Abstract
Background
Widal test, which has poor predictive outcomes in predominant typhoid population, is not standard enough to predict accurate diagnosis. This study aims to compare the diagnostic accuracy of Widal test to ELISA using blood culture as gold standard.
Methods
The blood samples were collected in Capital Hospital, Kathmandu, Nepal from febrile patients having ≥48 h fever in 3 years study period for blood culture, Widal test and IgG-IgM ELISA.
Results
Amongst 1371 febrile cases, 237 were Salmonella typhi positive to blood culture and 71.4 % typhoid fever patient were of 46–60 years old with male to female ratio of 2:1. Blood culture confirmed patients had ≥1:40 anti-TH and anti-TO titre in 45.56 % (n = 108) and 43.88 % (n = 104) patients respectively. The sensitivity and specificity of IgG (0.96 and 0.95) and IgM (0.95 and 0.94) at 95 % confidence level were significant compared to Widal anti-TH (0.72 and 0.58) and TO (0.80 and 0.51) test (p value, 0.038) at titre level ≥1:200. Further the PPV of Widal TH and TO (0.38 and 0.23) was low compared to IgG and IgM ELISA (0.78 and 0.77) (p value, 0.045).
Conclusion
Widal test is not sensitive enough for an endemic setting like Nepal and thus should be either replaced with more accurate test like ELISA or follow an alternative diagnostic methodology.
Keywords: Typhoid Fever, Salmonella typhi, Widal test, ELISA, Sensitivity, Specificity, Nepal
Background
Typhoid fever is becoming a key health problem in developing countries. Lack of safe and clean drinking water supplies to the people and adequate sewage disposal are the major reasons [1]. The fever has been one of the leading diagnosed fever ailment among the fever related caseses in most of the hospitals of Nepal [2]. It is popularly known as ‘Bisham Joro’ in local language meaning the ‘fever with poison’. Typhoid is prevalent in mid-hills, valleys and southern belts as an endemic disease with peak incidence in between April and August [3, 4]. Outbreaks are more common in summer season affecting mainly the children in Kathmandu [5–7]. Diagnosis is done by culture and immunological tests, however, isolation of the etiological agent, the Salmonella enterica (serovar typhi) from bone marrow culture is an ideal gold standard [8]. Invasive procedure and unavailability of culture facilities in rural health centers are chief limiting factors. Besides, the widely used blood culture has poor sensitivity of 40–60 % making room for false negative results to around half of the typhoid patients [9]. In addition, the requirement of 3 days time duration for diagnosis delays the line of treatment loosing applicability of early diagnosis. Further, usage of the antibiotics prior to hospital admittance, which is a common practice in Nepal, cause poor sensitivity to the culture base diagnosis [10]. In spite of the all, blood culture technique is still the gold standard in the febrile cases of typhoid. Routine Widal test is alternatively adopted second most popular choice for diagnosis as blood culture remains controversial due to its biased diagnosis [11]. Enzyme-linked immunosorbent assay (ELISA) based diagnosis has also been studied previously with good diagnostic accuracy [12–15]. This study aims to compare diagnostic accuracy of Widal test and ELISA in febrile patients taking blood culture as gold standard tool for the diagnosis of typhoid fever.
Material and methods
Patients, inclusion/exclusion criteria and data analysis
Patients attending Capital Hospital, a centrally located hospital at Kathmandu, during the months January 2011 to December 2013 with complaint of fever over 72 h without obvious focus of infection and clinical suspicion of typhoid fever (high fever, malaise, headache, constipation or diarrhoea) were prospectively enrolled in this study. Patients were divided into five age groups i.e. 1–15 (children), 16–30 (young), 31–45 (young adults), 46–60 (adults) and >60 years (olds). Pregnant women were excluded from the study. The ELISA and Widal tests were performed by a single specialized clinical researcher who was blind to the patient's diagnosis in reference to standard throughout the study period. The patients with febrile cases were screened when found positive to reference standard (Blood Culture). The control populations with negative blood culture reports were also included in the study, so as to make self evaluation of reference standard. The sample population inclusive of blood culture positive was grouped into five different groups (Fig. 1).
Fig. 1.
