompassed to fully understand what the illness means to an individual [16, 17].
There is a great need to educate the public toward a greater understanding of the connection between pain and their reactions toward the symptoms. Healthcare providers that are less familiar with SCD patients might underestimate the impact of SCD on the quality of life of an individual with SCD (e.g., describing SCD patients as drug dependent [18]). This is due to insufficient knowledge of the severity of SCD and the disease in general. Some providers may not know how to minimize the burden of SCD patients to achieve as normal a life as possible. Therefore, measuring the QoL among adults with SCD might provide significant attention to the health outcome and the degree of severity of the disease. This study represents the first investigation of SCD patients’ QoL in an adult Saudi Arabia population. The current study describes the health-related QoL of Saudi adults with SCD, and examines explanatory predictors that might be associated with poorer QoL. Specifically, we hypothesized that the presence of signs, symptoms, or complications of SCD as reported by fever, skin redness swelling in hands or feet, and blood transfusion are associated with worse HRQoL. The study also investigates the effect of gender, age, physical activity, and other characteristics on HRQoL among adult Saudi patients with SCD. Another purpose of this study was to build predictive models to explain the variation in each of the SF-36 domains.
Methods
A multicenter, cross-sectional study was conducted in King Fahad Hospital, Hofuf, Eastern region and King Fahad Central Hospital, Jazan, Southern region, Saudi Arabia. This study was approved by the Ministry of Health (IRB Log No. 15-247E), Kingdom of Saudi Arabia, and the King Abdullah International Medical Research Center, Research Protocol - RC12/127/R. Participants in the study were adult patients with sickle cell who were treated in King Fahad Hospital in Hofuf and King Fahad Central Hospital in Jazan. All respondents provided verbal agreement to participate in the study. A total of 629 questionnaires were completed out of the 823 that were distributed, a response rate of 76.4 %. The exclusion criteria included: age < 18 years or patient who can’t read or write. Data about patient demographics and clinical characteristics collected included age, gender, marital status, education, obesity (body mass index of 30 or greater), and employment status. The study participants were asked to report fever (Yes/No), skin redness (Yes/No), swelling in hands or feet (Yes/No), and blood transfusion (Yes/No) during the past three months. In addition to SCD symptoms and complications, the participants were asked to report family history of anemia (Yes/No), presence of other chronic diseases (Yes/No), regular exercise (Yes/No), and whether they are receiving family support (Yes/No).
Study instrument
The study measured the HRQoL in adult patients with SCD. The Medical Outcomes Study (MOS) short form (SF-36) is a 36-item tool for measuring health status and outcomes from the patients’ perceptions [19]. The English version of the RAND-36 provides a reliable measure of HRQoL, and Cronbach’s alpha values range from 0.78 to 0.93 [19]. This survey has already been translated into Arabic and tested for internal consistency and reliability in a sample of Saudi Arabian citizens [20]. It was found that both the Arabic and English versions of the RAND-36 are equivalent. A previous study used the Arabic version of the RAND-36 to assess health-related quality of life, but this study was conducted in an adolescent population [13]. In our study, adults patients with SCD rated their QoL in terms of their satisfaction and feelings with regard to eight different components, with a total of 36 items addressing eight health concepts: physical function (10 items); physical role health (4 items); emotional role functions (3 items); vitality (4 items); emotional wellbeing (5 items); social function (2 items); bodily pain (2 items); and generalica health perceptions (5 items). Data from SF-36 were scored based on the scoring system reported by RAND Health. Each component has a single summary variable ranging from 0 = poor health to 100 = good health. The internal consistency and reliability of the SF-36 has been investigated in a pilot study of 80 patients with SCD. High internal consistency (Cronbach’s alpha > 0.6) have been reported for physical function (Cronbach’s alpha = 0.81); physical role health (Cronbach’s alpha = 0.84); emotional role functions (Cronbach’s alpha = 0.86); vitality (Cronbach’s alpha = 0.79); emotional wellbeing (Cronbach’s alpha = 0.67); social function (Cronbach’s alpha = 0.67); bodily pain (Cronbach’s alpha = 0.84); and general health (Cronbach’s alpha = 0.60).
Statistical analyses
The data analysis was performed using IBM SPSS Statistics 20 (SPSS, Chicago, IL).
Patients’ characteristics
Descriptive statistics such as means and standard deviation (mean ± SD) were used to describe the quantitative variables. Frequencies and percentages n (%) were used to describe categorical variables (Table 1).
Table 1.
