Clinicians make many patient care decisions each day. The cumulative cognitive demand of these decisions may erode clinicians’ abilities to resist making potentially inappropriate choices. Psychologists, who refer to the erosion of self-control after making repeated decisions as decision fatigue,1,2 have found evidence that it affects nonmedical professionals. For example, as court sessions wear on, judges are more likely to deny parole, the “easier” or “safer” option.3
In primary care, prescribing unnecessary antibiotics for acute respiratory infections (ARIs) is a common, in appropriate service. Clinicians may prescribe unnecessary antibiotics—again, the easy, safe option—due to perceived or explicit patient demand, a desire to do something meaningful for patients, a desire to conclude visits quickly, or an unrealistic fear of complications.4,5 We hypothesized that decision fatigue, if present, would increase clinicians’ likelihood of prescribing antibiotics for patients presenting with ARIs as clinic sessions wore on.
Methods
The protocol for this study was approved by the Partners HealthCare Human Research Committee, including a waiver of patient informed consent. We merged billing and electronic health record data for patient visits to 1 of 23 Partners HealthCare–affiliated primary care practices between May 1, 2011, and September 30, 2012. We identified visit diagnoses using billing codes, and, using electronic health record data, identified visit times, antibiotic prescriptions, and chronic illnesses.6
We analyzed ARI visits by adults (aged 18–64 years), which occurred during two 4-hour sessions—8 AM to noon and 1 PM to 5 PM—Monday through Friday. We excluded visits by patients with chronic illnesses (eg, cancer, diabetes mellitus) or concomitant acute diagnoses (eg, skin infections) for which antibiotics would be indicated. We excluded clinicians who had fewer than 40 ARI visits during the study. Consistent with national guidelines, we classified specific ARI diagnoses as antibiotics sometimes indicated or antibiotics never indicated (Table).6
Table.
Sample Characteristics and Antibiotic Prescribinga
| Characteristic | Overall Sample (N = 21 867) | Antibiotic | P Value | |
|---|---|---|---|---|
| Prescribed (9722 [44%]) | Not Prescribed (12 145 [56%]) | |||
| Patient age, mean (SD), y | 40.4 (12.0) | 40.9 (11.9) | 40.0 (12.1) | <.001 |
| Median annual household income by zip code, mean (SD), $ | 76 481 (28 522) | 78 134 (29 009) | 75 158 (28 057) | <.001 |
| Patient sex, No. (%) | ||||
| Men | 7111 (33) | 3115 (32) | 3996 (33) | .18 |
| Women | 14 756 (67) | 6607 (68) | 8149 (67) | |
| Patient race/ethnicity | ||||
| White | 15 958 (73) | 7327 (75) | 8631 (71) | <.001 |
| Latino | 2276 (10) | 983 (10) | 1293 (11) | |
| Black | 1296 (6) | 498 (5) | 798 (7) | |
| Asian | 1041 (5) | 365 (4) | 676 (6) | |
| Other/unknown | 1296 (6) | 549 (6) | 747 (6) | |
| Language | ||||
| English | 20 042 (92) | 8969 (92) | 11 073 (91) | .003 |
| Spanish | 1196 (5) | 512 (5) | 684 (6) | |
| Other | 629 (3) | 241 (2) | 388 (3) | |
| Insurance | ||||
| Private | 18 762 (86) | 8367 (86) | 10 395 (86) | .15 |
| Medicaid | 2003 (9) | 856 (9) | 1147 (9) | |
| Medicare | 474 (2) | 202 (2) | 272 (2) | |
| None or other | 628 (3) | 297 (3) | 331 (3) | |
| Clinician type | ||||
| Staff physician | 17 206 (79) | 7221 (74) | 9985 (82) | <.001 |
| Nurse practitioner or physician assistant | 4196 (19) | 2320 (24) | 1876 (15) | |
| Fellow (physician trainee) | 465 (2) | 181 (2) | 284 (2) | |
| Clinician is the primary care clinician | ||||
| Yes | 4938 (23) | 2180 (22) | 2758 (23) | <.001 |
| No | 5708 (26) | 2909 (30) | 2799 (23) | |
| Unknown | 11 221 (51) | 4633 (48) | 6588 (54) | |
| Diagnosis typeb | ||||
| Antibiotics sometimes indicated | 7544 (35) | 5301 (55) | 2243 (18) | <.001 |
| Antibiotics never indicated | 14 323 (65) | 4421 (45) | 9902 (82) | |
Percentages may not sum to 100 owing to rounding.
