Abstract
Hypogonadism or Testosterone Deficiency (TD) in adult men as defined by low levels of serum testosterone accompanied by characteristic symptoms and/or signs as detailed further on can be found in long-recognized clinical entities such as Klinefelter syndrome, Kallmann syndrome, pituitary or testicular disorders, as well as in men with idiopathic, metabolic or iatrogenic conditions that result in testosterone deficiency. These recommendations do not encompass the full range of pathologies leading to hypogonadism (testosterone deficiency), but instead focus on the clinical spectrum of hypogonadism related to metabolic and idiopathic disorders that contribute to the majority of cases that occur in adult men.
Keywords: Hypogonadism, late-onset, men, testosterone deficiency, testosterone
Introduction
The International Society for the Study of the Aging Male (ISSAM) Hypogonadism panel consists of a multidisciplinary group of experts, including urologists, endocrinologists, andrologists and internists with various subspecialties. The first recommendations were published in 2002 [1]. Due to the need for ongoing re-evaluation of the information presented in the recommendations they were revised in 2005 [2]. Clinical guidelines present the best evidence available to the experts at the time of writing, but as knowledge increased they were again updated in 2009 [3]. Since then a great amount of new information accumulated which encouraged us in 2013 to prepare a draft proposal for a further update [4]. This proposal was presented at the VII ISSAM congress in Moscow. A final form was presented at the ISSAM congress in Almaty, Kazakhstan, and the final version was accepted by consensus. It must however be remembered that recommendations can never replace clinical expertise. Treatment decisions, selection of treatment protocols or choice of products for individual patients must take into account patients' personal needs and wishes. The multidisciplinary group of experts received no corporate funding or remuneration for preparing these recommendations.
Hypogonadism or Testosterone Deficiency (TD) in adult men as defined by low levels of serum testosterone accompanied by characteristic symptoms and/or signs as detailed further on can be found in long-recognized clinical entities such as Klinefelter syndrome, Kallmann syndrome, pituitary or testicular disorders, as well as in men with idiopathic, metabolic or iatrogenic conditions that result in testosterone deficiency. These recommendations do not encompass the full range of pathologies leading to hypogonadism (testosterone deficiency), but instead focus on the clinical spectrum of hypogonadism related to metabolic and idiopathic disorders that contribute to the majority of cases that occur in adult men.
Recommendation 1: Definition
Hypogonadism (testosterone deficiency) in adult men is a clinical and biochemical syndrome associated with low level of testosterone, which may adversely affect multiple organ functions and quality of life.
Although the clinical significance of hypogonadism in adult men is becoming increasingly recognized, the extent of its prevalence in the general population is underappreciated. A large number of men with hypogonadism remain undiagnosed and untreated [5].
Recommendation 2: Clinical diagnosis
The diagnosis of hypogonadism requires the presence of characteristic symptoms and signs (Level 2, Grade A) in combination with decreased serum concentration of testosterone.
Symptoms of hypogonadism may be categorized as sexual and non-sexual. Sexual symptoms include erectile dysfunction (ED), diminished frequency of morning erections [6] and decrease in sexual thoughts (low libido) [7–9], as well as difficulty in achieving orgasm and reduced intensity of orgasm. Non-sexual symptoms include fatigue, impotence, impaired concentration, depression and decreased sense of vitality and/or wellbeing. Signs of hypogonadism also include anemia, osteopenia and osteoporosis, abdominal obesity and the metabolic syndrome [10].
Principally, the clinician has to distinguish between forms of congenital hypogonadism that require lifelong substitution and which can be congenital (e.g. Kallmann syndrome, Klinefelter syndrome) or acquired (e.g. anorchia due to trauma or orchiectomy, pituitary lesions/tumors, late-onset hypogonadism (LOH)) and forms of hypogonadism that might be reversible. The latter, potentially reversible forms of hypogonadism are most often found in co-existence with metabolic disorders such as obesity/type 2 diabetes mellitus (T2DM), inflammatory diseases (e.g. chronic obstructive pulmonary disease, chronic inflammatory bowel diseases) or psychological problems such as depressive mood or stress.
Screening questionnaires on male symptomatic hypogonadism, although sensitive, have low specificity. Morley et al. compared the most commonly used questionnaires in 148 men using bioavailable testosterone (BT) as the biochemical “gold standard” for the diagnosis of hypogonadism, and found the sensitivity to be 97% for the ADAM (Androgen Deficiency in the Aging Male questionnaire), 83% for the AMS (Aging Male's Symptoms scale) and 60% for the MMAS (Massachusetts Male Aging Study questionnaire). Specificity was 30% for the ADAM, 59% for the MMAS and 39% for the AMS [11] (now validated in many languages [12,13]). Despite having low specificity, the AMS and other male hypogonadism questionnaires may be useful to assess the presence and severity of symptoms as a prerequisite for initiating [14] and for monitoring the clinical response to testosterone therapy [15–18].
Physical examination of patients with suspected hypogonadism should include an assessment of the amount and distribution of body hair (including beard growth and pubic hair); presence of acanthosis nigricans, associated with insulin resistance [19–22], presence and degree of breast enlargement; size and consistency of the testes; abnormalities in the scrotum and size, appearance of the penis, presence of subcutaneous plaque. The prostate should be examined in older patients for size, consistency, symmetry and presence of nodules or induration; it should be noted that the prostate may be enlarged in older men, despite a low testosterone level [23]. Weight, height, body mass index (BMI) and waist circumference should also be measured, since symptoms and signs potentially indicative of testosterone deficiency in men include height loss, reduced muscle bulk and strength and increased body fat, in particular, abdominal fat accumulation and BMI [24,25]. The greater the number of symptoms in a man, the greater the probability that he truly has testosterone deficiency [26]. However, the presence of even one symptom may raise suspicion of symptomatic hypogonadism. A high prevalence of symptomatic hypogonadism has been observed in populations of aging men, and those with diabetes mellitus type 2, obesity [27], benign prostatic hyperplasia (BPH) and lower urinary tract symptoms (LUTS) [28,29].
The presence of symptoms alone does not constitute testosterone deficiency. Symptoms must be accompanied by decreased serum concentrations of total testosterone (TT) or free T level to support a diagnosis of symptomatic hypogonadism (Level 2, Grade A).
Various prospective studies have reported the occurrence of hypogonadal symptoms as side effects of androgen-deprivation therapy, including hot flashes, decreased libido and ED [30,31]. Other complications of androgen-deprivation therapy include osteoporosis, with increased risk of fractures, and worsening of comorbidities such as diabetes mellitus, cardiovascular disease and metabolic syndrome, as well as physical, functional and cognitive impairment [32–35].
Based on the above and below mentioned data, we recommend the investigation of hypogonadism in men with the following conditions:
Low libido
Poor morning erections
Erectile dysfunction
Depressed mood
Fatigue
Decreased vitality
Cognitive impairment
Insulin resistance
Obesity, abdominal obesity
Metabolic syndrome
Arterial hypertension
Diabetes mellitus type 2
Decreased muscle mass and strength
Decreased bone mineral density and osteoporosis
Use of glucocorticoids, opioids, antipsychotics
Recommendation 3: Pathogenesis
The metabolic disorders such as obesity, T2DM, inflammatory diseases and other co-morbidities mentioned above modify the hypothalamic–pituitary–gonadal axis by suppressing one or more of its components (decreased hypothalamic–pituitary/decreased Leydig cell function) but not in a constant fashion as in the permanent forms of hypogonadism where one of the components has irrevocably lost function.
Age-related decrease in testosterone production (also called Late-onset hypogonadism) is also related to an impairment of hypothalamic–pituitary–gonadal axis [36], but in contrast may not be reversible.
Current opinion is that hypogonadism and the respective co-morbidity reinforce each other and that a (potentially transient) testosterone replacement therapy (TRT) can mitigate this vicious cycle.
Risk factors for hypogonadism may include chronic illnesses, including T2DM, impaired thyroid gland function, hyperprolactinemia, chronic obstructive lung disease, rheumatoid arthritis, renal and HIV-related diseases, obesity, metabolic syndrome [37], stress and hemachromatosis, vitamin D deficiency [38–40]. Such chronic diseases should be investigated and treated (Level 2, Grade A).
Though there is still a controversy in defining normal TSH levels in the elderly [41–44], thyroid gland function impairment should be excluded in all patients with hypogonadism, as symptoms of hypothyroidism may overlap those of hypogonadism.
TT levels have been reported to be lower in depressed men compared with non-depressed men. TT is particularly low in men with severe, treatment-resistant depression [45]. TRT has been shown to reduce depression symptoms in hypogonadal men, including middle-aged men with hypogonadism and those using antidepressants [46].
Drugs such as glucocorticoids, opioids, antipsychotics induce TD [47–49]. Glucocorticoids are widely used as anti-inflammatory drugs. However, prolonged use of glucocorticoids results in undesirable side effects, including hypogonadism [49]. It has also been reported that statins may reduce TT [50].
