Abstract
Hypertension is a common chronic condition, but the burden of emergency department visits due to hypertension and associated patient and hospital characteristics are not well described. The goals of this study were to 1) establish the burden of hypertension-related emergency department visits, estimated by the total number, proportion of adult visits, and population-based rate, 2) evaluate for change over time, and 3) identify associated patient and hospital characteristics. The Nationwide Emergency Department Sample from 2006 to 2012 was used to identify hypertension-related emergency department visits (ICD-9 CM codes 401 through 405, inclusive, and 437.2), and this was linked to US Census Bureau July population estimates to determine population-based rates for each study year. Negative binomial regression was performed to determine whether rates of hypertension-related emergency department visits changed over time. A total of 165,946,807 hypertension-related emergency department visits occurred during the seven-year study period (23.6% of all adult ED visits), and hypertension was the primary diagnosis for 6,399,088 (0.9% of all adult ED visits). The estimated yearly incidence rate rose 5.2% per year (incident rate ratio 1.052, 95% confidence interval 1.044 to 1.061, p<0.001) for hypertension-related visits, and 4.4% per year (incidence rate ratio 1.044, 95% confidence interval 1.038 to 1.051, p<0.001) for ED visits with a primary diagnosis of hypertension. Over the same time, the proportion hospitalized declined and the proportion of visits rose at safety net hospitals and among uninsured patients. In conclusion, these data indicate that hypertension-related ED visits are common and rising.
Keywords: hypertension, emergency care, safety-net hospital
Background
Hypertension is a common and costly disease that increases the risk of heart attack, stroke, heart failure, renal failure, and death.1,2 Uncontrolled hypertension for even a few weeks is associated with increased risk of acute cardiovascular events and death.3 From 2000 to 2011, hospitalizations for hypertension rose more than 27%,4 and from 2003 to 2006 the cost of hypertension-associated hospitalizations was $113 billion, or 15% of all hospital costs.5 In the United States (US), there are an estimated 136.3 million emergency department (ED) visits annually, or 44.5 per 100 persons.6 Increasingly, Americans seek ED care for chronic conditions or acute manifestations of chronic disease.7 Elevated blood pressure is common during ED visits,8 and total hospitalizations for hypertension have risen over time.9 Chronic conditions such as hypertension that have traditionally been managed in primary care clinics are being evaluated and treated with greater frequency in the ED.10 Using a national administrative database, the goals of this study were to: 1) establish the burden of hypertension-related emergency department visits, estimated by the total number, proportion of adult visits, and population-based rate, 2) evaluate for change over time, and 3) identify associated patient and hospital characteristics.
Methods
We conducted a descriptive epidemiological analysis of hypertension-related ED visits from 2006 to 2012 using the Nationwide Emergency Department Sample (NEDS). NEDS is a publicly available database from the Healthcare Cost and Utilization Project (HCUP) maintained by the Agency for Healthcare Research and Quality (AHRQ) and is the largest source of US ED administrative data.11 NEDS is designed to be representative of all ED visits and is constructed from the HCUP State Emergency Department Databases and the State Inpatient Databases. In 2012, 30 states and 950 hospitals contributed data for 31 million ED visits, for an approximate 20% stratified sample of US hospital-based EDs. For each ED visit, there are up to 15 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM) codes, as well as more than 50 other patient, visit, hospital, and region-level variables. For hospitals included in NEDS, all ED visits from each institution are included. Weighting is required to calculate national estimates. Estimates of ED utilization using NEDS are similar to other national datasets, such as the National Hospital Ambulatory Medical Care Survey.11,12 This study was approved after IRB review.
We included adult (age ≥18 years) ED visits from 2006 to the end of 2012. Hypertension was identified by the following ICD-9 CM codes: 401–405 (inclusive) and 437.2.13,14 This combination of ICD-9 CM codes has been shown to have specificity of 0.95 and positive predictive value of 0.97 for identifying visits truly related to hypertension.13 Hypertension-related ED visits were defined as ED visits with any diagnosis code of hypertension. ED visits with a primary diagnosis of hypertension were defined ED visits in which hypertension was the first diagnosis code.
Comorbid conditions were identified using ICD-9 CM codes, where an asterisks indicates inclusion of sub-codes15,16: hypertension (401.1, 401.9, 405.1*, 405.9*), diabetes (250.00, 250.01, 250.02, 250.03), coronary artery disease (412, 414.00, 414.01, 414.02, 414.03, 414.04, 414.05, 414.06, 414.07, 414.8, 414.9), chronic kidney disease (575*), heart failure (428*), chronic obstructive pulmonary disease (491*, 492*, 496*), and cerebrovascular disease (430, 431, 432.0, 432.9, 434.01, 434.11, 434.91, 435.9). ED visits without hospitalization were considered outpatient ED visits.
