Abstract
Purpose
The aim of this study was to assess the influence of position of mandibular 3rd molar on angle and condylar fractures.
Materials and Methods
Panoramic radiographs were used to determine the mandibular fracture patterns based on the presence or absence of the third molar.
Results
Of the 64 patients with mandibular fractures, condyle and angle fractures were found to be 67 and 33 % respectively. The greatest percentage (75 %) of condylar fractures were associated with erupted third molar teeth, and 25 % had impacted teeth. Subcondylar region was found to be the most common site that predisposes to fracture. Moderate force lead to condylar fracture when third molar is erupted or absent and mild force showed angle fracture when third molar is impacted. Increased incidence of angle fracture was observed when tooth is in mesioangular and distoangular position.
Conclusion
Impacted mandibular 3rd molar leads to an increased risk of angle fracture and decreased risk of condylar fracture especially when they are more deeply seated.
Keywords: Mandibular impacted 3rd molar, Condyle fracture, Angle fracture, Pedersen difficulty index
Introduction
Mandible is perceived to be one of the strongest and most rigid bone of the facial skeleton. It often leads to fracture at various sites and accounts for 40–65 % of all facial fractures [1]. Fractures of angle (25–33 %) and condyle (26 %) share almost an equal weightage in sites of mandible [1]. Patterns of fracture largely depend on multiple clinical factors, as the size of the object, direction, nature and surface area of the impacting force. Other contributing factors include presence of soft tissue bulk and biomechanical characteristics of the mandible [2, 3].
The weight of evidence in support of increased risk of mandibular angle fracture in the presence or absence of unerupted or impacted third molars is overwhelming [1, 2, 4–6]. However, it will be sheer folly to rely on the current evidence to confirm the relationship between 3rd molar position and the risk of angle and condyle fractures.
There is scanty evidence in proving the influence of impacted third molar on angle and condyle fractures [1, 2, 7, 8]. Very few of them emphasised on the influence of position, severity of impaction, injury mechanism and injury cause on angle and condyle fractures along with other associated facial fractures [1, 7]. Purpose of this study was to assess the influence of the presence, position of third molar and the severity of impacted third molars. Injury mechanism on the incidence and frequency of mandibular angle and condyle fractures were evaluated.
Materials and Methods
From January 2010 to January 2014, patients who were diagnosed with mandibular fractures and treated with open reduction and internal fixation in our unit were selected. This study included 64 patients who were diagnosed with condylar or angle fractures. The case records of these patients were collected and retrospectively reviewed. Data included age, sex, etiological factor, the presence and position of the lower third molars, and the anatomical location of the mandible fracture.
For this study, the magnitude of trauma force was categorised based on the number of fracture sites. Low trauma force resulted in one mandibular fracture site. Moderate trauma force resulted in two mandibular fracture sites and high trauma force resulted in three or more mandibular fracture sites.
Taking Winter’s classification [9] into consideration impacted molars were classified into mesioangular, distoangular, vertical, and horizontal. Relationship of the third molar to the ramus of the mandible was grouped according to the classification of Pell and Gregory [10]. The relative depth of the third molar was grouped according to the classification of Archer [11]. In the present study, as described by Dingman and Natvig the mandible was divided into six regions which include condylar process, ramus, angle, body, symphysis and parasymphysis. Mandibular angle fracture was determined by the definition given by Kelly and Harrigan [12]. Condylar fracture was divided into three categories—head, subcondylar and neck. From the obtained information the patients were divided into three groups based on status of the 3rd molar into group I (erupted), group II (unerupted) and group III (absent).
