Abstract
Background
The developmental need to fit in may lead to higher alcohol and other drug use among socially anxious youths which exacerbates the drink/trouble cycle. In treatment, youths with social anxiety disorder (SAD) may avoid participating in therapeutic activities with risk of negative peer appraisal. Peer-helping is a low-intensity, social activity in the 12-step program associated with greater abstinence among treatment-seeking adults. This study examined the influence of SAD on clinical severity at intake, peer-helping during treatment, and outcomes in a large sample of adolescents court-referred to residential treatment.
Methods
Adolescents (N = 195; 52% female, 30% Black) aged 14 to 18 were prospectively assessed at treatment admission, treatment discharge, and 6 months after treatment discharge. Data were collected using rater-administered assessments, youth reports, clinician reports, medical charts, and electronic court records. The influence of SAD on peer-helping and outcomes was examined using hierarchical linear regression and event history methods.
Results
Forty-two percent of youths reported a persistent fear of being humiliated or scrutinized in social situations, and 15% met current diagnostic criteria for SAD. SAD onset preceded initial use for two-thirds of youths with SAD and substance dependency. SAD youths presented for treatment with greater clinical severity in terms of earlier age of first use (p < 0.01), greater lifetime use of heroin and polysubstance use (p < 0.05), incarceration history (p < 0.01), and lifetime trauma (p < 0.001). Twelve-step participation patterns during treatment did not differ between youths with and without SAD except for peer-helping, which was associated with reduced risk of relapse (p < 0.01) and incarceration (p < 0.05) in the 6 months posttreatment.
Conclusions
This study found evidence of an association between SAD and earlier age of first use, greater lifetime use of heroin, incarceration history, and lifetime trauma. SAD was associated with higher service participation during treatment, which was associated with reduced risk of relapse and incarceration in the 6 months posttreatment. Findings indicate the benefits of service participation for juveniles with SAD which provides a nonjudgmental, task-focused venue for developing sober networks in the transition back into the community.
Keywords: Alcohol Use, Adolescents, Service, Alcoholics Anonymous, Social Anxiety, Longitudinal
THE 21ST CENTURY has witnessed a dramatic increase in addiction among U.S. youth, with similar rates of alcohol and other drug (AOD)-use disorders among both boys and girls (Mulye et al., 2009). The recent legalization of marijuana in several states, the plethora of prescription medications, and harder street drugs including methamphetamines gives youths the greatest access to controlled substances than our nation has seen since the initiation of the “War on Drugs” (Hurley and Mazor, 2013). In response, research targeting adolescent AOD use specifically has developed sophisticated tools to determine causal factors and effects of this epidemic. Adolescent AOD use curtails brain development and scholastic achievements; increases incidence and spread of infectious disease; potentiates the danger of risky sex, teenage pregnancy, school dropout, and criminal activity; and shortens life-course trajectories with associated medical comorbidities (Guerri and Pascual, 2010). The rising cost of AOD problems is estimated at $500 billion in increased criminal activity, higher healthcare costs, and lost productivity.
Social instincts and developmental tasks during adolescence can intersect in ways that increase risk of AOD-use disorders. The need to fit in, the prominence of peers, establishing an identity independent of parents, and the tendency for drinking to organize social activities are forefront in this developmental stage (National Institute on Drug Abuse, 2014). Symptoms of social anxiety disorder (SAD) emerge well before adolescents begin experimenting with AOD use. SAD is 5 times more likely to precede AOD-use disorders and the most common co-occurring anxiety disorder with AOD-use disorders (Buckner et al., 2008; Zimmer-man et al., 2003). The types of situations feared usually involve interacting with others, such as socializing at a party, performing in front of others, or speaking to a group (Randall et al., 2001). Socially anxious youths soon discover that AOD use can diminish their discomfort (Robinson et al., 2011; Terra et al., 2006); this self-medicating response can develop into addiction and set in motion a drink/trouble, drink/trouble cycle that may require treatment to interrupt. Young adults in correctional facilities well describe the drink/trouble, drink/trouble cycle: “We saw how often we got into trouble while drinking. Over and over, our troubles had some hookup with drinking” (Alcoholics Anonymous [AA], 2000).
Addiction treatment approaches for adolescents are frequently delivered in groups and behavioral in nature, as addiction medications have not been approved for use with minors. The majority of treatment programs encourage patients to attend AA, and the 12-step model is the prevailing therapeutic approach for treating substance abuse in the United States. Meta-analytic reviews of 12-step research show a modest benefit of 12-step participation on reduced AOD use (Forcehimes and Tonigan, 2008). Most active ingredients accounting for AA’s benefit are social in nature, such as attending meetings, and the 12 steps mention “we” 6 times but not “I” once.
The social platform of formal treatment and AA, however, may pose a challenge to socially anxious patients who no longer have alcohol or drugs to mitigate their discomfort. Treatment-seeking adults with social anxiety are less likely to speak up in group therapy, talk to their therapist, or participate in treatment activities involving public speaking (Book et al., 2009). Social anxiety can also interfere with participation in 12-step activities. For example, adults with SAD report not feeling as good after a meeting as those without SAD and are less likely to chair a meeting, and women with SAD are less likely to ask someone to sponsor them (Terra et al., 2006; Tonigan et al., 2010). The daunting reality is that 60 to 90% of patients relapse in the initial 6 months posttreatment (Miller et al., 2001), and the lifelong illness of addiction requires ongoing recovery supports. Addiction treatment usually does not assess for nor treat SAD specifically, SAD is nonremitting without treatment for this condition (Bruce et al., 2005), and patients with SAD are more likely to relapse after treatment if SAD is left untreated during addiction treatment (Kushner et al., 2005). Finding non-judgmental venues for social connectedness and personal growth is important to help socially anxious patients stay engaged in treatment and benefit from active participation.
