Abstract
Objectives
Healing in cancellous metaphyseal bone might be different from midshaft fracture healing due to different access to mesenchymal stem cells, and because metaphyseal bone often heals without a cartilaginous phase. Inflammation plays an important role in the healing of a shaft fracture, but if metaphyseal injury is different, it is important to clarify if the role of inflammation is also different. The biology of fracture healing is also influenced by the degree of mechanical stability. It is unclear if inflammation interacts with stability-related factors.
Methods
We investigated the role of inflammation in three different models: a metaphyseal screw pull-out, a shaft fracture with unstable nailing (IM-nail) and a stable external fixation (ExFix) model. For each, half of the animals received dexamethasone to reduce inflammation, and half received control injections. Mechanical and morphometric evaluation was used.
Results
As expected, dexamethasone had a strong inhibitory effect on the healing of unstable, but also stable, shaft fractures. In contrast, dexamethasone tended to increase the mechanical strength of metaphyseal bone regenerated under stable conditions.
Conclusions
It seems that dexamethasone has different effects on metaphyseal and diaphyseal bone healing. This could be explained by the different role of inflammation at different sites of injury.
Cite this article: Bone Joint Res 2015;4:170–175.
Article focus
- Contrasting the response to glucocorticoids in shaft fractures versus metaphyseal bone regeneration.
Key messages
- Metaphyseal and shaft bone healing responds differently to glucocorticoids.
- Stable metaphyseal healing tended to be stimulated by glucocorticoids.
- Stability did not influence the response to glucocorticoids in shaft fractures.
Strengths and limitations
Strength: this study is the first to compare metaphyseal bone regeneration and shaft fracture healing in mechanical terms.
Limitation: mechanical testing of so different fractures required different techniques and timing.
Introduction
Inflammation is thought to play a crucial role in the initiation of fracture healing. Inhibition of inflammation with non-steroidal anti-inflammatory drugs (NSAIDs) has a strong detrimental effect on the healing of diaphyseal fractures, but a weak effect on metaphyseal healing.1 This suggests that inflammation plays different roles in fractures in the metaphysis and the shaft. This might explain the perplexing discrepancy between the seemingly harmless clinical use of NSAIDs in patients with fractures, and the clearly detrimental effect of such treatment in animal models, as human fractures usually occur in metaphyses, while almost all animal models deal with shaft fractures.
Fractures in cancellous metaphyseal bone tend to heal by direct bone formation within the injured marrow compartment,2,3 suggesting that mesenchymal cells residing locally in the marrow might be sufficient for the bone regenerative process. In contrast, shaft fractures, at least in part, depend on the ability to recruit competent cells from surrounding tissues or circulation.4 It is possible that inflammation is crucial for this recruitment. If so, dampening of the inflammation would be detrimental to healing in a shaft fracture, but not to metaphyseal healing. We have previously tested this hypothesis using an NSAID to reduce inflammation.1 However, that study could not separate the roles of stability and location, i.e., the findings could be explained by a difference in stem cell availability, a difference in mechanical environment or a difference in the amount of new tissue that needed to be formed. We therefore now studied the role of inflammation by use of dexamethasone for inhibition, taking mechanical stability into account.
We hypothesised first that a stable metaphyseal bone healing model would be less impeded by a dampened inflammation than would an unstable, conventional diaphyseal fracture model. We then hypothesised that a difference would also appear if the diaphyseal model was mechanically stabilised.
Patients and Methods
Animals and surgery
In total, 120 male C57Bl/6 mice, then at ten weeks old, were used (Scanbur, Sollentuna, Sweden). All surgery was undertaken in a sterile fashion by a surgeon blinded to drug treatment. Isoflurane gas (Forene, Abbot Scandinavia, Solna, Sweden) was used in order to sedate. The animals received 0.1 mg/kg buprenorphine (Temgesic, Schering-Plough, Brussels, Belgium) every 12 hours for 36 to 72 hours (depending on the fracture model), starting just before surgery. Antibiotics, 0.2 mg/kg oxytetracycline (Engemycin, Intervet, Boxmeer, Holland) was also given by subcutaneous injection before surgery.
The animals had unrestricted access to food and water and were housed four per cage, in a 12:12 hour light cycle. All experiments were in accordance with ethical approvals 85-12 and 54-14 from the Regional Animal Ethics Board.