Results
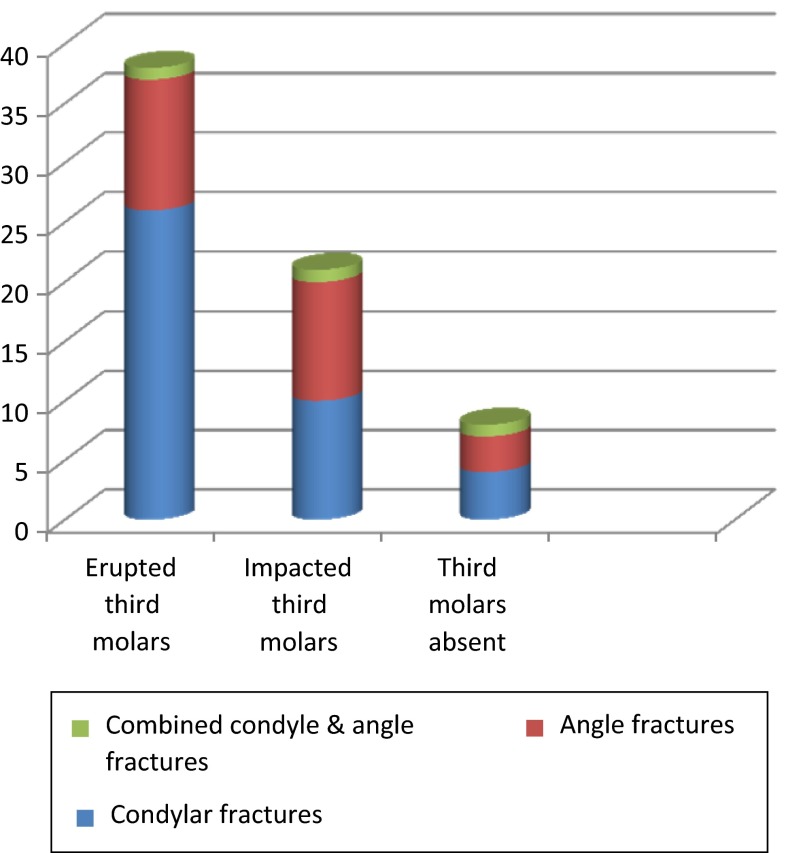
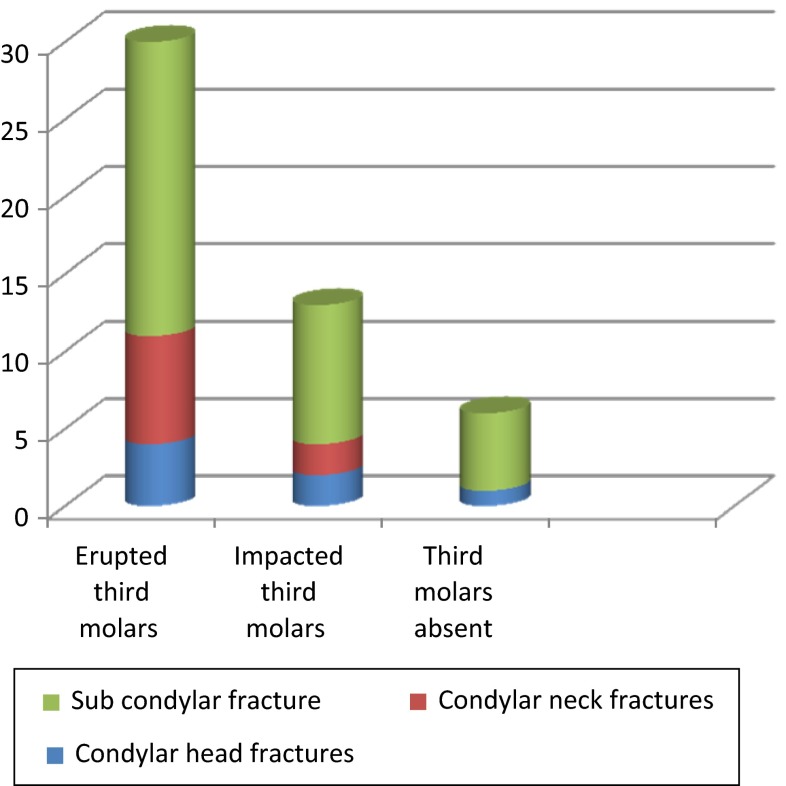
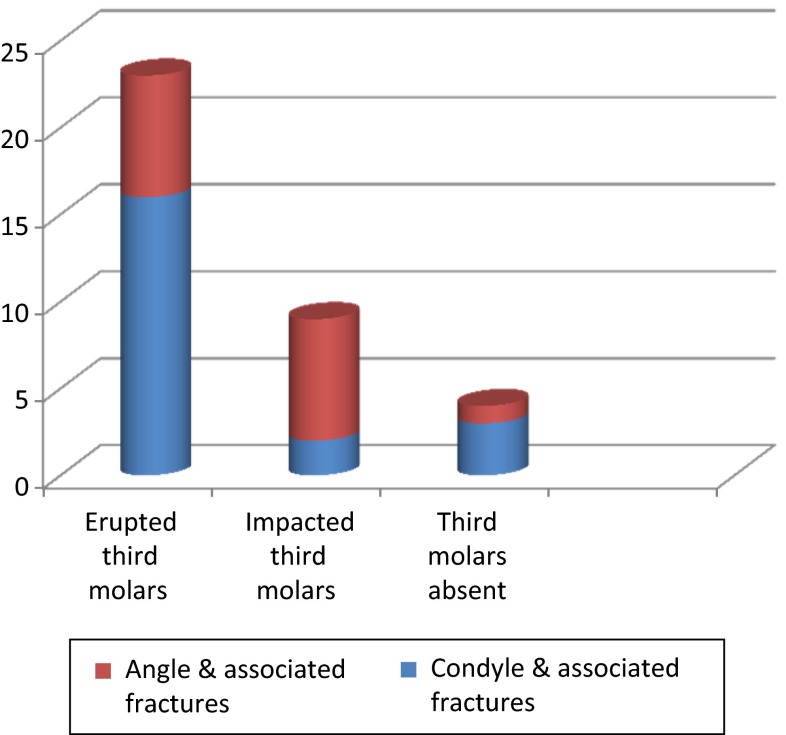
The study comprised of 64 patients with 109 mandibular fracture sites. This included 56 male and 8 female patients with an age range between 16 and 69 years. Road traffic accident was the most common reason for mandibular fracture in 56 patients (80 %), followed by assault 8(11 %), fall 5(6 %) and others 6(8 %). Majority of the patients had fracture at two anatomical locations, group consisting of 41 patients (64 %). In decreasing order the other groups were isolated fracture with 19 patients (29 %) and fractures at multiple locations with 4 patients (6 %). Fractures of the mandibular condyle were observed most frequently (33 %), followed by angle (25 %), parasymphysis (23 %) and body (10 %). Mandibular angle fractures were seen in 23 patients out of which 1 patient had bilateral angle fracture. Condylar fractures were observed in 43 patients among whom 7 had bilateral condylar fractures. Three patients had combined condylar and angle fracture (Table 1; Fig. 1). In condylar fractures, subcondylar takes the prime position (64 %), followed