Abstract
Gastroparesis is a very common condition, however many times it becomes difficult to manage even after long-term treatment due to multiple etiologies or improper therapy. Patients with severe gastroparesis are considered candidates for gastric electrical stimulants. The “Pulse Therapy” using metoclopramide and erythromycin to reprogram gastric motility can delay or even avoid the need for gastric electrical stimulants. This case report focuses on a patient with severe gastroparesis, who was considered for a gastric pacemaker implantation and was instead treated successfully with “Pulse Therapy.” As a part of this regimen, he was given metoclopramide continuously for 3 months along with pulses of erythromycin for 10 days a month for 3 months. Patient recovered dramatically that he no longer remained a candidate for gastric pacemaker implantation. This case study emphasizes on how the proper use of prokinetic agents based on symptoms and gastric emptying study can reprogram the stomach motility in these patients with severe gastroparesis.
Keywords: Diabetic gastroparesis, erythromycin, gastric emptying study, gastroparesis, Helicobacter pylori, idiopathic gastroparesis, metoclopramide, past Helicobacter pylori infection, prokinetic agents, severe gastroparesis
Introduction
Gastroparesis and its related symptoms are among the most common gastric problems faced by patients, which emphasizes the need for it to be addressed appropriately. Many etiologies are responsible for gastroparesis, such as diabetes, chronic renal failure (CRF), previous Helicobacter pylori infection, gastric surgery, low vitamin D level, hypothyroidism etc. Patients with no discernible etiology are labeled as “Idiopathic Gastroparesis.” The treatment varies depending on the etiology. In the presence of multiple etiologies and severe gastroparesis, as illustrated here, patients are then considered candidates for gastric electrical stimulants like gastric pacemakers. With the proper use of “Pulse Therapy,” one can improve symptoms of gastroparesis and possibly avoid such invasive procedures. We illustrate that “Pulse Therapy” with metoclopramide and erythromycin reprograms the gastric motility and restores the gastric rhythm.
Case Report
A 43-year-old man admitted to hospital on 05/08/2011 with severe nausea and vomiting and his past medical history including insulin dependent diabetes mellitus (DM), CRF, diabetic retinopathy and gastroparesis. At that time, gastric emptying scintigraphy revealed severe gastroparesis. Patient was referred for consultation for possible gastric pacemaker. Patient was initially treated with ondansetron 4 mg po qid, omeprazole magnesium 20 mg po daily, famotidine 20 mg po bid and metoclopramide HCL 5 mg po tid. His HbA1c at that time was 12. His DM was treated with insulin lispro 22 units before breakfast, insulin lispro 26-28 units at dinner and insulin glargine 15-18 units at bedtime. His HbA1c improved to six and his vomiting ceased. Patient also complained of weight loss and occasional nausea. He denied abdominal pain, postprandial fullness, bloating, heart burn, diarrhea, constipation or any other changes in bowel movements.
Patient was also being treated for high cholesterol, hypertension, vitamin D deficiency and hyperphosphatemia with Stage 4 and 5 CRF, requiring hemodialysis 3 times/week. His medications included, atorvastatin calcium 40 mg once daily (OD), losartan potassium 50 mg OD, ferrous sulfate 325 mg bid, carvedilol 25 mg bid, vitamin D 50,000 unit (ergocalciferol) one tab monthly, sevelamercarbonate 800 mg tid, lidocaine and prilocaine cream 2.5% 3 times weekly after dialysis and aspirin-dipyridamole bid.
As part of his initial evaluation, he underwent two esophagogastroduodenoscopies (EGD). The first was on 02/09/11, which revealed H. pylori infection on stomach biopsy specimen and he was treated with amoxicillin 500 mg po bid, clarithromycin 500 mg po bid and omeprazole magnesium 20 mg po bid for 14 days. A repeat EGD on 11/11/11 showed chronic inactive gastritis with reactive gastropathy and no further evidence of H. pylori. Duodenum biopsy performed did not show any pathology.
Gastric emptying study (GES) was ordered on March 8, 2012, which showed markedly delayed gastric emptying function. At the end of 3 h (180 min) of imaging, approximately 50% of administered activity was left in the stomach. His HbA1c at the time of the study was 6.2. Then patient was started on Pulse Therapy. He was given metoclopramide 10 mg qid for 3 months along with 250 mg erythromycin tid. Erythromycin was given in pulses of 10 days every month for 3 months. His GES was repeated after 3 months and revealed mild delayed gastric emptying with T1/2 117 min. After treatment with pulse therapy and improvement management of his DM, significant improvement was seen in all gastric emptying measurements compared with his prior study.
Discussion
Gastroparesis is a clinical condition in which patients have symptoms of delayed gastric emptying with no evidence of physiological obstruction. The most common etiology for gastroparesis is idiopathic followed by DM, post-surgical, connective tissue disorders, neurological disorders such as parkinsonism, ischemic diseases, metabolic disorders and many other less common causes.