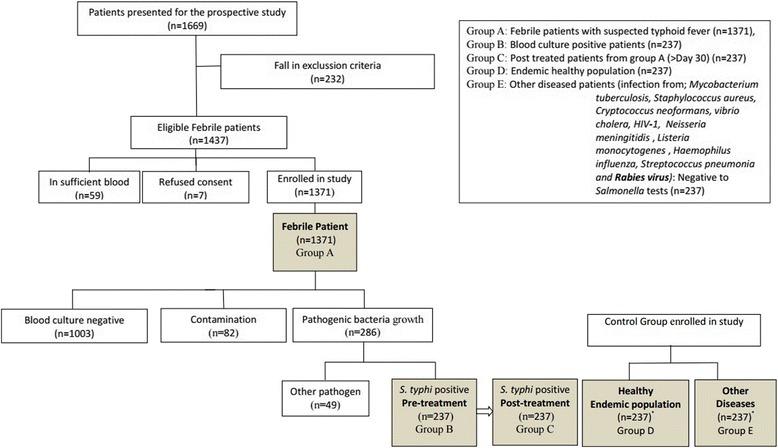
Consort chart for patients in study. Group A: Febrile patients with suspected typhoid fever (n = 1371), Group B: Blood culture positive patients (n = 237), Group C: Post treated patients from group A (>Day 30) (n = 237), Group D: Endemic healthy population (n = 237), Group E: Other diseased patients (infection from; Mycobacterium tuberculosis, Staphylococcus aureus, Cryptococcus neoformans, Vibrio cholera, HIV-1, Neisseria meningitidis, Listeria monocytogenes, Haemophilus influenza, Streptococcus pneumonia and Rabies virus): Negative to Salmonella tests (n = 237)
Blood collection and bacterial culture for pathogen isolation
Blood were collected in BACTEC Peds Plus™/F culture vials and immediately (within 10 min) transferred to laboratory to be loaded in Bactec 9240 (Becton Dickinson, USA) culture instrument for growth. Blood isolates which were found culture positive were reconfirmed for Salmonella by slide agglutination, using monospecific anti sera (Sifin, Germany) as described by the Kauffmann-White scheme [16–18].
Quantitative Widal test
The Widal tube agglutination test was performed using Wellcolex®(Remel, UK) in the group A (n = 1371) as well as for group B, C D and E according to the manufacturer's instructions parallel to the blood culture procedure of individual groups. Briefly, serum remained after keeping for blood culture was diluted in 0.86 % saline solution starting with 1:100. Salmonella ‘O’ and ‘H’ antigens from the standard preparation were added and the tubes were incubated at 37 °C for 1 h. After incubation, the tubes were centrifuged for 5 min, and respective agglutinations were observed. The Widal TO/TH titre were taken as the highest dilution of serum with visible agglutination. The cut off titre set for Salmonella typhi anti O was >1:80 while it was >1:160 for anti H in this study [11].
Enzyme Linked Immunosorbent Assay (ELISA)
Similar to the Widal test, Anti-IgM and anti-IgG sandwich ELISA (MyBioSource, Inc. CA, USA) was done in all the groups. Briefly, 100 μl of coating antigen (1 μg/ml) diluted in antigen coating buffer (Immunochemistry, MN, USA) were dispensed in Nunc-Immuno 96 MicroWell solid plates (Thermo Fisher Scientific, USA) along with negative control (Only coating buffer) according to plan. The plates were incubated at 4 °C overnight and the wells were blocked using 1 % bovine serum albumin (BSA) prepared in phosphate buffer saline (PBS). The plates were washed by 125 μl washing buffer (0.1%BSA with Tween20). Hundred microliter of serially diluted sera (1:200 to 1:3200) in PBS-BSA was dispensed to each well and incubated at 25 °C for 4 h. After washing, 100 μl detector antibody conjugated with horse reddish peroxidase (HRP) was added in dilutions (1:500 anti IgA, 1:5000 anti IgG, 1:2500 anti IgM) and incubated for 30 min at 25 °C. After that, 100 μl trimethyle benzidine (TMB) substrate was added and incubated for 15 min at dark. The reaction was stopped by addition of 1 N H2SO4 to measure optical density (OD) at 450 nm in ELISA plate reader (Bio-Rad). Cut off values were assessed following the mean ± SD of the OD from healthy endemic controls of group D which was 0.3 for IgG and 0.2 for IgM.