by neck (20 %) and head (16 %) (Table 2; Fig. 2). Most of the patients with associated fractures along with condyle were found to be in group I. Patients with angle and other associated fractures were found to be equal in groups I and II and less in group III (Table 3; Fig. 3).
Table 1.
Relation of third molars to fracture
| Condyle | Angle | |||
|---|---|---|---|---|
| Unilateral | Bilateral | Unilateral | Bilateral | |
| Group I | 22 | 4 | 11 | 0 |
| Group II | 8 | 2 | 9 | 1 |
| Group III | 3 | 1 | 3 | 0 |
| p value | 0.87; NS | 0.481; NS | ||
| Unilateral | Bilateral | |||
|---|---|---|---|---|
| Condyle | Angle | Condyle | Angle | |
| Group I | 22 | 11 | 4 | 0 |
| Group II | 8 | 9 | 2 | 1 |
| Group III | 3 | 3 | 1 | 0 |
| p value | 0.367; NS | 0.386; NS | ||
Group I—Erupted 3rd molar; group II—impacted 3rd molar; group III—3rd molar is absent
Fig. 1.
Relation of third molars to fracture
Table 2.
Relation of third molars to level of condylar fracture
| Head | Neck | Subcondylar | |
|---|---|---|---|
| Group I | 4 | 7 | 19 |
| Group II | 2 | 2 | 9 |
| Group III | 1 | 0 | 5 |
p = 0.749
Fig. 2.
Relation of third molars to level of condylar fracture
Table 3.