Peer Helping
Service is a programmatic component of the 12-step program that is associated with greater abstinence (Pagano et al., 2004, 2013b), reduced symptoms of depression and negative self-appraisal (Pagano et al., 2007, 2009), and increased social involvement (Pagano et al., 2013a). The benefits from helping others appear to be greatest for individuals who are socially isolated (Piliavin, 2005), and patients with SAD are prone to withdraw from others to avoid negative appraisal. Midlarsky (1991) proposed that helping others may benefit the helper because it distracts one from one’s own troubles, enhances a sense of value in one’s life, improves self-evaluations, increases positive moods, and causes social integration. However, the cofounders of AA incorporated service into the 12-step program primarily to correct self-absorbed thinking posited as a root cause of addiction. The myriad of existing service activities in AA are readily available inside and outside of meetings; are low-intensity; and do not require special skills, prior experience, time sober, long-term commitment, transportation, insurance, or parental permission. Peer-helping in AA, such as having the responsibility of making coffee at a meeting, empathetic listening to others, reading inspirational meditations to others, or sharing personal experiences in learning to live sober, may have the effect of greater engagement in treatment and improved outcomes due to patients’ active contributions. Given the extreme self-consciousness in social situations that characterizes SAD and the applicability of prosocial behaviors enhancing youth development, the limited data on youth participation patterns in peer-helping and effectiveness, particularly with socially anxious patients, are surprising. Many 12-step investigations consider the effects of getting but rarely giving support on improved outcomes, most addiction studies usually do not assess SAD specifically, and SAD studies tend to exclude participants with AOD-use disorders. Given the priority of peer-evaluations during adolescence and high sensitivity to deprecatory judgments—the hallmark of SAD—peer-helping may be particularly relevant to adolescents learning to live sober with and without SAD.
This study sought to extend prior research by evaluating effects of SAD on clinical presentation at intake, 12-step engagement patterns during treatment, and treatment outcomes in a large sample of high-risk minors (52% female, 30% minority) court-referred to residential treatment. We hypothesized that SAD youths would present with greater clinical impairment at intake than youths without SAD. Because SAD has been associated with lower meeting attendance and rates of having a sponsor among treatment-seeking adults (Tonigan et al., 2010), we hypothesized that SAD would be associated with lower meeting attendance and obtaining a sponsor during treatment. Because many forms of service involve low risk of public scrutiny (i.e., putting away chairs) and the evidence of improved outcomes associated with helping others during treatment (Pagano et al., 2013b), we hypothesized that SAD would be associated with peer-helping during treatment, which would increase the chances of SAD youths staying sober and out of jail in the high-risk, initial 6 months following discharge.
MATERIALS AND METHODS
Participants
Participants were 195 youths aged 14 to 18 years entering residential treatment at a large adolescent treatment facility in the northeastern United States. Approximately half were male (48%), from a rural or small town residence (53%) and living with a single parent (50%). The majority of participants entered residential treatment meeting current DSM-IV diagnostic criteria for marijuana dependency (92%) and comorbid alcohol dependency (61%), as reported in detail elsewhere (Kelly et al., 2011). Similar to other adolescent treatment research (Hall et al., 2010), approximately half (46%) misused prescription drugs on 10 or more occasions (Table 1).
Table 1.
Sample at Intake
| Intake characteristic | Total 195 (100%) | No SAD 165 (85%) | SADa 30 (15%) |
|---|---|---|---|
| Background | |||
| Age (M, SD) | 16.2 (1.1) | 16.1 (1.0) | 16.5 (1.2) |
| Male (%) | 93 (48) | 88 (53) | 5 (17)*** |
| Minority (%) | 59 (30) | 52 (27) | 7 (23) |
| Rural/small town (%) | 103 (53) | 84 (51) | 19 (63) |
| Single parent (%) | 98 (50) | 80 (48) | 18 (60) |
| Parent GED or less (%) | 142 (73) | 118 (72) | 24 (80) |
| Lifetime trauma (M, SD) | 1.7 (1.5) | 1.5 (1.5) | 2.7 (1.1)*** |
| Prior treatment (%) | 17 (9) | 12 (7) | 5 (17) |
| Alcohol/drugb | |||
| Alcohol (%) | 172 (88) | 146 (88) | 62 (87) |
| Marijuana (%) | 192 (98) | 164 (99) | 28 (93) |
| Heroin (%) | 101 (52) | 82 (50) | 19 (63)* |
| Ecstasy (%) | 99 (50) | 81 (49) | 18 (61) |
| Prescription drugs (%) | 90 (46) | 73 (44) | 17 (57) |
| Methamphetamine (%) | 80 (41) | 65 (39) | 15 (50) |
| Cocainea (%) | 79 (41) | 66 (40) | 13 (43) |
| Inhalants (%) | 49 (25) | 40 (24) | 9 (30) |
| Polysubstance (%) | 99 (50) | 79 (48) | 20 (67)* |
| Age of first use (M, SD) | 12.9 (1.7) | 13.0 (1.6) | 12.1 (1.8)** |
| Outcomes at intake | |||
| Percent days abstinentc (M, SD) | 0.4 (0.9) | 0.4 (0.3) | 0.3 (0.4) |
| Global functioning (M, SD) | 49.5 (2.7) | 49.5 (2.7) | 49.6 (2.4) |
| Incarceration historyd (%) | 18 (9) | 12 (7) | 6 (20)* |
| 12-step | |||
| Peer-helping (M, SD) | 26.2 (10.5) | 26.1 (10.3) | 26.5 (11.4) |
| Meeting attendance (M, SD) | 4.7 (11.7) | 4.5 (11.1) | 6.3 (12.4) |
| Has sponsor (%) | 10 (5) | 8 (5) | 2 (7) |
SAD, social anxiety disorder.
10+ lifetime uses.
Past 30 days.
Past 12 months.
p < 0.05,
p < 0.01,
p < 0.001.
Procedures
Recruitment for this study was conducted from February 2007 to August 2009. Inclusion criteria included the following: ages 14 to 18 years, English speaking, stable address and telephone, met diagnostic criteria (American Psychiatric Association, 2000) for current AOD dependency, not currently suicidal/homicidal, and medical clearance verifying the absence of acute withdrawal symptoms. Subjects were referred to treatment from multiple sources, including juvenile court (83%), mental health professionals (65%), and non-psychiatric physicians (2%). In the week before admission date, participants were sent an information packet with an invitation letter to participate in the study. Following the admission interview with clinical staff, participants were approached by research staff and given a brief description of the study. Eligible participants signed statements of informed consent/assent and were scheduled for a baseline interview. Research staff did not inform clinical staff of any research data and did not provide treatment services. Patients spent approximately 20 hours per week in therapeutic activities and attended at least three 12-step meetings each week of the 8-week residential treatment program. Patients were eligible to go on pass after their initial week in treatment, and clinicians collected urine toxicology screens upon their return as part of treatment procedures. Participants were paid $25 for completed assessments at each study interval (intake, discharge, and 6 months postdischarge).