Aloisi and colleagues [51] were the first to show that morphine induces a dramatic and long-lasting decrease in TT. This finding has now been corroborated by numerous subsequent studies [52].
Recommendation 4: Laboratory diagnosis
In patients at risk or suspected of hypogonadism, a thorough physical and biochemical work-up is recommended (Level 2, Grade A).
The key laboratory tests to confirm the diagnosis of hypogonadism are serum total and free testosterone. Note should be made that transient decreases of serum T levels can occur, due to acute illnesses [53], and this should be excluded by careful clinical evaluation and repeated hormone measurement.
We recommend 12.1 nmol/L as a lower limit of normal for TT level. However, due to individual differences in testosterone sensitivity some men may exhibit symptoms of hypogonadism with TT concentrations above this threshold, and may benefit from TRT. TRT may be reasonably offered to symptomatic men with testosterone concentrations higher than 12 nmol/L based on clinical judgment, and certainly if free T concentrations are reduced.
Free T levels as low as 225 pmol/L (65 pg/mL) [54] or 243 pmol/L (70 pg/mL) [10] have been recommended as a lower limit of normal range and together with the presence of one or more hypogonadal symptoms can provide supportive evidence for TRT (Level 2, Grade B). Others have proposed a more generous threshold of 347 pmol/L (100 pg/mL or 10.0 ng/dL) as a lower threshold for free T level based on clinical experience [55,56].
It is preferred to obtain a serum sample for TT determination between 07.00 and 11.00 h [57] (Level 2a, Grade A), although diurnal variation is substantially blunted in older men. In a cross-sectional study of 3006 men with the mean age 60.3 years presenting for prostate cancer screening, serum testosterone concentrations were unchanged from 6 am to 2 pm, and then decreased by only 13% between 2 pm and 6 pm [58].
It is our clinical impression that testosterone circadian rhythms may be blunted in symptomatic hypogonadal men regardless of age.
New data indicate that a glycaemic load may acutely decrease testosterone [59]. The clinical implications of this observation have not been tested adequately to currently recommend that blood testing for testosterone be performed in a fasting state. Although this would make it possible to permit to measure glucose and lipids at the same time and help to discover co-morbidities.
The most widely accepted parameter to establish the presence of hypogonadism is the measurement of TT. Unfortunately, no consensus has been reached regarding the lower TT threshold defining TD, and there are no generally accepted lower limits of normal TT [60]. This lack of consensus follows from the fact that no studies have shown a clear threshold for TT or free T that distinguishes men who will respond to treatment from those who will not. In a recent publication in NEJM the EMAS Group proposed 11 nmol/L as a lower cut-off value for TT [6]. Hypogonadism may be considered if TT level is below 12.1 nmol/L based on LCMS/MS (liquid chromatography–mass spectrometry) measurements in three large cohorts comprising more than 10 000 men of various ages [60].
Meanwhile the number of CAG (cytosine–adenine–guanine triplet) repeats in androgen receptor differs in men and influences the androgen receptor activity [61–64] (Figure 1). Hence testosterone sensitivity may vary in different individuals. It has also been argued that the magnitude of the decrease in serum T concentrations might be a better predictor of hypogonadism than the actual concentrations of TT and BT [65].
Figure 1.

Threshold continuum to hypogonadism.
The same applies to androgen receptor gene CAG repeat lengths >24 in the presence of symptoms and normal testosterone levels may be considered as a state of preclinical hypogonadism [66].
The prevalence of hypogonadal symptoms increases with TT levels below 12.1 nmol/L (350 ng/dL) [26] (Level 2b, Grade A). However, Zitzmann et al. have shown that testosterone deficiency symptoms may also be seen with TT levels as high as 15 nmol/L. This study showed that the prevalence of loss of libido or vigor increased at testosterone concentrations below 15 nmol/L (p < 0.001), whereas depression and T2DM (also in non-obese men) were significantly more prevalent in men with TT concentrations below 10 nmol/L (p < 0.001). ED has been identified as a composite pathology of metabolic risk factors, smoking and depression, whereas only TT concentrations below 8 nmol/L contributed to that symptom (p = 0.003). Behre et al. [14] demonstrated that 6 months of TRT improved body composition and quality of life in men aged 50–80 years with TT < 15 nmol/L and hypogonadal symptoms; these men showed further improvements in body composition and quality of life over the following 12 months of TRT. Lower TT levels have also been shown to be associated with sub-threshold symptoms of anxiety and depression [67]. There is also a recent study reporting increased hypogonadal symptoms in younger men ≤ 40 years with TT below 400 ng/dL (13.9 nmol/L) [68].
Free or bioavailable T should be considered when the TT concentration does not correspond with clinical presentation, since individual variation in SHBG concentrations may influence total testosterone results. Free or bioavailable T should also be particularly considered in obese men. Equilibrium dialysis is the gold standard for free T measurement but may not be routinely available or may be too costly in some regions. Free T assays based on analog displacement immunoassays are widely available and have been used clinically with good success [69], but their reliability has been questioned by some authors [56]. Alternatively, measurement of serum SHBG together with a reliable measurement of TT allows for the determination of the calculated free T level [70] (Level 2b, Grade A).
Measurements of serum LH will assist in differentiating between primary and secondary hypogonadism. All cases of elevated LH level and testosterone below normal or in the lower quartile range would indicate testicular failure and TRT should be considered [71]. A state of elevated LH in the presence of normal testosterone but with hypogonadal symptoms should be considered as hypogonadism. Measurement of serum prolactin level is indicated when TT is <5.2 nmol/L (150 ng/dL) [72,73] or when secondary hypogonadism due to a pituitary tumor (like prolactinoma) is suspected [24,74,75] (Level 2, Grade A).
In general, it is currently speculated that variable phenotypes of androgen insensitivity exist, mainly owing to mutated androgen receptors. A more subtle modulation of androgen effects is related to the CAG repeat polymorphism (CAGn) in exon 1 of the androgen receptor gene: transcription of androgen-dependent target genes is attenuated with increasing length of triplets. As a clinical entity, the CAG repeat polymorphism can relate to variations of androgenicity in men in various tissues and psychological traits: the longer the CAGn, the less prominent is the androgen effect when individuals with similar testosterone concentrations are compared. A strictly defined threshold to hypogonadism is likely to be replaced by a continuum spanned by genetics as well as symptom specificity. In addition, effects of externally applied testosterone can be markedly influenced by the CAGn and respective pharmacogenetic implications are likely to influence indications as well as modalities of testosterone treatment of hypogonadal men.
The other recommended laboratory parameters should include: LH, TSH, SHBG, prolactin and vitamin D.
Recommendation 5: Assessment of treatment outcome and decisions on continued therapy
Improvement in hypogonadal signs and symptoms occur at different times for different organ systems [76].
Reduction in fat mass and increased lean body mass and muscle strength occur within 12–16 weeks of starting TRT and stabilize at 6–12 months, but can continue to improve over years.
Significant improvement in libido is usually experienced within 3–6 weeks of commencing TRT. Up to 12 months of TRT may be required before significant improvement in erectile and ejaculatory function is observed [77]. Significant improvement in quality of life (QoL) usually occurs within 3–4 weeks of starting TRT; longer-term TRT is required to achieve maximum QoL benefit. Effects on depressive mood become detectable after 3–6 weeks of starting TRT, with maximum improvement occurring after 18–30 weeks. Improvements in bone are detectable after 6 months of TRT, while the full beneficial effect of TRT on bone mineral density may take 2–3 years [78,79] or even 6 years as suggested by Haider et al. [80].
Effects of TRT on lipids appear after 4 weeks, with maximal effects being seen after 6–12 months of treatment. Insulin sensitivity may improve within a few days of starting TRT, but effects on glycaemic control become evident only after 3–12 months. Failure to improve clinical symptoms within a reasonable period of time should result in re-evaluation of TRT with regard to dosage, compliance and level of serum T achieved. Further investigation should be undertaken to determine other causes of the symptoms (Level 1b, Grade A).
Recommendation 6: Body composition and mobility
In hypogonadal men, TRT improves body composition (decrease of fat mass, increase of lean body mass). Meta-analyses of randomized trials in middle-aged and older men have demonstrated the beneficial effects of TRT in reducing fat mass [81,82] (Level 1a, Grade A) with a significant increase in lean body mass and grip strength.
Rodrıguez-Tolra et al. demonstrated clearly that TRT in men with TD decreased fat mass overall, and to the greatest extent in the android and gynecoid regions and caused improvements in body composition, increasing lean mass, primarily in arms and legs [83].
TRT is potentially an effective treatment in aging obese men with TD [20]. There is also some evidence that long-term T may result in substantial and sustained reductions in body weight, waist circumference and BMI in obese hypogonadal men [84–86]. The successful achievement of weight loss, as well as the consistent increase in lean mass lead to beneficial effects on diabetes mellitus type 2 [87].
Higher free testosterone concentration is positively associated with lower risk of developing mobility limitation and progression of mobility limitations [88].
