Abstract
While influenza transmission is thought to occur primarily by droplet spread, the role of airborne spread remains uncertain. Understanding the beliefs and attitudes of infectious disease physicians regarding influenza transmission and respiratory and barrier protection preferences can provide insights into workplace decisions regarding respiratory protection planning. Physicians participating in the Infectious Diseases Society of America’s Emerging Infections Network were queried in November 2013 to determine beliefs and attitudes on influenza transmission. A subset of physicians involved in their facility’s respiratory protection decision making were queried about respirator and surgical mask choices under various pandemic scenarios; availability of, and challenges associated with, respirators in their facility; and protective strategies during disposable N95 shortages. The majority of 686 respondents (98%) believed influenza transmission occurs frequently or occasionally via droplets; 44% of respondents believed transmission occurs via small particles frequently (12%) or occasionally (32%). Among the subset of respondents involved in respiratory protection planning at their facility, over 90% preferred surgical masks during provision of non-aerosol-generating patient care for seasonal influenza. However, for the same type of care during an influenza pandemic, two-thirds of respondents opted for disposable N95 filtering facepiece respirators. In settings where filtering facepiece (disposable) N95 respirators were in short supply, preferred conservation strategies included extended use and reuse of disposable N95s. Use of reusable (elastomeric facepiece) respirator types was viewed less favorably. While respondents identified droplets as the primary mode of influenza transmission, during a high-severity pandemic scenario there was increased support for devices that reduced aerosol-based transmission. Use of potentially less familiar respirator types may partially relieve shortages of disposable N95s but also may require significant education efforts so that clinicians are aware of the characteristics of alternative personal protective equipment.
The National Academy of Sciences’ Institute of Medicine has characterized potential routes of influenza transmission as occurring via direct and indirect contact, droplet spray, and small particle aerosols.1 Historically, influenza transmission has been thought to occur primarily by respiratory droplet spread or from contact with infected secretions.2 The relative contribution to transmission of particles small enough to remain airborne for a prolonged period and which can be inhaled into the distal respiratory tract is controversial. However, there is some clinical evidence for small-particle aerosol transmission of influenza.3 In addition, studies involving quantitative air sampling of healthcare facilities suggest that small airborne particles could contribute to influenza exposure in these settings.4,5 Also, cough aerosols generated by influenza patients can have particles containing viable virus.6
Uncertainty regarding the relative importance of these differing modes of influenza spread has resulted in uncertainty in the optimal protective strategies for healthcare workers caring for patients with influenza. For instance, during the 2009–10 H1N1 influenza pandemic, the Centers for Disease Control and Prevention (CDC) issued guidance recommending the use of respirators with filters that are rated N95 or above when caring for patients with influenza.7 The N95 respirator contains filter media with a high level of efficiency so that the small particle aerosol inhalation is reduced; this prevents direct exposure of the wearer’s oronasal region to droplet spray. Surgical masks are loose-fitting devices that do not prevent inhalation of small particle aerosols. Instead, they provide barrier protection by blocking direct spray droplets.8 Some questioned the need for N95 or above respirators for all influenza-associated patient care scenarios during the 2009 H1N1 pandemic, with reported limited supplies of N95 respirators contributing to the debate.9
The 2009 CDC interim guidance also provided strategies for either the reuse or extended use of disposable N95 respirators or the use of nondisposable respirators, such as powered air-purifying respirators (PAPRs) and respirators with full- or half-mask elastomeric facepieces in the event of disposable N95 respirator shortages.10 Reuse of disposable respirators and use of nondisposable respirators have been raised as potential options for pandemic influenza planning by the Institute of Medicine,8 the Veterans’ Affairs national healthcare system,11 and CDC.12
With the emergence of H7N9 avian influenza in 2013, the current interim CDC guidance for the care of patients with known or suspected H7N9 influenza, or another novel influenza A associated with severe disease, recommends the use of respiratory protection with an N95 level or greater filter.13 This differs from seasonal influenza infection control recommendations, which recommend the use of N95 level or greater respiratory protection only during provision of patient care involving aerosol generation—for example, during procedures like bronchoscopy or intubation.14
To better understand the beliefs and attitudes of infectious disease physicians about the use of respiratory protective devices and surgical masks, we developed a query for members of the Infectious Diseases Society of America (IDSA) Emerging Infections Network (EIN). The specific goal of this query was to determine the perspective of EIN membership on influenza transmission and different respiratory protective strategies in the event of an influenza pandemic.