Of the 211 patients approached, none were ineligible and 16 refused to participate, resulting in an enrollment sample of 195 subjects. There were no significant differences between youths enrolled versus not enrolled but treated during the enrollment period in terms of intake characteristics and rates of treatment completion, as reported in detail elsewhere (Kelly et al., 2011). Ninety-six percent of the sample completed a discharge interview, with no significant differences at intake between participants with (N = 185, 96%) and without a discharge interview (N = 8, 4%). Eight percent (N = 16) of the enrollment sample were incarcerated at the time of their 6-month interview and were thus unable to be interviewed. Of those eligible for scheduling of their 6-month interview (N = 179), 87% (N = 156) completed a 6-month interview. There were no significant differences between participants with and without a 6-month interview in terms of intake characteristics, treatment completion, or treatment duration (Table 2). All study procedures were approved by the Case Medical Center Institutional Review Board for human investigation, and a Certificate of Confidentiality from the National Institute on Alcohol Abuse and Alcoholism was obtained. All individuals collecting data from subjects completed the Collaborative Institutional Training Initiative required courses for responsible conduct of research. Further details regarding study design, sample and assessment procedures are provided elsewhere (Kelly et al., 2011).
Table 2.
Sample Attrition Analyses
| Intake characteristic | Total 195 (100%) | Data present 156 (80%) | Lost to f/u 21(11%) | Jail 16 (8%) | Refused 2 (1%) |
|---|---|---|---|---|---|
| Background | |||||
| Age (M, SD) | 16.2 (1.1) | 16.2 (1.1) | 16.1 (1.1) | 16.2 (1.1) | 16.0 (1.4) |
| Female (%) | 102 (52) | 86 (55) | 8 (28) | 7 (44) | 1 (50) |
| Minority (%) | 59 (30) | 45 (29) | 6 (29) | 8 (50) | 0 (0) |
| Rural/small town (%) | 103 (53) | 82 (33) | 8 (50) | 11 (52) | 2 (100) |
| Single parent (%) | 98 (50) | 81 (51) | 10 (48) | 7 (44) | 0 (0) |
| Parent GED or less (%) | 142 (73) | 116 (74) | 16 (76) | 9 (56) | 1 (50) |
| Global functioning (M, SD) | 49.6 (2.7) | 49.4 (2.8) | 50.0 (1.9) | 49.3 (2.4) | 50.0 (2.8) |
| Lifetime trauma (M, SD) | 1.7 (1.5) | 1.8 (1.5) | 1.3 (1.6) | 1.6 (1.5) | 2.5 (0.7) |
| Prior treatmentb (%) | 17 (9) | 13 (8) | 2 (13) | 2 (10) | 0 (0) |
| 12-step | |||||
| Peer-helping (M, SD) | 26.2 (10.5) | 25.6 (10.4) | 24.8 (11.8) | 32.6 (7.7) | 27.5 (2.1) |
| Meeting attendance (M, SD) | 8.2 (15.0) | 7.8 (14.3) | 7.8 (14.9) | 9.9 (12.4) | 7.0 (9.9) |
| Has sponsor (%) | 16 (8) | 11 (7) | 2 (10) | 3 (19) | 0 (0) |
| Alcohol/drug | |||||
| Age of first use (M, SD) | 12.9 (1.7) | 12.8 (1.6) | 13.0 (1.7) | 12.4 (2.3) | 12.5 (1.0) |
| Outcomes at intake | |||||
| Percent days abstinenta (M, SD) | 0.4 (0.4) | 0.4 (0.4) | 0.3 (0.4) | 0.4 (0.4) | 0.5 (0.3) |
| Global functioning (M, SD) | 49.5 (2.7) | 49.3 (2.8) | 48.5 (2.2) | 49.8 (2.5) | 48.9 (2.6) |
| Incarceration historyb (%) | 18 (9) | 17 (9) | 1 (1) | 0 (0) | 0 (0) |
| Discharge status | |||||
| Treatment completion (%) | 173 (89) | 141 (93) | 19 (90) | 11 (69) | 2 (100) |
| Treatment duration (weeks) (M, SD) | 10.2 (1.1) | 10.4 (0.2) | 10.1 (0.5) | 9.4 (0.6) | 11.0 (1.7) |
f/u, follow-up.
Past 30 days.
Past 12 months.
Measures
Data were gathered via rater-administered interviews, youth reports, clinician reports, medical chart review, and electronic court records. Participants completed a semi-structured interview in a private location with a research assistant at 3 time points: at baseline in the week following the admissions interview (M = 7.0 days, range 0 to 10 days), at discharge, and at 6 months after the date of discharge. Semi-structured interviews were conducted in person by experienced clinical interviewers whose training ranged from BA to MD. Training of interviewers included didactic tutorials, mock interviews and role-playing, and supervised interviews with detailed feedback provided by the Principal Investigator.
Background
Background characteristics associated with outcomes in prior work (Pagano et al., 2004) were assessed at intake: age, gender, minority status, urbanicity of residence, parental marital status, parental education, lifetime trauma, treatment history, and lifetime Axis I disorders. Urbanicity of residence was assessed using the zip code approximation version of the census tract-based rural–urban commuting area codes (available at http://depts.washington.edu/uwruca/ruca-data.php). Lifetime trauma was assessed with the 4-item Traumatic Experiences scale adapted from the valid Massachusetts Youth Screening Inventory (Grisso and Barnum, 2000), which showed good internal consistency in the current sample (α = 0.86). Treatment history (inpatient, outpatient, residential, and detoxification episodes) in the prior 24 months was assessed with the Health Care Data Form (Larson et al., 1997). The valid, rater-administered MINI-International Neuropsychiatric Interview (Arnaud et al., 2010; Sheehan et al., 1998) was used to assess DSM-IV-TR lifetime anxiety disorders (American Psychiatric Association, 2000). Participants who endorsed criteria for generalized SAD (lifetime) or in the last 6 months (current) were considered positive for SAD diagnosis (N = 30, 15%). Few SAD youths met diagnostic criteria for another concurrent anxiety disorder (6% agoraphobia, 4% generalized anxiety, 4% panic, and 1% posttraumatic stress) or concurrent major depression (11%). Concurrent Axis I disorders onset an average of 2 years (M = 2.4, SD = 1.6) after SAD onset, as described elsewhere (Carruthers et al., 2012; Wang et al., 2013). All participants received an initial diagnostic evaluation by the medical director board-certified in child psychiatry as part of the admissions interview. Diagnostic agreement with clinician assessment of SAD was high (κ = 0.99).
