Abstract
Background:
The close sustained contact of family physician with their patients and local community makes preventive care an integral part of their routine work. Most cardiovascular diseases (CVD) can be prevented by addressing their risk factors. There are several guidelines that recommend different CV risk assessment tools to support CV prevention strategies.
Aim:
This study aimed to assess awareness and attitude of global CV risk assessment and use of their tools by family physicians; aiming to improve CV prevention service.
Methods:
The current study is a cross-sectional descriptive analytic. Sixty-five family physicians were asked to respond to, validated anonymous questionnaire to collect data about characteristics of family physicians, their awareness, attitude, current use, barriers, and recommendations of global CV risk assessment. Statistical Package for Social Sciences (SPSS) version 18 was used for data entry and analysis.
Results:
Awareness of guidelines of global CV risk assessment was relatively higher regarding the American guidelines (30.8%) than that recommended by World Health Organization (WHO) for Egypt (20.2%). 50.8% of participants had favorable attitude. There was statistical significant relationship between attitude scores and physician characteristics; age (P = 0.003), qualification (P = 0.001) and number of patients seen per week (P = 0.009). Routine use of global CV risk assessment tools was reported only (23%) by family physicians.
Conclusion:
Relative higher attitude scores than use of global CV risk assessment tools in practice. The most frequent barriers were related to lack of resources and shortage in training/skills and the raised suggestions were towards training.
Keywords: Cardiovascular diseases, family physician, prevention, risk assessment tools
Introduction
Over 80% of cardiovascular diseases (CVD) deaths take place in low- and middle-income countries.[1] In Egypt CVD deaths account for 39% of total deaths in all ages.[2] Family physicians’ contact with their patients and local community makes preventive care an integral part of their routine work.[3] CV risk factors interact with each other; moderate reductions in several risk factors can be more effective than major reductions in one.[4]
Early guidelines focused on those at the highest relative risks for developing CVD related to markedly individual risk factors. Later, researchers and policy makers have focused on absolute risk estimation to provide absolute probabilities of developing CVD within a given time frame.[5,6]
There are several guidelines that recommend global/total risk estimation, among them the American guidelines depend on Framingham Risk Score,[7] European guidelines that include Systematic Coronary Risk Evaluation (SCORE).[8] World Health Organization/International Society of Hypertension (WHO/ISH) provide CV prediction charts.[9] WHO charts that can be used in Egypt are Eastern Mediterranean (EMR D).[10] Availability of the different guidelines allows physicians to estimate total coronary heart disease (CHD) risk or CVD risk using simplified charts, tables, computer programs, and web-based tools in primary care. The challenge is not to be concerned as to which method of risk assessment is better, but rather to encourage their implementation in day-to-day risk evaluation and management.[11,12]
The present study aimed to assess awareness, attitude, and use of global CV risk assessment by family physicians; aiming to improve cardiovascular prevention and management strategies in primary care.
Materials and Methods
The current study is a cross-sectional analytic one that was conducted from March 2012 to November 2012. It was carried out in nine Family Medicine Centers affiliated to Suez Canal University that are distributed in Ismailia, Suez and Port Said Governorates. Convenience sampling was done and it included all family physicians (65) working in Family Medicine Centers. The participants were asked to respond to anonymous semistructured questionnaire. The questionnaire was developed by the researcher revised by the supervisors. The questionnaire included four sections: Part one, to collect selected demographic variables as (gender, age, qualification, experience years in family medicine, practice location, and number of adult patients usually seen per week) in addition to their awareness and sources of information about CV prevention guidelines. Part two included multiple choice questions about attitude. Attitude was assessed using four items about the importance, readiness, the routine of CV risk assessment, and importance of risk factors; and four items about usefulness of this assessment in relation to preventive measures, reduction of risks and its use within primary care. Five-point Likert Scale was used, defined by scoring: Strongly agree (5), agree (4), uncertain (3), disagree (2), and strongly disagree (1). Score was favorable attitude if it was equal or above their means which was estimated as ≥70%. Use of global risk assessment tools was self-reported to two questions about the frequency of using global CV risk assessment tools in adults for primary prevention and the use of WHO prediction charts. Physicians were as routine users if they responded by usually or always. Part three, to collect data about method of CV risk assessment was about self-reported documentation of CV risk factors (which included blood pressure, body mass index, family history of CVD-documentation of diabetic patient and follow-up, lipid profile) and documentation of CV risk scores by the family physicians in medical records. Part four was about family physicians’ barriers and recommended suggestion to support the use of global CV risk assessment tools in primary care. Pilot study was conducted on 10% of the study population (these were not included in the final results) to test the relevancy of the questionnaire to the intended topics and the degree to which the questions were interpreted and understood by different family physicians. Validity and reliability of the questionnaire were tested.