Methods
The EIN generates periodic, urgent queries of its membership regarding infectious disease topics. As of December 2013, there were 1,472 EIN infectious disease physician members who have responded to queries, representing 20% of the IDSA physician membership. These members represent a broad cross-section of the country, with members located in all 50 states, and a cross-section of practice types (ie, private practice, academics).15
An 8-question electronic query, developed and pilot tested by the coauthors on a convenience sample of infectious disease physicians and influenza subject matter experts, was sent to 1,472 EIN members on November 5, 2013. Practitioners were sent 2 follow-up reminders, and the query was closed 1 month after its original posting. Practitioners were also allowed to opt out if they were not involved in the care of patients with influenza. Specific questions, and the response options (which varied by type of question), can be found at http://www.int-med.uiowa.edu/Research/EIN/InfluenzaRespirator_finalquery.pdf.
Briefly, the query consisted of 2 initial questions to gauge EIN members’ beliefs about small-particle aerosol and droplet transmission of influenza (options included never, rarely, occasionally, frequently, and unsure). These questions were followed by a question to identify individuals involved in their healthcare facility’s decision about the type of respiratory and barrier protection for influenza.
The remaining questions focused on the subset of respondents involved in their facility’s decisions regarding respiratory protection (specifically, both actual decision making and providing recommendations or technical expertise to those who make the decisions). These questions related to:
beliefs regarding the type of respirator or surgical mask that should be used in different patient scenarios (options included surgical mask, N95 respirator, or other);
availability for routine patient care and stockpiling of various types of respirators (eg, disposable N95 respirators, elastomeric respirators, PAPRs) and surgical masks in the respondents’ facilities (options included yes/available, no/unavailable, or unsure);
rating of the respondents’ level of concern for potential barriers (eg, lack of user comfort, difficulty with patient communication, difficulty cleaning, and cost) that could be anticipated with expanded use of disposable N95 respirators, elastomeric respirators, and PAPRs (options included significant concern, mild concern, no concern, or unsure); and
respondents’ preferred strategies for providing respiratory and/or barrier protection to workers (eg, use of surgical masks; reuse of disposable N95 respirators; extended use of disposable N95 respirators; use of elastomeric respirators; use of PAPRs; or a free-text option for another strategy) in the setting of shortages of disposable N95s and in the setting of an influenza pandemic with an influenza strain with a high mortality and for which there was no vaccine available (options included a 5-point scale ranging from 1 for unlikely to endorse to 5 for likely to endorse).
Respondents did not have to answer all questions, and, where applicable, results for individuals who did not respond were combined with those that selected the unsure option.
Results
Demographics
A total of 686 out of 1,472 (47%) physicians responded to the query, with representation from all parts of the country and employment in a variety of settings, including hospitals/ clinics (183), private/group practice (162), university/ medical school (295), VA and military settings (38), and state government (6) (Table 1).
Table 1.
Geographic distribution and employment type of respondents (N =686) to EIN query, November-December 2013
| Respondent Demographics | Respondents/Total Queried (%) |
|---|---|
|
| |
| Location of respondents | |
| New England | 54/98 (55) |
| Mid-Atlantic | 93/205 (45) |
| East North Central | 95/204 (47) |
| West North Central | 66/133 (50) |
| South Atlantic | 125/271 (46) |
| East South Central | 34/72 (47) |
| West South Central | 46/98 (47) |
| Mountain | 41/95 (43) |
| Pacific | 121/264 (43) |
| Puerto Rico | 1/5 (20) |
| Canada | 10/26 (38) |
| Employment type | |
| Hospital/clinic | 183/415 (44) |
| Private/group practice | 162/402 (40) |
| University/medical school | 295/560 (53) |
| Federal facilities | 38/79 (48) |
| State government | 6/13 (46) |
Influenza Transmission
A total of 552 respondents answered questions about their beliefs regarding influenza transmission. When asked to comment on whether influenza is transmitted via respiratory droplets (using a scale of frequently, occasionally, rarely, never, and unsure), 98% indicated that they believed that influenza is frequently (92%) or occasionally (6%) transmitted via droplets. When asked whether influenza was transmitted via small-particle aerosols, 12% of respondents indicated that they believed that influenza is frequently transmitted via small-particle aerosols, while 32% believed it was occasionally transmitted this way, and 48% indicated this occurred rarely (46%) or never (2%).
