Abstract
Background
In sub-Saharan Africa many children live in extreme poverty and experience a burden of illness and disease that is disproportionately high. The emergence of HIV and AIDS has only exacerbated long-standing challenges to improving children’s health in the region, with recent cohorts experiencing pediatric AIDS and high levels of orphan status, situations which are monitored globally and receive much policy and research attention. Children’s health, however, can be affected also by living with HIV-infected adults, through associated exposure to infectious diseases and the diversion of household resources away from them. While long recognized, far less research has focused on characterizing this distinct and vulnerable population of HIV-affected children.
Methods
Using Demographic and Health Survey data from 23 countries collected between 2003 and 2011, we estimate the percentage of children living in a household with at least one HIV-infected adult. We assess overlaps with orphan status and investigate the relationship between children and the adults who are infected in their households.
Results
The population of children living in a household with at least one HIV-infected adult is substantial where HIV prevalence is high; in Southern Africa, the percentage exceeded 10% in all countries and reached as high as 36%. This population is largely distinct from the orphan population. Among children living in households with tested, HIV-infected adults, most live with parents, often mothers, who are infected; nonetheless, in most countries over 20% live in households with at least one infected adult who is not a parent.
Conclusion
Until new infections contract significantly, improvements in HIV/AIDS treatment suggest that the population of children living with HIV-infected adults will remain substantial. It is vital to on-going efforts to reduce childhood morbidity and mortality to consider whether current care and outreach sufficiently address the distinct vulnerabilities of these children.
Introduction
In sub-Saharan Africa many children live in extreme poverty and experience a burden of illness and disease that is disproportionately high [1, 2]. Despite declines, the under-five mortality rate in the region is still 16 times that of developed countries, and children continue to die from preventable or treatable causes, including infectious diseases such as pneumonia, diarrhea, or malaria [2]. The emergence of HIV and AIDS several decades ago, which disproportionately affects sub-Saharan Africa, has only exacerbated long-standing challenges to improving children’s health. In 2013, 25 million adults and children lived with HIV in sub-Saharan Africa—71% of the total infected global population [3].
The importance of this HIV context for children’s vulnerabilities has been recognized by scholars, practitioners, and policymakers [4]. The Global Plan towards the elimination of new infections among children has emphasized reducing mother-to-child transmission, and between 2009 and 2013, the number of new HIV infections in children has been reduced by 43% in the designated 21 priority countries in sub-Saharan Africa [3], though many children remain undiagnosed [5]. Aside from pediatric infection, vulnerabilities result from living in families and communities deeply affected by HIV. A particularly visible consequence has been a rise in the number of orphans in the region. While not all parental deaths result from AIDS, in 2013 over 15 million children in sub-Saharan Africa were estimated to have lost one or both parents to AIDS [4]. In Swaziland and Lesotho, the countries with the highest HIV prevalence, an estimated 70% of orphans lost their parents to AIDS [1]. Children who experience parental death have been found to be at increased risk of poorer health and schooling outcomes relative to other children [6–11].
Even in the absence of pediatric infection or adult mortality, living in households or families with HIV-infected adults can render children vulnerable. Children living in close proximity to infected adults face exposure to opportunistic infections (OIs) like tuberculosis, hepatitis, pneumonia, and diarrheal disease [12]. While the introduction of antiretroviral therapy (ART) has contributed to a marked improvement in the quality of life and OI mortality of HIV-infected persons, risks of OIs persist because individuals may not know their HIV status, patients may not be on needed ART, or patients on ART may have poor adherence [12]. While all co-resident household members may be at increased risk of exposure to OIs, young children may be especially susceptible because they experience the most direct contact with adults, spend much of their time in the home, and upon exposure, can experience more severe illness than older household members. In addition, children’s symptoms, such as respiratory symptoms associated with TB or pneumonia, can be mistakenly attributed to less serious common childhood illnesses, and not treated [13]. Older children are also at risk, particularly because it is not uncommon for them to provide care for ill adults [14].
Besides direct exposure to adult illness, the health and well-being of children living in a household with an HIV-infected adult can be compromised if attention of household adults or older children is redirected toward the infected adult; children’s household responsibilities increase; or resources needed for schooling, nutrition, or medical care are diverted away from the child [15–18]. This situation may be compounded by financial strain associated with a change in the work status of an ill adult. In addition, children sometimes experience HIV-associated stigma in their communities and schools, and among networks of family and friends, which may negatively affect their health and well-being, including mental health [19, 20].
Several strands of emerging research in the region provide evidence of diminished outcomes for children living with and caring for HIV-infected adults. Single and multi-country studies link having an HIV-infected parent with malnutrition, lack of medical care, excess infant and childhood mortality risk, and decreased likelihood of school attendance [21–25]. Research also reveals higher burdens of acute and chronic morbidity for children whose parents have an AIDS-related illness [17], and elevated risk of pulmonary tuberculosis symptoms for children who provide care for co-resident ill adults [13, 14, 26].
In this article, we document the extent to which children in sub-Saharan Africa live in households with HIV-infected adults. Despite growing recognition that children living with HIV-infected adults are also HIV-affected, most publications that monitor the situation of children in the context of AIDS report only the prevalence and incidence of pediatric HIV, the percentage of HIV-infected pregnant women receiving treatment, and the prevalence of children who have lost one or both parents to AIDS or other causes [4, 27]. A notable exception is a Demographic and Health Survey (DHS) report that assessed the situation of orphans and vulnerable children across eight sub-Saharan African countries, and included a measure of the proportion of children living in households with an HIV-infected adult [28]. In this study, we estimate the prevalence of children living in households with HIV-infected adults based on recent DHS data from 23 countries in the region. We also characterize this population of children further by assessing its overlaps with the orphan population, as a child whose parent has died from complications of AIDS may also be likely to live with an HIV-infected adult if he or she lives with a surviving parent. In addition, because it is quite common for children in the region to be co-resident with non-parental adults [29–34], we document how frequently the HIV-infected adults in children’s households are their mothers or fathers. Since interventions targeted at children in families involve outreach to adults, additional detail on the nature of the relationship between the children and the HIV-infected adults in their households may be useful for focusing multi-sector response.
Measuring the population of children living in households with HIV-infected adults is critical and timely. Global efforts to encourage HIV testing and treatment have resulted in substantial increases in the number of people receiving treatment [35]. The United Nations reports that there was a 20-fold increase in the uptake of antiretroviral treatment (ART) in the developing world between 2003 and 2011 [36]. In sub-Saharan Africa, 7.5 million people received ART for HIV or AIDS in 2012 [37], though in 2013, treatment coverage was estimated to be at only 37% of all people living with HIV [3]. As treatment grows, and more adults learn their status and receive treatment, parents and other adult household members who in past years might have died of AIDS-related illnesses can be expected to live longer. Programmatic news on efforts to reduce HIV infections is also positive, but new infections are still far too common. In 2013, 1.5 million people were newly infected with HIV in sub-Saharan Africa [38]; efforts to reduce infections among adults have been far less successful than efforts to reduce infections among children [3]. The combination of reductions in HIV mortality due to increased treatment, sustained population growth, and the persistent addition of newly-infected individuals who are more frequently adults and less frequently children, suggests that the population of children living in households with HIV-infected adults, now and in the near future, will be substantial [39].
Methods
Ethical Considerations
All analyses conducted in this paper are based on secondary data with all participant identifiers removed. The ICF International Institutional Review Board (IRB), which requires compliance with the U.S. Department of Health and Human Services regulations for the protection of human subjects (45 CFR 46), reviewed and approved all procedures and questionnaires. In addition, typically an IRB in the host country ensured that the survey complied with laws and norms of the nation. Ethical permission to use the data was obtained from ORC Macro Inc. Additional detail on the procedures regarding the protection of human subjects is available on the DHS website (http://dhsprogram.com/What-We-Do/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm#sthash.YAZ3GK1r.dpuf).