Ethical considerations
The study was approved by the ethics committee of Faculty of Medicine, Suez Canal University and has been performed in accordance with the ethical standards laid down in the Declaration of Helsinki (1964). Questionnaire was anonymous, did not contain any critical questions, and confidentiality of the data were maintained.
Statistical analysis
The obtained data were coded, entered, and processed on a personal computer using Statistical Package of Social Science (SPSS) version 16. Data were presented in tables and graphs. The appropriate statistical tests were used to identify significant difference. Continuous values were expressed as mean ± SD. Chi-square or Fisher exact test was (if cells including frequency <5) used to compare categorical variables. P-value of <0.05 will be considered statistically significant.
Results
Physician characteristics
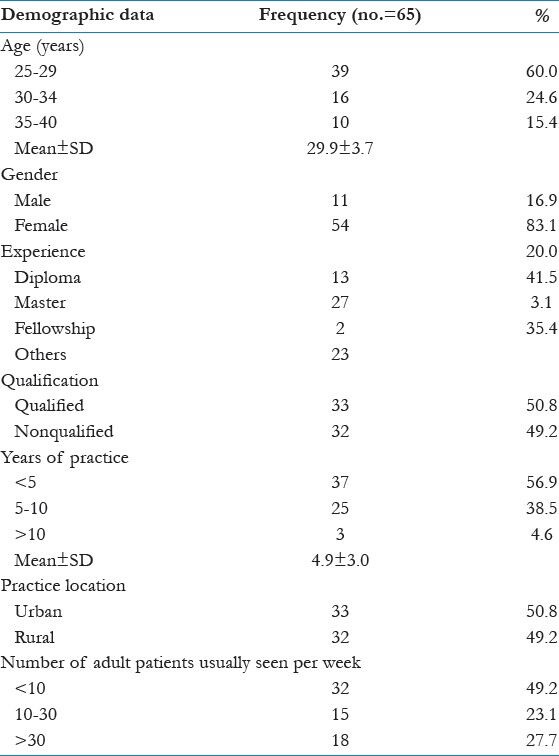
Table 1 showed that Sixty-five physicians were included in the present study; their mean age was 29.9 ± 3.7 years. Most of them were females (83.1%). Twenty-seven (41.5%) of the participants were under training for master degree, half of them (50.8%) were qualified with master degree/diploma. 56.9% of physicians worked for <5 years with the mean years of practice for 4.9 ± 3.0 and unfortunately half of them (49.2%) examined <10 patients per week within practice. Physicians worked in urban and rural areas were almost equal (50.8 and 49.2%, respectively).
Table 1.
Personal characteristics of the family physicians (N = 65)
Physician awareness
The study revealed that (82%) of family physicians were aware of the different guidelines providing CV risk assessment either individual or global. Of these guidelines; American Heart Association (AHA), (30.8%), WHO (20.2%), Adult Treatment Panel III (ATP III), (20%), and European (6.2%) were the sources for global CVD risk assessment information. High awareness was for individual risk guidelines of hypertension or diabetes as reported by more than two-thirds of physicians (70%) for both.