The remainder of the query focused on 289 of 686 individuals (42%) who reported involvement in their facility’s decisions about respiratory/barrier protection for influenza. When compared to the larger population of 686 respondents, the 289 members had similar geographic distribution. Of these 289 respondents, 35% were employed by a university/medical school, and 32% were employed directly by a hospital or clinic. Of the 289 respondents involved in facility-level decisions regarding respiratory/barrier protection for influenza, 284 (98%) indicated that they believed that influenza is frequently or occasionally transmitted by droplets. Regarding aerosol transmission of influenza, 9% believed this occurred frequently, 34% believed this occurred occasionally, 49.8% believed this occurred rarely, and 2.1% indicated no aerosol transmission.
Personal Protective Equipment Preferences
Respondents’ preferences for types of personal protective equipment differed for varying types of patient care activities, and the level of protection desired increased as the severity of an influenza pandemic scenario increased (Table 2). Among the individuals involved in facility-level decisions regarding respiratory/barrier protection for influenza, 89% indicated that the preferred strategy for worker protection when entering the room of a patient with seasonal influenza but without patient contact was use of a surgical mask (89%). When providing direct care for a patient with seasonal influenza, 92% selected the option of a surgical mask. In contrast, during a mild-to-moderate pandemic, preference for use of surgical masks for direct patient care decreased to 72% and preference for use of N95s increased to 27%. In addition, during a severe pandemic scenario (associated with ≥1% mortality), 58% preferred N95 respirators for room entry and 67% preferred N95 respirators for providing routine care for influenza patients.
Table 2.
Respondents’ (n = 289) N95 respirator and surgical mask preferences by patient care setting and influenza severity
| Patient Care Activity | Type of Personal Protective Equipment | Scenario
|
||
|---|---|---|---|---|
| Seasonal Influenza (%) | Mild to Moderate Severity Pandemic (eg, mortality similar to 2009) or Severe Seasonal Influenza (%) | Severe Pandemic Disease (eg, mortality ≥1%) (%) | ||
| Entry into patient room (no patient contact and >6 feet from patient) | Surgical masks | 89 | 79 | 40 |
| Disposable N95 respirators | 5 | 18 | 58 | |
| Other* | 6 | 3 | 2 | |
|
| ||||
| Routine patient care without aerosol-generating procedures (eg, examining patient) | Surgical masks | 92 | 72 | 31 |
| Disposable N95 respirators | 7 | 27 | 67 | |
| Other* | 1 | 1 | 2 | |
|
| ||||
| Provision of patient care involving aerosol generation | Surgical masks | 38 | 25 | 8 |
| Disposable N95 respirators | 60 | 72 | 87 | |
| Other* | 2 | 3 | 5 | |
“Other” represents an option other than surgical masks or disposable N95s for respondents to select in the questionnaire, but additional data were not collected.