ED visits for uninsured patients were those classified as self-pay. Safety net hospitals were defined as: 1) >30% of ED visits for patients insured by Medicaid; 2) >30% of visits for patients without insurance; or 3) combined Medicaid and uninsured pool >40%.17
Analyses were conducted in accordance with AHRQ recommendations, including weighting and stratification; all reported values are weighted. Using US Census Bureau July population estimates,18 incidence rates (annual and monthly) were calculated separately for hypertension-related ED visits and ED visits with a primary diagnosis of hypertension for each study year. Patient and hospital level characteristics were computed for each year of the study and for the entire study period of 7 years. Two negative binomial regression models were used to estimate the annual change in incidence rates for: 1) hypertension-related ED visits, and 2) ED visits with a primary diagnosis of hypertension.
In exploratory analyses, annual incidence rates of hypertension-related ED visits were stratified by age (<45, 45–64, 65–79, ≥80 years of age) and geographic region (Northeast, South, Midwest, West, defined according to US census boundaries19). Given seasonal variation in blood pressure,20 monthly incidence rates were computed. To better understand conditions associated with ED visits for hypertension, the most common co-occurring diagnoses were determined for ED visits with a primary and, separately, secondary diagnosis of hypertension. Analyses were conducted using survey packages in SAS 9.4 (SAS Institute, Cary, NC) and Stata 14 IC (STATA Corp, College Station, TX).
Results
During the seven-year study period from 2006 to 2012, there were 701,952,422 adult ED visits. Of these, 165,946,807 were hypertension-related ED visits (23.6% of all adult ED visits), and 6,399,085 were ED visits with a primary diagnosis of hypertension (0.9% of all adult ED visits). The rate of hypertension-related ED visits was 101.4 per 1,000 adults per year (Table 1); the rate of ED visits with a primary diagnosis of hypertension was 3.9 per 1,000 adults per year (Table 2).
Table 1.
Hypertension-Related Emergency Department Visits (weighted), 2006–2012
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2006–2012 | |
|---|---|---|---|---|---|---|---|---|
| Number of Hypertension-Related ED visits | 19,160,992 | 20,513,627 | 22,437,862 | 23,981,420 | 25,720,355 | 26,785,981 | 27,346,570 | 165,946,807 |
| Proportion of Adult ED Visits | 20.5% | 21.5% | 22.8% | 23.9% | 24.9% | 25.8% | 25.7% | 23.6% |
| Rate (per 1,000 Adult Population per Year) | 84.8 | 89.7 | 97.0 | 102.5 | 108.8 | 112.1 | 113.3 | 101.4 |
| Age (median, Q1, Q3) | 65 (51, 78) | 64 (50, 78) | 64 (50, 78) | 63 (50, 77) | 63 (50, 77) | 63 (50, 77) | 63 (50, 76) | 63 (50, 77) |
| Female | 57.3% | 57.0% | 56.8% | 56.6% | 56.4% | 56.2% | 55.9% | 56.5% |
| Primary payer | ||||||||
| Medicare | 55.3% | 53.6% | 53.9% | 53.1% | 52.6% | 54.0% | 53.7% | 53.7% |
| Medicaid | 9.5% | 9.9% | 10.2% | 11.1% | 11.8% | 12.2% | 12.7% | 11.2% |
| Private insurance | 24.2% | 24.4% | 24.6% | 23.9% | 22.9% | 21.6% | 20.3% | 23.0% |
| Self-pay | 7.3% | 8.7% | 7.8% | 8.2% | 9.1% | 8.5% | 9.3% | 8.5% |
| No charge or other | 3.8% | 3.4% | 3.5% | 3.8% | 3.6% | 3.7% | 4.1% | 3.7% |
| Location of care | ||||||||
| Safety net hospital | 49.4% | 51.9% | 49.5% | 56.8% | 63.0% | 62.9% | 68.0% | 58.2% |
| Academic medical center | 39.4% | 37.5% | 37.2% | 36.9% | 40.6% | 39.7% | 42.9% | 39.3% |
| Median household income, by patient zip code | ||||||||
