Abstract
Aging is associated with numerous changes, including changes in sleep timing, duration, and quality. The circadian timing system interacts with a sleep-wake homeostatic system to regulate human sleep, including sleep timing and structure. Here, we review key features of the human circadian timing system, age-related changes in the circadian timing system, and how those changes may contribute to the observed alterations in sleep.
Keywords: aging, circadian, human, light, melatonin, sleep
1. Introduction
Earlier Sleep Timing and Reduced Sleep Consolidation With Age
A common feature of aging is the advance of the timing of sleep to earlier hours [1-8], often earlier than desired [9-11]. The sleep of older people is also characterized by an increased number of awakenings [12] and a reduction of the deeper stages of nonREM sleep (also called slow wave sleep, SWS, Stages 3 and 4 sleep) [4, 13-32]. These age-related changes are also associated with sleep complaints, with most studies finding that more than one third of older adults report early morning awakening and/or difficulty maintaining sleep on a regular (several times per week) basis [9-11, 33-35]. Although sleep disorders are far more prevalent in older adults [36, 37], even otherwise healthy older individuals also show characteristic changes in sleep, including reductions in SWS and sleep efficiency and increases in awakenings [38-42]. In fact, age-related changes in sleep structure are seen even in middle-aged adults [38-42].
Circadian Timing System Regulates Sleep Timing and Consolidation
The circadian timing system is one of the two major sleep regulatory systems [43, 44] (the other being a homeostatic sleep-wake process). The circadian timing system is a major determinant of the timing of sleep and sleep structure in humans, and many aspects of sleep vary markedly with circadian phase in both young and older adults [45-48]. A proper alignment between the timing of sleep and the circadian phase of sleep is important for sleep duration and quality, as demonstrated in both healthy subjects [49-51] and in some clinical conditions [52, 53]. The circadian timing system has a major influence on the timing and duration REM sleep [44], and has a smaller but still significant impact on many aspects of nonREM sleep. The circadian drive for wakefulness increases across the biological day, reaching its maximum in the evening hours when homeostatic sleep pressure is high, the so-called “wake-maintenance zone” [54, 55]. The circadian drive for sleep reaches its maximum during the early morning hours just prior to habitual awakening time, when homeostatic sleep pressure is low [29, 56]. Under ideal conditions, the circadian rhythm of sleep-wake interacts with the homeostatic sleep-wake process to allow for consolidated sleep (and wake) in humans [57-63]. Studies in young adults have demonstrated that even a small change in the circadian time of sleep can have large impact on the ability to consolidate sleep throughout the night. Thus, age-related changes in circadian rhythms or circadian sleep regulation may underlie the sleep timing and consolidation changes seen in aging, and if so may be a target for therapeutics to improve sleep.
As outlined in earlier chapters, circadian rhythms are endogenously generated oscillations in physiology and behavior with a near-24-hour period. Human circadian period averages slightly longer than 24 hours, with a range of about 23.5 – 24.5 hours in sighted adults [64-70]. The circadian system is synchronized to the 24-hour day by signals from the environment, a process called entrainment. In humans, as in most mammals, entrainment typically occurs via light-dark exposure. Light has a phase-dependent effect on the circadian system, meaning that the effect of a given light stimulus is dependent on the phase (or biological time of day) at which the light exposure occurs. Light exposure in the late evening and early night shifts the timing of rhythms later (phase delay shifts), light exposure in the late night and early morning shifts the timing of rhythms earlier (phase advance shifts), while light exposure in the middle of the biological day produces very small changes in rhythm timing [71, 72]. Plots of the magnitude of the phase shift with respect to the phase at which the light exposure was given are called phase response curves (PRCs). The phase relationship between the circadian system and the entraining signal is referred to as the phase angle (or phase angle of entrainment; see Figure 1). Circadian period interacts with the PRC in the entrainment process, and individuals with different periods (and/or different magnitude PRCs) will have different phase angles of entrainment [70, 73].
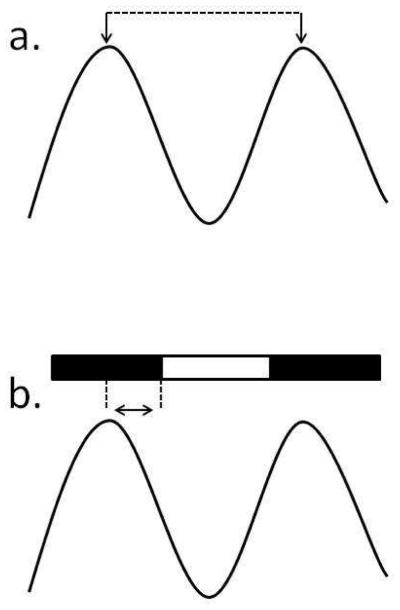
Figure 1.
Schematic illustrating some of the key features of circadian rhythms. A. Phase (down arrows) refers to a reference point in the ~24-hour rhythm, in this case the peak of the rhythm. The duration from the phase on one cycle to the same phase on the next cycle (dashed line) is the period (cycle length) of the rhythm. Period can only be assessed under controlled experimental conditions. B. The near-24-hour circadian rhythms are entrained (synchronized) to the environment through periodic signals from the environment, typically light-dark exposure (indicated by the bar across the top of Panel B). The relationship between the entraining signal (here, lights on, represented by the right dashed vertical line) and the phase of the rhythm (here the peak of the rhythm, represented by the left dashed vertical line) is referred to as the phase angle of entrainment (horizontal arrow). This phase angle is dependent on the period of the rhythm, the strength of the entraining signal, and the phase-dependent response to that entraining signal.
Age-related changes in any of the structures involved in generating or entraining circadian rhythms, and/or age-related changes in any of the critical features or processes involved in entrainment may therefore contribute to altered circadian rhythm timing with advancing age. We outline below the evidence for alterations in circadian rhythms with age, and how these might contribute to age-related changes in sleep timing and consolidation.
Methods for Assessing Human Circadian Rhythms
Circadian phase is typically assessed in humans by measuring one or more of the physiologic parameters that are controlled in part by the circadian timing system. The most widely used measures of circadian phase in humans are the rhythms of core body temperature and melatonin (although many other hormones have rhythms), and each has its advantage and disadvantage. Body temperature has the advantage of being able to be collected continuously, whereas melatonin, which is typically measured in saliva or plasma, can only be collected at less frequent intervals (typically every 30-60 minutes). Body temperature can be measured using a rectal sensor or an ingestible transmitter. A major disadvantage of using body temperature as a marker of circadian timing is that the variations in temperature across the day are not only due to circadian rhythmicity, but also due to such factors as posture, sleep-wake state, and activity level. Furthermore, the influence of those behavioral factors on body temperature is phase-dependent, such that the change in temperature produced by the behavior is different depending on where in the circadian cycle the behavior occurs. Thus, diurnal variations in temperature, particularly the time of the nadir of the temperature cycle, may not reflect the underlying circadian variation. Melatonin has the advantage of being far less influenced by posture, sleep-wake state, and activity level than temperature, although there is some evidence that periodic changes in behavior can influence melatonin level. Melatonin is suppressed by light exposure, so ambient lighting must be strictly controlled at low levels throughout all sampling segments. One disadvantage of using melatonin as a circadian phase marker is that collection of samples during sleep may require interruption of sleep, although specialized blood collection systems used in many laboratories avoid sleep interruption. Because of this limitation, in many studies only the onset of melatonin secretion is used as a phase marker, rather than collection the entire 24-hour rhythm. While in many cases this dim light melatonin onset (DLMO) is sufficient to determine changes in rhythm timing, it will miss out on any changes in melatonin rhythm amplitude, duration, or offset timing.
The constant routine (CR) protocol was developed to assess the phase and amplitude of circadian rhythms [74, 75]. The CR consists of a 24+ hour period of wakefulness in a semi-recumbent posture, such that sleep-wake state, posture, and activity level are kept constant. Room temperature, humidity, and light level are similarly kept constant, and food and fluid intake are divided into small snacks that are consumed at regular intervals. In this way, many of the factors known to influence physiologic rhythms are either eliminated or are spread across day and night, allowing the underlying circadian oscillation to be observed. In studies of circadian rhythmicity where sleep deprivation is a major concern, melatonin can be used as the sole circadian phase marker. Protocols in which 24 or more hours of data are collected under controlled conditions allow for assessment of circadian phase and amplitude, making the CR protocol ideal for such assessments.
