Abstract
Urinary incontinence after robot-assisted radical prostatectomy (RARP) is one of the most bothersome complications affecting patients’ daily lives. The efficacy of the bladder neck plication stitch technique in promoting an earlier return of continence was prospectively evaluated in 158 patients who underwent RARP for clinically localized prostate cancer by a single surgeon at our institute from March 2012 to January 2013. Patients were randomized 1:1 to undergo surgery with (n = 79) or without (n = 79) the bladder neck plication stitch, and their time to recovery from incontinence, defined as being pad free, was compared. Recovery from incontinence at 1, 3, and 6 months were observed in 22 (27.8%), 42 (53.2%), and 57 (72.2%) patients, respectively, treated with, and 23 (29.1%), 47 (59.5%), and 59 (74.7%) patients, respectively, treated without the bladder neck plication stitch, with no significant difference in time to recovery from incontinence between the two groups. Multivariate analysis showed that age, membranous urethral length and shape of the prostatic apex on magnetic resonance imaging were independent predictors of early recovery from urinary incontinence after RARP. The bladder neck plication stitch had no effect on time to recovery from postoperative urinary incontinence following RARP.
Keywords: prostatectomy, prostatic neoplasms, urinary incontinence, urologic surgical procedures
INTRODUCTION
Although robot-assisted radical prostatectomy (RARP) has many advantages over open retropubic radical prostatectomy, postoperative urinary incontinence is a complication of radical prostatectomy that significantly compromises patient quality of life and has serious psychosocial effects, regardless of oncologic and sexual functional outcomes.1 The etiology of postprostatectomy incontinence is not completely understood. However, both functional and anatomical changes associated with prostate removal lead to alterations in the urinary sphincter complex and pelvic floor musculature.2 The prevalence of incontinence after radical prostatectomy is reported to vary widely, from 2.5% to 87%,3 whereas continence rates following RARP are >90%.4,5,6 These rates, however, depend on the definition of urinary control, the methodology of determining outcomes, and surgical technique. Many refined surgical techniques have been developed to improve postoperative urinary incontinence, such as posterior rhabdosphincter reconstruction,7,8 apical dissection modifications,9 anatomic bladder neck preservation,10 total reconstruction of the vesicourethral junction,11 seminal vesicle sparing techniques,12 and puboprostatic ligament sparing.13,14
A bladder neck plication stitch has also been reported to improve urinary continence during bladder neck reconstruction.15 This stitch was derived from the intussusception stitch technique introduced for open radical prostatectomy procedures to improve the postoperative recovery of continence.16 Altering the bladder neck plication technique resulted in shorter recovery times to urinary continence, with multivariate analysis showing significantly increased odds of recovery 1 and 12 months after surgery.15 That the study, however, had several limitations, being retrospective and nonrandomized in design. Therefore, this prospective, randomized, control study was designed to evaluate the efficacy of the bladder neck plication stitch technique in facilitating an earlier return to continence.
MATERIALS AND METHODS
Enrollment
The study was a two-arm single-blind randomized controlled trial design involving 158 men with clinically localized prostate cancer scheduled for RARP from March 2012 to January 2013. Men with preexisting symptoms of incontinence, any previous bladder or urethral surgery, or previous radiation therapy for the pelvis were excluded due to the possible effects of these factors on postoperative continence. The study protocol was approved by the Institutional Review Board of the Asan Medical Center, Seoul, Korea, and all patients provided written informed consent.
Randomization and masking
After completion of baseline assessments, participants were randomized 1:1 to undergo RARP with or without the bladder neck plication stitch technique. The randomization process was performed by a senior nurse with no other involvement in the study. Functional outcomes were assessed by a senior nurse in an outpatient clinic who was blinded to group allocations.
Sample size
Three studies showed that the bladder neck plication stitch technique, during radical retropubic prostatectomy or RARP, enhanced the postoperative continence rate, by a median 20% at 3 months.15,16,17 Assuming similar outcomes, the sample size was calculated to show a difference of 20% with a two sided significance level at 0.05% and 80% power. This required a total of 142 patients. To account for a dropout and noncompliance rate of 10%, 158 patients were finally included in the study cohort.
