Abstract
First episode of psychosis can occur at any age and it can be primarily psychiatric or secondary to other occult diseases. It is of great therapeutic relevance to be cautious about organic etiology as early diagnosis can help in early initiation of disease modifying treatments. To study patients who presented with first episode of psychosis and later turned out to be due to lupus erythematosus with varying periods of delay. Details of patients who were considered as treatment unresponsive psychosis and later turned out to be due to vasculitis were entered in excel sheet and analyzed. The details of patients including neuropsychological features, apparent soft signs which were initially ignored, lab data and signs during follow-up were tabulated and warning signs analysed. All our patients were highly intelligent young females and there were stressors in all of them. They presented with panic, followed by psychotic symptoms which was resistant to regular psychiatric treatment and therefore possibility of organicity explored. All of them had history of transient symptoms referable to other systems which were treated as such and patients did not volunteer the same unless questioned. During follow-up full-fledged features of SLE came up in all patients. When a young female with no past or family history of mental illness presents with psychotic features, unprovoked panic, and limbic symptoms always ask for minor or transient symptoms and signs referable to the other systems which might give valuable clues.
Keywords: First episode psychosis, neuropsychiatric lupus, neuropsychology
INTRODUCTION
Systemic Lupus Erythematosis (SLE) is an auto immune disease which involves multiple systems where tissue injury is mediated by auto anti bodies and immune complexes. Interaction between environmental factors and susceptibility genes is believed to result in destructive immune responses, which include activation of innate immunity in RNA protein self-antigens, DNA in immune complexes, lowered activation threshold for adaptive immunity, ineffective regulatory and inhibitory CD cells and reduced clearance of apoptotic cells and immune complexes.[1] There is excessive secretion of pro-inflammatory cytokines like interferons, tumor necrosis factor and interleukin10.[1,2] However, females are more vulnerable than the males, more so when exposed to oral contraceptives or when they are put on hormone replacement therapy as Estradiol binds to receptors on T and B cells and activates them. Exposure to ultra violet light, infections both viral and bacterial are known to unmask the first episode of clinical disease.[2] The diagnostic criteria for lupus erythematosus by Mchochberg et al., in 1997 suggest the following. Malar Rash, Discoid Rash, Photosensitivity, oral ulcers, arthritis, serositis, renal involvement, neurological involvement, hematological involvement, immunological abnormalities in the form of anti dsDNA antibody, anti Sm, anti phospho lipid antibody and anti-nuclear antibody by immune fluorescence suggest the possibility of SLE if four of these are present at any time in a patient's history.[1,2,3]
Neuro psychiatric manifestations of SLE is however a diagnosis of exclusion when it occurs as a first manifestation of disease. It is believed to be least understood and missed but probably a not uncommon form of lupus.[1] The common manifestations are encephalopathy, coma, depression and psychosis.[2] Pathogenesis of neuro psychiatric manifestations are believed to be due to lupus cerebritis, auto anti- neuronal antibody, auto antibody mediated neurolysis, vasculopathy, cytokine mediated injury, etc. This is prevalent mostly among African Americans, Asians, and Hispanics. Neuro psychiatric symptoms precede overt manifestations of SLE in 28-40 % of patients, and this group of patients face diagnostic difficulty. Whereas in 63% of patients these symptoms occur within the first year of clinical diagnosis of lupus. Diamond et al., (2004) and others reported anti DNA auto antibody, which cross reacts with NR2 sub unit of anti NMDA receptor results in Hippocampal damage. Entry of epinephrine is supposed to result in damage to lateral amygdala. There can be anti-phospholipid mediated direct neuronal injury. Anti cardiolipin IgA is believed to cause psychiatric manifestations and anti cardiolipin IgG is believed to cause myelitis. The common central nervous system manifestations are aseptic meningitis, cerebrovascular accidents, cognitive dysfunction, head ache, movement disorders, seizures, acute confusional state, anxiety mood disorders, psychosis, demyelination, myelitis, features of mono neuritis, plexitis, acute and chronic inflammatory demyelinating radiculo neuropathies, myasthenia gravis, etc.[3,4,5,6,7] The direct role of the various anti bodies in production of the specific neurological symptoms is not clear. However they serve as very sensitive proxy markers of the underlying disease. In this article we present three consecutive patients, who presented with psychiatric manifestation as the first symptom of SLE.
