Abstract
This study was designed to investigate whether reduced adenosine formation linked to deficits in extracellular ATP hydrolysis by NTPDases contributes to detrusor neuromodulatory changes associated with bladder outlet obstruction in men with benign prostatic hyperplasia (BPH). The kinetics of ATP catabolism and adenosine formation as well as the role of P1 receptor agonists on muscle tension and nerve-evoked [3H]ACh release were evaluated in mucosal-denuded detrusor strips from BPH patients (n = 31) and control organ donors (n = 23). The neurogenic release of ATP and [3H]ACh was higher (P < 0.05) in detrusor strips from BPH patients. The extracellular hydrolysis of ATP and, subsequent, adenosine formation was slower (t1/2 73 vs. 36 min, P < 0.05) in BPH detrusor strips. The A1 receptor-mediated inhibition of evoked [3H]ACh release by adenosine (100 μM), NECA (1 μM), and R-PIA (0.3 μM) was enhanced in BPH bladders. Relaxation of detrusor contractions induced by acetylcholine required 30-fold higher concentrations of adenosine. Despite VAChT-positive cholinergic nerves exhibiting higher A1 immunoreactivity in BPH bladders, the endogenous adenosine tonus revealed by adenosine deaminase is missing. Restoration of A1 inhibition was achieved by favoring (1) ATP hydrolysis with apyrase (2 U mL−1) or (2) extracellular adenosine accumulation with dipyridamole or EHNA, as these drugs inhibit adenosine uptake and deamination, respectively. In conclusion, reduced ATP hydrolysis leads to deficient adenosine formation and A1 receptor-mediated inhibition of cholinergic nerve activity in the obstructed human bladder. Thus, we propose that pharmacological manipulation of endogenous adenosine levels and/or A1 receptor activation might be useful to control bladder overactivity in BPH patients.
Keywords: Adenosine A1 receptors, ATP catabolism, Acetylcholine release, Ectonucleotidases, Human urinary bladder, Bladder outlet obstruction
Introduction
Detrusor dysfunction associated with bladder outlet obstruction (BOO) has long been considered a key factor in the mechanism through which benign prostatic hyperplasia (BPH) causes persistent lower urinary tract symptoms (LUTS) (reviewed in [1]). Although there is a lack of information regarding the way obstruction may cause bladder dysfunction, morphologic and functional abnormalities of the bladder detrusor are frequent in patients affected with BPH. Most of these changes can be regarded as a consequence of mechanical stress and hypoxic changes caused by BOO at the molecular level in the epithelium, smooth muscle fibers, extracellular matrix, and neuronal network of the urinary bladder [1].
Although it is generally accepted that acetylcholine (ACh) acting on smooth muscle muscarinic receptors is the primary effector controlling bladder emptying, neural stimulation of the bladder is only partially inhibited by atropine in many species, including humans [2, 3]. In keeping with the purinergic hypothesis proposed by Burnstock, it is now accepted that ATP is responsible for the atropine-resistant component of parasympathetic contraction of the detrusor [4, 5]. While the purinergic component of detrusor contraction via P2 purinoceptors activation is lacking in healthy humans, it may increase with age [6] and is responsible for up to 40 % of nerve-evoked bladder contractions in pathological conditions, including hypertrophic unstable bladder, overactive detrusor, neurogenic bladder, and interstitial cystitis (reviewed in [7]).
In patients with idiopathic detrusor instability, appearance of atropine-resistant P2 purinergic tone is related to decreased ecto-NTPDase activity, thus limiting the breakdown of ATP released from bladder nerves or the urothelium [8]. Nonetheless, decreased activity of ecto-NTPDases may also have profound implications for endogenous adenosine formation and P1 receptors activation. Surprisingly, this mechanism has never been explored in the human bladder despite the fact that the adenosine content of human bladder smooth muscle is 6.7 times higher than in the striated muscle and the adenosine/ATP ratio is 1:9 compared with 1:450 for skeletal muscle [9].
Previous studies have shown that adenosine partially relaxes pre-contracted urinary bladder detrusor strips exposed to carbachol, acetylcholine (ACh), or potassium depolarization in rats, guinea-pigs [10–14], and humans [15]. Besides direct actions of adenosine on P1 receptors located on detrusor smooth muscle fibers, the nucleoside and its analogues may act indirectly by inhibiting nerve-evoked contractions as demonstrated in rats [10, 13, 14, 16], guinea pigs [14], cats [17], and humans [18]. All four subtypes of adenosine receptors (A1, A2A, A2B, and A3) have been identified in the bladder of experimental animals and humans by RT-PCR analysis; results show that A2A and A2B mRNAs are more expressed than A1, with the A3 being the least expressed receptor [19, 20]. Discrepancy between the relative abundance of A1 and A2 receptor subtypes in the detrusor [19] may be attributed to their preferential localization on tiny nerve terminals and smooth muscle fibers, respectively [10, 12], which supports previous pharmacological data obtained in rodents. There are, however, no published reports on subtype distribution of adenosine receptors in the human urinary bladder.
Therefore, this study was designed to investigate the kinetics of ATP catabolism and adenosine formation as well as the role of specific adenosine receptor ligands on electrically evoked [3H]-ACh release and muscle tension in mucosal-denuded detrusor strips, which were collected from men with outflow obstruction due to BPH (patients) and control organ donors. Because RT-PCR results do not necessarily correlate with the presence of functional adenosine receptors on the cell surface, we evaluated the expression of adenosine receptor subtypes in the human detrusor by immunofluorescence confocal microscopy.
Patients and methods
Human detrusor samples
Samples of human detrusor were collected from the bladder dome of 31 male patients (62 ± 6 years of age) with bladder outlet obstruction due to BPH submitted to transvesical prostatectomy and from 23 male organ donors (56 ± 4 years of age) at the time of harvesting organs for transplantation. Bladder outflow obstruction (BOO) and prostate enlargement were confirmed by uroflowmetry and ultrasonography, respectively. Collected samples were immediately placed at 4–6 °C in mannitol transplantation solution at 400 mOsm kg−1 (M-400) not supplemented with ATP or adenosine (230 mM mannitol, 15 mM KH2PO4, 43 mM K2HPO4 · 3H2O, 15 mM KCl, and 10 mM NaHCO3, pH 7.4) and transported to the laboratory. Experiments were performed within the first 24 h after collection, which corresponds to the tissue viability window. This study and all its procedures were approved by the Ethics Committees of CHP and ICBAS-UP and were authorized by the National Transplantation Committee. All BPH patients signed an informed consent approved by the Ethics Committee of CHP for using the biological material. Regarding deceased organ donation, the legal frame work allows the “Presumed Consent” stating that residents in Portugal are consenting donors unless the individual previously objected during his or her life. The investigation conforms to the principles outlined in The Code of Ethics of the World Medical Association (Declaration of Helsinki).
