Abstract
Respiratory anthrax is a fatal disease in the absence of early treatment with antibiotics. Rabbits are highly susceptible to infection with Bacillus anthracis spores by intranasal instillation, succumbing within 2 to 4 days postinfection. This study aims to test the efficiency of antibiotic therapy to treat systemic anthrax in this relevant animal model. Delaying the initiation of antibiotic administration to more than 24 h postinfection resulted in animals with systemic anthrax in various degrees of bacteremia and toxemia. As the onset of symptoms in humans was reported to start on days 1 to 7 postexposure, delaying the initiation of treatment by 24 to 48 h (time frame for mass distribution of antibiotics) may result in sick populations. We evaluated the efficacy of antibiotic administration as a function of bacteremia levels at the time of treatment initiation. Here we compare the efficacy of treatment with clarithromycin, amoxicillin-clavulanic acid (Augmentin), imipenem, vancomycin, rifampin, and linezolid to the previously reported efficacy of doxycycline and ciprofloxacin. We demonstrate that treatment with amoxicillin-clavulanic acid, imipenem, vancomycin, and linezolid were as effective as doxycycline and ciprofloxacin, curing rabbits exhibiting bacteremia levels of up to 105 CFU/ml. Clarithromycin and rifampin were shown to be effective only as a postexposure prophylactic treatment but failed to treat the systemic (bacteremic) phase of anthrax. Furthermore, we evaluate the contribution of combined treatment of clindamycin and ciprofloxacin, which demonstrated improvement in efficacy compared to ciprofloxacin alone.
INTRODUCTION
Bacillus anthracis, the causative agent of anthrax, is a Gram-positive aerobic spore-forming bacillus (1). The exact disease caused by this virulent bacterium depends on the route of infection (2, 3). Cutaneous exposure causes a local disease with typical lesions that without treatment might develop into systemic disease. Oral consumption of spores can lead to an oropharyngeal or gastrointestinal infection, which can be fatal. In contrast, respiratory exposure to spores leads directly to a fulminant systemic disease which is fatal without treatment (4, 5). In respiratory anthrax in humans, the incubation time from infection until the onset of symptoms is estimated to be 1 to 7 days. The disease begins with nonspecific flu-like symptoms lasting 2 to 3 days, with a sudden progression to severe respiratory distress and shock leading to death within 24 to 36 h. In experimental animal models, there are no preceding physiological symptoms, even with bacteremia, until the development of severe respiratory distress at the late stage in close proximity to death (6). Therefore, disease progression is characterized by levels of blood bacteremia and protective antigen (PA) concentrations, two closely correlated markers considered a reliable measure of disease severity in animal models (7).
The importance of timely and effective treatment was demonstrated in the 2001 anthrax bioterrorism attack in the United States, when 5 of the 10 inhalational anthrax patients died in spite of massive antibiotic administration, probably due to the use of ineffective antibiotic therapy and/or delayed treatment initiation (i.e., during the fulminating stage of the disease) (8, 9). Effective postexposure therapy protocols preventing the establishment of fatal anthrax disease have been reported in the literature. Postexposure treatment with penicillin (10–12), doxycycline (10), ciprofloxacin (10, 13), and levofloxacin (13) efficiently protected rhesus monkeys following inhalation of lethal doses of virulent B. anthracis spores. In guinea pigs, treatment with penicillin (14), doxycycline (15), tetracycline (16), ciprofloxacin (15, 16), and erythromycin (16) protected the animals, but upon treatment termination, the animals died due to anthrax relapse (12, 15, 16). To develop improved/alternative treatment protocols for systemic anthrax, we previously evaluated the efficacy of antibiotic treatment at different stages based on bacteremia levels (17). In rabbits, treatment with ciprofloxacin (17), levofloxacin (18), or doxycycline (17) was efficient in preventing the death of animals with systemic anthrax. Furthermore, combination of anti-PA antibodies with either ciprofloxacin or levofloxacin therapy demonstrated improved efficacy compared to the single-antibiotic treatment (17, 19).
Recently, the Centers for Disease Control and Prevention (CDC) updated the guidelines for prevention and treatment of anthrax, designating three treatment protocols for the disease: postexposure prophylaxis, systemic anthrax without meningitis, and systemic anthrax with suspected or confirmed meningitis (20). The current version emphasizes combination antimicrobial therapy for systemic anthrax with three or more drugs. Optional antimicrobials include the following: ciprofloxacin, levofloxacin, moxifloxacin, doxycycline, amoxicillin, clindamycin, meropenem, penicillin or ampicillin, linezolid, chloramphenicol, rifampin, and vancomycin. It should be mentioned that only in vitro sensitivity data are available for the majority of the suggested antimicrobial drugs (21), while there is a substantial gap in knowledge regarding their individual in vivo efficacy, as well as the efficacy of combined therapy.
Herein, we tested single- or dual-antibiotic administration in order to evaluate their efficacy, in a relevant animal model, both as postexposure prophylaxis and as systemic anthrax therapy (characterized by the presence of both bacteria and toxins in the circulation system).
MATERIALS AND METHODS
B. anthracis strain.
The B. anthracis strain used in this study was ATCC 14578 (Vollum) (Tox+ Cap+) from the Israel Institute for Biological Research (IIBR) collection (22).