| 1st quartile | 31.5 | 33.3 | 31.9 | 31.9 | 32.9 | 32.2 | 33.8 | 32.6 |
| 2nd quartile | 26.4 | 26.4 | 28.7 | 28.6 | 27.4 | 25.4 | 25.3 | 26.8 |
| 3rd quartile | 23.5 | 23.1 | 21.4 | 22.5 | 21.9 | 23.9 | 22.6 | 22.7 |
| 4th quartile | 18.6 | 17.2 | 17.9 | 16.9 | 17.8 | 18.5 | 18.4 | 17.9 |
| ED Disposition | ||||||||
| Discharged Home, From ED | 49.8% | 51.8% | 53.7% | 55.3% | 56.8% | 58.1% | 59.9% | 55.5% |
| Admitted | 46.5% | 45.3% | 44.2% | 42.8% | 40.9% | 39.7% | 37.8% | 42.1% |
| Other* | 3.7% | 3.0% | 2.0% | 2.0% | 2.4% | 2.2% | 2.3% | 2.5% |
| Hospital disposition | ||||||||
| Home | 59.0% | 58.6% | 57.9% | 58.4% | 57.9% | 57.1% | 57.6% | 58.0% |
| Transfer to acute care facility; nursing facility or rehab | 25.2% | 24.9% | 25.1% | 24.8% | 24.6% | 24.9% | 24.3% | 24.8% |
| Home health care | 11.8% | 12.4% | 13.0% | 12.8% | 13.6% | 14.3% | 14.3% | 13.2% |
| Died in hospital | 2.9% | 2.8% | 2.8% | 2.7% | 2.5% | 2.4% | 2.4% | 2.6% |
| Other† | 1.2% | 1.3% | 1.3% | 1.3% | 1.3% | 1.3% | 1.4% | 1.3% |
| Length of stay for Hospitalized Patients, days (median, Q1, Q3) | 3.1 (1.6, 5.6) | 3.0 (1.5, 5.6) | 3.1 (1.6, 5.6) | 3.0 (1.6, 5.5) | 3.0 (1.5, 5.4) | 3.0 (1.5, 5.3) | 2.9 (1.5, 5.3) | 3.0 (1.6, 5.5) |
| Any chronic disease other than chronic hypertension | 52.4 | 53.4 | 54.0 | 53.9 | 53.7 | 54.0 | 53.6 | 53.6 |
| Listed Chronic Conditions | ||||||||
| Diabetes | 25.3% | 26.1% | 26.5% | 26.6% | 27.0% | 27.0% | 27.2% | 26.6% |
| Coronary artery disease | 20.7% | 20.8% | 21.1% | 20.6% | 19.9% | 20.1% | 19.5% | 20.3% |
| Kidney disease | 6.9% | 10.6% | 11.3% | 12.0% | 12.2% | 12.4% | 12.3% | 11.3% |
| Heart failure | 13.3% | 12.6% | 12.5% | 12.4% | 12.1% | 12.2% | 11.8% | 12.3% |
| Chronic obstructive pulmonary disease | 11.5% | 11.4% | 11.7% | 11.6% | 11.4% | 11.8% | 11.6% | 11.6% |
| Cerebrovascular disease or stroke | 3.2% | 3.0% | 2.9% | 2.8% | 2.7% | 2.6% | 2.5% | 2.8% |
| Rate by Region (per 1,000 Adult Population Per Year) | ||||||||
| Northeast | 75.5 | 83.1 | 90.2 | 92.2 | 99.3 | 106.5 | 104.3 | 93.2 |
| Midwest | 88.1 | 93.4 | 95.9 | 104.1 | 115.5 | 116.2 | 120.3 | 104.9 |
| South | 103.4 | 109.5 | 117.9 | 124.9 | 129.2 | 130.9 | 131.9 | 121.4 |
| West | 59.4 | 59.8 | 67.0 | 73.3 | 77.2 | 82.6 | 84.1 | 72.6 |
| Weekend | 27.6% | 27.3% | 27.3% | 27.2% | 27.0% | 27.0% | 27.0% | 27.2% |
Abbreviations: ED, emergency department; Q1, Q3, first quartile, third quartile
Other ED includes: Transfer to another hospital, died in the emergency department, and unknown disposition
Other hospital disposition includes: Against medical advice, discharged alive, destination unknown
Table 2.
Emergency Department Visits with a Primary Diagnosis of Hypertension (weighted), 2006–2012
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2006–2012 | |
|---|---|---|---|---|---|---|---|---|
| Number of Adult ED visits with Primary Diagnosis of Hypertension | 776,240 | 803,118 | 850,128 | 930,484 | 982,566 | 1,004,127 | 1,052,422 | 6,399,088 |
| Proportion of Adult ED Visits | 0.8% | 0.8% | 0.9% | 0.9% | 1.0% | 1.0% | 1.0% | 0.9% |
| Rate (per 1,000 Adult Population per Year) | 3.4 | 3.5 | 3.7 | 4.0 | 4.2 | 4.2 | 4.4 | 3.9 |
| Age (median, Q1, Q3) | 57 (45, 73) | 58 (45, 73) | 57 (46, 72) | 57 (46, 72) | 57 (45, 71) | 58 (46, 72) | 58 (46, 72) | 57 (46, 72) |
| Female (%) | 58.4 | 58.3 | 58.1 | 57.7 | 57.5 | 58.0 | 57.2 | 57.8 |
| Primary payer | ||||||||
| Medicare | 42.8% | 41.2% | 41.3% | 40.5% | 40.6% | 42.8% | 42.9% | 41.7% |
| Medicaid | 10.2% | 10.6% | 10.9% | 11.6% | 12.3% | 13.1% | 13.3% | 11.8% |