Recommendation 7: Bone density and fracture rate
Osteopenia, osteoporosis and fracture prevalence rates are increased in younger and older hypogonadal men [89]. In a recent meta-analysis and in the FRAX algorithm hypogonadism was identified as a known disorder strongly associated with secondary osteoporosis [90,91]. According to the latest Endocrine Society's guidelines on osteoporosis total testosterone measurement is suggested in all men evaluated for osteoporosis or considered for pharmacological treatment with bone-active agents [92].
Bone density in hypogonadal men of all ages is increased with TRT (Level 1b, Grade A).
In older men low testosterone levels are associated with increased risk of falls [93]. TRT has beneficial effects on muscle mass and strength that may reduce propensity to fall and therefore decrease fracture risk. Physical exercise, including stretching and equilibrium exercises are mandatory in combination with TRT.
Assessment of bone density at 2-year intervals is recommended in aging, hypogonadal men with normal bone density. In men with lowered bone mineral density receiving TRT, stabilization or progress may be monitored with annual DXA. This should be performed using DXA as a gold standard method providing the largest amount of reliable data. It is possible to use quantitative computer tomography (qCT) but this is exposing patients to a high amount of radiation. For clinical follow-up, methods of ultrasound measuring bone density reflect the changes achieved by testosterone substitution and may be used if other methods are not available [94].
Recommendation 8: Testosterone and sexual function
The initial assessment of men with ED and/or diminished libido should include determination of TT and whenever possible a free T level. These symptoms, with or without a testosterone deficiency, might be related to co-morbidities (i.e. T2DM, hyperprolactinemia, the metabolic syndrome, bladder outlet obstruction, peripheral vascular disease or medications) (Level 2a, Grade A).
Men with poor morning erections, ED and/or diminished libido and documented TD are candidates for TRT. Meta-analyses of randomized, placebo-controlled trials of TRT in men with sexual dysfunction and varying TT levels demonstrated benefits in some aspects of sexual desire, erectile function and performance [95] (Level 2a, Grade A).
In sildenafil non-responders with T2DM, a combination of oral T undecanoate and sildenafil was associated with improvement in erections, a significant increase in IIEF-5 scale and increased sexual contacts [96]. In hypogonadal men with an inadequate response to phosphodiesterase type-5 inhibitors, TRT has been shown to be of benefit.
In the international, multicenter, prospective study IPASS with a sample of 1493 men TRT showed a significant improvement in libido, erectile function and response to PDE-5 inhibitors therapy [97].
In aging men presenting with one or more sexual dysfunction symptoms and low-normal TT levels, a short (3–6 months) trial of TRT may be justified. Meanwhile there is data that a 12-months period is necessary to see an improvement in sexual function in some men [77]. If no improvement in sexual function is noted after an adequate trial of treatment, further investigation should be undertaken to determine other causes of ED (Level 2a, Grade B).
An inadequate response to TRT requires reassessment of the causal mechanisms responsible for the sexual dysfunction.
Recommendation 9: Testosterone and obesity, metabolic syndrome and type 2 diabetes mellitus
Many of the components of the metabolic syndrome (MetS) such as obesity, hypertension, dyslipidemia, impaired glucose regulation and insulin resistance are also present in hypogonadal men [98]. The MetS and T2DM are associated with low TT levels and majority of the patients with these conditions display symptoms of hypogonadism [27,99,100].
In a large epidemiologic study of more than 1150 healthy middle-aged Japanese men the probability of MetS was associated with lower levels of serum TT [101].
We suggest measurement serum T level in all men with obesity and diabetes mellitus type 2 (Level 2b, Grade A).
In addition to improving TD symptoms, TRT may have other benefits on metabolic status in hypogonadal men with diabetes and/or MetS (Level 2a, Grade B), that include improvement of surrogate parameters of cardiometabolic risk [102], such as significant reductions in fasting plasma glucose, homeostasis model assessment index (HOMA), triglycerides and waist circumference. It has been demonstrated that low- to intermediate-dose TRT may be safely utilized to ameliorate somatic and psychological frailty symptoms in association with improved anthropometric and glycometabolic parameters in aging, overweight men with LOH and impaired fasting glucose [103]. TRT improved significantly glycaemic control (HbA1c), insulin levels and sensitivity, and C-reactive protein levels [77,104].
Recommendation 10: Testosterone and Cardiovascular disease
Numerous studies have reported significant inverse associations for serum T levels and markers of atherosclerosis. Cross-sectional studies associated a low T level in men with endothelial dysfunction [105] and carotid intima–media thickness (IMT) independent of other cardiovascular risk factors [106]. Prospective studies in TRT-treated men with coronary artery disease (CAD) showed that TRT improved endothelial function [107] and reduced carotid IMT, with these effects being independent of BMI [102,108].
While the role of inflammation in cardiovascular disease is becoming apparent [109], more studies confirm the association between low testosterone and low-grade systemic inflammation. Observational evidence suggests that several pro-inflammatory cytokines and TT are inversely associated in patients with coronary artery disease and T2DM [110], while TRT in hypogonadal men with the MetS may reduce levels of inflammatory markers [97,111–113].
In a meta-analysis of all placebo-controlled randomized clinical trials on the effect of TRT on cardiovascular-related problems that included almost 5 500 patients, TRT was not related to any increase in CV risk [114]. In RCTs performed in subjects with metabolic derangements a protective effect of TS on CV risk was observed [114] (Level 1, Grade A).
In a recently presented study by Tan et al. that included 19 968 hypogonadal men who received TRT during a 5-year period, the risk for myocardial infarction was 7-fold lower and the risk for stroke nine times lower compared with samples from the general population. No worsening of preexisting myocardial infarction or stroke in patients on TRT was observed [115,116].
TD may influence not only quality of life in men, but also life span. There are strong observational data indicating that low endogenous testosterone levels are associated with increased risk of all-cause and cardiovascular disease-related mortality [117–119]. Given the important limitations of these types of studies [120,121], however, it is impossible to conclude that serum T concentrations had a causal effect. There are no adequate prospective controlled data examining the effect of testosterone therapy on mortality.
Recommendation 11: Depression and cognitive function
Recent meta-analysis showed a significant positive effect of TRT in depressed patients, assessed by the Hamilton Rating Scale for Depression when compared with placebo [122] (Level 1a, Grade A). TRT has been shown to reduce depression symptoms in hypo-gonadal men, including middle-aged men with MetS [123], LOH and those using antidepressants [46].
Though the effect of TRT on cognitive function in men with hypogonadism remains controversial [124,125], it can be considered after exclusion of other causes of cognitive impairment [126,127].
Recommendation 12: Benign prostatic hyperplasia (BPH) and lower urinary tract symptoms (LUTS)
Approximately one in five men with BPH has low TT. There is a well-established relationship between LUTS/BPH and increased BMI and low TT [128].
At present, there is no evidence that TRT either increases the risk of BPH or contributes to worsening of LUTS [76,129]. A limited number of studies have reported that TRT improves LUTS in hypogonadal men with mild BPH [130,131].
Recommendation 13: Prostate cancer (PCa)
Recent evidence fails to support the longstanding fear that T therapy will increase prostate cancer risk, or cause rapid growth of an occult cancer. Indeed, several small series have shown low rates of prostate cancer progression or recurrence with T therapy in men following definitive treatment of localized prostate cancer [132] or in men with untreated prostate cancer undergoing active surveillance [133].
To our opinion the relationship between testosterone and prostate cancer appears to follow a saturation curve, present in many biological systems, in which growth corresponds with concentration of a key nutrient until a concentration is reached in which an excess of the nutrient is achieved [134] (Figure 2).
Figure 2.
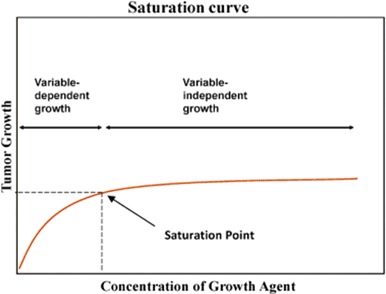
Saturation curve, demonstrating the relationship between testosterone and prostate cancer.
There is no evidence that TRT will convert sub-clinical prostatic lesions to clinically detectable PCa (Level 2, Grade B).
Analysis of pooled worldwide data from 18 prospective studies (more than 3000 cases and 6000 controls) found no significant association between serum testosterone concentrations and prostate cancer risk [135]. A meta-analysis showed no significant association between TRT and the incidence of PCa or the need for prostate biopsy when compared with the placebo/non-intervention group [136].
In the multicenter, prospective study IPASS with a sample of 1493 men, the prevalence of such adverse effects like increase of the hematocrit and increase of the PSA was 51%, no cases of prostate cancer were observed [97]. In an observational, prospective registry studies in 1023 patients receiving long-term TRT with a median follow-up of 5–6 years, the incidence of prostate cancer remained well below the incidence reported in screening studies in the general population [137].
Large observational studies fail to show increased risk with higher endogenous T, no increased risk was seen in a meta-analysis of 19 placebo-controlled T studies [138], and the placebo arm of the REDUCE trial showed no increased risk of cancer associated with serum T or DHT levels in >3000 men who underwent study biopsies of the prostate at year 2 and year 4.