Stable metaphyseal injury model
We used a screw in the metaphyseal region as a metaphyseal injury model. The pull-out force of a screw one week after implantation, with or without various drug treatments, correlates with the amount of newly formed bone both around the screw and in empty drill holes.5 In total, 20 mice received a custom-made screw implant (Rydahl Precision Components, Karlstad, Sweden) into the fronto-medial aspect of the proximal right tibia. First, a 0.6 mm diameter drill hole was made. A screw made of titanium with a length of 1 mm and thread M 0.7, was then screwed in place (Fig. 1). The mice also received a drill hole 0.6 mm in diameter at the corresponding site on the contralateral tibia, here without a screw. These techniques have been previously described in greater detail,1 and can be considered mechanically stable. The relevance of this model for fracture healing is discussed below.
Fig. 1.
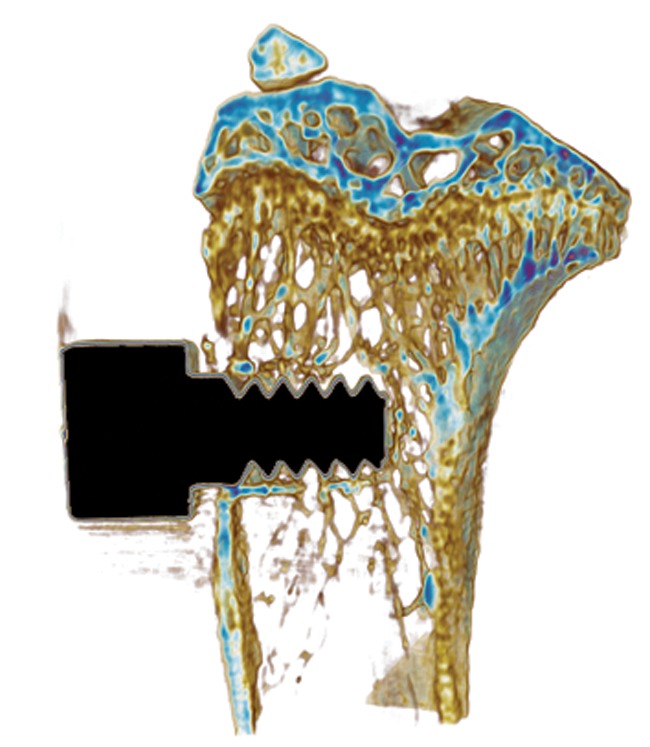
MicroCT scan of a screw newly inserted in the tibial metaphysis.
The animals were randomised to receive either dexamethasone (Vorenvet, Boehringer Ingelheim, Germany) or control injections. Dexamethasone was given subcutaneously at a dose of 2 mg/kg three times per week, starting on the day of surgery. Control animals received an equal volume of saline. One week after surgery, the animals were killed with carbon dioxide, and both tibias were harvested for evaluation. The first 20 mice in the metaphyseal model showed a trend (p = 0.06) towards increased pull-out resistance in the dexamethasone group. Therefore, the experiment was repeated twice, with 24 and 30 mice, bringing the total number of mice used for this model up to 74. As there was no significant difference in outcome between the groups (p = 0.4), and no difference in the effect of dexamethasone between the groups (p = 0.2), they were pooled.
Unstable shaft fracture model
A total of 26 mice had their right knee opened, the patella dislocated medially, and an intramedullary pin, with a diameter of 0.4 mm, inserted into the femur. The femur was then cut transversely in the shaft, using a custom-made pair of tongs. The patella was sutured back in place and the skin closed. The process has been described in greater detail elsewhere.1
The mice were randomised to receive dexamethasone or control injections, as described above, for the metaphyseal fracture group. The animals were killed after 17 days, the femur harvested, the intramedullary pin pulled out, and the femur frozen at -20°C for later analysis.
Stable shaft fracture model
A total of 20 mice had an external fixator (MouseExFix simple XL, RISystem, Davos, Switzerland) inserted. After opening the skin over the left femur and applying the external fixator using four threaded pins, the shaft of the femur was transected using a 0.22 mm diameter Gigli wire, leaving a 0.22 mm osteotomy. The muscle and the skin were then sutured, with the screws sticking out through the suture and the plate outside the skin.