Surgical technique
All procedures were performed by the same experienced robotic surgeon (Hanjong Ahn) using the da Vinci Si robotic system (Intuitive Surgical, Sunnyvale, CA, USA) and a transperitoneal approach. The bladder neck plication technique used was similar to that described previously.15 Briefly, beginning with the anastomosis, Denonvilliers’ fascia was posteriorly reconstructed using the Rocco et al. technique,7,8 and running, double-armed 3–0 absorbable polyglactin suture with a Van Velthoven stitch used for urethrovesical anastomosis.18 After completion of vesicourethral anastomosis, 3–0 absorbable polyglactin single suture was used to plicate the bladder neck in a figure-of-8 fashion (Figure 1). The first suture bite was taken at about the 3 o’clock position about 2 cm proximal to the edge of the bladder neck or anastomosis. A similar small bite was taken at the 9 o’clock position. This process was repeated at a position 5 mm more proximal on the bladder neck. The suture was then tied down directly on top. This plication of the bladder neck created a funnel configuration, such that the distal bladder neck remained narrower during bladder filling.15 The bladder neck plication stitch was very simple and required <2 min.15
Figure 1.
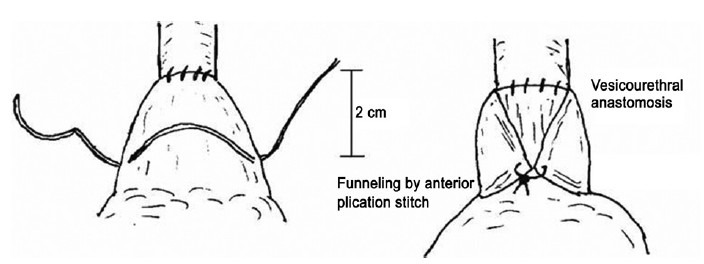
Schematic (from Lee et al.) showing the bladder neck plication stitch technique.15 The bladder neck plication stitch is positioned 2 cm proximal to the vesicourethral anastomosis at 3 o’clock and 9 o’clock.
Outcome measures
Data were collected prospectively. The primary outcome measure was time to recovery from postoperative urinary incontinence, which was assessed by the Expanded Prostate Cancer Index Composite questionnaire19 at the 1, 3, and 6 months postoperative follow-up visits. Continence was defined as being pad free. The continence status of patients lost to follow-up was defined as that recorded during the last follow-up visit. The secondary outcome measures included factors associated with the recovery of continence; clinicopathological and patient-specific parameters, including age, body mass index (BMI), level of prostate-specific antigen (PSA), prostate volume, membranous urethral length (MUL) and shape of the prostatic apex on preoperative magnetic resonance imaging. Also included were the results of the neurovascular bundle (NVB) saving, pathologic stage, Gleason score, lymph node involvement, and contrast leakage from urethrovesical anastomosis sites. Continence was also assessed in patients who received postoperative radiation therapy during follow-up to assess the effects of radiation therapy on continence rate. The MUL was estimated by measuring the length from the prostatic apex to the level of the urethra at the penile bulb in the midline sagittal plane of T2-weighted magnetic resonance imaging of the prostate. Data were analyzed on an intent-to-treat basis. Continuous variables were analyzed using unpaired Student's t-tests, and categorical variables were analyzed using Fisher's exact tests and Pearson's chi-square test. Factors associated with recovery of continence were assessed by multivariate logistic regression model. P < 0.05 was considered as statistically significant.
RESULTS
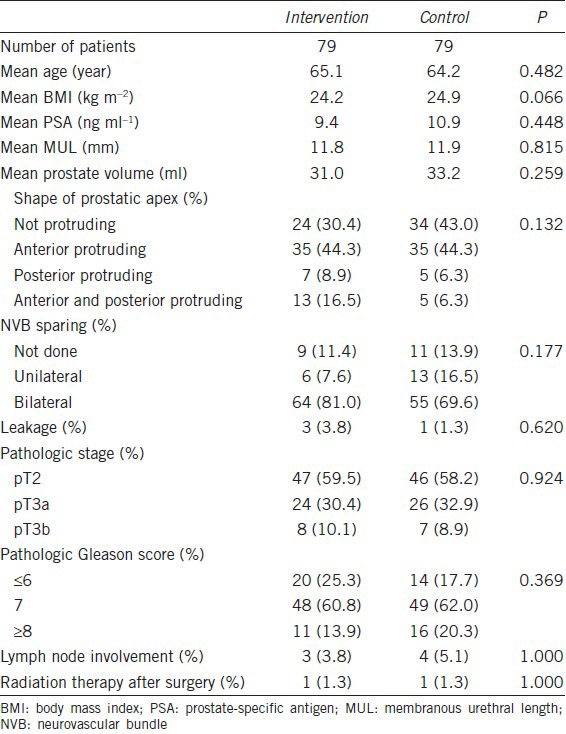
Between March 2012 and January 2013, 158 patients at our institute were recruited to this study. All underwent RARP, 79 with and 79 without the bladder neck plication stitch technique (Figure 2). Five patients were lost to follow-up prior to 6 months postoperatively. There were no significant differences between these two groups in age (65.1 vs 64.2 years, P = 0.482), BMI (24.2 vs 24.9 kg m−2, P = 0.066), PSA (9.4 vs 10.9 ng ml−1, P = 0.448), prostate volume (31.0 vs 33.2 ml, P = 0.259), or MUL (11.8 vs 11.9 mm, P = 0.815). Patient distributions, including the prostatic apical shape, results of NVB saving, pathologic stage, Gleason score, lymph node involvement, and contrast leakage from urethrovesical anastomosis sites, were also similar in the two groups. Only two patients received adjuvant radiation therapy during follow-up (Table 1).