While circadian period is typically assessed in animals by putting the animal into constant darkness and observing the rest-activity cycle over several days, other methods are used to assess human circadian period. One method is the forced desynchrony (FD) protocol, in which the participant is scheduled to live on a rest-activity cycle much shorter or longer than 24 hours while continuous measurement of physiologic rhythms are collected [64]. FD data are then analyzed by accounting for the imposed periodicity resulting from the rest-activity cycle, while searching for periodicity within the circadian range. That method has been validated against period assessments from CRs, and by multiple physiologic measures in the same individual showing the same periodicity [64]. More recently, ultra-short sleep-wake cycles have been used to assess circadian period, although in most cases there has been no independent validation of this method of assessing period.
2. Evidence for Circadian Changes In Aging In Humans
Circadian Phase
Circadian phase has been shown to move earlier, or advance, with age [76-81]. As described above, most rhythms controlled by the circadian system are also influenced by many external and behavioral factors, and therefore the best evidence about circadian phase comes from studies conducted under laboratory conditions such as the Constant Routine, designed to control for effects of light exposure, posture, ambient temperature, sleep, and food intake [75]. The timing of the circadian rhythm of core body temperature has been reported to be earlier in both middle-aged and older (>age 60) adults than in young (~age 20-30) adults [1, 78, 82-85]. The circadian phase of melatonin has also been reported to move earlier with age [85-88], as has the timing of the cortisol rhythm [80, 81, 89, 90]. Figure 2 illustrates the advanced phase observed in studies of older adults.
Figure 2.
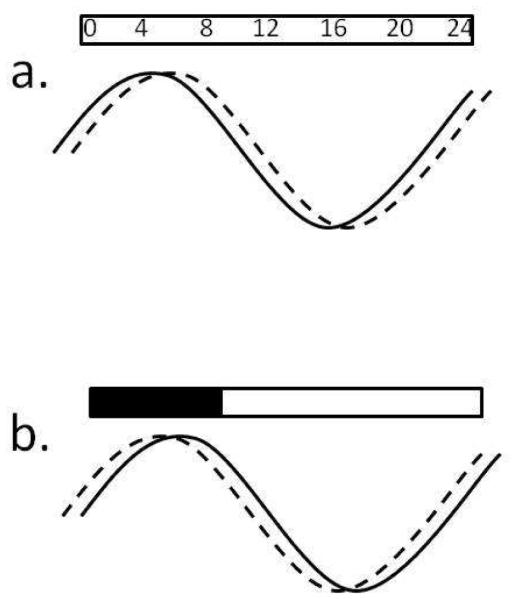
Schematic illustrating the altered phase in older adults. A. When compared with clock time, the phase of both core body temperature and plasma melatonin is earlier in older adults (solid line) than it is in young adults (dashed line). B. However, when compared with their usual sleep-wake and dark-light timing, the phase of both core body temperature and plasma melatonin is later with respect to sleep/darkness in older adults (solid line) than it is in young adults (dashed line).
Phase of Entrainment
The phase relationship between a circadian rhythm of interest and the signal from the environment that entrains the rhythm (typically the light-dark cycle) is referred to as the phase angle of entrainment [91]. There is evidence from animals that the timing of the rhythm of locomotor activity with respect to the timing of the light-dark cycle is altered in aging. Studies in hamsters found that activity onset is earlier with respect to lights out in older animals, and reentrainment after the light-dark cycle is shifted is faster [92, 93]. However, a study in mice reported delayed activity onset and slower reentrainment [94]. Studies of phase angle in humans have either reported no difference with age [83, 95-97], or have found that older people show an altered phase angle, such that the timing of the phase of their rhythms of core body temperature and melatonin occur later with respect to sleep (and lights out) [1, 86, 87]. This latter finding means that older adults are not only sleeping at an earlier clock time, they are sleeping at an earlier biological time.
Circadian Amplitude
There are numerous reports of reduced circadian rhythm amplitude with aging. In animals, reduced amplitude of the rest-activity cycle [94, 98-100], as well as the amplitude of multi-unit electrical activity in the SCN have been reported [101-104]. In studies of human circadian rhythms, most reports find a reduced temperature amplitude with age [31, 78, 82, 105], and many but not all find reduced amplitude of the rhythms of melatonin and other hormones [7, 96, 106]. While changes in the electrical activity of the SCN likely lead to alterations in output rhythm amplitude, the functional consequences of alterations in output rhythm amplitude are not well understood.
Circadian-Sleep Interaction
As outlined above, the circadian system interacts with a sleep-wake homeostatic process to regulate the timing and consolidation of sleep in humans. Studies using protocols such as the forced desynchrony protocol have been used to separate circadian from sleep-wake-dependent influences on sleep and waking performance, and to compare those influences between young and older adults. Those studies have demonstrated that the sleep of older adults is much more vulnerable to circadian misalignment than the sleep of young adults [12, 29, 31, 32, 39, 48, 107]. There is a much narrower range of circadian times when the end of sleep can remain consolidated in older adults compared with young adults, and a corresponding reduction in the range of circadian phases at which alertness and performance is impaired in older subjects [1, 62, 108, 109], suggesting an age-related reduction in the circadian drive for sleep in the early morning [12, 29, 31, 32, 39, 107]. Studies using ultra-short sleep-wake cycles have also reported a reduction in the circadian drive for wakefulness in the evening (the “wake-maintenance zone”) [39, 96]. Together, these findings suggest that there may be a reduction in the circadian rhythm of sleep-wake propensity that occurs in aging.
Circadian Period
It was hypothesized that a shortening of circadian period with age could explain the shift in sleep timing with age, and there was evidence from some animal studies that period was shorter in older animals [110-112]. An initial series of forced desynchrony studies in which circadian period was assessed in healthy older adults and compared with young adults found no difference in period with age [64], and in a follow-up study of a larger group of young and older adults we found the same result [70]. A study of six blind men who each had their period estimated twice over a ~10-year interval found no evidence for a shortening of period with age within an individual [113]. Together, these findings suggest that an age-related shortening of circadian period does not underlie the advance in circadian rhythms and sleep timing with age in humans.
Response to Light
Light is the primary environmental signal influencing circadian rhythms, and serves to synchronize the near-24-h circadian system to the 24-h environmental day [64-67, 91, 114-116]. Most humans spend relatively little time in outdoor levels of light [117-119] and therefore indoor light plays a dominant role in synchronizing circadian rhythms for most people. Use of artificial illumination in the evening has been shown to partially suppress and alter the timing of the melatonin rhythm and sleep in young adults [120-123]. Thus, the pattern of exposure to light in the evening is a likely mechanism contributing to circadian timing and sleep in older adults, and there is evidence to support age-related differences in light exposure patterns in older adults living in the community [124, 125].
Whether the response to light differs between young and older adults is also relevant to sleep and circadian rhythm timing, and a number of studies of the circadian response to light in older vs. young adults have been carried out over the past two decades, with mixed findings. Klerman and colleagues [126] used a bright (10,000 lux) light stimulus of 5 hours/day over 3 days in young and older adults, and delivered the light stimuli across the phase delay and the phase advance regions of the PRC. They found no evidence for an age difference in phase-shifting response when light was presented in the phase delay region, and a suggestion that there might be reduced responses in the older participants in the phase advance region. Benloucif and colleagues [127] used a 4-hour 3,500 lux stimulus delivered in the phase delay region and also found no evidence for an age difference in phase-shifting response. Kim and colleagues [85] tested a 2-hour light stimulus of 2,000 or 8,000 lux delivered at a variety of different phases and did not find significant differences in phase-shifting responses between young and older participants. Duffy and colleagues [128] used a 6.5-hour light stimulus in the phase delay region and tested a wide range of stimulus intensities. They found no difference in phase delay response for low (<100 lux) or high (>1,000 lux) light levels, but did find evidence for a reduced responsiveness among the older subjects in the intermediate range, with a half-maximal response shifted to 263 lux compared with 119 lux in the young adults.
While all the previous studies used polychromatic light sources, additional studies using monochromatic light stimuli have also been conducted. Herljevic and colleagues [129] used a 30-minute light stimulus of short (456nm) wavelength light delivered in the phase delay region and found significant differences in melatonin suppression between young and older women, but no age difference when a longer (548nm) wavelength light stimulus was used. In a study of 2 hours of intermittent short or long wavelength monochromatic light delivered in the phase advance region, Sletten and colleagues [130] reported that phase shifting responses were slightly larger in the young participants, although the difference was not statistically significant. Najjar et al. [131] studied a series of non-visual responses to monochromatic light in young and older adults and found a shift in peak sensitivity to longer wavelengths in the older participants, but no change in melatonin suppression. Thus, while there are some suggestions of changes in light sensitivity with aging in humans, the differences in response to light in healthy older adults are not strong, and additional research in this area is needed to better understand whether changes in light sensitivity contribute to sleep and circadian rhythm timing changes with age.