The animals were randomised to dexamethasone or control injections, and given doses as described above. After 17 days the animals were killed and the femurs harvested. The fixator was removed and the femurs were frozen at -20°C for analysis.
Mechanical testing
All tests were performed on the same computerised materials testing machine (100R; DDL Inc., Eden Prairie, Minnesota). All experiments used force at failure as the primary outcome variable.
Immediately after harvest, the tibias containing a metaphyseal screw were placed in a custom-made mount on the materials testing machine. The screw was attached to the force transducer by the use of a clamp and was pulled out by the machine at a cross-head speed of 0.01 mm/s.
Both stable and unstable shaft femurs were thawed and tested with three-point bending in the sagittal plane. The support bars were 6 mm apart, and the loading bar was applied on the frontal area of the bone with a cross-head speed of 0.05 mm/s. Before the mechanical testing, the samples were analysed by microCT (µCT) as described below.
µCT morphometry
A µCT machine (type1174; Bruker, Boston, Massachusetts) was used, with a 0.25 mm Al filter, 50 kV, in 180° scans. Beam hardening and ring artifacts were corrected for. Reconstruction and analysis were undertaken with NRecon and CTAn (Bruker). For all experiments, standards with 0.25 g and 0.75 g of calcium hydroxyapatite per cm3 were used to assess mineral density.
The metaphyseal drill hole of the left tibia was analysed for new bone formation using a pixel size of 8 µm, a rotation step of 0.5°, and a frame averaging of three. The volume of interest (VOI) was defined as a 0.5 mm diameter cylinder covering where the drill had been passed through, starting at the endosteum and extending 1 mm into the marrow compartment (Fig. 2). This volume was analysed for bone volume (BV) and tissue mineral density (TMD).
Figs. 2a - 2b.
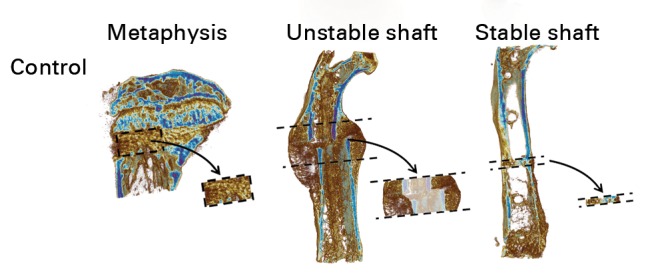
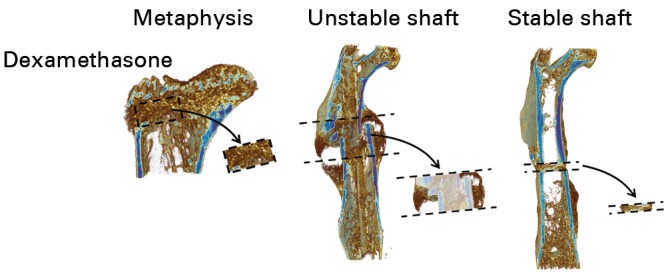
MicroCT scans with the volumes of interest (VOI) extracted. In order to ensure that the images in this figure are representative, the figure shows the specimen with the median value for bone volume (BV), or bone area, from each treatment group. Areas with decreased opacity in the unstable shaft VOIs indicate areas that were excluded from calculations of BV and tissue mineral density.
The two diaphyseal fracture models were analysed with a pixel size of 12 um, a frame averaging of two, and a rotation step of 0.4° for the unstable model, and 0.3° for the stable model. For the unstable model, the VOI was defined as a segment delineated by two planes 2 mm apart, perpendicular to the longitudinal axis of the femur and centred on the osteotomy. Old bone and the volume corresponding to the original marrow space were excluded manually (Fig. 2). The remaining VOI was analysed for BV and TMD. For the stable diaphysis, the VOI comprised the newly formed callus in the fracture gap, excluding old bone, also done manually (Fig. 2). The VOI was analysed for TMD and mean bone area, i.e. BV per mm gap (since different animals had slightly different lengths of the gap, total BV could not be used).
Statistical analysis
Data were tested with the Shapiro–Wilk test for normality, and parametric or non-parametric tests were used accordingly. Data not normally distributed are noted as such in the results section. Hodges–Lehmann was used to estimate the 95% confidence interval (CI) for the non-parametric data, and t-tests were used to estimate the CIs for the parametric data. A p-value of < 0.05 was considered significant.