| Private insurance | 27.1% | 27.7% | 27.8% | 26.6% | 25.4% | 23.3% | 22.1% | 25.5% |
| Self-pay | 15.4% | 16.7% | 15.7% | 16.5% | 17.3% | 16.4% | 17.1% | 16.5% |
| No charge or other | 4.6% | 3.8% | 4.3% | 4.8% | 4.3% | 4.5% | 4.6% | 4.4% |
| Location of care | ||||||||
| Safety net hospital | 56.3% | 57.1% | 55.6% | 62.8% | 68.5% | 68.1% | 72.8% | 63.7% |
| Academic medical center | 38.9% | 38.8% | 39.4% | 39.7% | 42.7% | 41.9% | 44.7% | 41.1% |
| Median household income, by patient zip code | ||||||||
| 1st quartile | 37.3 | 38.8 | 36.9 | 37.9 | 38.8 | 35.9 | 38.2 | 37.7 |
| 2nd quartile | 26.1 | 25.8 | 27.8 | 28.0 | 26.6 | 24.9 | 25.1 | 26.3 |
| 3rd quartile | 21.1 | 20.5 | 19.6 | 20.1 | 19.6 | 23.3 | 21.5 | 20.9 |
| 4th quartile | 15.6 | 14.9 | 15.7 | 14.0 | 15.0 | 16.0 | 15.3 | 15.2 |
| ED Disposition | ||||||||
| Discharged Home, From ED | 67.2% | 69.5% | 71.5% | 72.2% | 72.8% | 74.0% | 74.9% | 72.0% |
| Admitted | 28.8% | 28.1% | 27.3% | 26.7% | 25.7% | 25.0% | 24.0% | 26.3% |
| Other* | 4.0% | 2.4% | 1.3% | 1.2% | 1.6% | 1.1% | 1.1% | 1.7% |
| Hospital disposition | ||||||||
| Home | 72.7% | 72.5% | 72.5% | 73.3% | 72.7% | 71.5% | 71.2% | 72.3% |
| Transfer to acute care facility; nursing facility or rehab | 13.8% | 13.3% | 13.0% | 12.7% | 12.2% | 12.9% | 12.5% | 12.9% |
| Home health care | 9.9% | 10.4% | 11.1% | 10.7% | 11.7% | 12.5% | 12.7% | 11.3% |
| Died in hospital | 1.5% | 1.3% | 1.2% | 1.0% | 1.1% | 0.9% | 1.0% | 1.1% |
| Other† | 2.2% | 2.5% | 2.3% | 2.3% | 2.4% | 2.2% | 2.5% | 2.3% |
| Length of stay for Hospitalized Patients, days (median, Q1, Q3) | 2.7 (1.3, 5.0) | 2.5 (1.2, 4.8) | 2.6 (1.2, 4.8) | 2.4 (1.2, 4.6) | 2.4 (1.1, 4.4) | 2.3 (1.1, 4.4) | 2.3 (1.1, 4.3) | 2.4 (1.2, 4.6) |
| Any chronic disease other than chronic hypertension | 35.3 | 36.8 | 37.5 | 37.6 | 38.3 | 37.9 | 38.2 | 37.5 |
| Listed Chronic Conditions | ||||||||
| Diabetes | 15.2% | 15.6% | 16.6% | 16.7% | 17.5% | 17.7% | 17.8% | 16.8% |
| Coronary artery disease | 11.5% | 11.6% | 12.0% | 11.8% | 11.6% | 11.9% | 11.8% | 11.8% |
| Kidney disease | 11.5% | 16.0% | 16.2% | 16.5% | 16.8% | 16.0% | 16.7% | 15.8% |
| Heart failure | 13.7% | 12.3% | 12.6% | 12.4% | 12.0% | 11.7% | 11.6% | 12.2% |
| Chronic obstructive pulmonary disease | 5.2% | 5.0% | 4.9% | 4.8% | 4.8% | 5.1% | 5.0% | 5.0% |
| Cerebrovascular disease or stroke | 0.8% | 0.8% | 0.8% | 0.8% | 0.7% | 0.7% | 0.6% | 0.7% |
| Rate by Region (per 1,000 Adult Population Per Year) | ||||||||
| Northeast | 2.8 | 3.0 | 3.4 | 3.5 | 3.9 | 4.1 | 3.9 | 3.52 |
| Midwest | 3.1 | 3.2 | 3.2 | 3.7 | 4.1 | 4.0 | 4.3 | 3.66 |
| South | 4.5 | 4.6 | 4.8 | 5.2 | 5.2 | 5.2 | 5.5 | 5.00 |
| West | 2.5 | 2.5 | 2.6 | 2.6 | 2.8 | 3.0 | 2.9 | 2.71 |
| Weekend | 25.0% | 24.5% | 24.2% | 24.2% | 24.0% | 23.9% | 24.0% | 24.2% |
Abbreviations: ED, emergency department; Q1, Q3, first quartile, third quartile
Other ED includes: Transfer to another hospital, died in the ED, and unknown disposition
Other hospital disposition includes: Against medical advice, discharged alive, destination unknown
Hypertension-Related ED Visits
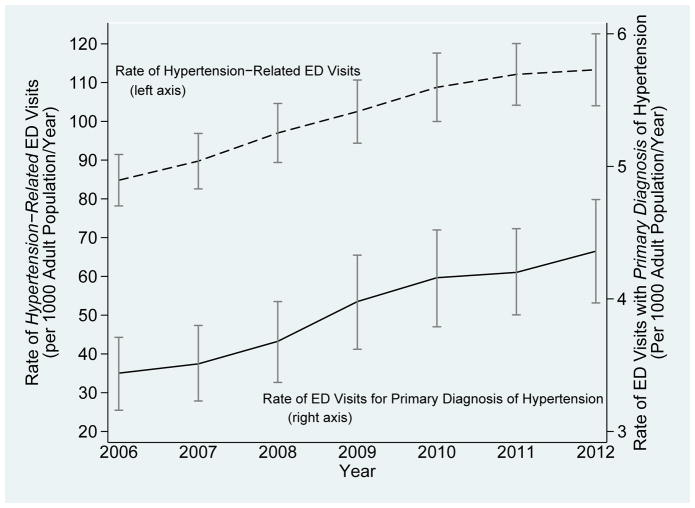
For hypertension-related ED visits from 2006 to 2012, the absolute number of ED visits increased 29.9%, the proportion of adult ED visits increased 20.3%, and population-based rate rose 25.2% (Table 1, Figure 1). According to the negative binomial regression model, the population based incidence rate of hypertension-related ED visits rose 5.2% per year of the 7-year study (incident rate ratio 1.05, 95% CI 1.044 to 1.061 p<0.001).