Diabetes is the second most common etiology for gastroparesis. Studies showed that 31% of patient with gastroparesis has a diabetic etiology. Diabetic patients often have more gastrointestinal (GI) complications than the general population due to their higher prevalence of gastroparesis.[1] Nearly, 18% of the diabetic patients experienced upper GI symptoms; specifically, delayed gastric emptying is found in 27-65% of patients with Type 1 diabetes while it is found in 30% of patients with Type 2 diabetes.[1] The etiology of diabetic gastroparesis itself is numerous and not clearly established. Certain important factors include autonomic neuropathy, acute hyperglycemia, abnormalities of gut hormones and neurotransmitters, thyroid function, gastric acid secretion and H. pylori infection.[2] A causal relationship linking DM and gastroparesis is poor glycemic control since postprandial blood glucose concentrations are both determined by and a determinant of the delivery of nutrients from the stomach into the small intestines.[3]
CRF may be the cause of delayed gastric emptying theoretically because of uremia-induced neuropathy, electrolyte disturbance, vitamin D deficiency, metabolic acidosis and anemia.[4] To conclude, CRF as a cause of delayed gastric emptying, we have to take into consideration several factors specific to patient such as current blood urea nitrogen and creatinine level, duration of renal failure, history of hemodialysis or peritoneal dialysis or conservative treatment and the study used for timing gastric emptying. There are conflicting reports for improvement of gastric retention after hemodialysis; while some report shows improvement.[5] Others showing no improvement.[6]
Non-pharmacological therapy should be tried first in patients who have less severe symptoms of gastroparesis. Non-pharmacological measures includes mainly dietary modifications such as small frequent meals, more liquid based diet and avoidance of solid foods and high fat meals.[7] Symptomatic gastroparesis requires pharmacological treatment mainly with prokinetic medications such as metoclopramide, erythromycin and domperidone.[7,8] Amongst these, domperidone is not approved for any medical condition in US.[9] Metoclopramide is a combined serotonin (5-hydroxytryptamine4) agonist and dopamine D2 antagonist.[7,10] It stimulates esophageal, stomach and small intestinal contractions and enhances gastric emptying. Erythromycin acts on motilin receptors present on neural and smooth muscles, which potentiates gastro-duodenal motility.[7,11]
Following two tables [Tables 1 and 2] are the proposed algorithms for the use of prokinetic agents in gastroparesis based on GES and severity of symptoms.
Table 1.
Gastroparesis grading and proposed treatment
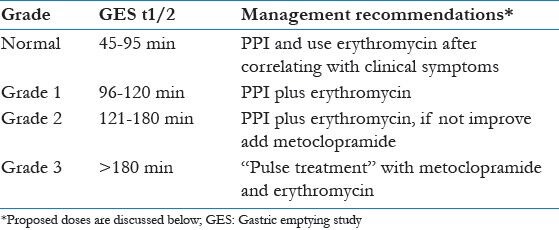
Table 2.
Gastroparesis grading and management plan according to symptoms and symptom score
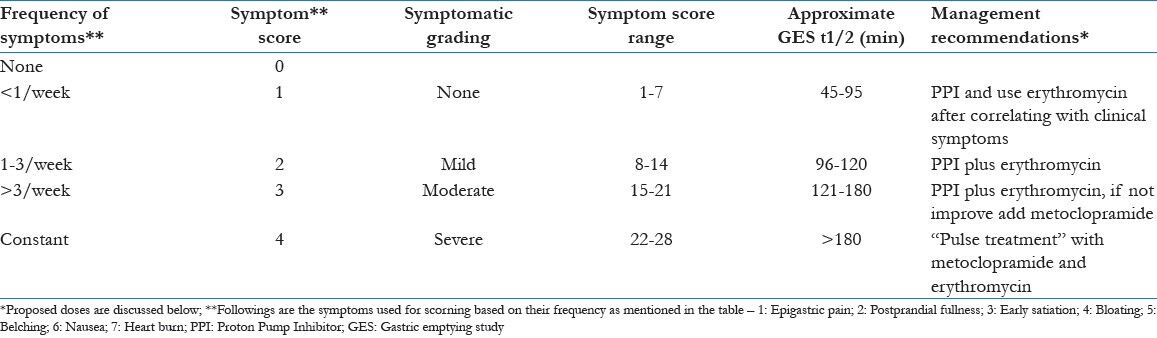
Erythromycin should be given 250 mg 3 times a day. Metoclopramide should be started 5 mg 2 times daily and can increase up to 40 mg/day according to symptoms. When taking metoclopramide, patient should be followed-up regularly every 2 weeks to monitor symptom control and to identify any development of side-effects of metoclopramide, especially those related to cardiac and central nervous system.