SCD sample characteristics (n =629)
| Characteristics | Levels | Number | Percent |
|---|---|---|---|
| Gender | Female | 374 | 59.6 |
| Male | 253 | 40.4 | |
| Older age | No | 523 | 83.1 |
| Yes | 106 | 16.9 | |
| University | No | 440 | 72.5 |
| Yes | 167 | 27.5 | |
| Married | No | 342 | 55.6 |
| Yes | 273 | 44.4 | |
| Employed | No | 407 | 71.4 |
| Yes | 163 | 28.6 | |
| Obese | No | 440 | 90.9 |
| Yes | 44 | 9.1 | |
| Fever | No | 246 | 40.3 |
| Yes | 365 | 59.7 | |
| Skin redness | No | 407 | 66.6 |
| Yes | 204 | 33.4 | |
| Swelling | No | 324 | 53.0 |
| Yes | 287 | 47.0 | |
| History of blood transfusion | No | 100 | 16.1 |
| Yes | 520 | 83.9 | |
| Family history of anemia | No | 59 | 9.6 |
| Yes | 554 | 90.4 | |
| Family support | No | 47 | 7.7 |
| Yes | 560 | 92.3 | |
| Other Chronic disease | No | 509 | 83.3 |
| Yes | 102 | 16.7 | |
| Regular exercise | No | 410 | 66.3 |
| Yes | 208 | 33.7 | |
| Spleen removed | No | 508 | 81.8 |
| Yes | 113 | 18.2 | |
| FS-36 Subscales | Mean | SD | |
| Physical functioning | 55.1 | 23.3 | |
| Role limitations due to physical health | 35.9 | 36.0 | |
| Role limitations due to emotional problems | 40.1 | 40.5 | |
| Vitality | 47.8 | 19.1 | |
| Emotional well being | 59.3 | 19.4 | |
| Social functioning | 60.1 | 25.0 | |
| Pain | 47.9 | 27.6 | |
| General health | 47.8 | 15.6 |
Bivariate analyses
The impact of patients’ characteristics on health status components (8 components of the SF-36) was evaluated by independent sample t-tests (Tables 2 and 3). Specifically, we compared physical functioning, role limitation due to physical health, role limitations due to emotional problems, vitality, emotional wellbeing, social functioning, bodily pain, and general health perceptions across socio-demographic/ clinical characteristics. In order to account for 15 multiple comparisons, the p-values were adjusted using a Bonferroni correction for all the sub-group Analyses. Significance level was evaluated at P < 0.05/15 (0.003).
Table 2.
Differences in health-related quality of life by socio-demographic and clinical characteristics (N = 629)
| Physical functioning | Role limitations due to physical health | Role limitations due to emotional problems | Vitality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | P | Mean | SD | P | Mean | SD | P | Mean | SD | P | ||
| Gender | Female | 57.0 | 23.7 | 0.019 | 36.5 | 37.1 | 0.630 | 39.1 | 41.7 | 0.423 | 49.0 | 20.0 | 0.060 |
| Male | 52.3 | 22.5 | 35.0 | 34.5 | 41.8 | 38.5 | 46.0 | 17.4 | |||||
| Older age | No | 55.5 | 23.4 | 0.472 | 36.1 | 35.4 | 0.767 | 39.0 | 39.2 | 0.218 | 48.0 | 18.8 | 0.484 |
| Yes | 53.5 | 22.7 | 34.9 | 39.1 | 45.1 | 46.1 | 46.6 | 20.2 | |||||
| University | No | 53.3 | 22.9 | 0.004 | 32.9 | 34.9 | 0.002* | 38.1 | 39.7 | 0.020 | 45.9 | 18.3 | 0.001* |
| Yes | 59.5 | 23.5 | 43.8 | 37.7 | 47.1 | 42.1 | 53.2 | 19.4 | |||||
| Married | No | 56.0 | 23.6 | 0.401 | 38.4 | 34.8 | 0.078 | 42.3 | 39.1 | 0.183 | 49.1 | 18.2 | 0.061 |
| Yes | 54.3 | 23.1 | 33.1 | 37.6 | 37.8 | 42.2 | 46.1 | 19.9 | |||||
| Employed | No | 53.4 | 22.5 | 0.002* | 35.7 | 36.0 | 0.379 | 39.6 | 39.9 | 0.283 | 45.6 | 18.6 | 0.001* |
| Yes | 60.1 | 23.3 | 38.7 | 37.6 | 43.8 | 41.8 | 52.1 | 19.6 | |||||
| Obese | No | 56.3 | 23.9 | 0.086 | 37.6 | 36.8 | 0.309 | 42.2 | 40.3 | 0.766 | 48.2 | 19.5 | 0.188 |
| Yes | 49.7 | 23.4 | 31.5 | 34.9 | 40.3 | 42.8 | 44.2 | 15.6 | |||||
| Fever | No | 55.9 | 23.8 | 0.555 | 44.6 | 36.5 | 0.001* | 46.5 | 41.8 | 0.002* | 53.7 | 19.2 | 0.001* |