Quantification of ATP and [3H]ACh release
After dissecting out the mucosa through cleavage at the lamina propria, detrusor muscle strips (∼1.5 × 5 mm) were mounted in 3-mL capacity vertical perfusion chambers heated at 37 °C. The procedures used for labeling the preparations and measuring evoked [3H]ACh release were described previously [21–23]. Briefly, the preparations were superfused with gassed (95 % O2 and 5 % CO2) Tyrode’s solution (pH 7.4) containing (mM) NaCl 137, KCl 2.7, CaCl2 1.8, MgCl2 1, NaH2PO4 0.4, NaHCO3 11.9, glucose 11.2, and choline 0.001. After a 30-min equilibration period, cholinergic neurons were loaded with 1 μM [3H]choline (specific activity 2.5 μCi nmol−1) under electrical field stimulation (EFS, 1 Hz frequency, 0.5 ms pulse width, 40 V) during 40 min. Washout of the preparations was performed for 60 min by superfusion (15 mL min−1) with Tyrode’s solution supplemented with the choline uptake inhibitor, hemicholinium-3 (10 μM). Tritium content was measured by liquid scintillation spectrometry (TriCarb2900TR; Perkin Elmer, Boston, USA) (% counting efficiency = 58 ± 2 %) after appropriate background subtraction, using 400-μL bath samples collected automatically every 3 min with a fraction collector (Gilson, FC203B, France). In control experiments, aliquots of matched samples were immediately freeze-dried in liquid nitrogen and preserved at −80 °C for subsequent ATP quantification by bioluminescence using the luciferin-luciferase ATP kit HS II (Roche Applied Science, Indianapolis, USA) according to manufacturer’s instructions. Luminescence was determined using a multi-detection microplate reader (Synergy HT; BioTek Instruments) [23–25].
[3H]ACh release was evoked by two periods of electrical field stimulation (S1 and S2, 200 pulses of 0.5 ms duration delivered at 10 Hz frequency). Therefore, the evoked [3H]ACh release was calculated by subtracting the basal tritium outflow from the total tritium outflow during the stimulation period (see, e.g., [21–23]). Likewise, stimulation-evoked release of ATP was calculated by subtracting the basal release, measured in the sample collected before stimulation, from the total release of the nucleotide determined after stimulus application [23–25].
Myographic recordings
Detrusor muscle strips without the mucosa were mounted in 10-mL capacity perfusion chambers connected to isometric force transducers. The changes in tension were recorded continuously with a PowerLab data acquisition system (Chart 5, v.4.2; AD Instruments, USA). Tissues were preloaded with 5 mN of tension and allowed to equilibrate for 90 min in Tyrode’s solution, at 37 °C. To evaluate the inhibitory role of adenosine (0.03–3 mM) and its enzymatically stable analogue, 5′-(N-ethylcarboxamide) adenosine (NECA, 0.3–300 μM), on detrusor strips contractions induced by ACh (10 μM), these drugs were added to the incubation media 6 min before ACh which contacted with the preparations for 2 min before washout of all drugs. Under these experimental conditions, exogenous ACh (0.1–1000 μM) concentration-dependently increased myogenic contractions of detrusor strips from control individuals and BPH patients with a similar potency (EC50 3 μM); a higher (P < 0.05) maximal contraction amplitude was achieved in control preparations (4.74 ± 0.46 mN mg−1 of wet weight, n = 8) than in obstructed human bladders (2.64 ± 0.27 mN mg−1 of wet weight, n = 14). ACh, applied in the low micromolar concentration range close to the EC50 value, has been instrumental to evoke sustained myogenic contractions to investigate the effects of detrusor smooth muscle relaxants (see, e.g., [16, 18]).
Kinetic of the extracellular catabolism of adenine nucleotides by HPLC
For the kinetic experiments of the extracellular catabolism of adenine nucleotides, detrusor strips without the mucosa were mounted in a 2-mL organ bath. All experiments were performed at 37 °C. Preparations were superfused with gassed (95 % O2 and 5 % CO2) Tyrode’s solution. After equilibrium, the preparations were incubated with 30 μM of ATP or AMP (zero time). Samples of 75 μL were collected from the organ bath at different times up to 45 min for HPLC (with UV detection) analysis (LaChrome Elite; Merck, Germany) of the variation of substrate disappearance and product formation [21, 22, 26]. The stoichiometry of ATP and AMP conversion into their metabolites was kept unaltered (30 μM). Considering that the curvilinear decrease of the initial substrate with time is characteristic of first-order kinetics, the half-degradation time was estimated from polynomial fitting of linear semi-logarithmic progress curves of the catabolism of adenine nucleotides for each separate experiment (see, e.g., [21]).
Immunofluorescence staining and confocal microscopy observation
Detrusor strips without the mucosa were stretched in all directions and pinned onto a Petri dish coated with Sylgard®. The strips were then fixed in PLP solution (paraformaldehyde 2 %, lysine 0.075 M, sodium phosphate 0.037 M, sodium periodate 0.01 M) for 16 h at 4 °C. Sixteen-micron sections were incubated with selected primary antibodies (Table 1) diluted in an incubation buffer (fetal bovine serum 5 %, serum albumin 1 %, Triton X-100 0.3 % in PBS), at 4 °C, for 16 h. For double immunostaining, antibodies were combined before application to tissue samples. After washing away unbound primary antibody, the sections were incubated with secondary antibodies in the dark for 2 h at room temperature. Negative controls were carried out by replacing the primary antibodies with non-immune serum; cross-reactivity of the secondary antibodies was tested in control experiments in which primary antibodies were omitted. Specificity of primary antibodies used to target human P1 receptors were all previously validated in heterologous expression systems according to references provided in manufacturers’ websites. Finally, tissue samples were mounted on optical-quality glass slides using VectaShield as antifade mounting media (VectorLabs) and stored in the dark at 4 °C. Observations were performed and analyzed with a laser-scanning confocal microscope (Olympus FluoView, FV1000, Tokyo, Japan). During documentation of detrusor sections from control and BPH patients, settings on the confocal microscope were kept unaltered to minimize bias.
Table 1.
Primary and secondary antibodies used to label human detrusor strips
| Primary antibodies | Code | Host | Dilution | Source |
| Anti-VAChT | ab69000 | Goat (gt) | 1:75 | Abcam |
| Anti-A1 receptor | ab75177 | Rabbit (rb) | 1:250 | Abcam |
| Anti-A2A receptor | sc-13937 | Rabbit (rb) | 1:75 | Santa Cruz |
| Anti-A2B receptor | ab1589P | Rabbit (rb) | 1:75 | Abcam |
| Anti-A3 receptor | sc-7508 | Goat (gt) | 1:50 | Santa Cruz |
| Secondary antibodies | Code | Host | Dilution | Source |
| Alexa Fluor 488 anti-rb | A-21206 | Donkey | 1:1500 | Molecular Probes |
| Alexa Fluor 568 anti-gt | A-11057 | Donkey | 1:1500 | Molecular Probes |
Drugs and solutions
Acetylcholine, adenosine deaminase (ADA, type VI, 1803 U mL−1, EC 3.5.4.4), ATP, ADP, AMP, adenosine, apyrase (from potato, EC 3.6.1.5), erythro-9-(2-hydroxy-3-nonyl)adenine hydrochloride (EHNA), inosine, hemicholinium-3, hypoxanthine, N6-(L-2-phenylisopropyl)adenosine (R-PIA), 5′-(N-ethylcarboxamide) adenosine (NECA), 1,3-dipropyl-8-cyclopentylxanthine (DPCPX), choline chloride, paraformaldehyde (prills), lysine, sodium periodate, anhydrous glycerol, fetal bovine (Sigma, St Louis, MO, USA); dipyridamole (Boehringer Ingelheim, Germany); [methyl-3H] choline chloride (ethanol solution, 80.6 Ci mmol−1) (PerkinElmer, Boston, USA); serum albumin, Triton X-100 (Merck, Darmstadt, Germany). EHNA was dissolved in a 5-mM stock solution in ethanol. DPCPX was dissolved in a 5-mM stock solution in 99 % dimethylsulfoxide (DMSO) + 1 % NaOH 1 M (v v−1). ZM 241385 and R-PIA were dissolved in 5- and 50-mM stock solutions in DMSO, respectively. All stock solutions were stored as frozen aliquots at −20 °C. Dilutions of these stock solutions were made daily and appropriate solvent controls were done.