Animals.
New Zealand White rabbits (2.5 to 3.5 kg) were obtained from Charles River (USA). The animals received food and water ad libitum. The animals were inoculated via the respiratory route by intranasal (i.n.) instillation. The estimation of a 50% lethal dose (LD50) administered i.n. in rabbits is 2 × 104 CFU (23).
This study was carried out in strict accordance with the recommendations of the Guide for the Care and Use of Laboratory Animals of the National Research Council (24). The protocols were approved by the Committee on the Ethics of Animal Experiments of the IIBR.
Exposure and treatment regimens.
Groups of 12 to 30 rabbits were inoculated i.n. with 2 × 106 to 6 × 106 (100 LD50) B. anthracis Vollum spores. For single-antibiotic treatments, 32 h postinoculation, blood samples were drawn from the rabbit's ear vein to determine the level of bacteremia, and the animals were immediately treated with antibiotics. For dual-antibiotic treatment with ciprofloxacin and clindamycin, blood samples were drawn from the ear vein starting at 30 h, and every 2 h afterwards for determination of serum PA levels by immune assay. For each animal, the individual treatment initiation time was defined according to the blood PA level (>40 ng/ml). Single-antibiotic treatment continued twice daily for a period of 14 days, and combined treatment continued for 3 days (due to known toxicity of clindamycin to rabbits) followed by single treatment with ciprofloxacin alone for 11 days. Afterwards, the animals were monitored for survival for an additional 30 days. To test the effect of treatment on the development of specific protective immune response, the surviving animals were tested for acquired protective immunity by subcutaneous injection of 2 × 104 (1,000 LD50) Vollum spores (23).
ELISA for PA.
Serum levels of PA were determined as previously reported (17). Briefly, PA levels were determined by direct enzyme-linked immunosorbent assay (ELISA) in 96-well microtiter plates (Nunc, Roskilde, Denmark), using purified PA as the reference standard. The wells in the plates were coated with 100 μg/ml of diluted rabbit serum anti-PA in NaHCO3 buffer (50 mM, pH 9.6), and the reaction was subsequently blocked with 5% skim milk (Becton Dickinson, Sparks, MD). The wells were washed with phosphate-buffered saline containing 0.05% Tween 20 (PBST) and incubated with the tested sera (diluted 1:2 in 0.5% skim milk) for 1 h at 37°C. For the standard curve, known concentrations of purified PA in 50% serum were used. The wells were washed with PBST and incubated with diluted rabbit anti-PA serum. After the wells were rinsed with PBST, the plates were developed with alkaline phosphatase-conjugated goat anti-rabbit immunoglobulin G (IgG) (Sigma, St. Louis, MO) as the detecting reagent and p-nitrophenyl phosphate (Sigma, St. Louis, MO) as the substrate. Absorbance at 405 nm was determined using a Spectramax 190 microplate reader (Molecular Devices, Sunnyvale, CA). The endpoint was defined as the highest dilution at which the absorbance was >3 standard deviations above that of the negative control. The sensitivity of this assay was determined as 10 ng/ml PA.
In vitro toxin secretion assays.
The level of PA secretion in response to different concentrations of ciprofloxacin and clindamycin was determined by a broth microdilution test. The antibiotic was diluted in NBY-HCO3 medium (8 g nutrient broth, 3 g yeast extract, 5 g glucose, 9 g NaHCO3 in 1 liter medium), and the B. anthracis Vollum vegetative bacteria were added to a final concentration of 5 × 105 CFU/ml. The plates were incubated at 37°C in 10% CO2 atmosphere for 16 h. The PA concentration was determined by an ELISA, and the bacterial concentration was determined by serial dilution and colony counts on tryptose agar plates.
Determination of bacteremia.
Bacterial levels in blood were determined as previously reported (16). Briefly, each blood sample was plated undiluted and after serial dilutions in saline. The plates were incubated for 16 h at 37°C, and bacteremia was determined by colony counting. The lower limit of detection was 5 CFU/ml.
Pharmacokinetics of the antibiotics in rabbits.
The pharmacokinetics of each antibiotic used in this work are presented in Table 1. Blood samples were drawn from rabbits at various time points after antibiotic administration, and the concentration of the antibiotic in serum was defined by determining the highest serum dilution that inhibits the growth of B. anthracis VollumΔpXO1ΔpXO2. The serum inhibitory concentration (SIC) is presented as the reciprocal of the maximal inhibitory dilution. All the antibiotics tested, administered by different routes, showed significant serum inhibitory concentration, lasting for several hours.
TABLE 1.