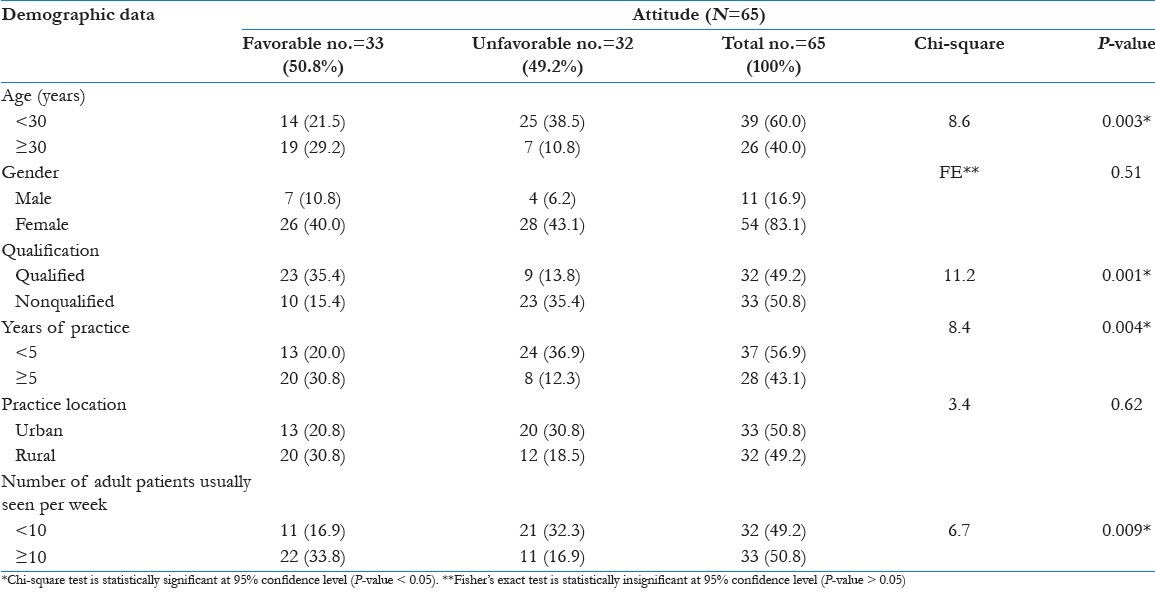
Physician attitude
Concerning physicians’ attitude, the current study revealed that approximately half of the participant physicians had favorable attitude (50.8%) and there was a significant relation between physicians’ attitude and each of age, qualification, years of experience, and patient number seen per week. The difference was statistically significant P < 0.05 as shown in Table 2.
Table 2.
The relationship of family physicians’ attitude towards global cardiovascular risk assessment and their personal characteristics
Cardiovascular risk assessment
This current study showed that 87.7, 86.2, and 81.5% of participating physicians would always register individual risk factors as the smoking status, family history of CVD, and blood pressure, respectively to assess CVD risk and only 60.5% of them document blood glucose. Unfortunately, they did not record the estimated CV risks.
CV risk assessment tools uses were reported by about less than quarter of physicians (23%). 14.9% of participant physicians use WHO risk prediction charts.
Barriers and recommendations
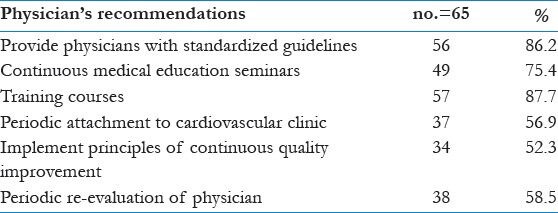
In the present study, the most frequent barriers for CV risk assessment were deficient laboratory investigations within primary care settings (90.8%), poor skills/training of physicians (81.5%), and financial resources (80%) as shown in table 3. The majority of participating physicians (87.7%) recommended training courses and 86.2% recommended providing physicians with standardized guidelines as shown in table 4.