Nonetheless, in the absence of large-scale, long-term controlled studies, it is impossible to definitively assert the safety of TRT with regard to PCa. Therefore, prior to starting TRT, a patient's risk of PCa must be assessed using, at a minimum measurement of serum prostate-specific antigen (PSA). Annual DRE is recommended during TRT to identify the development of new palpable abnormalities, although evidence supporting DRE as a diagnostic tool is lacking. Pre-treatment assessment should include PCa risk predictors such as age, family history of PCa and ethnicity/race. If suspicion of PCa exists, it may be reasonable to perform prostate biopsy if warranted by clinical presentation. Testosterone therapy may be initiated in these men if prostate biopsy is negative (Level 2a, Grade B).
After initiation of TRT, patients should be monitored for prostate disease with measurement of serum PSA at 3–6 months, 12 months and at least annually thereafter (Level 2, Grade B).
An initial increase of PSA and prostate volume (PV) with TRT is frequently seen over the first 2–6 months because the prostate is an androgen-dependent organ. The increase in PSA will be greatest in men with marked testosterone deficiency and least (or absent) in men with milder degrees of hypogonadism [139]. The PSA level at 6 months after initiation of TRT should be used as the new baseline.
Should a patient's PCa risk be sufficiently high based on suspicious finding on DRE/prostate ultrasound or PSA > 4.0 ng/ml, transrectal ultrasound-guided biopsies of the prostate are recommended and the patient should be referred to an urologist for further clinical examination. Referral to an urologist for prostate evaluation and possible biopsy during TRT should be made with development of a new palpable prostate abnormality on DRE, or with a worrisome rise in PSA. Recommendations regarding what constitutes a concerning rise in PSA include an increase of 1.0 ng/ml over baseline PSA [140] or a PSA velocity greater than 0.35 ng/ml per year [141] (Level 2b, Grade A).
Recommendation 14: Treatment and delivery systems
Preparations of aromatizable T should be used for TRT. Currently available intramuscular, subdermal, transdermal, oral and buccal T preparations are safe and effective (Level 1b, Grade A).
The treating physician should have sufficient knowledge and adequate understanding of the pharmacokinetics as well as of the advantages and drawbacks of each TRT preparation. The selection of the TRT preparation should be a joint decision of an informed patient and physician.
Because the possible development of an adverse event during treatment (especially elevated hematocrit or PCa) requires rapid discontinuation of TRT, short-acting TRT preparations may be preferred over the long-acting depot preparations in the initial treatment of patients with LOH. However, it must be noted that elevated hematocrit is typically only associated with high serum T concentrations and uncommon occurs with TRT preparations, which have been formulated to maintain maximal serum T levels well within the normal range.
TRT is associated with a dose-dependent increase in hematocrit and hemoglobin level. This has raised concerns regarding possible adverse events due to increased viscosity. Some authors recommend that TRT be discontinued if hematocrit is >54%, which may be reasonable while baseline hematocrit level >50% is a relative contraindication for starting testosterone therapy [24]. However, these recommendations are based on assumptions – the clinical significance of a hematocrit >54% is unknown. The meta-analysis by Fernandez-Balsells [136] showed that, despite a higher incidence of elevated hematocrit, no clinical adverse affects were reported. Results of earlier studies (MEDLINE database search from 1966 to 2004) showed that, despite TRT-treated men being nearly four times as likely to have hematocrit >50% compared with placebo-treated men (OR = 3.69, 95% CI, 1.82–7.51), the frequency of cardiovascular events, sleep apnea or death was not significantly different between the two groups. Abnormal hematocrit elevations were reported in 43.8% of patients administered intramuscular T enanthate injections and in 15.4% of patients administered transdermal T treatment [142]. The lack of increase in cardiovascular events with elevated hematocrit may be due to the fact that T has vasodilator and anti-atherosclerotic effects [143]. Isolated hematocrit elevations can be the result of insufficient fluid intake on a hot day. Only repeated measures of hematocrit >54% should be followed by concomitant administration of aspirin, bleeding, therapeutic phlebotomy and/or discontinuation of TRT until hematocrit declines below 54%. After normalization of hematocrit level TRT may be continued with a reduced dosage.
Periodic hematological assessment is, however, indicated, i.e. before TRT, then 3–4 months and 12 months in the first year of treatment, and annually thereafter. Although it is not yet clear what upper limit of hematocrit level is clinically desirable, dose adjustments may be necessary to keep hematocrit below 52–54%.
It is recommended to clinically apply the various time-dependent effects of TRT. Each target symptom or tissue has a specific time frame of expected response to androgen replacement (Figure 3).
Figure 3.

Time-dependent onset of effects of testosterone substitution therapy.
Inadequate data are available to determine the optimal target serum T level for men with LOH. For the present time, the treatment goal with TRT is to maintain serum T levels in the normal range. Sustained supra-physiological serum T levels should be avoided. No evidence exists for or against the need to maintain the physiological circadian rhythm of serum T levels (Level 2, Grade B).
Men with significant erythrocytosis (hematocrit >52%) (Level 3, Grade A), severe untreated obstructive sleep apnoe (Level 3, Grade B) or untreated severe congestive heart failure (Level 3, Grade B) should not be started on treatment with TRT without prior resolution of the co-morbid condition.
Declaration of interest
This guidelines document was developed without any financial support. No external sources of funding and support have been involved. No honoraria or other reimbursements have been provided.
Bruno Lunenfeld received no financial support from pharmaceutical companies with testosterone products.
George Mskhalaya has received payments from the following companies with testosterone products for consulting and/or scientific advisory boards – Bayer Pharma, Besins Healthcare.
Michael Zitzmann has not conflict of interest in relation to the content of this manuscript.
Stefan Arver has not conflict of interest in relation to the content of this manuscript.
Svetlana Kalinchenko has received payments from the following pharmaceutical companies with testosterone products for consulting and/or scientific advisory boards – Bayer Pharma, Besins Healthcare.
Yulya Tishova has received payments from the following companies with testosterone products for consulting and/or scientific advisory boards – Bayer Pharma, Besins Healthcare.
Abraham Morgentaler has received payments from the following pharmaceutical companies with testosterone products for consulting and/or scientific advisory boards, or research grants – AbbVie, Antares, Auxilium, Clarus, Endo, Lilly.
The authors alone are responsible for the content and writing of this article.