Pharmacokinetics of tested antibiotics in rabbitsa
| Trade name or product name (company) | Antibiotic agent(s) | Administration route | Dose (mg/kg) | Cmax (SIC) | Tmax (h) | Tmin (h) |
|---|---|---|---|---|---|---|
| Augmentin | Amoxicillin-clavulanic acid | i.v. | 150b | 125 | 1 | 12 |
| s.c. | 100 | 125 | 1 | 9 | ||
| Vancomycin (Mylan) | Vancomycin | i.v. | 40 | 55 | 1 | 7 |
| s.c. | 30 | 2 | 12 | |||
| Tienam | Imipenem-cilastatin | i.v. | 20 | 12 | 0.5 | 2.5 |
| s.c. | 12 | 0.5 | 4 | |||
| Rifadin | Rifampin | p.o. | 50 | 13 | 0.5 | 6 |
| Kalcidc | Clarithromycin | p.o. | 80 | 8 | 2 | 12 |
| Zyvoxid | Linezolid | p.o. | 50 | 30 | 3 | 6 |
Abbreviations: Cmax, maximum concentration of drug in serum; SIC, serum inhibitory concentration; Tmax, time to maximum concentration of drug in serum, Tmin, time to minimum concentration of drug in serum.
Concentration of amoxicillin.
Pharmacokinetic data for Kalcid are from Shirtliff et al. (30).
Statistical analysis.
The statistical significance of the differences in survival rates between treated groups and untreated controls and differences in bacteremia and time to treatment was determined by Fisher's exact test, two tailed, using Prism 6 software (Graphpad, USA).
RESULTS
Efficacy of single-antibiotic treatments.
In this study, we evaluated the efficiency of different antibiotic agents, which are available in hospitals or in community health care centers, to treat experimentally induced respiratory anthrax. The antibiotics tested were selected according to their mechanism of action. Amoxicillin-clavulanic acid (Augmentin) (β-lactams), vancomycin (glycopeptides), and imipenem (carbapenems) represent the cell wall synthesis inhibitory agents. Rifampin was tested as an RNA inhibitor, and from the protein synthesis inhibitors, clarithromycin (macrolides) and linezolid (oxazolidinone) were used. Treatment efficacy was studied using our previously reported rabbit model (17), in which bacteremia levels serve as a marker for systemic disease progression following intranasal instillation of B. anthracis Vollum spores. Based on our experience, we defined 32 h postexposure as the time point to determine the bacteremia level and administer antibiotics, allowing for a wide range of bacteremia levels for treatment. In all experiments, the inoculation dose was 100 to 200 LD50 of Vollum spores, and antibiotic treatment started 32 h postinjection and continued twice daily for 14 days. To ensure rapid systemic antibiotic dispersion, the first dose was administered intravenously (i.v.) (when the adequate product was available) and the following doses were administered subcutaneously (s.c.).
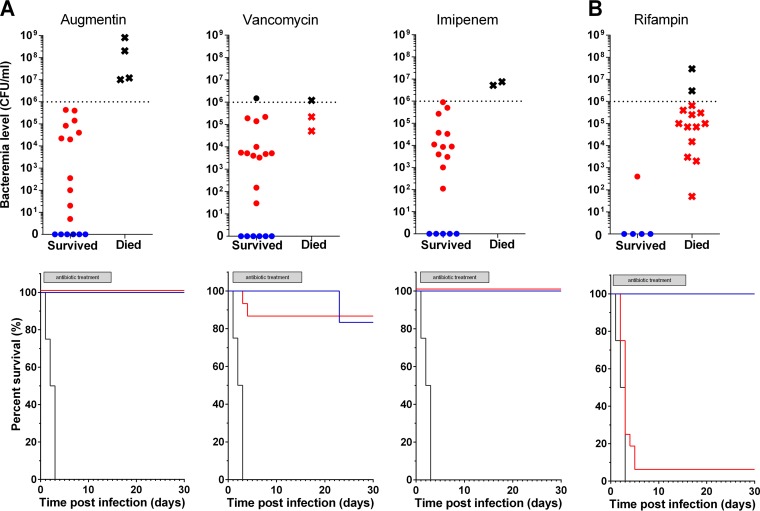
Cell wall synthesis inhibitor treatment regimens initiated with an i.v. antibiotic administration and were followed by s.c. antibiotic injections (Table 1). The antibiotic treatment was given to groups of 21, 23, and 19 rabbits (for amoxicillin-clavulanic acid, vancomycin, and imipenem, respectively). As demonstrated in Fig. 1A (top panels), all the cell wall inhibitors were very effective as postexposure prophylaxis, preventing the development of anthrax when the treatment started before the onset of bacteremia (blue symbols). Those antibiotics were also very effective in curing highly bacteremic rabbits (red symbols) with bacteremia loads of up to 106 CFU/ml (amoxicillin-clavulanic acid [Augmentin] and imipenem) and 105 CFU/ml (vancomycin). After the cessation of antibiotic treatment, all the surviving animals were monitored for an additional period of 14 days. Our findings demonstrate that except for one animal (treated with imipenem), all the animals were cured (Fig. 1A, bottom panels). Seroconversion was observed in all the bacteremic animals that were treated with vancomycin and imipenem (data not shown). It should be mentioned that after cessation of treatment with amoxicillin-clavulanic acid, the rabbits developed severe, non-anthrax-related diarrhea that caused death in five animals.
FIG 1.
