Abstract
Objective
To evaluate associations between handwashing promotion and child growth and development.
Design
Cluster randomized controlled trial.
Setting
Informal settlements in Karachi, Pakistan.
Participants
A total of 461 children who were enrolled in a trial of household-level handwashing promotion in 2003 and were younger than 8 years at reassessment in 2009.
Interventions
In 2003, neighborhoods were randomized to control (n=9), handwashing promotion (n=9), or handwashing promotion and drinking water treatment (n=10); intervention households received free soap and weekly handwashing promotion for 9 months.
Main Outcome Measures
Anthropometrics and developmental quotients measured with the Battelle Developmental Inventory II at 5 to 7 years of age.
Results
Overall, 24.9% (95% CI, 20.0%–30.6%) and 22.1% (95% CI, 18.0%–26.8%) of children had z scores that were more than 2 SDs below the expected z scores for height and body mass index for age, respectively; anthropometrics did not differ significantly across study groups. Global developmental quotients averaged 104.4 (95% CI, 101.9–107.0) among intervention children and 98.3 (95% CI, 93.1–103.4) among control children (P=.04). Differences of similar magnitude were measured across adaptive, personal-social, communication, cognitive, and motor domains.
Conclusions
Although growth was similar across groups, children randomized to the handwashing promotion during their first 30 months of age attained global developmental quotients 0.4 SDs greater than those of control children at 5 to 7 years of age. These gains are comparable to those of at-risk children enrolled in publicly funded preschools in the United States and suggest that handwashing promotion could improve child wellbeing and societal productivity.
Trial Registration
clinicaltrials.gov Identifier: NCT01538953
The first few years of life are critical to children’s cognitive, social, emotional, and motor development, and efforts to preserve children’s developmental potential can have diverse and far-reaching benefits. A recent review1 of data from developing countries reported an association between higher developmental quotients or IQs in early childhood and improved school outcomes, including reduced school dropout and greater number of grades completed. Each additional year of schooling completed by an individual may, in turn, yield 9.7% higher wages.2 Furthermore, a meta-analysis of 16 studies found that a 1-SD increase in childhood cognitive test scores was associated with a 24% decreased risk of adult mortality.3 However, an estimated 200 million children are at risk for impaired development because of their social and environmental conditions.1
The determinants of children’s development are complex and multifactorial, and several of the implicated causes of lost developmental potential—stunting, micronutrient deficiencies, and diarrhea—are likely tightly intertwined.4 High diarrheal disease burdens before 2 years of age have been linked with delayed school entry and poorer performance on intelligence tests,5,6 whereas multiple infections with Giardia per year were associated with a 4-point (0.27 SD) deficit on a standardized intelligence test at 9 years of age.7
Although handwashing promotion programs have been associated with 30% to 50% reductions in diarrheal disease,8,9 it is unclear how handwashing relates to children’s development. In 2003, families in Karachi, Pakistan, with young children were enrolled in a study to evaluate the effects of promoting drinking water disinfection and handwashing with soap.10 Participants who received the interventions experienced less than half the diarrhea of control participants. We returned to this population approximately 5 years later to evaluate whether intensive handwashing promotion early in life is associated with medium-term growth and development. Because of resource constraints, we were unable to assess the developmental effects of drinking water disinfection alone.
METHODS
SETTING
The study was set in multiethnic squatter settlements in central Karachi, in areas that typically have access to at least 2 hours of running water per week. Health-Oriented Preventive Education (HOPE), a local nongovernmental organization that administers health clinics, schools, and community development programming in Pakistan, conducted the field work.
RANDOMIZATION, INTERVENTIONS, AND MASKING
The 2003 study was a cluster randomized controlled trial of handwashing and drinking water interventions.10 Neighborhoods were used as the unit of randomization because components of the interventions, such as community meetings, occurred at this level. We identified 47 neighborhoods that received at least 1 hour of running water twice weekly and enrolled households containing a child younger than 5 years. The neighborhoods were randomized as previously described to 5 groups: 10 received sodium hypochlorite solution for drinking water treatment; 9 received a flocculent-disinfectant product for drinking water treatment; 10 received soap, handwashing promotion, and flocculent-disinfectant for drinking water treatment; 9 received soap and handwashing promotion; and 9 served as the control group. Field workers visited households at least weekly from April to December 2003 to assess diarrhea incidence; households assigned to interventions also regularly received instruction and encouragement to use the products supplied as part of the respective interventions. Children born to enrolled families during the follow-up period were also enrolled.
In 2005, we reenrolled households from the control group and the two study groups that received soap and handwashing promotion to assess retention of handwashing knowledge and practices and to determine whether differences in diarrhea rates were sustained after the original study.11 Households were visited weekly from August 2005 to September 2006 for surveillance of diarrhea and hand soap purchases; we did not provide health education or handwashing or water treatment supplies during this study.