Results
Excluded samples
The exclusions in the experiment are presented in Table I.
Table I.
The exclusions and cause thereof
| Model | Dexamethasone | Control | Comment |
|---|---|---|---|
| Metaphyseal | 1 | 1 | Computer error |
| Shaft (ExFix) | 3 | 2 | Infection or faulty surgical procedure |
| Shaft (IM-nail) | 3 | 1 | IM-nail protruded distally and relative stability was lost |
ExFix, stable external fixation; IM-nail; unstable nailing
Mechanical testing
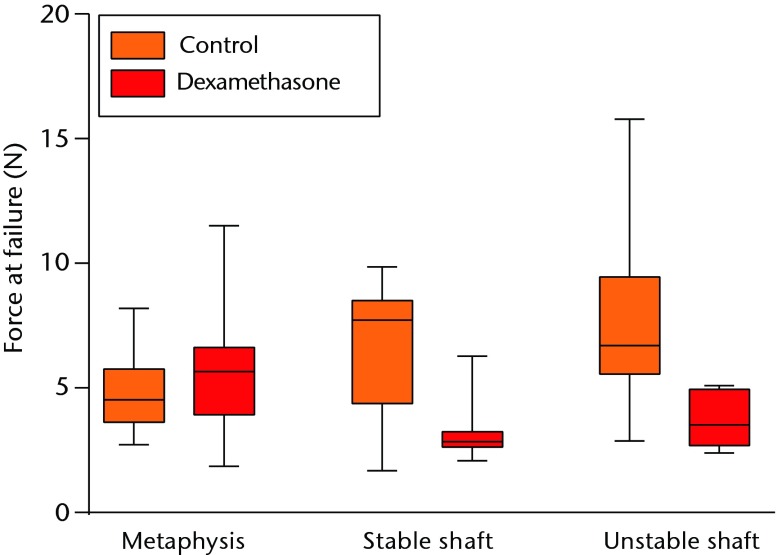
The pull-out force of the metaphyseal screws was increased by 18% by dexamethasone, after pooling results from the three metaphyseal experiments (95% CI 0.12 to 36; p = 0.049; Fig. 3). The 95% CI suggests that inhibition owing to dexamethasone is highly unlikely. In contrast, the force at failure of the shaft was decreased by 50% in the unstable model (95% CI 19 to 81; p = 0.003). In the stable model, data were not normally distributed. Median decrease was 51% (95% CI 15 to 74; p = 0.02).
Fig. 3.
