Abstract
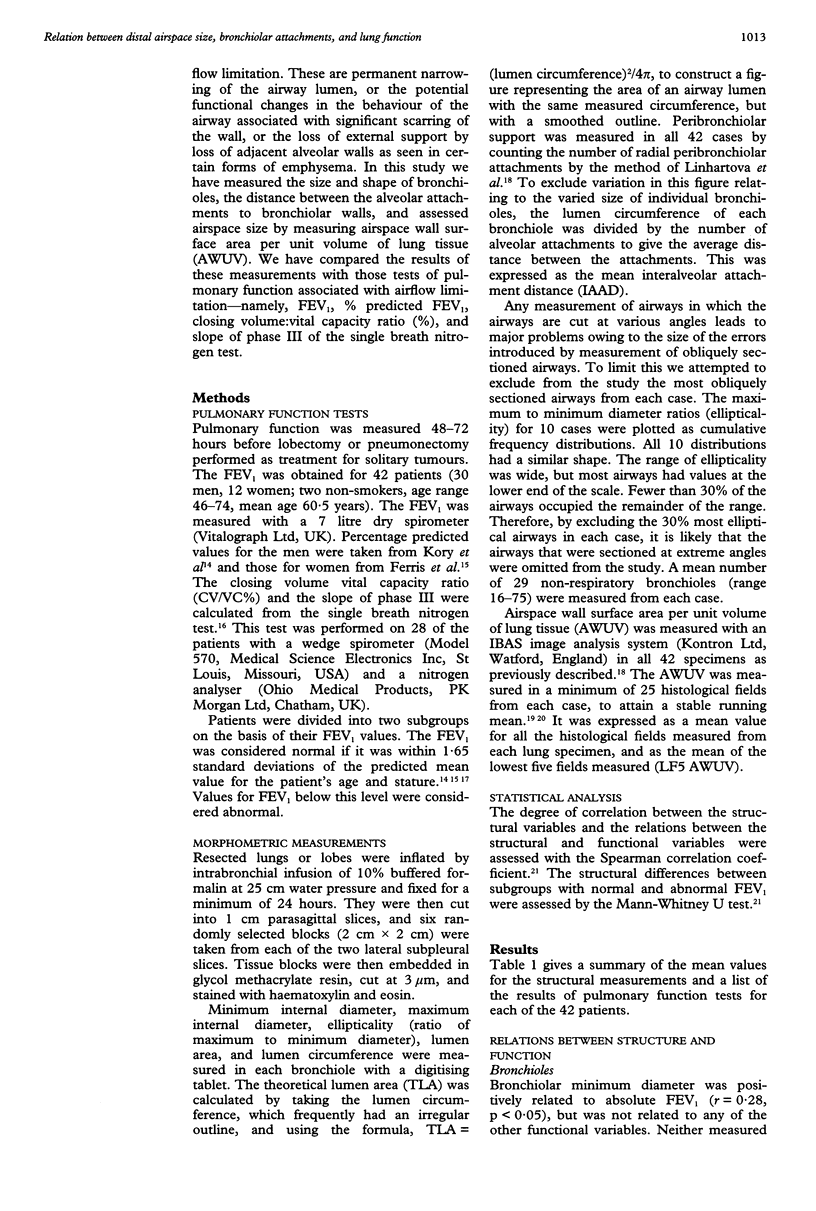
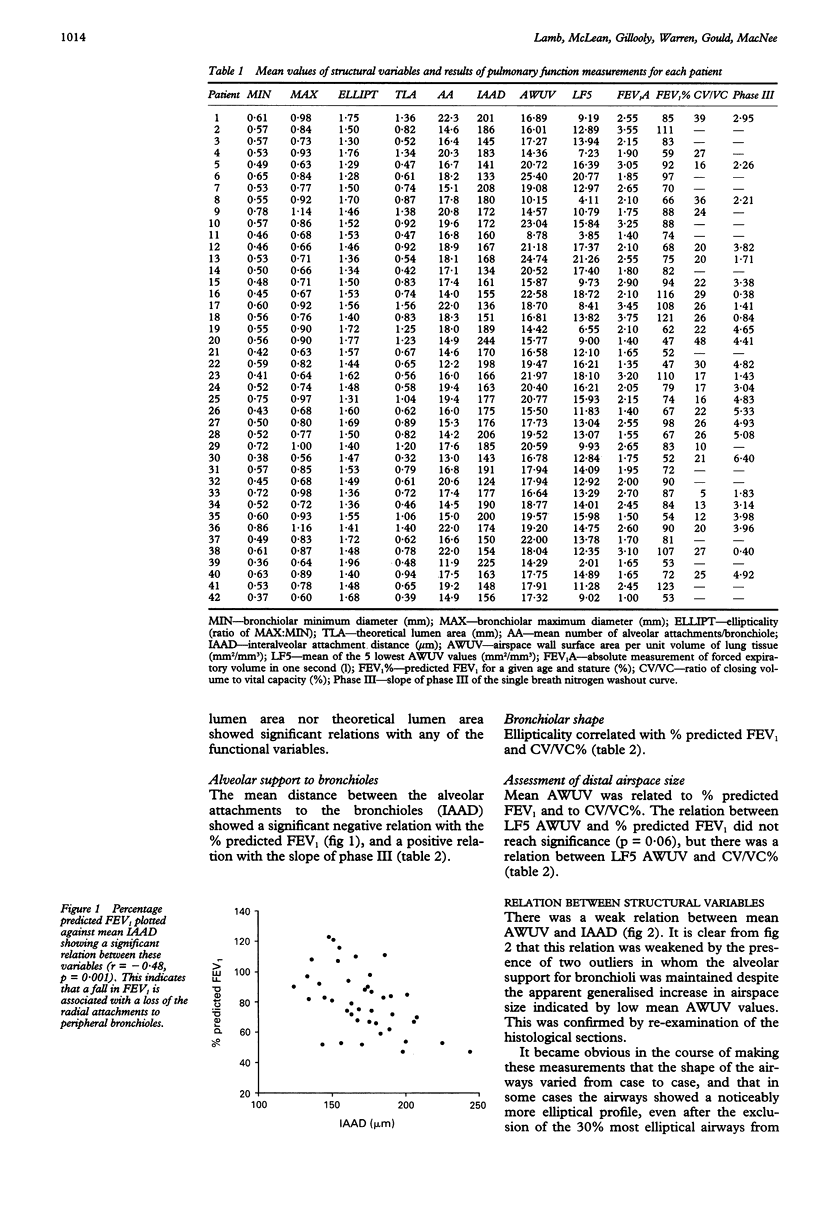
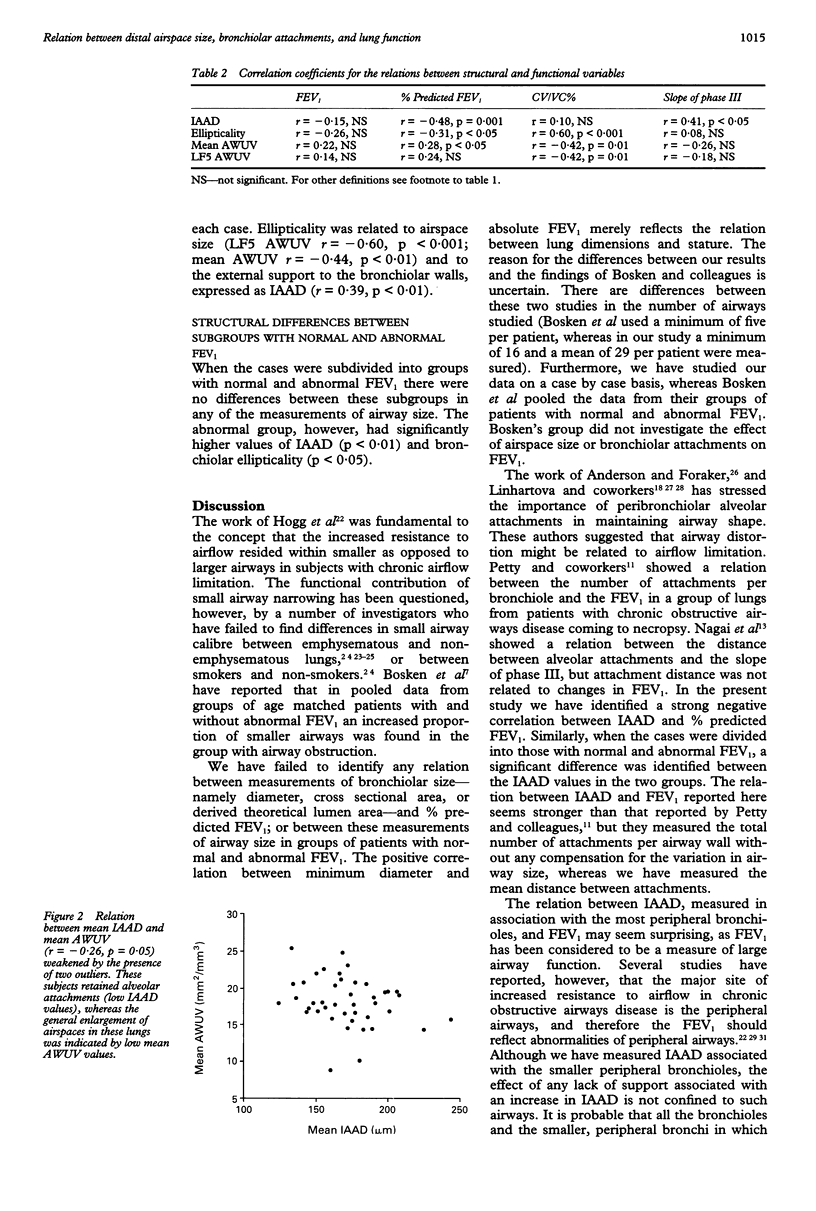
BACKGROUND--Smoking related fixed airway obstruction may be due to airway scarring and narrowing or decreased support due to loss of adjacent alveolar walls. In this study of resected specimens, preoperative pulmonary function was compared with results of a morphometric study of lung structure. METHODS--Morphometric measurements were made on 42 inflation fixed lung specimens as follows: airspace wall surface area per unit volume (AWUV) was measured on at least 25 l mm2 histological fields from each specimen, expressed as a mean, and the mean of the lowest five measurements for each case (LF5). Minimum diameter, maximum diameter, diameter ratio (ellipticality), lumen area, and lumen circumference were measured on at least 16 non-respiratory bronchioles from each lung. Peribronchiolar alveolar support was measured as mean interalveolar attachment distance (IAAD). Measurements of pulmonary function included forced expiratory volume in one second (FEV1) (absolute and % predicted values; n = 42), slope of phase III (single breath nitrogen test; n = 28), closing volume (expressed as a percentage of vital capacity (CV/VC%); n = 28). RESULTS--Bronchiolar size was not independently related to the tests of lung function used. Percentage predicted FEV1 was related to mean IAAD, ellipticality, and mean AWUV. CV/VC% showed significant relation with ellipticality, mean AWUV, and LF5 AWUV. Slope of phase III increased with increasing IAAD. Significant correlations were found between ellipticality and AWUV (mean and LF5), and between ellipticality and IAAD. Both IAAD and ellipticality were significantly increased in patients with abnormally low FEV1. CONCLUSION--Destruction of airspace walls, particularly those attached to the peripheral bronchioles, is more influential in determining airflow limitation than bronchiolar size.