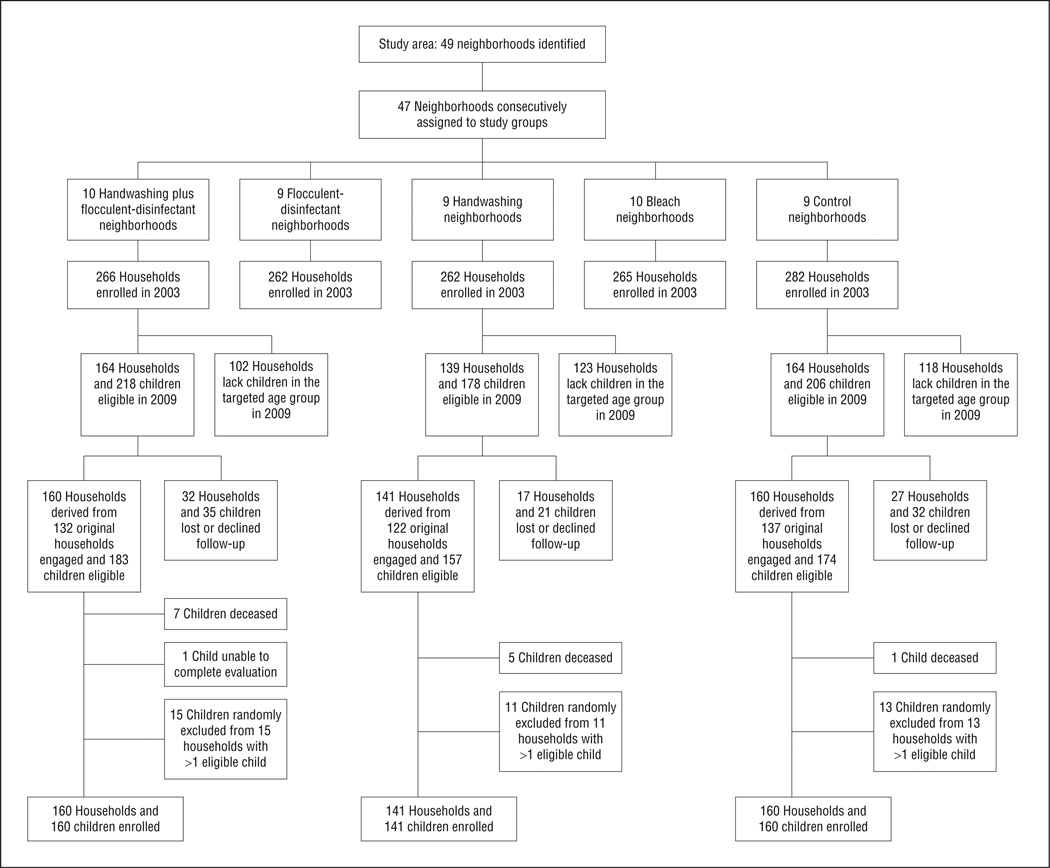
The current study aimed to learn about the effects of these interventions during a critical window in child development. Between February and December 2009, we attempted to reenroll children who were enrolled in these same 3 study groups and who were younger than 30 months at the conclusion of the 2003 study. We excluded children who would have been 96 months or older at the time of the current study because the developmental inventory we used had an upper age boundary of 96 months.12–14 To avoid multilevel clustering, we enrolled a single child from each household. If a household contained more than one living eligible child, we used a random number generator to assign a unique number to each child in the household and then invited the child associated with the largest number to enroll in the current study (Figure 1).
Figure 1.
Flow of participants through the study.
Although group allocation was not disclosed to the field workers who conducted household interviews during this study, some field workers had been employed during the 2003 study and might have recalled the original study allocations. Group allocation was concealed from personnel who conducted and scored the developmental tests.
MEASUREMENTS
A parent from each household was interviewed about household characteristics, handwashing practices, and the child’s schooling status and general health using a standard questionnaire in the local language. Developmental testing was performed using the full-length Battelle Developmental Inventory II (BDI-2). The BDI-2 is a 450-item, norm-referenced developmental testing instrument designed to assess adaptive, cognitive, motor, personal-social, and communication skills among children younger than 96 months. Results can be reported as age-adjusted domain-level developmental quotients and a composite developmental quotient for each child, with a mean (SD) score of 100 (15).13 The instrument was translated into Urdu and back-translated into English to ensure accuracy of translation. Twenty Karachi-based child experts, including pediatricians, psychiatrists, psychologists, and elementary school headmasters, reviewed the translated product for accuracy and cultural appropriateness. A team of 15 pediatricians and general psychologists was trained by a US-based pediatrician-psychologist to administer the instrument, and the team of examiners field-tested the instrument with 40 children before the study began. Translation and some minor changes, such as altering illustrations to depict more conservatively dressed people or rephrasing instructions to capture meaning more clearly than direct translation had, were approved by the instrument publisher. All children were individually tested in one room in a HOPE facility reserved for this purpose.
Children’s vision was screened using a standard Snellen E chart. Auditory acuity was screened in each ear with a portable pure tone audiometer (model MA 25; Maico Diagnostics) at a threshold of 25 dB at 500, 1000, 2000, and 4000 Hz.15 Venous hemoglobin was assessed at a HOPE hospital laboratory. Standing height was measured in duplicate to the nearest 0.1 cm using a standard height board (model 0114500; Unicef). Weight was measured in duplicate to the nearest 0.1 kg using a standing digital scale (model 0141015; Unicef).