Data and Analyses
Data are from nationally representative population samples collected as part of the Demographic and Health Surveys. The DHS use standardized questionnaires and protocols to facilitate cross-country analyses. Since 2001, many DHS surveys have included HIV testing. We include in our analysis all DHS surveys conducted in sub-Saharan Africa that include HIV testing as part of the Standard DHS or AIDS Indicator Surveys (AIS). In addition, we limit the sample to surveys that possess the information required to link children with their biological parents and ascertain parents’ survival status. In the case of a country with repeated surveys that fit these criteria, results from the most recent survey are reported. Our final sample includes data for 23 countries collected between 2003 and 2011. Background detail, including characteristics of the sampled populations, DHS/AIS testing rates, and adult HIV prevalence, are summarized in Table 1.
Table 1. Sample Characteristics and Adult HIV Prevalence.
| Country | Survey year | Total N | Age range of women tested for HIV | Percent of eligible women tested* | Age range of men tested for HIV | Percent of eligible men tested* | Adult HIV prevalence (15–49)** |
|---|---|---|---|---|---|---|---|
| Southern Africa | |||||||
| Lesotho | 2009 | 9,987 | 15–49 | 93.6 | 15–59 | 88.0 | 23.0 |
| Malawi | 2010 | 22,788 | 15–49 | 90.5 | 15–54 | 83.7 | 10.6 |
| Mozambique | 2009 | 14,028 | 15–64 | 92.3 | 15–64 | 91.7 | 11.5 |
| Swaziland | 2007 | 11,190 | 15–49 | 87.2 | 15–49 | 77.6 | 25.9 |
| Zambia | 2007 | 19,462 | 15–49 | 77.1 | 15–59 | 72.2 | 14.3 |
| Zimbabwe | 2011 | 20,458 | 15–49 | 79.9 | 15–54 | 69.3 | 15.2 |
| Central and East Africa | |||||||
| Cameroon | 2011 | 17,864 | 15–49 | 93.7 | 15–59 | 92.3 | 4.3 |
| DRC | 2007 | 12,799 | 15–49 | 90.3 | 15–59 | 86.3 | 1.3 |
| Ethiopia | 2011 | 39,538 | 15–49 | 89.3 | 15–59 | 81.8 | 1.5 |
| Kenya | 2009 | 9,615 | 15–49 | 86.3 | 15–54 | 79.2 | 6.3 |
| Rwanda | 2010 | 14,342 | 15–49 | 98.9 | 15–59 | 98.2 | 3.0 |
| Sao Tome and Principe | 2009 | 6,727 | 15–49 | 87.5 | 15–59 | 70.9 | 1.5 |
| Tanzania | 2008 | 23,895 | 15–49 | 89.5 | 15–49 | 79.8 | 5.7 |
| West Africa | |||||||
| Burkina Faso | 2010 | 21,976 | 15–49 | 96.3 | 15–59 | 93.7 | 1.0 |
| Burundi | 2010 | 11,202 | 15–49 | 91.8 | 15–59 | 88.8 | 1.4 |
| Cote D’Ivoire | 2005 | 11,970 | 15–49 | 79.1 | 15–49 | 76.3 | 4.7 |
| Ghana | 2003 | 13,287 | 15–49 | 89.3 | 15–59 | 80.0 | 2.2 |
| Guinea | 2005 | 10,286 | 15–49 | 92.5 | 15–59 | 88.2 | 1.5 |
| Liberia | 2007 | 18,048 | 15–49 | 87.0 | 15–49 | 80.4 | 1.6 |
| Mali | 2006 | 13,630 | 15–49 | 90.7 | 15–59 | 83.7 | 1.3 |
| Niger | 2006 | 13,669 | 15–49 | 90.7 | 15–59 | 84.2 | 0.7 |
| Senegal | 2011 | 15,698 | 15–49 | 83.7 | 15–59 | 76.3 | 0.7 |
| Sierra Leone | 2008 | 10,934 | 15–49 | 87.7 | 15–59 | 85.0 | 1.5 |
Source: Demographic and Health Surveys (DHS)
* Respondent present on the day of interview, consented to HIV serostatus testing, and tested during their DHS/AIS interview. Percent tested as reported in Demographic patterns of HIV testing uptake in sub-Saharan Africa: DHS Comparative Reports 30. [42] and DHS Country Reports.
** HIV prevalence as available from the HIV/AIDS Survey Indicators Database (accessed at http://hivdata.dhsprogram.com/ on July 17, 2015)
The DHS data reflect nationally representative samples of mostly reproductive aged women and men, with some variability in selected age ranges across the 23 countries. In each country, households were randomly selected for participation and age-eligible men and women completed surveys and were offered HIV testing. Table 1 provides detailed information on age eligibility; in most countries, women aged 15–49 and men 15–59 were eligible. In eight surveys, all households participating in the DHS survey were selected for the HIV test, while in the remaining surveys a random sub-sample of households (usually one-half or one-third) were selected. In most surveys, HIV testing was conducted using dried blood spot (DBS) samples of capillary blood from a finger prick. Details on sample collection and laboratory testing are available elsewhere [40].
We link the results from HIV testing with information on children, their families, and their households collected through the DHS household interviews. We consider the HIV status of all adults who are members of children’s households. As is common in UNICEF reports, children are defined to be those aged 0–17, whenever possible [27]. In five countries, information about parental survival status and residence is collected only for children through age 14, and for these countries, calculations related to orphan status are limited to children through age 14. We report only on co-residence with HIV-infected adults because HIV tests in the vast majority of DHS surveys are not administered to children. We adjust our analyses using DHS provided household sample weights. Because these sample weights are at the household level, rather than the level of the individual child, we further adjust the DHS provided weights by the child’s household size.
We calculate the percentage of children living in households with at least one HIV-infected adult from the population of children living in households in which at least one eligible adult aged 18 and older was successfully tested for HIV (i.e., had a positive or negative test). Test participation varies across settings, and is reported in Table 1. Recent assessment of bias in non-response from two-stage and multi-stage estimates suggests that where non-response bias exists, it is in the direction of underestimating HIV prevalence [41]. Consequently, the estimates presented of the percentage of children living in households with infected adults based on the tested population are likely conservative estimates.
Nonetheless, we also calculate a still lower bound estimate that expands the denominator to include all children in households that were selected for HIV testing, regardless of whether any adults in the household were present, eligible, or participated in the test. In effect, we assume that all non-tested adults would have tested negative had they been tested. Since children who live in households with adults eligible for testing who are not tested, or who live in households with adults who are not eligible for testing (such as older adults), may well live with an HIV-infected adult, these estimates provide the most conservative benchmark [43].
After estimating the percentage of children living in households with seropositive adults, we investigate overlap between this group and the group of children who are orphaned. The denominator for these calculations is limited to children living in households in which at least one adult 18 or older had a positive or negative HIV test result. Orphan status is determined through responses to questions about parental survival status in DHS household questionnaires. Children who have lost at least one biological parent to death are coded as orphans. When parental status is unknown, children are coded as non-orphans.
In analyses of kin connection, we limit the sample to children who live with at least one seropositive adult. We construct measures that indicate kin connection between each child and the seropositive adults with whom they share a household. We distinguish between mothers, fathers, and other adults, using information from the household schedule on survivorship and residence of biological mothers and fathers. Children can live with more than one adult who has tested positive, and thus separate measures are coded to reflect each relationship. In analysis, we further describe co-residence with HIV-infected adults by summarizing with four mutually exclusive categories: mother but not father, father but not mother, mother and father, or neither mother nor father. In this analysis, co-residence with seropositive adults who are neither mothers nor fathers is possible in every category. Given sample limitations associated with testing, and patterns of non-testing, we emphasize that the estimates presented summarize kin connection only for the sample of children who live in a household with at least one adult with a valid test result, and take into account only tested adults in the household. Other non-tested adults who are seropositive may well live with these children and would not be captured in these figures.