Figure 1. Annual Incidence of Hypertension-Related Emergency Department Visits and Emergency Department Visits With a Primary Diagnosis of Hypertension, 2006–2012.
Left Y-axis, dashed line: Rate of Hypertension-Related ED Visits (per 1,000 Adult Population Per Year); bars, 95% Confidence Intervals
Right Y-axis, solid line: Rate of ED Visits with Primary Diagnosis of Hypertension (per 1,000 Adult Population Per Year); bars, 95% Confidence Intervals
Abbreviations: ED, emergency department
Patient and hospital characteristics for hypertension-related ED visits are found in Table 1. More than half of ED visits occurred among women, and private health insurance was uncommon (23.0%). More than 40% of these ED visits resulted in hospitalization, and 58.2% occurred at safety net hospitals, while 42.3% of all ED visits occurred at safety net hospitals.21 Over the study period, the proportion of hypertension-related ED visits resulting in hospitalization decreased, with no clinically meaningful change in hospital length of stay or in-hospital mortality. The proportion of uninsured visits rose, as did the proportion of ED visits occurring at safety net hospitals.
ED Visits With a Primary Diagnosis of Hypertension
Over the seven-year study period, there were a total of 6,399,088 ED visits with a primary diagnosis of hypertension. For ED visits with a primary diagnosis of hypertension, the absolute number of ED visits rose 26.2%, the proportion of adult ED visits rose 16.2%, and the population-based incidence rate rose 21.1% (Figure 1, Table 2). According to the negative binomial regression model, the population based incidence rate of hypertension-related ED visits rose 4.4% per year of the 7-year study (incident rate ratio 1.044, 95% CI 1.038 to 1.051 p<0.001). Over the study period, the proportion of ED visits with a primary diagnosis of hypertension occurring at safety net hospitals and among uninsured patients rose, while the proportion hospitalized from the ED decreased, without a clinically meaningful change in hospital length of stay or inhospital mortality.
Compared to hypertension-related ED visits, ED visits with a primary diagnosis of hypertension occurred among patients who were younger and less likely to have private insurance; the proportion of patients hospitalized from the ED was lower, hospital length of stay was shorter, and in-hospital mortality was lower.
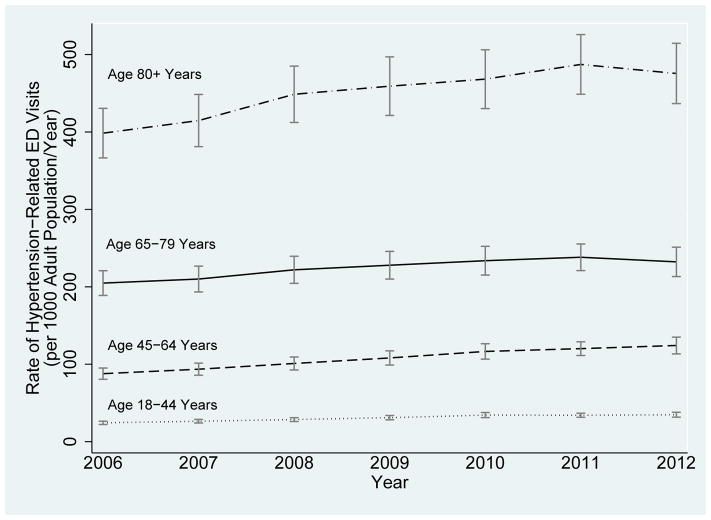
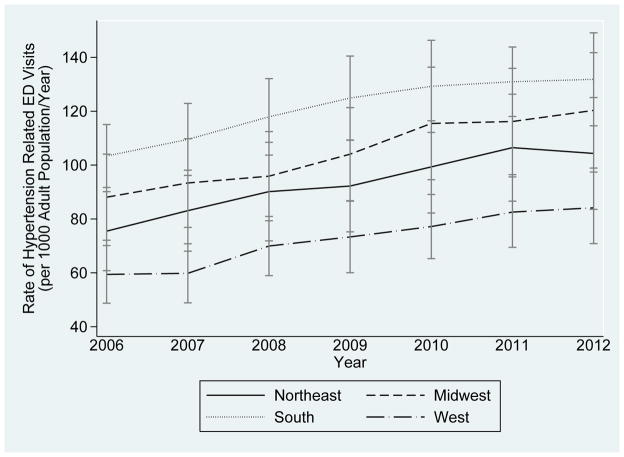
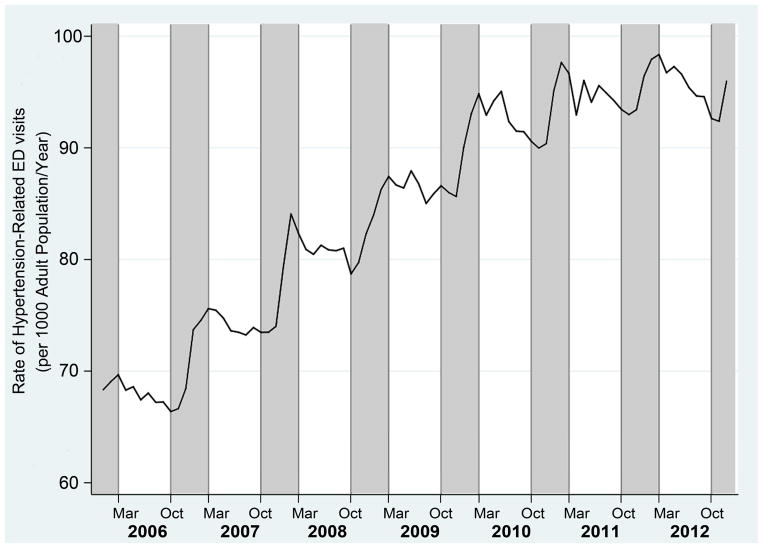
Annual incidence rates of hypertension-related ED visits rose the most among ED visits for patients ≥80 years of age (Figure 2). The rate of hypertension-related ED visits was highest in the South, followed by the Midwest, Northeast, and West (Figure 3). The rate of hypertension-related ED visits was higher during winter months than the summer (Figure 4), coinciding with rise in blood pressure during the winter.20
Figure 2. Annual Incidence of Hypertension-Related Emergency Department Visits By Age Group, 2006–2012.
All Rates of Hypertension-Related ED Visits are Per 1,000 Adult Population Per Year)
Dotted Line: Age 19–44 Years
Dashed Line: Age 45–64 Years
Solid Line: Age 65–79 Years
Dot-Dashed Line: Age 80 and Greater Years