STATISTICAL ANALYSIS
We estimated that we would enroll 144 children per group (approximately 40% dropout rate from the 2003 study), resulting in 86% power to detect a 6-point deficit in developmental quotients among control children, assuming an average developmental quotient of 100 among children exposed to handwashing promotion, 95% CI, and a design effect of 1.6 due to cluster sampling. We used statistical methods adjusting for cluster design because randomization occurred at the neighborhood rather than the individual level. We compared characteristics of enrolled and eligible but nonenrolled households as reported in 2003 and current characteristics of enrolled children and house holds across the 3 study groups using a second-order Rao-Scott χ2 test in SAS statistical software, version 9.3 (SAS Institute, Inc). The primary analysis included design-adjusted regression of developmental quotients by intervention. Because we did not detect heterogeneity in developmental outcomes between the two intervention groups, we collapsed them into a single group for the primary analysis. We reported intracluster correlation coefficients using analysis of variance in STATA statistical software, version 11.2 (StataCorp). All analyses were by intent to treat.
Height-for-age, weight-for-age, and body mass index–forage z scores were calculated with WHO AnthroPlus for personal computers (World Health Organization; http://www.who.int/growthref/tools/en), accounting for the cluster design.
ETHICS
Informed consent documents were read to an adult in each household, and the adult was asked to provide written consent on behalf of the household and enrolled child. Children were additionally asked to assent to vision, hearing, and hemoglobin screening. Children found to have anemia, hearing loss, visual defects, or developmental delays were referred to HOPE physicians for additional evaluation and management at no charge. The protocol was approved by the institutional review boards at the Centers for Disease Control and Prevention and HOPE.
RESULTS
During the randomized controlled trial in 2003, 810 households were enrolled in the handwashing promotion, handwashing promotion plus water treatment, and control groups. Of these households, 468 were eligible for reenrollment during the 2009 follow-up study. Between 2003 and 2009, many of these households divided into separate households; ultimately, we recruited 461 households that derived from 391 (83.5%) of the eligible original households (Figure 1). Households that reenrolled did not differ significantly from those that declined reenrollment or were lost to follow-up (Table 1).
Table 1.
Comparison of Characteristics in 2003 of Households Reenrolled and Not Reenrolled in the Current Study
| No. (%) of Households | ||
|---|---|---|
| Characteristic | Not Reenrolled (n = 76) |
Reenrolled (n = 461) |
| Father literate | 43 (56.6) | 277 (60.1) |
| Mother literate | 27 (35.5) | 163 (35.4) |
| Father is salaried employee | 43 (56.6) | 237 (51.4) |
| Monthly income >4000 rupees (~US $46) | 14 (18.5) | 130 (28.2) |
| Ownership | ||
| Television | 40 (52.6) | 286 (62.0) |
| Refrigerator | 13 (17.1) | 114 (24.7) |
| Household hygiene | ||
| Receive municipal water supply | 22 (28.9) | 141 (30.6) |
| Flush toilet | 2 (2.6) | 8 (1.7) |
| Soap visible in handwashing placea | 55 (84.6) | 289 (79.8) |
| Feces visible where children can access | 9 (11.8) | 59 (12.8) |
| Handwashing demonstration | ||
| Uses soap | 49 (64.5) | 300 (65.1) |
| Rubs hands on soap at least 3 times | 15 (19.7) | 125 (27.1) |
| Lathers hands for at least 10 s | 13 (17.1) | 104 (22.6) |
| Dries hands on clean cloth | 11 (14.5) | 44 (9.5) |
| Randomized to control | 27 (35.5) | 160 (34.7) |
| Randomized to soap group | 17 (22.4) | 141 (30.6) |
| Randomized to soap and water treatment group | 32 (42.1) | 159 (34.5) |
Data were available for 65 households that were not reenrolled and 362 households that were reenrolled.
Among reenrolled households, 13 eligible children are known to have died between March 2003 and reenrollment; however, each had an eligible sibling who enrolled in the current study (Figure 1). Causes of death reported by parents included diarrhea (n = 4), pneumonia (n = 3), heart disease (n = 2), fever (n = 2), asthma (n = 1), and trauma (n = 1). Overall mortality was higher in the intervention groups than in the control group (12 of 348 and 1 of 178, respectively; P = .01), but mortality did not significantly differ by study group when deaths due to heart disease, asthma, and trauma were excluded (8 of 348 and 1 of 178, respectively; P = .23). One child was unable to complete the study procedures because of physical and cognitive impairments and was excluded. All children passed the hearing screen. Visual acuity was measured as 6/9 or 6/12 in at least 1 eye among 6 children (1.3%); all others scored 6/6 or better in both eyes.
Reenrolled children were similar across study arms with respect to age, household size, parental education and literacy, socioeconomic indicators, breastfeeding exposure, schooling, exposure to stimulating activities, and anthropometrics (Table 2). Hemoglobin levels were low across the study population16; however, those of children in the control arm were slightly but significantly higher than those among children in the other two groups. Mean height-for-age, weight-for-age, and body mass index– for-age z scores did not differ significantly among the groups. Overall, 24.9% (95% CI, 20.0%–30.6%) and 22.1% (95% CI, 18.0%–26.8%) of children were more than 2 SDs below expected for height-for-age and body mass index–for-age z scores, respectively. In addition, children in the intervention groups were approximately half as likely as children in the control group to have experienced diarrhea on more than 10% of days during the 2003 study (P = .02).
Table 2.