Results
As shown in Table 2, the percentage of children ages 0–17 living with at least one HIV-infected adult is highest in southern Africa, mid-range in central and east Africa, and lowest in West Africa. In Southern Africa, it ranges from about 14% in Mozambique to 36% in Swaziland. In Central and East Africa, prevalence ranges between 2% in Ethiopia and Sao Tome and Principe to 10% in Kenya. Prevalence is lowest in West Africa, at 1% in Niger and Senegal, but nonetheless, over 7% in Cote D’Ivoire.
Table 2. Co-residence of Children 0–17 with HIV-infected adults, by Country.
| Among households with at least one adult tested for HIV… | Among all households selected for an HIV test…. | ||||||
|---|---|---|---|---|---|---|---|
| Country | Survey year | Adult HIV Prevalence* | N | % children living with at least one HIV+ adult** | N | % children living with adults, but adults not tested | % children living with at least one HIV+ adult***(LOWER BOUND) |
| Southern Africa | |||||||
| Lesotho | 2009 | 23.0 | 7,386 | 33.2 | 9,987 | 27.2 | 24.2 |
| (32.2–34.3) | (26.3–28.1) | (23.4–25.0) | |||||
| Malawi | 2010 | 10.6 | 18,256 | 15.5 | 22,788 | 22.4 | 12.0 |
| (15.0–16.0) | (21.9–23.0) | (11.6–12.4) | |||||
| Mozambique | 2009 | 11.5 | 12,118 | 14.2 | 14,028 | 14.4 | 12.2 |
| (13.6–14.9) | (13.8–15.0) | (11.6–12.7) | |||||
| Swaziland | 2007 | 25.9 | 9,219 | 36.3 | 11,190 | 19.1 | 29.4 |
| (35.4–37.3) | (18.3–19.8) | (28.6–30.3) | |||||
| Zambia | 2007 | 14.3 | 14,317 | 19.6 | 19,462 | 29.1 | 13.9 |
| (18.9–20.2) | (28.4–29.7) | (13.4–14.4) | |||||
| Zimbabwe | 2011 | 15.2 | 14,384 | 22.1 | 20,458 | 29.7 | 15.6 |
| (21.5–22.8) | (29.1–30.3) | (15.1–16.1) | |||||
| Central and East Africa | |||||||
| Cameroon | 2011 | 4.3 | 15,492 | 7.6 | 17,864 | 15.3 | 6.4 |
| (7.2–8.0) | (14.8–15.8) | (6.1–6.8) | |||||
| DRC | 2007 | 1.3 | 11,221 | 2.6 | 12,799 | 13.0 | 2.3 |
| (2.3–2.9) | (12.5–13.6) | (2.0–2.5) | |||||
| Ethiopia | 2011 | 1.5 | 34,594 | 2.2 | 39,538 | 14.6 | 1.9 |
| (2.0–2.3) | (14.3–15.0) | (1.7–2.0) | |||||
| Kenya | 2009 | 6.3 | 8,520 | 10.4 | 9,615 | 13.7 | 9.0 |
| (9.8–11.1) | (13.0–14.4) | (8.4–9.6) | |||||
| Rwanda | 2010 | 3.0 | 13,241 | 5.0 | 14,342 | 10.7 | 4.5 |
| (4.6–5.4) | (10.2–11.2) | (4.1–4.8) | |||||
| Sao Tome and Principe | 2009 | 1.5 | 5,653 | 2.3 | 6,727 | 19.5 | 1.9 |
| (2.0–2.7) | (18.5–20.4) | (1.6–2.2) | |||||
| Tanzania | 2008 | 5.7 | 19,957 | 9.2 | 23,895 | 20.5 | 7.3 |
| (8.8–9.6) | (19.9–21.0) | (7.0–7.7) | |||||
| West Africa | |||||||
| Burkina Faso | 2010 | 1.0 | 19,784 | 1.7 | 21,976 | 11.6 | 1.5 |
| (1.6–1.9) | (11.2–12.0) | (1.4–1.7) | |||||
| Burundi | 2010 | 1.4 | 10,172 | 2.4 | 11,202 | 11.6 | 2.1 |
| (2.1–2.7) | (11.0–12.2) | (1.9–2.4) | |||||
| Cote D’Ivoire | 2005 | 4.7 | 9,247 | 7.5 | 11,970 | 27.8 | 5.4 |
| (6.9–8.0) | (27.0–28.6) | (5.0–5.8) | |||||
| Ghana | 2003 | 2.2 | 10,525 | 3.0 | 13,287 | 23.8 | 2.3 |
| (2.6–3.3) | (23.1–24.6) | (2.0–2.5) | |||||
| Guinea | 2005 | 1.5 | 8,587 | 2.4 | 10,286 | 19.1 | 1.9 |
| (2.0–2.7) | (18.3–19.8) | (1.6–2.2) | |||||
| Liberia | 2007 | 1.6 | 14,455 | 1.8 | 18,048 | 20.4 | 1.4 |
| (1.6–2.0) | (19.9–21.0) | (1.3–1.6) | |||||
| Mali | 2006 | 1.3 | 11,458 | 1.9 | 13,630 | 17.9 | 1.6 |
| (1.7–2.2) | (17.3–18.5) | (1.4–1.8) | |||||
| Niger | 2006 | 0.7 | 11,547 | 1.0 | 13,669 | 18.1 | 0.8 |
| (0.8–1.2) | (17.5–18.8) | (0.7–1.0) | |||||
| Senegal | 2011 | 0.7 | 13,569 | 1.3 | 15,698 | 15.2 | 1.1 |
| (1.2–1.5) | (14.6–15.7) | (1.0–1.3) | |||||
| Sierra Leone | 2008 | 1.5 | 8,579 | 2.0 | 10,934 | 23.0 | 1.5 |
| (1.7–2.3) | (22.2–23.8) | (1.3–1.8) | |||||
Source: Demographic and Health Surveys (DHS)
Note: The measures use household weights provided by the DHS as well as weights for household size.
* DHS estimates, HIV prevalence among adults 15–49.
** Denominator is limited to children 0–17 living in households in which at least one adult aged 18+ had a positive or negative HIV test result.
*** Denominator includes all children 0–17 living in households selected for HIV testing. The lower bound estimate assumes that in households in which no adult was tested, if all eligible adults were tested none would test positive.
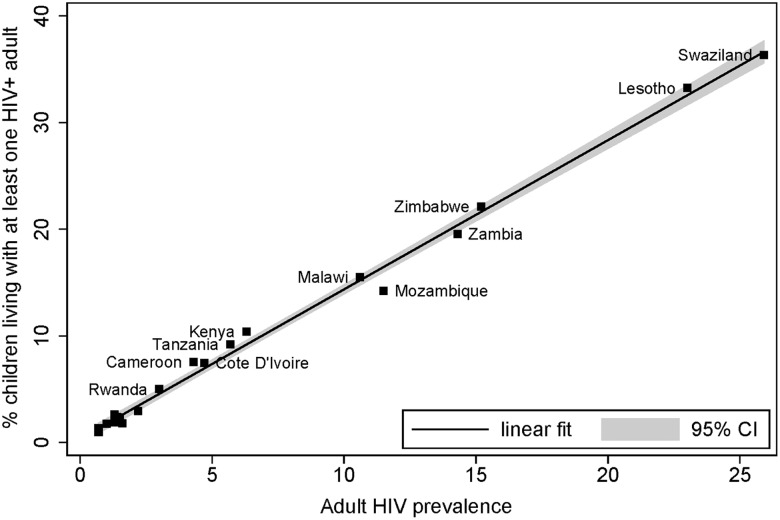
Fig 1 plots the percentage of children living in a household with at least one HIV-infected adult against adult HIV prevalence for each country. Although the timing and nature of the HIV/AIDS epidemic varies across countries, as do programmatic responses and family organization, the plot suggests that children’s likelihood of living in households with HIV-infected adults tracks HIV prevalence closely, such that the relationship is near linear.
