Abstract
Context:
Neuro-cognitive functions have not been extensively studied among young bipolar disorder patients. Researchers have found cognitive deficits in bipolar disorder and many have found such deficits even in euthymic states of the disorder but results are still inconclusive.
Aim:
To study sustained attention and executive functioning in remitted adolescents with bipolar disorder.
Settings and Design:
Present study was a hospital-based cross-sectional study.
Materials and Methods:
Twenty adolescents, aged 14-17 years with bipolar disorder, were selected for the study. Subjects were euthymic for at least 2 months. The performance of patients was matched with normal controls. Sustained attention was primarily measured by Letter Cancellation Test (LCT) and Wisconsin Card Sorting Test (WCST), Trail Making Test (TMT) and Stroop Colour Word Test were used to assess executive functions. Two groups differed significantly on level of education and thus multivariate linear model was used and education was put as a covariate.
Results:
Results revealed that patients preformed less well than control. Significant poor performance was reported on LCT (omission scores), TMT, Stroop and WCST.
Conclusion:
The study confirmed previous findings stating that cognitive deficits like sustained attention and executive functions continue to be present in adolescent bipolar patients even in euthymic states.
Keywords: Adolescent bipolar disorder, executive functions, sustained attention
INTRODUCTION
Neuropsychological deficits have been reported even in euthymic states in adolescent bipolar disorder.[1,2] But still have not been studied in depth.[3] Many studies report no impairment in sustained attention among stable adolescent bipolar patients.[4,5] But majority of studies report that poor performances on attention, verbal memory and verbal fluency during their manic and euthymic states.[6,7,8] Specifically, deficits in verbal memory have been found to be relatively clearly.[9] Similarly, deficits in inhibition, working memory, set shifting, visuo-spatial memory and problem-solving are not found consistently in studies further leaving results inconclusive.[3] Thus, need was felt to study same from this part of the world.
MATERIALS AND METHODS
Sample
The present study was done on 20 adolescents (age range 14-17 years) who were diagnosed with bipolar disorder and were currently in remission for at least 2 months, as per the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) DCR criteria and as assessed by Young Mania Rating Scale (YMRS) score less than 6 and Hamilton Depression Rating Scale (HDRS) score less than 7. Sample consisted of total six female subjects. Sample was collected from outpatient department (OPD) of Child and Adolescent Psychiatric Unit. Co-morbid mental retardation, epilepsy, substance abuse and serious medical illnesses were screened out. Patients who had received electroconvulsive therapy (ECT) in past 6 months were also screened out. The performances of patients were matched on age and sex with 20 normal control subjects. Normal control subjects were selected on the basis of General Health Questionnaire (GHQ-12) score less than 3 and who did not had any past history of any psychiatric or serious medical illness. Also, positive family history of any psychiatric illness was screened out. Whole sample was collected by purposive sampling method.
Tools
Young Mania Rating Scale (YMRS)[10]
This scale has 11 items and scores may range from 0 to 60 and gives us information regarding the severity of manic symptoms. Score of less than 6 is considered as euthymic.
Hamilton Depression Rating Scale (HDRS)[11]
This scale provides us information about depressive features present if any. This scale has total of 17 items and total score can range from 0 to 50. Score of less than 7 was considered as euthymic.
General Health Questionaire-12 (GHQ-12)[12]
This scale has 12 items and is sensitive to presence of psychiatric disorders. Score of less than 3 is considered free from psychological disturbances.
Wisconsin Card Sorting Test (WCST)[13]
This test is best known for assessing executive functioning, requiring the ability to develop and maintain an appropriate problem-solving strategy across different changing stimulus conditions. It has two decks of 64 cards each and additional 4 stimulus cards.
Stroop Colour Word Test[14]
This test was used to assess interference effect. This test is known to measure cognitive inhibitory control. It has three forms where subject is required to read out names of colours as fast and as many as possible and form three requires to name colours with which names are written.
Trial Making Test (TMT)[15]
TMT both A & B forms were used to assess mental flexibility and executive functions. Form A has numbers and subject has to draw line connecting numbers in sequence as fast as possible. Form B has both letters and numbers and subject has to start with number and then letter and then again another number following the sequence.
Letter Cancellation Test (LCT)
This was primarily used to assess sustained attention. This consists of letters printed in capitals randomly though out the page and subject has to cancel the given six letters without cancelling other letters or leaving any of the target letters.