Comparison of Children and Households on Reenrollment by Study Group
| Factor | Control (n = 9 Clusters and 160 Participants) |
Handwashing (n = 9 Clusters and 141 Participants) |
Handwashing and Water Treatment (n = 10 Clusters and 160 Participants) |
P Valuea |
|---|---|---|---|---|
| Male sexb | 82 (51.2) | 75 (53.2) | 85 (53.1) | .94 |
| Age at time of BDI-2, moc | 85.7 (81.0 to 90.3) | 84.9 (80.2 to 89.6) | 84 (81.8 to 86.3) | .14 |
| Age at completion of RCT, moc | 18.6 (14.4 to 22.9) | 18.5 (14.2 to 22.7) | 17.5 (15.5 to 19.5) | .34 |
| Household size, No. of personsc | 8.5 (7.7 to 9.4) | 8.5 (7.9 to 9.1) | 8.4 (7.6 to 9.2) | .81 |
| Mother literateb | 50 (31.2) | 52 (36.9) | 53 (33.1) | .65 |
| Father literateb | 88 (55.0) | 84 (59.6) | 103 (64.4) | .62 |
| Speak Urdu within homeb | 153 (95.6) | 134 (95.0) | 153 (95.6) | .87 |
| Own radiob | 21 (13.1) | 18 (12.8) | 22 (13.8) | .97 |
| Own televisionb | 147 (91.9) | 129 (91.5) | 146 (91.2) | .88 |
| Own refrigeratorb | 89 (55.6) | 96 (68.1) | 89 (55.6) | .09 |
| Home receives municipal water supplyb | 55 (34.4) | 50 (35.5) | 50 (31.2) | .92 |
| Ever breastfedb | 159 (99.4)d | 141 (100) | 157 (98.1) | .15 |
| Duration of breastfeeding, moc | 18.7 (17.3 to 20.1) | 19.4 (18.0 to 20.8) | 19.24 (18.1 to 20.4) | .37 |
| Family history of mental retardationb | 7 (4.4) | 5 (3.5) | 7 (4.4) | .92 |
| Current hemoglobin, g/dLc | 10.6 (10.3 to 10.9) | 10.2 (9.8 to 10.6) | 10.3 (10.0 to 10.5) | .04 |
| Ever enrolled in schoolb | 107 (66.9) | 103 (73.0) | 117 (73.1) | .69 |
| Age at which first enrolled in preschool or school, yc | 5 (4.5 to 5.5) | 4.7 (4.4 to 5.0) | 4.6 (4.5 to 4.8) | .11 |
| Receives private tutoring | 57 (35.6) | 54 (38.3) | 69 (43.1) | .64 |
| Involved in organized sports or danceb | 46 (28.8) | 55 (39.0) | 66 (41.2) | .10 |
| Enriched home environment, defined as any children’s books, toys, or puzzles in homeb | 30 (18.8) | 46 (32.6) | 43 (26.9) | .29 |
| Height-for-age z scoreb | −1.09 (−1.46 to −0.72) | −1.12 (−1.40 to −0.84) | −1.22 (−1.44 to −1.01) | .46 |
| Weight-for-age z scorec | −1.55 (−1.85 to −1.26) | −1.52 (−1.79 to −1.26) | −1.69 (−1.90 to −1.47) | .39 |
| Body mass index–for-age z scorec | −1.29 (−1.54 to −1.04) | −1.19 (−1.35 to −1.03) | −1.34 (−1.57 to −1.10) | .75 |
| Children with diarrhea on > 10% of days during 2003 studyc,e | 63 (42.0) | 31 (23.8) | 34 (23.4) | .02 |
Abbreviations: BDI-2, Battelle Developmental Inventory II; RCT, randomized controlled trial.
Second-order Rao-Scott P value.
Data are presented as number (percentage).
Data are presented as mean (95% CI).
Breastfeeding information was missing for 1 child in the control group, but 159 of the 159 respondents were ever breastfed.
Data available for 150, 130, and 145 children in the control, handwashing, and handwashing and water treatment groups, respectively.
Global developmental quotients among children enrolled in the intervention groups averaged 6.1 points (95% CI, 0.4–11.8) or 0.4 SD higher than those of children enrolled as controls (Table 3). Developmental quotients were comparable between the two handwashing arms, and the difference in developmental quotients between the intervention and control groups was similar across all 5 domains of the BDI-2.
Table 3.
Developmental Quotients of Children at 5 to 7 Years of Age as Measured With the Battelle Developmental Inventory II, by Study Group
| Developmental Domain |
Control (n = 9 Clusters and 160 Participants) Mean (95% CI) |
Handwashing (n = 9 Clusters and 141 Participants) |
Handwashing and Water Treatment (n = 10 Clusters and 160 Participants) |
Combined Handwashing Groups (n = 19 Clusters and 301 Participants) |
Effect Size | ICC | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) |
P Valuea |
Mean (95% CI) |
P Valuea |
Mean (95% CI) |
P Valuea |
Absolute (95% CI)b |
SDc | |||
| Composite | 98.3 (93.1 to 103.4) | 104.5 (101.4 to 107.7) | .04 | 104.3 (100.4 to 108.2) | .07 | 104.4 (101.9 to 107.0) | .04 | 6.1 (0.4 to 11.8) | 0.4 | 0.066 |
| Adaptive | 107.9 (102.7 to 113.1) | 111.4 (108.5 to 114.2) | .24 | 112.6 (109.5 to 115.7) | .12 | 112.0 (110.0 to 114.1) | .14 | 4.1 (−1.4 to 9.7) | 0.3 | 0.019 |
| Personal-social | 106.6 (103.2 to 110.0) | 111.0 (108.6 to 113.5) | .04 | 109.6 (106.8 to 112.4) | .17 | 110.3 (108.3 to 112.2) | .06 | 3.7 (−0.2 to 7.5) | 0.2 | 0.006 |
| Communication | 99.7 (95.1 to 104.4) | 105.1 (102.3 to 107.8) | .05 | 106.2 (103.0 to 109.4) | .03 | 105.7 (103.5 to 107.8) | .02 | 5.9 (0.9 to 11.0) | 0.4 | 0.039 |
| Cognitive | 91.1 (85.0 to 97.3) | 97.9 (94.2 to 101.5) | .06 | 97.0 (91.6 to 102.3) | .15 | 97.4 (94.1 to 100.7) | .08 | 6.2 (−0.7 to 13.2) | 0.4 | 0.092 |
| Motor | 90.3 (84.7 to 96.0) | 97.1 (92.5 to 101.7) | .07 | 95.5 (90.8 to 100.2) | .16 | 96.2 (92.9 to 99.5) | .08 | 5.9 (−0.6 to 12.4) | 0.4 | .061 |
Abbreviation: ICC, intracluster correlation coefficient.