Table 3.
Barriers for cardiovascular (CV) risk assessment tools application as reported by the participating physicians
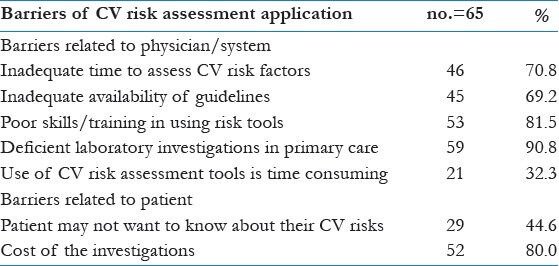
Table 4.
Physician's recommendations for improving cardiovascular risk assessment practice in primary care centers
Discussion
The study revealed that 82% of family physicians were aware of the different guidelines providing CV risk assessment for primary prevention of CVDs. The commonest sources for global CVD risk assessment information was only reported for AHA (30.8%), WHO (20.2%), ATP III (20%), and European (6.2%); meanwhile their awareness was higher to individual risk guidelines as Joint National Committee VI (JNC VI) in management of hypertension and American diabetes Association (ADA) for management of diabetes.
This was in agreement with the study by Doroodchi et al.,[13] to identify practice patterns and barriers among US general internists and family physicians in regard to CV risk management found that the clinical practice guidelines were identified by approximately one-third of survey respondents as the most important tool for delivering optimal care to their patients. But it was inconsistent with the study by Shillinglaw et al.,[14] who use a web-based survey of US 952 physicians (family physicians, general internists, and cardiologists) to examine awareness of tools, attitude, method, and use of CHD risk assessment and frequency of using CHD risk assessment to guide primary prevention. He found that awareness of tools to calculate global CHD risk appears high (92%) in spite of their lowered use practice.
Favorable attitude was found by only 50.2% and it was not consistent with the study by Shillinglaw et al.,[14] who found that over 80% agreed that CHD risk calculation is useful, improves patient care, and leads to better decisions about recommending preventive therapies. Favorable attitude was found among qualified physicians older than 30 years and with experience of more than 5 years which are closely related to each other and is expected to be improved with professional development.
This current study showed that 87.7, 86.2, and 81.5% of participating physicians would always document individual risk factors as the smoking status, family history of CVD, and blood pressure, respectively to assess CVD risk and only 60.5% of them assess blood glucose. Unfortunately, physician did not document CV risk scores. Registration of risk factors allows the physicians, selection of adult for application of CV risk tools, and estimation of risk score.
The total risk assessment needs considering group of factors and unfortunately the low use of global risk assessment and the better awareness of individual risk guidelines, this means that frequently physicians still follow individual CV risk factors assessment which is not coping with recent guidelines of primary prevention. This to some extent in agreement with Australian study by Torley et al.,[15] which found few physicians formally, assessed CV risk. Instead, they assessed individual risks such as blood pressure, weight, smoking, and family history; estimating the CV risk informally with clinical judgment.
CV risk assessment tools were reported in routine work by only 23%. WHO risk prediction charts use that fit more with Egyptian population, only reported by 14.9% of family physicians and these results were far less than other studies in US by Shillinglaw et al.,[14] who reported that 41% physicians use CHD risk assessment in practice. Also the European study by Schmieder et al.,[16] a multinational, cross-sectional study in 12 European countries including Germany from May 2009 to January 2010 found that 54.5% German physicians reported routine use of global risk assessment tools to calculate CV risk in their patients. Also the European study by Graham et al., 2006 of the 220 respondents (155 primary care physicians, 65 cardiologists; most (85%) based assessment of CV risk on all risk factors, reflecting a global approach to risk, rather than considering risk factors individually. Less than half (48%) used guidelines or risk calculators to determine total risk. Also the results of the current study were inconsistent with the Australian study by Imms et al.,[17] a cross-sectional, postal, self-administered survey of general physicians in the General Practice South Division in southern Tasmania. This study was designed to investigate general practitioners’ knowledge of absolute risk estimation, and whether they used it to guide their management of CV disease found that CV risk calculator was used by (72%). The less reported use of CV risk assessment could be in light of the relative low awareness of guideline of global risk assessment, barriers related to physicians’ knowledge/training regarding topic and that fact that not all family medicine centers were supplied with standardized guidelines, risk scoring records, sufficient laboratory investigations, or equipped with networked internet to use calculators.