Respirator Supplies
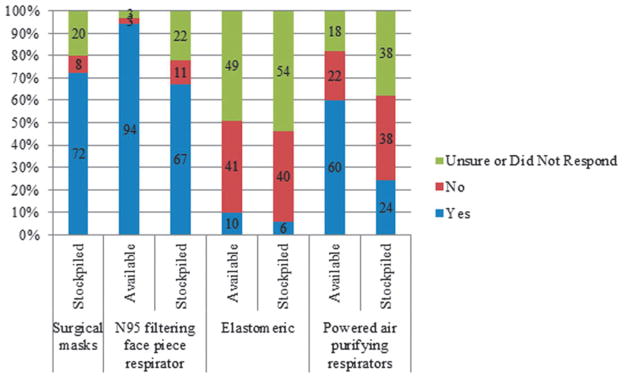
Ninety-four percent of respondents noted the availability of N95s in their facility for routine patient care (Figure 1). However, 22% of the 289 individuals involved in facility-level decisions regarding respiratory/barrier protection for influenza indicated they were unsure about, or did not respond to, whether their facility stockpiled N95s. PAPRs were reported by 60% of respondents to be available for routine use, but 38% were unsure or did not respond about the stockpiling of PAPRs. Few participants reported that their facility uses or stockpiles elastomeric respirators, with only 10% of respondents reporting that these devices were available; most respondents were unsure or did not respond.
Figure 1.
Respondents’ (n = 289) awareness of availability or stockpiling of various respiratory protective devices and surgical masks in their facility
Barriers to Expanded Use of Respirators
Participants were given a set of potential barriers to respirator use, such as comfort, cost, and ease of communication. They were then asked to categorize their level of concern about these barriers as “significant concerns,” “mild concerns,” “no concerns,” or “unsure” (the latter option reflecting individuals who either selected “unsure” or did not respond to the question). The majority of the subgroup of 289 respondents involved in their facility’s decisions about respiratory/barrier protection for influenza noted mild to no concerns for use of disposable N95s related to lack of comfort, difficulty communicating, difficulty cleaning, or costs (Table 3). Compared to N95s, there were more “significant concerns” for PAPRs—specifically lack of comfort, difficulty communicating, difficulty cleaning, and cost. A majority of individuals were unsure, or did not respond, regarding the comfort, communication, cleaning, and cost associated with the potential expanded use of elastomerics.
Table 3.
Respondents’ (n = 289) level of concern for possible barriers to expanded use of respirators, by type
| Type of Barrier | Respirator Type | Level of Concern (% of respondents)
|
|||
|---|---|---|---|---|---|
| None | Mild | Significant | Unsure | ||
| Lack of comfort | Disposable N95s | 24 | 49 | 27 | 0 |
| PAPRs | 8 | 31 | 46 | 15 | |
| Elastomerics | 1 | 16 | 21 | 62 | |
| Difficulty communicating | Disposable N95s | 27 | 53 | 19 | 1 |
| PAPRs | 3 | 22 | 61 | 14 | |
| Elastomerics | 2 | 14 | 25 | 59 | |
| Difficulty cleaning | Disposable N95s | 72 | 11 | 13 | 4 |
| PAPRs | 5 | 31 | 42 | 22 | |
| Elastomerics | 3 | 14 | 19 | 64 | |
| Cost | Disposable N95s | 26 | 49 | 21 | 4 |
| PAPRs | 2 | 12 | 70 | 16 | |
| Elastomerics | 3 | 9 | 29 | 59 | |
Ranking Respirator Conservation Strategies
Respondents were asked to rank various respirator conservation strategies on a scale of 0 (unlikely to endorse) to 5 (likely to endorse) for a hypothetical setting where N95-level protection was recommended but there was a shortage of N95 respirators; the scenario included a circulating influenza strain with high mortality and no available vaccine. For this scenario, 253 of 289 respondents (88%) provided a ranking for each strategy. The most to least endorsed strategies were: extended use of N95s (median score, 5; mean score, 4.25), reuse of N95s (median score, 4; mean score, 3.99), use of PAPRs (median score, 4; mean score, 3.73), use of surgical masks (median score, 4; mean score, 3.6), and use of elastomerics (median score, 3; mean score, 3.17).
Respondent Comments
Several themes emerged from the last section of the query, which allowed for free text responses, including the lack of data by which to make informed decisions regarding respirators; challenges associated with fit testing of N95s, particularly during an emergency situation; the need to consider forms of personal protective equipment other than respirators to reduce exposure to influenza, in particular eye protection; the need to use greater protection until the mortality rate was known; and the lack of knowledge about elastomeric respirators.