Light Transmission
The changes in circadian responses to light that have been observed in some studies may be due to age-related changes in the pathway through the eye, along the RHT, and/or within the SCN [132]. There is extensive evidence for changes in the transmission of light through the crystalline lens with age [132-134]. The aging lens accumulates yellow pigmentation which selectively reduces transmission of short wavelength light [131, 132, 134]. While the exact relevance of this for humans living freely in environments where they can control ambient polychromatic lighting is not yet clear, a study of nearly 1,000 Danish adults found that the age-related increase in yellowing of the lens was associated with greater reported sleep disturbances [135].
There are also changes in the pupil with aging, with older adults having a smaller pupil than young adults. Daneault and colleagues tested whether this impacts response to monochromatic light exposure. They found that while older adults had smaller pupils at dark-adapted baseline and at all light levels tested, the reduction in pupil size in response to light was not different between young and older subjects [136]. Thus, available evidence suggests that light transmission through the lens is altered with age, specifically reducing transmission of short wavelength light. Age-related changes in retinal function have also been reported in humans [137, 138], and there is a report that the number of ipRGCs declines with age in rodless-coneless mice [139], although that same group reported no change in responsiveness to light in the same type of older mice [140].
SCN
While studies of human SCN function cannot be carried out, there is a general consensus based on animal studies that there are age-related changes in the SCN (reviewed e.g. in [141]). Studies carried out more than two decades ago demonstrated that the locomotor activity pattern of aged animals was much more consolidated after transplantation of fetal SCN, suggesting that some unknown factor(s) that had declined with age had been re-introduced or improved [142-145]. There is strong evidence of altered patterns of electrical activity in the SCN of aged animals [101-103]. This is likely due to altered synchrony amongst SCN neurons, which leads to a reduced rhythm of multi-unit activity [104]. Within individual SCN cells, changes in cell membrane properties that alter electrical activity of the cells have been demonstrated in older animals [146]. There is conflicting evidence about whether the size or cell number within the SCN is altered with age [147-150], but there is general consensus that the aged SCN shows reductions in the number of cells expressing two major peptides, vasoactive intestinal polypeptide (VIP) and arginine-vasopressin (AVP) in both animals and humans [148-158].
Clock Gene Expression
There is some evidence from animal studies that clock gene expression is altered in aging, although not all studies are in agreement. One study found that expression of Per1 in response to an entraining light stimulus was reduced in aged hamsters, and this was associated with a significantly longer time to resynchronization [159]. That same study also found that the amplitude of Per1 and Per2 were not altered in older hamsters studied in constant darkness, but Bmal1 and Clock were altered in older hamsters. In a study of young and older mice, the amplitude of Per2 expression (but not expression of Per1, Clock, or Cry) was found to be reduced in the SCN of older mice [160]. A more comprehensive study of clock gene expression in young and older mice found age-related differences in expression of Per2, Bmal1, Rev-erbα, Dbp, and Dec1 expression in the SCN of the older mice [161]. Thus, even with the limited number of studies thus far, there is evidence that the molecular clockwork itself may be altered in aging, although much more research in this area remains to be done.
Circadian Rhythm Sleep Wake Disorders
Older adults in general sleep and wake at earlier times than do young adults, and in general older adults are more likely to report Advanced Sleep Wake Phase Disorder than are young adults [162, 163]. These patients report inability to stay awake in the evening and earlier than desired wake time. Delayed Sleep Wake Phase Disorder and Non-24-h Sleep Wake Disorder show the reverse trend, with far fewer older adults complaining of sleep timing that is later than desired [163]. There is evidence that older adults are more prone to Shift Work Disorder [164-169] and Jet Lag Disorder, and this has been hypothesized to be due to a greater inability to sleep at an adverse biological time with age [12, 29, 31, 32, 48], and/or a reduced ability to phase shift with age. In addition to those circadian rhythm sleep disorders that impact community-dwelling older adults, there is evidence that institutionalized older adults and older adults with neurodegenerative diseases such as Alzheimer’s Disease have very high rates of Irregular Sleep Wake Rhythm Disorder [170-174]. This disorder is characterized by extremely irregular and fragmented sleep-wake patterns, and the disrupted sleep-wake rhythms are associated with very little bright light exposure [175-177], which may potentially feed back and exacerbate the disrupted sleep patterns [177]. Interventions in which ambient lighting is increased have been tested in institutionalized settings, and in some cases have been demonstrated to improve sleep-wake consolidation [178-180].
3. Summary
The most prominent age-related change in biological timing in humans is the shift of sleep to earlier hours. Why this occurs is still largely unknown. There is evidence for age-related changes in many aspects of circadian rhythmicity, including the transcriptional-translational feedback loops involved in circadian rhythm generation, the neuroanatomical structures, the transmission and responsiveness to light, and the timing and amplitude of output rhythms.
Key Points.
Sleep timing changes with age;
The circadian system is a major sleep regulatory system;
There are age-associated changes in human circadian rhythms;
There are age-associated changes in components of the circadian system in both animals and humans;
There is evidence for alterations in circadian rhythmicity contributing to age-related changes in sleep.
5. Acknowledgments
The authors wish to thank Ms. J. Hong for assistance with the manuscript. This work was supported in part by NIH grants P01 AG09975, R01 AG044416, and R01 HL094654. KMZ is supported by a fellowship from the Finnish Cultural Foundation and a grant from the Gyllenberg Foundation; EDC is supported by a fellowship from institutional training grant T32 HL007901.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
4. References
- [1].Duffy JF, Dijk DJ, Klerman EB, et al. Later endogenous circadian temperature nadir relative to an earlier wake time in older people. Am J Physiol. 1998;275:R1478–R87. doi: 10.1152/ajpregu.1998.275.5.r1478. [DOI] [PubMed] [Google Scholar]
- [2].Gerard P, Collins KJ, Dore C, et al. Subjective characteristics of sleep in the elderly. Age Ageing. 1978;7:55–9. doi: 10.1093/ageing/7.suppl.55. [DOI] [PubMed] [Google Scholar]
- [3].Miles LE, Dement WC. Sleep and aging. Sleep. 1980;3:119–220. [PubMed] [Google Scholar]
- [4].Minors DS, Rabbitt PMA, Worthington H, et al. Variation in meals and sleep-activity patterns in aged subjects; its relevance to circadian rhythm studies. Chronobiol Int. 1989;6:139–46. doi: 10.3109/07420528909064624. [DOI] [PubMed] [Google Scholar]
