Abstract
Vasectomy reversal (VR) has traditionally been performed with the operative microscope. Recently, robot assistance has been applied to VR. Retrospective chart review from a single VR center included men who underwent either robot-assisted VR (RAVR) or microsurgical VR (MVR) by a single fellowship trained microsurgeon between 2011 and 2013 and had a 6 weeks postoperative semen analysis. Fifty-two men who were interested in VR were counseled and given the option of RAVR versus MVR. Twenty-seven men elected to have MVR while 25 men elected RAVR. These included vasovasostomies and vasoepididymostomies in both groups, as well as redo VRs in men who had failed previous VR attempts by other surgeons. There was no statistically significant difference between the microsurgical group and the robot-assisted group, respectively, in overall patency rates (89% vs 92%), 6 weeks post-VR mean sperm concentrations (28 million ml−1 vs 26 million ml−1) or total motile counts (29 million vs 30 million), or mean operative times (141 min vs 150 min). There was a statistically significant difference in anastomosis time (64 min vs 74 min), however, clinically this only represented a 10 min longer anastomosis time in the early robotic experience, which was found to be decreasing as the case series continued. Transitioning from MVR to RAVR is feasible with comparable outcomes.
Keywords: patency, robot-assisted, vasectomy reversal, vasoepididymostomy, vasovasostomy
INTRODUCTION
Approximately, 500 000 men undergo vasectomy for contraception every year in the United States. Approximately, 6% of these men will ultimately seek vasectomy reversal (VR) during their lifetime.1,2 Patency rates have been associated with time since vasectomy, intraoperative assessment of vasal fluid quality, as well as the presence of sperm in vasal fluid intraoperatively, surgical technique, and the training and experience of the surgeon.3,4,5,6,7 Since the advent of the operative microscope and its use for VR in the 1970s, there have been some changes in the instrumentation used for this procedure, but little in the way of alternative magnification sources or truly different technology.8 Relatively recently, the robotic platform was applied to VR in humans and may offer some potential advantages.9,10,11,12,13
MATERIALS AND METHODS
Vasectomy reversal was performed for 52 consecutive men by one fellowship trained microsurgeon between 2011 and 2013. Of these men, 27 elected to have microsurgical VR (MVR) while 25 elected robot-assisted VR (RAVR). Each patient was counseled on both surgical techniques and selected the technique of choice for them. This may have also been based on cost for some patients, as the robot-assisted technique costs a total of 315 dollars more than the microsurgical technique due to the hospital fee being higher than the surgery center fee. The cases in the study included vasovasostomies and vasoepididymostomies in both groups, as well as men who were having repeated attempts at reconstruction after failing VR with another surgeon. Both MVRs and RAVRs were set up for the anastomosis in the same manner. The scrotal incision for all vasovasostomies was 1 cm in length longitudinally, and bilateral vasectomy defects were isolated and delivered through this single incision. For vasoepididymostomies, the testicles were delivered through a median raphe incision. For vasovasostomies, the abdominal and testicular ends of the vas deferens were sharply divided above and below the vasectomy defect, the fluid from the testicular end was examined under the light microscope, and saline was injected through the abdominal end to demonstrate patency. The microspike vas clamp was utilized to approximate the ends, and the anastomosis was performed with either the da Vinci SI robotic system or the operative microscope. Vasoepididymostomies were performed in five men in the microsurgical group and two men in the robot-assisted group, and the remainder underwent vasovasostomies. Vasovasostomies were performed in the straight, as well as the convoluted vas deferens depending on intraoperative findings. Regardless of whether the VR was performed by microsurgical or robot-assisted technique, a modified one-layer anastomosis was performed with interrupted 9-0 nylon sutures. Vasoepididymostomies were performed using the two suture intussuscepted technique with 10-0 nylon suture.14
A retrospective chart review was performed after obtaining Institutional Review Board approval from the Austin Multi-Institutional Review Board. The outcomes measured included overall patency rates between the two groups as well as patency rates subdivided in intervals from the time since vasectomy. The three intervals assessed included 0–8 years postvasectomy, 9–15 years postvasectomy, as well > 15 years since vasectomy. Patency was defined as the presence of sperm in the semen at 6 weeks post-VR. The other outcomes measured included mean sperm concentration and total motile count at the 6 weeks post-VR semen analysis, operative time, and anastomosis time.