Diagnoses for which antibiotics are sometimes indicated were otitis media (International Classification of Diseases, Ninth Revision [ICD-9] 381 and 382), sinusitis (ICD-9 461 and 473), pneumonia (ICD-9 481–486), and streptococcal pharyngitis (ICD-9 034.0). Diagnoses for which antibiotics are never indicated were nonspecific upper respiratory infection (ICD-9 460, 464, and 465), acute bronchitis (ICD-9 466 and 490), influenza (ICD-9 487), and nonstreptococcal pharyngitis (ICD-9 462 and 463).
Clinicians worked in 4-hour morning and afternoon sessions; many clinicians worked only 1 session on a given day. We used the scheduled hour of each ARI visit (1 through 4) to represent visit time.
Using logistic regression, we estimated the probability of antibiotic prescribing for ARI visits as a function of session hour, number of visits per session, calendar month of visit, patient-level confounders (Table), and fixed effects for clinicians. We used generalized estimating equations to account for clinician-level clustering. We used SAS (version 9.3, SAS Institute) and considered P < .05 statistically significant.
Results
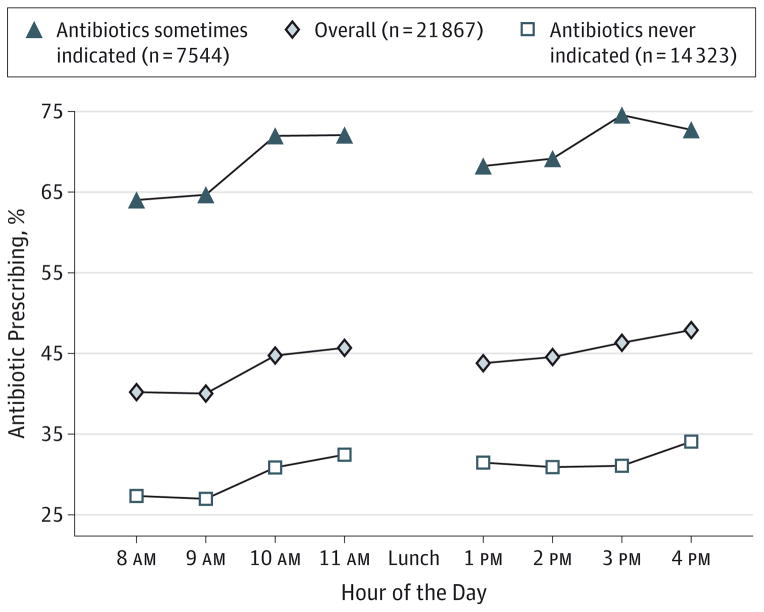
There were 21 867 ARI visits to 204 clinicians in 23 practices that met our inclusion criteria; 44% resulted in antibiotic prescriptions (Table). Antibiotic prescribing increased throughout the morning and afternoon clinic sessions for antibiotics sometimes indicated and antibiotics never indicated ARIs (Figure). Relative to the first hour of a session, the adjusted odds ratios of antibiotic prescribing in the second, third, and fourth hours were 1.01 (95% CI, 0.91–1.13), 1.14 (95% CI, 1.02–1.27), and 1.26 (95% CI, 1.13–1.41), respectively (P < .001 for linear trend).
Figure. Antibiotic Prescribing by Hour of the Day.