Lifetime AOD Use
Eight items from the Youth Risk Behavior Survey (YRBS; Kann et al., 2000) were collected at intake and indexed participant lifetime use of alcohol, cocaine, inhalants, heroin, methamphetamines, ecstasy, prescription medications without a doctor’s prescription, and marijuana. Each YRBS item was rated from 1 (0 use), 2 (1 to 2 uses), 3 (3 to 9 uses), 4 (10 to 19 uses), 5 (20 to 39 uses) to 6 (40+ uses), and age of first use was recorded. Using a threshold adopted by Hall and colleagues (2010) for comparability, high AOD users were participants with 10 or more lifetime uses of a particular substance. YRBS items showed high internal consistency (α = 0.92 to 0.93).
12-Step Participation
Participants reported their participation in the 12-step program at intake (past 90 days) and at discharge (days in treatment) in 3 programmatic activities: peer-helping, meeting attendance, and having a sponsor. Peer-helping was assessed with the Service to Others in Sobriety (SOS) questionnaire (Pagano et al., 2013b), a 12-item self-report of service participation that is performed at and outside of 12-step meetings. Nine items assess forms of help given on a one-to-one basis or to several alcoholics/ addicts. Only 1 item has a potential risk of public scrutiny if it is given at a podium (i.e., shared personal story with another alcoholic/addict). Three items involve instrumental tasks in group contexts, but can executed with no or minimal social interaction (i.e., held service position; put away chairs after the meeting; donated money to AA). Items are rated on a Likert scale from 1 (rarely) to 5 (always) and summed to form a unidimensional scale ranging from 12 to 60; a cutoff score of 40 indicates high peer-helping. The SOS showed good psychometric properties with adults and the current sample, and was significantly correlated (r = 0.5) with clinician report of youth peer-helping on the SOS (Pagano et al., 2013b). After completing the SOS, participants rated 2 additional items with reference to the assessment period: “how many meetings did you attend?” and “did you have a sponsor?” Intracorrelations between 12-step indices were low to moderate at intake (rs = 0.2 to 0.4, p < 0.01) and discharge (rs = 0.2 to 0.3, p < 0.01).
Outcomes
AOD use and psychosocial functioning were outcomes collected at intake, discharge, and 6 months posttreatment. AOD use was assessed with the valid and reliable Timeline Follow-Back interview (TLFB). Following the TLFB administration manual (Sobell and Sobell, 1996), the interviewer used a calendar grid and memory anchor points to aid participant recall of daily drinking and/or drug use. Data on alcohol use were collected on the first pass through the calendar, followed by use of 7 drug types (cannabis, cocaine, hallucinogens, sedatives/hypnotics, narcotics, stimulants, and inhalants). Percentage of days abstinent (PDA) was calculated as the number of days a subject was abstinent from AOD divided by the number of days in the assessment period multiplied by 100. PDA scores showed high agreement with testing positive for AOD use during the treatment period (κ = 0.87). Time to first AOD use after the nominal end of treatment, a primary time-to-event outcome measure in Project MATCH (Babor et al., 2003), was considered a relapse in this study.
Psychosocial indices included the global functioning and incarceration incidences. The clinician-rated Children’s Global Assessment Scale (Shaffer et al., 1983) assessed the worst psychosocial functioning week in prior month across home, school, and with peers, with scores ranging from 1 to 100. Incarceration incidences were assessed from electronic legal records maintained by 17 referring municipal court counties in northeast Ohio that were made available for this study. Because youths as young as 16 years could be charged as adults, adult criminal records were also collected across referring municipal court counties. In accordance with Ohio Revised Code (3321.19) and the Ohio Incident-Based Reporting System (see ocjs.ohio.gov/oibrs), county booking databases documented the start/end dates of jail episodes, and whether incidences were AOD-related (yes/no). Participants were matched to booking databases on last name, first name, gender, and date of birth. Incarceration episodes with start dates occurring within the 12 months prior to date of admission and within the 6 months following the date of discharge were recoded and reviewed by an experienced peer interviewer for completeness and accuracy. Court records have shown high correlation with self-report of legal involvement (Moffitt et al., 1996). Jail incidences showed high correlation with youth report of legal involvement on the Substance Abuse Subtle Screening Inventory at intake (r = 0.5, p < 0.001). Intracorrelations between outcomes (AOD use, psychosocial functioning) collected at intake, discharge, and 6 months posttreatment were low (rs = −0.1 to 0.2, ns).
Statistical Analysis
Statistical analyses were performed with SAS Version 9.2 (SAS Institute Inc., 2008). Distributions of variables were first examined for normality; positively skewed distributions were given a logarithmic transformation and negatively skewed variables received an arcsine transformation, as was done in the primary MATCH outcome analyses (Project MATCH Research Group, 1993). Fisher’s exact test for categorical variables and Mann–Whitney U-test for continuous variables were used to test for differences between groups. Nonparametric t-tests and Cochran’s Q tests were used to examine changes at discharge from intake. Main effects of SAD on 12-step participation during treatment, treatment completion, and outcomes at discharge were tested in random effects regression models using PROC GENMOD for binary variables and PROC MIXED for continuous variables; model covariates included background variables, pretreatment 12-step participation (meeting attendance, having a sponsor, AA-related helping [AAH]), and the dependent variable at intake. Main effects of SAD on likelihood of relapse posttreatment were tested using event history methods (survival analysis, Cox proportional hazard regression); main effects of SAD on likelihood of incarceration were tested using a negative binomial logistic regression with a robust variance correction for overdispersion. For prospective (lagged) hypothesis testing of mediational effects of peer-helping, main effects of SAD, peer-helping (high/low) during treatment, and a SAD × peer-helping interaction term were used to predict 6-month outcomes, controlling for background variables, other 12-step activity during treatment (meeting attendance, having a sponsor), treatment duration, and the dependent variable at intake. Mediational effects of peer-helping were analyzed using the test of joint significance method of MacKinnon and colleagues (2002); both the path between SAD and mediator (peer-helping), and the path from the peer-helping mediator to the 6-month outcome need to be significant to support mediation. Preliminary analyses suggested that linear modeling was adequate. Examination of the correlation matrix for independent variables in analytic models found no correlation to exceed 0.3 and collinearity diagnostics indicated no problems. Tests for violations of the proportional hazard assumption found no evidence of nonproportionality in the Cox regression model. For the purposes of interpretation, Cohen (1988) considers r = 0.10 “small,” r = 0.30 “medium,” and r = 0.50 “large.” We reported all 2-tailed tests with significance values greater than 95% (p < 0.05).