Compared with control group.
Mean difference in developmental quotient between control participants and participants in the combined handwashing intervention groups.
Proportion of a standard deviation that the absolute effect size represents.
COMMENT
At 5 to 7 years of age, children randomized to home-based handwashing promotion during their first 30 months of life attained global developmental quotients more than 6 points (0.4 SD) greater than control children. The effect size was similar across all 5 domains (adaptive, personalsocial, communication, cognitive, and motor) included in the survey instrument and is comparable to gains after participation in the US publicly funded Head Start preschool program for poor children (SD, 0.33–0.46 compared with parental care)17 and early intervention programs for premature infants (SD, 0.46).18 Such an effect size is regarded as clinically meaningful,19 and some estimate that a societal shift of this magnitude would yield trillions of dollars in increased productivity.20 The handwashing intervention in this study was associated with substantial health benefits among children during a critical developmental window: intervention children experienced approximately half the diarrhea burden of control children during their first 2½ years of life,10 and a subsequent evaluation suggested that improvements in handwashing practices and disease experience were sustained for at least 2 additional years, although the difference in diarrhea prevalence in the latter evaluation was not statistically significant.11,21 To our knowledge, this is the first report of long-term child developmental outcomes after a cluster randomized controlled trial of handwashing interventions, and our findings suggest that handwashing promotion could be an important additional strategy for improving child welfare.
This study included a large number of participants, and original treatment allocations were randomly assigned, which should result in balanced distribution of known and unknown predictive and confounding factors across groups. In addition, we were able to reenroll 83.5% of eligible households, and reenrolled and nonreenrolled households did not significantly or meaningfully differ on a large number of key variables. We therefore considered it inappropriate to apply postrandomization corrections to attain our primary objective of assessing whether handwashing promotion affected child growth or development.22
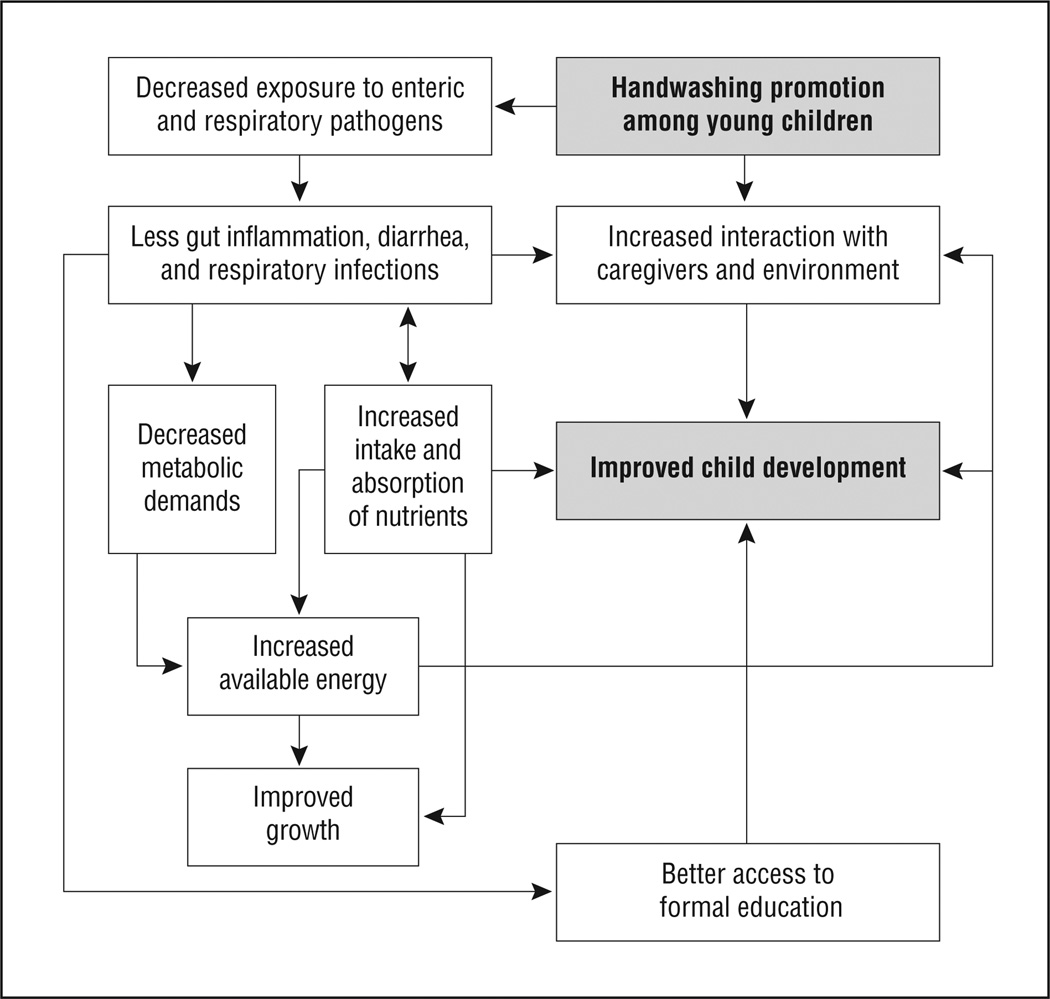
Although the randomized study design helps ensure that the developmental differences we report resulted from the interventions rather than through confounding, we had limited capacity to assess which aspects of the interventions and which mechanisms underpinned our findings. Nonetheless, we propose some possible pathways (Figure 2). Some previous nonrandomized studies have linked heavy diarrhea5,6,23 or intestinal parasite burdens24 in early childhood to delays in development, whereas others have not found an association between childhood diarrhea and cognition.7,25 Furthermore, long-term ingestion of large numbers of fecal pathogens, as might have occurred to a greater degree among control children, can lead to increased intestinal permeability, immune response, and poor growth and development even in the absence of diarrhea.26–28 Immune stimulation is metabolically costly, and children who are required to invest less energy fighting pathogens are likely to direct more energy toward growth and development.21 This finding may be particularly important among very young children, as in our study population, for whom metabolic demands for brain development and growth are maximal, and in settings such as Karachi, where exposure to pathogens is common.21 Next, prolonged breastfeeding was almost universal among our population, which limited our power to assess the effect of this factor. Although hemoglobin concentrations were low across study groups,16 mean hemoglobin concentration was slightly but significantly higher among control children. Anemia at 5 to 7 years of age therefore did not explain the observed developmental differences; however, we were unable to assess either the prevalence or effect of anemia earlier in life. In addition, we do not know whether, perhaps due to a smaller burden of infectious illness, children in the intervention group experienced more time involved in stimulating play or whether parents became more engaged with children in the intervention group because they had been encouraged to assist them with handwashing several times per day or because the children were generally healthier. Moreover, we lacked prospectively collected measures of anthropometrics, diet, micronutrient supplementation, lead and other toxin exposure, gut permeability, helminth load, and malaria exposure during the 2003 study, and we could not obtain reliable information about birth weight, gestational age, or maternal micronutrient supplementation during pregnancy, so we were unable to explore these factors in our analysis. Finally, we cannot determine whether intervention households sold study soap to buy food or other goods in 2003; however, field workers removed soap wrappers at the time of distribution to discourage resale, and participants were provided a mean of only 3.5 g of soap per person per day during the trial.10