Procedure
Sample of 20 adolescents were selected by purposive sampling method and who were diagnosed with Bipolar Disorder satisfying all inclusion and exclusion criteria, also who scored less than 7 on HDRS and less than 6 on YMRS and who were euthymic for at least 2 months. Further 20 controls were selected satisfying all inclusion and exclusion criteria and who score less than 3 on GHQ-12. Controls were matched on age and sex. Both the groups were tested on WCST, TMT, LCT and Stroop Colour Word Test.
Statistical analysis
Statistical analysis was done by using Statistical Package of Social Sciences (SPSS) 16.0 version for windows. Chi Square and t-test were used. The years of education were not matching between patients and normal controls and significant difference was found between the two groups on years of education by using t-Test. Thus, multivariate linear model was used and education was put as a covariate keeping in mind that level of education has effect on cognitive functions and was controlled statistically.
RESULTS
The two groups, patient group and normal control were matched on age and sex. Mean age was 15.85 ± 1.04 and 14 were male and 6 were female in each group. Mean years of education of patients was 9.60 ± 1.14 years and that of control group was 10.55 ± 1.23 years. t-test showed that the two groups were not matching on the basis of level of education (P = 0.02). Total of eight patients (40%) had positive family history of mental illness. Mean age of onset of illness was 13.85 ± 2.16 with total number of episodes as 2.30 ± 0.47. With respect to history of episodes, 9 (45%) had mania, 9 (45%) had depression and 2 (10%) had mixed episode as their first episode of illness. 14 (70%) patients had mania, 4 (20%) had mixed affective episode and 2 (10%) had depression as their second mood episode. Six (30%) had total of three episodes and among them 5 had mania and only one had depression as their third episode and out of twenty patients maximum number, i. e., 13 (65%) were on Lithium with varying doses and similarly 16 (80%) were also on different anti-psychotics [Table 1].
Table 1.
Comparison of performances on different cognitive tests between remitted bipolar adolescents and normal control
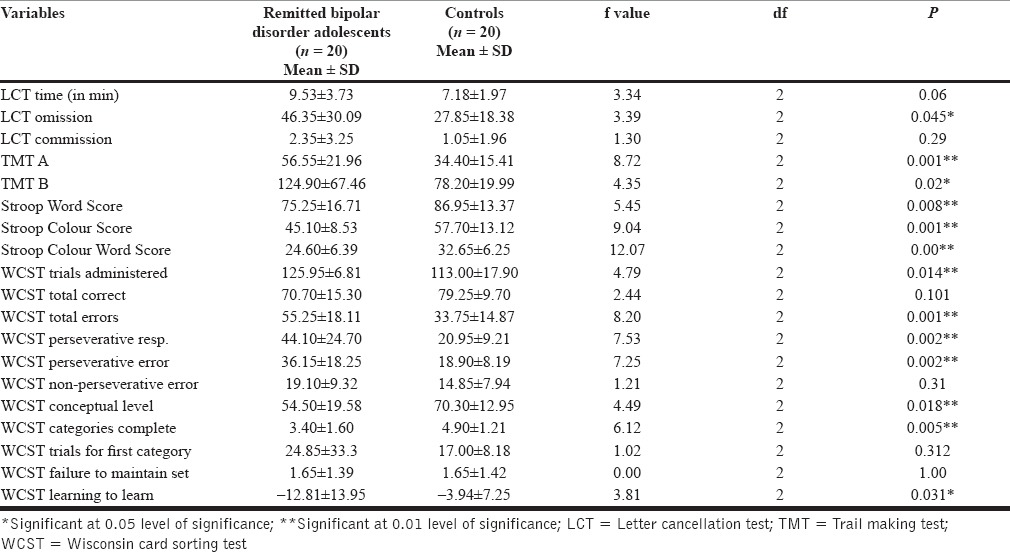
Results revealed significant difference between two groups on LCT omission score and trend towards significance on LCT total time taken to complete the test and no difference was found on LCT commission score. Significant differences on TMT both A & B and on Stroop test (in all domains, i. e., Word score, Colour score and Colour Word score) were also found. On WCST, significant differences were found on WCST trial administered, total errors, perseverative responses, perseverative error, conceptual level, categories complete and learning to learn. While no difference was found on WCST total correct, non-perseverative error, trials for first category and failure to maintain set.