Relation of third molars to other associated fractures
| Condyle + other associated fractures | Angle + other associated fractures | |
|---|---|---|
| Group I | 16 | 7 |
| Group II | 2 | 7 |
| Group III | 3 | 1 |
| Total | 21 | 15 |
p = 0.039; Sig
Fig. 3.
Relation of third molars to other associated fractures
Out of 64 patients, 37 patients had fully erupted third molars, 20 patients had impacted 3rd molars and 7 patients had missing third molars. Pertaining to the 20 patients with impacted teeth, the severity of impaction is as follows: mesioangular 10(50 %), followed by distoangular 7(35 %), vertical 2(10 %), horizontal 1(5 %). The most frequent position was class II 19(95 %) followed by class I (5 %). With respect to the level of impacted third molar: position A 13(65 %), followed by position B 6(30 %), position C 1(5 %). We found that mandibular angle is more prone to fracture when a third molar is in mesioangular, class II, position A.
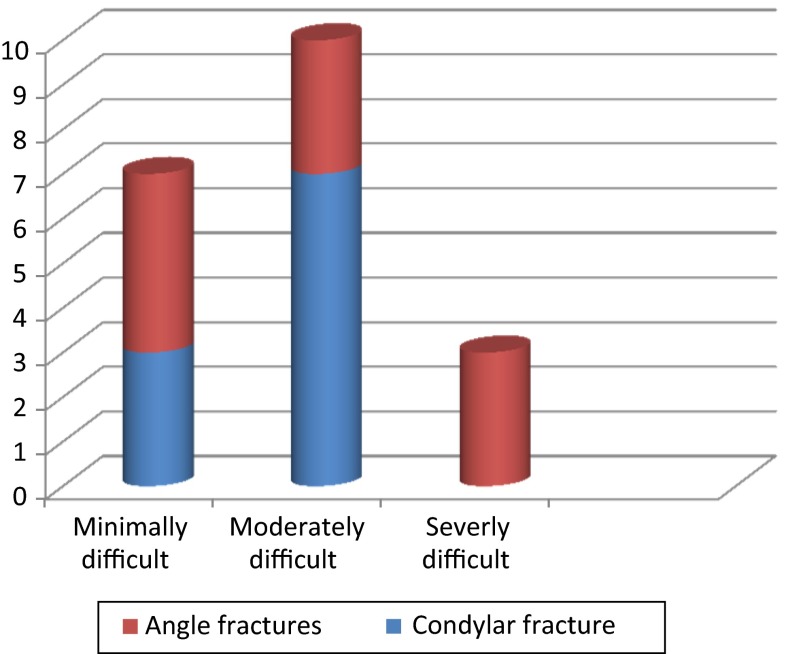
Pedersen difficulty index was taken into consideration to assess the final position and severity of impaction. It was noticed that even an impacted tooth with minimal difficulty led to the angle fracture (Table 4; Fig. 4). Patients in group II were statistically younger and more likely to be male than patients in groups I and III. Patients sustaining condylar fractures were older and more likely to be male than those without condylar fractures. Collectively the data revealed that patients in groups I and III had a higher risk of sustaining condylar fractures than patients in group II. In angle fractures it was found to be vice versa.
Table 4.
Fracture related to Pedersen’s difficulty index for impacted third molars
| Difficulty index (Pedersen Scale) | Condyle | Angle |
|---|---|---|
| Minimally difficult | 3 | 4 |
| Moderately difficult | 7 | 3 |
| Severe difficult | 0 | 3 |
p = 0.093; NS
Fig. 4.
Fracture related to Pedersen’s difficulty index for impacted third molars
With respect to injury mechanism, the impacted forces were categorically identified to be mild, moderate and severe (Table 5). Where mild force included patients with isolated fracture site, moderate force included patients with two fracture sites and severe force included patients with more than two fracture sites. Patients in groups I and III had a higher risk of condylar fractures and a lower risk of angle fractures and patients in group II had a lower risk of condylar fracture and a higher risk of angle fracture when impacted by moderate force. In contrary, patients in group II had a higher risk of angle fracture than groups I and III, when injured by mild force, whereas the difference was not statistically significant for condylar fractures. Patients with or without impacted 3rd molars showed no statistically significant difference when injured by severe force.