Figure 2.
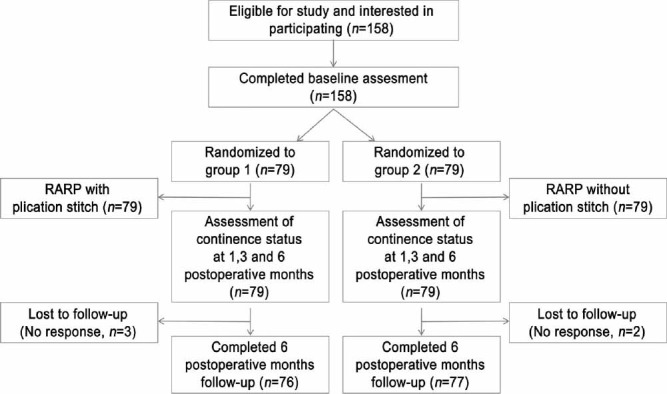
CONSORT diagram of recruitment and loss to follow-up in the study.
Table 1.
Clinical and pathological characteristics of the patients
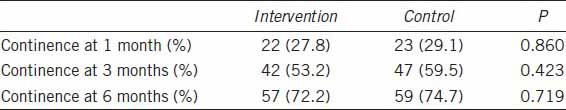
Recovery from incontinence at 1, 3, and 6 months was observed in 22 (27.8%), 42 (53.2%), and 57 (72.2%) patients, respectively, treated with the bladder neck plication stitch, and 23 (29.1%), 47 (59.5%), and 59 (74.7%) patients, respectively, treated without the bladder neck plication stitch (Table 2). No significant between-group differences were found in patterns of recovery or mean times to recovery from incontinence (3.84 vs 3.32 months, P = 0.324). No patient in either group experienced bladder neck contracture or other urinary complications.
Table 2.
Continence status of the patients at 1, 3 and 6 months after surgery
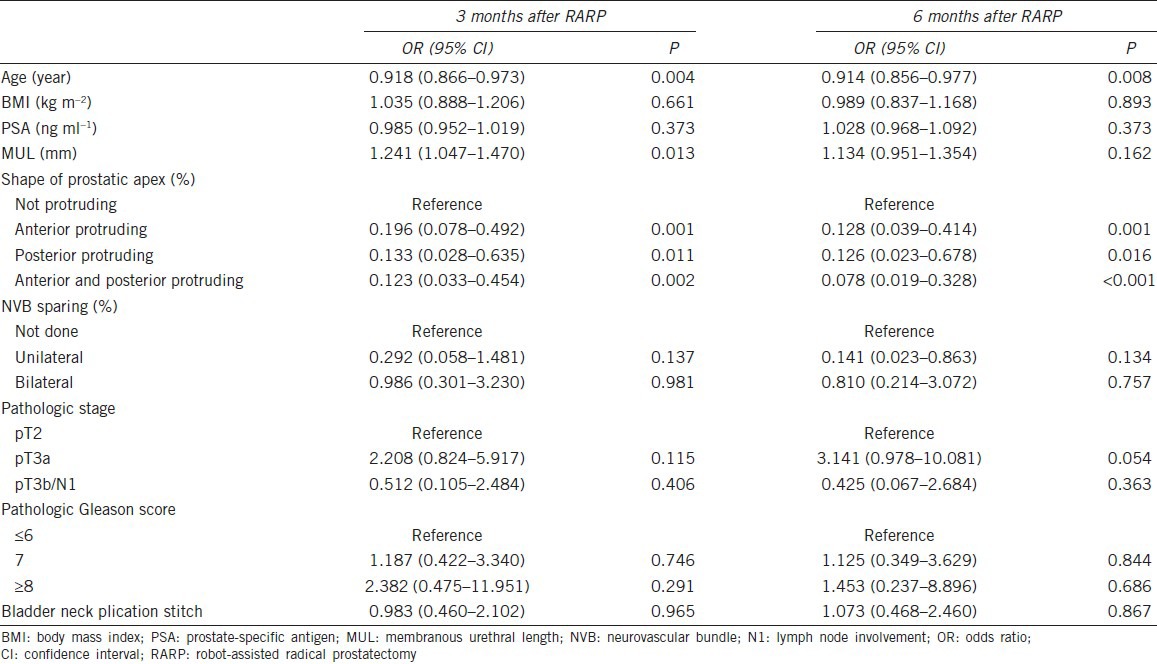
Multivariate analysis showed that continence at 3 and 6 months was inversely associated with age (odds ratio (OR) =0.918, P = 0.004; OR = 0.914, P = 0.008) and protrusion of the prostatic apex, including anterior protrusion (OR = 0.196, P = 0.001; OR = 0.128, P = 0.001), posterior protrusion (OR = 0.133, P = 0.011; OR = 0.126, P = 0.016), and both protrusions (OR = 0.123, P = 0.002; OR = 0.078, P < 0.001). MUL was associated with continence status at 3 months (OR = 1.241, P = 0.013), but not at 6 months (Table 3).
Table 3.
Factors associated with recovery of continence within 3 and 6 months after RARP
DISCUSSION
Intussusception of the bladder neck has been reported to result in earlier restoration of continence after retropubic radical prostatectomy.16 In that study, 82% men were continent 3 months after the intussusception of the bladder neck compared with only 54% men who underwent retropubic radical prostatectomy without intussusception. The precise mechanism by which intussusception of the bladder neck promotes earlier recovery from postoperative incontinence remains unclear, although two possibilities were suggested: (1) buttressing