Statistical analysis
The positive predictive value is the principle finding of this study which elucidates the efficacy of current diagnostic assays. The sensitivity, specificity and predictive values were calculated as described earlier [19]. Receiver operating Characteristics (ROC) used to establish cut off titre, was determined by plotting specificity (x-axis) versus sensitivity (y-axis) at all tested cut off titres. The highest number of true positive and the lowest false positive results were used to represent cut off values by comparing the points with maximum Youden index (J = maxc [Se (c) + Sp (c) – 1]). Collected data were analyzed and interpreted statistically using graphPad prism version 6.0 and SPSS 17.0. Normal distribution of data sets were analysed by Kolmogorov-Smirnov test. All the values are expressed as mean ± SD and are analyzed using Student’s t test which is parametric as well Mann–Whitney test wherever applicable. A value (p value, <0.05) was considered significant unless stated otherwise. Sensitivity, specificity and predictive values were calculated as described elsewhere [20, 21]
Ethical statement
The study was approved by the Capital Hospital Ethical Review Board (CHRB). The adult participants gave written informed consent while children below 18 year were enrolled only after the written informed consent from their guardian was received.
Results
Demographic and geographical distribution
The 1371 patients, enrolled in the study held between January 2011 and December 2013, had representation from all the three geographical regions of Nepal viz. Mountain, Hill and Terai, as Kathmandu, the capital city, hosts a broad range of people from all over the country. The prevalence of typhoid cases in Terai region was highest (69 %; p value, 0.03) in comparison to mid hill regions around Kathmandu valley (30 %) and the least in mountain region (1.39 %) (Table 1). There were 400 females and 971 males who consented for this study. The infection was found more in males of 16–30 years (median age, 21.5 years) age group with male–female ratio of 2:1, among the positive cases (n = 237) of typhoid as confirmed by blood culture, and was followed by age groups of 1–15, 31–45, 46–60 and >60 year.
Table 1.
Distribution of Typhoid patients according to regions and sex
| Geographical Regions | Patients | ||
|---|---|---|---|
| Male | Female | Total | |
| Terai Region (<2297 ft) | 621 (65.92 %) | 321 (34.07 %) | 942 (68.71 %)* |
| Hill Region (2000–10000 ft) | 340 (82.92 %) | 70 (17.07 %) | 410 (29.91 %) |
| Mountain Region (>10000 ft) | 10 (52.63 %) | 9 (47.36 %) | 19 (1.39 %) |
*p value, <0.05 while comparing the patients from Hill region
Pathogen distribution among febrile cases
Out of 1371 cases, only 237 samples (17.28 %) showed positive growth of S. typhi in the blood culture and 120 patients were admitted in the hospital for treatment. The cultures also had co-infection of Actinobacteria (n = 3, 2.5 %) and Klebsiella pneumonia (n = 2, 1.67 %) in the admitted inpatients of the typhoid fever (Table 2). In 237 patients, Actinobacteria (0.21 %) was found only in male while Klebsiella pneumoniae (0.14 %) were found only in female. Pathogen other than Salmonella was isolated from 49 patients (Fig. 1).
Table 2.
Culture report of S.typhi positive cases and co-infection with other pathogens among inpatient and outpatient of capital hospital
| Inpatients | Outpatients | |
|---|---|---|
| Salmonella typhi | 115 (95.83 %) | 122 (100 %) |
| Actinobacteria | 3 (2.5 %)* | 0 (0 %) |
| Klebsiella pneumonia | 2 (1.67 %)* | 0 (0 %) |
*Co-infection with S.typhi
Clinical symptoms of the disease
Different symptoms were found in the typhoid positive cases. The absolute symptom was fever (100 %; p value, 0.04) however, other major symptoms observed were headache (97.47 %; p value, <0.034), loss of appetite (90.3 %; p value, 0.028) and chill (74.26 %; p value, 0.034). Abdominal discomfort, myalgia, vomiting, constipation, rigor, diarrhea, and dysuria were other symptoms observed in less than half of culture confirmed typhoid patient. Hence, fever, headache and loss of appetite were significant symptoms for the fever ailment (Table 3).
Table 3.