Table 5.
Relation between injury mechanism and fracture pattern
| Condyle | Angle | |||||
|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Mild | Moderate | Severe | |
| Group I | 7 | 19 | 1 | 4 | 5 | 2 |
| Group II | 6 | 4 | 0 | 2 | 7 | 0 |
| Group III | 1 | 3 | 0 | 1 | 1 | 1 |
| p value | 0.372; NS | 0.417; NS | ||||
Discussion
This study was intended to relate the association between mandibular 3rd molar position to angle and condylar fractures. Many clinical investigators stated that the risk of angle and condyle fractures depend on impacted 3rd molars [2, 4, 5, 13, 14]. Our results confirmed that there is an increased risk of angle fracture when impacted 3rd molars were present as well as there is a variable risk for angle to fracture which depends on 3rd molar position. The results of this study revealed that injury mechanism was also an important factor which supports the results obtained in a study by Duan and Zhang [8]. In patients where moderate force resulted in two fracture areas; impacted 3rd molars played an important role in angle and condyle fractures along with other associated fractures. In patients sustained with low force which resulted in single fracture site, 3rd molar position either impacted or erupted played an insignificant role in condyle and angle fracture. In patients injured by a high traumatic force, who sustained multiple fracture sites, an influence of impacted 3rd molars on angle and condylar fracture was not demonstrated. The severity of injury was the primary factor resulting in multiple fractures, not the presence or absence of 3rd molars.
Considering injury causes, the risk of angle fracture was much more affected by impacted 3rd molars than that of condylar fracture. This can be explained because of lowered resistance to external forces when there is an impacted 3rd molar in angle region [15]. Reitzik et al. [16] showed that the mandible with impacted third molars required 40 % less force to be fractured than the mandible with fully erupted third molars, and they suggested that the unerupted third molars could weaken the mandible because the tooth occupied more of the osseous space. One important finding in the present study was that patients with erupted 3rd molars were two times more likely to have a condyle fracture than those with unerupted third molars.
When a small area of mandible is exposed to large forces, fracture will occur at the site of impact and also elsewhere in the region of weak sections. As many studies suggested, when there is parasymphysis fracture on one side, in case of erupted 3rd molars, condyle being the weak point tends to fracture on contralateral side and when an impacted 3rd molar is present, angle tends to fracture on the contralateral side [7, 13]. The present study also showed a similar result. Wolujewicz [17] depicted the relation between impacted teeth and angle fracture, as one of the predisposing factor to their weakness but concluded that there was no relationship between the position of third molar and the incidence of angle fractures. Contrary to this study, our results demonstrate that 3rd molar position also poses a variable risk for angle fractures. Of the ten cases of angle fractures associated with impacted teeth we found that very less available space, deeply positioned and moderately inclined teeth was associated with an increased risk of angle fractures. The highest incidence of angle fracture was observed in position A impacted mandibular third molars which is similar to the results observed by Rajasekhar et al. [18].
Few opinions have been put forth on position of impacted 3rd molar and its risk on angle fracture. Rajkumar et al. [19] stated that more superficial position of an impacted third molar was associated with an increased risk of angle fractures. According to Fuselier et al. [13] angle fractures are more common in subjects with mesioangular third molars. In contrast, Maaita et al. [5] found a higher prevalence for vertical and distoangular third molars. Regarding the vertical position, these authors suggested that deeply impacted third molars are mainly responsible for the higher risk of angle fractures. In contrast, Lee et al. [2] did not agree that completely impacted teeth increase the relative risk of fracture compared to erupted third molars. Halmos et al. [20] confirmed this observation and added that superficial impactions may be more frequently associated with an increased risk of these fractures. Our results were in accordance with Duan and Zhang [8].