RESULTS
Intake
Forty-two percent of the sample reported a persistent fear of being humiliated or scrutinized in social situations, and 15% met current diagnostic criteria for SAD (12% current only, 3% current and lifetime, 0% lifetime only). There were no gender differences in persistent fear of scrutiny by others, although SAD was more prevalent among girls (54%) than boys (42%; χ2 = 13.6, p < 0.001). SAD was associated with greater incarceration history, lifetime use of heroin, polysub-stance use, and earlier age of first use (Table 1). SAD onset before initial AOD use for most SAD youths (67%) at the average age of 11.2 years (SD = 3.1). Excluding concurrent onsets (17%), the null hypothesis of half of SAD onsets occurring prior to and following initial AOD use was rejected (z = 3.0, p < 0.01).
Discharge
The majority of the sample (89%) completed the 2-month treatment period (M = 10.2 weeks, SD = 1.1). Participants overall showed significant improvements in PDA (t = −23.6, p < 0.001), although only half (50%) were abstinent throughout the treatment period. Twelve-step participation significantly improved in terms of increased meeting attendance (t = −15.7, p < 0.001), peer-helping (t = −7.8, p < 0.001), and the proportion having a sponsor at discharge (23%; Q = 8.1, p < 0.001). At discharge, there were no differences between youths with or without SAD in terms of treatment completion or duration, PDA, global functioning, meeting attendance, and having a sponsor (Table 3). However, SAD was significantly associated with higher levels of peer-helping and scoring above threshold for high helping (43% SAD vs. 30% no SAD; χ2 = 4.5, p < 0.05). The top 2 peer-helping activities that were rated “often” or “always” by SAD youths were putting away chairs after a meeting (80%) and guiding another with step-work (75%). In comparison, peer-helping activities rated “often” or “always” the most by youths without SAD were sharing one’s personal story with another alcoholic (70%) and reading introductory/closing literature at a meeting (65%). Twelve-step participation patterns among SAD youths did not differ by gender.
Table 3.
Sample at Discharge
| Discharge characteristic | Total 195 (100%) | No SAD 165 (85%) | SAD 30 (15%) |
|---|---|---|---|
| Discharge status | |||
| Treatment completion (%) | 173 (89) | 147 (89) | 26 (87) |
| Transferred (%) | 13 (7) | 12 (7) | 1 (3) |
| Premature discharge (%) | 9 (5) | 6 (4) | 3 (10) |
| Treatment duration (weeks) (M, SD) | 10.2 (1.1) | 10.1 (1.0) | 10.9 (1.2) |
| Outcomes | |||
| Percent days abstinenta (M, SD) | 0.7 (0.1) | 0.7 (0.1) | 0.8 (0.2) |
| Global functioning (M, SD) | 60.9 (4.3) | 61.5 (4.0) | 60.8 (4.2) |
| 12-stepa | |||
| Peer-helping (M, SD) | 36.7 (1.3) | 36.6 (1.1) | 40.1 (2.0)* |
| Meeting attendance (M, SD) | 31.9 (3.7) | 31.8 (3.2) | 31.9 (4.3) |
| Has sponsor (%) | 42 (23) | 33 (21) | 9 (30) |
SAD, social anxiety disorder.
N = 185.
p < 0.05.
Analytic models controlled for age, gender, race, urbanicity of residence, parental education and marital status, lifetime trauma, and treatment history.
Six Months Post Treatment
Approximately half (56%) of the 16 youths in jail at the 6-month interview were incarcerated with AOD-related felonies, and the probability of relapse among the nonincarcerated youths was 0.60. Similar to other adolescent residential treatment samples (Winters et al., 2000), most relapses involved marijuana and alcohol (85%), with a portion using marijuana with inhalants (11%) or narcotics only (4%). While there was no association between SAD and likelihood of incarceration posttreatment, high helping was associated with lower risk of incarceration (Table 4). The likelihood of relapse was significantly lower for SAD youths and high helpers, with evidence of a mediational effect of peer-helping. As shown in Fig. 1, low helpers with SAD had the lowest survival rate (0.2) in terms of avoided taking a drink or drug posttreatment, followed by low helpers without SAD (0.4), high helpers with SAD (0.6), and high helpers without SAD (0.7; χ2 = 8.9, p < 0.001).
Table 4.
Predictors of 6-Month Outcomes
| Incarceration (N = 16)
|
Relapse (N = 84)
|
|||||
|---|---|---|---|---|---|---|
| Predictor | B (SE) | χ2 | OR | B (SE) | χ2 | HR |
| Background | ||||||
| Age | 0.02 (0.03) | 0.77 | 1.22 | 0.21 (0.12) | 3.40 | 1.23 |
| Male | −0.04 (0.04) | 0.85 | 0.45 | −0.01 (0.30) | 0.01 | 0.98 |
| Minority | −0.02 (0.05) | 0.16 | 0.71 | 0.25 (0.29) | 0.75 | 1.29 |
| Rural/small town | 0.02 (0.04) | 0.28 | 1.32 | 0.29 (0.25) | 1.32 | 1.33 |
| Single parent | 0.01 (0.04) | 0.05 | 1.04 | −0.16 (0.25) | 0.40 | 0.86 |
| Parent GED or less | 0.02 (0.05) | 0.23 | 1.04 | −0.36 (0.26) | 1.86 | 0.70 |
| Lifetime trauma | 0.02 (0.08) | 0.04 | 0.81 | 0.27 (0.44) | 0.38 | 1.31 |
| Prior treatment | −0.05 (0.08) | 0.36 | 0.46 | 0.51 (0.54) | 0.90 | 1.67 |
| Treatment duration (weeks) | 0.01 (0.02) | 1.81 | 1.01 | −0.07 (0.06) | 1.47 | 0.93 |
| Dependent variable at intake | 0.03 (0.02) | 2.10 | 1.03 | 0.02 (0.01) | 2.60 | 1.02 |
| 12-step | ||||||
| Peer-helping | −0.12 (0.04) | 5.79* | 0.79 | −1.38 (0.63) | 4.85* | 0.61 |
| Meeting attendance | −0.01 (0.01) | 0.09 | 0.99 | −0.01 (0.01) | 0.09 | 0.99 |
| Has sponsor | −0.04 (0.10) | 0.65 | 0.89 | 0.53 (0.32) | 2.05 | 1.30 |
| SAD | −0.03 (0.06) | 0.31 | 0.65 | −0.74 (0.39) | 3.64* | 0.45 |
| SAD × Peer-helping | −0.11 (0.04) | 0.23 | – | 0.76 (0.60) | 2.50* | – |
SAD, social anxiety disorder.
p < 0.05.
