Abstract
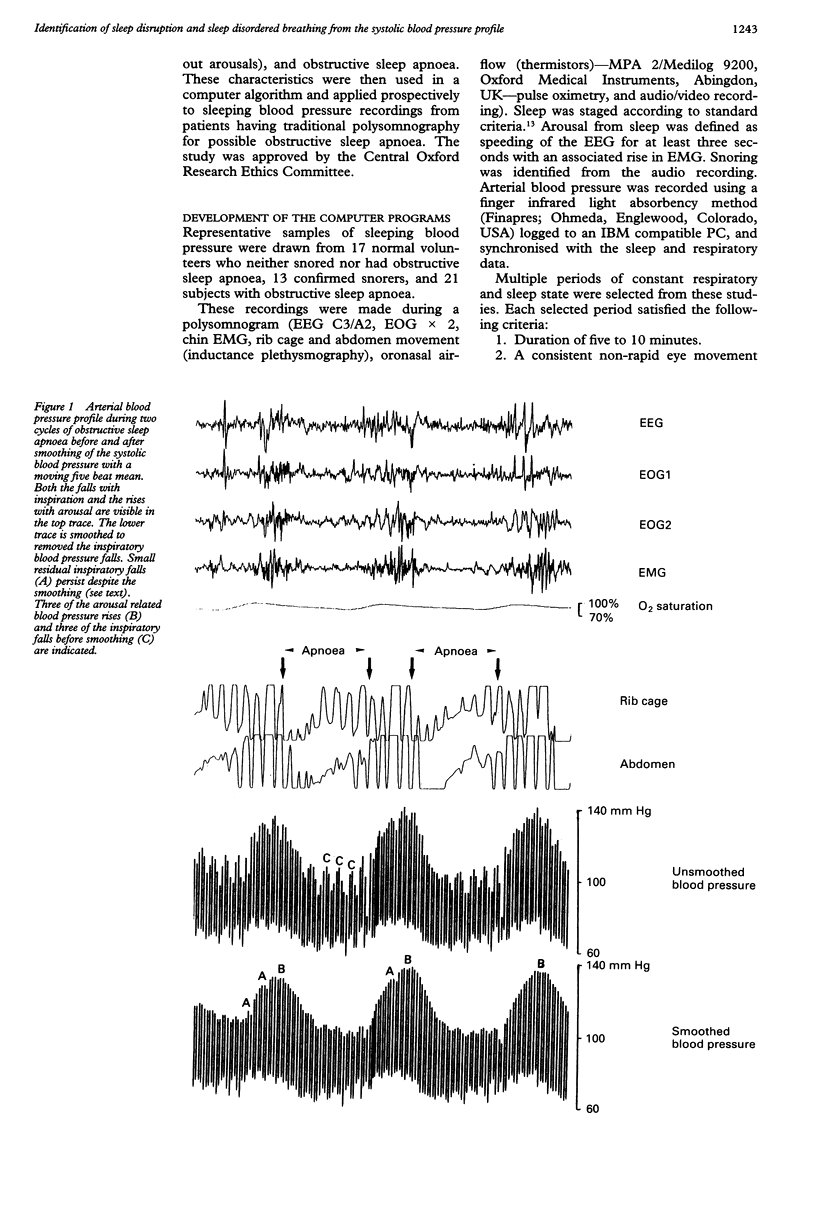
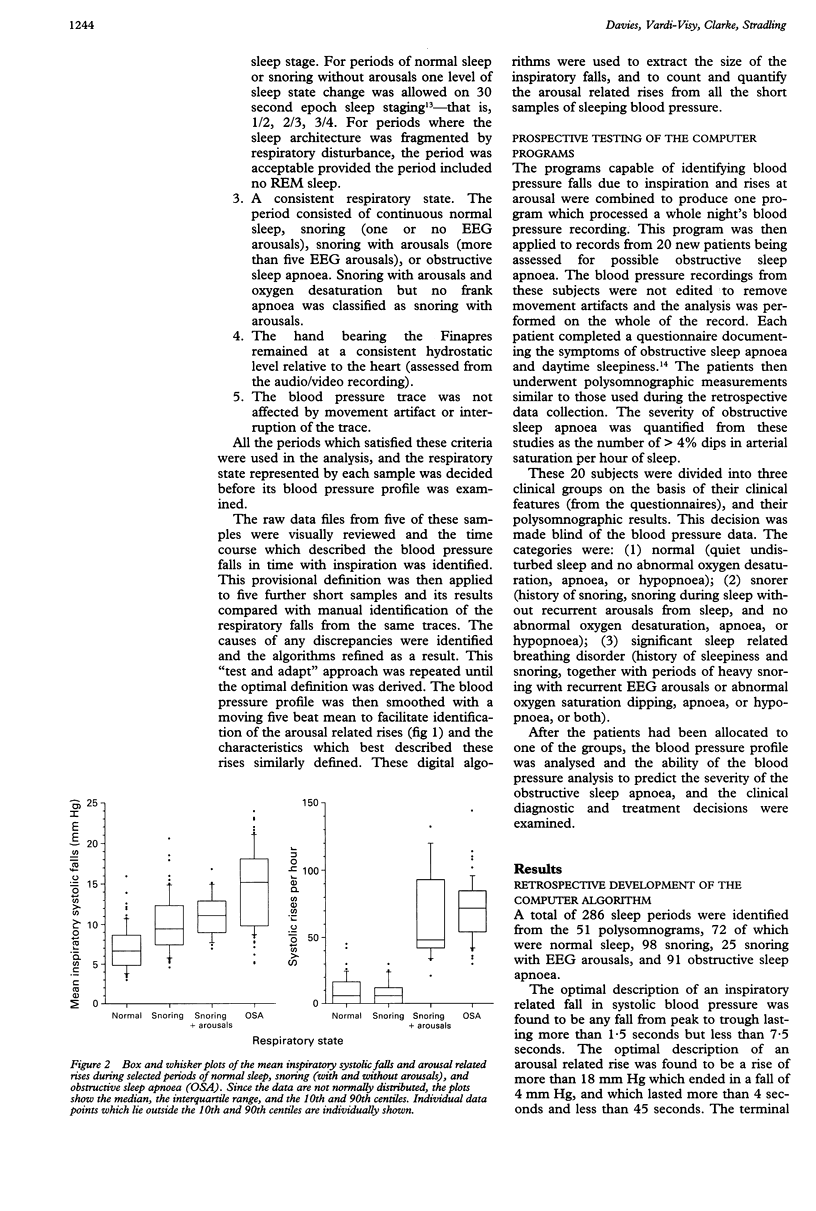
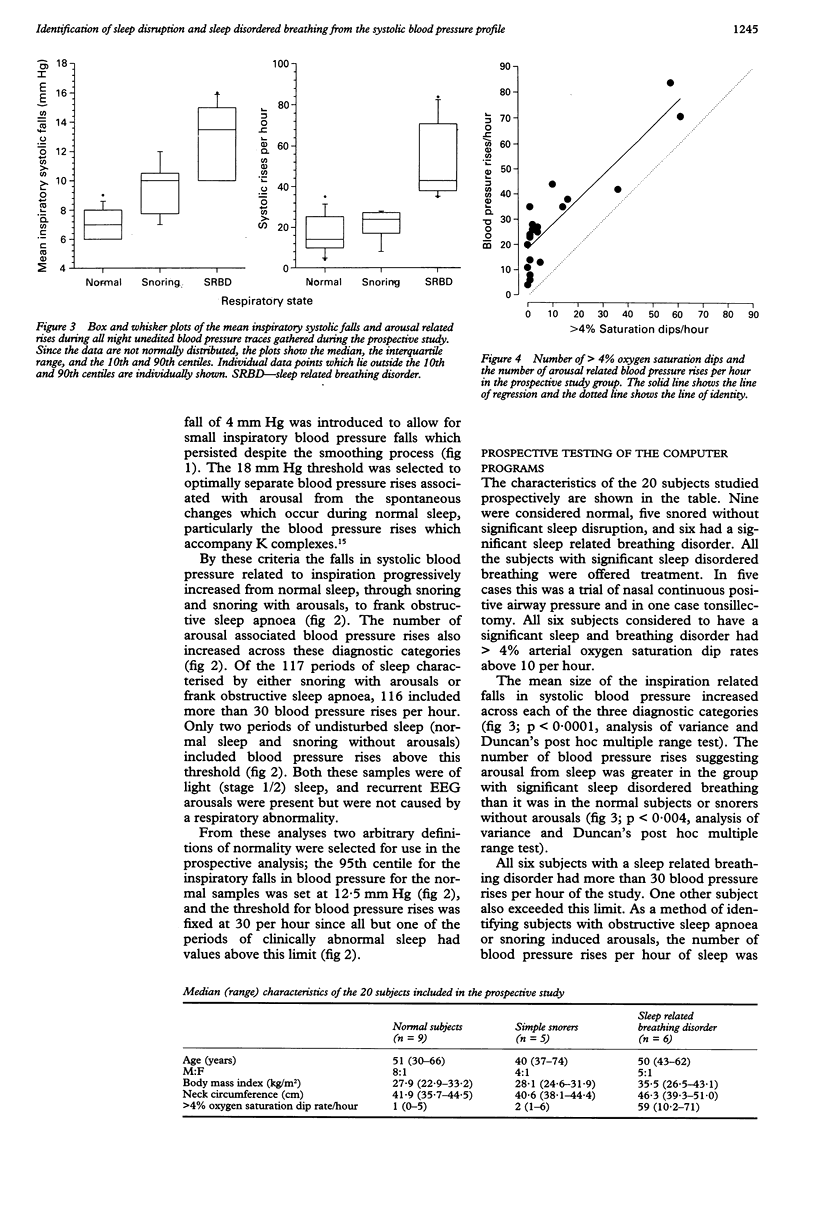
BACKGROUND--Respiratory sleep studies are frequently performed to identify sleep disruption resulting from upper airway obstruction. Traditional polysomnographic studies may not detect brief recurrent sleep disruption and thus fail to recognise a significant problem when apnoea, hypopnoea, or arterial desaturation are not present. Arousal from sleep causes a transient blood pressure rise, and each inspiration causes a transient blood pressure fall. This study assesses whether these blood pressure changes are a useful indirect marker of disturbed sleep, obstructed sleep apnoea, and snoring related sleep disturbance. METHODS--Computer algorithms were developed to identify blood pressure falls caused by inspiration and rises related to arousal from 286 sleeping blood pressure samples of a consistent respiratory state drawn from 51 polysomnographic studies. From these samples, normal ranges for the number of arousal related systolic rises and the average size of the inspiratory falls were established. These were then applied prospectively to all night unedited blood pressure recordings from a further 20 subjects. RESULTS--The size of the inspiratory falls in blood pressure progressively increased from normal sleep, through snoring, to frank obstructive sleep apnoea. The 95th centile of normal was 12.5 mm Hg. The number of arousal related blood pressure rises also increased during obstructive sleep apnoea and periods of snoring with associated arousals, compared with normal undisturbed sleep, and all these periods of disturbed sleep included more than 30 such rises per hour. When these blood pressure features were examined in the 20 subjects studied prospectively, the six with a sleep related breathing disorder could all have been identified from their systolic blood pressure profile alone. CONCLUSIONS--The systolic blood pressure profile may be helpful in identifying patients with obstructive sleep apnoea, snoring with arousals, or other sleep disruption syndromes.