Graph demonstrating that the dexamethasone had different effects on force at failure in the metaphysis and the shaft. In the metaphysis an 18% increase (p = 0.049), and in the stable and unstable shafts, a decrease by 50% and 51% (p = 0.02 and p = 0.003). There was no discernible difference between the effect on the stable and the unstable shaft fractures.
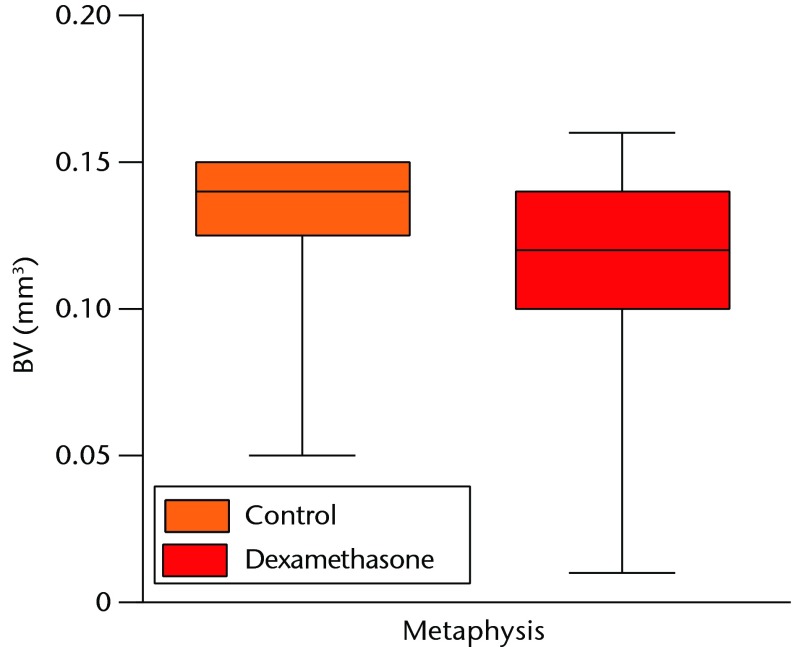
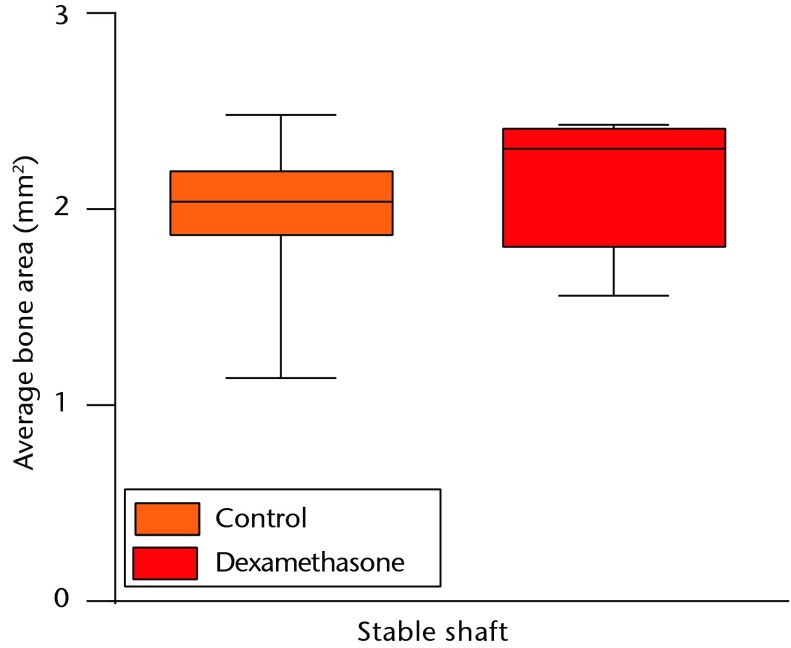
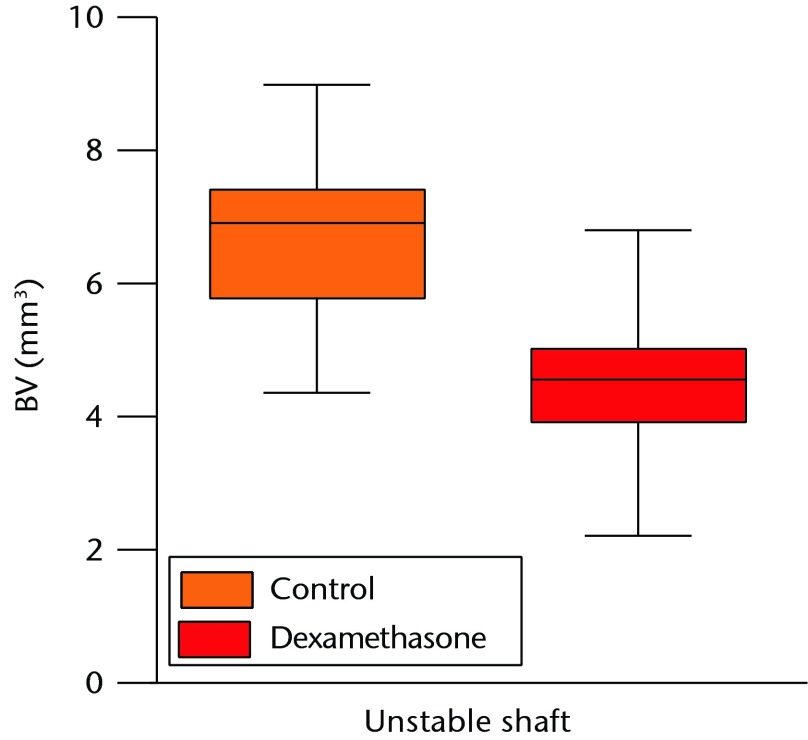
µCT morphometry
The metaphyseal drill hole BV and TMD were not normally distributed. The median BV was decreased by 11% by dexamethasone (Figs 2 and 4, p = 0.006, 95% CI 3.6 to 19). The median TMD was decreased by 16% (95% CI 5.4 to 24; p = 0.005). In a few specimens, small localised areas with low density were seen within the newly formed bone. In the model of the unstable shaft fracture, dexamethasone decreased the BV of the callus by 33% (Figs 2 and 4, 95% CI 16 to 49; p < 0.001). The TMD of the unstable shaft fracture was not normally distributed. The median TMD was decreased by 8% (95% CI 2.3 to 12; p = 0.004). In the stable diaphyseal model there was no detectable effect on mean bone area (Figs 2 and 4, 95% CI -12 to 29; p = 0.36) or TMD (95% CI -6 to 25; p = 0.20).