Presentation of data and statistical analysis
Results are expressed as mean ± SD, with n indicating the number of individuals used for a particular set of experiments. Only one experimental procedure (e.g., agonist in the absence and in the presence of the antagonist) was performed per individual. Statistical analysis of data was carried out using Graph Pad Prism 6.04 for Windows software (La Jolla, USA). Paired and unpaired Student’s t test with Welch’s correction was used for statistical analysis when parametric data was considered. One-way analysis of variance (ANOVA) followed by the Holm-Sidak correction was used for multiple comparisons. P <0.05 (two-tailed) values were considered statistically significant.
Results
Downregulation of ecto-NTPDase1/CD39 and ecto-5′-nucleotidase/CD73 leads to deficient adenosine formation in the detrusor of BPH patients
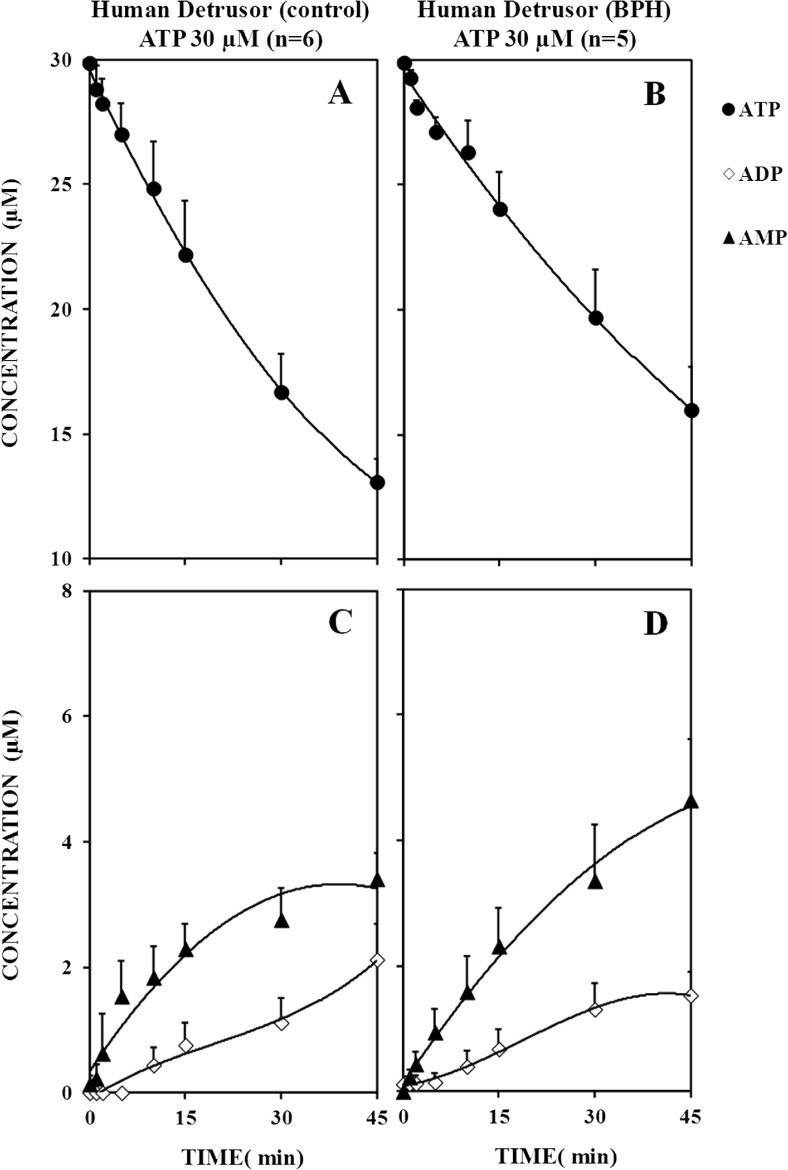
Figure 1 illustrates the kinetics of the extracellular catabolism of ATP (30 μM) and, subsequent, formation of ADP and AMP in mucosal-denuded detrusor strips from control individuals and BPH patients. Extracellular ATP (30 μM) was hydrolyzed with a half-degradation time of 36 ± 5 min (n = 6) in control individuals (Fig. 1a), but the catabolism of the nucleotide was significantly (P < 0.05) slower (t1/2 = 73 ± 16 min, n = 5) in detrusor strips from BPH patients (Fig. 1b). In both groups, the amount of AMP generated in the extracellular milieu was higher (P < 0.05) than that of ADP at all time points considered after ATP (30 μM) application (Fig. 1c, d). This pattern suggests a dominant involvement of ecto-NTPDase1/CD39 (also called ATP diphosphohydrolase or apyrase, EC 3.6.1.5) converting extracellular ATP directly into AMP, removing one phosphate at a time with almost no release of the intermediate ADP. As a matter of fact, the activity of ecto-NTPDase1/CD39 calculated 5 min after ATP (30 μM) application by the ratio of [AMP]/[ATP + ADP] per minute decreased (P < 0.01) from 11.40 ± 0.85 × 10−3 (n = 6) in control subjects to 6.94 ± 0.53 × 10−3 (n = 5) in BPH patients, while up to this time point no ADP could be detected in incubation media (Fig. 1c, d).
Fig. 1.
The extracellular catabolism of ATP is slower in mucosal-denuded detrusor strips from patients with outflow obstruction due to benign prostatic hyperplasia (BPH) as compared to control organ donors (Control). ATP (30 μM) was added at zero time to the incubation medium. Samples were collected from the incubation fluid at the indicated times on the abscissa and analyzed by HPLC with UV detection to quantify ATP (filled circles) and its metabolites, ADP (open lozenges), and AMP (filled triangles). Average results obtained from six control individuals (a, c) and five BPH patients (b, d); the vertical bars represent SD and are shown when they exceed the symbols in size
Figure 2 shows that extracellular AMP (30 μM) is subsequently dephosphorylated into adenosine, inosine, and hypoxanthine in the human detrusor. Interestingly, hydrolysis of AMP (30 μM) to adenosine and inorganic phosphate by ecto-5′-nucleotidase/CD73 (EC 3.1.3.5) was significantly (P < 0.05) diminished in bladder samples from BPH patients (t1/2 = 79 ± 7 min, n = 5; Fig. 2b) compared to control individuals (t1/2 = 45 ± 4 min, n = 5; Fig. 2a). Impairment of the extracellular AMP (30 μM) catabolism in the detrusor of BPH patients led to a significant (P < 0.01) decrease in adenosine formation (Fig. 2d) compared to control individuals (Fig. 2c); this difference reached a maximum of 4.14 ± 0.58 μM (n = 5) at 10-min incubation time which diminished thereafter. The decrease in the rate of adenosine formation from extracellular AMP was also accompanied by a deficient generation of inosine resulting from the irreversible deamination of adenosine catalyzed by ecto-adenosine deaminase (ecto-ADA, also known as adenosine aminohydrolase, EC 3.5.4.4) (Fig. 2c, d). Inosine was then deribosylated by purine nucleoside phosphorylase (EC 2.4.2.1) leading to small amounts of hypoxanthine.
Fig. 2.
The kinetics of extracellular AMP dephosphorylation is slower in mucosal-denuded detrusor strips from patients with outflow obstruction due to benign prostatic hyperplasia (BPH) as compared to control organ donors (control). AMP (30 μM) was added at zero time to the incubation medium. Samples were collected from the incubation fluid at the indicated times on the abscissa and analyzed by HPLC with UV detection to quantify AMP (filled triangles) and its metabolites, adenosine (ADO, open squares), inosine (INO, filled squares), and hypoxanthine (HX, filled lozenges). Average results obtained from five individuals of each group, control (a, c), and BPH (b, d); the vertical bars represent SD and are shown when they exceed the symbols in size
All together, these results indicate that adenosine formation from the extracellular catabolism of adenine nucleotides is impaired in the detrusor of BPH patients due to deficient activity of both ecto-NTPDase1/CD39 and ecto-5′-nucleotidase/CD73.