Efficacy during and after treatment with cell wall synthesis inhibitors (A) and nucleic acid synthesis inhibitors (B). The rabbits were infected by i.n. instillation of B. anthracis Vollum spores, and treatment was initiated 32 h postinfection. (Top) Bacteremia level of each individual rabbit at treatment initiation and the outcome of the treatment (during the antibiotic administration; live [circle] or dead [x]). The animals that received prophylactic treatment (sterile at treatment initiation) are shown in blue. Rabbits with bacteremia in the range of 10 to 106 CFU/ml are shown in red. Rabbits with bacteremia higher than 106 CFU/ml are shown in black. Each symbol represents the value for an individual animal. (Bottom) Survival rate with time. Treatment of the groups is indicated by color as follows: black, untreated animals; blue, prophylactic treatment; red, treatment of bacteremic animals with bacteremia of 10 to 106 CFU/ml. The gray boxes indicate the duration of antibiotic treatment. Dotted lines indicate the highest bacteremia levels included in the lower panels.
Treatment with the RNA inhibitor rifampin was conducted on 20 infected rabbits, and treatment was administered per os (p.o.) twice daily (Table 1). Prophylactic treatment was given to five rabbits, whereas the rest were bacteremic at treatment initiation. As can be clearly seen from the data presented in Fig. 1B (top and bottom panels), rifampin failed to cure bacteremic animals or even delay the time to death and was effective only as a prophylactic treatment. No relapse of the disease was observed in the group given rifampin prophylactically (Fig. 1B, bottom panel).
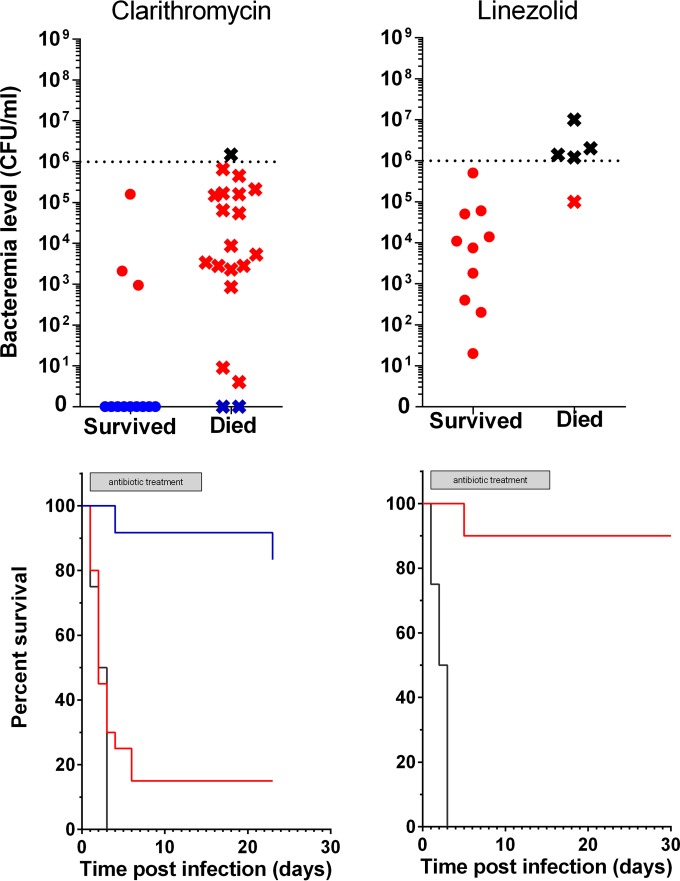
The treatment regimen for protein synthesis inhibitors included p.o. administration of clarithromycin or linezolid (Table 1). Our data demonstrate that these two antibiotics were effective as prophylactic treatments (Fig. 2, blue symbols and lines) and that linezolid was very efficient in curing highly bacteremic animals, with bacteremia levels of 105 to 106 CFU/ml (Fig. 2. red symbols and lines). Clarithromycin, on the other hand, failed to cure animals even at very low bacteremia levels (Fig. 2, red symbols and lines) and was effective only as a prophylactic treatment (Fig. 2, blue symbols and lines).
FIG 2.
Efficacy during and after treatment with protein synthesis inhibitors. The rabbits were infected by i.n. instillation of B. anthracis Vollum spores, and treatment was initiated 32 h postinfection. (Top) Bacteremia level of each individual rabbit at treatment initiation and the outcome of the treatment (during the antibiotic administration; live [circle] or dead [x]). The animals that received prophylactic treatment (sterile at treatment initiation) are shown in blue. Rabbits with bacteremia in the range of 10 to 106 CFU/ml are shown in red. Rabbits with bacteremia higher than 106 CFU/ml are shown in black. (Bottom) Survival rate with time. Treatment of the groups is indicated by color as follows: black, untreated animals; blue, prophylactic treatment; red, treatment of bacteremic animals with bacteremia of 10 to 106 CFU/ml. The gray boxes indicate the duration of antibiotic treatment. Dotted lines indicate the highest bacteremia levels included in the lower panels.
Efficacy of combined antibiotic treatment.