Fig. 1.
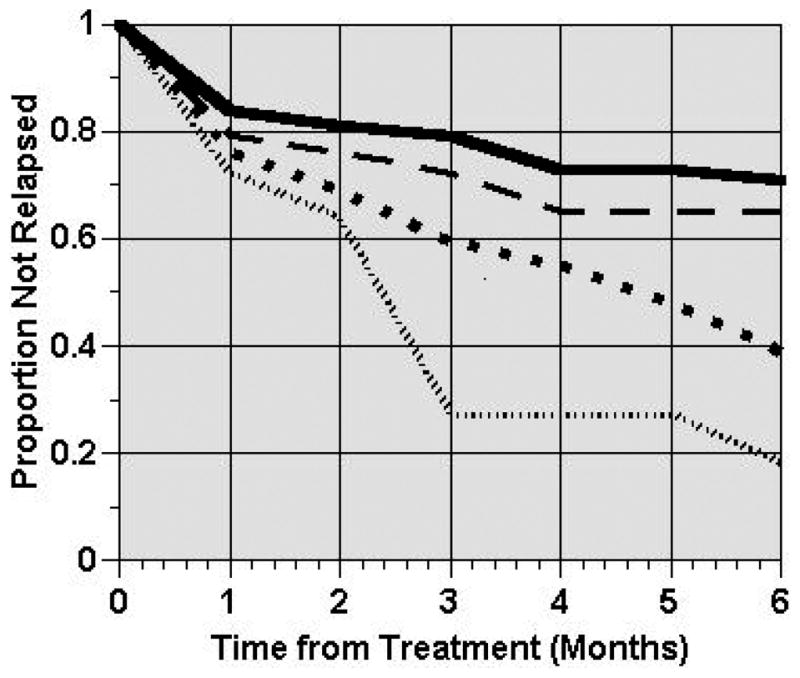
 No social anxiety disorder (SAD), high helping. - - - SAD, high helping.
No social anxiety disorder (SAD), high helping. - - - SAD, high helping.
 No SAD, low helping.
No SAD, low helping.
 SAD, low helping.
SAD, low helping.
DISCUSSION
This study examined the influence of SAD on clinical presentation at treatment admission, 12-step participation during treatment, and 6-month outcomes in a large sample of substance dependent adolescents court-referred to treatment. Our hypothesis of greater clinical severity associated with SAD was confirmed with some markers of impairment. Fifteen percent of the sample met diagnostic criteria for SAD, and almost half (40%) entered treatment with a persistent fear of being scrutinized in social situations. Youths endured SAD 2 years on average before they begin to experiment with AOD, began using AOD at earlier ages, used more heroin and polysubstances, had more stays in jail, and more trauma experiences than youths without SAD. The higher trauma experiences associated with SAD may contribute to lower ability to refuse polysubstances and harder drugs such as heroin, as trauma victims often have problems in setting boundaries. These markers of clinical impairment associated with SAD come at a high cost. While not feeling socially accepted by peers may matter less with age, it strongly influences decisions to drink during adolescence (Crosnoe et al., 2012) with long-term ramifications. In this digital age and public access to criminal records, getting a job will undoubtably add to the challenges these juveniles face.
Our hypothesis of higher peer-helping associated with SAD was confirmed, with one-to-one service activities engaged in the most. In contrast, youths without SAD had higher rates of service activities performed in front of an audience, such as reading literature at the opening or closing of a meeting. Contrary to our hypothesis, meeting attendance and rates of having a sponsor were similar between youths with and without SAD. Higher peer-helping among SAD youths is likely to have promoted their meeting attendance and facilitated conversations with other AA members to ask for their sponsorship. Twelve-step participation patterns among SAD youths did not differ by gender, even though meetings were coed. However, the gender segregation of living quarters and gender-specific group sessions during treatment may have minimized SAD girls’ fear of scrutiny and being accepted by the opposite sex to allow for more practice in speaking up and sharing vulnerabilities in coed settings. Gender-specific modalities are the norm for adolescent residential treatment programs, but not easy to come by once alcoholics turn 19 years of age. Nonetheless, results indicate that SAD youths engage more in peer-helping than youths without SAD and that SAD interferes with willingness to give speeches but not to meet strangers in the social context of AA. In contrast to back and forth dialogue when meeting someone new, sharing at a podium has minimal input from the audience to help an SAD youth accurately gauge their perceptions, and an informational vacuum creates anxiety (Kolb, 2000). Future research is warranted to explore rates of giving leads at meetings increase among SAD youths as duration of time assisting service activities in AA increases.
Results indicated that peer-helping increased the chances of SAD youths staying sober posttreatment, confirming our hypothesis for 1 of 2 outcomes. Consistent with AAH research with adults (Pagano et al., 2004), helping others during treatment doubled the chances of staying sober in the initial months following treatment, a high-risk period when most patients relapse and meeting attendance sharply declines. Peer-helping was also associated with reduced risk of incarceration, which involved AOD use in most incidences. Although SAD was associated with more jail episodes prior to treatment, there was no main effect of SAD on incarceration posttreatment. It is unclear if a negative impact of SAD on incarceration would have been detected if peer-helping was discouraged during treatment, as may be the case if clinicians consider peer-helping as a form of giving back rather than as an agent in shifting perspective. In this study, SAD youths with low helping behavior had the lowest rate of sustained sobriety in the 6 months posttreatment, whereas SAD youths with high helping maintained sobriety at rates comparable to high helpers without SAD.
Learning to live sober with social anxiety is a challenge in a competitive society where people can be quick to judge others (Aronson et al., 2010; Gray, 1993). Coping with a persistent fear of being scrutinized in social situations often requires learning to tolerate the opinions of others, feeling different, appropriate boundary setting, and enduring short-term discomfort for long-term gain—skills that are in short supply among adolescents and those in early recovery. The low-intensity service activities in AA offer youths—and those with SAD in particular—a nonjudgmental, task-focused venue for social connectedness, reduce self-preoccupation and feeling like a misfit, and transform a troubled past to usefulness with others (Pagano et al., 2011). Given finite treatment resources and the reality that addiction is lifelong, AAH should be encouraged for socially anxious youths in particular. Many patients may not be aware of the many ways they can participate in this programmatic activity that clinicians should bring to their attention, thereby increasing the chances for hypersensitive youths to thrive in sobriety. As stated by a young adult, “I wanted to be at peace with myself and comfortable with other people. The belonging I always wanted I have found in AA. I got into service work right away and really enjoyed it” (Alcoholics Anonymous, 2001).