In the present study more than 62 % of mandibular fractures were noted at the condylar region. Kober et al. [21] showed that condyle is prone to fracture in fully erupted molar as angle would be resistant to fracture and more impact forces would transmit to the condyle and result in fracture. In impacted molars, the impact forces that cause condylar fractures transmit to the mandibular angle on the same side, which is biomechanically stronger than the condyle. The findings of this study suggest that the mandibular angles that contain impacted third molars are significantly more susceptible to fracture than the angle regions without impacted third molars. These results are consistent with and can be explained in terms of the stress–strain distribution within the mandible, as outlined by Huelke and Burdi [22].
Tevepaugh and Dodson, found that patients with mandibular third molars were 3.8 times more susceptible to angle fracture than patients without third molar [13]. However, Ugboko et al. [6] depict that the presence of a third molar does not predispose to angle fractures. In this study it was noticed that Pedersen Difficulty index score can also be related to the risk of angle and condyle fracture. Seven cases with moderate difficulty showed increased incidence of condylar fractures. This can be explained by the amount of space occupied by the impacted molar and also the amount and direction of impacted force. It is also evident in the results that whatever the position or angle of the teeth, angle has a higher risk of fracture. By assessing the difficulty index in patients who are more involved in contact sports, we can reduce the incidence of fracture. Schwimmer et al. [23] have advocated removing impacted mandibular third molars to prevent mandibular fractures in athletes involved in contact sports. Tevepaugh and Dodson’s study further supports their recommendation [13]. Hence, if the patient is at risk of further trauma to the region of mandibular angle as a result of occupation or lifestyle, it may be appropriate to remove the tooth to strengthen the mandible in this area.
The results of this study demonstrate that unerupted mandibular 3rd molars make the mandibular angle more susceptible to fracture and that the incidence of angle fracture is increased by mesioangular and distoangular types of impactions. Irrespective of the status or position of 3rd molar, condyle and angle region were susceptible to fracture but angle has a much higher risk. When the 3rd molar is completely erupted, condyle has the tendency to fracture especially the subcondylar region. Patients with impacted 3rd molars were at higher risk of angle fractures than those without impacted 3rd molars no matter how deep they are positioned. Considering the injury mechanism and injury cause, the risk of angle fracture is much more influenced by the impacted 3rd molar. Position of 3rd molar also influences the other associated fracture sites along with angle and condyle, which is more common with angle fracture. The results of the study show that the 3rd molar can dictate the fracture pattern in mandible taking some of the above mentioned factors into consideration.
Conclusion
Presence or absence of mandibular 3rd molar definitely has a bearing on the mandibular fracture pattern. Injury mechanism and etiological factor play an adjunct role. We feel that by knowing the severity of third molar impaction based on Pedersen’s difficulty index one can assess the mandibular fracture pattern. Impacted 3rd molar leads to an increased risk of angle fracture and decreased risk of condylar fracture especially when they are more deeply seated.
References
- 1.Meisami T, Sojat A, Sandor GKB, Lawrence HP, Clokie CML. Impacted third molars and risk of angle fracture. Int J Oral Maxillofac Surg. 2002;31(2):140–144. doi: 10.1054/ijom.2001.0215. [DOI] [PubMed] [Google Scholar]
- 2.Lee JT, Dodson TB. The effect of mandibular third molar presence and position on the risk of an angle fracture. J Oral Maxillofac Surg. 2000;58(4):394–398. doi: 10.1016/S0278-2391(00)90921-2. [DOI] [PubMed] [Google Scholar]
- 3.Weiss L (1965) Static loading of the mandible. Oral Surg Oral Med Oral Pathol 19:253 [DOI] [PubMed]