Full text
PDF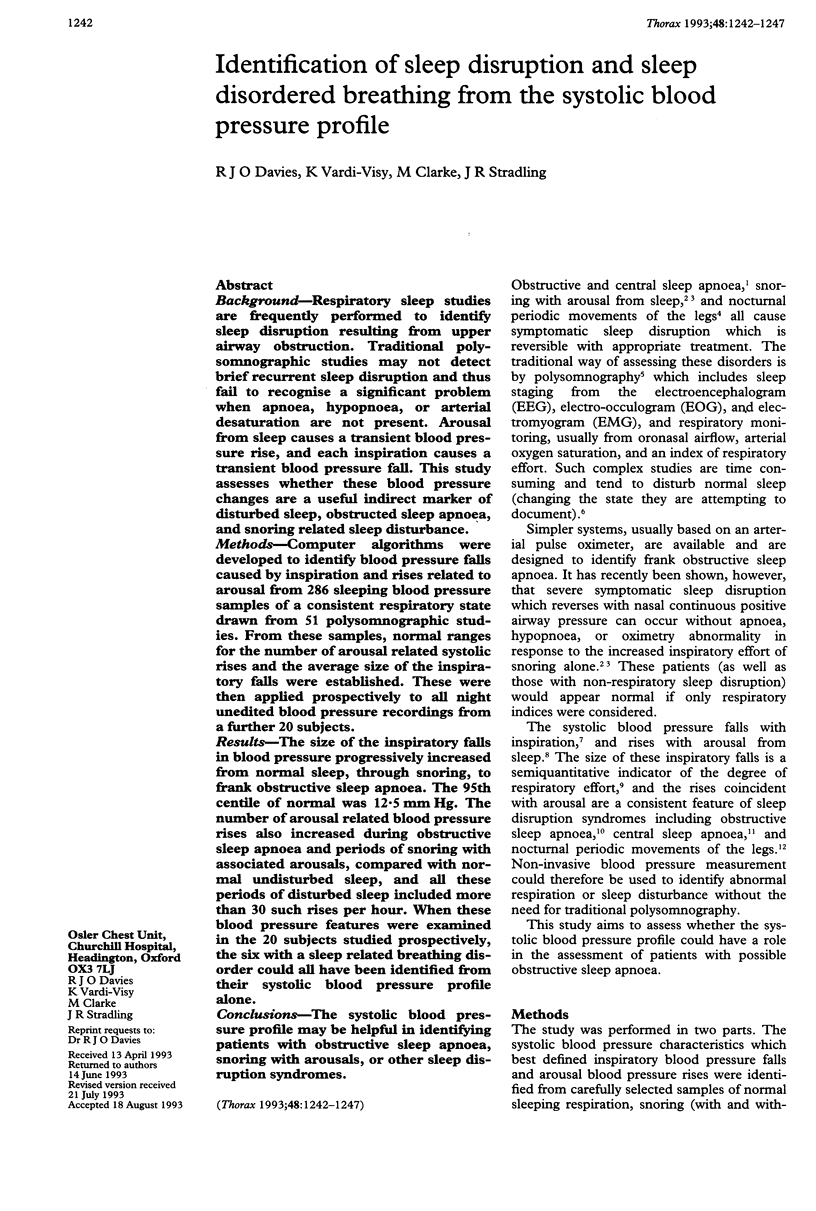
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ali N. J., Davies R. J., Fleetham J. A., Stradling J. R. Periodic movements of the legs during sleep associated with rises in systemic blood pressure. Sleep. 1991 Apr;14(2):163–165. [PubMed] [Google Scholar]
- Anholm J. D., Powles A. C., Downey R., 3rd, Houston C. S., Sutton J. R., Bonnet M. H., Cymerman A. Operation Everest II: arterial oxygen saturation and sleep at extreme simulated altitude. Am Rev Respir Dis. 1992 Apr;145(4 Pt 1):817–826. doi: 10.1164/ajrccm/145.4_Pt_1.817. [DOI] [PubMed] [Google Scholar]
- Block A. J., Cohn M. A., Conway W. A., Hudgel D. W., Powles A. C., Sanders M. H., Smith P. L. Indications and standards for cardiopulmonary sleep studies. Sleep. 1985 Dec;8(4):371–379. [PubMed] [Google Scholar]
- Boehmer R. D. Continuous, real-time, noninvasive monitor of blood pressure: Penaz methodology applied to the finger. J Clin Monit. 1987 Oct;3(4):282–287. doi: 10.1007/BF03337384. [DOI] [PubMed] [Google Scholar]
- Coccagna G., Mantovani M., Brignani F., Manzini A., Lugaresi E. Laboratory note. Arterial pressure changes during spontaneous sleep in man. Electroencephalogr Clin Neurophysiol. 1971 Sep;31(3):277–281. doi: 10.1016/0013-4694(71)90098-8. [DOI] [PubMed] [Google Scholar]
- Davies R. J., Ali N. J., Stradling J. R. Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax. 1992 Feb;47(2):101–105. doi: 10.1136/thx.47.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies R. J., Belt P. J., Roberts S. J., Ali N. J., Stradling J. R. Arterial blood pressure responses to graded transient arousal from sleep in normal humans. J Appl Physiol (1985) 1993 Mar;74(3):1123–1130. doi: 10.1152/jappl.1993.74.3.1123. [DOI] [PubMed] [Google Scholar]
- Guilleminault C., Stoohs R., Duncan S. Snoring (I). Daytime sleepiness in regular heavy snorers. Chest. 1991 Jan;99(1):40–48. doi: 10.1378/chest.99.1.40. [DOI] [PubMed] [Google Scholar]
- Guilleminault C., Tilkian A., Dement W. C. The sleep apnea syndromes. Annu Rev Med. 1976;27:465–484. doi: 10.1146/annurev.me.27.020176.002341. [DOI] [PubMed] [Google Scholar]
- Hillerdal G., Hetta J., Lindholm C. E., Hultcrantz E., Boman G. Symptoms in heavy snorers with and without obstructive sleep apnea. Acta Otolaryngol. 1991;111(3):574–581. doi: 10.3109/00016489109138386. [DOI] [PubMed] [Google Scholar]