- [5].Monk TH, Reynolds CF, III, Buysse DJ, et al. Circadian characteristics of healthy 80-year-olds and their relationship to objectively recorded sleep. J Gerontol. 1991;46:M171–M5. doi: 10.1093/geronj/46.5.m171. [DOI] [PubMed] [Google Scholar]
- [6].Tune GS. The influence of age and temperament on the adult human sleep-wakefulness pattern. Br J Psychol. 1969;60:431–41. doi: 10.1111/j.2044-8295.1969.tb01216.x. [DOI] [PubMed] [Google Scholar]
- [7].Van Coevorden A, Mockel J, Laurent E, et al. Neuroendocrine rhythms and sleep in aging men. Am J Physiol. 1991;260:E651–E61. doi: 10.1152/ajpendo.1991.260.4.E651. [DOI] [PubMed] [Google Scholar]
- [8].Van Someren EJ. Circadian and sleep disturbances in the elderly. Exp Gerontol. 2000;35:1229–37. doi: 10.1016/s0531-5565(00)00191-1. [DOI] [PubMed] [Google Scholar]
- [9].Foley DJ, Monjan AA, Brown SL, et al. Sleep complaints among elderly persons: An epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- [10].Mant A, Eyland EA. Sleep patterns and problems in elderly general practice attenders: An Australian survey. Community Health Stud. 1988;12:192–9. doi: 10.1111/j.1753-6405.1988.tb00160.x. [DOI] [PubMed] [Google Scholar]
- [11].McGhie A, Russell SM. The subjective assessment of normal sleep patterns. J Ment Sci. 1962;108:642–54. [Google Scholar]
- [12].Dijk DJ, Duffy JF, Czeisler CA. Age-related increase in awakenings: Impaired consolidation of nonREM sleep at all circadian phases. Sleep. 2001;24:565–77. doi: 10.1093/sleep/24.5.565. [DOI] [PubMed] [Google Scholar]
- [13].Bixler EO, Kales A, Jacoby JA, et al. Nocturnal sleep and wakefulness: effects of age and sex in normal sleepers. Int J Neurosci. 1984;23:33–42. doi: 10.3109/00207458408985343. [DOI] [PubMed] [Google Scholar]
- [14].Blois R, Feinberg I, Gaillard JM, et al. Sleep in normal and pathological aging. Experientia. 1983;39:551–8. doi: 10.1007/BF01971096. [DOI] [PubMed] [Google Scholar]
- [15].Brezinova V. The number and duration of the episodes of the various EEG stages of sleep in young and older people. Electroencephalogr Clin Neurophysiol. 1975;39:273–8. doi: 10.1016/0013-4694(75)90149-2. [DOI] [PubMed] [Google Scholar]
- [16].Dijk DJ, Beersma DGM, van den Hoofdakker RH. All night spectral analysis of EEG sleep in young adult and middle-aged male subjects. Neurobiol Aging. 1989;10:677–82. doi: 10.1016/0197-4580(89)90004-3. [DOI] [PubMed] [Google Scholar]
- [17].Ehlers CL, Kupfer DJ. Effects of age on delta and REM sleep parameters. Electroencephalogr Clin Neurophysiol. 1989;72:118–25. doi: 10.1016/0013-4694(89)90172-7. [DOI] [PubMed] [Google Scholar]
- [18].Feinberg I. Changes in sleep cycle patterns with age. J Psychiatr Res. 1974;10:283–306. doi: 10.1016/0022-3956(74)90011-9. [DOI] [PubMed] [Google Scholar]
- [19].Foret J, Webb WB. Evolution de l'organisation temporelle des stades de sommeil chez l'homme de 20 a 70 ans. Rev Electroencephalogr Neurophysiol Clin. 1980;10:171–6. doi: 10.1016/s0370-4475(80)80050-5. [DOI] [PubMed] [Google Scholar]
- [20].Hayashi Y, Endo S. All-night sleep polygraphic recordings of healthy aged persons: REM and slow-wave sleep. Sleep. 1982;5:277–83. doi: 10.1093/sleep/5.3.277. [DOI] [PubMed] [Google Scholar]
- [21].Kahn E, Fisher C. The sleep characteristics of the normal aged male. J Nerv Ment Dis. 1969;148:477–94. doi: 10.1097/00005053-196905000-00002. [DOI] [PubMed] [Google Scholar]
- [22].Prinz PN. Sleep patterns in the healthy aged: Relationship with intellectual function. J Gerontol. 1977;32:179–86. [Google Scholar]
- [23].Prinz PN, Vitiello MV, Raskind MA, et al. Geriatrics: Sleep disorders and aging. New Engl J Med. 1990;323:520–6. doi: 10.1056/NEJM199008233230805. [DOI] [PubMed] [Google Scholar]
- [24].Reynolds CF, III, Kupfer DJ, Taska LS, et al. Sleep of healthy seniors: A revisit. Sleep. 1985;8:20–9. doi: 10.1093/sleep/8.1.20. [DOI] [PubMed] [Google Scholar]
- [25].Webb WB. The measurement and characteristics of sleep in older persons. Neurobiol Aging. 1982;3:311–9. doi: 10.1016/0197-4580(82)90019-7. [DOI] [PubMed] [Google Scholar]
- [26].Webb WB, Campbell SS. Awakenings and the return to sleep in an older population. Sleep. 1980;3:41–6. [PubMed] [Google Scholar]
- [27].Bliwise DL. Sleep in normal aging and dementia. Sleep. 1993;16:40–81. doi: 10.1093/sleep/16.1.40. [DOI] [PubMed] [Google Scholar]
- [28].Prinz PN. Sleep and sleep disorders in older adults. J Clin Neurophysiol. 1995;12:139–46. doi: 10.1097/00004691-199503000-00004. [DOI] [PubMed] [Google Scholar]
- [29].Dijk DJ, Duffy JF, Riel E, et al. Ageing and the circadian and homeostatic regulation of human sleep during forced desynchrony of rest, melatonin and temperature rhythms. J Physiol (Lond) 1999;516.2:611–27. doi: 10.1111/j.1469-7793.1999.0611v.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Dijk DJ, Kelly TK, Riel E, et al. Altered homeostatic delta EEG response to sleep loss in older people? Sleep. 1999;22:S226. [Google Scholar]
- [31].Dijk DJ, Duffy JF. Circadian regulation of human sleep and age-related changes in its timing, consolidation and EEG characteristics. Ann Med. 1999;31:130–40. doi: 10.3109/07853899908998789. [DOI] [PubMed] [Google Scholar]
- [32].Dijk DJ, Duffy JF, Czeisler CA. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol Int. 2000;17:285–311. doi: 10.1081/cbi-100101049. [DOI] [PubMed] [Google Scholar]
- [33].Morgan K, Dallosso H, Ebrahim S, et al. Characteristics of subjective insomnia in the elderly living at home. Age Ageing. 1988;17:1–7. doi: 10.1093/ageing/17.1.1. [DOI] [PubMed] [Google Scholar]
- [34].Executive summary of the 2003 "Sleep in America" Poll. National Sleep Foundation; Washington, DC: 2003. [Google Scholar]
- [35].Ohayon MM, Caulet M, Guilleminault C. How a general population perceives its sleep and how this relates to the complaint of insomnia. Sleep. 1997;20:715–23. doi: 10.1093/sleep/20.9.715. [DOI] [PubMed] [Google Scholar]
- [36].McCurry SM, Ancoli-Israel S. Sleep dysfunction in Alzheimer's Disease and other dementias. Curr Treat Options Neurol. 2003;5:261–72. doi: 10.1007/s11940-003-0017-9. [DOI] [PubMed] [Google Scholar]
- [37].Ribeiro JA, Sebastiao AM, de Mendonca A. Adenosine receptors in the nervous system: pathophysiological implications. Prog Neurobiol. 2002;68:377–92. doi: 10.1016/s0301-0082(02)00155-7. [DOI] [PubMed] [Google Scholar]
- [38].Ehlers CL, Kupfer DJ. Slow-wave sleep: Do young adult men and women age differently? J Sleep Res. 1997;6:211–5. doi: 10.1046/j.1365-2869.1997.00041.x. [DOI] [PubMed] [Google Scholar]
- [39].Haimov I, Lavie P. Circadian characteristics of sleep propensity function in healthy elderly: A comparison with young adults. Sleep. 1997;20:294–300. doi: 10.1093/sleep/20.4.294. [DOI] [PubMed] [Google Scholar]
- [40].Carrier J, Frenette S, Montplaisir J, et al. Effects of periodic leg movements during sleep in middle-aged subjects without sleep complaints. Mov Disord. 2005;20:1127–32. doi: 10.1002/mds.20506. [DOI] [PubMed] [Google Scholar]
- [41].Carrier J, Monk TH, Buysse DJ, et al. Sleep and morningness-eveningness in the 'middle' years of life (20-59y) J Sleep Res. 1997;6:230–7. doi: 10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- [42].Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- [43].Borbély AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1:195–204. [PubMed] [Google Scholar]