Fig 1. Co-residence of Children 0–17 with HIV-infected Adults and Adult HIV Prevalence (15–49), by Country.
Source: Demographic and Health Surveys (DHS).
While only a small fraction of children live in households without an adult (less than 1.6% in every country, not shown), substantial fractions of children live in households in which no adults, or not all adults, were tested. While testing rates are high in most of the DHS/AIS surveys (Table 1), they are based on those eligible for testing. Further, in some cases, both women and men are selected for interview and testing, but only one may be tested. In other cases, one or more adults in the household may fall out of the eligible age range for testing. In cases where one adult tests negative, non-tested adults could be positive. Accordingly, in the final two columns of Table 2, we present a lower bound and upper bound estimate that takes into account the population not tested. The lower bound estimate is the percentage of children living in a household with at least one HIV-infected adult, under the assumption that all non-tested adults are not infected. The lower bound calculations affect the estimates most in Southern Africa, where both HIV prevalence and the percentage of those not tested is high. Still, even under the assumption that all non-tested adults are negative, the percentage of children living with HIV-infected adults is close to 30% in Swaziland, and between 12% and 24% across the remaining five countries in Southern Africa.
In Table 3 we explore the degree to which the population of children living with HIV-infected adults is distinct from that of children who are orphans. Results indicate that most are not orphans. For example, while 33% of children in Lesotho in 2010 were living with an HIV-infected adult, only 10% were both living with an HIV-infected adult and orphaned. Similarly, in Zimbabwe, while 22% of children lived with an HIV-infected adult, only 6% both lived with an HIV-infected adult and were orphaned. Considering both adult mortality and infection reveals the extensive reach of the epidemic into children’s lives. In Lesotho and Swaziland, where about 70% of orphans are estimated to be orphaned due to AIDS, a staggering 50% of children are either orphans or live in a household with an HIV-infected adult [1].
Table 3. Co-residence of Children 0–17* with HIV-infected Adults and Orphan Status, by Country**.
| Country | Survey year | N | Adult HIV Prevalence*** | % living with HIV+ adult, not orphaned | % living with HIV+ adult, orphaned | % not living with HIV+ adult, orphaned | % not living with HIV+ adult, not orphaned |
|---|---|---|---|---|---|---|---|
| Southern Africa | |||||||
| Lesotho | 2009 | 7,386 | 23.0 | 23.2 | 10.0 | 16.3 | 50.4 |
| (22.3–24.2) | (9.3–10.7) | (15.5–17.2) | (49.3–51.6) | ||||
| Malawi | 2010 | 18,256 | 10.6 | 12.3 | 3.2 | 7.1 | 77.4 |
| (11.8–12.7) | (3.0–3.5) | (6.7–7.5) | (76.8–78.0) | ||||
| Mozambique | 2009 | 12,118 | 11.5 | 11.4 | 2.8 | 9.2 | 76.5 |
| (10.9–12.0) | (2.5–3.1) | (8.7–9.7) | (75.8–77.3) | ||||
| Swaziland | 2007 | 9,219 | 25.9 | 26.5 | 9.8 | 13.7 | 49.9 |
| (25.6–27.4) | (9.2–10.4) | (13.0–14.5) | (48.9–50.9) | ||||
| Zambia | 2007 | 14,317 | 14.3 | 15.7 | 3.9 | 7.6 | 72.8 |
| (15.1–16.3) | (3.6–4.2) | (7.2–8.1) | (72.1–73.5) | ||||
| Zimbabwe | 2011 | 14,384 | 15.2 | 16.0 | 6.1 | 11.5 | 66.3 |
| (15.4–16.6) | (5.7–6.5) | (11.0–12.1) | (65.6–67.1) | ||||
| Central and East Africa | |||||||
| Cameroon | 2011 | 15,492 | 4.3 | 6.6 | 1.0 | 8.5 | 84.0 |
| (6.2–7.0) | (0.8–1.1) | (8.0–8.9) | (83.4–84.6) | ||||
| DRC | 2007 | 11,221 | 1.3 | 2.2 | 0.4 | 8.2 | 89.2 |
| (2.0–2.5) | (0.3–0.5) | (7.7–8.7) | (88.7–89.8) | ||||
| Ethiopia | 2011 | 34,594 | 1.5 | 1.7 | 0.5 | 8.4 | 89.4 |
| (1.5–1.8) | (0.4–0.6) | (8.2–8.7) | (89.1–89.7) | ||||
| Kenya**** | 2003 | 6,429 | 6.3 | 8.5 | 2.3 | 8.8 | 80.3 |
| (7.9–9.2) | (2.0–2.7) | (8.1–9.5) | (79.4–81.3) | ||||
| Rwanda | 2010 | 13,241 | 3.0 | 3.7 | 1.4 | 12.2 | 82.9 |
| (3.3–4.0) | (1.2–1.5) | (11.6–12.7) | (82.2–83.5) | ||||
| Sao Tome and | 2009 | 5,653 | 1.5 | 2.3 | 0.1 | 3.6 | 94.1 |
| Principe | (1.9–2.7) | (0.0–0.1) | (3.1–4.0) | (93.5–94.7) | |||
| Tanzania | 2008 | 19,957 | 5.7 | 7.5 | 1.7 | 7.3 | 83.5 |
| (7.1–7.9) | (1.5–1.9) | (7.0–7.7) | (83.0–84.0) | ||||
| West Africa | |||||||
| Burkina Faso | 2010 | 18,106 | 1.0 | 1.6 | 0.1 | 3.6 | 94.7 |
| (1.4–1.8) | (0.1–0.2) | (3.3–3.9) | (94.4–95.1) | ||||
| Burundi | 2010 | 10,172 | 1.4 | 2.0 | 0.4 | 11.8 | 85.8 |
| (1.7–2.2) | (0.3–0.6) | (11.2–12.4) | (85.2–86.5) | ||||
| Cote D’Ivoire | 2005 | 9,247 | 4.7 | 6.6 | 0.9 | 6.1 | 86.4 |
| (6.1–7.1) | (0.7–1.1) | (5.6–6.6) | (85.7–87.1) | ||||
| Ghana | 2003 | 10,525 | 2.2 | 2.7 | 0.3 | 4.9 | 92.2 |
| (2.4–3.0) | (0.2–0.4) | (4.5–5.3) | (91.7–92.7) | ||||
| Guinea | 2005 | 8,035 | 1.5 | 1.8 | 0.5 | 5.9 | 91.8 |
| (1.5–2.1) | (0.3–0.6) | (5.4–6.4) | (91.2–92.4) | ||||
| Liberia | 2007 | 14,455 | 1.6 | 1.6 | 0.2 | 6.1 | 92.2 |
| (1.4–1.8) | (0.1–0.3) | (5.7–6.4) | (91.7–92.6) | ||||
| Mali | 2006 | 10,748 | 1.3 | 1.8 | 0.2 | 5.5 | 92.6 |
| (1.5–2.0) | (0.1–0.2) | (5.1–5.9) | (92.1–93.1) | ||||
| Niger | 2006 | 10,970 | 0.7 | 0.8 | 0.2 | 4.4 | 94.6 |
| (0.6–1.0) | (0.1–0.2) | (4.0–4.8) | (94.2–95.1) | ||||
| Senegal | 2011 | 13,569 | 0.7 | 1.3 | 0.1 | 6.4 | 92.3 |
| (1.1–1.5) | (0.0–0.1) | (5.6–6.8) | (91.8–92.7) | ||||
| Sierra Leone | 2008 | 8,579 | 1.5 | 1.8 | 0.2 | 8.6 | 89.4 |
| (1.5–2.1) | (0.1–0.3) | (8.1–9.2) | (88.7–90.0) | ||||
Source: Demographic and Health Survey (DHS)
Note: The measures use household weights provided by the DHS as well as weights for household size.