Exogenous NTPDase1/CD39 (apyrase) re-adjusts cholinergic nerve hyperactivity to control levels in the detrusor of BPH patients
Electrical field stimulation of detrusor strips increases the outflow of [3H]ACh above the basal level (Fig. 3). Prevention of the evoked tritium outflow in the absence of calcium (Ca2+ ∅ + EGTA, 1 mM) and in the presence of tetrodotoxin (1 μM) indicates that [3H]ACh release results from vesicle exocytosis of depolarized nerve terminals (data not shown). The amount of [3H]ACh released from stimulated cholinergic nerves during S1 was 1.5-fold higher (P < 0.001) in the detrusor of BPH patients (27.6 ± 2.7 × 103 DPM g−1 of wet tissue weight, n = 12) than in control organ donors (11.1 ± 0.2 × 103 DPM g−1 of wet tissue weight, n = 14). In some of the experiments, we measured in parallel the ATP content of collected samples. Electrical stimulation of detrusor strips from BPH patients produced 2.5-fold higher (P < 0.001) amounts of ATP in the incubation fluid (4.9 ± 0.4 pM, n = 4) than those observed in control individuals (1.4 ± 0.2 pM, n = 8). Exogenously added apyrase (2 U mL−1), the enzyme that catalyzes ATP inactivation into AMP bolstering the formation of adenosine, decreased [3H]ACh release from stimulated cholinergic nerves. The inhibitory effect of apyrase (2 U mL−1) was more evident (P < 0.05) in detrusor strips from BPH patients (18 ± 6 %, n = 4) than from control subjects (2 ± 4 %, n = 4), i.e., in conditions where extracellular ATP accumulation was higher (Fig. 3).
Fig. 3.
Effects of apyrase on electrically evoked [3H]ACh release from urothelium-denuded detrusor strips from control individuals (Control, a) and patients with outflow obstruction due to benign prostatic hyperplasia (BPH, b). Tritium outflow (ordinates) is expressed as a percentage of the total radioactivity present in the tissue at the beginning of the collection period (fractional release, %) (see, e.g., [21]). Abscissa indicates the times at which samples were collected. [3H]ACh release was elicited by electrical field stimulation (10 Hz, 200 pulses of 0.5 ms duration) twice, starting at 12th (S1) and 39th (S2) minutes after the end of washout (zero time). Apyrase (2 U mL−1, closed circles) was added to the incubation media 15 min before S2 (horizontal bar). The vertical bars represent SD of four different individuals. *P < 0.05 (unpaired Student’s t test with Welch’s correction) represents significant differences when compared to the situation without apyrase. Note that the spontaneous tritium outflow was not changed in the presence of apyrase
Adenosine A1 receptors located on cholinergic nerve endings play a dominant role to reduce detrusor activity in the human bladder
Despite the observation that adenosine is able to relax pre-contracted detrusor strips from the human bladder [15], we found that this is only valid for concentrations of the nucleoside in the millimolar range (Fig. 4). In our hands, adenosine reduced acetylcholine (10 μM)-induced contractions of BPH patient’s detrusor only when it was applied in a 3-mM concentration (Fig. 4b), but not when the nucleoside was tested in lower (eventually more physiological) amounts (30 and 300 μM). The enzymatically stable adenosine analogue, NECA (0.3–300 μM), which activates preferentially A2 receptors (IC50 ∼16 nM), was unable to cause relaxation of the pre-contracted human detrusor (Fig. 4a, b), notwithstanding the fact that A2A and/or A2B subtypes are considered the most expressed receptors in the detrusor smooth muscle [19, 20]. Water solubility limitation precluded the use of millimolar concentrations of NECA.
Fig. 4.
Adenosine and its stable analogues, NECA and R-PIA, preferentially activates DPCPX-sensitive inhibitory A1 receptors on cholinergic nerve terminals of the human detrusor and their potency increase in patients with outflow obstruction due to benign prostatic hyperplasia (BPH) as compared to controls. a Myographic recordings of mucosal-denuded detrusor strips from BPH patients. Contractile responses were elicited by ACh (10 μM) applied either in the absence or in the presence of NECA (0.3–300 μM) and adenosine (30–3000 μM), in which concentration-response curves are shown in (b). The vertical bars represent SD of an n number of individuals. *P < 0.05 (unpaired Student’s t test with Welch’s correction) represents significant differences when compared to the control situation without any drug added (100 %, horizontal dashed line). c Effects of NECA (1 μM) and adenosine (100 μM) on electrically evoked [3H]ACh release from mucosal-denuded detrusor strips of BPH patients; NECA (1 μM) and adenosine (100 μM) were added to the incubation media 15 min before S2 (horizontal bar). The vertical bars represent SD of four different individuals. d The inhibitory effects of NECA (1 μM) and R-PIA (300 nM) on electrically evoked [3H]ACh release from detrusor strips of organ donors (control) and BPH patients in the absence and in the presence of DPCPX (100 nM); the selective A1 receptor antagonist was present throughout the assay, including S1 and S2. The ordinates are changes in S2/S1 ratios compared to the S2/S1 ratio obtained without addition of any drug. The data are means ± SD of four to six individuals. #,* P < 0.05 (unpaired Student’s t test with Welch’s correction) represents significant differences when compared to control individuals or to the situation where the adenosine analogue was tested in the absence of DPCPX, respectively
Figure 4c and d also shows that adenosine (100 μM) and its analogues, NECA (1 μM) and R-PIA (0.3 μM, a selective A1 receptor agonist), inhibit [3H]ACh release from stimulated cholinergic nerves of the human detrusor, when these drugs were used in concentrations unable to cause relaxation of myogenic contractions induced by acetylcholine (10 μM, EC50 ∼3 μM). The inhibitory effects of NECA (1 μM) and R-PIA (0.3 μM) were of higher magnitude in BPH patients than in control individuals (Fig. 4d). Likewise, the native compound adenosine (100 μM) diminished nerve-evoked [3H]ACh release by 9 ± 8 % (n = 5, P > 0.05) and 39 ± 2 % (n = 5, P < 0.05) in the detrusor of control organ donors and BPH patients, respectively. The selective A1 receptor antagonist, DPCPX (100 nM), significantly (P < 0.05) attenuated the inhibitory effects of NECA (1 μM) and R-PIA (0.3 μM) on evoked [3H]ACh release (Fig. 4d), thus suggesting that A1 receptors located on cholinergic nerve endings exert a dominant effect to reduce detrusor hyperactivity in the human bladder.
The immunolocalization studies shown in Fig. 5a suggest that A1 and A2A are the most expressed receptors in the human detrusor, whereas immunoreactivity of A2B and A3 receptors is less evident. Co-localization experiments show for the first time a differential distribution of the A1 receptor, which is localized preferentially on VAChT-positive cholinergic nerves (Fig. 5b), whereas the A2A receptor is diffusely expressed on smooth muscle fibers of the human detrusor (Fig. 5a, panel E). Interestingly, the A1 receptor immunolabeling becomes more intense in the detrusor of obstructed BPH patients as compared to control individuals (Fig. 5a, respectively panels A and C). The relative increase in A1 receptor immunoreactivity in the detrusor of obstructed BPH patients was not evidenced for any other P1 receptor subtype.