- [44].Dijk DJ, Czeisler CA. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. J Neurosci. 1995;15:3526–38. doi: 10.1523/JNEUROSCI.15-05-03526.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Czeisler CA, Weitzman ED, Moore-Ede MC, et al. Human sleep: Its duration and organization depend on its circadian phase. Science. 1980;210:1264–7. doi: 10.1126/science.7434029. [DOI] [PubMed] [Google Scholar]
- [46].Strogatz SH, Kronauer RE, Czeisler CA. Circadian regulation dominates homeostatic control of sleep length and prior wake length in humans. Sleep. 1986;9:353–64. doi: 10.1093/sleep/9.2.353. [DOI] [PubMed] [Google Scholar]
- [47].Carskadon MA, Dement WC, Mitler MM, et al. Guidelines for the multiple sleep latency test (MSLT): A standard measure of sleepiness. Sleep. 1986;9:519–24. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- [48].Hughes R, Sack RL, Lewy AJ. The role of melatonin and circadian phase in age-related sleep-maintenance insomnia: Assessment in a clinical trial of melatonin replacement. Sleep. 1998;21:52–68. [PubMed] [Google Scholar]
- [49].Fookson JE, Kronauer RE, Weitzman ED, et al. Induction of insomnia on a non-24 hour sleep-wake schedule. Sleep Res. 1984;13:220. [Google Scholar]
- [50].Orth DN, Island DP. Light synchronization of the circadian rhythm in plasma cortisol (17-OHCS) concentration in man. J Clin Endocrinol Metab. 1969;29:479–86. doi: 10.1210/jcem-29-4-479. [DOI] [PubMed] [Google Scholar]
- [51].Campbell SS, Dawson D. Aging young sleep: a test of the phase advance hypothesis of sleep disturbance in the elderly. Sleep Res. 1991;20:447. doi: 10.1111/j.1365-2869.1992.tb00040.x. [DOI] [PubMed] [Google Scholar]
- [52].Ozaki S, Uchiyama M, Shirakawa S, et al. Prolonged interval from body temperature nadir to sleep offset in patients with delayed sleep phase syndrome. Sleep. 1996;19:36–40. [PubMed] [Google Scholar]
- [53].Campbell SS, Dawson D, Anderson MW. Alleviation of sleep maintenance insomnia with timed exposure to bright light. J Am Geriatr Soc. 1993;41:829–36. doi: 10.1111/j.1532-5415.1993.tb06179.x. [DOI] [PubMed] [Google Scholar]
- [54].Lavie P. Ultrashort sleep-waking schedule III. "Gates" and "forbidden zones" for sleep. Electroencephalogr Clin Neurophysiol. 1986;63:414–25. doi: 10.1016/0013-4694(86)90123-9. [DOI] [PubMed] [Google Scholar]
- [55].Strogatz SH, Kronauer RE, Czeisler CA. Circadian pacemaker interferes with sleep onset at specific times each day: Role in insomnia. Am J Physiol. 1987;253:R172–R8. doi: 10.1152/ajpregu.1987.253.1.R172. [DOI] [PubMed] [Google Scholar]
- [56].Dijk DJ, Czeisler CA. Paradoxical timing of the circadian rhythm of sleep propensity serves to consolidate sleep and wakefulness in humans. Neurosci Lett. 1994;166:63–8. doi: 10.1016/0304-3940(94)90841-9. [DOI] [PubMed] [Google Scholar]
- [57].Dijk DJ, Duffy JF, Czeisler CA. Circadian and sleep/wake dependent aspects of subjective alertness and cognitive performance. J Sleep Res. 1992;1:112–7. doi: 10.1111/j.1365-2869.1992.tb00021.x. [DOI] [PubMed] [Google Scholar]
- [58].Boivin DB, Czeisler CA, Dijk DJ, et al. Complex interaction of the sleep-wake cycle and circadian phase modulates mood in healthy subjects. Arch Gen Psychiatry. 1997;54:145–52. doi: 10.1001/archpsyc.1997.01830140055010. [DOI] [PubMed] [Google Scholar]
- [59].Cajochen C, Wyatt JK, Czeisler CA, et al. Separation of circadian and wake duration-dependent modulation of EEG activation during wakefulness. Neurosci. 2002;114:1047–60. doi: 10.1016/s0306-4522(02)00209-9. [DOI] [PubMed] [Google Scholar]
- [60].Duffy JF, Dijk DJ, Czeisler CA. Circadian and homeostatic modulation of cognitive throughput in older subjects. Sleep. 1998;21:301. [Google Scholar]
- [61].Johnson MP, Duffy JF, Dijk DJ, et al. Short-term memory, alertness and performance: A reappraisal of their relationship to body temperature. J Sleep Res. 1992;1:24–9. doi: 10.1111/j.1365-2869.1992.tb00004.x. [DOI] [PubMed] [Google Scholar]
- [62].Silva EJ, Wang W, Ronda JM, et al. Circadian and wake-dependent influences on subjective sleepiness, cognitive throughput, and reaction time performance in older and young adults. Sleep. 2010;33:481–90. doi: 10.1093/sleep/33.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Lee JH, Wang W, Silva EJ, et al. Neurobehavioral performance in young adults living on a 28-h day for 6 weeks. Sleep. 2009;32:905–13. doi: 10.1093/sleep/32.7.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Czeisler CA, Duffy JF, Shanahan TL, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284:2177–81. doi: 10.1126/science.284.5423.2177. [DOI] [PubMed] [Google Scholar]
- [65].Campbell SS, Dawson D, Zulley J. When the human circadian system is caught napping: evidence for endogenous rhythms close to 24 hours. Sleep. 1993;16:638–40. [PubMed] [Google Scholar]
- [66].Middleton B, Arendt J, Stone BM. Human circadian rhythms in constant dim light (8 lux) with knowledge of clock time. J Sleep Res. 1996;5:69–76. doi: 10.1046/j.1365-2869.1996.d01-67.x. [DOI] [PubMed] [Google Scholar]
- [67].Hiddinga AE, Beersma DGM, van den Hoofdakker RH. Endogenous and exogenous components in the circadian variation of core body temperature in humans. J Sleep Res. 1997;6:156–63. doi: 10.1046/j.1365-2869.1997.00047.x. [DOI] [PubMed] [Google Scholar]
- [68].Carskadon MA, Labyak SE, Acebo C, et al. Intrinsic circadian period of adolescent humans measured in conditions of forced desynchrony. Neurosci Lett. 1999;260:129–32. doi: 10.1016/s0304-3940(98)00971-9. [DOI] [PubMed] [Google Scholar]
- [69].Smith MR, Burgess HJ, Fogg LF, et al. Racial differences in the human endogenous circadian period. PLoS ONE. 2009;4:e6014. doi: 10.1371/journal.pone.0006014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Duffy JF, Cain SW, Chang AM, et al. Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc Nat Acad Sci. 2011;108:15602–8. doi: 10.1073/pnas.1010666108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Czeisler CA, Kronauer RE, Allan JS, et al. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science. 1989;244:1328–33. doi: 10.1126/science.2734611. [DOI] [PubMed] [Google Scholar]
- [72].Khalsa SBS, Jewett ME, Cajochen C, et al. A phase response curve to single bright light pulses in human subjects. J Physiol (Lond) 2003;549:945–52. doi: 10.1113/jphysiol.2003.040477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Wright KP, Jr., Gronfier C, Duffy JF, et al. Intrinsic period and light intensity determine the phase relationship between melatonin and sleep in humans. J Biol Rhythms. 2005;20:168–77. doi: 10.1177/0748730404274265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Mills JN, Minors DS, Waterhouse JM. Adaptation to abrupt time shifts of the oscillator[s] controlling human circadian rhythms. J Physiol (Lond) 1978;285:455–70. doi: 10.1113/jphysiol.1978.sp012582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Duffy JF, Dijk DJ. Getting through to circadian oscillators: Why use constant routines? J Biol Rhythms. 2002;17:4–13. doi: 10.1177/074873002129002294. [DOI] [PubMed] [Google Scholar]
- [76].Monk TH, Buysse DJ, Reynolds CF, III, et al. Circadian temperature rhythms of older people. Exp Gerontol. 1995;30:455–74. doi: 10.1016/0531-5565(95)00007-4. [DOI] [PubMed] [Google Scholar]
- [77].Lieberman HR, Wurtman JJ, Teicher MH. Circadian rhythms of activity in healthy young and elderly humans. Neurobiol Aging. 1989;10:259–65. doi: 10.1016/0197-4580(89)90060-2. [DOI] [PubMed] [Google Scholar]
- [78].Weitzman ED, Moline ML, Czeisler CA, et al. Chronobiology of aging: Temperature, sleep-wake rhythms and entrainment. Neurobiol Aging. 1982;3:299–309. doi: 10.1016/0197-4580(82)90018-5. [DOI] [PubMed] [Google Scholar]