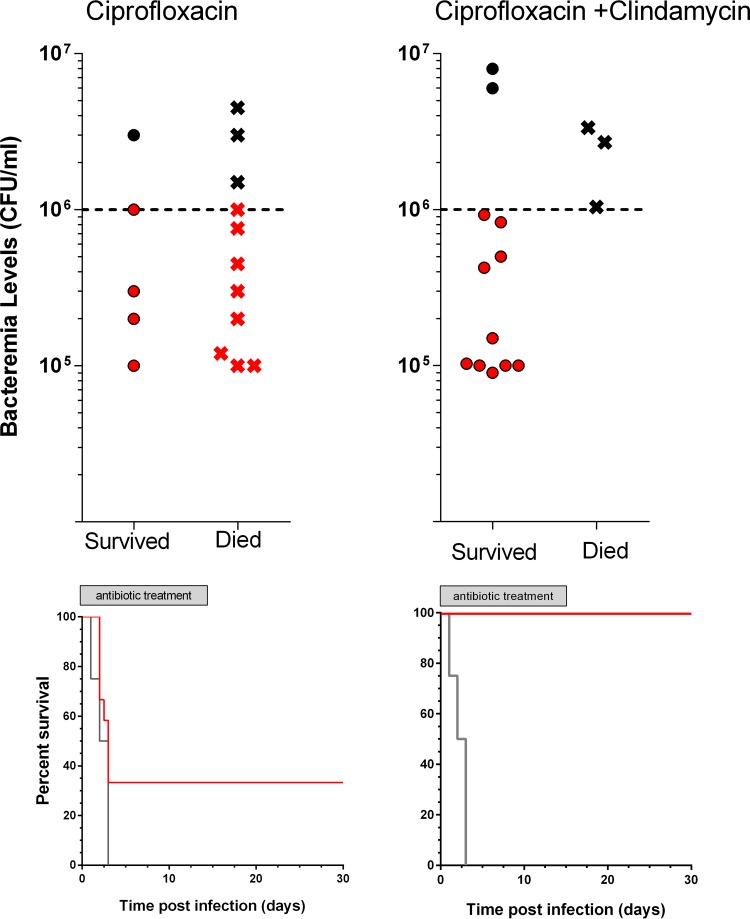
In a previous study (17), we had demonstrated that ciprofloxacin treatment was effective for treating animals with bacteremia levels of up to 105 CFU/ml. We were also able to demonstrate the added benefit of combined treatment of ciprofloxacin with anti-PA antibodies in animals that had bacteremia levels in the range between 105 and 106 CFU/ml. Therefore, we decided to evaluate the efficacy of combined treatment with ciprofloxacin and clindamycin, a combination that was recommended by the CDC (20), in animals with bacteremia levels of 105 to 107 CFU/ml. In order to determine when each individual animal was in the required bacteremia range for treatment initiation, levels of PA in the sera were used to predict the level of bacteremia (7). For that purpose, 32 animals were inoculated with 100 to 200 LD50 B. anthracis Vollum spores. Blood was drawn from the ear vein, and serum PA levels were determined by a rapid immunoassay, starting 30 h postinfection and every 2 h thereafter. Antibiotic treatment was initiated when the infected animals had serum PA levels higher than 40 ng/ml. The initial combined treatment, with ciprofloxacin (60 mg/kg of body weight, p.o.) and clindamycin (60 mg/kg, i.v.), was given to 15 animals and was compared to single-antibiotic treatment (only ciprofloxacin) that was given to 16 animals (one animal died before antibiotics were administered). The combined treatment was continued for 3 days (with clindamycin administered subcutaneously), and from days 4 to 14, both groups were treated with ciprofloxacin only. As seen in Fig. 3, both groups were statistically identical, exhibiting similar bacteremia ranges and treated at similar time points after infection. Whereas the ciprofloxacin treatment cured only 33% of the animals (4/12), the combined treatment of animals with initial bacteremia of up to 106 CFU/ml exhibited an impressive statistically significant improvement (P = 0.0102) by curing 100% of the treated animals (10/10). No monotreatment experiment using clindamycin was preformed due to known toxicity to rabbits.
FIG 3.
Efficacy during and after combined treatment. (Top) Bacteremia level of each individual rabbit at treatment initiation and the outcome of the treatment (live [circle] or dead [x]). Rabbits with bacteremia in the range of 10 to 106 CFU/ml are shown in red. Rabbits with bacteremia higher than 106 CFU/ml are shown in black. (Bottom) Survival rate with time. Treatment of the groups is indicated by color as follows: black, untreated; red, treatment of bacteremic animals with bacteremia of 10 to 106 CFU/ml. The gray boxes indicate the duration of antibiotic treatment. Dotted lines indicate the highest bacteremia levels included in the lower panels.