Fig. 5.
a Confocal micrographs showing the immunoreactivity against A1, A2A, A2B, and A3 receptors in transverse sections of the detrusor from organ donors (control) and BPH patients. A1, A2A, A2B, and A3 receptor immunoreactivity is shown in green. Images are representative of five individuals per group, Control and BPH. A1 and A2A are the most expressed receptors in the human detrusor (panels A–H), whereas immunoreactivity of A2B and A3 receptors is only vestigial (panels I–P). The A1 receptor immunolabeling is more evident (arrows) in the detrusor of obstructed BPH patients (panel C) as compared to controls (panel A). Scale bars = 50 μm. b Co-localization experiments show that the A1 receptor is localized with VAChT in cholinergic nerve terminals; yellow staining denotes co-localization. Fluorescence intensity plots drawn from lines crossing regions of interest delineated in the overlay image clearly evidence co-localization of A1 receptors (green) and VAChT-positive (red) cholinergic nerve terminals. c Cross-reactivity of secondary antibodies in control experiments in which primary antibodies were omitted (see Table 1). Differential interference contrast (DIC) images are also shown for comparison
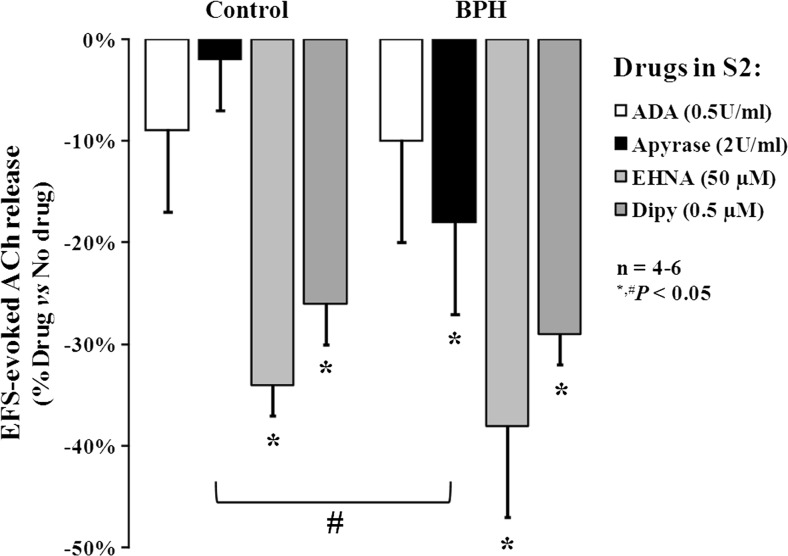
Inhibition of adenosine uptake and/or deamination rehabilitates the A1 receptor inhibitory tonus in the detrusor of BPH patients
To study the net tonic inhibitory effect of endogenous adenosine on [3H]ACh release from stimulated cholinergic nerves of the human detrusor, we tested the effect of adenosine deaminase (ADA, 0.5 U mL−1), the enzyme that inactivates adenosine by converting it into inosine [27]. In contrast to apyrase (2 U mL−1) that catalyzes ATP metabolism into AMP bolstering the formation of adenosine (see also Fig. 3), ADA (0.5 U mL−1) had virtually no effect (P > 0.05) on evoked [3H]ACh release from the human detrusor (Fig. 6). Discrepancies between the effects of ADA (0.5 U mL−1) and apyrase (2 U mL−1) prompted us to evaluate whether the A1-receptor-mediated inhibitory control of [3H]ACh release from stimulated cholinergic nerves could emerge by favoring endogenous adenosine accumulation in the human detrusor with dipyridamole (0.5 μM, a nucleoside uptake blocker) [28] or EHNA (50 μM, an adenosine deaminase inhibitor) [29]. These drugs reduced [3H]ACh release from stimulated cholinergic nerve terminals. The inhibitory effects of adenosine uptake and deamination blockers were not significantly (P > 0.05) different in bladders from control individuals and BPH patients (Fig. 6). Pretreatment with the selective A1 receptor antagonist, DPCPX (100 nM), abolished the inhibitory effects of both dipyridamole (0.5 μM, 9 ± 6 %, n = 4) and EHNA (50 μM, 7 ± 1 %, n = 5) on evoked [3H]ACh release from detrusor strips of BPH patients, indicating that their effects are indeed mediated by increases in the extracellular concentration of adenosine leading to activation of membrane-bound A1 inhibitory receptor.
Fig. 6.
Effects of adenosine deaminase (ADA), apyrase, erythro-9-(2-hydroxy-3-nonyl)adenine (EHNA), and dipyridamole (Dipy) on electrically evoked [3H]-ACh release from urothelium-denuded detrusor strips from cadaveric organ donors (control) and BPH patients. ADA (0.5 U mL−1), apyrase (2 U mL−1), EHNA (50 μM), and Dipy (0.5 μM) were applied 15 min before S2. The ordinates are changes in S2/S1 ratios compared to the S2/S1 ratio obtained without addition of any drug. The data are means ± SD of four to six individuals. *,# P < 0.05 (unpaired Student’s t test with Welch’s correction) represents significant differences when compared with zero percent of change or with the effect of the same drug in control individuals, respectively
Discussion
It is widely accepted that purines, in particular ATP, are involved in a number of physiological processes in the lower urinary tract. ATP was shown (1) to be a co-transmitter with acetylcholine (ACh) in the parasympathetic control of bladder contraction [30], (2) to activate sensory nerves during bladder filling conveying both normal and abnormal sensations like urgency and pain [31, 32], and (3) to participate in the central control of bladder reflexes [33]. However, not so much is known about the effects of adenosine, the breakdown product of extracellular ATP metabolism. First reports of the effect of adenosine in the lower urinary tract suggested that it reduces the tone and spontaneous activity of the guinea-pig urinary bladder [30, 34].
ATP release from both neuronal and non-neuronal cells (e.g., urothelial cells, interstitial cells, fibroblast-like cells, smooth muscle fibers) and its extracellular metabolism into adenosine has been observed in the urinary bladder of rodents [35–37]. Roughly 50 % of the extracellular adenosine results from the breakdown of ATP [38] which is currently regarded to be the most important route of generating extracellular adenosine [39]. Using mucosal-denuded human detrusor strips, we show here that in control conditions, the ecto-NTPDase1/CD39 enzyme exerts a dominant role converting ATP directly into AMP, which is then sequentially hydrolyzed into adenosine and inosine by ecto-5′-nucleotidase/CD73 and ecto-adenosine deaminase, respectively. Despite the distribution of ectonucleotidase subtypes may present specificities among species and differ within the various layers of the bladder wall, immunofluorescence studies in the mouse showed that ecto-5′-nucleotidase/CD73 is present exclusively in the detrusor smooth muscle together with ecto-NTPDase1/CD39 [37]. Data from a previous study demonstrated that adenosine formation from extracellular ATP is negligible in isolated epithelial cells from the human urinary tract [40]. This layout suggests that biosynthesis of adenosine from released ATP is positioned to favor a more important role of the nucleoside in suburothelial and detrusor muscle layers as compared to the urothelium where ecto-5′-nucleotidase/CD73 is almost absent if one excludes the basal cell layer [37]; see also preliminary results in the human bladder in [41].