Bars, 95% Confidence Intervals
Abbreviations: ED, emergency department
Figure 3. Annual Incidence of Hypertension-Related Emergency Department Visits By Geographic Region, 2006–2012.
All Rates of Hypertension-Related ED Visits are Per 1,000 Adult Population Per Year)
Dot-Dashed Line: West
Solid Line: Northeast
Dashed Line: Midwest
Dotted Line: South
Bars, 95% Confidence Intervals
Abbreviations: ED, emergency department
Figure 4. Seasonal Variation: Monthly Incidence of Hypertension-Related Emergency Department Visits, 2006–2012.
Solid Line: Hypertension-Related ED Visits (Per 1,000 Adult Population Per Year)
Gray Shading: Winter (October 1 through last day of February of the following year)
Abbreviations: ED, emergency department
Of 10,009 different primary diagnosis codes for ED visits with a secondary diagnosis of hypertension, the most frequent were: chest pain (ICD-9 CM 786.59 and ICD-9 CM 786.50; 6.8%), pneumonia (ICD-9 CM 486; 3.1%), urinary tract infection (ICD-9 CM 599.0; 2.2%), syncope and collapse (ICD-9 CM 780.2; 1.7%), and heart failure (ICD-9 CM 428.0; 1.6%).
Of the 7,164 co-occurring diagnosis codes among ED visits with a primary diagnosis of hypertension, the most common were: diabetes (ICD-9 CM 250.00; 15.4%), headache (ICD-9 CM 784.0; 11.7%), heart failure (ICD-9 CM 428.0; 11.7%), hyperlipidemia (ICD-9 CM 272.4; 11.0%), and tobacco use disorder (ICD-9 CM 305.1; 9.8%), followed by end stage renal disease (ICD-9 CM 585.6; 7.3%) and personal history of non-compliance with medical treatment, presenting hazards to health (ICD-9 CM V15.81; 7.2%).
Discussion
In this analysis of a national sample of US ED visits from 2006 to 2012, we report that the population-based incidence rate of hypertension-related ED visits rose by an estimated 5.2% per year (p<0.001) and the rate of ED visits with a primary diagnosis of hypertension rose 4.4% per year (p<0.001). Over the entire 7-year study period, the rates, proportion of adult ED visits, and absolute number of hypertension-related ED visits and visits with a primary diagnosis of hypertension all rose substantially. Overall, hypertension was included as a diagnosis in more than 1/5th of all adult ED visits from 2006 to 2012, and it was listed as the primary diagnosis in approximately 1% of all adult ED visits. Despite the increase in rate and proportion of hypertension-related ED visits, the proportion hospitalized after a hypertension-related ED visit decreased, without clinically meaningful change in hospital length of stay or in-hospital mortality. During the same time, the proportion of visits rose at safety net hospitals and among uninsured patients. Taken together, these data suggest that over time hypertension was more common among ED patients, more often managed by emergency physicians, more frequently recognized as contributing to ED visits, or a combination of the these factors.
Compared to hypertension-related ED visits overall, ED visits with a primary diagnosis of hypertension occurred among patients who were overall younger, healthier, more likely to be uninsured, more likely to have an income in the lowest quartile, and less likely to be hospitalized after the ED visit. This suggests that these patients may be utilizing the ED as a source of primary care.