Clinical sign and symptoms distribution
| S.N. | Symptom expressed by patient | Salmonella typhi (n) | Percentage |
|---|---|---|---|
| 1 | Fever | 237 | 100.00 |
| 2 | Headache | 231 | 97.47 |
| 3 | Loss of appetite | 214 | 90.30 |
| 4 | Chills | 176 | 74.26 |
| 5 | Abdominal Discomfort | 109 | 45.99 |
| 6 | Myalgia | 99 | 41.77 |
| 7 | Vomiting | 89 | 37.55 |
| 8 | Constipation | 64 | 27.00 |
| 9 | Rigor | 55 | 23.21 |
| 10 | Diarrhea | 45 | 18.99 |
| 11 | Dysuria | 42 | 17.72 |
Qualitative slide agglutination Widal test
Widal test used as the primary screening assay by typing O and H antigen of Salmonella showed overall positivity rate of 21.74 % and 22.68 % respectively at the titre ≥1:40. (Table 4). Among culture confirmed patients, group A (n = 237), the number of TH (n = 108) and TO (n = 104) positive at titre ≥1:40 was significantly lower (p value, 0.04) than from the culture negative patients (n = 1134) group. Though blood culture showed negative to typhoid test, Widal test was found positive to TH antigen (n = 203, 17.92 %) and TO antigen (n = 194, 17.11 %) test at same titre (Table 4).
Table 4.
Number of anti TH and anti TO levels in blood isloates
| Titration Record | Total Patients (n = 1371) | Culture positive patients (n = 237) | Culture negative patients (n = 1134) |
|---|---|---|---|
| Anti TH | |||
| Aggutinition | 311 (22.68 %) | 108 (45.57 %) | 203 (17.92 %) |
| ≥1:640 | 78 (25.08 %) | 36 (33.33 %) | 42 (20.69 %) |
| 1:320 | 156 (50.16 %) | 55 (50.93 %) | 101 (49.75 %) |
| 1:160 | 176 (56.59 %) | 89 (82.41 %) | 87 (42.86 %) |
| 1:80 | 201 (64.63 %) | 98 (90.74 %) | 103 (50.74 %) |
| 1:40 | 311 (100 %) | 108 (100 %) | 203 (100 %) |
| No Agglutination | 1060 (77.32 %) | 129 (54.43) | 931 (82.14 %) |
| Anti TO | |||
| Aggutinition | 298 (21.74 %) | 104 (43.88 %) | 194 (17.11 %) |
| ≥1:640 | 71 (23.83 %) | 29 (27.88 %) | 42 (21.65 %) |
| 1:320 | 147 (49.33 %) | 45 (43.27 %) | 102 (52.58 %) |
| 1:160 | 164 (55.03 %) | 84 (80.77 %) | 80 (41.24 %) |
| 1:80 | 198 (66.44 %) | 91 (87.5 %) | 107 (55.15 %) |
| 1:40 | 298 (100 %) | 104 (100 %) | 194 (100 %) |
| No Agglutination | 1073 (78.26 %) | 133 (56.12 %) | 940 (82.89 %) |
Assessment of ELISA for the diagnosis of typhoid fever
The OD value for IgM in the culture confirmed group B (n = 237) was significantly higher (p value, 0.041) than that of control groups C, D and E. There was no significant difference between the control groups D and E (p value, 0.039). Titre value of 3200 for IgM and 200 for IgG, was observed for group B patients (193 of 237) only after ≥3 days of reported fever case, which were undetectable in initial 3 days of feverish condition. Patients of group C (n = 237), who were enrolled in medication and recovered, showed significant level of serum IgG (p value, 0.046) but not IgM, when compared to previous data from same patients before medication. For the endemic healthy group D (n = 237), the titre for IgG was 400 but with no significant IgM titre value. In case of other disease patients of group E (without Salmonella but other infections), the ELISA results were negative for both Salmonella anti IgM and IgG (Fig. 2). Serology based typhoid diagnostic tests using sera from the culture confirmed typhoid patients and the control subjects showed that both IgG and IgM based ELISA tests were superior to the Widal TH and TO tests. When sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of ELISA was compared among group A (n = 1371) patients against Widal test, ELISA (IgG/IgM) had higher PPV at ≥1:400 (Table 5). The IgM/IgG titre ≥1:200 had a high sensitivity (95.50 %/96.85 %) and specificity (94.69 %/94.95 %). The diagnostic sensitivity of Widal TO test at titre ≥1/400 was 84.09 % and specificity was 52.65 %. There was a significant difference between case definition for suspected and probable cases of typhoid fever (Table 6).