Adenosine is a homeostatic metabolite in most organic systems mainly because it regulates neuronal excitability, vasodilation, smooth muscle relaxation, and release of vasoactive and neuroactive substances [42, 43]; the nucleoside is also protective against ischemic and inflammatory insults. Therefore, we hypothesized that deficits in adenosine formation from released adenine nucleotides along with lifetime increments of ATP could contribute to detrusor overactivity in BPH patients. Deterioration of bladder neuromodulatory control has been hypothesized to explain the increase on nerve-evoked detrusor contractions in obstructed patients [44]. We show here that detrusor strips from BPH patients release higher amounts of ATP and ACh when stimulated electrically. The greater purinergic tone observed in detrusor strips from obstructed BPH patients (see also [45]) may be partially related to the impairment of ecto-NTPDase1/CD39 activity, thus limiting the breakdown of ATP released from bladder nerves and/or the urothelium, a situation that is in agreement with data from several pathological bladder conditions [8]. In this study, we expanded this concept by demonstrating that decreased activity of ectonucleotidases impacts on endogenous adenosine formation and, thus, on the inhibitory P1 receptors tonus of the human bladder. In parallel to the slower kinetics of the extracellular ATP catabolism, we demonstrated that AMP dephosphorylation leading to adenosine formation via ecto-5′-nucleotidase/CD73 was significantly decreased in bladder samples from obstructed BPH patients as compared to control individuals.
Several authors have shown that adenosine directly relaxes pre-contracted urinary bladder detrusor strips in different species [10–14], including humans [15]. However, our results clearly indicate that adenosine-induced relaxation of detrusor contractions requires high (unphysiological) millimolar concentrations of the nucleoside. On the contrary, our findings show that inhibition of nerve-evoked ACh release by adenosine and its stable analogues, NECA and R-PIA, was 30 times more potent than the relaxing effects of the nucleoside on ACh-induced detrusor contractions. Involvement of the A1 receptor in the inhibitory action of adenosine and its analogues on transmitter release from the stimulated human detrusor was suggested by the selective blockade of their effects with DPCPX. Immunolocalization confocal microscopy data demonstrate for the first time that VAChT-positive cholinergic nerves are endowed with A1 receptors, whereas the A2A receptor is diffusely expressed on smooth muscle fibers of the human detrusor. A1 receptor immunostaining is more intense in the detrusor of obstructed BPH patients as compared to control individuals, which may be caused in reaction to long-term deficits of adenosine formation from the catabolism of released ATP (see above). Thus, upregulation of A1 receptors on cholinergic nerves innervating the detrusor may contribute to explain the increased inhibitory sensitivity of nerve-evoked [3H]ACh release to exogenous adenosine receptor agonists in bladders from BPH patients.
The way adenosine builds its influence to control cells communication depends on the extracellular concentration of the nucleoside, which is achieved by balancing extracellular formation and inactivation mechanisms, both cellular uptake via equilibrative nucleoside transporters and/or extracellular deamination into inosine by adenosine deaminase [46, 47]. Given the disparity between deficits in the adenosine-mediated tone (detected by the lack of effect of ADA on evoked [3H]ACh release) and upregulation of inhibitory A1 receptors expression in the detrusor of BPH patients, we evaluated whether the A1-receptor-mediated control of [3H]ACh release could be rehabilitated by favoring adenosine accumulation with inhibitors of the nucleoside uptake system and adenosine deaminase. We concluded that both dipyridamole and EHNA might be useful for decreasing cholinergic nerve hyperactivity in patients with obstructed bladder due to BPH. Taking into consideration that there are differences in the potency of activation of pre-synaptic A1 receptors on cholinergic nerves and A2A receptors on smooth muscle fibers, prolongation of endogenous adenosine lifetime may be clinically safe because it would hardly affect detrusor contractile tension that is essential to overcome outlet pressure during voiding in BPH patients.
Interestingly, in vivo cystometry experiments performed in the rat showed that both NECA and R-PIA administered intrathecally delayed the voiding reflex [48]. Moreover, prolongation of the intercontraction interval without affecting the amplitude of micturition was also observed when A1 receptor agonists were applied into the lumen of the urinary bladder [49]. Overall, these findings suggest that adenosine controls the micturition cycle by acting predominantly on the nervous circuitry, both central and peripheral, without significantly affecting the voiding pressure that would result in urinary retention.
We are aware of possible limitations of the current study which may be attributed to age-related variance in the bladder cholinergic and purinergic tone among BPH patients (62 ± 6 years of age) and the slightly younger control group (56 ± 4 years of age). Although we did not explore the urological status of control men before harvesting the tissue, care was taken to prevent inclusion of individuals in the control group with a history of LUTS, as far as we could perceive from the clinical records of the intensive care unit and from interviewing close relatives. Yoshida et al. [6] demonstrated age-related increases and decreases respectively in purinergic and cholinergic contractions of stimulated strips of the bladder of patients undergoing total cystectomy due to bladder carcinoma, but they also did not attempt to define if the patients had any kind of bladder dysfunction [6]. We show here that electrical stimulation of detrusor strips from BPH patients release 2.5 times more ATP than control preparations, which is in agreement with the purinergic neurotransmission changes detected in obstructed bladder patients using myographic recordings [50]. Controversy, however, exists concerning the negative correlation between age and the cholinergic neurotransmission [51] because we observed a 1.5-fold increase rather than a decrease in evoked ACh release from the bladder of BPH patients, meaning that age-related changes cannot be the sole factor contributing to modifications in the bladder function among BPH patients and younger controls.
In conclusion, data from this study show for the first time that impairment of ecto-NTPDase1/CD39 activity unbalances extracellular ATP accumulation and endogenous adenosine formation leading to increased neuronal excitation in mucosal-denuded detrusor strips from BPH patients. While extracellular ATP accumulation may contribute to hyperexcitation of suburothelial nerve afferents via P2X3 receptors and to detrusor reactivity via P2X1 subunit-containing receptors, our study demonstrates that deficits in adenosine formation may also play a role in generating symptoms of bladder dysfunction in BPH patients. The loss of the inhibitory tone exerted by prejunctional A1 receptors on ACh release from stimulated cholinergic nerves in the detrusor may, thus, be a target for therapeutic intervention of bladder dysfunctions associated with outflow obstruction due to BPH. Evidence for the therapeutic potential of adenosine A1 receptor activation to decrease acetic acid-induced bladder overactivity has been recently gathered using anesthetized rats [49].
Acknowledgments
This research was partially supported by Fundação para a Ciência e a Tecnologia (FCT, FEDER funding, projects PTDC/SAU-OSM/104369/2008, REEQ/1168/SAU/2005, REEQ/1264/SAU/2005, and PEst-OE/SAU/UI0215/2014), Associação Portuguesa de Urologia (APU), and University of Porto/Caixa Geral de Depósitos (Investigação Científica na Pré-Graduação). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. IS was in receipt of a PhD Studentship from FCT (SFRH/BD/88855/2012). The authors wish to thank Mrs. Helena Costa e Silva and Belmira Silva for their valuable technical assistance.
Abbreviations
- ADA
Adenosine deaminase (EC 3.5.4.4)
- [3H]ACh
[3H]acetylcholine
- ANOVA
One-way analysis of variance
- BOO
Bladder outlet obstruction
- BPH
Benign prostatic hyperplasia
- DAPI
4′,6-Diamidino-2-phenylindole
- DPCPX
1,3-Dipropyl-8-cyclopentylxanthine
- DPM
Disintegrations per minute
- EFS
Electrical field stimulation
- EHNA
Erythro-9-(2-hydroxy-3-nonyl)adenine hydrochloride
- E-NTPDases
Ecto-nucleoside triphosphate diphosphohydrolases
- HPLC
High-performance liquid chromatography
- LUTS
Lower urinary tract symptoms
- R-PIA
N6-(L-2-phenylisopropyl) adenosine
- NECA
5′-(N-ethylcarboxamide) adenosine
- PBS
Physiological buffer solution
- PLP
Paraformaldehyde
- SD
Standard deviation
- VAChT
Vesicular acetylcholine transporter
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Author contributions
MSR and IS contributed equally to this work. PCS supervised the project, designed the experiments, and analyzed data. MSR, IS, and PCS wrote the paper. IS and MTMC performed and analyzed data from enzymatic kinetic experiments by HPLC. MF, IS, and MSR performed and analyzed data from in vitro myographic recordings. IS and MSR performed and analyzed data from acetylcholine and ATP release experiments. IS, JC, and FF performed immunofluorescence staining and confocal microscopy observations. MSR recruited the patients and collected the bladder samples. MSR, IS, MF, MTMC, JC, FF, and PCS interpreted data, discussed the clinical implications, and commented on the manuscript at all stages.