Full text
PDF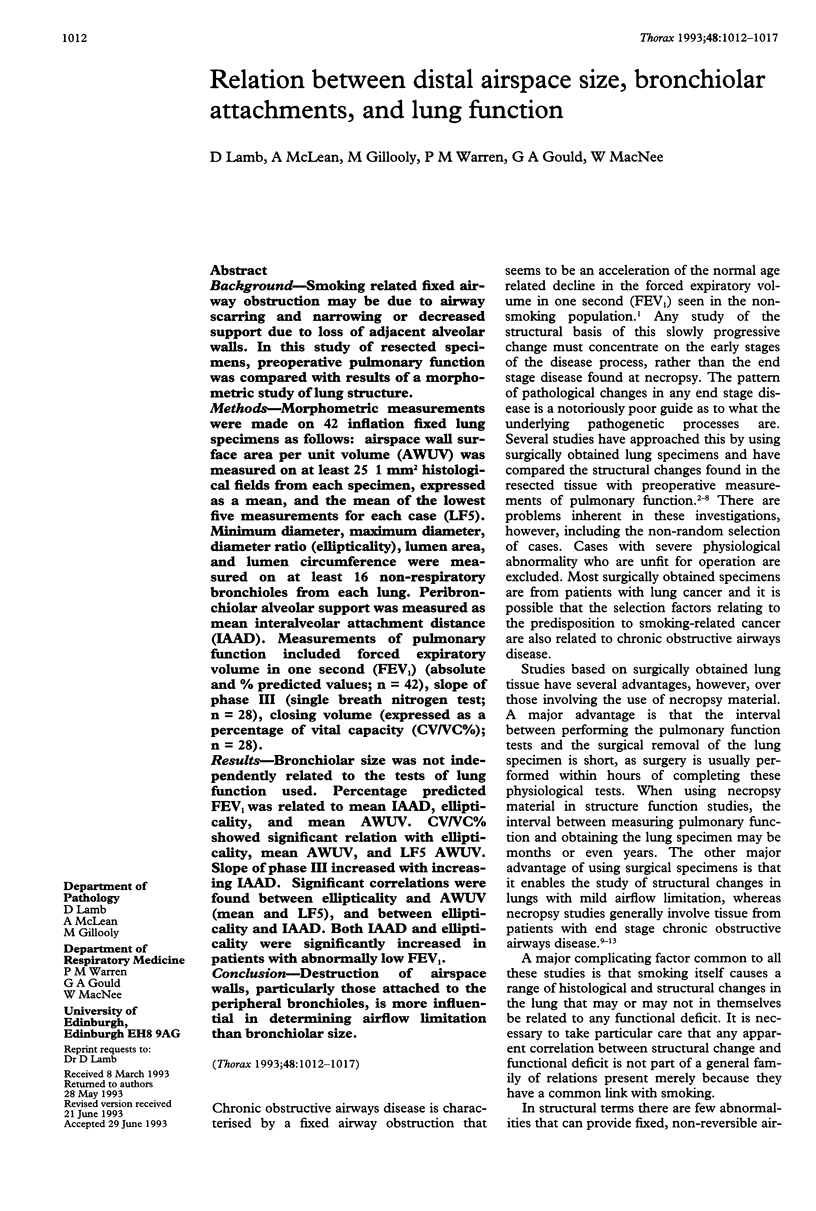

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ANDERSON A. E., Jr, FORAKER A. G. Relative dimensions of bronchioles and parenchymal spaces in lungs from normal subjects and emphysematous patients. Am J Med. 1962 Feb;32:218–226. doi: 10.1016/0002-9343(62)90291-7. [DOI] [PubMed] [Google Scholar]
- Berend N., Thurlbeck W. M. Correlations of maximum expiratory flow with small airway dimensions and pathology. J Appl Physiol Respir Environ Exerc Physiol. 1982 Feb;52(2):346–351. doi: 10.1152/jappl.1982.52.2.346. [DOI] [PubMed] [Google Scholar]
- Bosken C. H., Wiggs B. R., Paré P. D., Hogg J. C. Small airway dimensions in smokers with obstruction to airflow. Am Rev Respir Dis. 1990 Sep;142(3):563–570. doi: 10.1164/ajrccm/142.3.563. [DOI] [PubMed] [Google Scholar]
- Buist A. S., Ross B. B. Quantitative analysis of the alveolar plateau in the diagnosis of early airway obstruction. Am Rev Respir Dis. 1973 Nov;108(5):1078–1087. doi: 10.1164/arrd.1973.108.5.1078. [DOI] [PubMed] [Google Scholar]
- Cosio M. G., Hale K. A., Niewoehner D. E. Morphologic and morphometric effects of prolonged cigarette smoking on the small airways. Am Rev Respir Dis. 1980 Aug;122(2):265–221. doi: 10.1164/arrd.1980.122.2.265. [DOI] [PubMed] [Google Scholar]
- Cosio M., Ghezzo H., Hogg J. C., Corbin R., Loveland M., Dosman J., Macklem P. T. The relations between structural changes in small airways and pulmonary-function tests. N Engl J Med. 1978 Jun 8;298(23):1277–1281. doi: 10.1056/NEJM197806082982303. [DOI] [PubMed] [Google Scholar]
- FERRIS B. G., Jr, ANDERSON D. O., ZICKMANTEL R. PREDICTION VALUES FOR SCREENING TESTS OF PULMONARY FUNCTION. Am Rev Respir Dis. 1965 Feb;91:252–261. doi: 10.1164/arrd.1965.91.2.252. [DOI] [PubMed] [Google Scholar]
- Hogg J. C., Macklem P. T., Thurlbeck W. M. Site and nature of airway obstruction in chronic obstructive lung disease. N Engl J Med. 1968 Jun 20;278(25):1355–1360. doi: 10.1056/NEJM196806202782501. [DOI] [PubMed] [Google Scholar]
- KORY R. C., CALLAHAN R., BOREN H. G., SYNER J. C. The Veterans Administration-Army cooperative study of pulmonary function. I. Clinical spirometry in normal men. Am J Med. 1961 Feb;30:243–258. doi: 10.1016/0002-9343(61)90096-1. [DOI] [PubMed] [Google Scholar]
- Linhartová A., Anderson A. E., Foraker A. G. Nonrespiratory bronchiolar deformities. Graphic assessment in normal and emphysematous lungs. Arch Pathol. 1973 Jan;95(1):45–47. [PubMed] [Google Scholar]