* The statistics for Kenya, Burkina Faso, Guinea, Mali, and Niger exclude children 15–17 because parental survival status is not available for this age group.
** In columns 5–8, the denominator is limited to children living in households in which at least one adult 18+ had a positive or negative HIV test result.
*** DHS estimates, HIV prevalence among adults 15–49.
**** Data from the Kenya 2003 survey are used in the current table because information on parental survival status was not collected in the 2009 survey.
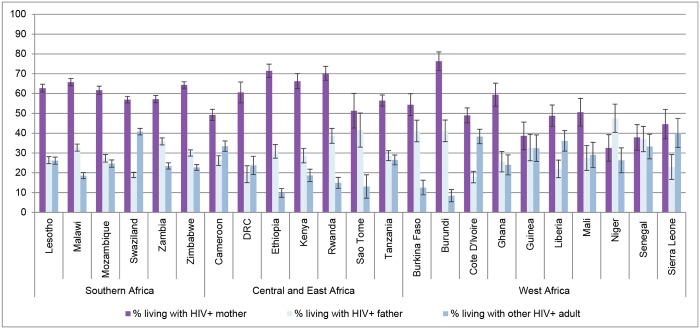
Next, Fig 2 shows the relationship between children and the HIV-infected adults in their households, as reflected in the tested sample. In the majority of cases, children who are living with an HIV-infected adult in the household are living with at least one HIV-infected parent, most often an HIV-infected mother. In Southern Africa, where HIV prevalence is highest, over two-thirds, and usually about 80%, of children who live in households with an HIV-infected adult, live with a parent who is HIV-infected. These percentages are similar in Central, East, and West Africa. Despite the preponderance of co-residence with HIV-infected parents, it is nonetheless important to note that in most countries over 20%, and sometimes over one-third, of children live in a household with at least one HIV-infected adult who is not a parent.
Fig 2. Among Children 0–17* Living with at Least One HIV-infected Adult, Percent Living with HIV-infected Mothers, Fathers, and Others, by Country.
Source: Demographic and Health Surveys (DHS). * The statistics for Kenya, Burkina Faso, Guinea, Mali, and Niger exclude children 15–17 because information on parental co-residence was not collected for this age group. ** Data from the Kenya 2003 survey are used because information on parental co-residence was not collected in the 2009 survey. Note: The measures use household weights provided by the DHS as well as weights for household size.
Finally, Table 4 presents the extent to which children live with an HIV-infected mother, father, both, or neither, among the sample of children who live with at least one HIV-infected adult in their household. While it is most common for children to live with an HIV-infected mother only, a substantial fraction, more than 10% in every country, live in a household in which both their mother and father is infected. We emphasize, however, that children’s living arrangements vary significantly across these settings, and these statistics reflect the relationships of the tested, HIV-infected adults in the household to the children; parents who are not HIV-infected may be present or absent, and some who are present may not be tested. Nonetheless, these data provide a glimpse into the nature of relationships among tested adults and children as available in the DHS.
Table 4. Among Children 0–17* Living with HIV-infected Adults, Percent Living with HIV-infected Parents.
| Country | Survey year | N | % living with HIV+ mother and not HIV+ father | % living with HIV+ father and not HIV+ mother | % living with HIV+ father and HIV+ mother | % living with neither HIV+ father nor HIV+ mother |
|---|---|---|---|---|---|---|
| Southern Africa | ||||||
| Lesotho | 2009 | 2,340 | 51.6 | 15.2 | 11.1 | 22.1 |
| (49.6–53.6) | (13.8–16.7) | (9.9–12.4) | (20.4–23.7) | |||
| Malawi | 2010 | 2,624 | 51.7 | 18.6 | 14.1 | 15.6 |
| (49.8–53.6) | (17.1–20.1) | (12.8–15.4) | (14.2–17.0) | |||
| Mozambique | 2009 | 2,096 | 51.5 | 17.2 | 10.2 | 21.2 |
| (49.4–53.7) | (15.5–18.8) | (8.9–11.5) | (19.4–23.0) | |||
| Swaziland | 2007 | 3,349 | 48.0 | 10.0 | 8.9 | 33.1 |
| (46.3–49.7) | (9.0–11.0) | (7.9–9.8) | (31.5–34.7) | |||
| Zambia | 2007 | 2,784 | 44.6 | 23.3 | 12.5 | 19.6 |
| (42.8–46.5) | (21.7–24.9) | (11.3–13.8) | (18.1–21.0) | |||
| Zimbabwe | 2011 | 3,308 | 50.6 | 16.2 | 13.7 | 19.5 |
| (48.9–52.3) | (15.0–17.5) | (12.6–14.9) | (18.1–20.8) | |||
| Central and East Africa | ||||||
| Cameroon | 2011 | 1,232 | 43.3 | 20.2 | 6.0 | 30.6 |
| (40.5–46.0) | (17.9–22.4) | (4.7–7.3) | (28.0–33.2) | |||
| DRC | 2007 | 333 | 57.3 | 16.0 | 3.2 | 23.4 |
| (52.0–62.7) | (12.1–20.0) | (1.3–5.1) | (18.8–28.0) | |||
| Ethiopia | 2011 | 696 | 60.8 | 20.1 | 10.7 | 8.4 |
| (57.1–64.4) | (17.1–23.1) | (8.4–13.0) | (6.4–10.5) | |||
| Kenya** | 2009 | 596 | 55.0 | 17.4 | 11.2 | 16.3 |
| (51.0–59.0) | (14.4–20.5) | (8.7–13.8) | (13.4–19.3) | |||
| Rwanda | 2010 | 657 | 48.9 | 17.4 | 21.3 | 12.4 |
| (45.1–52.8) | (14.5–20.3) | (18.1–24.4) | (9.9–15.0) | |||
| Sao Tome and | 2009 | 129 | 45.4 | 35.6 | 5.9 | 13.0 |
| Principe | (36.7–54.1) | (27.3–44.0) | (1.8–10.0) | (7.2–18.9) | ||
| Tanzania | 2008 | 1,207 | 49.1 | 21.2 | 7.4 | 22.3 |
| (46.3–51.9) | (18.9–23.6) | (5.9–8.9) | (20.0–24.7) | |||
| West Africa | ||||||
| Burkina Faso | 2010 | 312 | 47.1 | 33.9 | 7.2 | 11.8 |
| (41.6–52.7) | (28.6–39.1) | (4.3–10.1) | (8.2–15.4) | |||
| Burundi | 2010 | 317 | 50.4 | 15.3 | 25.9 | 8.4 |
| (44.9–56.0) | (11.3–19.2) | (21.1–30.8) | (5.3–11.5) | |||
| Cote D’Ivoire | 2005 | 680 | 45.8 | 14.6 | 3.2 | 36.4 |
| (42.0–49.5) | (12.0–17.3) | (1.9–4.5) | (32.8–40.0) | |||
| Ghana | 2003 | 277 | 51.7 | 17.9 | 7.7 | 22.7 |
| (45.8–57.7) | (13.4–22.4) | (4.5–10.8) | (17.7–27.7) | |||
| Guinea | 2005 | 192 | 34.9 | 29.0 | 3.7 | 32.4 |
| (28.1–41.7) | (22.5–35.5) | (1.0–6.4) | (25.7–39.1) | |||
| Liberia | 2007 | 335 | 44.7 | 17.9 | 4.1 | 33.4 |
| (39.4–50.1) | (13.7–22.0) | (2.0–6.2) | (28.3–38.4) | |||
| Mali | 2006 | 198 | 43.5 | 20.4 | 7.1 | 29.0 |
| (36.5–50.5) | (14.8–26.1) | (3.5–10.7) | (22.6–35.4) | |||
| Niger | 2006 | 192 | 26.8 | 41.8 | 5.7 | 25.7 |
| (20.5–33.2) | (34.8–48.9) | (2.4–9.0) | (19.4–31.9) | |||
| Senegal | 2011 | 222 | 31.0 | 30.2 | 6.9 | 32.0 |
| (24.8–37.1) | (24.1–36.2) | (3.5–10.3) | (25.8–38.2) | |||
| Sierra Leone | 2008 | 176 | 37.6 | 15.9 | 7.0 | 39.5 |
| (30.4–44.8) | (10.5–21.4) | (3.2–10.8) | (32.3–46.8) | |||
Source: Demographic and Health Survey (DHS)
Note: The measures use household weights provided by the DHS as well as weights for household size.