Figure 2.
Hypothesized pathways among handwashing promotion, growth, and development. Boldface type indicates the start and end points of the pathway.
One-quarter of children in this study were stunted, a prevalence similar to previous reports from this age group and region, and anthropometric measurements did not differ significantly among the study groups.29 Although some studies26,30,31 have measured an association, it is unclear whether diarrhea in early childhood causes permanent stunting. Stunting is generally the product of cumulative nutritional deficiencies, including inadequate caloric and nutrient intake or absorption,32 and the effects of caloric intake and diarrhea on stunting have been shown to be independent.33 Because diets are marginal in this population, reduced exposure to enteric pathogens early in life might not have been sufficient to affect growth through 5 to 7 years of age. In developing countries, stunting also tends to begin within the first several months of life and thereafter to become intractable.34 In contrast, the developing brain appears to be sensitive to environmental conditions for a broader period.35 Few children enrolled into the 2003 study as neonates; thus, they might have been young enough to experience gains in development, but not growth, due to improved hygiene. Finally, it is possible that handwashing affects child development through a larger number of pathways than it does growth (Figure 2).
These results are constrained by several additional limitations. We could not assess development of the children who had died, and we cannot know whether evaluating their surviving siblings biased our results. In addition, because our study population experienced high rates of disease and environmental contamination, our results might not be generalizable to less contaminated settings or healthier populations. Next, because no validated developmental tests were available in Pakistan at the time of this study, we used an instrument that had been validated among a North American population. We attempted to translate and adapt the instrument carefully for children in Pakistan; however, we cannot be certain that it accurately measured developmental quotients among this population. Still, we believe that any systematic cultural problems with the instrument would be balanced by comparing results across the study groups. Next, a number of children were approaching the upper age limit for the BDI-2, which resulted in less test sensitivity, particularly within the motor domain.13 Accurate age calculations for each child are required to score the BDI-2 and to calculate anthropometric z scores. We had confirmed children’s dates of birth through birth certificates, immunization records, or event calendars during the 2003 study,10 but it is possible that not all birthdates, and therefore developmental quotient and anthropometric z-score calculations, are accurate. Such measurement error would, however, likely bias our results toward the null.
Nonetheless, this is, to our knowledge, the first report of improvements in child development after a randomized controlled trial of handwashing interventions. The developmental gains we measured are both meaningful and consistent across developmental domains. If the developmental quotients of children in developing countries can indeed be raised 0.4 SD through handwashing promotion early in life, this extremely low-tech, accessible intervention could help decrease the role of inequity in child well-being and greatly affect both individual and societal productivity.1,20,35 Handwashing promotion could easily be integrated with nutritional support, parenting education, and high-quality preschool to create comprehensive child development interventions. Additional efforts should be undertaken to understand the processes described and to promote handwashing behavior change, particularly among families with young children, quickly and efficiently worldwide.