References
- 1.Morales A, Lunenfeld B International Society for the Study of the Aging Male. Aging Male. Investigation, treatment and monitoring of late-onset hypogonadism in males. Official recommendations of ISSAM. Aging Male. 2002;5:74–86. [PubMed] [Google Scholar]
- 2.Nieschlag E, Swerdloff R, Behre HM, et al. Investigation, treatment and monitoring of late-onset hypogonadism in males. Aging Male. 2005;8:56–8. doi: 10.1080/13685530500130969. [DOI] [PubMed] [Google Scholar]
- 3.Wang C, Nieschlag E, Swerdloff RS, et al. ISA, ISSAM, EAU, EAA and ASA recommendations: investigation, treatment and monitoring of late-onset hypogonadism in males. Aging Male. 2009;12:5–12. doi: 10.1080/13685530802389628. [DOI] [PubMed] [Google Scholar]
- 4.Lunenfeld B, Mskhalaya G, Kalinchenko S, Tishova Y. Recommendations on the diagnosis, treatment and monitoring of late-onset hypogonadism in men – a suggested update. Aging Male. 2013;16:143–50. doi: 10.3109/13685538.2013.853731. [DOI] [PubMed] [Google Scholar]
- 5.Trinick TR, Feneley MR, Welford H, Carruthers M. International web survey shows high prevalence of symptomatic testosterone deficiency in men. Aging Male. 2011;14:10–15. doi: 10.3109/13685538.2010.511325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu FC, Tajar A, Beynon JM, et al. EMAS Group. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123–35. doi: 10.1056/NEJMoa0911101. [DOI] [PubMed] [Google Scholar]
- 7.AACE Hypogonadism Task Force. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the evaluation and treatment of hypogonadism in adult male patients 2002. Endocr Pract. 2002;8:439–56. [PubMed] [Google Scholar]
- 8.Lejeune H, Huyghe E, Droupy S. Hypoactive sexual desire and testosterone deficiency in men. Prog Urol. 2013;23:621–8. doi: 10.1016/j.purol.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 9.Lunenfeld B, Arver S, Moncada I, et al. How to help the aging male? Current approaches to hypogonadism in primary care. Aging Male. 2012;15:187–97. doi: 10.3109/13685538.2012.729110. [DOI] [PubMed] [Google Scholar]
- 10.Dohle GR, Arver S, Bettocchi C, et al. EAU 2014 guideline on male hypogonadism. ISBN: 978-90-79754-83-0. Available from: http://www.uroweb.org/gls/pdf/16_Male_Hypogonadism_LR%20II.pdf [last accessed 8 Dec 2014]
- 11.Morley JE, Perry HM, III, Kevorkian RT, Patrick P. Comparison of screening questionnaires for the diagnosis of hypogonadism. Maturitas. 2006;53:424–9. doi: 10.1016/j.maturitas.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Chen W, Liu ZY, Wang LH, et al. Are the Aging Male's Symptoms (AMS) scale and the Androgen Deficiency in the Aging Male (ADAM) questionnaire suitable for the screening of late-onset hypogonadism in aging Chinese men? Aging Male. 2013;16:92–6. doi: 10.3109/13685538.2013.805319. [DOI] [PubMed] [Google Scholar]
- 13.Rabah DM, Altaweel W, Arafa MA. Clinical assessment and validation of an Arabic Aging Male Symptoms questionnaire in patients with androgen deficiency. Aging Male. 2011;14:33–6. doi: 10.3109/13685538.2010.512373. [DOI] [PubMed] [Google Scholar]
- 14.Behre HM, Tammela TL, Arver S, et al. European Testogel Study Team. A randomized, double-blind, placebo-controlled trial of testosterone gel on body composition and health-related quality-of-life in men with hypo-gonadal to low-normal levels of serum testosterone and symptoms of androgen deficiency over 6 months with 12 months open-label follow-up. Aging Male. 2012;15:198–207. doi: 10.3109/13685538.2012.699562. [DOI] [PubMed] [Google Scholar]
- 15.Zengerling F, Schrader AJ, Cronauer MV, et al. The “Aging Males' Symptoms” Scale (AMS): predictive value for lowered circulating androgens. Aging Male. 2012;15:253–7. doi: 10.3109/13685538.2012.729232. [DOI] [PubMed] [Google Scholar]
- 16.Lee CP, Jiang JR, Chen Y, et al. The “Aging Males' Symptoms” (AMS) Scale assesses depression and anxiety. Aging Male. 2013;16:97–101. doi: 10.3109/13685538.2013.807428. [DOI] [PubMed] [Google Scholar]
- 17.Moore C, Huebler D, Zimmermann T, et al. The Aging Males' Symptoms scale (AMS) as outcome measure for treatment of androgen deficiency. Eur Urol. 2004;46:80–7. doi: 10.1016/j.eururo.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura M, Fujimura T, Nagata M, et al. Association between lower urinary tract symptoms and sexual dysfunction assessed using the core lower urinary tract symptom score and International Index of Erectile Function-5 questionnaires. Aging Male. 2012;15:111–14. doi: 10.3109/13685538.2011.646342. [DOI] [PubMed] [Google Scholar]
- 19.Hermanns-Le T, Scheen A, Pierard GE. Acanthosis nigricans associated with insulin resistance: pathophysiology and management. Am J Clin Dermatol. 2004;5:199–203. doi: 10.2165/00128071-200405030-00008. [DOI] [PubMed] [Google Scholar]
- 20.Saad F, Aversa A, Isidori AM, et al. Testosterone as potential effective therapy in treatment of obesity in men with testosterone deficiency: a review. Curr Diabetes Rev. 2012;8:131–43. doi: 10.2174/157339912799424573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corona G, Rastrelli G, Vignozzi L, et al. Testosterone, cardiovascular disease and the metabolic syndrome. Best Pract Res Clin Endocrinol Metab. 2011;25:337–53. doi: 10.1016/j.beem.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Corona G, Rastrelli G, Morelli A, et al. Hypogonadism and metabolic syndrome. J Endocrinol Invest. 2011;34:557–67. doi: 10.3275/7806. [DOI] [PubMed] [Google Scholar]
- 23.Brunton SA, Sadovsky R. Late-onset male hypogonadism and testosterone replacement therapy in primary care. J Fam Pract. 2010;59:1–8. [PubMed] [Google Scholar]
- 24.Bhasin S, Cunningham GR, Hayes FJ, et al. Task Force, Endocrine Society. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536–59. doi: 10.1210/jc.2009-2354. [DOI] [PubMed] [Google Scholar]
- 25.Schneider G, Nienhaus K, Gromoll J, et al. Depressive symptoms in ≥50-year-old males and their relation to genetic androgen receptor polymorphism and sex hormone levels in 3 different samples. Am J Geront Psychiatr. 2011;19:274–83. doi: 10.1097/JGP.0b013e3181e70c22. [DOI] [PubMed] [Google Scholar]
- 26.Zitzmann M, Faber S, Nieschlag E. Association of specific symptoms and metabolic risks with serum testosterone in older men. J Clin Endocrinol Metab. 2006;91:4335–43. doi: 10.1210/jc.2006-0401. [DOI] [PubMed] [Google Scholar]
- 27.Mulligan T, Frick MF, Zuraw QC, et al. Prevalence of hypogonadism in males aged at least 45 years: the HIM study. Int J Clin Pract. 2006;60:762–9. doi: 10.1111/j.1742-1241.2006.00992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaplan SA, O'Neill E, Lowe RS, et al. Testosterone in aging men with benign prostatic hyperplasia: data from the Proscar Long-term Efficacy and Safety Study (PLESS) Aging Male. 2013;16:48–51. doi: 10.3109/13685538.2013.773421. [DOI] [PubMed] [Google Scholar]
- 29.Schatzl G, Brossner C, Schmid S, et al. Endocrine status in elderly men with lower urinary tract symptoms: correlation of age, hormonal status, and lower urinary tract function. The Prostate Study Group of the Austrian Society of Urology. Urology. 2000;55:397–402. doi: 10.1016/s0090-4295(99)00473-2. [DOI] [PubMed] [Google Scholar]
- 30.Higano C. Androgen deprivation therapy: monitoring and managing the complications. Hematol Oncol Clin North Am. 2006;20:909–23. doi: 10.1016/j.hoc.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 31.Choong K, Basaria S. Emerging cardiometabolic complications of androgen deprivation therapy. Aging Male. 2010;13:1–9. doi: 10.3109/13685530903410625. [DOI] [PubMed] [Google Scholar]
- 32.Sharifi N, Gulley JL, Dahut WL. Androgen deprivation therapy for prostate cancer. JAMA. 2005;294:238–44. doi: 10.1001/jama.294.2.238. [DOI] [PubMed] [Google Scholar]
- 33.Joly F, Alibhai SM, Galica J, et al. Impact of androgen deprivation therapy on physical and cognitive function, as well as quality of life of patients with non metastatic prostate cancer. J Urol. 2006;176:2443–7. doi: 10.1016/j.juro.2006.07.151. [DOI] [PubMed] [Google Scholar]
- 34.Mohile SG, Bylow K, Dale W, et al. A pilot study of the vulnerable elders survey-13 compared with the comprehensive geriatric assessment for identifying disability in older patients with prostate cancer who receive androgen ablation. Cancer. 2007;109:802–10. doi: 10.1002/cncr.22495. [DOI] [PubMed] [Google Scholar]
- 35.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 36.Saad F, Gooren LJ. Late onset hypogonadism of men is not equivalent to the menopause. Maturitas. 2014;79:52–7. doi: 10.1016/j.maturitas.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 37.Cattabiani C, Basaria S, Ceda GP, et al. Relationship between testosterone deficiency and cardiovascular risk and mortality in adult men. J Endocrinol Invest. 2012;35:104–20. doi: 10.3275/8061. [DOI] [PubMed] [Google Scholar]
- 38.Lee DM, Tajar A, Pye SR, et al. The EMAS Study Group. Association of hypogonadism with vitamin D status: the European Male Ageing Study. Eur J Endocrinol. 2012;166:77–85. doi: 10.1530/EJE-11-0743. [DOI] [PubMed] [Google Scholar]
- 39.Pilz S, Frisch S, Koertke H, et al. Effect of vitamin D supplementation on testosterone levels in men. Horm Metab Res. 2011;43:223–5. doi: 10.1055/s-0030-1269854. [DOI] [PubMed] [Google Scholar]