CASE REPORTS
Case 1
A 21-year-old female who is a student, was admitted to our institution with the following features. She had experienced fatigue, vague aches and pains 6 months before admission to our institution. Later patient developed excessive fear and delusions, kept on repeating that she had committed some major mistake, was having episodes of anxiety, agitation and aggressive behaviour. Therefore she was treated by a psychiatrist, with which she had partial improvement of symptoms. But was unable to concentrate. On retrospective questioning there was evidence for occasional oral ulcers and rashes over the face, which was managed with local ointments with dermatologist. There was no family history of any psychiatric illness. Hence the possibility of an organic psychosis secondary to some Vasculitic disorder was considered. Her investigations showed ESR 70 mm/hour, APLA negative, anti-nuclear antibody positive 1in 160 dilution, anti-centromere anti-body positive, other vasculitic parameters negative, work up for chronic infection in blood and CSF including TB, HSV, Brucella, sarcoidosis were negative. Mantoux test was negative, Chest X-ray was Normal, Ultrasound Abdomen was Normal, Lip Biopsy Showed lobules of minor salivary glands with salivary acini and ducts. The acini are enlarged and coalesced with obliteration of the lumen. Ducts were dilated in few areas suggestive of Vasculitis. Her evoked responses were normal. Autonomic Function test showed Sympathovagal imbalance with sympathetic dominance. MRI brain showed mild diffuse atrophy and minimum signal changes in the medial temporal lobe in FLAIR images [Figure 1a]. EEG showed a background of alpha mixed with theta. Neuro psychological assessment revealed deficits in mental speed, sustained attention, category fluency, set shifting, response inhibition, memory, verbal and visual learning suggestive of left fronto temporal and right temporal involvement.[7,8] Her Vitamin B12 was 553 pg/mL, folate was 24 ng/mL. Her INR was 1.3. C-Reactive Protein (CRP) 203.1mg/L normal range is 0-5. Peripheral smear showed hypochromic microcytic anemia. Immune fixation electrophoresis showed no M-band. So with the above features even though the criteria where all not satisfied patient was diagnosed as a probable case of neuro psychiatric lupus and started on steroids and Azathioprine. Within about one month time patient developed severe leucopenia which needed stopping of the drug and blood transfusion. Then she was shifted to Mycophenolate Mofetil, low dose at 500 mg per day. Patient had a complete remission of all her neuro psychiatric symptoms. During third month of follow-up, patient developed new systemic features like joint pains of the small joints and the classical malar rash [Figure 2]. This is probably due to very low dose of Mycophenolate Mofetil used and therefore dosage was titrated to 1 gram per day. But patient progressed to extensive skin rashes and fever and therefore steroids were increased and Azathioprine was restarted and Mycophenolate Mofetil was withdrawn. Currently the patient is clinically stable.
Figure 1.
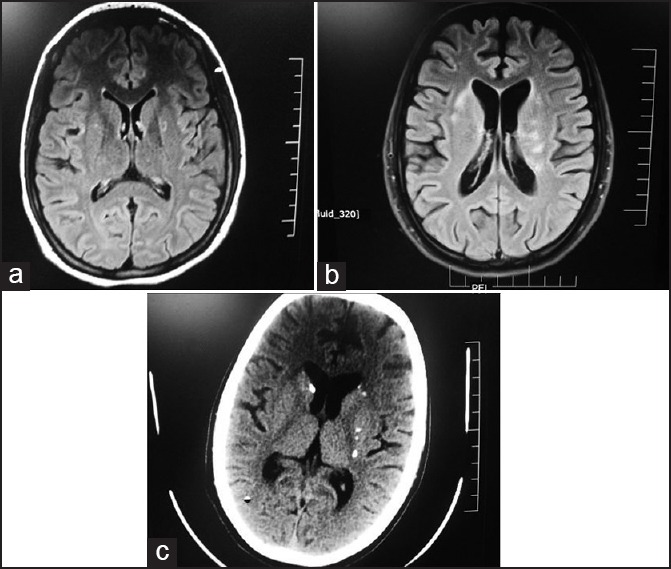
MRI (a) Diffuse atrophy, (b) Diffuse atrophy with White matter signal changes (c) CT brain showing diffuse atrophy with old calcified granulomas
Figure 2.