Fig. 2.

IgG and IgM occurrence in group B, C, D and E
Table 5.
Sensitivity, Specificity, PPV and NPV for typhoid fever of ELISA and Widal test in different cut off titers
| Test | Titer | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| 95 % CI | 95 % CI | 95 % CI | 95 % CI | ||
| IgM | ≥1:200 | 95.50 % | 94.69 % | 77.66 % | 99.09 % |
| 91.87 % to 97.82 % | 93.23 % to 95.92 % | 72.24 % to 82.46 % | 98.33 % to 99.56 % | ||
| ≥1:400 | 81.23 % | 98.29 % | 91.77 % | 95.70 % | |
| 75.95 % to 85.78 % | 97.34 % to 98.97 % | 87.45 % to 94.98 % | 94.36 % to 96.80 % | ||
| ≥1:800 | 61.97 % | 96.48 % | 78.38 % | 92.50 % | |
| 55.41 % to 68.21 % | 95.24 % to 97.48 % | 71.74 % to 84.08 % | 90.85 % to 93.93 % | ||
| ≥1:1600 | 51.89 % | 93.79 % | 60.44 % | 91.42 % | |
| 44.94 % to 58.78 % | 92.24 % to 95.11 % | 52.94 % to 67.60 % | 89.68 % to 92.95 % | ||
| ≥1:3200 | 47.44 % | 92.73 % | 54.84 % | 90.46 % | |
| 40.61 % to 54.34 % | 91.08 % to 94.16 % | 47.39 % to 62.13 % | 88.65 % to 92.08 % | ||
| IgG | ≥1:200 | 96.85 % | 94.95 % | 78.75 % | 99.36 % |
| 93.61 % to 98.72 % | 93.52 % to 96.14 % | 73.42 % to 83.45 % | 98.69 % to 99.74 % | ||
| ≥1:400 | 85.95 % | 98.76 % | 93.69 %** | 97.04 % | |
| 80.92 % to 90.07 % | 97.93 % to 99.32 % | 89.65 % to 96.51 % | 95.89 % to 97.94 % | ||
| ≥1:800 | 62.61 % | 97.09 % | 81.87 % | 92.51 % | |
| 56.12 % to 68.77 % | 95.93 % to 97.99 % | 75.49 % to 87.18 % | 90.87 % to 93.95 % | ||
| ≥1:1600 | 51.89 % | 94.48 % | 63.22 % | 91.48 % | |
| 44.94 % to 58.78 % | 93.00 % to 95.72 % | 55.59 % to 70.39 % | 89.75 % to 93.00 % | ||
| ≥1:3200 | 47.44 % | 92.73 % | 54.84 % | 90.46 % | |
| 40.61 % to 54.34 % | 91.08 % to 94.16 % | 47.39 % to 62.13 % | 88.65 % to 92.08 % | ||
| TO | ≥1:100 | 90.32 % | 52.41 % | 44.22 % | 92.12 % |
| 87.25 % to 92.47 % | 49.10 % to 53.91 % | 41.18 % to 50.73 % | 88.71 % to 94.83 % | ||
| ≥1:200 | 80.95 % | 51.77 % | 23.29 % | 93.76 % | |
| 74.98 % to 86.03 % | 48.85 % to 54.68 % | 20.27 % to 26.53 % | 91.60 % to 95.50 % | ||
| ≥1:400 | 84.09 % | 52.65 % | 25.34 % | 94.54 % | |
| 78.58 % to 88.66 % | 49.72 % to 55.57 % | 22.22 % to 28.66 % | 92.49 % to 96.17 % | ||
| TH | ≥1:100 | 80.32 % | 53.22 % | 48.40 % | 90.87 % |
| 75.28 % to 85.91 % | 46.42 % to 55.36 % | 42.83 % to 50.27 % | 87.14 % to 92.84 % | ||
| ≥1:200 | 72.23 % | 58.33 % | 38.13 % | 89.37 % | |
| 68.24 % to 79.72 % | 52.93 % to 64.22 % | 31.23 % to 43.10 % | 83.11 % to 94.07 % | ||
| ≥1:400 | 62.47 % | 55.23 % | 39.48 % | 90.62 % | |
| 59.23 % to 66.82 % | 47.21 % to 59.99 % | 31.34 % to 45.83 % | 86.92 % to 95.27 % |
**Highest PPV value
Table 6.