sutures may prevent the bladder neck from pulling apart as the bladder fills; and (2) functional residual urethral length may be increased by preventing the proximal end of urethral stump from opening. Two subsequent comparative studies of intussusception of the bladder neck yielded contradictory findings. One study found that intussusception of the bladder neck during retropubic radical prostatectomy resulted in a significantly greater continence rate of (77% vs 60%) after 3 months although continence rates at 12 months were similar.17 By contrast, the other study found that continence rates at 1, 3, and 6 months were 37.5%, 67.7%, and 95.8%, respectively, in patients with, and in 33.3%, 62.5%, and 95.8%, respectively, of patients without intussusception of the bladder neck after retropubic radical prostatectomy, with no significant between-group differences at any time point.20
A modification of the intussusception stitch technique16 led to the development of the bladder neck plication stitch in RARP.15 This method involved anterior stitching only after urethrovesical anastomosis because posterior bladder neck stitching is technically difficult to perform robotically. The bladder neck plication stitch causes the bladder neck to become more funneled in appearance, likely decreasing the degree of stretch on the bladder neck and urinary sphincter at rest. Furthermore, this funneling may lengthen the functional length of the urethra. That study reported total continence rates in patients with and without bladder neck plication stitching were higher at 1 month (16% vs 8.9%, P = 0.097) and 3 months (36.3% vs 31.3%, P = 0.63), and were significantly higher at 12 months (85.7% vs 74.4%, P = 0.042). By contrast, our study found that the percentages of continent patients with and without bladder neck plication stitching after RARP similar at 1 month (27.8% vs 29.1%), 3 months (53.2% vs 59.5%), and 6 months (72.2% vs 74.7%). These findings were also consistent with the results of per-protocol analysis in our study.