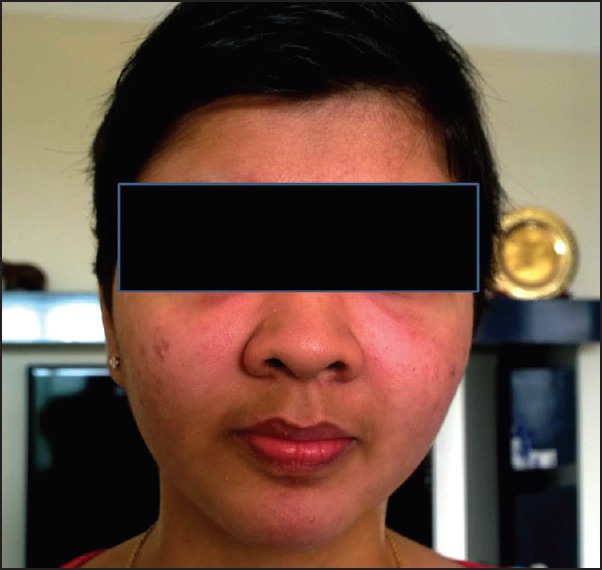
Malar rash in patient 1 during follow-up
Case 2
A 21-year-old female dental student, staying in hostel noticed occasional rashes over her thighs which was treated by her dermatologist and improved over few days with local ointments. This was followed by loss of eye lashes and slight eversion of the eye lid and treated as blepharitis. She had reddish streaks in the bulbar conjunctiva and watering from eyes which was treated as allergic conjunctivitis. Later patient developed fever and cough which lasted for about fifteen days and improved with local hospital treatment. This was followed by severe insomnia, extreme fear which she reported to her parents. Later patient reports a brief period of unawareness at night. However the details associated with that are not clear as patient was in the hostel. Then while bathing patient developed severe panic and ran down from the second floor of her hostel to the ground floor which was suspected as a psychiatric problem and was admitted to a local hospital with a psychiatrist. On treatment with anti-psychotics patient did not improve and therefore referred to the psychiatric department of our institution. Later, with psychiatric treatment in our institution, she did not improve and was referred to Neurology to rule out organic disease. At the time of examination the patient was slightly confused, her eye lashes were absent, there were mild reticular changes in her conjunctiva and there was restriction of extreme lateral movement of the right eye. Assessment of her speech and language, suggested aphasia as evidenced by word finding difficulty, circumloculation, paraphasic errors and naming defect. She had mild asymmetry of reflexes on the right side. The next day in neurology, the patient developed tonic clonic seizures. Therefore the possibility of Vasculitis, auto immune encephalitis, chronic CNS infection were considered as possibilities. Her investigation showed strongly positive anti RO52, Strongly positive anti body to Sm antigen (Smith antigen), Antibody to SS-A(RO) and Antibody to UI-nRNP/Sm. Her workup for chronic infection, autoimmune encephalitis, Leptospira, Brucella and Hashimoto encephalopathy were negative. Ultrasound abdomen showed ascites. Her renal functions, liver functions, hematological workup were normal. Vitamin B12 level were 88.7 pg/mL (normal range180-914 pg/mL). MRI showed atrophy of frontal and temporal regions with multiple periventricular white matter signal changes [Figure 1b]. There was mild medial temporal hyper intensity on both sides. Patient was treated with methylprednisolone 1 gram daily for five days in addition to anticonvulsants followed by Azathioprine at the dose of 1 mg/Kg body weight. Patient went into complete remission and joined back to continue her studies as a dental surgeon at six months follow-up.