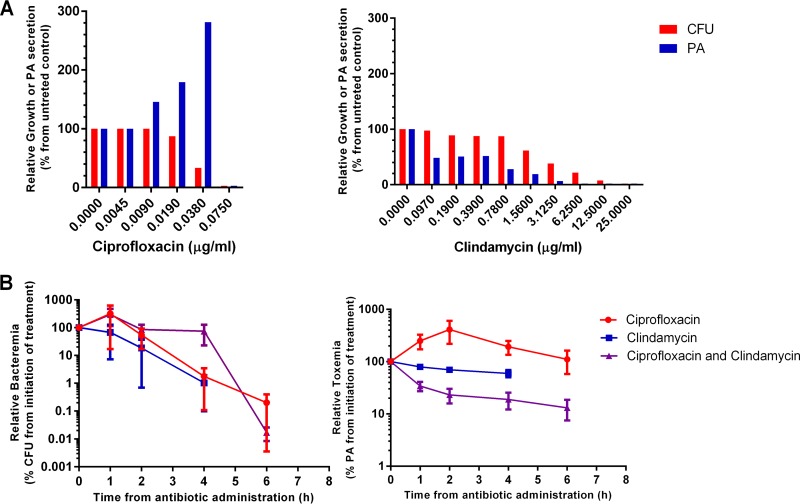
In an attempt to elucidate the mechanisms underlying this observation, we studied the effects of the two antibiotics on the proliferation of the bacteria and on the release of the toxins (PA), both in vitro and in vivo. As can be seen in Fig. 4A (in vitro experiments), ciprofloxacin exhibits strong inhibition of bacterial proliferation, accompanied by a significant increase in toxin concentration. In contrast, clindamycin showed a strong reduction in toxin secretion, even at concentrations subinhibitory for proliferation. Therefore, we can assume that clindamycin's contribution to the increased curative effect of the combined treatment relies on its ability to inhibit the increased toxin secretion. This conclusion is substantiated by the in vivo studies (Fig. 4B), where our data suggest an increased effect of the combined antibiotic treatment on the toxin secretion, but not on bacterial proliferation in comparison to single-antibiotic treatments with ciprofloxacin or clindamycin.
FIG 4.
Pharmacodynamics of ciprofloxacin and clindamycin in vitro and in vivo. (A) In vitro effect of increasing concentrations of ciprofloxacin or clindamycin on bacterial growth (red) or PA secretion (blue). (B) Pharmacodynamics of bacteremia (left) or serum PA (right) following the initiation of antibiotic treatment.
DISCUSSION
Rapid initiation of antimicrobial therapy is crucial in the management of severe infection and sepsis. Proper selection of an antimicrobial treatment regimen against the infectious agent, with optimal pharmacokinetic and pharmacodynamic characteristics, is highly important (25). The same principles are important in the case of systemic anthrax, for which the delay in antibiotic treatment is tightly associated with increased mortality. The recommendations for antibiotic treatment of inhalational anthrax are mainly based on in vitro susceptibility testing, in vivo animal studies, and fragmented clinical experience, as no clinical human studies of these infections are available. Previous studies of animal models and reports on the treatment of systemic anthrax in humans have demonstrated that ciprofloxacin treatment is highly efficient (26). Current CDC guidelines recommend single treatment with a fluoroquinolone or tetracycline as postexposure prophylaxis and combination therapy for the established disease. For patients with proven or suspected meningitis, the recommended combination includes a fluoroquinolone (ciprofloxacin or levofloxacin), a bactericidal cell wall-acting agent (e.g., meropenem), and a protein synthesis inhibitor (e.g., linezolid). If meningitis is ruled out, treatment can include a fluoroquinolone and a protein synthesis inhibitor only (e.g., linezolid or clindamycin). Combinational antimicrobial treatment is not usually recommended for most infectious diseases due to possible unexpected antagonistic effects of the antibiotics. It has, however, an important role for specific indications, including broad coverage of polymicrobial infections, empirical coverage for agents with suspected antibacterial resistance, and in cases of synergistic effects of the individual components. Limited in vitro testing has been done to evaluate combination therapy for B. anthracis. In a study by Athamna et al. (27), most combinations have shown no synergism, including the recommended combinations of ciprofloxacin with linezolid, clindamycin, and rifampin, and some combinations were even antagonistic. Only the combination of rifampin and clindamycin was shown to be synergistic (27). Brook et al. (28) have examined the effect of combination treatment in an irradiated mouse model with B. anthracis Sterne infection. The addition of clindamycin to ciprofloxacin actually increased mortality (28). Clinically, retrospective studies have shown that combination treatment was associated with decreased mortality (29).
In this article, we report on our studies of rabbits, determining the efficacy of treatment with single antibiotics on anthrax in different stages of the disease from postexposure prophylaxis to advanced systemic disease (highly bacteremic animals). As can be seen, all the antibiotics tested were effective as prophylactic treatments for as long as the drugs were given. Prophylactic treatment with vancomycin and clarithromycin failed to prevent disease upon cessation of treatment. Antibiotic treatment does not eliminate all the spores from the lungs, and residual spores can initiate the development of the disease. This can be prevented by either prolonged treatment or combining treatment with the administration of active-PA-based vaccines.
In previous publications, we and others have shown in several animal models that established systemic anthrax can be treated with antibiotics. In this study, we tested additional antibiotics demonstrating their relative efficacy. Whereas the cell wall synthesis inhibitors amoxicillin-clavulanic acid, vancomycin, and imipenem were very efficient in treating systemic anthrax, the RNA inhibitor rifampin failed to cure rabbits. Imipenem and rifampin, with similar SICs and kinetics, achieve a completely different treatment outcome, indicating a possible difference between their in vivo and in vitro efficacies. The protein synthesis inhibitors show variations in their efficacy, as linezolid did cure bacteremic rabbits, while clarithromycin completely failed to save them. A possible reason for the discrepancy in this case relies on the fact that clarithromycin's MIC for B. anthracis (0.25 to 0.5 μg/ml) is in the upper borderline of the sensitive range (as determined for staphylococcus) (www.medsafe.govt.nz/Profs/datasheet/k/klacidtabsuspivinj.pdf), whereas all the other protein synthesis inhibitors are in the sensitive range.