Discussion
This survey highlighted ongoing concerns and uncertainties concerning appropriate respiratory protection for health-care workers during seasonal and pandemic influenza. The vast majority of individuals in this query (98%) believed that influenza is frequently or occasionally transmitted via droplets, with a much smaller group (44%) believing that influenza is frequently or occasionally transmitted by aerosol. Among respondents who are involved in making decisions about respiratory protection at their healthcare facilities, the vast majority (98%) endorsed droplet transmission as the predominant mode of influenza transmission and most agreed with the CDC recommendation to use surgical masks for patient care activities during influenza season. Only a minority favored the use of N95 respirators during a pandemic with mild severity, similar to the 2009 pandemic. However, when presented with the scenario of a pandemic influenza strain with high mortality, approximately two-thirds preferred N95 respirators over surgical masks. In the setting of a hypothetical pandemic-associated respirator shortage, the respondents preferred extended use or reuse of disposable N95 respirators over PAPRs or elastomerics. Additionally, participants reported more concerns about comfort, communication, cleaning, and costs associated with PAPRs versus disposable N95s.
The uncertainty and diversity of opinions among infectious disease physicians may reflect a lack of clarity in the data needed to make recommendations. And some of the preference for disposable N95s over reusable devices may reflect less familiarity among clinicians with these alternatives, as evidenced by the fact that there was a higher percentage of respondents who reported being unsure about (or not responding to) facility availability or stockpiling of PAPRs and elastomerics compared to disposable N95s.
The use of higher-level respiratory protection, such as N95 respirators or greater, over surgical masks for barrier protection has not been conclusively shown to reduce influenza transmission in the healthcare setting. A 2008 randomized clinical trial to evaluate the role of surgical masks versus N95 respirators for prevention of influenza found noninferior rates of laboratory-confirmed influenza among healthcare workers using surgical masks compared to those using N95 respirators.16 In another trial comparing use of surgical masks with intermittent or continuous N95 use among healthcare workers, there was a significantly greater rate of clinical respiratory infections (defined as the presence of 2 or more respiratory symptoms or a combination of a systemic symptom and 1 respiratory symptom) among those who used surgical masks. However, no significant difference in confirmed viral infections (de-fined as a positive test from a symptomatic patient using a multiplex PCR to detect a group of respiratory pathogens including influenza) was found between the study arms.17 This may reflect a true lack of difference between the 2 groups, or it may reflect an underpowering of the study to detect a difference. In the face of current uncertainties, CDC recommends the precautionary approach of using N95 respirators for influenza outbreaks that are greater in severity than seasonal strains to prevent severe cases of influenza among healthcare personnel.13
Other studies have shown that healthcare workers prefer disposable over reusable respirators.18 Furthermore, in a study to evaluate the use of elastomeric respirators in the ICU, investigators identified that significant healthcare worker education and multiple logistic issues (storage, cleaning) needed to be addressed in order to increase the likelihood of successfully introducing these devices into healthcare settings.19
The current study suggests that providers prefer surgical masks in typical seasonal influenza settings; this is consistent with the vast majority of the respondents’ view that influenza is predominantly spread via droplets. Respiratory protection to reduce inhalation of small-particle aerosols was preferred only under higher-risk settings, such as a severe pandemic scenario associated with ≥1% mortality. The reasons for a switch from droplet to small-particle aerosol protection against increasingly severe influenza strains were not systematically explored in this investigation and may benefit from additional investigation.
This query has several limitations. Regarding bias, although the overall response rate was 47%, similar to previous EIN queries,15 there may have been responder bias given that respondents may have been more likely to support a particular respiratory protection strategy compared to nonrespondents. For instance, nonrespondents were significantly more likely than respondents to have fewer than 15 years of infectious disease experience, be adult infectious disease practitioners, and work in a private/group practice and in a community hospital. Also, IDSA EIN represents approximately 20% of IDSA physician membership; thus, the results may not reflect the opinions of the broader IDSA community. And the unit of analysis for most of the query was the individual physician; thus, multiple respondents from 1 facility could have biased the results. However, there were only 20 facilities with more than 1 respondent, representing less than 10% of the sample size.