In the present study, the participants identified seven barriers; the most frequent reported barrier for CV risk assessment was deficient laboratory investigations within primary care settings by 90.8% of the participating physicians followed by poor skills/training of physicians and cost of the required investigations (81.5 and 80%, respectively). These results were consistent with a Dutch qualitative study by van Steenkiste et al.,[18] which identified 25 barriers related to the risk table application related general practitioner or environmental factors of which there is lack of knowledge. Also the Croatian study of Reiner et al.,[19] which reported that most physicians (general practitioners/family medicine specialists, internists, and cardiologists) considered lack of financial resources as the main barrier in use CVD prevention guidelines. Lack of knowledge also was reported by Schmieder et al.,[16] The present study found time consuming was the least reported barrier by physicians (32.3%). Other researches rely on time as main barrier.[14,16,20,21,22] System support could be the reason that explains the frequently reported barriers in this study as it could support the training of physician, dissemination of standardized guidelines, and ensure sufficient resources. Health policy as a barrier was reported by other researches.[20,22]
The current study showed that majority of participating physicians (87.7%) recommended training courses and 86.2% recommended providing physicians with standardized guidelines. This was in part similar to the study by Hobbs and Erhardt[21] that centered on more education, both for physicians themselves (29%) and patients (25%) promoting, publicizing, or increasing guideline availability (23%); simplifying the guidelines (17%) and making them clearer (12%). Also Graham et al.,[22] found that suggestions for improving implementation of guidelines included financial opportunities (24%), clear and easy to use guidelines (23%), and development of simpler guidelines (46%).
Limitations of the study
A number of limitations to the present study were recognized which include this data was self-reported. The sample size was small relative to other similar studies in spite of having comprehensive sample. We can not generalize our results on all family physicians as the study was on physicians under training within family medicine department.
Conclusion and Recommendations
Relatively higher attitude than use of global CV risk assessment tools but both were low. Training and resources including laboratory investigations and availability of guidelines were among the barriers of using global CV risk assessment related to the physicians. This calls for educational intervention and system support to implement and establish evidence based CV risk assessment to improve CV prevention in primary care.
Acknowledgments
The authors would like to thank all family physicians who accept to participate in this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.WHO. Cardiovascular diseases (CVDs), FACT sheet No. 317. [Last accessed on Mar 2013]. Available from: http://www.who.int/mediacentre/factsheets/fs317/en/index.html .
- 2.WHO. Noncommunicable diseases and mental health. Country profiles 2011, Egypt. [Last accessed on Mar 2013]. Available from: http://www.who.int/nmh/countries/egy_en.pdf .
- 3.Katić M, Juresa V, Bergman-Marković B, Jurković D, Predavec S, Hrastinski M, et al. Preventive work in family medicine – proactive approach. Acta Med Croatica. 2010;64:443–52. [PubMed] [Google Scholar]
- 4.Jackson R, Lawes CM, Bennett DA, Milne RJ, Rodgers A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual's absolute cardiovascular risk. Lancet. 2005;365:434–41. doi: 10.1016/S0140-6736(05)17833-7. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM. Cardiovascular risk prediction: Basic concepts, current status, and future directions. Circulation. 2010;121:1768–77. doi: 10.1161/CIRCULATIONAHA.109.849166. [DOI] [PubMed] [Google Scholar]
- 6.Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388–91. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 7.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:2748–64. doi: 10.1161/CIR.0b013e3182051bab. [DOI] [PubMed] [Google Scholar]
- 8.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR) Eur Heart J. 2012;33:1635–701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 9.WHO. Prevention of Cardiovascular Disease Pocket Guidelines for Assessment and Management of CVD Risk. [Last accessed on Mar 2013]. Available from http://www.who.int/cardiovascular_diseases/guidelines/PocketGL.ENGLISH.AFR-D-E.rev1.pdf .