- 40.Wehr E, Pilz S, Boehm BO, et al. Association of vitamin D status with serum androgen levels in men. Clin Endocrinol. 2010;73:243–8. doi: 10.1111/j.1365-2265.2009.03777.x. [DOI] [PubMed] [Google Scholar]
- 41.Bremner AP, Feddema P, Leedman PJ, et al. Age-related changes in thyroid function: a longitudinal study of a community-based cohort. J Clin Endocrinol Metab. 2012;97:1554–62. doi: 10.1210/jc.2011-3020. [DOI] [PubMed] [Google Scholar]
- 42.Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) J Clin Endocrinol Metab. 2002;87:489–99. doi: 10.1210/jcem.87.2.8182. [DOI] [PubMed] [Google Scholar]
- 43.Brochmann H, Bjoro T, Gaarder PI, et al. Prevalence of thyroid dysfunction in elderly subjects. A randomized study in a Norwegian rural community (Naeroy) Acta Endocrinol (Copenh) 1988;117:7–12. doi: 10.1530/acta.0.1170007. [DOI] [PubMed] [Google Scholar]
- 44.Boucai L, Hollowell JG, Surks MI. An approach for development of age-, gender-, and ethnicity-specific thyrotropin reference limits. Thyroid. 2011;21:5–11. doi: 10.1089/thy.2010.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dobs AS, Few WL, III, Blackman MR, et al. Serum hormones in men with human immunodeficiency virus-associated wasting. J Clin Endocrinol Metab. 1996;81:4108–12. doi: 10.1210/jcem.81.11.8923868. [DOI] [PubMed] [Google Scholar]
- 46.Khera M, Bhattacharya RK, Blick G, et al. The effect of testosterone supplementation on depression symptoms in hypogonadal men from the Testim Registry in the US (TRiUS) Aging Male. 2012;15:14–21. doi: 10.3109/13685538.2011.606513. [DOI] [PubMed] [Google Scholar]
- 47.Knegtering H, van der Moolen AE, Castelein S, et al. What are the effects of antipsychotics on sexual dysfunctions and endocrine functioning? Psychoneuroendocrinology. 2003;28:109–23. doi: 10.1016/s0306-4530(02)00130-0. [DOI] [PubMed] [Google Scholar]
- 48.Molitch ME. Drugs and prolactin. Pituitary. 2008;11:209–18. doi: 10.1007/s11102-008-0106-6. [DOI] [PubMed] [Google Scholar]
- 49.Martens HF, Sheets PK, Tenover JS, et al. Decreased testosterone levels in men with rheumatoid arthritis: effect of low dose prednisone therapy. J Rheumatol. 1994;21:1427–31. [PubMed] [Google Scholar]
- 50.Schooling CM, Au Yeung SL, Freeman G, Cowling BJ. The effect of statins on testosterone in men and women, a systematic review and meta-analysis of randomized controlled trials. BMC Med. 2013;11:57. doi: 10.1186/1741-7015-11-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aloisi AM, Aurilio C, Bachiocco V, et al. Endocrine consequences of opioid therapy. Psychoneuroendocrinology. 2009;34:162–8. doi: 10.1016/j.psyneuen.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 52.Reddy RG, Aung T, Karavitaki N, Wass JAH. Opioid induced hypogonadism. BMJ. 2010;341:605–60. doi: 10.1136/bmj.c4462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Isidori AM, Lenzi A. Risk factors for androgen decline in older males: lifestyle, chronic diseases and drugs. J Endocrinol Invest. 2005;28:14–22. [PubMed] [Google Scholar]
- 54.Rosner W, Auchus RJ, Azziz R, et al. Utility, limitations, and pitfalls in measuring testosterone: an Endocrine Society Position Statement. J Clin Endocrinol Metab. 2007;92:405–13. doi: 10.1210/jc.2006-1864. [DOI] [PubMed] [Google Scholar]
- 55.Morgentaler A, Khera M, Maggi M, Zitzmann M. Commentary: who is a candidate for testosterone therapy? A synthesis of international expert opinions. J Sex Med. 2014;11:1636–45. doi: 10.1111/jsm.12546. [DOI] [PubMed] [Google Scholar]
- 56.Kacker R, Hornstein A, Morgentaler A. Free testosterone by direct and calculated measurement versus equilibrium dialysis in a clinical population. Aging Male. 2013;16:164–8. doi: 10.3109/13685538.2013.835800. [DOI] [PubMed] [Google Scholar]
- 57.Diver MJ, Imtiaz KE, Ahmad AM, et al. Diurnal rhythms of serum total, free and bioavailable testosterone and of SHBG in middle-aged men compared with those in young men. Clin Endocrinol (Oxf) 2003;58:710–17. doi: 10.1046/j.1365-2265.2003.01772.x. [DOI] [PubMed] [Google Scholar]
- 58.Crawford ED, Barqawi AB, O'Donnell C, Morgentaler A. The association of time of day and serum testosterone concentration in a large screening population. BJU Int. 2007;100:509–13. doi: 10.1111/j.1464-410X.2007.07022.x. [DOI] [PubMed] [Google Scholar]
- 59.Caronia LM, Dwyer AA, Hayden D, et al. Abrupt decrease in serum testosterone levels after an oral glucose load in men: implications for screening for hypogonadism. Clin Endocrinol (Oxf) 2013;78:291–6. doi: 10.1111/j.1365-2265.2012.04486.x. [DOI] [PubMed] [Google Scholar]
- 60.Bhasin S, Pencina M, Jasuja GK, et al. Reference ranges for testosterone in men generated using liquid chromatography tandem mass spectrometry in a community-based sample of healthy nonobese young men in the Framingham Heart Study and applied to three geographically distinct cohorts. J Clin Endocrinol Metab. 2011;96:2430–9. doi: 10.1210/jc.2010-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chamberlain NL, Driver ED, Miesfeld RL. The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function. Nucleic Acids Res. 1994;22:3181–6. doi: 10.1093/nar/22.15.3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rajender S, Singh L, Thangaraj K. Phenotypic heterogeneity of mutations in androgen receptor gene. Asian J Androl. 2007;9:147–79. doi: 10.1111/j.1745-7262.2007.00250.x. [DOI] [PubMed] [Google Scholar]
- 63.Zitzmann M. The role of the CAG repeat androgen receptor polymorphism in andrology. Front Horm Res. 2009;37:52–61. doi: 10.1159/000175843. [DOI] [PubMed] [Google Scholar]
- 64.Zitzmann M. Pharmacogenetics of testosterone replacement therapy. Pharmacogenomics. 2009;10:1341–9. doi: 10.2217/pgs.09.58. [DOI] [PubMed] [Google Scholar]
- 65.Holm AC, Fredrikson MG, Theodorsson E, et al. Change in testosterone concentrations over time is a better predictor than the actual concentrations for symptoms of late onset hypogonadism. Aging Male. 2011;14:249–56. doi: 10.3109/13685538.2011.582527. [DOI] [PubMed] [Google Scholar]
- 66.Canale D, Caglieresi C, Moschini C, et al. Androgen receptor polymorphism (CAG repeats) and androgenicity. Clin Endocrinol (Oxf) 2005;63:356–61. doi: 10.1111/j.1365-2265.2005.02354.x. [DOI] [PubMed] [Google Scholar]
- 67.Berglund LH, Prytz HS, Perski A, Svartberg J. Testosterone levels and psychological health status in men from a general population: the Troms⊘ study. Aging Male. 2011;14:37–41. doi: 10.3109/13685538.2010.522276. [DOI] [PubMed] [Google Scholar]
- 68.Scovell JM, Ramasamy R, Wilken N, et al. Hypogonadal symptoms in young men are associated with a serum total testosterone threshold of 400 ng/dL. BJU Int. 2014. [Epub ahead of print] doi: 10.1111/bju.12970. [DOI] [PubMed]
- 69.Morgentaler A. Commentary: guideline for male testosterone therapy: a clinician's perspective. J Clin Endocrinol Metab. 2007;92:416–17. doi: 10.1210/jc.2006-2629. [DOI] [PubMed] [Google Scholar]
- 70.Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–72. doi: 10.1210/jcem.84.10.6079. [DOI] [PubMed] [Google Scholar]
- 71.Tajar A, McBeth J, Lee DM, et al. European Male Aging Study Group. Elevated levels of gonadotrophins but not sex steroids are associated with musculoskeletal pain in middle-aged and older European men. Pain. 2011;152:1495–501. doi: 10.1016/j.pain.2011.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Citron JT, Ettinger B, Rubinoff H, et al. Prevalence of hypothalamic-pituitary imaging abnormalities in impotent men with secondary hypogonadism. J Urol. 1996;155:529–33. [PubMed] [Google Scholar]
- 73.Bunch TJ, Abraham D, Wang S, Meikle AW. Pituitary radiographic abnormalities and clinical correlates of hypogonadism in elderly males presenting with erectile dysfunction. Aging Male. 2002;5:38–46. [PubMed] [Google Scholar]
- 74.Araujo AB, O'Donnell A, Brambilla DJ, et al. Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the Massachusetts male aging study. J Clin Endocrinol Metab. 2004;89:5920–6. doi: 10.1210/jc.2003-031719. [DOI] [PubMed] [Google Scholar]
- 75.Vermeulen A. Hormonal cut-offs of partial androgen deficiency: a survey of androgen assays. J Endocrinol Invest. 2005;28:28–31. [PubMed] [Google Scholar]
- 76.Saad F, Aversa A, Isidori AM, et al. Onset of effects of testosterone treatment and time span until maximum effects are achieved. Eur J Endocrinol. 2011;165:675–85. doi: 10.1530/EJE-11-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hackett G, Cole N, Bhartia M, et al. Blast Study Group. The response to testosterone undecanoate in men with type 2 diabetes is dependent on achieving threshold serum levels (the BLAST study) Int J Clin Pract. 2014;68:203–15. doi: 10.1111/ijcp.12235. [DOI] [PubMed] [Google Scholar]
- 78.Snyder PJ, Peachey H, Berlin JA, et al. Effects of testosterone replacement in hypogonadal men. J Clin Endocrinol Metab. 2000;85:2670–7. doi: 10.1210/jcem.85.8.6731. [DOI] [PubMed] [Google Scholar]
- 79.Aversa A, Bruzziches R, Francomano D, et al. Effects of long-acting testosterone undecanoate on bone mineral density in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 36 months controlled study. Aging Male. 2012;15:96–102. doi: 10.3109/13685538.2011.631230. [DOI] [PubMed] [Google Scholar]
