Abstract
Xanthogranulomatous pyelonephritis (XGP) is rare and aggressive form of chronic infectious pyelonephritis. No single clinical or radiological feature is diagnostic of XGP. A 75-year-old man with prostatic enlargement presented with difficulty and burning micturition fever, abdominal and flank pain. X-ray, ultrasonography and computed tomography scan diagnosis was right kidney pyonephrosis. Intravenous urography revealed non-excretory right kidney. Right nephrectomy was done. Histological diagnosis of XGP was made. In all patients of prostatic enlargement, renal function must be assessed for the extent of damage. Surgery is the treatment choice in most cases. Pre- and post-operative antibiotics are key factors for successful management and better prognosis.
Keywords: Neprectomy, pyelonephritis, xanthogranulomatous pyelonephritis
Introduction
Xanthogranulomatous pyelonephritis (XGP) is a rare, distinct and aggressive form of chronic infectious pyelonephritis. Schlagenhaufer described it first in 1916 and Osterlin in 1944, called it xanthogranuloma. It accounts for lesser than 1% of chronic pyelonephritis. Though common in fifth to sixth decade, it can occur at any age. Women are more frequently affected than men.[1] Urinary obstruction is almost invariably present, most often caused by renal stones.[2] Complications can occur in the form of psoas abscess, nephro cutaneous fistula, enterocolonic fistula, paranephric abscess and sepsis. Treatment involves antibiotics and surgery in most cases.[3] It is essential to suspect and diagnose this condition early to prevent the morbidity and mortality. Owing to its rarity and clinical curiosity; we report this case of XGP with unusual presentation.
Case Report
A 75-year-old man presented with difficulty in micturition since 15 days, fever, abdominal and flank pain and burning micturition since 7 days. He gave a history of recurrent urinary tract infection. There was no other significant medical history. After through clinical examination diagnosis of benign prostatic hyperplasia (BPH) was made. He had no history of diabetes and hypertension. Amongst laboratory findings, blood urea nitrogen (BUN) and serum creatinine was raised viz. 42 mg/dl and 1.7 mg/dl respectively. Erythrocyte sedimentation rate was 22 mm/1h. Urine microscopy showed numerous pus cells. Urine culture was positive for Escherichia coli. Rest of the haematology and biochemical parameters were within the normal limits.
X-ray, ultrasonography (USG) and computed tomography (CT) scan abdomen findings include pyonephrosis and cortical atrophy in the right kidney. Intravenous urography (IVU) revealed non-excretory right kidney. Left kidney showed normal excretion. No renal calculi were seen. Patient underwent right nephrectomy. Pre- and post-operative broad spectrum antibiotics were given. Resected specimen was yellowish lobulated renal mass measuring 13 × 8 × 6 cm with ureter [Figure 1a]. Cut section showed dilated pelvis, calyces and cortical atrophy due to extensive destruction of renal parenchyma, which were covered with thick purulent material [Figure 1b]. Histopathology revealed atrophic and dilated renal tubules showing thyroidisation and sclerosed glomeruli and interstitial fibrosis [Figure 2]. Giant cells and cholesterol clefts were seen [Figure 2 Inset]. Many areas showed histiocytes with abundant foamy cytoplasm, lymphoplasmacytic inflammatory cells with foci of polymorph nuclear leukocytes [Figure 3 and Inset] Ziehl Nelsen stain was negative for acid fast bacilli. No perodic acid schiff positivity was seen in the cytoplasm.
Figure 1.
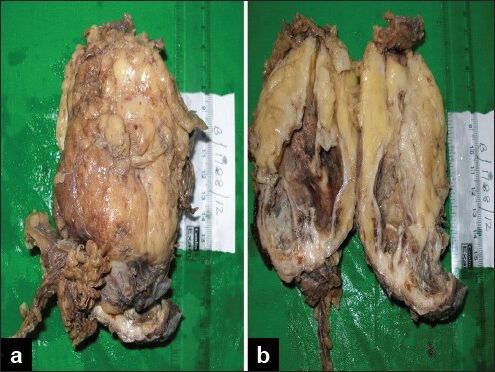
(a) Yellowish lobulated renal mass with ureter; (b) dilated pelvis, calyces and cortical atrophy covered with thick purulent material
Figure 2.
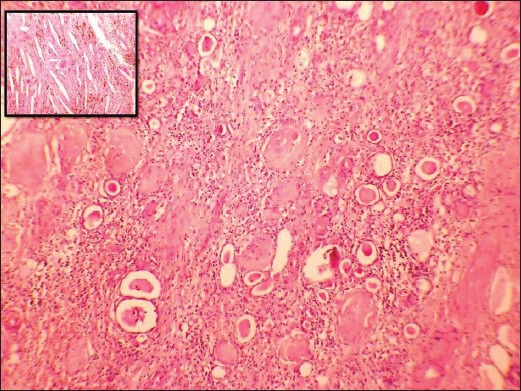
Atrophic and dilated renal tubules showing thyroidisation, sclerosed glomeruli and fibrosis. Inset show giant cells and cholesterol clefts (H and E, ×400)
Figure 3.