ED visits, particularly for chronic conditions, are rising faster than the US population is growing.22,23 Our results are consistent with prior work, which found increases in ED visits for hypertension, diabetes, and pulmonary heart disease of 25%, 33%, and 29% from 2006 to 2011.24 The rise in ED visits related to chronic conditions may be due to a growing shortage of primary care providers,25 poor healthcare access despite health insurance,22 or rising prevalence of chronic conditions. These findings suggest that the burden of hypertension-related ED visits is an issue of increasing significance. The role of ED clinicians in identifying, evaluating, and managing hypertension and elevated blood pressure is a topic of ongoing debate.26 From a public health perspective, the ED may potentially play an important role in chronic disease management, particularly among patients who do not otherwise have access to care.27 Despite this, there is little evidence to guide the evaluation and treatment of hypertension in the ED setting.26 ED providers can help manage hypertension for discharged patients,28 and work is on-going to determine the safest and most efficient scope of care that can and should be provided in the ED. Given that hypertension is the number one risk factor for cardiovascular disease,1 these findings support the need for more rigorous study of the role of ED providers in acute as well as chronic management of this important condition.
The highest rates of hypertension-related ED visits occurred in the South, where hypertension and tobacco are most prevalent.29 Age was an additional factor in hypertension-related ED visits, with patients 80 years and older experiencing the largest increase in population-based incidence rates. Such individuals are at significant risk for consequences of uncontrolled hypertension, and future research is needed to address whether this apparent rise in ED visits is due to issues of blood pressure control, increased awareness, or change in coding practices. We also found evidence for seasonal variation in hypertension-related ED visits, which may help focus future ED-based hypertension interventions and research.20
The most common primary diagnosis codes among ED visits with a secondary diagnosis of hypertension were chest pain, pneumonia, urinary tract infection, syncope, and heart failure. In contrast, among ED visits with a primary diagnosis of hypertension, the most frequent associated co-listed diagnoses were diabetes, headache, heart failure, hyperlipidemia, and tobacco use disorder, followed by end stage renal disease and personal history of non-compliance. Although interpretation of such data is limited by the administrative nature of NEDS, these findings identify common comorbid conditions for future study among patients with hypertension-related ED visits.
Limitations of this exploratory, observational study include the inability to determine whether the rise in incidence of hypertension-related ED visits was due to true increase in disease burden versus increased awareness or changes in coding practices or a combination of both. Because NEDS does not include measured blood pressures, findings are restricted to visits with a diagnosis code of hypertension; use of ICD-9 CM codes may underestimate the overall burden of hypertension and comorbid conditions.13,14,30 Findings of trends among uninsured patients and safety net hospitals are exploratory; further work is needed to confirm these findings in prospective studies.
In conclusion, in this observational study of a national sample of US ED visits, hypertension-related ED visits and ED visits with a primary diagnosis of hypertension rose significantly from 2006 to 2012, while the proportion hospitalized declined. These data indicate that hypertension-related ED visits are common and rising.
Acknowledgments
Grant support: The project described was supported by the following federal grants: K12 HL109019, K23 HL125670, K23 GM110469 (Nashville, TN, USA), and R01 MD 005849 (Detroit, MI, USA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institute of General Medical Sciences, the National Institute of Minority Health and Health Disparities, or the National Institutes of Health.
Footnotes
Conflict(s) of Interest/Disclosure(s): The authors have no relevant conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics C, Stroke Statistics S. Executive summary: heart disease and stroke statistics--2014 update: a report from the american heart association. Circulation. 2014;129:399–410. doi: 10.1161/01.cir.0000442015.53336.12. [DOI] [PubMed] [Google Scholar]
- 2.CDC. Vital signs: prevalence, treatment, and control of hypertension--United States, 1999–2002 and 2005–2008. MMWR. 2011;60:103–108. [PubMed] [Google Scholar]
- 3.Xu W, Goldberg SI, Shubina M, Turchin A. Optimal systolic blood pressure target, time to intensification, and time to follow-up in treatment of hypertension: population based retrospective cohort study. BMJ. 2015;350:h158. doi: 10.1136/bmj.h158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Polgreen LA, Suneja M, Tang F, Carter BL, Polgreen PM. Increasing trend in admissions for malignant hypertension and hypertensive encephalopathy in the United States. Hypertension. 2015;65:1002–1007. doi: 10.1161/HYPERTENSIONAHA.115.05241. [DOI] [PubMed] [Google Scholar]
- 5.Wang G, Fang J, Ayala C. Hypertension-associated hospitalizations and costs in the United States, 1979–2006. Blood Press. 2014;23:126–133. doi: 10.3109/08037051.2013.814751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. CDC: National Center for Health Statistics; [Accessed August 31, 2015]. Available at: http://www.cdc.gov/nchs/fastats/emergency-department.htm. [Google Scholar]
- 7.McCusker J, Roberge D, Levesque JF, Ciampi A, Vadeboncoeur A, Larouche D, Sanche S. Emergency department visits and primary care among adults with chronic conditions. Med Care. 2010;48:972–980. doi: 10.1097/MLR.0b013e3181eaf86d. [DOI] [PubMed] [Google Scholar]
- 8.Niska RW. NCHS Data Brief. Vol. 27. Hayattsville, MD: National Center for Health Statistics; 2011. Blood Pressure Measurements at Emergency Department Visits by Adults: United States, 2007–2008. [PubMed] [Google Scholar]
- 9.Liu L, An Y, Chen M, Liu Z, Hu X, Chou E, Eisen HJ. Trends in the prevalence of hospitalization attributable to hypertensive diseases among United States adults aged 35 and older from 1980 to 2007. Am J Cardiol. 2013;112:694–699. doi: 10.1016/j.amjcard.2013.04.050. [DOI] [PubMed] [Google Scholar]
- 10.Morganti K, Bauhoff S, Blanchard J, Abir M, Iyer N, Smith A, Vesely J, Okeke E, Kellerman A. The Evolving Role of Emergency Departments in the United States. Santa Monica, CA: RAND; 2013. [PMC free article] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Quality and Research. [Accessed June 23, 2015];Overview of the National Emergency Department Sample (NEDS) Available at: http://www.hcup-us.ahrq.gov/nedsoverview.jsp.