| Yes | 54.7 | 23.1 | 30.0 | 34.8 | 35.8 | 39.2 | 43.9 | 17.9 | |||||
| Skin redness | No | 57.5 | 22.6 | 0.001* | 40.3 | 36.4 | 0.001* | 42.7 | 40.6 | 0.040 | 50.3 | 19.3 | 0.001* |
| Yes | 50.5 | 23.6 | 27.1 | 34.1 | 35.3 | 40.3 | 42.9 | 17.5 | |||||
| Swelling | No | 59.2 | 22.9 | 0.001* | 41.0 | 36.9 | 0.001* | 44.8 | 41.5 | 0.002* | 52.1 | 20.0 | 0.001* |
| Yes | 51.2 | 22.9 | 29.7 | 34.1 | 34.7 | 39.0 | 42.9 | 16.9 | |||||
| History of blood transfusion | No | 61.7 | 25.1 | 0.003* | 47.9 | 37.1 | 0.001* | 50.2 | 41.5 | 0.007 | 53.3 | 21.1 | 0.002* |
| Yes | 53.7 | 22.8 | 33.6 | 35.4 | 37.9 | 40.0 | 46.6 | 18.5 | |||||
| Family history of anemia | No | 53.3 | 19.6 | 0.547 | 38.5 | 37.5 | 0.623 | 44.2 | 41.1 | 0.480 | 51.7 | 17.5 | 0.102 |
| Yes | 55.4 | 23.5 | 35.9 | 36.1 | 40.1 | 40.5 | 47.2 | 19.1 | |||||
| Family support | No | 57.7 | 21.3 | 0.424 | 35.9 | 40.0 | 0.983 | 45.2 | 47.2 | 0.469 | 46.7 | 22.2 | 0.659 |
| Yes | 54.8 | 23.6 | 35.8 | 35.9 | 39.9 | 40.0 | 48.0 | 18.7 | |||||
| Other Chronic disease | No | 56.0 | 23.2 | 0.032 | 37.6 | 36.2 | 0.034 | 41.4 | 40.7 | 0.242 | 49.0 | 19.3 | 0.002* |
| Yes | 50.4 | 22.7 | 29.1 | 34.6 | 36.1 | 39.3 | 42.4 | 17.2 | |||||
| Regular exercise | No | 54.1 | 22.6 | 0.134 | 34.8 | 36.4 | 0.261 | 40.3 | 41.0 | 0.694 | 44.7 | 18.6 | 0.001* |
| Yes | 57.3 | 24.6 | 38.3 | 35.1 | 38.9 | 39.4 | 53.5 | 18.5 | |||||
| Spleen removed | No | 55.1 | 23.0 | 0.877 | 34.7 | 35.5 | 0.088 | 39.5 | 40.5 | 0.451 | 47.7 | 19.1 | 0.931 |
| Yes | 54.7 | 24.9 | 41.3 | 38.3 | 42.8 | 40.8 | 47.9 | 18.8 | |||||
*The factor is significant using Bonferroni correction cut-off at α/n = 0.05/15 = 0.003
Table 3.
Differences in health-related quality of life by socio-demographic and clinical characteristics (N = 629)
| Emotional well being | Social functioning | Pain | General health | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | P | Mean | SD | P | Mean | SD | P | Mean | SD | P | ||
| Gender | Female | 60.1 | 19.7 | 0.241 | 60.6 | 25.7 | 0.510 | 49.0 | 28.5 | 0.268 | 47.8 | 15.7 | 0.876 |
| Male | 58.2 | 19.1 | 59.2 | 24.0 | 46.5 | 26.4 | 48.0 | 15.6 | |||||
| Older age | No | 59.4 | 19.1 | 0.711 | 59.6 | 24.8 | 0.280 | 48.5 | 27.3 | 0.257 | 47.8 | 15.8 | 0.980 |
| Yes | 58.6 | 21.0 | 62.5 | 26.1 | 45.1 | 29.4 | 47.9 | 15.1 | |||||
| University | No | 57.3 | 19.1 | 0.001* | 58.4 | 24.6 | 0.003* | 46.0 | 26.9 | 0.004 | 46.3 | 15.2 | 0.001* |
| Yes | 63.9 | 19.3 | 65.4 | 25.6 | 53.2 | 28.5 | 51.6 | 16.1 | |||||
| Married | No | 60.7 | 18.8 | 0.064 | 61.8 | 24.8 | 0.100 | 50.0 | 27.7 | 0.058 | 48.6 | 15.3 | 0.167 |
| Yes | 57.7 | 20.2 | 58.4 | 24.8 | 45.7 | 27.3 | 46.8 | 16.2 | |||||
| Employed | No | 58.2 | 19.5 | 0.132 | 58.8 | 25.2 | 0.044 | 46.1 | 27.7 | 0.018 | 47.0 | 15.2 | 0.230 |
| Yes | 61.0 | 19.4 | 63.6 | 24.4 | 52.3 | 27.7 | 48.8 | 16.6 | |||||
| Obese | No | 59.3 | 19.4 | 0.836 | 61.0 | 24.7 | 0.099 | 48.5 | 27.9 | 0.455 | 47.8 | 16.1 | 0.395 |
| Yes | 58.6 | 20.8 | 54.5 | 22.1 | 45.2 | 24.4 | 45.5 | 15.2 | |||||
| Fever | No | 63.1 | 18.5 | 0.001* | 65.9 | 25.3 | 0.001* | 54.4 | 28.4 | 0.001* | 51.5 | 15.3 | 0.001* |
| Yes | 56.9 | 19.7 | 56.2 | 24.0 | 43.4 | 26.2 | 45.6 | 15.3 | |||||
| Skin redness | No | 61.2 | 19.7 | 0.001* | 62.6 | 24.8 | 0.001* | 50.6 | 28.6 | 0.001* | 50.6 | 15.3 | 0.001* |
| Yes | 55.8 | 18.4 | 55.0 | 24.6 | 42.6 | 25.4 | 42.5 | 15.1 | |||||
| Swelling | No | 63.0 | 19.4 | 0.001* | 65.7 | 24.7 | 0.001* | 56.4 | 28.8 | 0.001* | 50.9 | 15.4 | 0.001* |
| Yes | 55.1 | 18.9 | 53.5 | 23.9 | 38.4 | 23.3 | 44.5 | 15.3 | |||||