Figs. 4a - 4c.
Graphs demonstrating the microCT data for the amount of newly formed bone in the three models. a) In the metaphysis there was an 11% decrease in bone volume (BV) of the drill hole; b) the mean bone area of the callus of the stable shaft fracture was not significantly affected, whereas c) the BV of the central 2 mm callus of the unstable shaft was reduced by 33% with dexamethasone injection*p < 0.05.
Discussion
Stable metaphyseal bone healing was not impaired by dexamethasone, while there was a detrimental effect in both stable and unstable healing of a shaft fracture.
The result can be partly explained by three differences between metaphyseal and shaft injuries. First, metaphyseal marrow is rich in stem cells compared with the shaft marrow, the former also being more committed towards an osteogenic fate.6 If a shaft fracture is dependent on stem cell recruitment from distant sources,4 and inflammation is required for this process, then dampening of inflammation would be harmful. In contrast, the marrow compartment in the metaphysis has a stem cell supply, which might already be sufficient.
Second, metaphyseal fractures heal with less new tissue formation, and with a much smaller callus. This means that fewer progenitor cells are needed for new tissue formation. Hence, a drug that decreases progenitor cell recruitment could be expected to have smaller effects in a metaphyseal fracture.
Third, shaft fractures heal via an endochondral phase which is not usually found in metaphyseal fractures, neither in drill holes in mice, nor in proximal tibial osteotomies in rabbits, or distal radial fractures in patients.2,3 Blocking glucocorticoid receptor signaling in chondrocytes increases cartilage formation in endochondral bone formation after fracture, suggesting that inflammation is needed for cartilage formation after fracture.7
Dexamethasone tended to improve the healing of metaphyseal injury, as measured by the pull-out force. However, long-term glucocorticoid treatment is known to have a negative effect on bone formation8 and is a leading cause of secondary osteoporosis,9 possibly because of induction of osteoblast and osteocyte apoptosis.10 Yet, glucocorticoids, together with other anti-inflammatory drugs, have also demonstrated positive effects on bone metabolism in patients with upregulated inflammation such as in rheumatoid arthritis.11 In line with our findings, a recent in vivo study showed that dexamethasone treatment improved the quality of metaphyseal bone while impairing the same in shaft bone, in both ovariectomised (OVX) and non-OVX mice.12 The positive effect in the metaphysis was dependent on the presence of lymphocytes, as the effect was absent in mice with severe combined immunodeficiency (SCID). An NSAID, carprofen, did not have the same positive effect in the metaphysis as glucocorticoids did.12 This corresponds well with previous findings from our lab that the NSAID indomethacin had no positive effect in our metaphyseal screw model.1
The main limitation of this study is that different models had to be used in order to enable mechanical evaluation of shaft and metaphyseal fractures. Comparing a screw pull-out model to a three-point bending model is not ideal, but both give a measure of the most important variable for a patient with a fracture, namely mechanical strength.
The relevance for screw fixation as a measure of bone healing requires some discussion. The pull-out force immediately after insertion is minimal, and then increases over time as new bony threads are formed.1 This bone formation is a response to trauma and occurs also in the absence of a screw in the drill hole. The mechanical testing estimates the strength of this newly formed bone, and the pull-out force correlates with the amount of this newly formed bone.5 As the amount and quality of the new bone in metaphyseal fracture healing are most important in clinical cases, we consider this screw model relevant for metaphyseal fracture healing. It is a practical and simple model that allows for mechanical evaluation. In contrast, a screw model in shaft bone would not yield relevant information as fixation would largely be dependent on the pre-existing cortex, and not on newly formed bone.