DISCUSSION
This study provided extra evidence that neuro-cognitive deficits persist in adolescent bipolar disorder patients in euthymic states. Performances on different measures of sustained attention and executive functions that this study aimed at were found significantly different between euthymic adolescents and normal controls with normal controls performing better. The two groups were found to be significantly different with respect to level of education. Matching levels of education is always a difficult problem to be taken care of as bipolar disorder causes many adolescents to stop schooling at least for time being and thus patient group lacks behind in terms of years of education.[16] And since education can have direct influence upon cognitive performances it is necessary to control it. Education was put as covariate and thus controlled statistically.
We found impaired performance on sustained attention tasks. LCT was used to assess sustained attention. Most studies have used many different versions of Continuous Performance Test (CPT).[17] but keeping in mind the feasibility and the exposure of patients to computers LCT was used as an assessment of sustained attention. We found significant difference on LCT omission scores and trend towards significance was found in total time taken to complete the test and no significant difference was found in LCT commission scores. Total time taken has been found to measure processing speed, omission score measures inattention and commission score measures impulsivity.[18] Since no difference was found on LCT total time taken but that could be simply because patients omitted many letters and finished the test quickly. Similar findings have been confirmed on adolescent population in other studies with respect to omission scores[8,19] and in remitted population.[20] However, many other studies found no difference in sustained attention.[4,5] In TMT A & B, total time taken to complete the test was used for calculations and performances of patients were found to be significantly less than normal controls and on pediatric bipolar population same findings were reported.[8] Performances on Stroop test were also found to be impaired in adolescent bipolar patients and similarly in paediatric euthymic bipolar disorder patients Lera-Miguel et al.,[3] in 2011, found impaired performances in patient group. Also Doyle[19] did find significant difference on Stroop Colour scores and Stroop Colour Word score but not on Stroop Word score. This study found significant difference on WCST trials administered, total errors, perseverative response, perseverative error, conceptual level, catagories complete the test and learning to learn. On adolescent bipolar subjects, Doyle[19] found no significant difference on total categories completed and failure to maintain set and significant difference was found in non-perseverative error and trend towards significance in perseverative error. Lera-Miguel et al.,[3] found significant difference between adolescent bipolar subjects and normal controls in WCST non-perseverative errors and no significant difference was found on WCST perseverative errors.
There is definitely relationship between bipolar symptoms and cognitive dysfunctions but still what is the cause at first place is still followed by question mark and still the way left is to assess temporal relationship between mood symptoms and cognitive functioning. Cognitive functions are repeatedly reported as impaired even in euthymic states but it always becomes difficult to attribute such deficits to illness itself as such deficits are also known to be secondary to medications, negative impact on social functioning, number of episodes, etc.[21] Similarly, increased frequency of mood episodes makes it further difficult to access the actual attribution. The main problem with most of the studies, as in our study, is that they are cross sectional and it becomes difficult to find the status of cognitive functions pre-morbidly. It is very difficult to say whether cognitive deficits are because of mood symptoms or were present even before acute phase of illness because of diathesis and thus would help us to find out the possible potential endophenotypes to develop mood disorder. Efforts should be invested in investigating cognitive functions in healthy individuals who are at high risk of developing mood disorder avoids much of the confounding variables. Present study could have included richer sample as the sample size was only 20. Similarly, education matched control group would have been better to compare.