For the question focusing on facility respirator supplies, we performed an additional sensitivity analysis, limiting the analysis to a single respondent who was either the hospital epidemiologist, was involved in the facility’s infection control, or was the respondent with the least “unsure” responses, and the results were similar. More broadly, while infectious disease providers are an important group often involved in institutional decisions related to infection control policies, other types of clinical providers frequently use respiratory protective devices and surgical masks during the provision of care to influenza patients, such as intensive care unit and emergency department nurses and physicians. These providers may have had different responses.
In terms of the results, subjective response terms such as “rarely, occasionally, frequently” may have had different meanings for different respondents. Finally, this type of “expert opinion” data is considered a lower level quality of evidence compared to randomized, controlled trial, or observational study data.20 But it has also been noted that this type of data can provide important insights, given that it is based on the clinical judgment of subject matter experts.20
Continued research is critical to determine the relative importance of different modes of transmission of influenza and the effectiveness of respiratory protection devices in real-world use. However, until such data are available, public health officials will need to make recommendations based on the limited available data, the potential benefits, and the costs and barriers of each strategy. The results of this survey suggest that clinicians prefer not to use higher levels of respiratory protection (ie, devices that provide protection against aerosol transmission) unless there is a clear increase in severity of the disease. Shortages of protective devices can be anticipated, and clear guidance on how to optimize protection in the setting of shortages is needed. While devices such as elastomeric respirators may currently be unfamiliar to healthcare personnel, the use of these reusable devices during an influenza pandemic, even in limited settings, could potentially conserve disposable N95 respirators for other uses.
Further research is needed before the next influenza pandemic to understand the best way to optimize the use of N95 respirators during a shortage and to determine the feasibility and acceptability of reusable devices such as PAPRs and elastomeric respirators. Public health officials will need to adjust respirator guidance as additional data, such as transmission risk factors and severity of disease, become available during the pandemic event.
Acknowledgments
This publication was supported by Cooperative Agreement Number 1U50CK000187 from the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Contributor Information
Satish K. Pillai, Medical Officer, National Center for Emerging and Zoonotic Infectious Diseases/Division of Preparedness and Emerging Infections, Centers for Disease Control and Prevention, Atlanta, Georgia.
Susan E. Beekmann, Program Coordinator, Infectious Diseases, Carver College of Medicine, University of Iowa, Iowa City, Iowa.
Hilary M. Babcock, Associate Professor of Medicine, Department of Internal Medicine, Washington University School of Medicine, St. Louis, Missouri.
Andrew T. Pavia, Professor, Division of Pediatric Infectious Diseases, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, UT.
Lisa M. Koonin, Acting Director, Influenza Coordination Unit, Office of Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, GA.
Philip M. Polgreen, Associate Professor of Internal Medicine, Department of Infectious Diseases and Associate Professor of Epidemiology, College of Public Health, Carver College of Medicine, University of Iowa, Iowa City, Iowa.
References
- 1.Larson EL, Liverman CT, editors. Committee on Personal Protective Equipment for Healthcare Personnel to Prevent Transmission of Pandemic Influenza and Other Viral Respiratory Infections: Current Research Issues; Institute of Medicine. Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases: Personal Protective Equipment for Healthcare Personnel: Update 2010. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Valenti WM. Influenza viruses. In: Mayhall CG, editor. Hospital Epidemiology and Infection Control. 4. ch 42 Philadelphia: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 3.Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110(1):1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 4.Lindsley WG, Blachere FM, Davis KA, et al. Distribution of airborne influenza virus and respiratory syncytial virus in an urgent care medical clinic. Clin Infect Dis. 2010;50(5):693–698. doi: 10.1086/650457. [DOI] [PubMed] [Google Scholar]
- 5.Bischoff WE, Swett K, Leng I, Peters TR. Exposure to influenza virus aerosols during routine patient care. J Infect Dis. 2013;207(7):1037–1046. doi: 10.1093/infdis/jis773. [DOI] [PubMed] [Google Scholar]
- 6.Lindsley WG, Noti JD, Blachere FM, et al. Viable influenza A virus in airborne particles from human coughs. J Occup Environ Hyg. 2015;12(2):107–113. doi: 10.1080/15459624.2014.973113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Interim guidance on infection control measures for 2009 H1N1 influenza in healthcare settings, including protection of healthcare personnel. [Accessed April 27, 2015];Centers for Disease Control and Prevention website. 2010 Jul 15; http://www.cdc.gov/h1n1flu/guidelines_infection_control.htm. [PubMed]
- 8.Reusability of Facemasks During an Influenza Pandemic: Facing the Flu. Washington, DC: National Academies Press; 2006. Committee on the Development of Reusable Facemasks for Use During an Influenza Pandemic. [Google Scholar]
- 9.Society for Healthcare Epidemiology of America. [Accessed June 9, 2015];SHEA Position Statement: Interim Guidance on Infection Control Precautions for Novel Swine-Origin Influenza A H1N1 in Healthcare Facilities. 2009 Jun 10; http://www.shea-online.org/assets/files/policy/061209_h1n1_statement.pdf.