The beneficial effect of the combination of antibiotics with different mechanisms of action is demonstrated in the ciprofloxacin-clindamycin experiments. The reduction in toxin secretion induced by clindamycin seems to contribute to the increased curative effect of the combined antibiotic treatment. Further studies should be carried out to demonstrate that the suggested mechanism underlies the additive effect.
Herein, we report the efficacy of single-antibiotic treatments on different stages of systemic anthrax. These data can contribute to the building of a robust experimental base for crafting better recommendations for efficient prevention and treatment of anthrax.
ACKNOWLEDGMENTS
We thank Nili Rothschild for excellent technical assistance. Special thanks to Avigdor Shafferman, Arie Ordentlich, Shmuel Yitzhaki, and Tal Brosh-Nissimov for fruitful discussions.
REFERENCES
- 1.Hanna P. 1998. Anthrax pathogenesis and host response. Curr Top Microbiol Immunol 225:13–35. [DOI] [PubMed] [Google Scholar]
- 2.Swartz MN. 2001. Recognition and management of anthrax - an update. N Engl J Med 345:1621–1626. [DOI] [PubMed] [Google Scholar]
- 3.Dixon TC, Meselson M, Guillemin J, Hanna PC. 1999. Anthrax. N Engl J Med 341:815–826. doi: 10.1056/NEJM199909093411107. [DOI] [PubMed] [Google Scholar]
- 4.Taft SC, Weiss AA. 2008. Toxicity of anthrax toxin is influenced by receptor expression. Clin Vaccine Immunol 15:1330–1336. doi: 10.1128/CVI.00103-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abbott NJ, Patabedige AAK, Dolman DEM, Yusof SR, Begley DJ. 2010. Structure and function of the blood-brain barrier. Neurobiol Dis 37:13–25. doi: 10.1016/j.nbd.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 6.Chitlaru T, Altboum Z, Reuveny S, Shafferman A. 2011. Progress and novel strategies in vaccine development and treatment of anthrax. Immunol Rev 239:221–236. doi: 10.1111/j.1600-065X.2010.00969.x. [DOI] [PubMed] [Google Scholar]
- 7.Kobiler D, Weiss S, Levy H, Fisher M, Mechaly A, Pass A, Altboum Z. 2006. Protective antigen as a correlative marker for anthrax in animal models. Infect Immun 74:5871–5876. doi: 10.1128/IAI.00792-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jernigan DB, Raghunathan PL, Bell BP, Brechner R, Bresnitz EA, Butler JC, Cetron M, Cohen M, Doyle T, Fischer M, Greene C, Griffith KS, Guarner J, Hadler JL, Hayslett JA, Meyer R, Petersen LR, Phillips M, Pinner R, Popovic T, Quinn CP, Reefhuis J, Reissman D, Rosenstein N, Schuchat A, Shieh WJ, Siegal L, Swerdlow DL, Tenover FC, Traeger M, Ward JW, Weisfuse I, Wiersma S, Yeskey K, Zaki S, Ashford DA, Perkins BA, Ostroff S, Hughes J, Fleming D, Koplan JP, Gerberding JL. 2002. Investigation of bioterrorism-related anthrax, United States, 2001: epidemiologic findings. Emerg Infect Dis 8:1019–1028. doi: 10.3201/eid0810.020353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jernigan JA, Stephens DS, Ashford DA, Omenaca C, Topiel MS, Galbraith M, Tapper M, Fisk TL, Zaki S, Popovic T, Meyer RF, Quinn CP, Harper SA, Fridkin SK, Sejvar JJ, Shepard CW, McConnell M, Guarner J, Shieh WJ, Malecki JM, Gerberding JL, Hughes JM, Perkins BA, Anthrax Bioterrorism Investigation Team. 2001. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg Infect Dis 7:933–944. doi: 10.3201/eid0706.010604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedlander AM, Welkos SL, Pitt ML, Ezzell JW, Worsham PL, Rose KJ, Ivins BE, Lowe JR, Howe GB, Mikesell P, Lawrence WB. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J Infect Dis 167:1239–1243. doi: 10.1093/infdis/167.5.1239. [DOI] [PubMed] [Google Scholar]
- 11.Brojatsch J, Casadevall A, Goldman DL. 2014. Molecular determinants for a cardiovascular collapse in anthrax. Front Biosci (Elite Ed) 6:139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henderson DW, Peacock S, Belton FC. 1956. Observations on the prophylaxis of experimental pulmonary anthrax in the monkey. J Hyg (Lond) 54:28–36. doi: 10.1017/S0022172400044272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beste KY, Spangler CM, Burhenne H, Koch KW, Shen Y, Tang WJ, Kaever V, Seifert R. 2013. Nucleotidyl cyclase activity of particulate guanylyl cyclase A: comparison with particulate guanylyl cyclases E and F, soluble guanylyl cyclase and bacterial adenylyl cyclases CyaA and edema factor. PLoS One 8:e70223. doi: 10.1371/journal.pone.0070223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seifert R, Dove S. 2013. Inhibitors of Bacillus anthracis edema factor. Pharmacol Ther 140:200–212. doi: 10.1016/j.pharmthera.