| History of blood transfusion | No | 62.8 | 18.7 | 0.045 | 69.6 | 24.1 | 0.001* | 59.0 | 28.2 | 0.001* | 53.2 | 15.4 | 0.001* |
| Yes | 58.5 | 19.5 | 57.7 | 24.6 | 45.8 | 27.2 | 46.7 | 15.5 | |||||
| Family history of anemia | No | 63.0 | 18.3 | 0.126 | 66.4 | 24.7 | 0.057 | 55.8 | 29.0 | 0.023 | 48.9 | 14.6 | 0.610 |
| Yes | 58.8 | 19.4 | 59.5 | 24.8 | 47.0 | 27.3 | 47.7 | 15.7 | |||||
| Family support | No | 56.9 | 20.6 | 0.328 | 60.6 | 23.8 | 0.896 | 53.9 | 28.4 | 0.126 | 51.5 | 15.3 | 0.118 |
| Yes | 59.8 | 19.2 | 60.0 | 25.2 | 47.4 | 27.5 | 47.6 | 15.7 | |||||
| Other Chronic disease | No | 60.8 | 19.1 | 0.001* | 61.7 | 24.5 | 0.002* | 49.1 | 27.9 | 0.088 | 48.4 | 15.9 | 0.056 |
| Yes | 52.5 | 19.8 | 53.0 | 24.9 | 43.8 | 25.1 | 44.9 | 14.3 | |||||
| Regular exercise | No | 57.5 | 19.3 | 0.002* | 58.5 | 24.5 | 0.031 | 45.8 | 27.0 | 0.011 | 45.9 | 15.5 | 0.001* |
| Yes | 62.8 | 19.3 | 63.2 | 25.4 | 51.8 | 28.5 | 51.0 | 15.0 | |||||
| Spleen removed | No | 59.9 | 19.3 | 0.079 | 60.7 | 25.0 | 0.277 | 48.0 | 27.5 | 0.981 | 48.1 | 15.6 | 0.477 |
| Yes | 56.2 | 20.3 | 57.8 | 23.9 | 48.0 | 28.2 | 46.9 | 16.0 | |||||
*The factor is significant using Bonferroni correction cut-off at α/n = 0.05/15 = 0.003
Regression analyses
Multiple linear regression models were used to identify important predictors of each health status component (Table 4). In multiple linear regression analyses, P < 0.05 was considered significant.
Table 4.
Multiple regression showing predictors of health-related quality of life in patients with SCD
| Physical functioning | Role limitations due to physical health | Role limitations due to emotional problems | Vitality | Emotional well being | Social functioning | Pain | General health | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | B | P | B | P | B | P | B | P | B | P | B | P | B | P | B | P |
| (Constant) | 76.3 | 61.7 | 45.3 | 50.6 | 74.6 | 77.5 | 77.3 | 59.6 | ||||||||
| Gender | −3.1 | 0.278 | −0.2 | 0.964 | 1.7 | 0.714 | 1.1 | 0.619 | −0.6 | 0.801 | 1.9 | 0.503 | 4.6 | 0.126 | 2.9 | 0.113 |
| Age | −0.2 | 0.327 | 0.2 | 0.519 | 0.6 | 0.020* | 0.3 | 0.036* | 0.0 | 0.772 | 0.2 | 0.202 | −0.1 | 0.704 | 0.0 | 0.834 |
| University | 4.9 | 0.077 | 10.9 | 0.009* | 13.9 | 0.003* | 5.3 | 0.013* | 3.7 | 0.102 | 2.6 | 0.359 | 4.1 | 0.179 | 3.4 | 0.060 |
| Married | −3.8 | 0.191 | −8.4 | 0.056 | −15.7 | 0.001* | −6.9 | 0.002* | −5.2 | 0.029* | −6.1 | 0.036* | −5.7 | 0.069 | −2.8 | 0.146 |
| Employed | 5.1 | 0.086 | 1.9 | 0.673 | 0.2 | 0.960 | 7.3 | 0.001* | 3.5 | 0.139 | 3.9 | 0.190 | 6.8 | 0.036* | 1.8 | 0.347 |
| Obese | −1.5 | 0.717 | −3.7 | 0.555 | 3.0 | 0.667 | −2.8 | 0.366 | 2.1 | 0.544 | −6.1 | 0.143 | −1.4 | 0.750 | −1.0 | 0.711 |
| Fever | 3.2 | 0.241 | −8.7 | 0.032* | −5.6 | 0.212 | −6.6 | 0.001* | −3.0 | 0.162 | −5.2 | 0.054 | −4.2 | 0.148 | −1.9 | 0.292 |
| Skin redness | −5.7 | 0.033* | −10.9 | 0.008* | −5.5 | 0.226 | −2.5 | 0.220 | −1.9 | 0.382 | −3.5 | 0.203 | −2.1 | 0.472 | −4.3 | 0.016* |
| Swelling | −8.1 | 0.003* | −6.0 | 0.131 | −7.1 | 0.108 | −4.2 | 0.036* | −3.4 | 0.111 | −8.4 | 0.002* | −14.4 | 0.001* | −4.3 | 0.013* |
| Blood transfusion | −6.7 | 0.046* | −9.8 | 0.052 | −12.9 | 0.022* | −1.6 | 0.524 | −0.9 | 0.726 | −7.4 | 0.026* | −8.3 | 0.024* | −5.9 | 0.007* |
| Family history of anemia | −2.8 | 0.620 | −8.6 | 0.291 | 2.4 | 0.788 | −5.2 | 0.208 | −7.0 | 0.119 | −6.2 | 0.239 | −8.8 | 0.125 | −2.1 | 0.564 |
| Family support | −3.7 | 0.381 | −3.2 | 0.621 | −3.3 | 0.652 | 1.1 | 0.730 | −1.1 | 0.754 | −2.1 | 0.638 | −7.6 | 0.107 | −4.0 | 0.160 |