Footnotes
MSR and IS contributed equally to this work.
References
- 1.Mirone V, Imbimbo C, Longo N, Fusco F. The detrusor muscle: an innocent victim of bladder outlet obstruction. Eur Urol. 2007;51:57–66. doi: 10.1016/j.eururo.2006.07.050. [DOI] [PubMed] [Google Scholar]
- 2.Cowan WD, Daniel EE. Human female bladder and its noncholinergic contractile function. Can J Physiol Pharmacol. 1983;61:1236–1246. doi: 10.1139/y83-182. [DOI] [PubMed] [Google Scholar]
- 3.Dean DM, Downie JW. Contribution of adrenergic and “purinergic” neurotransmission to contraction in rabbit detrusor. J Pharmacol Exp Ther. 1978;207:431–445. [PubMed] [Google Scholar]
- 4.Levin RM, Ruggieri MR, Wein AJ. Functional effects of the purinergic innervation of the rabbit urinary bladder. J Pharmacol Exp Ther. 1986;236:452–457. [PubMed] [Google Scholar]
- 5.Burnstock G. Therapeutic potential of purinergic signalling for diseases of the urinary tract. BJU Int. 2011;107:192–204. doi: 10.1111/j.1464-410X.2010.09926.x. [DOI] [PubMed] [Google Scholar]
- 6.Yoshida M, Homma Y, Inadome A, et al. Age-related changes in cholinergic and purinergic neurotransmission in human isolated bladder smooth muscles. Exp Gerontol. 2001;36:99–109. doi: 10.1016/S0531-5565(00)00175-3. [DOI] [PubMed] [Google Scholar]
- 7.Ruggieri MR, Sr, Braverman AS. Regulation of bladder muscarinic receptor subtypes by experimental pathologies. Auton Autacoid Pharmacol. 2006;26:311–325. doi: 10.1111/j.1474-8673.2006.00377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey RA, Skennerton DE, Newgreen D, Fry CH. The contractile potency of adenosine triphosphate and ecto-adenosine triphosphatase activity in guinea pig detrusor and detrusor from patients with a stable, unstable or obstructed bladder. J Urol. 2002;168:1235–1239. doi: 10.1016/S0022-5347(05)64632-0. [DOI] [PubMed] [Google Scholar]
- 9.Wedenberg K, Ronquist G, Waldenstrom A, Ulmsten U. Low energy charge and high adenosine content in smooth muscle of human bladder in comparison with striated muscle. Int J Clin Lab Res. 1994;24:230–232. doi: 10.1007/BF02592470. [DOI] [PubMed] [Google Scholar]
- 10.Acevedo CG, Contreras E, Escalona J, Lewin J, Huidobro-Toro JP. Pharmacological characterization of adenosine A1 and A2 receptors in the bladder: evidence for a modulatory adenosine tone regulating non-adrenergic non-cholinergic neurotransmission. Br J Pharmacol. 1992;107:120–126. doi: 10.1111/j.1476-5381.1992.tb14473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown C, Burnstock G, Cocks T. Effects of adenosine 5′-triphosphate (ATP) and beta-gamma-methylene ATP on the rat urinary bladder. Br J Pharmacol. 1979;65:97–102. doi: 10.1111/j.1476-5381.1979.tb17337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicholls J, Hourani SM, Kitchen I. Characterization of P1-purinoceptors on rat duodenum and urinary bladder. Br J Pharmacol. 1992;105:639–642. doi: 10.1111/j.1476-5381.1992.tb09032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King JA, Huddart H, Staff WG. Purinergic modulation of rat urinary bladder detrusor smooth muscle. Gen Pharmacol. 1997;29:597–604. doi: 10.1016/S0306-3623(96)00573-3. [DOI] [PubMed] [Google Scholar]
- 14.Burnstock G, Cocks T, Crowe R, Kasakov L. Purinergic innervation of the guinea-pig urinary bladder. Br J Pharmacol. 1978;63:125–138. doi: 10.1111/j.1476-5381.1978.tb07782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubinstein R, Shalev M, Nissenkorn I, Cohen S. Effect of exogenous adenosine and its monophosphate on the contractile response to acetylcholine in the human isolated detrusor muscle strips. J Auton Pharmacol. 1998;18:99–104. doi: 10.1046/j.1365-2680.1998.1820099.x. [DOI] [PubMed] [Google Scholar]
- 16.Parija SC, Raviprakash V, Mishra SK. Adenosine- and alpha,beta-methylene ATP-induced differential inhibition of cholinergic and non-cholinergic neurogenic responses in rat urinary bladder. Br J Pharmacol. 1991;102:396–400. doi: 10.1111/j.1476-5381.1991.tb12185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang SJ, An JY, Shim JO, Park CH, Huh IH, Sohn UD. The mechanism of contraction by 2-chloroadenosine in cat detrusor muscle cells. J Urol. 2000;163:652–658. doi: 10.1016/S0022-5347(05)67952-9. [DOI] [PubMed] [Google Scholar]
- 18.Husted S, Sjogren C, Andersson KE. Direct effects of adenosine and adenine nucleotides on isolated human urinary bladder and their influence on electrically induced contractions. J Urol. 1983;130:392–398. doi: 10.1016/s0022-5347(17)51175-1. [DOI] [PubMed] [Google Scholar]
- 19.Dixon AK, Gubitz AK, Sirinathsinghji DJ, Richardson PJ, Freeman TC. Tissue distribution of adenosine receptor mRNAs in the rat. Br J Pharmacol. 1996;118:1461–1468. doi: 10.1111/j.1476-5381.1996.tb15561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Owen SJ, Massa HH, Rose’Meyer RB. Loss of adenosine A2B receptor mediated relaxant responses in the aged female rat bladder; effects of dietary phytoestrogens. Naunyn Schmiedeberg’s Arch Pharmacol. 2012;385:539–549. doi: 10.1007/s00210-011-0722-y. [DOI] [PubMed] [Google Scholar]
- 21.Duarte-Araújo M, Nascimento C, Timóteo MA, Magalhães-Cardoso T, Correia-de-Sá P. Dual effects of adenosine on acetylcholine release from myenteric motoneurons are mediated by junctional facilitatory A(2A) and extrajunctional inhibitory A(1) receptors. Br J Pharmacol. 2004;141:925–934. doi: 10.1038/sj.bjp.0705697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Correia-de-Sá P, Adães S, Timóteo MA, et al. Fine-tuning modulation of myenteric motoneurons by endogenous adenosine: on the role of secreted adenosine deaminase. Auton Neurosci. 2006;126–127:211–224. doi: 10.1016/j.autneu.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Carneiro I, Timóteo MA, Silva I, et al. Activation of P2Y6 receptors increases the voiding frequency in anaesthetized rats by releasing ATP from the bladder urothelium. Br J Pharmacol. 2014;171:3404–3419. doi: 10.1111/bph.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinheiro AR, Paramos-de-Carvalho D, Certal M, et al. Histamine induces ATP release from human subcutaneous fibroblasts, via pannexin-1 hemichannels, leading to Ca2+ mobilization and cell proliferation. J Biol Chem. 2013;288:27571–27583. doi: 10.1074/jbc.M113.460865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Timóteo MA, Carneiro I, Silva I, et al. ATP released via pannexin-1 hemichannels mediates bladder overactivity triggered by urothelial P2Y6 receptors. Biochem Pharmacol. 2014;87:371–379. doi: 10.1016/j.bcp.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Vieira C, Magalhães-Cardoso MT, Ferreirinha F, et al. Feed-forward inhibition of CD73 and upregulation of adenosine deaminase contribute to the loss of adenosine neuromodulation in postinflammatory ileitis. Mediat Inflamm. 2014;2014:254640. doi: 10.1155/2014/254640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arch JR, Newsholme EA. Activities and some properties of 5′-nucleotidase, adenosine kinase and adenosine deaminase in tissues from vertebrates and invertebrates in relation to the control of the concentration and the physiological role of adenosine. Biochem J. 1978;174:965–977. doi: 10.1042/bj1740965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Griffith DA, Jarvis SM. Nucleoside and nucleobase transport systems of mammalian cells. Biochim Biophys Acta. 1996;1286:153–181. doi: 10.1016/S0304-4157(96)00008-1. [DOI] [PubMed] [Google Scholar]