A possible explanation for the discrepancy between our current findings and those reportedly previously15 was that the early study only included age, BMI, and prostate volume as preoperative parameters. Several studies have suggested that the mechanism regulating continence is multifactorial, with many factors related to the recovery of urinary continence after radical prostatectomy. Hence, to determine continence status after RARP, not only age, BMI, and prostate volume, but also MUL, shape of the prostatic apex, and nerve-sparing surgery should be considered.21,22,23,24,25 We, therefore, utilized a logistic regression model to determine whether these factors affect the recovery of continence within 3 and 6 months after RARP. We found that patient age, MUL, and shape of the prostatic apex were significantly and independently associated with early recovery from postoperative urinary incontinence. These results are in accordance with those of prior studies, further indicating that younger age at operation, a nonprotruding prostatic apex and a longer MUL are predictors of earlier postoperative recovery of continence.21,22,23,24,25
We also found that the bladder neck plication stitch did not have a significant impact on continence status. Indeed, the continence rates 1, 3, and 6 months after the surgery were slightly higher in the absence than in the presence of bladder neck plication stitching, although none of these differences were statistically significant. Although not significant, mean age was lower and mean MUL slightly longer in patients who did not than who did undergo bladder neck plication stitching. Furthermore, the percentage of patients with nonprotruding prostatic apex on preoperative magnetic resonance imaging was slightly higher in patients who did not undergo bladder neck plication stitching. Those findings indicate that factors associated with postoperative incontinence, including age, MUL, and shape of the prostatic apex, have a greater impact on continence recovery than the use of a bladder neck plication stitch. Other potential reason for the differing results is that in the study of Lee et al.15 the mean patient age, which is one of the predictive factors for continence recovery after RARP,25 was significantly younger than that of our study.
Regarding the safety and difficulty of the bladder neck plication stitch technique, no patient in either of our study groups experienced bladder neck contracture or other urinary complications. In addition, the technique was easy to learn and reproduce using robotic surgery.15 These findings indicate the need for prospective randomized controlled trials of modified stitches or other methodologies based on new concepts to develop an effective surgical technique for the earlier recovery from urinary incontinence after RARP. Preoperative factors associated with postoperative urinary incontinence should be considered when counseling patients before surgery.
AUTHOR CONTRIBUTIONS
SP was responsible for the concept and framework of the paper. SP and SKC participated in collecting and evaluating the data. SKC wrote the paper. HA supervised the study. All the authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Stanford JL, Feng Z, Hamilton AS, Gilliland FD, Stephenson RA, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA. 2000;283:354–60. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- 2.Song C, Doo CK, Hong JH, Choo MS, Kim CS, et al. Relationship between the integrity of the pelvic floor muscles and early recovery of continence after radical prostatectomy. J Urol. 2007;178:208–11. doi: 10.1016/j.juro.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 3.Foote J, Yun S, Leach GE. Postprostatectomy incontinence. Pathophysiology, evaluation, and management. Urol Clin North Am. 1991;18:229–41. [PubMed] [Google Scholar]
- 4.Badani KK, Kaul S, Menon M. Evolution of robotic radical prostatectomy: assessment after 2766 procedures. Cancer. 2007;110:1951–8. doi: 10.1002/cncr.23027. [DOI] [PubMed] [Google Scholar]
- 5.Patel VR, Coelho RF, Palmer KJ, Rocco B. Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: description of the technique and continence outcomes. Eur Urol. 2009;56:472–8. doi: 10.1016/j.eururo.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Tewari A, Jhaveri J, Rao S, Yadav R, Bartsch G, et al. Total reconstruction of the vesico-urethral junction. BJU Int. 2008;101:871–7. doi: 10.1111/j.1464-410X.2008.07424.x. [DOI] [PubMed] [Google Scholar]
- 7.Rocco F, Carmignani L, Acquati P, Gadda F, Dell’Orto P, et al. Restoration of posterior aspect of rhabdosphincter shortens continence time after radical retropubic prostatectomy. J Urol. 2006;175:2201–6. doi: 10.1016/S0022-5347(06)00262-X. [DOI] [PubMed] [Google Scholar]