| Other Chronic disease | −4.0 | 0.293 | −5.5 | 0.328 | −1.0 | 0.867 | −6.7 | 0.019* | −9.7 | 0.001* | −10.1 | 0.008* | −3.7 | 0.369 | −0.7 | 0.786 |
| Regular exercise | 0.0 | 0.988 | 4.7 | 0.239 | −1.3 | 0.764 | 5.6 | 0.005* | 1.7 | 0.433 | 6.1 | 0.024* | 7.5 | 0.009* | 5.2 | 0.003* |
| Spleen removed | 4.2 | 0.192 | 8.1 | 0.090 | 11.8 | 0.027* | 0.9 | 0.716 | −5.1 | 0.048* | −3.1 | 0.326 | 2.2 | 0.514 | 2.3 | 0.267 |
| F-value | 3.2 | 3.6 | 2.8 | 5.4 | 3 | 4.3 | 5.7 | 4.1 | ||||||||
| P-value | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | ||||||||
| R Square | 0.12 | 0.13 | 0.10 | 0.18 | 0.11 | 0.15 | 0.18 | 0.15 | ||||||||
| R | 0.35 | 0.36 | 0.32 | 0.42 | 0.33 | 0.39 | 0.43 | 0.38 | ||||||||
* Controlling for other predictors in model, predictor is significant at α = 0.05
Results
Patients’ characteristics
Characteristics of the patients are presented in Table 1. Of 629 SCD patients included in the study, 40.4 % were males. The mean age of the patients was 28.8 (SD ± 9.1 years) with range between 18 and 75 years. A total of 273 patients (44.4 %) were married, 407 (71.4 %) were unemployed, and 44 (9.1 %) were obese. Among 629 SCD patients, 59.7 % had fever, 33.4 % had skin redness, and 47 % had swelling. The majority (83.9 %) of the patients had a history of blood transfusion, (90.4 %) had a family history of anemia, 92.3 % reported that they receive family support, and 16.7 % reported having chronic disease other than anemia. Of 366 SCD patients, 75 (18.2 %) had their spleen removed.
Bivariate analyses
The bivariate impacts of patients’ characteristics on SF-36 subscales are presented in (Tables 2 and 3). The average physical function score was 55.1 (SD = 23.3). Unemployed patients had a significantly lower physical function than employed patients, as did patients who had a history of skin redness, swelling, and blood transfusions. Patients had a mean physical role function of 35.9 (SD = 36). Table 2 displays the bivariate associations between patients’ characteristics and physical role functions. Patients with a university degree had better physical role function than in patients with no university degree. Conversely, physical role function was considerably worse among patients with fever, skin redness, swelling, and history of blood transfusion. The mean emotional role function of patients was 40.1 (SD = 40.5). The emotional role function was considerably worse in those with fever and swelling. The vitality component had a mean of 47.8 (SD = 19.1). Vitality scores were somewhat higher for patients with a university degree. Unemployed patients had significantly poorer vitality. Furthermore, patients with fever, skin redness, swelling, history of blood transfusion, presence of other chronic diseases, and no regular exercise had poorer scores in vitality.
The mean of emotional wellbeing was 59.3 (SD = 19.4). Patients with a university degree had significantly better emotional wellbeing than patients with no university degree. Our bivariate analyses identified fever, skin redness, swelling, no regular exercise, and the presence of other chronic diseases as demonstrating significantly poorer emotional wellbeing. The mean social function component was 60.1 (SD = 25). Patients with a university degree had significantly better social function than patients with no university degree. The clinical predictors that were significantly associated with reduced social function were fever, skin redness, swelling, blood transfusion, and presence of chronic disease other than SCD.