- 29.Agarwal RP, Spector T, Parks RE., Jr Tight-binding inhibitors—IV. Inhibition of adenosine deaminases by various inhibitors. Biochem Pharmacol. 1977;26:359–367. doi: 10.1016/0006-2952(77)90192-7. [DOI] [PubMed] [Google Scholar]
- 30.Burnstock G, Dumsday B, Smythe A. Atropine resistant excitation of the urinary bladder: the possibility of transmission via nerves releasing a purine nucleotide. Br J Pharmacol. 1972;44:451–461. doi: 10.1111/j.1476-5381.1972.tb07283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birder L, Andersson KE (2013) Urothelial signaling. Physiol Rev 93:653-80 [DOI] [PMC free article] [PubMed]
- 32.Aizawa N, Igawa Y, Andersson KE, Iijima K, Nishizawa O, Wyndaele JJ. Effects of intravesical instillation of ATP on rat bladder primary afferent activity and its relationship with capsaicin-sensitivity. Neurourol Urodyn. 2011;30:163–168. doi: 10.1002/nau.20940. [DOI] [PubMed] [Google Scholar]
- 33.Rocha I, Burnstock G, Spyer KM. Effect on urinary bladder function and arterial blood pressure of the activation of putative purine receptors in brainstem areas. Auton Neurosci. 2001;88:6–15. doi: 10.1016/S1566-0702(00)00284-8. [DOI] [PubMed] [Google Scholar]
- 34.Burnstock G, Cocks T, Kasakov L, Wong HK. Direct evidence for ATP release from non-adrenergic, non-cholinergic (“purinergic”) nerves in the guinea-pig taenia coli and bladder. Eur J Pharmacol. 1978;49:145–149. doi: 10.1016/0014-2999(78)90070-5. [DOI] [PubMed] [Google Scholar]
- 35.Cusack NJ, Hourani SM. Some pharmacological and biochemical interactions of the enantiomers of adenylyl 5′-(beta, gamma-methylene)-diphosphonate with the guinea-pig urinary bladder. Br J Pharmacol. 1984;82:155–159. doi: 10.1111/j.1476-5381.1984.tb16453.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang SX, Kobayashi T, Okada T, Garcia del Saz E, Seguchi H. Alkaline phosphatase, 5′-nucleotidase and magnesium-dependent adenosine triphosphatase activities in the transitional epithelium of the rat urinary bladder. Histol Histopathol. 1991;6:309–315. [PubMed] [Google Scholar]
- 37.Yu W, Robson SC, Hill WG. Expression and distribution of ectonucleotidases in mouse urinary bladder. PLoS One. 2011;6:e18704. doi: 10.1371/journal.pone.0018704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith DO, Lu Z. Adenosine derived from hydrolysis of presynaptically released ATP inhibits neuromuscular transmission in the rat. Neurosci Lett. 1991;122:171–173. doi: 10.1016/0304-3940(91)90850-S. [DOI] [PubMed] [Google Scholar]
- 39.Zhang Y, Xia Y. Adenosine signaling in normal and sickle erythrocytes and beyond. Microbes Infect. 2012;14:863–873. doi: 10.1016/j.micinf.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohlin C, Save S, Nilsson M, Persson K. Studies of the extracellular ATP-adenosine pathway in human urinary tract epithelial cells. Pharmacology. 2009;84:196–202. doi: 10.1159/000235908. [DOI] [PubMed] [Google Scholar]
- 41.Correia-de-Sá P. Pathophysiological significance of nucleotide hydrolyzing enzymes in urologic disorder. Purinergic Signal. 2010;6:S13.3. [Google Scholar]
- 42.Sheth S, Brito R, Mukherjea D, Rybak LP, Ramkumar V. Adenosine receptors: expression, function and regulation. Int J Mol Sci. 2014;15:2024–2052. doi: 10.3390/ijms15022024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burnstock G. Purinergic signalling in the urinary tract in health and disease. Purinergic Signal. 2014;10:103–155. doi: 10.1007/s11302-013-9395-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kosan M, Tul M, Ozturk B, Hafez G, Inal G, Cetinkaya M. Alteration in contractile responses in human detrusor smooth muscle from obstructed bladders with overactivity. Urol Int. 2008;80:193–200. doi: 10.1159/000112613. [DOI] [PubMed] [Google Scholar]
- 45.Bayliss M, Wu C, Newgreen D, Mundy AR, Fry CH. A quantitative study of atropine-resistant contractile responses in human detrusor smooth muscle, from stable, unstable and obstructed bladders. J Urol. 1999;162:1833–1839. doi: 10.1016/S0022-5347(05)68247-X. [DOI] [PubMed] [Google Scholar]
- 46.Correia-de-Sá P, Ribeiro JA (1996) Adenosine uptake and deamination regulate tonic A2a receptor facilitation of evoked [3H]acetylcholine release from the rat motor nerve terminals. Neuroscience 73:85–92 [DOI] [PubMed]
- 47.Gonçalves J, Queiroz G (1993) Facilitatory and inhibitory modulation by endogenous adenosine of noradrenaline release in the epididymal portion of rat vas deferens. Naunyn Schmiedeberg’s Arch Pharmacol 348:367–371 [DOI] [PubMed]
- 48.Sosnowski M, Yaksh TL. The role of spinal and brainstem adenosine receptors in the modulation of the volume-evoked micturition reflex in the unanesthetized rat. Brain Res. 1990;515:207–213. doi: 10.1016/0006-8993(90)90597-5. [DOI] [PubMed] [Google Scholar]
- 49.Kitta T, Chancellor MB, de Groat WC, Kuno S, Nonomura K, Yoshimura N. Roles of adenosine A1 and A2A receptors in the control of micturition in rats. Neurourol Urodyn. 2014;33:1259–1265. doi: 10.1002/nau.22487. [DOI] [PubMed] [Google Scholar]
- 50.Saito M, Kondo A, Kato T, Levin RM. Response of isolated human neurogenic detrusor smooth muscle to intramural nerve stimulation. Br J Urol. 1993;72:723–727. doi: 10.1111/j.1464-410X.1993.tb16256.x. [DOI] [PubMed] [Google Scholar]
- 51.Yoshida M, Miyamae K, Iwashita H, Otani M, Inadome A. Management of detrusor dysfunction in the elderly: changes in acetylcholine and adenosine triphosphate release during aging. Urology. 2004;63:17–23. doi: 10.1016/j.urology.2003.11.003. [DOI] [PubMed] [Google Scholar]