- Hornyak M., Cejnar M., Elam M., Matousek M., Wallin B. G. Sympathetic muscle nerve activity during sleep in man. Brain. 1991 Jun;114(Pt 3):1281–1295. doi: 10.1093/brain/114.3.1281. [DOI] [PubMed] [Google Scholar]
- Johnson L. C., Lubin A. The orienting reflex during waking and sleeping. Electroencephalogr Clin Neurophysiol. 1967 Jan;22(1):11–21. doi: 10.1016/0013-4694(67)90004-1. [DOI] [PubMed] [Google Scholar]
- Karam M., Wise R. A., Natarajan T. K., Permutt S., Wagner H. N. Mechanism of decreased left ventricular stroke volume during inspiration in man. Circulation. 1984 May;69(5):866–873. doi: 10.1161/01.cir.69.5.866. [DOI] [PubMed] [Google Scholar]
- Mendels J., Hawkins D. R. Sleep laboratory adaptation in normal subjects and depressed patients ("first night effect"). Electroencephalogr Clin Neurophysiol. 1967 Jun;22(6):556–558. doi: 10.1016/0013-4694(67)90063-6. [DOI] [PubMed] [Google Scholar]
- Parati G., Casadei R., Groppelli A., Di Rienzo M., Mancia G. Comparison of finger and intra-arterial blood pressure monitoring at rest and during laboratory testing. Hypertension. 1989 Jun;13(6 Pt 1):647–655. doi: 10.1161/01.hyp.13.6.647. [DOI] [PubMed] [Google Scholar]
- Rauscher H., Popp W., Zwick H. Quantification of sleep disordered breathing by computerized analysis of oximetry, heart rate and snoring. Eur Respir J. 1991 Jun;4(6):655–659. [PubMed] [Google Scholar]
- Roehrs T., Zorick F., Wittig R., Conway W., Roth T. Predictors of objective level of daytime sleepiness in patients with sleep-related breathing disorders. Chest. 1989 Jun;95(6):1202–1206. doi: 10.1378/chest.95.6.1202. [DOI] [PubMed] [Google Scholar]
- Shepard J. W., Jr Gas exchange and hemodynamics during sleep. Med Clin North Am. 1985 Nov;69(6):1243–1264. doi: 10.1016/s0025-7125(16)30985-3. [DOI] [PubMed] [Google Scholar]
- Smith N. T., Wesseling K. H., de Wit B. Evaluation of two prototype devices producing noninvasive, pulsatile, calibrated blood pressure measurement from a finger. J Clin Monit. 1985 Jan;1(1):17–29. doi: 10.1007/BF02832685. [DOI] [PubMed] [Google Scholar]
- Smyth H. S., Sleight P., Pickering G. W. Reflex regulation of arterial pressure during sleep in man. A quantitative method of assessing baroreflex sensitivity. Circ Res. 1969 Jan;24(1):109–121. doi: 10.1161/01.res.24.1.109. [DOI] [PubMed] [Google Scholar]