Case 3
A 22-years-old female who following a stressful family event and an abortion, had to move away from her family and lived under difficult situations, following that she noticed severe weight loss. This was treated with supportive measures and her general health improved. Then she developed severe fear, anxiety, irritability, and sleeplessness for which she was suspected as having reactive depression secondary to family stressors. While on treatment she came to NIMHANS with weakness of right sided limbs with inability to speak. Examination revealed thin built patient who was pale. Her blood pressure was 70/46 mm of Hg. She had right hemiplegia with global aphasia. Her fundus showed mild temporal pallor and she had pigmentation over both legs and sparse hair. There was history of mild intermittent fever on questioning, which improved with symptomatic measures. There was history of another episode of transient left sided weakness in the past which improved on its own and was ignored. Patient underwent investigation for vasculitis including skin biopsy. Her skin biopsy specimen showed oedema of Capillary dermis with scattered lymphocytes and histocytes that are also seen in the deeper dermis surrounding hair follicles and small venules. Pigment incontinence with melanin pigment laden macrophages seen just beneath the epidermis which is flattened with vacuolation of basal keratinocytes suggestive of vasculitis. Her Anti-Phospholipid antibody both IgG and IgM were positive. MRI done outside showed diffuse atrophy with slight increase in the mineralization of the basal ganglia. CT scan showed diffuse atrophy with old calcified granulomas [Figure 1c]. CSF showed antimicrobial antibody positive which corroborates with the CT finding of calcified granulomas, with 1 cell/mm3, Chloride– 122 mEq/L, Glucose 35 mg/dl and Protein 155 mg/dl. Two months after diagnosis and initiation of treatment patient conceived again inspite of advice to the contrary. Therefore patient had to be maintained with steroids and Heparin throughout pregnancy. She had an IUD at 9 months of gestation. Following that her neurological status deteriorated with severe behavioral problems, recurrent seizures, Transient Ischemic attacks (TIAs) with skin changes over the face and limbs. The skin changes were in the form of strawberry tongue, cheilitis, hyper pigmented as well as erythematous rashes over the face and persistent fever with oral thrush, leucopoenia and anaemia. She was referred to multidisciplinary hospital for follow-up.
DISCUSSION
New onset Psychosis in young females need to be evaluated for organic causes even if there is severe personal stress reported as precipitating factor. In this study we report three patients with neuropsychiatric lupus who were diagnosed as varying type of psychiatric illness based on the presenting symptoms and there had been an onset to diagnosis delay of 6-9 months. Lupus erythematosus presents with diverse clinical features and psychiatric symptoms can precede other obvious features.[9,10] Clinical and laboratory data available may be scarce. High index of suspicion and exploration of history for previous soft symptoms like malaise, evanescent rashes, fatigue, and feverishness which had been ignored will give valuable clue. Albuminuria, elevated ESR and positive titers in one or more of the Vasculitic panel should be viewed with great suspicion for further workup on Lupus. During the course of illness over six months to one year, these patients develop the other systemic manifestations. Early diagnosis is crucial for initiation of treatment and prevention of complications. As most of these patients belong to child bearing age group they should be investigated for secondary Anti phospholipid Antibody (APLA) syndromes [Tables 1-6].
Table 1.
Demographic details
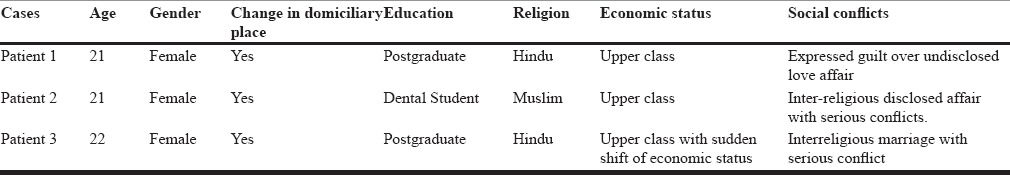
Table 6.