- Linhartová A., Anderson A. E., Jr, Foraker A. G. Affixment arrangements of peribronchiolar alveoli in normal and emphysematous lungs. Arch Pathol Lab Med. 1982 Oct;106(10):499–502. [PubMed] [Google Scholar]
- Linhartová A., Anderson A. e., Jr, Foraker A. G. Radial traction and bronchiolar obstruction in pulmonary emphysema. Observed and theoretical aspects. Arch Pathol. 1971 Nov;92(5):384–391. [PubMed] [Google Scholar]
- Matsuba K., Thurlbeck W. M. The number and dimensions of small airways in emphysematous lungs. Am J Pathol. 1972 May;67(2):265–275. [PMC free article] [PubMed] [Google Scholar]
- Matsuba K., Thurlbeck W. M. The number and dimensions of small airways in nonemphysematous lungs. Am Rev Respir Dis. 1971 Oct;104(4):516–524. doi: 10.1164/arrd.1971.104.4.516. [DOI] [PubMed] [Google Scholar]
- Matsuba K., Wright J. L., Wiggs B. R., Pare P. D., Hogg J. C. The changes in airways structure associated with reduced forced expiratory volume in one second. Eur Respir J. 1989 Oct;2(9):834–839. [PubMed] [Google Scholar]
- McLean A., Warren P. M., Gillooly M., MacNee W., Lamb D. Microscopic and macroscopic measurements of emphysema: relation to carbon monoxide gas transfer. Thorax. 1992 Mar;47(3):144–149. doi: 10.1136/thx.47.3.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell R. S., Stanford R. E., Johnson J. M., Silvers G. W., Dart G., George M. S. The morphologic features of the bronchi, bronchioles, and alveoli in chronic airway obstruction: a clinicopathologic study. Am Rev Respir Dis. 1976 Jul;114(1):137–145. doi: 10.1164/arrd.1976.114.1.137. [DOI] [PubMed] [Google Scholar]
- Nagai A., West W. W., Paul J. L., Thurlbeck W. M. The National Institutes of Health Intermittent Positive-Pressure Breathing trial: pathology studies. I. Interrelationship between morphologic lesions. Am Rev Respir Dis. 1985 Nov;132(5):937–945. doi: 10.1164/arrd.1985.132.5.937. [DOI] [PubMed] [Google Scholar]
- Nagai A., Yamawaki I., Takizawa T., Thurlbeck W. M. Alveolar attachments in emphysema of human lungs. Am Rev Respir Dis. 1991 Oct;144(4):888–891. doi: 10.1164/ajrccm/144.4.888. [DOI] [PubMed] [Google Scholar]
- Petty T. L., Silvers G. W., Stanford R. E. Functional correlations with mild and moderate emphysema in excised human lungs. Am Rev Respir Dis. 1981 Dec;124(6):700–704. doi: 10.1164/arrd.1981.124.6.700. [DOI] [PubMed] [Google Scholar]