* The statistics for Kenya, Burkina Faso, Guinea, Mali, and Niger exclude children 15–17 because information on parental co-residence is not available for this age group.
** Data from the Kenya 2003 survey are used because information on parental co-residence was not collected in the 2009 survey.
Discussion
The estimates we present from 23 countries across sub-Saharan Africa demonstrate that the population of children living in a household with an HIV-infected adult is large where HIV prevalence is high, and that it is somewhat distinct from the orphan population. The majority of children living in households with HIV-infected adults, at least as represented in the DHS samples, live with parents, often mothers, who are HIV-infected. Nonetheless, a non-trivial share of children lives with an HIV-infected adult who is not a parent.
As Richter and colleagues have observed, children and families have been severely neglected in response to the HIV/AIDS epidemic [44]. We suggest that children living in households with HIV-infected adults are distinct from other HIV-affected children, and call for an increase in targeted attention to their needs, at the same time emphasizing that their lives are enriched and enhanced because they share their households with these very same adults. Thus, the challenge and opportunity is to design effective family outreach that both affirms the family and supports healthy child development. We observe that current efforts to develop and monitor the care cascade—which brings heightened attention to the sustained, effective treatment of HIV-infected individuals—brings needed resources that will support the health of HIV-infected individuals and their families.
Indeed, family-based care has been recognized as critical to effective AIDS response, although targeted attention to the population of children living with HIV-infected adults is limited. For example, the PEPFAR blueprint for creating an AIDS-free generation [35] suggested that programmatic activities include family outreach to HIV-infected mothers who have participated in PMTCT programs. This outreach is focused on extending HIV testing and counseling, prevention, and ART services to partners and families; providing mothers with counseling and support related to infant feeding and infant care; and providing links to OVC social services. Similarly, Heymann, Clark, and Brewer [45] have advocated for a “preventing family illness and death” (PFID) approach to protecting families from HIV/AIDS. This approach focuses on prevention of adult infection, treatment of children’s infected parents and caregivers, and orphan care. Deepening outreach to children co-residing with HIV-infected adults in ways that recognize their specific vulnerabilities could enhance ongoing and planned strategies geared toward maintaining wellness in families affected by HIV/AIDS [14, 17]. It would also be consistent with approaches that recognize risk in a social determinants framework, which situates HIV/AIDS vulnerability in family and other social and environmental contexts [46–50].
Fortunately, programs that provide support for vulnerable and AIDS-affected children exist. Further, they can be associated with positive outcomes in children. Many take the form of cash transfers to poor and vulnerable, often AIDS-affected, households, thus targeting a broad group of children and families in need [51–53]. Given the growing care deficit, and the physical and mental health challenges that may beset children in high HIV prevalence areas, such interventions are increasingly evaluated for their effects on children’s physical and mental health. A recent prospective study in Kenya suggested that orphans and vulnerable adolescents in cash transfer households reported better psychological health than those in non-cash transfer households [53]. New interventions are also experimenting with supplementing cash transfers with other forms of support. A randomized control trial in South Africa suggests that “cash plus care” interventions, and specifically the receipt of both economic and psychosocial support, can be associated with reduced HIV-risk behaviors among adolescents [54]. In Botswana, local support programs include caregiving support for HIV-affected families, and the need for such care has garnered significant attention and interest in expanding quality programming [55]. Together, these efforts, spread across numerous settings, suggest an increase in targeted interventions is likely, although the financial and logistical challenges to such programs are many [55].
We acknowledge several key limitations of this study. First, the estimates we present include only countries with available DHS data on HIV testing and parental survival. Some countries with high HIV prevalence (such as South Africa) or well-known HIV/AIDS programs (such as Uganda) are thus not included. Second, our estimates are biased downward because the DHS limits testing to adults of reproductive age in most countries, excluding adults over the age of 50, some of whom are likely to be infected [43]. Substantial levels of non-response among adults eligible for testing render our results among households with adults tested still more conservative, for reasons explained above. In addition, in using cross-sectional data, we present a snapshot at one point in time. If appropriate cross-national data existed to allow us to estimate the percentage of children who ever lived in a household with an HIV-infected adult before age 18, it is likely that many more children would be affected. Finally, we do not know whether the adults know their status or are ill as a result of HIV infection. The implications for children will depend on adults knowing their status and accessing recommended treatment.
Notably, we call for attention to the population of children co-residing with HIV-infected adults in sub-Saharan Africa at the same time others urge programs to move away from a focus on orphans and AIDS-affected children and towards a more general emphasis on vulnerable children [56]. We propose that these two suggestions need not be at odds, and both should be pursued. All vulnerable children, including all children living in poverty, should be targeted in efforts to promote child well-being. However, children living with adults who are HIV-infected may have distinct vulnerabilities. Not only may they be at increased risk of direct exposure to opportunistic infections, but they may well experience a cascade of challenges associated with HIV, including stigma and disrupted social networks, diversion of resources and attention, and increases in poverty, all of which may influence their mental and physical health [26, 44, 57–59]. Notably, this cascade is characterized by overlaps which can intensify the challenges. For example, increased exposure to infection is a specific vulnerability that may be exacerbated by poverty, or a disruption in social networks, or limited child care that results from competing household demands [57, 60]. Further, community context can amplify these challenges; children living in households with HIV-infected adults may be particularly vulnerable to the growing care deficit in high prevalence settings or they may live in communities where AIDS is highly stigmatized [61].
In closing, more relevant to the suggestion that HIV-exposed children receive targeted intervention is the practical challenge of identifying such children. Family outreach upon the birth of a child, during testing and counseling, or during treatment, may offer opportunity in this regard. However, in settings with the highest HIV prevalence, where up to one-third of children live in households with HIV-infected adults, in the absence of individual identification and intervention, targeted public health messages promoting children’s health in areas of a generalized HIV epidemic would be of potential benefit to all children and families.
Acknowledgments
We thank Ying Liu and Sabah Gulamali for their contributions to the data analysis and Meredith Pustell for research assistance.
Data Availability
Data are available from the Demographic and Health Survey Program at http://www.dhsprogram.com/data after completing a registration process. Access to HIV testing data requires an online acknowledgment of the conditions of use. Our analysis makes use of the household, household member, and HIV test results recode files for the following surveys (available at http://www.dhsprogram.com/data/available-datasets.cfm): Burkina Faso 2010 Standard DHS, Burundi 2010 Standard DHS, Cameroon 2011 Standard DHS, Cote D'Ivoire 2005 Standard AIS, DRC 2007 Standard DHS, Ethiopia 2011 Standard DHS, Ghana 2003 Standard DHS, Guinea 2005 Standard DHS, Kenya 2008-09 Standard DHS, Lesotho 2009 Standard DHS, Liberia 2007 Standard DHS, Malawi 2010 Standard DHS, Mali 2006 Standard DHS, Mozambique2009 Standard AIS, Niger 2006 Standard DHS, Rwanda 2010 Standard DHS, Sao Tome and Principe 2008-09 Standard DHS, Senegal 2010-11 Standard DHS, Sierra Leone 2008 Standard DHS, Swaziland 2006-07 Standard DHS, Tanzania 2007-08 Standard AIS, Zambia 2007 Standard DHS, and Zimbabwe 2010-11 Standard DHS.