- [79].Touitou Y, Sulon J, Bogdan A, et al. Adrenal circadian system in young and elderly human subjects: A comparative study. J Endocrinol. 1982;93:201–10. doi: 10.1677/joe.0.0930201. [DOI] [PubMed] [Google Scholar]
- [80].Sherman B, Wysham C, Pfohl B. Age-related changes in the circadian rhythm of plasma cortisol in man. J Clin Endocrinol Metab. 1985;61:439–43. doi: 10.1210/jcem-61-3-439. [DOI] [PubMed] [Google Scholar]
- [81].Sharma M, Palacios-Bois J, Schwartz G, et al. Circadian rhythms of melatonin and cortisol in aging. Biol Psychiatry. 1989;25:305–19. doi: 10.1016/0006-3223(89)90178-9. [DOI] [PubMed] [Google Scholar]
- [82].Czeisler CA, Dumont M, Duffy JF, et al. Association of sleep-wake habits in older people with changes in output of circadian pacemaker. Lancet. 1992;340:933–6. doi: 10.1016/0140-6736(92)92817-y. [DOI] [PubMed] [Google Scholar]
- [83].Carrier J, Monk TH, Reynolds CF, III, et al. Are age differences in sleep due to phase differences in the output of the circadian timing system? Chronobiol Int. 1999;16:79–91. doi: 10.3109/07420529908998714. [DOI] [PubMed] [Google Scholar]
- [84].Carrier J, Paquet J, Morettini J, et al. Phase advance of sleep and temperature circadian rhythms in the middle years of life in humans. Neurosci Lett. 2002;320:1–4. doi: 10.1016/s0304-3940(02)00038-1. [DOI] [PubMed] [Google Scholar]
- [85].Kim SJ, Benloucif S, Reid KJ, et al. Phase-shifting response to light in older adults. J Physiol. 2014;592:189–202. doi: 10.1113/jphysiol.2013.262899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Duffy JF, Zeitzer JM, Rimmer DW, et al. Peak of circadian melatonin rhythm occurs later within the sleep of older subjects. Am J Physiol. 2002;282:E297–E303. doi: 10.1152/ajpendo.00268.2001. [DOI] [PubMed] [Google Scholar]
- [87].Lewy AJ, Bauer VK, Singer CM, et al. Later circadian phase of plasma melatonin relative to usual waketime in older subjects. Sleep. 2000;23:A188–A9. [Google Scholar]
- [88].Tozawa T, Mishima K, Satoh K, et al. Stability of sleep timing against the melatonin secretion rhythm with advancing age: clinical implications. J Clin Endocrinol Metab. 2003;88:4689–95. doi: 10.1210/jc.2003-030147. [DOI] [PubMed] [Google Scholar]
- [89].Van Cauter E, Leproult R, Kupfer DJ. Effects of gender and age on the levels and circadian rhythmicity of plasma cortisol. J Clin Endocrinol Metab. 1996;81:2468–73. doi: 10.1210/jcem.81.7.8675562. [DOI] [PubMed] [Google Scholar]
- [90].Kripke DF, Elliott JA, Youngstedt SD, et al. Circadian phase response curves to light in older and young women and men. J Circadian Rhythms. 2007;5:4. doi: 10.1186/1740-3391-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Pittendrigh CS, Daan S. A functional analysis of circadian pacemakers in nocturnal rodents. IV. Entrainment: Pacemaker as clock. J Comp Physiol [A] 1976;106:291–331. [Google Scholar]
- [92].Zee PC, Rosenberg RS, Turek FW. Effects of aging on entrainment and rate of resynchronization of circadian locomotor activity. Am J Physiol. 1992;263:R1099–R103. doi: 10.1152/ajpregu.1992.263.5.R1099. [DOI] [PubMed] [Google Scholar]
- [93].Scarbrough K, Losee-Olson S, Wallen EP, et al. Aging and photoperiod affect entrainment and quantitative aspects of locomotor behavior in Syrian hamsters. A J Physiol. 1997;272:R1219–R25. doi: 10.1152/ajpregu.1997.272.4.R1219. [DOI] [PubMed] [Google Scholar]
- [94].Valentinuzzi VS, Scarbrough K, Takahashi JS, et al. Effects of aging on the circadian rhythm of wheel-running activity in C57BL/6 mice. Am J Physiol. 1997;273:R1957–R64. doi: 10.1152/ajpregu.1997.273.6.R1957. [DOI] [PubMed] [Google Scholar]
- [95].Buysse DJ, Monk TH, Carrier J, et al. Circadian patterns of sleep, sleepiness, and performance in older and younger adults. Sleep. 2005;28:1365–76. doi: 10.1093/sleep/28.11.1365. [DOI] [PubMed] [Google Scholar]
- [96].Münch M, Knoblauch V, Blatter K, et al. Age-related attenuation of the evening circadian arousal signal in humans. Neurobiol Aging. 2005;26:1307–19. doi: 10.1016/j.neurobiolaging.2005.03.004. [DOI] [PubMed] [Google Scholar]
- [97].Yoon IY, Kripke DF, Elliott JA, et al. Age-related changes of circadian rhythms and sleep-wake cycles. J Am Geriatr Soc. 2003;51:1085–91. doi: 10.1046/j.1532-5415.2003.51356.x. [DOI] [PubMed] [Google Scholar]
- [98].Davis FC, Viswanathan N. Stability of circadian timing with age in Syrian hamsters. Am J Physiol. 1998;275:R960–R8. doi: 10.1152/ajpregu.1998.275.4.R960. [DOI] [PubMed] [Google Scholar]
- [99].Duffy JF, Viswanathan N, Davis FC. Free-running circadian period does not shorten with age in female Syrian hamsters. Neurosci Lett. 1999;271:77–80. doi: 10.1016/s0304-3940(99)00519-4. [DOI] [PubMed] [Google Scholar]
- [100].Penev P, Zee P, Turek FW. Quantitative analysis of the age-related fragmentation of hamster 24-h activity rhythms. Am J Physiol. 1997;273:R2132–R7. doi: 10.1152/ajpregu.1997.273.6.R2132. [DOI] [PubMed] [Google Scholar]
- [101].Satinoff E, Li H, Tcheng TK, et al. Do the suprachiasmatic nuclei oscillate in old rats as they do in young ones? Am J Physiol. 1993;265:R1216–R22. doi: 10.1152/ajpregu.1993.265.5.R1216. [DOI] [PubMed] [Google Scholar]
- [102].Watanabe A, Shibata S, Watanabe S. Circadian rhythm of spontaneous neuronal activity in the suprachiasmatic nucleus of old hamster in vitro. Brain Res. 1995;695:237–9. doi: 10.1016/0006-8993(95)00713-z. [DOI] [PubMed] [Google Scholar]
- [103].Nakamura TJ, Nakamura W, Yamazaki S, et al. Age-related decline in circadian output. J Neurosci. 2011;31:10201–5. doi: 10.1523/JNEUROSCI.0451-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Farajnia S, Michel S, Deboer T, et al. Evidence for neuronal desynchrony in the aged suprachiasmatic nucleus clock. J Neurosci. 2012;32:5891–9. doi: 10.1523/JNEUROSCI.0469-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Carrier J, Monk TH, Buysse DJ, et al. Amplitude reduction of the circadian temperature and sleep rhythms in the elderly. Chronobiol Int. 1996;13:373–86. doi: 10.3109/07420529609012661. [DOI] [PubMed] [Google Scholar]
- [106].Zeitzer JM, Daniels JE, Duffy JF, et al. Do plasma melatonin concentrations decline with age? Am J Med. 1999;107:432–6. doi: 10.1016/s0002-9343(99)00266-1. [DOI] [PubMed] [Google Scholar]
- [107].Silva EJ, Cain SW, Munch MY, et al. Age-related differences in the effect of chronic sleep restriction on sleep quality. Sleep. 2011;34:A24. [Google Scholar]
- [108].Cain SW, Silva EJ, Munch MY, et al. Chronic sleep restriction impairs reaction time performance more in young than in older subjects. Sleep. 2010;33:A85. [Google Scholar]
- [109].Zitting K-M, Cain SW, Munch MY, et al. Objective sleepiness in young and older adults during 3-weeks of chronic sleep restriction. J Sleep Res. 2014;23:269. [Google Scholar]
- [110].Pittendrigh CS, Daan S. Circadian oscillations in rodents: A systematic increase of their frequency with age. Science. 1974;186:548–50. doi: 10.1126/science.186.4163.548. [DOI] [PubMed] [Google Scholar]
- [111].Morin LP. Age-related changes in hamster circadian period, entrainment, and rhythm splitting. J Biol Rhythms. 1988;3:237–48. [Google Scholar]
- [112].Rosenberg RS, Zee PC, Turek FW. Phase response curves to light in young and old hamsters. Am J Physiol. 1991;261:R491–R5. doi: 10.1152/ajpregu.1991.261.2.R491. [DOI] [PubMed] [Google Scholar]
- [113].Kendall AR, Lewy AJ, Sack RL. Effects of aging on the intrinsic circadian period of totally blind humans. J Biol Rhythms. 2001;16:87–95. doi: 10.1177/074873040101600110. [DOI] [PubMed] [Google Scholar]