The predetermined primary outcome variable of this study was force at failure. The results of the morphometric analysis were slightly different. There was a small decrease in bone density in the metaphyseal drill hole, which contrasts with the increased pull-out force. A possible explanation could be related to the observation that small areas devoid of bone occurred within the VOI in some dexamethasone samples. Another explanation could be that the implant influenced the bone formation response, compared with the drill hole without a screw. Furthermore, there was no morphometric to correlate to the dramatic decrease in force at failure with dexamethasone in the stable model. It appears that force at failure is a more sensitive outcome variable, summarising the effects of subtle morphological changes owing to treatment.
In this experiment, the interaction between stability and dexamethasone on metaphyseal healing was not studied. It is known that relative stability has an effect on metaphyseal fractures. A very stable situation has been demonstrated to lead to slower healing compared with a less stable situation.13 However, since we could not see an effect of stability in the shaft, and since instability is not usually a property of metaphyseal fractures, we did not investigate this avenue.
Because shaft and metaphyseal fractures do not heal at the same pace, we had to use different healing periods before performing the measurements. All time points were chosen to optimise the ability to reveal the effect of impaired fracture healing, based on pilot experiments. For the screw model, the time point followed the dramatic early rise in pull-out force that occurs during the first week.1 For the shaft models, the time point corresponded to the earliest time when there was bony bridging and a distinct failure point at the mechanical testing curves.
In conclusion, inhibition of inflammation by use of dexamethasone had strikingly different effects in metaphyseal versus shaft fractures. Stable and unstable shaft fractures responded similarly. These results underline the difference between metaphyseal and shaft healing, and suggest a different role for inflammation in healing at the two sites.
Funding Statement
P. Aspenberg acknowledges grants received from the Swedish Research Council (VR 2009-6725), Linköping University, Östergötland County Council, King Gustav V and Queen Victoria Mason Foundation, and the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement N° 279239, all of which are related to this paper.
Footnotes
Author contributions:O. H. Sandberg: Experiment design, carrying out the experiment, data collection, data analysis, writing the paper
P. Aspenberg: Experiment design, data analysis, writing the paper
ICMJE Conflict of Interest:None declared
References
- 1.Sandberg O, Aspenberg P. Different effects of indomethacin on healing of shaft and metaphyseal fractures. Acta Orthop 2015;86:243–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aspenberg P, Sandberg O. Distal radial fractures heal by direct woven bone formation. Acta Orthop 2013;84:297–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen WT, Han C, Zhang PX, et al. A special healing pattern in stable metaphyseal fractures. Acta Orthop 2015;86:238–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumagai K, Vasanji A, Drazba JA, Butler RS, Muschler GF. Circulating cells with osteogenic potential are physiologically mobilized into the fracture healing site in the parabiotic mice model. J Orthop Res 2008;26:165–175. [DOI] [PubMed] [Google Scholar]
- 5.Bernhardsson M, Sandberg O, Aspenberg P. Experimental models for cancellous bone healing in the rat. Acta Orthop 2015;27:1–6. (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siclari VA, Zhu J, Akiyama K, et al. Mesenchymal progenitors residing close to the bone surface are functionally distinct from those in the central bone marrow. Bone 2013;53:575–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tu J, Henneicke H, Zhang Y, et al. Disruption of glucocorticoid signaling in chondrocytes delays metaphyseal fracture healing but does not affect normal cartilage and bone development. Bone 2014;69:12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ton FN, Gunawardene SC, Lee H, Neer RM. Effects of low-dose prednisone on bone metabolism. J Bone Miner Res 2005;20:464–470. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein RS. Glucocorticoid-induced osteoporosis and osteonecrosis. Endocrinol Metab Clin North Am 2012;41:595–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest 1998;102:274–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haugeberg G, Strand A, Kvien TK, Kirwan JR. Reduced loss of hand bone density with prednisolone in early rheumatoid arthritis: results from a randomized placebo-controlled trial. Arch Intern Med 2005;165:1293–1297. [DOI] [PubMed] [Google Scholar]
- 12.Grahnemo L, Jochems C, Andersson A, et al. Possible role of lymphocytes in glucocorticoid-induced increase in trabecular bone mineral density. J Endocrinol 2015;224:97–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Claes L, Reusch M, Göckelmann M, et al. Metaphyseal fracture healing follows similar biomechanical rules as diaphyseal healing. J Orthop Res 2011;29:425–432. [DOI] [PubMed] [Google Scholar]