Sensitivity, specificity, PPV and NPV for typhoid fever of WHO case definition
| Suspected case of Typhoid fever | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| 95 % CI | 95 % CI | 95 % CI | 95 % CI | |
| Isolation in Blood culture of; | ||||
| S. typhi | 76.81 % | 99.22 % | 97.07 % | 92.71 % |
| 71.99 % to 81.16 % | 98.47 % to 99.66 % | 94.31 % to 98.73 % | 91.01 % to 94.18 % | |
| Probable case of Typhoid fever | ||||
| TH(1:160) | 45.22 % | 82.32 % | 34.23 % | 87.83 % |
| 41.27 % to 49.17 % | 79.91 % to 87.82 % | 29.46 % to 38.96 % | 81.59 % to 91.31 % | |
| TO(1:80) | 43.45 % | 82.31 % | 34.11 % | 87.14 % |
| 39.29 % to 48.97 % | 78.96 % to 84.78 % | 31.41 % to 38.85 % | 83.72 % to 92.91 % | |
Discussion
Typhoid is a major public health problem in third world countries [1,2]. In Nepal, typhoid fever is endemic and the major factors for high prevalence rate include, but are not limited to, illiteracy, poverty, poor sanitation and inadequate facilities for safe drinking water supply. The Widal test based on TO and TH titre values were observed higher in healthy subjects relating to the endemic setting of typhoid fever in Nepal. Even the typhoid relapsed subject group B had significant titre value of TH ≥1:160, describing the persistent anti H in blood sample [11] which also had higher serum IgG but lower IgM antibodies suggesting the late class switching from IgM to IgG in response to the infection well after elimination of pathogen [22]. The sensitivity and specificity of the IgG/IgM ELISA were higher than that of Widal test showing Widal’s incompetence in accurate diagnosis. The cut off titre is more in developing countries compared to developed countries due to sanitary and endemic reasons [23], thus the titre value from Widal test is not accurate enough to picture the complete diagnosis, since the PPV value of TO and TH were too low (0.44 and 0.48 respectively). In developing country like Nepal, the haphazard usage of antibiotic is common thus providing false negative in blood culture, though there were no patients who admitted taking antibiotic within two weeks before enrollment in this study. The false negative Widal test results were probably due to early blood collection before the adequate antibody production [24]. In case of Widal test, which when compared with the WHO case definition, didn’t perform well. The sensitivity dropped by >40 % compared to gold standard blood culture showing that Widal test alone can’t be used as diagnostic approach, though is widely used in rural setting in Nepal till date.
Conclusion
Higher titer value was observed in healthy endemic population which showed that typhoid diagnosis is biased when Widal test is used alone; however ELISA had more stringent data thus resulting a clear distinction of antibody production against salmonella, and making differential diagnosis more accurate among febrile cases. This findings also suggest implementing ELISA on daily routine diagnosis of typhoid fever especially in endemic typhoid area like Nepal.
Acknowledgement
The authors would like to thank the technical staff of Capital Hospital for their contribution in the study and National Aayurveda Training and Research Center (NATRC) as well University Grant Commission (UGC) for providing partial grants in support of this research.
Abbreviations
- BACTEC
Bactenecin
- ELISA
Enzyme Linked Immunosorbent Assay
- Peds
Pediatrics
- TH
Titer of Salmonella H- Flagellar antigen
- TO
Titer of Salmonella H- Somatic antigen
- BSA
Bovine Serum Albumin
- PBS
Phosphate Buffer Saline
- HRP
Horse Reddish Peroxidase
- TMB
Trimethyle Benzidine
- OD
Optical Density
- SD
Standard Deviation
- ROC
Receiver Operating Characteristics
- CHRB
Capital Hospital Ethical Review Board
- PPV
Positive Predictive Value
- NPV
Negative Predictive Value
- NATRC
Aayurveda Training and Research Center
- UGC
University Grant Commission
Footnotes
Competing interests
The authors declare that they have no competing interests.