- 8.Rocco B, Gregori A, Stener S, Santoro L, Bozzola A, et al. Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol. 2007;51:996–1003. doi: 10.1016/j.eururo.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Terakawa T, Takenaka A, Tunemori H, Taguchi I, Imanishi O, et al. Modifications in the technique for apical dissection of radical retropubic prostatectomy to improve urinary incontinence. Nihon Hinyokika Gakkai Zasshi. 2006;97:1–9. doi: 10.5980/jpnjurol1989.97.1. [DOI] [PubMed] [Google Scholar]
- 10.Freire MP, Weinberg AC, Lei Y, Soukup JR, Lipsitz SR, et al. Anatomic bladder neck preservation during robotic-assisted laparoscopic radical prostatectomy: description of technique and outcomes. Eur Urol. 2009;56:972–80. doi: 10.1016/j.eururo.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 11.Tan G, Srivastava A, Grover S, Peters D, Dorsey P, Jr, et al. Optimizing vesicourethral anastomosis healing after robot-assisted laparoscopic radical prostatectomy: lessons learned from three techniques in 1900 patients. J Endourol. 2010;24:1975–83. doi: 10.1089/end.2009.0630. [DOI] [PubMed] [Google Scholar]
- 12.John H, Hauri D. Seminal vesicle-sparing radical prostatectomy: a novel concept to restore early urinary continence. Urology. 2000;55:820–4. doi: 10.1016/s0090-4295(00)00547-1. [DOI] [PubMed] [Google Scholar]
- 13.Poore RE, McCullough DL, Jarow JP. Puboprostatic ligament sparing improves urinary continence after radical retropubic prostatectomy. Urology. 1998;51:67–72. doi: 10.1016/s0090-4295(97)00479-2. [DOI] [PubMed] [Google Scholar]
- 14.Stolzenburg JU, Liatsikos EN, Rabenalt R, Do M, Sakelaropoulos G, et al. Nerve sparing endoscopic extraperitoneal radical prostatectomy - effect of puboprostatic ligament preservation on early continence and positive margins. Eur Urol. 2006;49:103–11. doi: 10.1016/j.eururo.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Lee DI, Wedmid A, Mendoza P, Sharma S, Walicki M, et al. Bladder neck plication stitch: a novel technique during robot-assisted radical prostatectomy to improve recovery of urinary continence. J Endourol. 2011;25:1873–7. doi: 10.1089/end.2011.0279. [DOI] [PubMed] [Google Scholar]
- 16.Walsh PC, Marschke PL. Intussusception of the reconstructed bladder neck leads to earlier continence after radical prostatectomy. Urology. 2002;59:934–8. doi: 10.1016/s0090-4295(02)01596-0. [DOI] [PubMed] [Google Scholar]
- 17.Wille S, Varga Z, von Knobloch R, Hofmann R. Intussusception of bladder neck improves early continence after radical prostatectomy: results of a prospective trial. Urology. 2005;65:524–7. doi: 10.1016/j.urology.2004.09.066. [DOI] [PubMed] [Google Scholar]
- 18.Van Velthoven RF, Ahlering TE, Peltier A, Skarecky DW, Clayman RV. Technique for laparoscopic running urethrovesical anastomosis: the single knot method. Urology. 2003;61:699–702. doi: 10.1016/s0090-4295(02)02543-8. [DOI] [PubMed] [Google Scholar]
- 19.Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]
- 20.Sakai I, Harada K, Hara I, Eto H, Miyake H. Intussusception of the bladder neck does not promote early restoration to urinary continence after non-nerve-sparing radical retropubic prostatectomy. Int J Urol. 2005;12:275–9. doi: 10.1111/j.1442-2042.2005.01070.x. [DOI] [PubMed] [Google Scholar]
- 21.Coakley FV, Eberhardt S, Kattan MW, Wei DC, Scardino PT, et al. Urinary continence after radical retropubic prostatectomy: relationship with membranous urethral length on preoperative endorectal magnetic resonance imaging. J Urol. 2002;168:1032–5. doi: 10.1016/S0022-5347(05)64568-5. [DOI] [PubMed] [Google Scholar]
- 22.Paparel P, Akin O, Sandhu JS, Otero JR, Serio AM, et al. Recovery of urinary continence after radical prostatectomy: association with urethral length and urethral fibrosis measured by preoperative and postoperative endorectal magnetic resonance imaging. Eur Urol. 2009;55:629–37. doi: 10.1016/j.eururo.2008.08.057. [DOI] [PubMed] [Google Scholar]
- 23.Lee SE, Byun SS, Lee HJ, Song SH, Chang IH, et al. Impact of variations in prostatic apex shape on early recovery of urinary continence after radical retropubic prostatectomy. Urology. 2006;68:137–41. doi: 10.1016/j.urology.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 24.Takenaka A, Soga H, Sakai I, Nakano Y, Miyake H, et al. Influence of nerve-sparing procedure on early recovery of urinary continence after laparoscopic radical prostatectomy. J Endourol. 2009;23:1115–9. doi: 10.1089/end.2008.0512. [DOI] [PubMed] [Google Scholar]
- 25.Kim SC, Song C, Kim W, Kang T, Park J, et al. Factors determining functional outcomes after radical prostatectomy: robot-assisted versus retropubic. Eur Urol. 2011;60:413–9. doi: 10.1016/j.eururo.2011.05.011. [DOI] [PubMed] [Google Scholar]