- 10.WHO/ISH risk prediction charts for 14 WHO epidemiological sub-regions. [Last accessed Mar 2013]. Available from: http://ish-world.com/downloads/activities/colour_charts_24_Aug_07.pdf .
- 11.Cooney MT, Dudina A, D’Agostino R, Graham IM. Cardiovascular risk-estimation systems in primary prevention: Do they differ? Do they make a difference?. Can we see the future? Circulation. 2010;122:300–10. doi: 10.1161/CIRCULATIONAHA.109.852756. [DOI] [PubMed] [Google Scholar]
- 12.Brindle P, Beswick A, Fahey T, Ebrahim S. Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: A systematic review. Heart. 2006;92:1752–9. doi: 10.1136/hrt.2006.087932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doroodchi H, Abdolrasulnia M, Foster JA, Foster E, Turakhia MP, Skelding KA, et al. Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Fam Pract. 2008;9:42. doi: 10.1186/1471-2296-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shillinglaw B, Viera AJ, Edwards T, Simpson R, Sheridan SL. Use of global coronary heart disease risk assessment in practice: A cross-sectional survey of a sample of U.S. physicians. BMC Health Serv Res. 2012;12:20. doi: 10.1186/1472-6963-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torley D, Zwar N, Comino EJ, Harris M. GPs’ views of absolute cardiovascular risk and its role in primary prevention. Aust Fam Physician. 2005;34:503–4. 507. [PubMed] [Google Scholar]
- 16.Schmieder RE, Goebel M, Bramlage P. Barriers to cardiovascular risk prevention and management in Germany - an analysis of the EURIKA study. Vasc Health Risk Manag. 2012;8:177–86. doi: 10.2147/VHRM.S29915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Imms A, Quinn S, Nelson M. General practitioners’ use of cardiovascular risk calculators. Aust Fam Physician. 2010;39:57–60. [PubMed] [Google Scholar]
- 18.van Steenkiste B, van der Weijden T, Stoffers HE, Grol R. Barriers to implementing cardiovascular risk tables in routine general practice. Scand J Prim Health Care. 2004;22:32–7. doi: 10.1080/02813430310004489. [DOI] [PubMed] [Google Scholar]
- 19.Reiner Z, Sonicki Z, Tedeschi-Reiner E. Physicians’ perception, knowledge and awareness of cardiovascular risk factors and adherence to prevention guidelines: the PERCRO-DOC survey. Atherosclerosis. 2010;213:598–603. doi: 10.1016/j.atherosclerosis.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 20.Hobbs FD, Jukema JW, Da Silva PM, McCormack T, Catapano AL. Barriers to cardiovascular disease risk scoring and primary prevention in Europe. QJM. 2010;103:727–39. doi: 10.1093/qjmed/hcq122. [DOI] [PubMed] [Google Scholar]
- 21.Hobbs FD, Erhardt L. Acceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: The Reassessing European Attitudes about Cardiovascular Treatment (REACT) survey. Fam Pract. 2002;19:596–604. doi: 10.1093/fampra/19.6.596. [DOI] [PubMed] [Google Scholar]
- 22.Graham IM, Stewart M, Hertog MG. Cardiovascular Round Table Task Force. Factors impeding the implementation of cardiovascular prevention guidelines: Findings from a survey conducted by the European Society of Cardiology. Eur J Cardiovasc Prev Rehabil. 2006;13:839–45. doi: 10.1097/01.hjr.0000219112.02544.24. [DOI] [PubMed] [Google Scholar]