Author contributions
BPG, AA and RR designed the experiment. BPG, AA, RR, KDM performed the research study. BPG, AA, RR, PPR & KDM analyzed the data. BPG, AA, PPR & KDM wrote the manuscript. All authors have read and approved the final version of the manuscript.
Contributor Information
Anurag Adhikari, Email: adhikari_anurag13@yahoo.com.
Ramanuj Rauniyar, Email: rauniyarr23@gmail.com.
Pramod Prasad Raut, Email: Raut588inj@yahoo.com.
Krishna Das Manandhar, Email: krishna.manandhar@gmail.com.
Birendra Prasad Gupta, Email: birendraphd@gmail.com.
References
- 1.Crump JA, Mintz ED. Global trends in typhoid and paratyphoid fever. Clin Infect Dis. 2010;50(2):241–246. doi: 10.1086/649541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raza S, Tamrakar R, Bhatt CP, Joshi SK. Antimicrobial susceptibility patterns of Salmonella typhi and Salmonella paratyphi A in a tertiary care hospital. J Nepal Health Res Counc. 2012;10(22):214–217. [PubMed] [Google Scholar]
- 3.Prajapati B, Rai GK, Rai SK, Upreti HC, Thapa M, Singh G, et al. Prevalence of Salmonella typhi and paratyphi infection in children: a hospital based study. Nepal Med Coll J. 2008;10(4):238–241. [PubMed] [Google Scholar]
- 4.Sharma NP, Peacock SJ, Phumratanaprapin W, Day N, White N, Pukrittayakamee S. A hospital-based study of bloodstream infections in febrile patients in Dhulikhel Hospital Kathmandu University Teaching Hospital, Nepal. Southeast Asian J Trop Med Public Health. 2006;37(2):351–356. [PubMed] [Google Scholar]
- 5.Karkey A, Thompson CN, Tran Vu Thieu N, Dongol S, Le Thi PT, Voong Vinh P, et al. Differential epidemiology of Salmonella Typhi and Paratyphi A in Kathmandu, Nepal: a matched case control investigation in a highly endemic enteric fever setting. PLoS Negl Trop Dis. 2013;7(8):e2391. doi: 10.1371/journal.pntd.0002391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karki S, Shakya P, Cheng AC, Dumre SP, Leder K. Trends of etiology and drug resistance in enteric fever in the last two decades in Nepal: a systematic review and meta-analysis. Clin Infect Dis. 2013;57(10):e167–176. doi: 10.1093/cid/cit563. [DOI] [PubMed] [Google Scholar]
- 7.Charles RC, Sultana T, Alam MM, Yu Y, Wu-Freeman Y, Bufano MK, et al. Identification of immunogenic Salmonella enterica serotype Typhi antigens expressed in chronic biliary carriers of S. Typhi in Kathmandu, Nepal. PLoS Negl Trop Dis. 2013;7(8):e2335. doi: 10.1371/journal.pntd.0002335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parry CM, Wijedoru L, Arjyal A, Baker S. The utility of diagnostic tests for enteric fever in endemic locations. Expert Rev Anti Infect Ther. 2011;9(6):711–725. doi: 10.1586/eri.11.47. [DOI] [PubMed] [Google Scholar]
- 9.Fadeel MA, House BL, Wasfy MM, Klena JD, Habashy EE, Said MM, et al. Evaluation of a newly developed ELISA against Widal, TUBEX-TF and Typhidot for typhoid fever surveillance. J Infect Dev Ctries. 2011;5(3):169–175. doi: 10.3855/jidc.1339. [DOI] [PubMed] [Google Scholar]
- 10.Malla T, Malla KK, Thapalial A, Shaw C. Enteric fever: a retrospective 6-year analysis of 82 paediatric cases in a teaching hospital. Kathmandu Univ Med J (KUMJ) 2007;5(2):181–187. [PubMed] [Google Scholar]