Acknowledgments
Conflict of Interest Disclosures: The Centers for Disease Control and Prevention and Procter&Gamble Company maintain a Cooperative Research and Development Agreement (CRADA). Most of the funding for this study was obtained from Procter & Gamble Company via this CRADA, whereas the balance of funds was provided by the Centers for Disease Control and Prevention. Dr Bowen is a Centers for Disease Control and Prevention employee whose salary is partially funded through the CRADA. Dr Luby is a Centers for Disease Control and Prevention employee whose salary was partially funded through the CRADA until 2004. Timothy Tobery was an employee of Procter & Gamble Company from 2007 to 2009 and is currently an employee of Unilever. Both Procter & Gamble Company and Unilever manufacture soap.
Funding/Support: Most of the study funds were provided by the Procter & Gamble Company. The balance of the study funds was provided by the Centers for Disease Control and Prevention.
Role of the Sponsor: The funder participated in the design of the study.
Additional Contributions: We gratefully acknowledge the HOPE staff members who worked in the community; Maria Tariq, MBBS, who oversaw daily study activities; Sohail Hussain, MS, and Aleya Nizam, BS, who supervised data management; and Jennifer Jaeger, MD, for training field staff.
Footnotes
Author Contributions: Study concept and design: Bowen, Luby, Tobery, and Hoekstra. Acquisition of data: Agboatwalla. Analysis and interpretation of data: Bowen, Luby, Ayers, and Hoekstra. Drafting of the manuscript: Bowen. Critical revision of the manuscript for important intellectual content: Bowen, Agboatwalla, Luby, Tobery, Ayers, and Hoekstra. Statistical analysis: Bowen, Luby, Ayers, and Hoekstra. Obtained funding: Bowen and Tobery. Administrative, technical, and material support: Bowen, Agboatwalla, Luby, and Tobery. Study supervision: Bowen and Agboatwalla.
Disclaimer: The funder did not participate in the collection, analysis, or interpretation of data and did not prepare or have approval rights over the publication. The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. International Child Development Steering Group. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369(9555):60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Psacharopoulos G, Patrinos H. Returns to investment in education: a further update. [Accessed August 3, 2011];World Bank. 2002 Sep; http://siteresources.worldbank.org/EDUCATION/Resources/278200-1099079877269/547664-1099079934475/547667-135281504040/Returns_Investment_Edu.pdf. [Google Scholar]
- 3.Calvin CM, Deary IJ, Fenton C, et al. Intelligence in youth and all-causemortality: systematic review with meta-analysis. Int J Epidemiol. 2011;40(3):626–644. doi: 10.1093/ije/dyq190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlaudecker EP, Steinhoff MC, Moore SR. Interactions of diarrhea, pneumonia, and malnutrition in childhood: recent evidence from developing countries. Curr Opin Infect Dis. 2011;24(5):496–502. doi: 10.1097/QCO.0b013e328349287d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patrick PD, Oriá RB, Madhavan V, et al. Limitations in verbal fluency following heavy burdens of early childhood diarrhea in Brazilian shantytown children. Child Neuropsychol. 2005;11(3):233–244. doi: 10.1080/092970490911252. [DOI] [PubMed] [Google Scholar]
- 6.Lorntz B, Soares AM, Moore SR, et al. Early childhood diarrhea predicts impaired school performance. Pediatr Infect Dis J. 2006;25(6):513–520. doi: 10.1097/01.inf.0000219524.64448.90. [DOI] [PubMed] [Google Scholar]
- 7.Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002;359(9306):564–571. doi: 10.1016/S0140-6736(02)07744-9. [DOI] [PubMed] [Google Scholar]
- 8.Ejemot RI, Ehiri JE, Meremikwu MM, Critchley JA. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev. 2008;(1):CD004265. doi: 10.1002/14651858.CD004265.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM., Jr Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5(1):42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 10.Luby SP, Agboatwalla M, Painter J, et al. Combining drinking water treatment and hand washing for diarrhoea prevention: a cluster randomised controlled trial. Trop Med Int Health. 2006;11(4):479–489. doi: 10.1111/j.1365-3156.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- 11.Luby SP, Agboatwalla M, Bowen A, Kenah E, Sharker Y, Hoekstra RM. Difficulties in maintaining improved handwashing behavior, Karachi, Pakistan. Am J Trop Med Hyg. 2009;81(1):140–145. [PubMed] [Google Scholar]
- 12.From neurons to neighborhoods: the science of early childhood development. Washington, DC: 2000. [Accessed August 31, 2011]. Committee on Integrating the Science of Child Development. http://www.nap.edu/catalog.php?record_id=9824. [Google Scholar]
- 13.Newborg J. Battelle Developmental Inventory. 2nd ed. Itasca, IL: Riverside Publishing; 2005. [Google Scholar]
- 14.Grantham-McGregor S, Ani C. Cognition and undernutrition: evidence for vulnerable period. Forum Nutr. 2003;56:272–275. [PubMed] [Google Scholar]
- 15.World Health Organization. [Accessed May 11, 2011];Grades of hearing impairment. http://www.who.int/pbd/deafness/hearing_impairment_grades/en/index.html.