Outcome at follow up in Neurology at 6 months, 12 months and 18 months
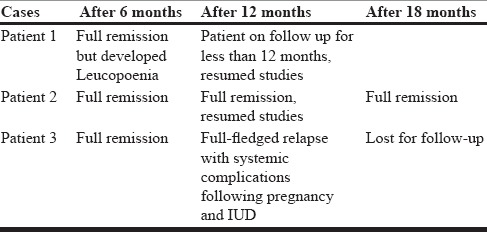
Table 2.
Neuropsychological features
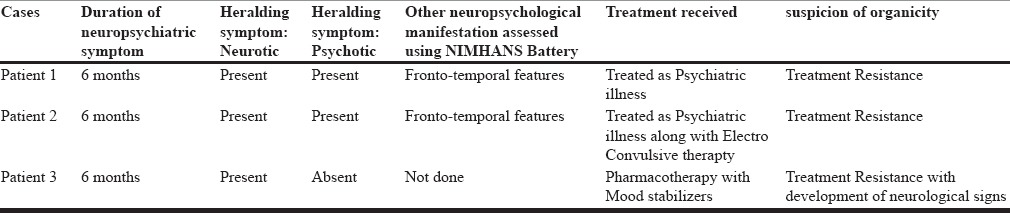
Table 3.
Neurological manifestations at presentation and follow up
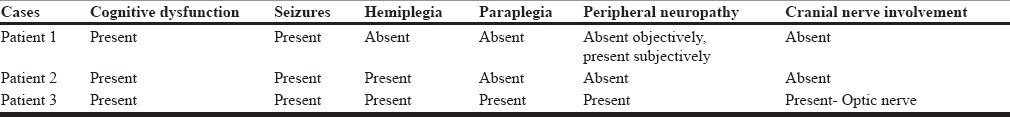
Table 4.
General systemic manifestations during follow up
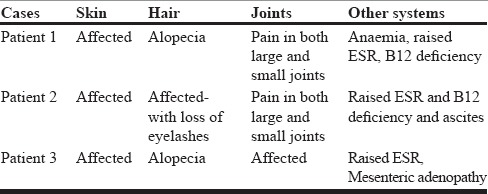
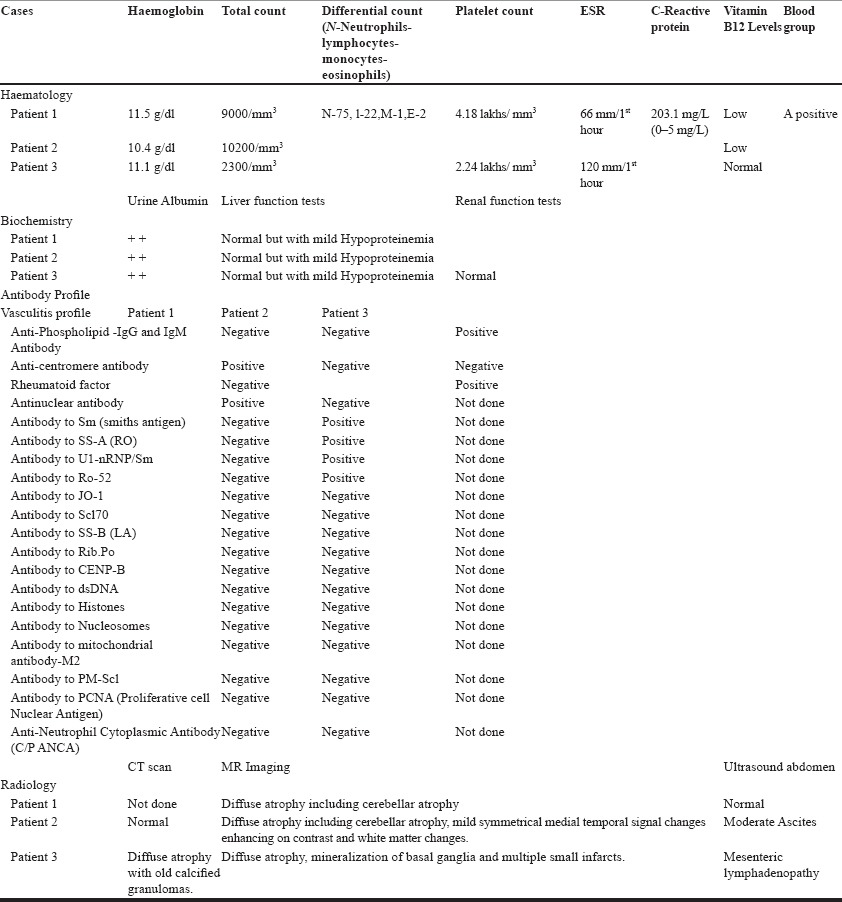
Table 5.