The mean bodily pain domain was 47.9 (SD = 27.6). Bivariate analyses showed that patients who hold a university degree had significantly less pain than patients with no university degree. However, more pain was associated with fever, skin redness, swelling, and history of blood transfusion (see Table 3 and Fig. 1). General health components had a mean of 47.8 (SD = 15.6). Better general health was significantly associated with a university degree. Worse general health was significantly associated with fever, skin redness, swelling, history of blood transfusion, and no regular exercise.
Fig. 1.
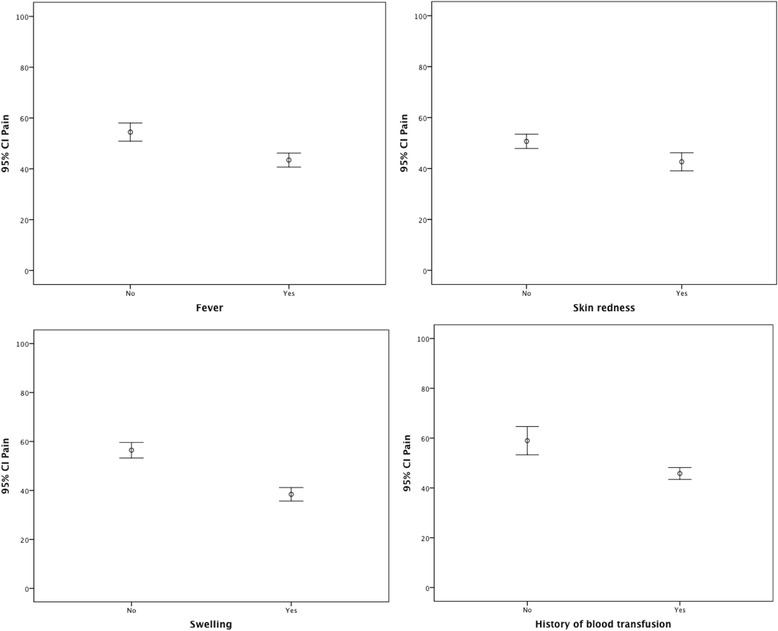
Error bar charts, impact of SCD complications on bodily pain ratings. The higher the score, the less pain
Regression analyses
Table 4 shows the results of the multiple linear regression models. Controlling for all 15 predictors, patients who hold a university degree tend to report higher scores on the physical role function, emotional role function, and vitality relative to patients with no university degree (increase in SF-36 scores of 10.9, 13.9, and 5.3, respectively). Married patients tend to report low scores on vitality, emotional wellbeing, and social functioning (decrease in SF-36 scores of 6.9, 5.2, 6.1, respectively) than unmarried patients. Employed patients tend to report better scores on vitality and pain (increase in SF-36 scores of 7.3 and 6.8, respectively) than unemployed patients.
Based on the multiple linear regression results in Table 4, patients who had a history of blood transfusion tend to have poor physical function, emotional role function, social function, general health, and worse pain, (decrease in SF-36 scores of 6.7, 12.9, 7.4, 5.9, 8.3, respectively) relative to patients who had no history of blood transfusion. Patients with a fever tend to have a negative impact on physical role function and vitality (decrease in SF-36 scores of 8.7 and 6.6, respectively) relative patients with no fever. Patients with swelling tend score less on physical function, vitality, social function, pain, and general health (decrease in SF-36 scores of 8.1, 4.2, 8.4, 14.4, and 4.3, respectively) relative to patients with no swelling. Patients with skin redness tend to have scores on physical function, physical role function, general health that are (decrease in SF-36 scores of 5.7,10.9, and 4.3, respectively) lower than patients with no skin redness. Regular exercise tends to increase vitality, social function, and general health and reduce pain (increase in SF-36 scores of 5.6, 6.1, 5.2, and 7.5, respectively).
Discussion
Research on health-related quality of life among patients with SCD in Saudi Arabia has not received the attention it deserves. Only one study assessed HRQoL in a sample of Saudi adolescents with SCD [13]. The current study represents the first investigation to assess the health-related quality of life in adult Saudi patients with SCD. There are no data about QoL in the Saudi general population to make comparisons with our SCD sample. A study was conducted at King Khalid University to describe the QoL among university students [21]. The university students demonstrated significantly better physical functioning (79.37 vs. 55.1) and general health (70.47 vs. 47.8) as compared with our SCD patients. Surprisingly, the bodily pain among the university students was even worse as compared with SCD patients (38.47 vs. 47.9) in our sample. However, a university sample is not the most appropriate sample to represent the general population.