- [114].Duffy JF, Czeisler CA. Effect of light on human circadian physiology. Sleep Med Clin. 2009;4:165–77. doi: 10.1016/j.jsmc.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Kelly TL, Neri DF, Grill JT, et al. Nonentrained circadian rhythms of melatonin in submariners scheduled to an 18-hour day. J Biol Rhythms. 1999;14:190–6. doi: 10.1177/074873099129000597. [DOI] [PubMed] [Google Scholar]
- [116].Orth DN, Besser GM, King PH, et al. Free-running circadian plasma cortisol rhythm in a blind human subject. Clin Endocrinol (Oxf) 1979;10:603–17. doi: 10.1111/j.1365-2265.1979.tb02120.x. [DOI] [PubMed] [Google Scholar]
- [117].Jean-Louis G, Kripke DF, Ancoli-Israel S, et al. Circadian sleep, illumination, and activity patterns in women: Influences of aging and time reference. Physiol Behav. 2000;68:347–52. doi: 10.1016/s0031-9384(99)00186-9. [DOI] [PubMed] [Google Scholar]
- [118].Guillemette J, Hébert M, Paquet J, et al. Natural bright light exposure in the summer and winter in subjects with and without complaints of seasonal mood variations. Biol Psychiatry. 1998;44:622–8. doi: 10.1016/s0006-3223(97)00543-x. [DOI] [PubMed] [Google Scholar]
- [119].Cole RJ, Kripke DF, Wisbey J, et al. Seasonal variation in human illumination exposure at two different latitudes. J Biol Rhythms. 1995;10:324–34. doi: 10.1177/074873049501000406. [DOI] [PubMed] [Google Scholar]
- [120].Burgess HJ, Eastman CI. Early versus late bedtimes phase shift the human dim light melatonin rhythm despite a fixed morning lights on time. Neurosci Lett. 2004;356:115–8. doi: 10.1016/j.neulet.2003.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96:E463–E72. doi: 10.1210/jc.2010-2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Santhi N, Thorne HC, van der Veen DR, et al. The spectral composition of evening light and individual differences in the suppression of melatonin and delay of sleep in humans. J Pineal Res. 2011;53:47–59. doi: 10.1111/j.1600-079X.2011.00970.x. [DOI] [PubMed] [Google Scholar]
- [123].Chang AM, Aeschbach D, Duffy JF, et al. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci. 2015;112:1232–7. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Scheuermaier K, Laffan AM, Duffy JF. Light exposure patterns in healthy older and young adults. J Biol Rhythms. 2010;25:113–22. doi: 10.1177/0748730410361916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [125].Kawinska A, Dumont M, Selmaoui B, et al. Are modifications of melatonin circadian rhythm in the middle years of life related to habitual patterns of light exposure? J Biol Rhythms. 2005;20:451–60. doi: 10.1177/0748730405280248. [DOI] [PubMed] [Google Scholar]
- [126].Klerman EB, Duffy JF, Dijk DJ, et al. Circadian phase resetting in older people by ocular bright light exposure. J Investig Med. 2001;49:30–40. doi: 10.2310/6650.2001.34088. [DOI] [PubMed] [Google Scholar]
- [127].Benloucif S, Green K, L'Hermite-Balériaux M, et al. Responsiveness of the aging circadian clock to light. Neurobiol Aging. 2006;27:1870–9. doi: 10.1016/j.neurobiolaging.2005.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128].Duffy JF, Zeitzer JM, Czeisler CA. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol Aging. 2007;28:799–807. doi: 10.1016/j.neurobiolaging.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [129].Herljevic M, Middleton B, Thapan K, et al. Light-induced melatonin suppression: age-related reduction in response to short wavelength light. Exp Gerontol. 2005;40:237–42. doi: 10.1016/j.exger.2004.12.001. [DOI] [PubMed] [Google Scholar]
- [130].Sletten TL, Revell VL, Middleton B, et al. Age-related changes in acute and phase-advancing responses to monochromatic light. J Biol Rhythms. 2009;24:73–84. doi: 10.1177/0748730408328973. [DOI] [PubMed] [Google Scholar]
- [131].Najjar RP, Chiquet C, Teikari P, et al. Aging of non-visual spectral sensitivity to light in humans: compensatory mechanisms? PLoS ONE. 2014;9:e85837. doi: 10.1371/journal.pone.0085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Brainard GC, Rollag MD, Hanifin JP. Photic regulation of melatonin in humans: Ocular and neural signal transduction. J Biol Rhythms. 1997;12:537–46. doi: 10.1177/074873049701200608. [DOI] [PubMed] [Google Scholar]
- [133].Barker FM, Brainard GC, Dayhaw-Barker P. Transmittance of the human lens as a function of age. ARVO Annual Meeting Abstracts. 1991 [Google Scholar]
- [134].Zhang Y, Brainard GC, Zee PC, et al. Effects of aging on lens transmittance and retinal input to the suprachiasmatic nucleus in golden hamsters. Neurosci Lett. 1998;258:167–70. doi: 10.1016/s0304-3940(98)00887-8. [DOI] [PubMed] [Google Scholar]
- [135].Kessel L, Siganos G, Jorgensen T, et al. Sleep disturbances are related to decreased transmission of blue light to the retina caused by lens yellowing. Sleep. 2011;34:1215–9. doi: 10.5665/SLEEP.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Daneault V, Vandewalle G, Hebert M, et al. Does pupil constriction under blue and green monochromatic light exposure change with age? J Biol Rhythms. 2012;27:257–64. doi: 10.1177/0748730412441172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Freund PR, Watson J, Gilmour GS, et al. Differential changes in retina function with normal aging in humans. Doc Ophthalmol. 2011;122:177–90. doi: 10.1007/s10633-011-9273-2. [DOI] [PubMed] [Google Scholar]
- [138].Gerth C, Garcia SM, Ma L, et al. Multifocal electroretinogram: age-related changes for different luminance levels. Graefes Arch Clin Exp Ophthalmol. 2002;240:202–8. doi: 10.1007/s00417-002-0442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139].Semo M, Lupi D, Peirson SN, et al. Light-induced c-fos in melanopsin retinal ganglion cells of young and aged rodless/coneless (rd/rd cl) mice. Eur J Neurosci. 2003;18:3007–17. doi: 10.1111/j.1460-9568.2003.03061.x. [DOI] [PubMed] [Google Scholar]
- [140].Semo M, Peirson S, Lupi D, et al. Melanopsin retinal ganglion cells and the maintenance of circadian and pupillary responses to light in aged rodless/coneless (rd/rd cl) mice. Eur J Neurosci. 2003;17:1793–801. doi: 10.1046/j.1460-9568.2003.02616.x. [DOI] [PubMed] [Google Scholar]
- [141].Gibson EM, Williams WP, 3rd, Kriegsfeld LJ. Aging in the circadian system: considerations for health, disease prevention and longevity. Exp Gerontol. 2009;44:51–6. doi: 10.1016/j.exger.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [142].Cai A, Scarbrough K, Hinkle DA, et al. Fetal grafts containing suprachiasmatic nuclei restore the diurnal rhythm of CRH and POMC mRNA in aging rats. Am J Physiol. 1997;273:R1764–70. doi: 10.1152/ajpregu.1997.273.5.R1764. [DOI] [PubMed] [Google Scholar]
- [143].Hurd MW, Zimmer KA, Lehman MN, et al. Circadian locomotor rhythms in aged hamsters following suprachiasmatic transplant. Am J Physiol. 1995;269:R958–R68. doi: 10.1152/ajpregu.1995.269.5.R958. [DOI] [PubMed] [Google Scholar]
- [144].Viswanathan N, Davis FC. Suprachiasmatic nucleus grafts restore circadian function in aged hamsters. Brain Res. 1995;686:10–6. doi: 10.1016/0006-8993(95)00423-n. [DOI] [PubMed] [Google Scholar]
- [145].Van Reeth O, Zhang Y, Zee PC, et al. Grafting fetal suprachiasmatic nuclei in the hypothalamus of old hamsters restores responsiveness of the circadian clock to a phase shifting stimulus. Brain Res. 1994;643:338–42. doi: 10.1016/0006-8993(94)90044-2. [DOI] [PubMed] [Google Scholar]