- 80.Haider A, Meergans U, Traish A, et al. Progressive improvement of T-scores in men with osteoporosis and subnormal serum testosterone levels upon treatment with testosterone over six years. Int J Endocrinol. 2014;2014:496948. doi: 10.1155/2014/496948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Isidori AM, Giannetta E, Greco EA, et al. Effects of testosterone on body composition, bone metabolism and serum lipid profile in middle-aged men a meta-analysis. Clin Endocrinol (Oxf) 2005;63:280–93. doi: 10.1111/j.1365-2265.2005.02339.x. [DOI] [PubMed] [Google Scholar]
- 82.Bhasin S, Calof OM, Storer TW, et al. Drug insight: testosterone and selective androgen receptor modulators as anabolic therapies for chronic illness and aging. Nat Clin Pract Endocrinol Metab. 2006;2:146–59. doi: 10.1038/ncpendmet0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rodrıguez-Tolra J, Torremude Bareda J, Del Rio L, et al. Effects of testosterone treatment on body composition in males with testosterone deficiency syndrome. Aging Male. 2013;16:184–90. doi: 10.3109/13685538.2013.839648. [DOI] [PubMed] [Google Scholar]
- 84.Saad F, Haider A, Doros G, Traish A. Long-term treatment of hypogonadal men with testosterone produces substantial and sustained weight loss. Obesity (Silver Spring) 2013;21:1975–81. doi: 10.1002/oby.20407. [DOI] [PubMed] [Google Scholar]
- 85.Yassin AA, Doros G. Testosterone therapy in hypogonadal men results in sustained and clinically meaningful weight loss. Clin Obesity. 2013;3:73–83. doi: 10.1111/cob.12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Francomano D, Ilacqua A, Bruzziches R, et al. Effects of 5-year treatment with testosterone undecanoate on lower urinary tract symptoms in obese men with hypogonadism and metabolic syndrome. Urology. 2014;83:167–74. doi: 10.1016/j.urology.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 87.Haider A, Yassin A, Doros G, Saad F. Effects of long-term testosterone therapy on patients with “diabesity”: results of observational studies of pooled analyses in obese hypogonadal men with type 2 diabetes. Int J Endocrinol. 2014;2014:683515. doi: 10.1155/2014/683515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Krasnoff JB, Basaria S, Pencina MJ, et al. Free testosterone levels are associated with mobility limitation and physical performance in community-dwelling men: the Framingham Offspring Study. J Clin Endocrinol Metab. 2010;95:2790–9. doi: 10.1210/jc.2009-2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kacker R, Conners W, Zade J, Morgentaler A. Bone mineral density and response to treatment in men younger than 50 years with testosterone deficiency and sexual dysfunction or infertility. J Urol. 2014;191:1072–6. doi: 10.1016/j.juro.2013.10.070. [DOI] [PubMed] [Google Scholar]
- 90.Drake MT, Murad MH, Mauck KF, et al. Risk factors for low bone mass-related fractures in men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2012;97:1861–70. doi: 10.1210/jc.2011-3058. [DOI] [PubMed] [Google Scholar]
- 91.Kanis JA, Oden A, Johansson H, et al. FRAX and its applications to clinical practice. Bone. 2009;44:734–43. doi: 10.1016/j.bone.2009.01.373. [DOI] [PubMed] [Google Scholar]
- 92.Watts NB, Adler RA, Bilezikian JP, et al. Endocrine Society. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:1802–22. doi: 10.1210/jc.2011-3045. [DOI] [PubMed] [Google Scholar]
- 93.Orwoll E, Lambert LC, Marshall LM, et al. Endogenous testosterone levels, physical performance, and fall risk in older men. Arch Intern Med. 2006;166:2124–31. doi: 10.1001/archinte.166.19.2124. [DOI] [PubMed] [Google Scholar]
- 94.Zitzmann M, Brune M, Vieth V, Nieschlag E. Monitoring bone density in hypogonadal men by quantitative phalangeal ultrasound. Bone. 2002;31:422–9. doi: 10.1016/s8756-3282(02)00831-1. [DOI] [PubMed] [Google Scholar]
- 95.Corona G, Isidori AM, Buvat J, et al. Testosterone supplementation and sexual function: a meta-analysis study. J Sex Med. 2014;11:1577–92. doi: 10.1111/jsm.12536. [DOI] [PubMed] [Google Scholar]
- 96.Kalinchenko SY, Kozlov GI, Gontcharov NP, Katsiya GV. Oral testosterone undecanoate reverses erectile dysfunction associated with diabetes mellitus in patients failing on sildenafil citrate therapy alone. Aging Male. 2003;6:94–9. [PubMed] [Google Scholar]
- 97.Zitzmann M, Mattern A, Hanisch J, et al. IPASS: a study on the tolerability and effectiveness of injectable testosterone undecanoate for the treatment of male hypogonadism in a worldwide sample of 1,438 men. J Sex Med. 2013;10:579–88. doi: 10.1111/j.1743-6109.2012.02853.x. [DOI] [PubMed] [Google Scholar]
- 98.Tan WS, Ng CJ, Khoo EM, et al. The triad of erectile dysfunction, testosterone deficiency syndrome and metabolic syndrome: findings from a multi-ethnic Asian men study (The Subang Men's Health Study) Aging Male. 2011;14:231–6. doi: 10.3109/13685538.2011.597463. [DOI] [PubMed] [Google Scholar]
- 99.Kapoor D, Aldred H, Clark S, et al. Clinical and biochemical assessment of hypogonadism in men with type 2 diabetes: correlations with bioavailable testosterone and visceral adiposity. Diabetes Care. 2007;30:911–17. doi: 10.2337/dc06-1426. [DOI] [PubMed] [Google Scholar]
- 100.Tajar A, Huhtaniemi IT, O'Neill TW, et al. EMAS Group. Characteristics of androgen deficiency in late-onset hypogonadism: results from the European Male Aging Study (EMAS) J Clin Endocrinol Metab. 2012;97:1508–16. doi: 10.1210/jc.2011-2513. [DOI] [PubMed] [Google Scholar]
- 101.Tsujimura A, Miyagawa Y, Takezawa K, et al. Is low testosterone concentration a risk factor for metabolic syndrome in healthy middle-aged men? Urology. 2013;82:814–19. doi: 10.1016/j.urology.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 102.Aversa A, Bruzziches R, Francomano D, et al. Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late onset hypogonadism and metabolic syndrome: results from a 24-months, randomized double blind placebo-controlled study. J Sex Med. 2010;7:3495–503. doi: 10.1111/j.1743-6109.2010.01931.x. [DOI] [PubMed] [Google Scholar]
- 103.Strollo F, Strollo G, More M, et al. Low-intermediate dose testosterone replacement therapy by different pharmaceutical preparations improves frailty score in elderly hypogonadal hyperglycaemic patients. Aging Male. 2013;16:33–7. doi: 10.3109/13685538.2013.773305. [DOI] [PubMed] [Google Scholar]
- 104.Heufelder AE, Saad F, Bunck MC, Gooren L. Fifty-two-week treatment with diet and exercise plus transdermal testosterone reverses the metabolic syndrome and improves glycemic control in men with newly diagnosed type 2 diabetes and subnormal plasma testosterone. J Androl. 2009;30:726–33. doi: 10.2164/jandrol.108.007005. [DOI] [PubMed] [Google Scholar]
- 105.Akishita M, Hashimoto M, Ohike Y, et al. Low testosterone level is an independent determinant of endothelial dysfunction in men. Hyperten Res. 2007;30:1029–34. doi: 10.1291/hypres.30.1029. [DOI] [PubMed] [Google Scholar]
- 106.Muller M, van den Beld AW, Bots ML, et al. Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation. 2004;109:2074–9. doi: 10.1161/01.CIR.0000125854.51637.06. [DOI] [PubMed] [Google Scholar]
- 107.Kang SM, Jang Y, Kim JY, et al. Effect of oral administration of testosterone on brachial arterial vasoreactivity in men with coronary artery disease. Am J Cardiol. 2002;89:862–4. doi: 10.1016/s0002-9149(02)02202-6. [DOI] [PubMed] [Google Scholar]
- 108.Zitzmann M, Vorona E, Wenk M, et al. Testosterone administration decreases carotid artery intima media thickness as indicator of vascular damage in middle-aged overweight men. J Androl. 2008;29:54–5. [Google Scholar]
- 109.Herring MJ, Mesbah Oskui P, Hale SL, Kloner RA. Testosterone and the cardiovascular system: a comprehensive review of the basic science literature. J Am Heart Assoc. 2013;2:e000271. doi: 10.1161/JAHA.113.000271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nettleship JE, Pugh PJ, Channer KS, et al. Inverse relationship between serum levels of interleukin-1beta and testosterone in men with stable coronary artery disease. Horm Metab Res. 2007;39:366–71. doi: 10.1055/s-2007-976543. [DOI] [PubMed] [Google Scholar]
- 111.Kalinchenko SY, Tishova YA, Mskhalaya GJ, et al. Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: the double-blinded placebo-controlled Moscow study. Clin Endocrinol (Oxf) 2010;73:602–12. doi: 10.1111/j.1365-2265.2010.03845.x. [DOI] [PubMed] [Google Scholar]
- 112.Kelly DM, Jones TH. Testosterone: a metabolic hormone in health and disease. J Endocrinol. 2013;217:R25–45. doi: 10.1530/JOE-12-0455. [DOI] [PubMed] [Google Scholar]
- 113.Vodo S, Bechi N, Petroni A, et al. Testosterone-induced effects on lipids and inflammation. Mediators Inflamm. 2013;2013:183041. doi: 10.1155/2013/183041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Corona G, Maseroli E, Rastrelli G, et al. Cardiovascular risk associated with testosterone-boosting medications: a systematic review and meta-analysis. Expert Opin Drug Saf. 2014;13:1327–51. doi: 10.1517/14740338.2014.950653. [DOI] [PubMed] [Google Scholar]
- 115.Tan Robert S, Cook Kelly R, Reilly William G. Testosterone therapy is not associated with higher risk of myocardial infarction or stroke: the low T experience. Presented at American Association of Clinical Endocrinologists 23rd Annual Scientific and Clinical Congress, Las Vegas, Nevada, May 13–18, 2014. Abstract # 1353.