Our patient is diabetic, with end stage renal disease on dialysis and was also previously treated for H. pylori infection in the past. H. pylori infection damages the gastric neurons and may subsequently account for the delayed gastric emptying. Even after eradication of infection, gastroparesis can occur after few years due to initial damage of gastric nervous system. This effect is more pronounced with the presence of diabetes.[12] Patient was referred to us after failing previous treatments for his gastroparesis. He continued to be symptomatic even after well management of his CRF and diabetes. Pulse Therapy for this patient would be beneficial since his stomach motility had also been altered by his previous H. pylori infection. He was started with two prokinetic drugs, metoclopramide and erythromycin. He was given metoclopramide 10 mg 4 times daily continuously for 3 months along with 10 days of erythromycin 250 mg 3 times daily every month for 3 months. This “Pulse Treatment” showed dramatic improvement in symptoms, as well as in gastric emptying time. This proposed regimen reprograms the disturbed gastric and intestinal movements. Patients’ symptoms have improved, however he may require low dose of metoclopramide for one more month after the initial treatment.
Conclusion
This case report focuses on how “Pulse Treatment” with prokinetic agents improved severe gastroparesis-related symptoms and gastric emptying time in patient with past H. pylori infection and well-controlled DM and CRF. We can avoid unnecessary endoscopic treatment or gastric electrical stimulants like pacemakers by modifying the medication approach and using two prokinetic agents as in our proposed “Pulse Therapy.”
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Hasler WL. Gastroparesis: Pathogenesis, diagnosis and management. Nat Rev Gastroenterol Hepatol. 2011;8:438–53. doi: 10.1038/nrgastro.2011.116. [DOI] [PubMed] [Google Scholar]
- 2.De Block CE, De Leeuw IH, Pelckmans PA, Callens D, Máday E, Van Gaal LF. Delayed gastric emptying and gastric autoimmunity in type 1 diabetes. Diabetes Care. 2002;25:912–7. doi: 10.2337/diacare.25.5.912. [DOI] [PubMed] [Google Scholar]
- 3.Sfarti C, Trifan A, Hutanasu C, Cojocariu C, Singeap AM, Stanciu C. Prevalence of gastroparesis in type 1 diabetes mellitus and its relationship to dyspeptic symptoms. J Gastrointestin Liver Dis. 2010;19:279–84. [PubMed] [Google Scholar]
- 4.Hirako M, Kamiya T, Misu N, Kobayashi Y, Adachi H, Shikano M, et al. Impaired gastric motility and its relationship to gastrointestinal symptoms in patients with chronic renal failure. J Gastroenterol. 2005;40:1116–22. doi: 10.1007/s00535-005-1709-6. [DOI] [PubMed] [Google Scholar]
- 5.Hirata ES, Mesquita MA, Alves Filho G, Camargo EE. Gastric emptying study by scintigraphy in patients with chronic renal failure. Rev Bras Anestesiol. 2012;62:39–47. doi: 10.1016/S0034-7094(12)70101-0. [DOI] [PubMed] [Google Scholar]
- 6.Adachi H, Kamiya T, Hirako M, Misu N, Kobayashi Y, Shikano M, et al. Improvement of gastric motility by hemodialysis in patients with chronic renal failure. J Smooth Muscle Res. 2007;43:179–89. doi: 10.1540/jsmr.43.179. [DOI] [PubMed] [Google Scholar]
- 7.Hasler WL. Gastroparesis – Current concepts and considerations. Medscape J Med. 2008;10:16. [PMC free article] [PubMed] [Google Scholar]
- 8.Sturm A, Holtmann G, Goebell H, Gerken G. Prokinetics in patients with gastroparesis: A systematic analysis. Digestion. 1999;60:422–7. doi: 10.1159/000007687. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. U.S. Food and Drug Administration; domperidone safety instructions. [Last updated on 2009 Jun 19, Last accessed on 2012, July 21]. Available from: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm154914.htm .
- 10.McCallum RW, Valenzuela G, Polepalle S, Spyker D. Subcutaneous metoclopramide in the treatment of symptomatic gastroparesis: Clinical efficacy and pharmacokinetics. J Pharmacol Exp Ther. 1991;258:136–42. [PubMed] [Google Scholar]
- 11.Lin HC, Sanders SL, Gu YG, Doty JE. Erythromycin accelerates solid emptying at the expense of gastric sieving. Dig Dis Sci. 1994;39:124–8. doi: 10.1007/BF02090071. [DOI] [PubMed] [Google Scholar]
- 12.Ojetti V, Migneco A, Silveri NG, Ghirlanda G, Gasbarrini G, Gasbarrini A. The role of H. pylori infection in diabetes. Curr Diabetes Rev. 2005;1:343–7. doi: 10.2174/157339905774574275. [DOI] [PubMed] [Google Scholar]