- Petty T. L., Silvers G. W., Stanford R. E. Radial traction and small airways disease in excised human lungs. Am Rev Respir Dis. 1986 Jan;133(1):132–135. doi: 10.1164/arrd.1986.133.1.132. [DOI] [PubMed] [Google Scholar]
- Saetta M., Ghezzo H., Kim W. D., King M., Angus G. E., Wang N. S., Cosio M. G. Loss of alveolar attachments in smokers. A morphometric correlate of lung function impairment. Am Rev Respir Dis. 1985 Oct;132(4):894–900. doi: 10.1164/arrd.1985.132.4.894. [DOI] [PubMed] [Google Scholar]
- Silvers G. W., Maisel J. C., Petty T. L., Mitchell R. S., Filley G. F. Central airway resistance in excised emphysematous lungs. Chest. 1972 Jun;61(7):603–612. doi: 10.1378/chest.61.7.603. [DOI] [PubMed] [Google Scholar]
- West W. W., Nagai A., Hodgkin J. E., Thurlbeck W. M. The National Institutes of Health Intermittent Positive Pressure Breathing trial--pathology studies. III. The diagnosis of emphysema. Am Rev Respir Dis. 1987 Jan;135(1):123–129. doi: 10.1164/arrd.1987.135.1.123. [DOI] [PubMed] [Google Scholar]
- Willems L. N., Kramps J. A., Stijnen T., Sterk P. J., Weening J. J., Dijkman J. H. Relation between small airways disease and parenchymal destruction in surgical lung specimens. Thorax. 1990 Feb;45(2):89–94. doi: 10.1136/thx.45.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willems L. N., Kramps J. A., Stijnen T., Sterk P. J., Weening J. J., Dijkman J. H. Relation between small airways disease and parenchymal destruction in surgical lung specimens. Thorax. 1990 Feb;45(2):89–94. doi: 10.1136/thx.45.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright J. L., Hobson J. E., Wiggs B., Pare P. D., Hogg J. C. Airway inflammation and peribronchiolar attachments in the lungs of nonsmokers, current and ex-smokers. Lung. 1988;166(5):277–286. doi: 10.1007/BF02714058. [DOI] [PubMed] [Google Scholar]
- Wright J. L., Lawson L. M., Pare P. D., Wiggs B. J., Kennedy S., Hogg J. C. Morphology of peripheral airways in current smokers and ex-smokers. Am Rev Respir Dis. 1983 Apr;127(4):474–477. doi: 10.1164/arrd.1983.127.4.474. [DOI] [PubMed] [Google Scholar]
- Zamel N., Hogg J., Gelb A. Mechanisms of maximal expiratory flow limitation in clinically unsuspected emphysema and obstruction of the peripheral airways. Am Rev Respir Dis. 1976 Mar;113(3):337–345. doi: 10.1164/arrd.1976.113.3.337. [DOI] [PubMed] [Google Scholar]