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Moayeri M, Crown D, Jiao GS, Kim S, Johnson A, Leysath C, Leppla SH. 2013. Small-molecule inhibitors of lethal factor protease activity protect against anthrax infection. Antimicrob Agents Chemother 57:4139–4145. doi: 10.1128/AAC.00941-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Altboum Z, Gozes Y, Barnea A, Pass A, White M, Kobiler D. 2002. Postexposure prophylaxis against anthrax: evaluation of various treatment regimens in intranasally infected guinea pigs. Infect Immun 70:6231–6241. doi: 10.1128/IAI.70.11.6231-6241.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiss S, Kobiler D, Levy H, Pass A, Ophir Y, Rothschild N, Tal A, Schlomovitz J, Altboum Z. 2011. Antibiotics cure anthrax in animal models. Antimicrob Agents Chemother 55:1533–1542. doi: 10.1128/AAC.01689-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corey A, Migone TS, Bolmer S, Fiscella M, Ward C, Chen C, Meister G. 2013. Bacillus anthracis protective antigen kinetics in inhalation spore-challenged untreated or levofloxacin/raxibacumab-treated New Zealand white rabbits. Toxins (Basel) 5:120–138. doi: 10.3390/toxins5010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schein CH, Chen D, Ma L, Kanalas JJ, Gao J, Jimenez ME, Sower LE, Walter MA, Gilbertson SR, Peterson JW. 2012. Pharmacophore selection and redesign of non-nucleotide inhibitors of anthrax edema factor. Toxins (Basel) 4:1288–1300. doi: 10.3390/toxins4111288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hendricks KA, Wright ME, Shadomy SV, Bradley JS, Morrow MG, Pavia AT, Rubinstein E, Holty J-EC, Messonnier NE, Smith TL, Pesilk N, Treadwell TA, Bower WA, Workgroup on Anthrax Clinical Guidelines. 2014. Centers for Disease Control and Prevention expert panel meetings on prevention and treatment of anthrax in adults. Emerg Infect Dis 20:e130687. doi: 10.3201/eid2002.130687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y, Cui X, Solomon SB, Remy K, Fitz Y, Eichacker PQ. 2013. B. anthracis edema toxin increases cAMP levels and inhibits phenylephrine-stimulated contraction in a rat aortic ring model. Am J Physiol Heart Circ Physiol 305:H238–H250. doi: 10.1152/ajpheart.00185.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levy H, Fisher M, Ariel N, Altboum Z, Kobiler D. 2005. Identification of strain specific markers in Bacillus anthracis by random amplification of polymorphic DNA. FEMS Microbiol Lett 244:199–205. doi: 10.1016/j.femsle.2005.01.039. [DOI] [PubMed] [Google Scholar]
- 23.Levy H, Weiss S, Altboum Z, Schlomovitz J, Glinert I, Sittner A, Shafferman A, Kobiler D. 2012. Differential contribution of Bacillus anthracis toxins to pathogenicity in two animal models. Infect Immun 80:2623–2631. doi: 10.1128/IAI.00244-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Research Council. 2011. Guide for the care and use of laboratory animals, 8th ed National Academies Press, Washington, DC. [Google Scholar]
- 25.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Seransky JE, Sprung CL, Douglas IS, Jeachke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R, Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup. 2013. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vietri NJ, Purcell BK, Lawler JV, Leffel EK, Rico P, Gamble CS, Twenhafel NA, Ivins BE, Heine HS, Sheeler R, Wright ME, Friedlander AM. 2006. Short-course postexposure antibiotic prophylaxis combined with vaccination protects against experimental inhalational anthrax. Proc Natl Acad Sci U S A 103:7813–7816. doi: 10.1073/pnas.0602748103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Athamna A, Athamna M, Nura A, Shlyakov E, Bast DJ, Farrell D, Rubinstein E. 2005. Is in vitro antibiotic combination more effective than single-drug therapy against anthrax? Antimicrob Agents Chemother 49:1323–1325. doi: 10.1128/AAC.49.4.1323-1325.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brook I, Germana A, Giraldo DE, Camp-Hyde TD, Bolduc DL, Foriska MA, Elliott TB, Thakar JH, Shoemaker MO, Jackson WE, Ledney GD. 2005. Clindamycin and quinolone therapy for Bacillus anthracis Sterne infection in 60Co-gamma-photon-irradiated and sham-irradiated mice. J Antimicrob Chemother 56:1074–1080. [DOI] [PubMed] [Google Scholar]
- 29.Holty J-EC, Bravata DM, Liu H, Olshen RA, McDonald KM, Owens DK. 2006. Systemic review: a century of inhalational anthrax cases from 1900 to 2005. Ann Intern Med 144:270–280. [DOI] [PubMed] [Google Scholar]
- 30.Shirtliff ME, Mader JT, Calhoun J. 1999. Oral rifampin plus azithromycin or clarithromycin to treat osteomyelitis in rabbits. Clin Orthop Relat Res 1999:229–236. [DOI] [PubMed] [Google Scholar]