- 12.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007:1–32. [PubMed] [Google Scholar]
- 13.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 14.Quam L, Ellis LB, Venus P, Clouse J, Taylor CG, Leatherman S. Using claims data for epidemiologic research. The concordance of claims-based criteria with the medical record and patient survey for identifying a hypertensive population. Med Care. 1993;31:498–507. [PubMed] [Google Scholar]
- 15.Friedman B, Jiang HJ, Elixhauser A, Segal A. Hospital inpatient costs for adults with multiple chronic conditions. MCRR. 2006;63:327–346. doi: 10.1177/1077558706287042. [DOI] [PubMed] [Google Scholar]
- 16.Chi MJ, Lee CY, Wu SC. The prevalence of chronic conditions and medical expenditures of the elderly by chronic condition indicator (CCI) Arch Gerontol Geriatr. 2011;52:284–289. doi: 10.1016/j.archger.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304:664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. [Accessed Feb 10, 2015];National Vital Statistics System: US Census Population With Bridged Race Categories. Available at: http://www.cdc.gov/nchs/nvss/bridged_race.htm.
- 19.U.S. Census Bureau. Census regions and divisions of the United States. US Department of Commerce, Economics, and Statistics Administration, Geography Division; [Accessed August 31, 2015]. Available at: http://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. [Google Scholar]
- 20.Youn JC, Rim SJ, Park S, Ko YG, Kang SM, Choi D, Ha JW, Jang Y, Chung N. Arterial stiffness is related to augmented seasonal variation of blood pressure in hypertensive patients. Blood Press. 2007;16:375–380. doi: 10.1080/08037050701642618. [DOI] [PubMed] [Google Scholar]
- 21.Fee C, Burstin H, Maselli JH, Hsia RY. Association of emergency department length of stay with safety-net status. JAMA. 2012;307:476–482. doi: 10.1001/jama.2012.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pitts SR, Carrier ER, Rich EC, Kellermann AL. Where Americans get acute care: increasingly, it’s not at their doctor’s office. Health Aff. 2010;29:1620–1629. doi: 10.1377/hlthaff.2009.1026. [DOI] [PubMed] [Google Scholar]
- 23.Derlet RW. Overcrowding in emergency departments: increased demand and decreased capacity. Ann Emerg Med. 2002;39:430–432. doi: 10.1067/mem.2002.122707. [DOI] [PubMed] [Google Scholar]
- 24.Skinner HG, Blanchard J, Elixhauser A. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): 2006. Trends in Emergency Department Visits, 2006–2011: Statistical Brief #179. [Google Scholar]
- 25.Kirch DG, Henderson MK, Dill MJ. Physician workforce projections in an era of health care reform. Annu Rev Med. 2012;63:435–445. doi: 10.1146/annurev-med-050310-134634. [DOI] [PubMed] [Google Scholar]
- 26.Decker WW, Godwin SA, Hess EP, Lenamond CC, Jagoda AS. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med. 2006;47:237–249. doi: 10.1016/j.annemergmed.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 27.Chernow SM, Iserson KV, Criss E. Use of the emergency department for hypertension screening: a prospective study. Ann Emerg Med. 1987;16:180–182. doi: 10.1016/s0196-0644(87)80012-4. [DOI] [PubMed] [Google Scholar]
- 28.Brody A, Rahman T, Reed B, Millis S, Ference B, Flack JM, Levy PD. Safety and efficacy of antihypertensive prescription at emergency department discharge. Acad Emerg Med. 2015;22:632–635. doi: 10.1111/acem.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001–2009. PLoS One. 2013;8:e60308. doi: 10.1371/journal.pone.0060308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bullano MF, Kamat S, Willey VJ, Barlas S, Watson DJ, Brenneman SK. Agreement between administrative claims and the medical record in identifying patients with a diagnosis of hypertension. Med Care. 2006;44:486–490. doi: 10.1097/01.mlr.0000207482.02503.55. [DOI] [PubMed] [Google Scholar]