Funding Statement
This work was funded by Eunice Kennedy Shriver National Institute of Child Health and Human Development [URL: http://www.nichd.nih.gov/]; HD050469 SES, 1F32HD078053-01 REG, 5R24HD041020 SES, 5T32HD007338 REG, R24-HD047879 REG. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.UNICEF. The State of the World’s Children 2015: Reimagine the Future: Innovation for every child. November 2014. Available: http://www.unicef.org/publications/index_77928.html.
- 2.United Nations. The Millennium Development Goals Report. 2014. Available: http://www.un.org/millenniumgoals/2014%20MDG%20report/MDG%202014%20English%20web.pdf.
- 3.UNAIDS. Fact Sheet 2014. Available: http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/factsheet/2014/20140716_FactSheet_en.pdf.
- 4.Towards an AIDS-Free Generation: Children and AIDS: Sixth Stocktaking Report, 2013. November 2013. Available: http://www.unicef.org/publications/files/Children_and_AIDS_Sixth_Stocktaking_Report_EN.pdf.
- 5. Pufall EL, Nyamukapa C, Eaton JW, Mutsindiri R, Chawira G, Munyati S, et al. HIV in Children in a General Population Sample in East Zimbabwe: Prevalence, Causes and Effects. PLOS ONE. 2014;9(11):e113415 10.1371/journal.pone.0113415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beegle K, De Weerdt J, Dercon S: Orphanhood and Human Capital Destruction. Is There Persistence Into Adulthood? Demography. 2010;47(1): 163–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Birdthistle I, Floyd S, Machingura A, Mudziwapasi N, Gregson S, Glynn J. From Affected to Infected? Orphanhood and HIV Risk Among Female Adolescents in Urban Zimbabwe. AIDS. 2008;22(6): 759–766. 10.1097/QAD.0b013e3282f4cac7 [DOI] [PubMed] [Google Scholar]
- 8. Case A, Ardington C. The Impact of Parental Death on School Outcomes: Longitudinal Evidence From South Africa. Demography. 2006;43(3): 401–420. [DOI] [PubMed] [Google Scholar]
- 9. Case A, Paxson C, Ableidinger J. Orphans in Africa: Parental Death, Poverty, and School Enrollment. Demography. 2004;41(3): 483–508. [DOI] [PubMed] [Google Scholar]
- 10. Evans DK, Miguel E. Orphans and Schooling in Africa: A Longitudinal Analysis. Demography. 2007;44(1): 35–57. [DOI] [PubMed] [Google Scholar]
- 11. Miller CM, Gruskin S, Subramanian S, Heymann JS. Emerging Health Disparities in Botswana: Examining the Situation of Orphans During the AIDS Epidemic. Social Science & Medicine. 2007;64(12): 2476–2486. [DOI] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. Morbidity and Mortality Weekly Report. 2009;58(RR-4): 1–198. [PubMed] [Google Scholar]
- 13.World Health Organization. No More Crying. No More Dying. Towards Zero TB Deaths in Children. 2012. Available: http://www.who.int/tb/ChildhoodTB_report_singles.pdf.
- 14. Cluver L, Orkin M, Moshabela M, Kuo C, Boyes M. The Hidden Harm of Home-Based Care: Pulmonary Tuberculosis Symptoms Among Children Providing Home Medical Care to HIV/AIDS-Affected Adults in South Africa. AIDS Care. 2013;25(6): 748–755. 10.1080/09540121.2013.772281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Foster G. Children Who Live in Communities Affected by AIDS. Lancet. 2006;367(9511): 700–701. [DOI] [PubMed] [Google Scholar]
- 16. Gray GE, van Niekerk R, Struthers H, Violari A, Martinson N, McIntyre J, et al. The Effects of Adult Morbidity and Mortality on Household Welfare and the Well-being of Children in Soweto. Vulnerable Children and Youth Studies. 2006;1(1): 15–28. [Google Scholar]
- 17. Kidman R, Hanley JA, Subramanian S, Foster G, Heymann JS. AIDS in the family and community: The impact on child health in Malawi. Social science & medicine. 2010;71(5): 966–974. [DOI] [PubMed] [Google Scholar]
- 18. Bauman LJ, Foster G, Johnson Silver E, Berman R, Gamble I, Muchaneta L. Children caring for their ill parents with HIV/AIDS. Vulnerable Children and Youth Studies. 2006;1(1): 56–70. [Google Scholar]
- 19. Goldberg RE, Short SE. “The Luggage that isn’t Theirs is Too Heavy…”: Understandings of Orphan Disadvantage in Lesotho. Population research and policy review. 2012;31(1): 67–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cluver LD, Gardner F, Operario D. Effects of stigma on the mental health of adolescents orphaned by AIDS. Journal of Adolescent Health. 2008;42(4): 410–417. 10.1016/j.jadohealth.2007.09.022 [DOI] [PubMed] [Google Scholar]
- 21. Floyd S, Crampin AC, Glynn J, Madise N, Mwenebabu M, Mnkhondia S, et al. The Social and Economic Impact of Parental HIV on Children in Northern Malawi: Retrospective Population-Based Cohort Study. AIDS Care. 2007;19(6): 781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mishra V, Arnold F, Otieno F, Cross A, Hong R. Educational and Nutritional Status of Orphans and Children of HIV-Infected Parents in Kenya. AIDS Education and Prevention. 2007;19(5): 383–395. [DOI] [PubMed] [Google Scholar]
- 23. Magadi MA. Household and Community HIV/AIDS Status and Child Malnutrition in sub-Saharan Africa: Evidence From the Demographic and Health Surveys. Social Science & Medicine. 2011;73(3): 436–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nakiyingi JS, Bracher M, Whitworth JAG, Ruberantwari A, Busingye J, Mbulaiteye SM, et al. Child Survival in Relation to Mothers HIV Infection and Survival: Evidence From a Ugandan Cohort Study. AIDS. 2003;17(12): 1827–1834. [DOI] [PubMed] [Google Scholar]
- 25. Zaba B, Whitworth J, Marston M, Nakiyingi JS, Ruberantwari A, Urassa M, et al. HIV and Mortality of Mothers and Children: Evidence from Cohort Studies in Uganda, Tanzania, and Malawi. Epidemiology. 2005;16(3): 275–280. [DOI] [PubMed] [Google Scholar]
- 26. Cluver L, Gardner F. Risk and protective factors for psychological well-being of children orphaned by AIDS in Cape Town: a qualitative study of children and caregivers’ perspectives. AIDS Care. 2007;19(3): 318–325. [DOI] [PubMed] [Google Scholar]
- 27.UNICEF. Children and AIDS: Fifth Stocktaking Report, 2010. November 2010. Available: http://www.unicef.org/publications/files/Children_and_AIDS-Fifth_Stocktaking_Report_2010_EN.pdf.
- 28. Mishra V, Bignami-Van Assche S. Orphans and vulnerable children in high HIV-prevalence countries in sub-Saharan Africa: DHS Analytical Studies 15. Calverton, Maryland,USA: Macro International Inc.; 2008. [Google Scholar]
- 29. Grant MJ, Yeatman S. The relationship between orphanhood and child fostering in sub-Saharan Africa, 1990s–2000s. Population Studies. 2012;66(3): 279–295. 10.1080/00324728.2012.681682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lloyd CB, Blanc AK. Children's Schooling in Sub-Saharan Africa: The Role of Fathers, Mothers, and Others. Population and Development Review. 1996;22: 265–298. [Google Scholar]
- 31. Lloyd CB, Desai S. Children's living arrangements in developing countries. Population Research and Policy Review. 1992;11(3): 193–216. [Google Scholar]
- 32. Madhavan S. Fosterage patterns in the age of AIDS: continuity and change. Social Science and Medicine. 2004;58(7): 1443–1454. [DOI] [PubMed] [Google Scholar]
- 33. Parker EM, Short SE. Grandmother Coresidence, Maternal Orphans, and School Enrollment in Sub-Saharan Africa. J Fam Issues. 2009;30(6): 813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Goldberg RE. Family instability and early initiation of sexual activity in Western Kenya. Demography. 2013;50(2): 725–750. 10.1007/s13524-012-0150-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.PEPFAR. PEPFAR Blueprint: Creating an AIDS-free Generation. PEPFAR. 2012. Available: http://www.pepfar.gov/documents/organization/201386.pdf.