A study from the United States [1] reported that the average bodily pain among patients with SCD was 47.4 which was consistent with our study (47.9). Saudi adolescents with SCD reported worse bodily pain compared to adults with SCD studied (33.74 [13] vs. 47.9 in the current investigation and 47.4 in McClish et al., [1]). Also, Saudi adolescents with SCD reported poorer social functioning than adults with SCD (44.73 [13] vs. 61.1 in the current investigation and 63.5 in McClish et al., [1]). This indicates that the impact of SCD on pain and social functioning for adolescents tended to be greater than that of adults. Previous study found that there were significant differences in QoL between men and women with SCD [1, 13, 21]. According to our study we found that men and women did not differ in any of the eight perceived health domains. There was no evidence of difference in HRQoL between young and old age groups. The current study revealed that HRQoL among SCD patients was observed significantly better among patients with a university degree as compared to patients with no university degree.
In our study, the most common clinical conditions observed in patients with SCD were fever, presented in (59.7 %) of the sample, history of blood transfusion (83.9 %), and family history of anemia (90.4 %). The bivariate analyses revealed that clinical conditions such as fever, skin redness, swelling, and history of blood transfusion were significant predictors of several perceived health domains. These clinical conditions tend to worsen SCD patient quality of life.
The results of multiple linear regression confirmed that swelling was negatively related to physical function, vitality, social function, bodily pain, and general health, whereas having a university degree was positively related with physical role function, emotional role function, and vitality. Regular exercise positively impacted general health, bodily pain, social functioning, and vitality.
The current study has highlighted certain factors that are necessary to manage in order to deal with the pain and improve QoL in patients with SCD. The research emphasizes the importance of regular exercise habits to control the disease burden by developing physical exercise/ training programs for people living with SCD. Proper education about the disease will play a major role in helping families understand what their patient is going through. It is essential to assess SCD patients’ QoL to effectively manage the physical pain caused by the disease. The presence of signs, symptoms, or complications of SCD seems to have a negative impact on QoL among Saudi SCD patients. We observed worse pain, physical function, and social function in Saudi SCD patients with skin redness or swelling. It is important for hematologists to evaluate patients’ QoL as part of the treatment and management of SCD. Our study suggests screening for SCD complications among patients with SCD and providing appropriate counseling to avoid worse health outcomes.
Interventional studies, such as one to assess the role of regular exercise to prevent poor QoL related to SCD, are needed. It is essential for the public as well as a patient’s close family and relatives to know that, although SCD is a serious condition, those with the disease can essentially lead fairly normal lives provided that they follow a regular exercise program. Several limitations were noted in our study. This is an observational study and only shows correlations, but that doesn’t necessarily imply causation. The comparison with the averages reported from other studies must to be taken with caution, given the different methodological issues and the subjectivity of the surveys. However, this is the first study in terms of assessing health-related quality of life among adult patients with SCD in Saudi Arabia and the entire Arabic world. The results of the study may be useful not only to SCD patients but also to physicians who assess signs or symptoms for these patients in their medical practice.
Conclusion
Regular clinical symptoms checks are important. Clinical symptoms such as fever, skin redness, swelling, and history of blood transfusion had considerable negative impact on several SF-36 domains. Regular exercise tends to lower pain and improves social functions and vitality. Interventional study is needed to evaluate the effectiveness of exercise on quality of life outcomes and pain management in SCD patients.
Acknowledgments
The authors would like to thank the Ministry of Health, Kingdom of Saudi Arabia for approving this study. The authors would also like to thank King Abdullah International Medical Research Center for approving and funding this research. The authors extend their sincere appreciation to the respondents for their participation in this study. The authors also acknowledge the efforts of Huda Salman Abdulla Al-Salman, Zakaria Ali Sharidah, Anas Walid Alhakim, Asim Mohamed Walid Mohamed Aldorrah, and Omar Abdulaziz who have been involved in collecting the data for this study.
Footnotes
Competing interests
The authors declare they have no competing interests.
Authors’ contributions
AEA and DKM involved in the design of the study, conducted the statistical analysis, and wrote the manuscript. ASA, AMA, AJ, MA, and HM involved in the design of the study and helped edit the manuscript. YZA, MAM, AOG, MEE, and WEE participated in the coordination of the study and helped with subject recruitment. All authors read and approved the final manuscript.
Contributor Information
Anwar E. Ahmed, Email: ahmeda5@vcu.edu
Ahmed S. Alaskar, Email: askaras@ngha.med.sa
Ahmad M. Al-Suliman, Email: Ahmed_suliman_sulimanm@yahoo.com
Abdul-Rahman Jazieh, Email: jazieha@ngha.med.sa.
Donna K. McClish, Email: mcclish@vcu.edu
Majid Al Salamah, Email: malsalamah@gmail.com.
Yosra Z. Ali, Email: aliyo@ngha.med.sa
Hafiz Malhan, Email: dr-hafiz@hotmail.com.
May Anne Mendoza, Email: mendozama2@NGHA.MED.SA.