- 16.World Health Organization. Iron Deficiency Anemia, Assessment, Prevention, and Control: A Guide for Programme Managers. Geneva, Switzerland: World Health Organization; 2001. [Accessed July 27, 2011]. http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf. [Google Scholar]
- 17.Zhai F, Brooks-Gunn J, Waldfogel J. Head Start and urban children’s school readiness: a birth cohort study in 18 cities. Dev Psychol. 2011;47(1):134–152. doi: 10.1037/a0020784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spittle AJ, Orton J, Doyle LW, Boyd R. Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database Syst Rev. 2007;(2):CD005495. doi: 10.1002/14651858.CD005495.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Nordhov SM, Rønning JA, Dahl LB, Ulvund SE, Tunby J, Kaaresen PI. Early intervention improves cognitive outcomes for preterm infants: randomized controlled trial. Pediatrics. 2010;126(5):e1088–e1094. doi: 10.1542/peds.2010-0778. [DOI] [PubMed] [Google Scholar]
- 20.Weiss B. Pesticides as a source of developmental disabilities. Ment Retard Dev Disabil Res Rev. 1997;3(3):246–256. [Google Scholar]
- 21.McDade TW. Life history theory and the immune system: steps toward a human ecological immunology. Am J Phys Anthropol. 2003;(suppl 37):100–125. doi: 10.1002/ajpa.10398. [DOI] [PubMed] [Google Scholar]
- 22.Austin PC, Manca A, Zwarenstein M, Juurlink DN, Stanbrook MB. A substantial and confusing variation exists in handling of baseline covariates in randomized controlled trials: a review of trials published in leading medical journals. J Clin Epidemiol. 2010;63(2):142–153. doi: 10.1016/j.jclinepi.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Niehaus MD, Moore SR, Patrick PD, et al. Early childhood diarrhea is associated with diminished cognitive function 4 to 7 years later in children in a northeast Brazilian shantytown. Am J Trop Med Hyg. 2002;66(5):590–593. doi: 10.4269/ajtmh.2002.66.590. [DOI] [PubMed] [Google Scholar]
- 24.Guerrant DI, Moore SR, Lima AA, Patrick PD, Schorling JB, Guerrant RL. Association of early childhood diarrhea and cryptosporidiosis with impaired physical fitness and cognitive function four-seven years later in a poor urban community in northeast Brazil. Am J Trop Med Hyg. 1999;61(5):707–713. doi: 10.4269/ajtmh.1999.61.707. [DOI] [PubMed] [Google Scholar]
- 25.Tarleton JL, Haque R, Mondal D, Shu J, Farr BM, Petri WA., Jr Cognitive effects of diarrhea, malnutrition, and Entamoeba histolytica infection on school age children in Dhaka, Bangladesh. Am J Trop Med Hyg. 2006;74(3):475–481. [PubMed] [Google Scholar]
- 26.Humphrey JH. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet. 2009;374(9694):1032–1035. doi: 10.1016/S0140-6736(09)60950-8. [DOI] [PubMed] [Google Scholar]
- 27.Solomons NW, Mazariegos M, Brown KH, Klasing K. The underprivileged, developing country child: environmental contamination and growth failure revisited. Nutr Rev. 1993;51(11):327–332. doi: 10.1111/j.1753-4887.1993.tb03758.x. [DOI] [PubMed] [Google Scholar]
- 28.Campbell DI, Elia M, Lunn PG. Growth faltering in rural Gambian infants is associated with impaired small intestinal barrier function, leading to endotoxemia and systemic inflammation. J Nutr. 2003;133(5):1332–1338. doi: 10.1093/jn/133.5.1332. [DOI] [PubMed] [Google Scholar]
- 29.Khuwaja S, Selwyn BJ, Shah SM. Prevalence and correlates of stunting among primary school children in rural areas of southern Pakistan. J Trop Pediatr. 2005;51(2):72–77. doi: 10.1093/tropej/fmh067. [DOI] [PubMed] [Google Scholar]
- 30.Checkley W, Buckley G, Gilman RH, et al. Childhood Malnutrition and Infection Network. Multi-country analysis of the effects of diarrhoea on childhood stunting. Int J Epidemiol. 2008;37(4):816–830. doi: 10.1093/ije/dyn099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmidt WP, Genser B, Luby SP, Chalabi Z. Estimating the effect of recurrent infectious diseases on nutritional status: sampling frequency, sample-size, and bias. J Health Popul Nutr. 2011;29(4):317–326. doi: 10.3329/jhpn.v29i4.8447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allen LH. Nutritional influences on linear growth: a general review. Eur J Clin Nutr. 1994;48(suppl 1):S75–S89. [PubMed] [Google Scholar]
- 33.Becker S, Black RE, Brown KH. Relative effects of diarrhea, fever, and dietary energy intake on weight gain in rural Bangladeshi children. Am J Clin Nutr. 1991;53(6):1499–1503. doi: 10.1093/ajcn/53.6.1499. [DOI] [PubMed] [Google Scholar]
- 34.Victora CG, de Onis M, Hallal PC, Blössner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125(3):e473–e480. doi: 10.1542/peds.2009-1519. [DOI] [PubMed] [Google Scholar]
- 35.From Neurons to Neighborhoods: The Science of Early Child Development. Washington, DC: Institute of Medicine; 2000. Institute of Medicine. [Google Scholar]