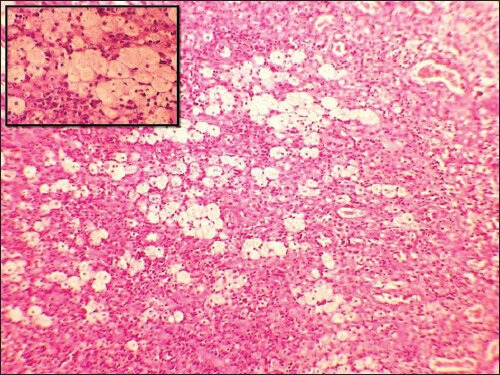
Foamy histiocytes, inflammatory cells. Inset show foamy cytoplasm of histiocytes (H and E, ×400)
Discussion
XGP is a severe chronic renal inflammatory condition leading to focal or diffuse kidney destruction. If uncontrolled, it spreads to adjacent tissues and destroys it.[4] It may be due to defect in degradation of bacteria in the macrophages especially when associated with infection and obstruction by stones. Three forms of XGP are recognised: Diffuse — is characterized by diffuse involvement of kidney, segmental — by segmental involvement and focal - is located within the cortex. No clinical or radiologic features are diagnostic of XGP. It is often misdiagnosed pre-operatively as pyelonephritis, tuberculosis, perinephric abscess and renal cell carcinoma (RCC).[5,6,7] Symptoms include flank or abdominal pain, fever, palpable mass, gross hematuria, pyuria, dysuria and weight loss.[7] In our case, symptoms were attributed to BPH.
The most common organisms found in urine culture are E. coli and Proteus mirabilis. Other organisms include Staphylococcus aureus, Group B Streptococcus, Candida, Klebsiella and Bacteroides.[2,6] Elevation of serum creatinine and BUN in our case can be attributed to impaired renal function.
Abdominal X-ray and USG shows usually renal stones.[8] Renal stones were absent in our case.
IVU is a reliable method of determining the renal function. Diffuse XGP show non-excretory kidney viz. non-functioning,[7] CT scan is the main stay of diagnostic imaging for XGP.[6,7,9] Fine-needle aspiration cytology plays an insignificant role in diagnosing XGP.[1] Malek and Elder[10] proposed three stages of XGP. Stage I lesion is confined to renal parenchyma. Stage II lesion involves perirenal space. Stage III involves perirenal and pararenal space. Our case was Stage II.
Pre-operative renal biopsy diagnosis of XGP is often challenging in focal lesions.
Several deaths have been reported directly from XGP due to post-operative sepsis.[6] XGP has been shown to be associated with transitional cell carcinoma of renal pelvis and RCC. They have even been reported in renal allograph.[9]
In diffuse or advanced stage XGP, nephrectomy is the treatment option. Focal or segmental XGP if diagnosed early pre-operatively can be treated with antibiotics. Pre- and post-operative broad spectrum antibiotics and symptomatic management are also key factors for successful management and better prognosis.[9] No post-operative complications occurred in our patient.
We presented this unusual case of elderly male to stress the importance of through evaluation of renal function who gave a history of recurrent urinary tract obstruction and infection.
Conclusion
Chronic renal infection and obstruction are two common etiological factors for XGP. In all patients of prostatic enlargement, renal function must be assessed for the extent of damage. In non-functioning kidney, XGP shall be suspected.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Li L, Parwani AV. Xanthogranulomatous pyelonephritis. Arch Pathol Lab Med. 2011;135:671–4. doi: 10.5858/2009-0769-RSR.1. [DOI] [PubMed] [Google Scholar]
- 2.Rosai J. Missouri: Elsevier; 2004. Surgical Pathology; p. 1227. [Google Scholar]
- 3.Tsai KH, Lai MY, Shen SH, Yang AH, Su NW, Ng YY. Bilateral xanthogranulomatous pyelonephritis. J Chin Med Assoc. 2008;71:310–4. doi: 10.1016/S1726-4901(08)70128-X. [DOI] [PubMed] [Google Scholar]
- 4.Shah KJ, Ganpule AP, Kurien A, Muthu V, Sabnis RB, Desai MR. Laparoscopic versus open nephrectomy for xanthogranulomatous pyelonephritis: An outcome analysis. Indian J Urol. 2011;27:470–4. doi: 10.4103/0970-1591.91434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leoni FA, Kinleiner P, Revol M, Zaya A, Odicio A. Xanthogranulomatous pyelonephritis: Review of 10 cases. Arch Esp Urol. 2009;62:259–71. doi: 10.4321/s0004-06142009000400001. [DOI] [PubMed] [Google Scholar]
- 6.Korkes F, Favoretto RL, Bróglio M, Silva CA, Castro MG, Perez MD. Xanthogranulomatous pyelonephritis: Clinical experience with 41 cases. Urology. 2008;71:178–80. doi: 10.1016/j.urology.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 7.Loffroy R, Guiu B, Watfa J, Michel F, Cercueil JP, Krausé D. Xanthogranulomatous pyelonephritis in adults: Clinical and radiological findings in diffuse and focal forms. Clin Radiol. 2007;62:884–90. doi: 10.1016/j.crad.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Craig WD, Wagner BJ, Travis MD. Pyelonephritis: Radiologic-pathologic review. Radiographics. 2008;28:255–77. doi: 10.1148/rg.281075171. [DOI] [PubMed] [Google Scholar]
- 9.Dwivedi US, Goyal NK, Saxena V, Acharya RL, Trivedi S, Singh PB, et al. Xanthogranulomatous pyelonephritis: Our experience with review of published reports. ANZ J Surg. 2006;76:1007–9. doi: 10.1111/j.1445-2197.2006.03919.x. [DOI] [PubMed] [Google Scholar]
- 10.Malek RS, Elder JS. Xanthogranulomatous pyelonephritis: A critical analysis of 26 cases and of the literature. J Urol. 1978;119:589–93. doi: 10.1016/s0022-5347(17)57559-x. [DOI] [PubMed] [Google Scholar]