- 36.UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2012. 2012. Available: http://www.unaids.org/sites/default/files/media_asset/20121120_UNAIDS_Global_Report_2012_with_annexes_en_1.pdf.
- 37.UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2013. 2013. Available: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf.
- 38.UNAIDS. 2013 Global Fact Sheet. 2013. Available: http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/20130923_FactSheet_Global_en.pdf.
- 39. Bongaarts J, Buettner T, Heilig G, Pelletier F. Has the HIV Epidemic Peaked? Population and Development Review. 2008;34(2): 199–224. [Google Scholar]
- 40. Mishra V, Vaessen M, Ties Boerma J, Arnold F, Way A, Cross A, et al. HIV Testing in National Population-Based Surveys: Experience from the Demographic and Health Surveys. Bulletin of the World Health Organization. 2006;84(7): 537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Clark SJ, Houle B. Validation, Replication, and Sensitivity Testing of Heckman-Type Selection Models to Adjust Estimates of HIV Prevalence. PLOS ONE. 2014;9(11): e112563 10.1371/journal.pone.0112563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Staveteig S, Wang S, Head S, Bradley S, Nybro E. Demographic Patterns of HIV Testing Uptake in Sub-Saharan Africa: DHS Comparative Reports 30. Calverton, Maryland, USA: ICF International; 2013. [Google Scholar]
- 43. Gómez-Olivé FX, Angotti N, Houle B, Klipstein-Grobusch K, Kabudula C, Menken J, et al. Prevalence of HIV among those 15 and older in rural South Africa. AIDS Care. 2013;25(9): 1122–1128. 10.1080/09540121.2012.750710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Richter LM, Sherr L, Adato M, Belsey M, Chandan U, Desmond C, et al. Strengthening families to support children affected by HIV and AIDS. AIDS Care. 2009;21(S1): 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Heymann JS, Clark S, Brewer TF. Moving from Preventing HIV/AIDS in Its Infancy to Preventing Family Illness and Death (PFID). International Journal of Infectious Diseases. 2008;12(2): 117–119. [DOI] [PubMed] [Google Scholar]
- 46. Harrison A, Short SE, Tuoane-Nkhasi M. Re-focusing the Gender Lens: Caregiving Women, Family Roles and HIV/AIDS Vulnerability in Lesotho. AIDS and Behavior. 2014;18(3): 595–604. 10.1007/s10461-013-0515-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Anglewicz P. Migration, marital change, and HIV infection in Malawi. Demography. 2012;49(1): 239–265. 10.1007/s13524-011-0072-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yeatman S. HIV infection and fertility preferences in rural Malawi. Stud Fam Plann. 2009;40(4): 261–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mojola SA. Fishing in dangerous waters: Ecology, gender and economy in HIV risk. Soc Sci Med. 2011;72(2): 149–156. 10.1016/j.socscimed.2010.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Short SE, Mollborn S. Social Determinants and Health Behaviors: Conceptual Frames and Empirical Advances. Current Opinion in Psychology. 2015;5: 78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Davis B, Gaarder M, Handa S, Yablonski J. Evaluating the impact of cash transfer programmes in sub-Saharan Africa: an introduction to the special issue. Journal of development effectiveness. 2012;4(1): 1–8. [Google Scholar]
- 52. Filipski MJ, Taylor JE, Thome KE, Davis B. Effects of treatment beyond the treated: a general equilibrium impact evaluation of Lesotho's cash grants program. Agricultural Economics. 2015;46(2): 227–243. [Google Scholar]
- 53.Shangani S, Operario D, Genberg B, Kirwa K, Midoun M, Hu L, et al. Cash transfers and psychological well-being among orphaned and vulnerable adolescents: A longitudinal study in western Kenya. 2015. Available: https://apha.confex.com/apha/143am/webprogram/Paper331976.html.
- 54. Cluver LD, Orkin FM, Boyes ME, Sherr L. Cash plus care: social protection cumulatively mitigates HIV-risk behaviour among adolescents in South Africa. AIDS. 2014;28: S389–S397. 10.1097/QAD.0000000000000340 [DOI] [PubMed] [Google Scholar]
- 55. Feranil I, Herstad B, Jallow W, Mbuya-Brown R. Assessing implementation of Botswana's program for orphans and vulnerable children. Washington D.C.: Futures Group, Health Policy Initiative, Task Order I; 2010. [Google Scholar]
- 56. Akwara P, Noubary B, Lim Ah Ken P, Johnson K, Yates R, Winfrey W, et al. Who is the Vulnerable Child? Using Survey Data to Identify Children at Risk in the Era of HIV and AIDS. AIDS Care. 2010;22(9): 1066–1085. 10.1080/09540121.2010.498878 [DOI] [PubMed] [Google Scholar]
- 57. Cluver L, Orkin M. Cumulative risk and AIDS-orphanhood: Interactions of stigma, bullying and poverty on child mental health in South Africa. Soc Sci Med. 2009;69(8): 1186–1193. 10.1016/j.socscimed.2009.07.033 [DOI] [PubMed] [Google Scholar]
- 58. Cluver L, Gardner F, Operario D. Poverty and psychological health among AIDS-orphaned children in Cape Town, South Africa. AIDS Care. 2009;21(6): 732–741. 10.1080/09540120802511885 [DOI] [PubMed] [Google Scholar]
- 59.Parker, EM, Short, SE, Goldberg, RE, Hlabana, T. Growing Up in the Context of High HIV Prevalence: Adult Death and Illness, Family Living Arrangements, and Children's Lives. Paper presented at the Union of African Population Studies (UAPS) Fifth African Population Conference: Arusha, Tanzania. 2007.
- 60. Schatz E, Madhavan S, Williams J. Female-headed households contending with AIDS-related hardship in rural South Africa. Health Place. 2011;17(2): 598–605. 10.1016/j.healthplace.2010.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Schatz E, Seeley J. Gender, ageing and carework in East and Southern Africa: A review. Global Public Health. 2015; 1–16. Available: http://www.tandfonline.com/doi/full/10.1080/17441692.2015.1035664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the Demographic and Health Survey Program at http://www.dhsprogram.com/data after completing a registration process. Access to HIV testing data requires an online acknowledgment of the conditions of use. Our analysis makes use of the household, household member, and HIV test results recode files for the following surveys (available at http://www.dhsprogram.com/data/available-datasets.cfm): Burkina Faso 2010 Standard DHS, Burundi 2010 Standard DHS, Cameroon 2011 Standard DHS, Cote D'Ivoire 2005 Standard AIS, DRC 2007 Standard DHS, Ethiopia 2011 Standard DHS, Ghana 2003 Standard DHS, Guinea 2005 Standard DHS, Kenya 2008-09 Standard DHS, Lesotho 2009 Standard DHS, Liberia 2007 Standard DHS, Malawi 2010 Standard DHS, Mali 2006 Standard DHS, Mozambique2009 Standard AIS, Niger 2006 Standard DHS, Rwanda 2010 Standard DHS, Sao Tome and Principe 2008-09 Standard DHS, Senegal 2010-11 Standard DHS, Sierra Leone 2008 Standard DHS, Swaziland 2006-07 Standard DHS, Tanzania 2007-08 Standard AIS, Zambia 2007 Standard DHS, and Zimbabwe 2010-11 Standard DHS.