- 10.Questions and answers regarding respiratory protection for preventing 2009 H1N1 influenza among healthcare personnel. [Accessed April 27, 2015];Centers for Disease Control and Prevention website. 2010 Feb 23; http://www.cdc.gov/h1n1flu/guidelines_infection_control_qa.htm#c.
- 11.Radonovich LJ, Magalian PD, Hollingsworth MK, Baracco G. Stockpiling supplies for the next influenza pandemic. Emerg Infect Dis. 2009;15(6):e1. doi: 10.3201/eid1506.081196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandemic planning: recommended guidance for extended use and limited reuse of N95 filtering facepiece respirators in healthcare settings. [Accessed April 27, 2015];Centers for Disease Control and Prevention website. 2014 Mar 13; http://www.cdc.gov/niosh/topics/hcwcontrols/RecommendedGuidanceExtUse.html.
- 13.Interim guidance for infection control within healthcare settings when caring for confirmed cases, probable cases, and cases under investigation for infection with novel influenza A viruses associated with severe disease. [Accessed April 27, 2015];Centers for Disease Control and Prevention website. Updated May 21, 2015. http://www.cdc.gov/flu/avianflu/h7n9-infection-control.htm.
- 14.Prevention strategies for seasonal influenza in healthcare settings: guidelines and recommendations. [Accessed April 27, 2015];Centers for Disease Control and Prevention website. 2013 Jan 9; http://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm.
- 15.Pillai SK, Beekmann SE, Santibanez S, Polgreen PM. The Infectious Diseases Society of America emerging infections network: bridging the gap between clinical infectious diseases and public health. Clin Infect Dis. 2014;58(7):991–996. doi: 10.1093/cid/cit932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loeb M, Dafoe N, Mahony J, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302(17):1865–1871. doi: 10.1001/jama.2009.1466. [DOI] [PubMed] [Google Scholar]
- 17.MacIntyre CR, Wang Q, Seale H, et al. A randomized clinical trial of three options for N95 respirators and medical masks in health workers. Am J Respir Crit Care Med. 2013;187(9):960–966. doi: 10.1164/rccm.201207-1164OC. [DOI] [PubMed] [Google Scholar]
- 18.Baig A, Knapp C, Eagan AE, Radonovich LJ., Jr Health care workers’ views about respirator use and features that should be included in the next generation of respirators. Am J Infect Control. 2010;38(1):18–25. doi: 10.1016/j.ajic.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ciconte R, Danyluk Q. Assessment and Determination of Practical Considerations for Wide-scale Utilization of Elastometric Half-facepiece Respirators during a Pandemic or Outbreak Situation. Richmond, BC: Work Safe BC; 2013. [Accessed June 9, 2015]. http://www.worksafebc.com/contact_us/research/funding_decisions/assets/pdf/2011/RS2011-IG13.pdf. [Google Scholar]
- 20.Khan A, Khan S, Zimmerman V, Baddour LM, Tleyjeh IM. Quality and strength of evidence of the Infectious Diseases Society of America clinical practice guidelines. Clin Infect Dis. 2010;51(10):1147–1156. doi: 10.1086/656735. [DOI] [PubMed] [Google Scholar]