In conclusion, our study found that sustained attention and executive dysfunction continue to be present in adolescent bipolar disorder even in euthymic states.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Glahn DC, Bearden CE, Niendam TA, Escamilla MA. The feasibility of neuropsychological endophenotypes in the search for genes associated with bipolar affective disorder. Bipolar Disord. 2004;6:171–82. doi: 10.1111/j.1399-5618.2004.00113.x. [DOI] [PubMed] [Google Scholar]
- 2.Rubinsztein JS, Michael A, Paykel ES, Sahakian BJ. Cognitive impairment in remission in bipolar affective disorder. Psychol Med. 2000;30:1025–36. doi: 10.1017/s0033291799002664. [DOI] [PubMed] [Google Scholar]
- 3.Lera-Miguel S, Andrés-Perpin S, Calvo R, Fatjo-Vilas M, Lourdes F, Lazaro L. Early-onset bipolar disorder: How about visual-spatial skills and executive functions? Eur Arch Psychiatry Clin Neurosci. 2011;261:195–203. doi: 10.1007/s00406-010-0169-z. [DOI] [PubMed] [Google Scholar]
- 4.Robertson HA, Kutcher SP, Lagace DC. No evidence of attentional deficits in stabilized bipolar youth relative to unipolar and control comparators. Bipolar Disord. 2003;5:330–9. doi: 10.1034/j.1399-5618.2003.00042.x. [DOI] [PubMed] [Google Scholar]
- 5.Delbello MP, Zimmerman ME, Mills NP, Getz GE, Strakowski SM. Magnetic resonance imaging analysis of amygdala and other subcortical brain regions in adolescents with bipolar disorder. Bipolar Disord. 2004;6:43–52. doi: 10.1046/j.1399-5618.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- 6.Doyle AE, Wozniak J, Wilens TE, Henin A, Seidman LJ, Petty C, et al. Neurocognitive impairment in unaffected siblings of youth with bipolar disorder. Psychol Med. 2009;39:1253–63. doi: 10.1017/S0033291708004832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glahn DC, Bearden CE, Caetano S, Fonseca M, Najt P, Hunter K, et al. Declarative memory impairment in pediatric bipolar disorder. Bipolar Disord. 2005;7:546–54. doi: 10.1111/j.1399-5618.2005.00267.x. [DOI] [PubMed] [Google Scholar]
- 8.Pavuluri MN, Schenkel LS, Aryal S, Harral EM, Hill SK, Herbener ES, et al. Neurocognitive function in unmedicated manic and medicated euthymic pediatric bipolar patients. Am J Psychiatry. 2006;163:286–93. doi: 10.1176/appi.ajp.163.2.286. [DOI] [PubMed] [Google Scholar]
- 9.Joseph MF, Frazier TW, Youngstrom EA, Soares JC. A quantitative and qualitative review of neurocognitive performance in pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2008;18:595–605. doi: 10.1089/cap.2008.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldburg DP, William PA. User guide to general health questionnaire. Windsor NFER Nelson. (GHQ-12) under realistic assumptions. Biomed Cent Public Health. 1988;8:355–62. [Google Scholar]
- 13.Heaton RK, Chelune GJ, Talley JL. Odessa: Psychological Assessment resources; 1993. Wisconsin card sorting test manual revised and expanded. [Google Scholar]
- 14.Golden CJ, Freshwater SM. Illinois: Stoelting Corporation; 1998. Stroop color and word test a manual for clinical and experimental uses. [Google Scholar]
- 15.Reitan RM, Wolfson D. In theory and clinical interpretation. 2nd ed. Tuscon: Neuropsychology press; 1993. The halstead reitan neuropsychogical test battery. [Google Scholar]
- 16.Saykin AJ, Gur RC, Gur RE, Mozley PD, Mozley LH, Resnick SM, et al. Neuropsychological function in schizophrenia. Selective impairment in memory and learning. Arch Gen Psychiatry. 1991;48:618–24. doi: 10.1001/archpsyc.1991.01810310036007. [DOI] [PubMed] [Google Scholar]
- 17.Ancín I, Santos JL, Teijeira C, Sánchez-Morla EM, Bescós MJ, Argudo I, et al. Sustained attention as a potential endophenotype for bipolar disorder. Acta Psychiatr Scand. 2010;122:235–45. doi: 10.1111/j.1600-0447.2009.01532.x. [DOI] [PubMed] [Google Scholar]
- 18.Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, et al. Behavioural impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depend. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doyle AE, Wilens TE, Kwon A, Seidman LJ, Faraone SV, Fried R, et al. Neuropsychological functioning in youth with bipolar disorder. Biol Psychiatry. 2005;58:540–8. doi: 10.1016/j.biopsych.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 20.Luby JL, Navsaria N. Pediatric bipolar disorder: Evidence for prodromal states and early markers. J Child Psychol Psychiatry. 2010;51:459–71. doi: 10.1111/j.1469-7610.2010.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robinson LJ, Ferrier IN. Evolution of cognitive impairment in bipolar disorder: A systematic review of cross-sectional evidence. Bipolar Disord. 2006;8:103–16. doi: 10.1111/j.1399-5618.2006.00277.x. [DOI] [PubMed] [Google Scholar]