Diagnoses for which antibiotics are sometimes indicated were otitis media, sinusitis, pneumonia, and streptococcal pharyngitis. Diagnoses for which antibiotics are never indicated were acute bronchitis, nonspecific upper respiratory infection, influenza, and nonstreptococcal pharyngitis. Linear trend in session hours (combining 8 AM with 1 PM, 9 AM with 2 PM, 10 AM with 3 PM, and 11 AM with 4 PM): P < .001 for antibiotics sometimes indicated; P < .001 for all acute respiratory infection visits; and P < .002 for antibiotics never indicated. During clinic sessions, the proportion of acute respiratory infection visits for which antibiotics were sometimes indicated did not vary significantly from hour to hour (P = .64).
Discussion
We found that primary care clinicians’ likelihood of prescribing antibiotics for ARIs increased during clinic sessions, consistent with the hypothesis that decision fatigue progressively impairs clinicians’ ability to resist ordering inappropriate treatments.
This finding should be interpreted in the context of the study design: we studied ARI visits in a single health care system, scheduled time was a proxy for actual visit time, and unmeasured confounding is possible. In addition, we used visit time as a proxy for decision fatigue, but other accumulating factors (eg, glucose depletion or general fatigue) could contribute to our findings.
Remedies for decision fatigue might include time-dependent decision support, modified schedules, shorter sessions, mandatory breaks, or snacks.3 Further studies could clarify the sources of the problem and test corresponding solutions.
Acknowledgments
Funding/Support: This work was supported by grant RC4 AG039115 from the National Institutes of Health/National Institute on Aging.
Footnotes
Conflict of Interest Disclosures: None reported.
Previous Presentations: This study was presented in part at AcademyHealth; June 24, 2013; Baltimore, Maryland; and at IDWeek; October 4, 2013; San Francisco, California.
Additional Contributions: Dwan Pineros, BA, Geisel School of Medicine at Dartmouth, provided assistance with the data analysis. He did not receive financial compensation.
Author Contributions: Dr Linder had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Linder, Doctor, Friedberg, Meeker, Fox.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Linder, Fox.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Linder, Friedberg, Reyes Nieva, Birks.
Obtained funding: Linder, Doctor, Meeker, Fox.
Administrative, technical, or material support: Linder, Doctor, Reyes Nieva.
Study supervision: Linder, Reyes Nieva.
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Vohs KD, Baumeister RF, Schmeichel BJ, Twenge JM, Nelson NM, Tice DM. Making choices impairs subsequent self-control: a limited-resource account of decision making, self-regulation, and active initiative. J Pers Soc Psychol. 2008;94(5):883–898. doi: 10.1037/0022-3514.94.5.883. [DOI] [PubMed] [Google Scholar]
- 2.Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychol Bull. 2000;126(2):247–259. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- 3.Danziger S, Levav J, Avnaim-Pesso L. Extraneous factors in judicial decisions. Proc Natl Acad Sci U S A. 2011;108(17):6889–6892. doi: 10.1073/pnas.1018033108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teixeira Rodrigues A, Roque F, Falcão A, Figueiras A, Herdeiro MT. Understanding physician antibiotic prescribing behaviour: a systematic review of qualitative studies. Int J Antimicrob Agents. 2013;41(3):203–212. doi: 10.1016/j.ijantimicag.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Tonkin-Crine S, Yardley L, Little P. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother. 2011;66(10):2215–2223. doi: 10.1093/jac/dkr279. [DOI] [PubMed] [Google Scholar]
- 6.Persell SD, Friedberg MW, Meeker D, et al. Use of behavioral economics and social psychology to improve treatment of acute respiratory infections (BEARI): rationale and design of a cluster randomized controlled trial [1RC4AG039115-01]—study protocol and baseline practice and provider characteristics. BMC Infect Dis. 2013;13:290. doi: 10.1186/1471-2334-13-290. [DOI] [PMC free article] [PubMed] [Google Scholar]