Limitations and Strengths
Some limitations of our study merit attention. First, the functional impairment threshold may underrepresent the rate of SAD if activities in school, work, and relationships selected have minimal distressing situations that trigger SAD symptoms. Future studies may consider use of continuous assessments like the Liebowitz Social Anxiety Scale. Second, causation of factors associated with SAD, such as childhood trauma, is inconclusive given the study design. Third, tested models were not exhaustive, and other nonspecified variables could also account for observed relationships. For example, spirituality may increase in tandem with helping behaviors (Lee et al., 2014), which may contribute to behavioral changes. Fourth, longer follow-up is needed to determine whether adult patterns of sustained helping and associated benefit over time (Pagano et al., 2013a) replicate with juvenile offenders. Reducing the risk of relapse and incarceration over a 1-year period would be particularly telling in light of all the formidable challenges and obstacles associated with maintaining juvenile rehabilitation.
There are a number of strengths to this study. This study is the first to explore SAD’s influence on peer-helping and other 12-step activities among boys and girls with substance dependency. The restructuring of social relationships, substance-free recreation, and tools to walk through life events without self-medicating are available to those who get engaged in AA and other 12-step programs of recovery. Other strengths include sufficient power (i.e., >80%) to detect at least moderate effects that extend our understanding of the benefits of peer-helping among youths with and without SAD. Data were collected prospectively using valid and reliable instruments that employed multiple informants (i.e., rater-administered, clinician assessments, and youth reports) and methods (i.e., biomarkers, semi-structured interviews, self-reports, medical chart review, and public records). On average, interviews were performed <3 years after the youth’s actual reported age of first AOD use, minimizing recall bias of onset ordering. Last, this study had high retention of a large, representative sample of juvenile offenders (52% female, 30% minority) notoriously difficult to follow.
Clinical Implications
Socially anxious youths entering addiction treatment are ideally given a full diagnostic evaluation, effective medications for SAD such as paroxetine (Book et al., 2008) are considered, and empirically based behavioral modalities for SAD are implemented into individualized treatment plans (Randall et al., 2001). Healthcare reform and the merging of mental health and addiction services offer hope for this ideal to materialize in addiction treatment. Until then, the recommendation to attend 12-step meetings could be tailored to promote service participation at meetings for improved outcomes for substance abusing juveniles with and without social anxiety.
Acknowledgments
SOURCES OF SUPPORT
This research was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism (NIA-AA, K01 AA015137) and the John Templeton Foundation awarded to MEP
Footnotes
AUTHOR CONTRIBUTIONS
MEP, ARW, MTL, and BRJ contributed to the conception and design of the research; MEP, ARW, and BMR. analyzed and interpreted the data; and MEP, ARW, BMR, MTL, and BRJ contributed to the writing and intellectual content of the article.
References
- Alcoholics Anonymous. It Sure Beats Sitting in a Cell. Alcoholics Anonymous World Services; New York, NY: 2000. [Google Scholar]
- Alcoholics Anonymous. Alcoholics Anonymous: The Story of How Many Thousands of Men and Women Have Recovered from Alcoholism. 4. Alcoholics Anonymous World Services; New York, NY: 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 2000. text rev. [Google Scholar]
- Arnaud M, Malet L, Teissedre F, Izaute M, Moustafa F, Geneste J, Schmidt J, Llorca P, Brousse G. Validity study of Kessler’s psychological distress scales conducted among patients admitted to French emergency department for alcohol consumption-related disorders. Alcohol Clin Exp Res. 2010;34:1127–1302. doi: 10.1111/j.1530-0277.2010.01201.x. [DOI] [PubMed] [Google Scholar]
- Aronson E, Wilson TD, Akert RM. Social Psychology. 7. Prentice Hall; Upper Saddle River, NJ: 2010. pp. 57–81. [Google Scholar]
- Babor TF, Steinberg K, Zweben A, Cisler R, Stout R, Tonigan JS, Anton RF, Allen JP. Treatment effects across multiple dimensions of outcome. In: Babor TF, Del Boca FK, editors. Treatment Matching in Alcoholism. Cambridge University. Press; New York, NY: 2003. pp. 150–165. [Google Scholar]
- Book SW, Thomas SE, Dempsey JP, Randall PK, Randall CL. Social anxiety impacts willingness to participate in addiction treatment. Addict Behav. 2009;34:474–476. doi: 10.1016/j.addbeh.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Book SW, Thomas SE, Randall PK, Randall CL. Paroxetine reduces social anxiety in individuals with a co-occurring alcohol use disorder. J Anxiety Disord. 2008;22:310–318. doi: 10.1016/j.janxdis.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano ME, Shea MT, Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carruthers KA, Delos Reyes CM, Mahfoud Y, Johnson SM, Carter RR, Ionescu R, Pagano ME. Gender differences in adolescents entering residential substance abuse treatment. Am J Addict. 2012;21:391. [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum; Mahwah, NJ: 1988. [Google Scholar]
- Crosnoe R, Benner AD, Schneider B. Drinking, socioemotional functioning, and academic progress in secondary school. J Health Soc Behav. 2012;53:150–162. doi: 10.1177/0022146511433507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forcehimes AA, Tonigan JS. Self-efficacy to remain abstinent and substance abuse. Alcohol Treat Q. 2008;26:480–489. [Google Scholar]
- Gray J. Men, Women, and Relationships: Making Peace with the Opposite Sex. Harper Collins Publishers Ltd; Toronto, ON, Canada: 1993. [Google Scholar]
- Grisso T, Barnum R. User’s Manual and Technical Reports. University of Massachusetts Medical School; Boston, MA: 2000. Massachusetts Youth Screening Instrument-second version. [Google Scholar]