- [146].Farajnia S, Meijer JH, Michel S. Age-related changes in large-conductance calcium-activated potassium channels in mammalian circadian clock neurons. Neurobiol Aging. 2015;36:2176–83. doi: 10.1016/j.neurobiolaging.2014.12.040. [DOI] [PubMed] [Google Scholar]
- [147].Madeira MD, Sousa N, Santer RM, et al. Age and sex do not affect the volume, cell numbers, or cell size of the suprachiasmatic nucleus of the rat: An unbiased stereological study. J Comp Neurol. 1995;361:585–601. doi: 10.1002/cne.903610404. [DOI] [PubMed] [Google Scholar]
- [148].Roozendaal B, van Gool WA, Swaab DF, et al. Changes in vasopressin cells of the rat suprachiasmatic nucleus with aging. Brain Res. 1987;409:259–64. doi: 10.1016/0006-8993(87)90710-4. [DOI] [PubMed] [Google Scholar]
- [149].Swaab DF, Fliers E, Partiman TS. The suprachiasmatic nucleus of the human brain in relation to sex, age and senile dementia. Brain Res. 1985;342:37–44. doi: 10.1016/0006-8993(85)91350-2. [DOI] [PubMed] [Google Scholar]
- [150].Hofman MA, Swaab DF. Living by the clock: The circadian pacemaker in older people. Ageing Res Rev. 2006;5:33–51. doi: 10.1016/j.arr.2005.07.001. [DOI] [PubMed] [Google Scholar]
- [151].Kawakami F, Okamura H, Tamada Y, et al. Loss of day-night differences in VIP mRNA levels in the suprachiasmatic nucleus of aged rats. Neurosci Lett. 1997;222:99–102. doi: 10.1016/s0304-3940(97)13355-9. [DOI] [PubMed] [Google Scholar]
- [152].Chee CA, Roozendaal B, Swaab DF, et al. Vasoactive intestinal polypeptide neuron changes in the senile rat suprachiasmatic nucleus. Neurobiol Aging. 1988;9:307–12. doi: 10.1016/s0197-4580(88)80070-8. [DOI] [PubMed] [Google Scholar]
- [153].Hofman MA, Fliers E, Goudsmit E, et al. Morphometric analysis of the suprachiasmatic and paraventricular nuclei in the human brain: Sex differences and age-dependent changes. J Anat. 1988;160:127–43. [PMC free article] [PubMed] [Google Scholar]
- [154].Aujard F, Cayetanot F, Bentivoglio M, et al. Age-related effects on the biological clock and its behavioral output in a primate. Chronobiol Int. 2006;23:451–60. doi: 10.1080/07420520500482090. [DOI] [PubMed] [Google Scholar]
- [155].Wang JL, Lim AS, Chiang WY, et al. Suprachiasmatic neuron numbers and rest-activity circadian rhythms in older humans. Ann Neurol. 2015;78:317–22. doi: 10.1002/ana.24432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Duncan MJ, Herron JM, Hill SA. Aging selectively suppresses vasoactive intestinal peptide messenger RNA expression in the suprachiasmatic nucleus of the Syrian hamster. Molecular Brain Res Mol Brain Res. 2001;87:196–203. doi: 10.1016/s0169-328x(01)00015-8. [DOI] [PubMed] [Google Scholar]
- [157].Zhou J-N, Hofman MA, Swaab DF. VIP neurons in the human SCN in relation to sex, age, and Alzheimer's disease. Neurobiol Aging. 1995;16:571–6. doi: 10.1016/0197-4580(95)00043-e. [DOI] [PubMed] [Google Scholar]
- [158].Krajnak K, Kashon ML, Rosewell KL, et al. Aging alters the rhythmic expression of vasoactive intestinal polypeptide mRNA but not arginine vasopressin mRNA in the suprachiasmatic nuclei of female rats. J Neurosci. 1998;18:4767–74. doi: 10.1523/JNEUROSCI.18-12-04767.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].Kolker DE, Fukuyama H, Huang DS, et al. 2003;18:159–69. doi: 10.1177/0748730403251802. [DOI] [PubMed] [Google Scholar]
- [160].Weinert D, Weinert H, Schurov I, et al. Impaired expression of the mPer2 circadian clock gene in the suprachiasmatic nuclei of aging mice. Chronobiol Int. 2001;18:559–65. doi: 10.1081/cbi-100103976. [DOI] [PubMed] [Google Scholar]
- [161].Bonaconsa M, Malpeli G, Montaruli A, et al. Differential modulation of clock gene expression in the suprachiasmatic nucleus, liver and heart of aged mice. Exp Gerontol. 2014;55:70–9. doi: 10.1016/j.exger.2014.03.011. [DOI] [PubMed] [Google Scholar]
- [162].Schrader H, Bovim G, Sand T. The prevalence of delayed and advanced sleep phase syndromes. J Sleep Res. 1993;2:51–5. doi: 10.1111/j.1365-2869.1993.tb00061.x. [DOI] [PubMed] [Google Scholar]
- [163].Sack RL, Auckley D, Auger RR, et al. Circadian rhythm sleep disorders: Part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. An American Academy of Sleep Medicine review. Sleep. 2007;30:1484–501. doi: 10.1093/sleep/30.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Sack RL, Auckley D, Auger RR, et al. Circadian rhythm sleep disorders: Part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep. 2007;30:1460–83. doi: 10.1093/sleep/30.11.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [165].Ftouni S, Sletten TL, Barger LK, et al. Shift Work Disorder. In: Barkoukis T, Matheson JK, Ferber R, Doghramji K, editors. Therapy in Sleep Medicine. Elsevier; Amsterdam: 2011. pp. 411–24. [Google Scholar]
- [166].Duffy JF. Shift work and aging: Roles of sleep and circadian rhythms. Clin Occup Environ Med. 2003;3:311–32. [Google Scholar]
- [167].Härmä MI, Hakola T, Åkerstedt T, et al. Age and adjustment to night work. Occup Environ Med. 1994;51:568–73. doi: 10.1136/oem.51.8.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Marquié JC, Foret J. Sleep, age, and shiftwork experience. J Sleep Res. 1999;8:297–304. doi: 10.1046/j.1365-2869.1999.00170.x. [DOI] [PubMed] [Google Scholar]
- [169].Åkerstedt T, Torsvall L. Age, sleep and adjustment to shiftwork. In: Koella WP, editor. Sleep. S. Karger; Basel: 1980. 1981. pp. 190–5. [Google Scholar]
- [170].Zee PC, Vitiello MV. Circadian Rhythm Sleep Disorder: Irregular Sleep Wake Rhythm Type. Sleep Med Clin. 2009;4:213–8. doi: 10.1016/j.jsmc.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Ancoli-Israel S, Parker L, Sinaee R, et al. Sleep fragmentation in patients from a nursing home. J Gerontol. 1989;44:M18–M21. doi: 10.1093/geronj/44.1.m18. [DOI] [PubMed] [Google Scholar]
- [172].Mirmiran M, Swaab DF, Kok JH, et al. Circadian rhythms and the suprachiasmatic nucleus in perinatal development, aging and Alzheimer's disease. Prog Brain Res. 1992;93:151–63. doi: 10.1016/s0079-6123(08)64570-7. [DOI] [PubMed] [Google Scholar]
- [173].Witting W, Kwa IH, Eikelenboom P, et al. Alterations in the circadian rest-activity rhythm in aging and alzheimer's disease. Biol Psychiatry. 1990;27:563–72. doi: 10.1016/0006-3223(90)90523-5. [DOI] [PubMed] [Google Scholar]
- [174].van Someren EJW, Hagebeuk EEO, Lijzenga C, et al. Circadian rest-activity rhythm disturbances in Alzheimer's disease. Biol Psychiatry. 1996;40:259–70. doi: 10.1016/0006-3223(95)00370-3. [DOI] [PubMed] [Google Scholar]
- [175].Campbell SS, Kripke DF, Gillin JC, et al. Exposure to light in healthy elderly subjects and Alzheimer's patients. Physiol Behav. 1988;42:141–4. doi: 10.1016/0031-9384(88)90289-2. [DOI] [PubMed] [Google Scholar]
- [176].Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep. 1997;20:18–23. [PubMed] [Google Scholar]
- [177].Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res. 2000;9:373–9. doi: 10.1046/j.1365-2869.2000.00221.x. [DOI] [PubMed] [Google Scholar]
- [178].Ancoli-Israel S, Gehrman P, Martin JL, et al. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer's disease patients. Behav Sleep Med. 2003;1:22–36. doi: 10.1207/S15402010BSM0101_4. [DOI] [PubMed] [Google Scholar]
- [179].van Someren EJW, Kessler A, Mirmiran M, et al. Indirect bright light improves circadian rest-activity rhythm disturbances in demented patients. Biol Psychiatry. 1997;41:955–63. doi: 10.1016/S0006-3223(97)89928-3. [DOI] [PubMed] [Google Scholar]
- [180].Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: A randomized controlled trial. JAMA. 2008;299:2642–55. doi: 10.1001/jama.299.22.2642. [DOI] [PubMed] [Google Scholar]