- 4.Safdar N, Meechan J. Relationship between fractures of the mandibular angle and the presence and state of eruption of the lower third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79(6):680–684. doi: 10.1016/S1079-2104(05)80299-9. [DOI] [PubMed] [Google Scholar]
- 5.Maaita J, Alwrikat A. Is the mandibular third molar a risk factor for mandibular angle fracture? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(2):143. doi: 10.1067/moe.2000.103527. [DOI] [PubMed] [Google Scholar]
- 6.Ugboko VI, Oginni FO, Owotade FJ. An investigation into the relationship between mandibular third molars and angle fractures in Nigerians. Br J Oral Surg. 2000;38:427–429. doi: 10.1054/bjom.2000.0312. [DOI] [PubMed] [Google Scholar]
- 7.Zhu SJ, Choi BH, Kim HJ, Park WS, Huh JY, Jung JH, Kim BY, Lee SH. Relationship between the presence of unerupted mandibular third molars and fractures of the mandibular condyle. Int J Oral Maxillofac Surg. 2005;34(4):382–385. doi: 10.1016/j.ijom.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Duan DH, Zhang Y. Does the presence of mandibular third molars increase the risk of angle fracture and simultaneously decrease the risk of condylar fracture? Int J Oral Maxillofac Surg. 2008;37(1):25–28. doi: 10.1016/j.ijom.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Winter GB. Impacted third molars. St. Louis: American Medical Book Co.; 1926. pp. 241–279. [Google Scholar]
- 10.Pell G, Gregory G. Impacted mandibular third molars, classification and modified technique for removal. Dental Dig. 1993;39:330–338. [Google Scholar]
- 11.Archer W (1975) Oral and maxillofacial surgery, vol 1, 5th edn. Saunders, Philadelphia, 311:259–260
- 12.Kelly D, Harrigan W. A survey of facial fractures related to teeth and edentulous regions. J Oral Surg. 1975;33:146–149. [PubMed] [Google Scholar]
- 13.Fuselier JC, Ellis EE, III, Dodson TB. Do mandibular third molars alter the risk of angle fracture? J Oral Maxillofac Surg. 2002;60(5):514–518. doi: 10.1053/joms.2002.31847. [DOI] [PubMed] [Google Scholar]
- 14.Vivek GK. The role of mandibular 3rd molars on the incidence of condylar fractures—a clinical study. IOSR J Dental Med Sci. 2014;13(5):27–30. doi: 10.9790/0853-13532730. [DOI] [Google Scholar]
- 15.Krimmel M, Reinert S. Mandibular fracture after third molar removal. J Oral Maxillofac Surg. 2000;58:1110–1112. doi: 10.1053/joms.2000.9566. [DOI] [PubMed] [Google Scholar]
- 16.Reitzik M, Lownie JF, Cleaton JP, Austin J. Experimental fractures of the monkey mandibles. Int J Oral Surg. 1978;7(2):100–103. doi: 10.1016/S0300-9785(78)80054-4. [DOI] [PubMed] [Google Scholar]
- 17.Wolujewicz MA. Fractures of the mandible involving the impacted third molar tooth: an analysis of 47 cases. Br J Oral Surg. 1980;18(2):125–131. doi: 10.1016/0007-117X(80)90028-1. [DOI] [PubMed] [Google Scholar]
- 18.Rajasekhar G, Sudhir R, Nandagopal V, Rajeev Reddy K, Vinay Kumar G (2014) Impacted mandibular third molars and their influence on mandibular angle and condyle fractures—a retrospective study. J Craniomaxillofac Surg 42(7):1102–1105 [DOI] [PubMed]
- 19.Rajkumar K, Sinha Ramen, Chowdhury Roy, Chattopadhyay PK. Mandibular third molars as a risk factor for angle fractures: a retrospective study. J Maxillofac Oral Surg. 2009;8(3):237–240. doi: 10.1007/s12663-009-0058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halmos D, Ellis E, III, Dodson T. Mandibular third molars and angle fractures. J Oral Maxillofac Surg. 2004;62(9):1076–1081. doi: 10.1016/j.joms.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Kober C, Sader R, Thiele H, Bauer HJ, Zeilhofer HF, Hoffmann KH, Horch HH. Stress analysis of the human mandible in standard trauma situations with numerical simulation. Mund Kiefer Gesichtschir. 2001;5:114–119. doi: 10.1007/s100060000262. [DOI] [PubMed] [Google Scholar]
- 22.Huelke and Burdi Location of mandibular fractures related to teeth and edentulous regions. J Oral Surg. 1964;22:396–405. [PubMed] [Google Scholar]
- 23.Schwimmer A, Stern R, Kritchman D. Impacted third molars: a contributing factor in mandibular fractures in contact sports. Am J Sports Med. 1983;11:262. doi: 10.1177/036354658301100415. [DOI] [PubMed] [Google Scholar]