- Guerri C, Pascual M. Mechanisms involved in the neurotoxic, cognitive, and neurobehavioral effects of alcohol consumption during adolescence. Alcohol. 2010;44:15–26. doi: 10.1016/j.alcohol.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Hall MT, Howard MO, McCabe SE. Prescription drug misuse among antisocial youths. J Stud Alcohol Drugs. 2010;71:917–924. doi: 10.15288/jsad.2010.71.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley W, Mazor S. Anticipated medical effects on children from legalization of marijuana in Colorado and Washington State: a poison center perspective. JAMA Pediatr. 2013;167:602–603. doi: 10.1001/jamapediatrics.2013.2273. [DOI] [PubMed] [Google Scholar]
- Kann L, Kinchen SA, Williams BI, Ross JG, Lowry R, Grunbaum JA, Kolbe LJ. Youth risk behavior surveillance—United States, 1999. MMWR CDC Surveill Summ. 2000;49:1–32. [PubMed] [Google Scholar]
- Kelly JF, Pagano ME, Stout RL, Johnson SM. Influence of religiosity on 12-step participation and treatment response among substance-dependent adolescents. J Stud Alcohol Drugs. 2011;72:1000–1011. doi: 10.15288/jsad.2011.72.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolb DM. Staying out of your own way. In: Kolb DM, Williams J, editors. The Shadow Negotiation: How Women can Master the Hidden Agendas that Determine Bargaining Success. Simon & Schuster; New York, NY: 2000. p. 48. [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL, Brekke M, Sletten S. Follow-up of anxiety disorder and alcohol dependence in co-morbid alcoholism treatment patients. Alcohol Clin Exp Res. 2005;29:1432–1443. doi: 10.1097/01.alc.0000175072.17623.f8. [DOI] [PubMed] [Google Scholar]
- Larson MJ, Shepard DS, Zwick W, Stout R. Validity of health care utilization reporting systems. Alcohol Clin Exp Res. 1997;21:2360. [Google Scholar]
- Lee MT, Veta PS, Johnson BR, Pagano ME. Daily spiritual experiences and adolescent treatment response. Alcohol Treat Q. 2014;32:271–298. doi: 10.1080/07347324.2014.907029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midlarsky E. Helping as coping. In: Clark M, editor. Prosocial Behavior: Review of Personality and Social Psychology. Sage; Thousand Oaks, CA: 1991. pp. 238–264. [Google Scholar]
- Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62:211–220. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Dickson N, Silva P, Stanton W. Childhood-onset versus adolescent-onset antisocial conduct problems in males. Dev Psychopathol. 1996;8:399–424. [Google Scholar]
- Mulye TP, Park MJ, Nelson CD, Adams SH, Irwin CE, Brindis CD. Trends in adolescent and young adult health in the United States. J Adolesc Health. 2009;45:8–24. doi: 10.1016/j.jadohealth.2009.03.013. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA) Principles of Adolescent Substance Use Disorder Treatment: A Research-based Guide: NIH Pub. No. 14-7953. National Institute on Drug Abuse; Rockville, MD: 2014. [Google Scholar]
- Pagano ME, Friend KB, Tonigan JS, Stout RL. Helping other alcoholics in Alcoholics Anonymous and drinking outcomes: findings from project MATCH. J Stud Alcohol Drugs. 2004;65:766–773. doi: 10.15288/jsa.2004.65.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Kelly JF, Scur MD, Ionescu RA, Stout RL, Post SG. Assessing youth participation in AA-related helping: validity of the service to others in sobriety (SOS) questionnaire in an adolescent sample. Am J Addict. 2013b;22:60–66. doi: 10.1111/j.1521-0391.2013.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Phillips KA, Stout RL, Menard W, Piliavin JA. Impact of helping behaviors on the course of substance use disorders in individuals with body dysmorphic disorder. J Stud Alcohol Drugs. 2007;68:291–295. doi: 10.15288/jsad.2007.68.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Post SG, Johnson SM. Alcoholics Anonymous-related helping and the helper therapy principle. Alcohol Treat Q. 2011;29:23–34. doi: 10.1080/07347324.2011.538320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, White WL, Kelly JF, Stout RL, Tonigan JS. The 10-year course of Alcoholics Anonymous participation and long-term outcomes: a follow-up study of outpatient subjects in Project MATCH. Subst Abus. 2013a;34:51–59. doi: 10.1080/08897077.2012.691450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Zemore SE, Onder CC, Stout RL. Predictors of initial AA-related helping: findings from project MATCH. J Stud Alcohol Drugs. 2009;70:117–125. doi: 10.15288/jsad.2009.70.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piliavin JA. Feeling good by doing good. In: Omoto AM, Oskamp S, editors. Processes of Community Change and Social Action. Lawrence Erlbaum Associates; Mahwah, NJ: 2005. pp. 29–50. [Google Scholar]
- Project MATCH Research Group. Project Match: rational and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: a first step toward developing effective treatment. Alcohol Clin Exp Res. 2001;25:210–220. [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: a longitudinal investigation. Arch Gen Psychiatry. 2011;68:800–807. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT User’s Guide, Version 9.2. SAS Institute Inc; Cary, NC: 2008. [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorimi P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The mini-international neuro-psychiatric interview. J Clin Psychiatry. 1998;59(S20):22–33. [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback User’s Guide. Addictions Research Foundation; Toronto, ON: 1996. [Google Scholar]
- Terra MB, Barros HM, Stein AT, Figueira I, Athayde LD, Spanemberg L, Possa MA, Filho LD, da Silveira DX. Does co-occurring social phobia interfere with alcoholism treatment adherence and relapse? J Subst Abuse Treat. 2006;31:403–409. doi: 10.1016/j.jsat.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Book SW, Pagano ME, Randall PK, Smith JP, Randall CL. 12-Step therapy and women with and without social phobia: a study of the effectiveness of 12-step therapy to facilitate AA engagement. Alcohol Treat Q. 2010;28:151–162. doi: 10.1080/07347321003648596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang AR, Scur MD, Pagano ME, Delos-Reyes CM. Associations between anxiety disorders and substance use disorders in substance-dependent adolescents. J Addict Med. 2013;7:E2. [Google Scholar]
- Winters KC, Stinchfield RD, Opland E, Weller C, Latimer WW. The effectiveness of the Minnesota Model approach in the treatment of adolescent drug abusers. Addiction. 2000;95:601–612. doi: 10.1046/j.1360-0443.2000.95460111.x. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Wittchen HU, Höfler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychol Med. 2003;33:1211–1222. doi: 10.1017/s0033291703008158. [DOI] [PubMed] [Google Scholar]