Laboratory data
CONCLUSION
Neuropsychiatric lupus is one of the common manifestations of lupus erythematosus in young females. It can be precipitated by severe stress which might serve as a red herring to diagnosis. Most of the patients are resistant to both pharmacotherapy and Electroconvulsive therapy for psychotic features. Soft systemic evanescent symptoms and signs are present in most patients which are missed by both patients and medical personnel during assessment. New onset psychoses with soft neurological signs need thorough evaluation to rule out Neuropsychiatric SLE. Albuminuria, raised ESR and mild hematological changes should be taken up as serious clues to diagnosis to avoid treatment delay resulting in serious complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Popescu A, Kao AH. Neuropsychiatric systemic lupus erythematosus. Curr Neuropharmacol. 2011;9:449–57. doi: 10.2174/157015911796557984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hahn BH. Harrisons Textbook of Internal Medicine. 18th Edition. New York: McGraw Hill Publising Company Ltd; 2008. Systemic Lupus Erythematosis; pp. 2728–2729. [Google Scholar]
- 3.Schurmd PH. (n.d.). Neuro Psychiatric Manifestations of SLE. [Last accessed on 2015 Jan 3]. Available from: www.rheumatology.org/publications/ar/1999/aprilappendix.asp .
- 4.Hanly JG, Urowitz MB, Sanchez-Guerrero J, Bae SC, Gordon C, Wallace DJ, et al. Systemic Lupus International Collaborating Clinics. Neuropsychiatric events at the time of diagnosis of systemic lupus erythematosus: An international inception cohort study. Arthritis Rheum. 2007;56:265–73. doi: 10.1002/art.22305. [DOI] [PubMed] [Google Scholar]
- 5.Kovacs J, Urowitz M, Gladman D. Dilemmas in neuropsychiatric lupus. Rheum Dis Clin North Am. 1993;19:795–819. [PubMed] [Google Scholar]
- 6.De Marcaida JA, Reik L., Jr Disorders that mimic central nervous system infections. Neurol Clin. 1999;17:901–41. doi: 10.1016/s0733-8619(05)70172-9. [DOI] [PubMed] [Google Scholar]
- 7.Huerta PT, Kowal C, DeGiorgio LA, Volpe BT, Diamond B. Immunity and behavior: Antibodies alter emotion. Proc Natl Acad Sci U S A. 2006;103:678–83. doi: 10.1073/pnas.0510055103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kowal C, DeGiorgio LA, Nakaoka T, Hetherington H, Huerta PT, Diamond B, et al. Cognition and immunity; antibody impairs memory. Immunity 2004. 2004 doi: 10.1016/j.immuni.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, et al. The European Working Party on Systemic Lupus Erythematosus. Systemic lupus erythematosusclinical and immunologic patterns of disease expression in a cohort of 1, 000 patients. The european working party on systemic lupus erythematosus. Med. 1993;72:113–24. [PubMed] [Google Scholar]
- 10.Schneebaum AB, Singleton JD, West SG, Blodgett JK, Allen LG, Cheronis JC, et al. Association of psychiatric manifestations with antibodies to ribosomal P proteins in systemic lupus erythematosus. Am J Med. 1991;90:54–62. doi: 10.1016/0002-9343(91)90506-s. [DOI] [PubMed] [Google Scholar]