- 11.Pokhrel BM, Karmacharya R, Mishra SK, Koirala J. Distribution of antibody titer against Salmonella enterica among healthy individuals in nepal. Ann Clin Microbiol Antimicrob. 2009;8:1. doi: 10.1186/1476-0711-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaka-ur-Rab Z, Abqari S, Shahab T, Islam N, Shukla I. Evaluation of salivary anti-Salmonella typhi lipopolysaccharide IgA ELISA for serodiagnosis of typhoid fever in children. Arch Dis Child. 2012;97(3):236–238. doi: 10.1136/adc.2011.300622. [DOI] [PubMed] [Google Scholar]
- 13.Fadeel MA, House BL, Wasfy MM, Klena JD, Habashy EE, Said MM, Maksoud MA, Rahman BA, Pimentel G: Evaluation of a newly developed ELISA against Widal, TUBEX-TF and Typhidot for typhoid fever surveillance. In.: DTIC Document; 2011 [DOI] [PubMed]
- 14.Parry CM, Wijedoru L, Arjyal A, Baker S. The utility of diagnostic tests for enteric fever in endemic locations. Expert Rev Anti Infect Ther. 2011;9(6):711–25. doi: 10.1586/eri.11.47. [DOI] [PubMed] [Google Scholar]
- 15.Quang NN, Tapchaisri P, Chongsa-nguan M, Van Vien C, Tra DT, Sakolvaree Y, et al. Diagnosis of enteric fever caused by Salmonella spp. in Vietnam by a monoclonal antibody-based dot-blot ELISA. Asian Pac J Allergy Immunol. 2011;15(4):205–12. [PubMed] [Google Scholar]
- 16.Brenner FW, Villar RG, Angulo FJ, Tauxe R, Swaminathan B. Salmonella nomenclature. J Clin Microbiol. 2000;38(7):2465–2467. doi: 10.1128/jcm.38.7.2465-2467.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Euzeby JP JP. Revised Salmonella nomenclature: designation of Salmonella enterica (ex Kauffmann and Edwards 1952, Le Minor and Popoff 1987 sp. nov., nom. rev. as the neotype species of the genus Salmonella Lignieres 1900 (approved lists 1980), rejection of the name Salmonella choleraesuis (Smith 1894) Weldin 1927 (approved lists 1980), and conservation of the name Salmonella typhi (Schroeter 1886) Warren and Scott 1930 (approved lists 1980). Request for an opinion. Int J Syst Bacteriol. 1999;49(Pt 2):927–930. doi: 10.1099/00207713-49-2-927. [DOI] [PubMed] [Google Scholar]
- 18.Popoff MY, Bockemuhl J, Brenner FW. Supplement 1998 (no. 42) to the Kauffmann-White scheme. Res Microbiol 2000. 1998;151(1):63–65. doi: 10.1016/s0923-2508(00)00126-1. [DOI] [PubMed] [Google Scholar]
- 19.Florkowski CM. Sensitivity, specificity, receiver-operating characteristic (ROC) curves and likelihood ratios: communicating the performance of diagnostic tests. Clin Biochem Rev. 2008;29(Suppl 1):S83–87. [PMC free article] [PubMed] [Google Scholar]
- 20.Stojanovic M, Andjelkovic Apostolovic M, Stojanovic D, Milosevic Z, Ignjatovic A, Lakusic VM, et al. Understanding sensitivity, specificity and predictive values. Vojnosanit Pregl. 2014;71(11):1062–1065. doi: 10.2298/VSP1411062S. [DOI] [PubMed] [Google Scholar]
- 21.Parikh R, Mathai A, Parikh S, Chandra Sekhar G, Thomas R. Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol. 2008;56(1):45–50. doi: 10.4103/0301-4738.37595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liang L, Juarez S, Nga TV, Dunstan S, Nakajima-Sasaki R, Davies DH, et al. Immune profiling with a Salmonella Typhi antigen microarray identifies new diagnostic biomarkers of human typhoid. Sci Rep. 2013;3:1043. doi: 10.1038/srep01043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chew SK, Cruz MS, Lim YS, Monteiro EH. Diagnostic value of the Widal test for typhoid fever in Singapore. J Trop Med Hyg. 1992;95(4):288–291. [PubMed] [Google Scholar]
- 24.Olopoenia LA, King AL. Widal agglutination test - 100 years later: still plagued by controversy. Postgrad Med J. 2000;76(892):80–84. doi: 10.1136/pmj.76.892.80. [DOI] [PMC free article] [PubMed] [Google Scholar]