- 116.Tan Robert S, Cook Kelly R, Reilly William G. Testosterone therapy is not associated with increased cardiovascular risk in study registry. J Men Health. 2014;11:139–139. [Google Scholar]
- 117.Araujo AB, Dixon JM, Suarez EA, et al. Endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011;96:3007–19. doi: 10.1210/jc.2011-1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hyde Z, Norman PE, Flicker L, et al. Low free testosterone predicts mortality from cardiovascular disease, but not other causes. The Health in Men Study. J Clin Endocrinol Metab. 2012;97:179–89. doi: 10.1210/jc.2011-1617. [DOI] [PubMed] [Google Scholar]
- 119.Shores MM, Smith NL, Forsberg CW, et al. Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab. 2012;97:2050–8. doi: 10.1210/jc.2011-2591. [DOI] [PubMed] [Google Scholar]
- 120.Yeap Bu B. Testosterone therapy and mortality in US veterans. Asian J Androl. 2012;14:667–8. doi: 10.1038/aja.2012.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wu FC. Caveat emptor: does testosterone treatment reduce mortality in men? J Clin Endocrinol Metab. 2012;97:1884–6. doi: 10.1210/jc.2012-1977. [DOI] [PubMed] [Google Scholar]
- 122.Zarrouf FA, Artz S, Griffith J, et al. Testosterone and depression: systematic review and meta-analysis. J Psychiatr Pract. 2009;15:289–305. doi: 10.1097/01.pra.0000358315.88931.fc. [DOI] [PubMed] [Google Scholar]
- 123.Giltay EJ, Tishova YA, Mskhalaya GJ, et al. Effects of testosterone supplementation on depressive symptoms and sexual dysfunction in hypogonadal men with the metabolic syndrome. J Sex Med. 2010;7:2572–82. doi: 10.1111/j.1743-6109.2010.01859.x. [DOI] [PubMed] [Google Scholar]
- 124.Morley JE, Kaiser F, Raum WJ, et al. Potentially predictive and manipulable blood serum correlates of aging in the healthy human male: progressive decreases in bioavailable testosterone, dehydroepiandrosterone sulfate, and the ratio of insulin-like growth factor 1 to growth hormone. Proc Natl Acad Sci USA. 1997;94:7537–42. doi: 10.1073/pnas.94.14.7537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Maggio M, Dall'Aglio E, Lauretani F, et al. The hormonal pathway to cognitive impairment in older men. J Nutr Health Aging. 2012;16:40–54. doi: 10.1007/s12603-012-0002-7. [DOI] [PubMed] [Google Scholar]
- 126.Janowsky JS. Thinking with your gonads: testosterone and cognition. Trends Cogn Sci. 2006;10:77–82. doi: 10.1016/j.tics.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 127.Etgen T, Sander D, Bickel H, Forstl H. Mild cognitive impairment and dementia: the importance of modifiable risk factors. Dtsch Arztebl Int. 2011;108:743–50. doi: 10.3238/arztebl.2011.0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kim JW, Oh MM, Yoon CY, et al. Nocturnal polyuria and decreased serum testosterone: is there an association in men with lower urinary tract symptoms? Int J Urol. 2014;21:518–23. doi: 10.1111/iju.12345. [DOI] [PubMed] [Google Scholar]
- 129.Pearl JA, Berhanu D, Francois N, et al. Testosterone supplementation does not worsen lower urinary tract symptoms. J Urol. 2013;190:1828–33. doi: 10.1016/j.juro.2013.05.111. [DOI] [PubMed] [Google Scholar]
- 130.Shigehara K, Sugimoto K, Konaka H, et al. Androgen replacement therapy contributes to improving lower urinary tract symptoms in patients with hypogonadism and benign prostate hypertrophy: a randomised controlled study. Aging Male. 2011;14:53–8. doi: 10.3109/13685538.2010.518178. [DOI] [PubMed] [Google Scholar]
- 131.Yassin DJ, El Douaihy Y, Yassin AA, et al. Lower urinary tract symptoms improve with testosterone replacement therapy in men with late-onset hypogonadism: 5-year prospective, observational and longitudinal registry study. World J Urol. 2014;32:1049–54. doi: 10.1007/s00345-013-1187-z. [DOI] [PubMed] [Google Scholar]
- 132.Pastuszak AW, Pearlman AM, Lai WS, et al. Testosterone replacement therapy in patients with prostate cancer after radical prostatectomy. J Urol. 2013;190:639–44. doi: 10.1016/j.juro.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Morgentaler A, Lipshultz LI, Bennett R, et al. Testosterone therapy in men with untreated prostate cancer. J Urol. 2011;185:1256–60. doi: 10.1016/j.juro.2010.11.084. [DOI] [PubMed] [Google Scholar]
- 134.Morgentaler A, Traish AM. Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth. Eur Urol. 2009;55:310–20. doi: 10.1016/j.eururo.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 135.Roddam AW, Allen NE, Appleby P, Key TJ Endogenous Hormones and Prostate Cancer Collaborative Group. Endogenous sex hormones and prostate cancer: a collaborative analysis of 18 prospective studies. J Natl Cancer Inst. 2008;100:170–83. doi: 10.1093/jnci/djm323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fernandez-Balsells MM, Murad MH, Lane M, et al. Clinical review. 1: adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2010;95:2560–75. doi: 10.1210/jc.2009-2575. [DOI] [PubMed] [Google Scholar]
- 137.Haider A, Zitzmann M, Doros G, et al. Incidence of prostate cancer in hypogonadal men receiving testosterone therapy: observations from 5-year median follow up of 3 registries. J Urol. 2014;193:80–6. doi: 10.1016/j.juro.2014.06.071. [DOI] [PubMed] [Google Scholar]
- 138.Calof OM, Singh AB, Lee ML, et al. Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol. 2005;60A:1451–7. doi: 10.1093/gerona/60.11.1451. [DOI] [PubMed] [Google Scholar]
- 139.Morgentaler A, Benesh JA, Denes BS, et al. Factors influencing prostate-specific antigen response among men treated with testosterone therapy for 6 months. J Sex Med. 2014;11:2818–25. doi: 10.1111/jsm.12657. [DOI] [PubMed] [Google Scholar]
- 140.Rhoden EL, Morgentaler A. Risks of testosterone-replacement therapy and recommendations for monitoring. N Engl J Med. 2004;350:482–92. doi: 10.1056/NEJMra022251. [DOI] [PubMed] [Google Scholar]
- 141.Carter HB, Pearson JD, Metter EJ, et al. Longitudinal evaluation of prostate-specific antigen in men with and without prostate disease. JAMA. 1992;267:2215–20. [PMC free article] [PubMed] [Google Scholar]
- 142.Dobs AS, Meikle AW, Arver S, et al. Pharmacokinetics, efficacy, and safety of a permeation-enhanced testosterone transdermal system in comparison with bi-weekly injections of testosterone enanthate for the treatment of hypogonadal men. J Clin Endocrinol Metab. 1999;84:3469–78. doi: 10.1210/jcem.84.10.6078. [DOI] [PubMed] [Google Scholar]
- 143.Jones TH, Saad F. The effects of testosterone on risk factors for, and the mediators of, the atherosclerotic process. Atherosclerosis. 2009;207:318–27. doi: 10.1016/j.atherosclerosis.2009.04.016. [DOI] [PubMed] [Google Scholar]