Abdulrahman O. Gorashi, Email: drabusabah@yahoo.com
Mohamed E. El-toum, Email: eltomm@ksau-hs.edu.sa
Wala E. El-toum, Email: wallo222@hotmail.com
References
- 1.McClish DK, Penberthy LT, Bovbjerg VE, Roberts JD, Aisiku IP, et al. Health related quality of life in sickle cell patients: The PiSCES Project. Health Qual Life Outcomes. 2005;3:50. doi: 10.1186/1477-7525-3-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anie KA. Psychological complications in sickle cell disease. Br J Haematol. 2005;129:723–729. doi: 10.1111/j.1365-2141.2005.05500.x. [DOI] [PubMed] [Google Scholar]
- 3.Bhagat VM, Baviskar SR, Mudey AB, Goyal RC. Poor health related quality of life among patients of sickle cell disease. Indian J Palliat Care. 2014;20(2):107–11. doi: 10.4103/0973-1075.132622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann-Jiles V, Morris DL. Quality of life of adult patients with sickle cell disease. J Am Acad Nurse Pract. 2009;21:340–349. doi: 10.1111/j.1745-7599.2009.00416.x. [DOI] [PubMed] [Google Scholar]
- 5.Midence K, Elander J. Adjustment and coping in adults with sickle cell disease: an assessment of research evidence. Br J Health Psychol. 1996;1:95–111. doi: 10.1111/j.2044-8287.1996.tb00495.x. [DOI] [Google Scholar]
- 6.Ohaeri JU, Shokunbi WA, Akinlade KS, Dare LO. The psychosocial problems of sickle cell disease sufferers and their methods of coping. Soc Sci Med. 1995;40:955–60. doi: 10.1016/0277-9536(94)00154-L. [DOI] [PubMed] [Google Scholar]
- 7.Spieth L, Harris C. Assessment of health related quality of life in children and adolescents: an integrative review. J Pediatr Psychol. 1996;21(2):175–93. doi: 10.1093/jpepsy/21.2.175. [DOI] [PubMed] [Google Scholar]
- 8.Strickland OL, Jackson G, Gilead M, Mcguire DB, Quarles S. Use of focus groups for pain and quality of life assessment in adults with sickle cell disease. J Natl Black Nurses Assoc. 2001;12:36–43. [PubMed] [Google Scholar]
- 9.Anie KA, Steptoe A, Bevan DH. Sickle cell disease: Pain, coping and quality of life in a study of adults in the UK. Br J Health Psychol. 2002;7:331–44. doi: 10.1348/135910702760213715. [DOI] [PubMed] [Google Scholar]
- 10.Trzepacz A, Vannatta K, Gerhardt C, Ramey C, Noll R. Emotional, social, and behavioral functioning of children with sickle cell disease and comparison peers. J Pediatr Hematol Oncol. 2004;26(10):642–8. doi: 10.1097/01.mph.0000139456.12036.8d. [DOI] [PubMed] [Google Scholar]
- 11.Panepinto JA, O'Mahar KM, DeBaun MR, Loberiza FR, Scott JP. Health-related quality of life in children with sickle cell disease: child and parent perception. Br J Haematol. 2005;130(3):437–44. doi: 10.1111/j.1365-2141.2005.05622.x. [DOI] [PubMed] [Google Scholar]
- 12.Dampier C, Lieff S, LeBeau P, Rhee S, McMurray M, Rogers Z, et al. Health-related quality of life in children with sickle cell disease: a report from the Comprehensive Sickle Cell Centers Clinical Trial Consortium. Pediatr Blood Cancer. 2010;55(3):485–494. doi: 10.1002/pbc.22497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdel-Monhem Amr M, Tawfik AT, Al-Omair AO. Health related quality of life among adolescents with sickle cell disease in Saudi Arabia. Pan Afr Med J. 2011;8:10. doi: 10.4314/pamj.v8i1.71057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alabdulaali MK. Sickle cell disease patients in eastern province of Saudi Arabia suffer less severe acute chest syndrome than patients with African haplotypes. Annals of Thoracic Medicine. 2007;2(4):158–162. doi: 10.4103/1817-1737.36550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohsen E-H. Heterogeneity and variation of clinical and hematological expression of hemoglobin S in Saudi Arabs. Acta Haematolo. 1992;88:67–71. doi: 10.1159/000204654. [DOI] [PubMed] [Google Scholar]
- 16.Muldoon MF, Barger SD, Flory JD, Manuck SB. What are quality of life measurements measuring? BMJ. 1998;316(7130):542–545. doi: 10.1136/bmj.316.7130.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asnani MR, Reid ME, Ali SB, Lipps G, Williams-Green P. Quality of life in patients with sickle cell disease in Jamaica: rural-urban differences. Rural Remote Health. 2008;8:890. [PubMed] [Google Scholar]
- 18.Wright K, Adeosum O. Barriers to effective pain management in sickle cell disease. Br J Nurs. 2009;18(3):158–161. doi: 10.12968/bjon.2009.18.3.39043. [DOI] [PubMed] [Google Scholar]
- 19.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) Med Care. 1992;30(6):473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Coons SJ, Alabdulmohsin SA, Draugalis JR, Hays RD. Reliability of an Arabic Version of the RAND 36-Item Health Survey and its Equivalence to the US-English Version. Med Care. 1998;36:428–432. doi: 10.1097/00005650-199803000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Megahed MM. Health-Related Quality of Life among Students at King Khalid University – Mohail Asser. Int J Nurs Sci. 2014;4(2):22–25. [Google Scholar]