RESULTS
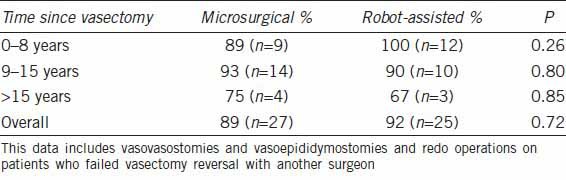
After counseling, 27 men underwent MVR while 25 underwent RAVR (Figures 1 and 2). In men who were 0–8 years from the time of vasectomy, there was no statistically significant difference in patency rates at 6 weeks post-VR, however, the robotic group demonstrated a 100% patency rate, whereas the microsurgical group had an 89% patency rate. There was no statistically significant difference in patency rates in men who were 9–15 years from the time of vasectomy, in the > 15 years postvasectomy group, or in overall patency rates regardless of obstructive interval (Table 1). All vasoepididymostomies were patent in both groups.
Figure 1.
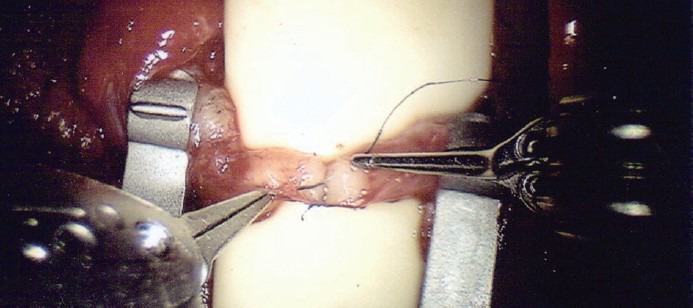
Vasovasostomy being performed with the robotic system, demonstrating anastomosing the ends of the vas deferens with interrupted 9-0 nylon suture with a modified one-layer technique.
Figure 2.
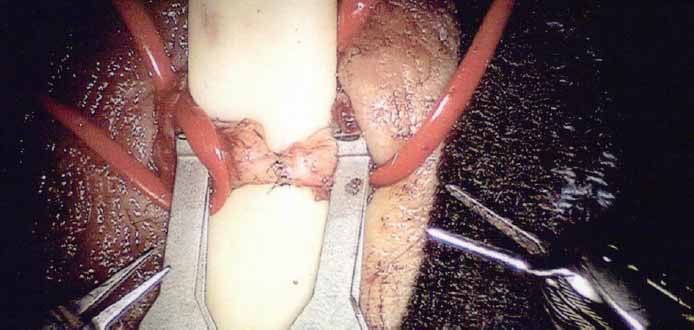
The appearance of the robot-assisted vasovasostomy anastomosis while maintaining the vasal adventitia for microvascular preservation.
Table 1.
Patency rates based on the number of years from vasectomy to vasectomy reversal
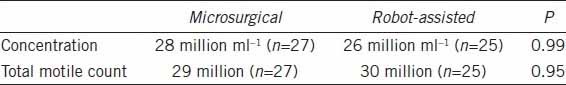
There was no difference between the microsurgical and robot-assisted groups in mean sperm concentration or total motile count on semen analysis 6 weeks post-VR (Table 2). There were no men in either group who demonstrated the sperm in the semen with no motility, indicative of stricture. Preliminary pregnancy data were reviewed, although a great deal of this data is still pending in many cases and a number have been lost to follow-up, for reasons such as many patients travel from surrounding regions for VR and find follow-up difficult due to distance. As these data include cases from the beginning of this private practice, the number of cases done early in the series are far outnumbered by the more recent ones with growth of the practice, therefore, a great deal of pregnancy data is still pending. Preliminary pregnancy data reveal 6 pregnancies in the MVR group and 7 pregnancies in the RAVR group thus far. The mean time to pregnancy in the MVR group was 9 months, and 2 of these pregnancies were following microsurgical vasoepididymostomies. The mean time to pregnancy in the RAVR group was 5 months, and these were all following robot-assisted vasovasostomies. The mean operative time for the MVR group was 141 min (n = 27) compared to 150 min (n = 25) in the RAVR group. There was not a statistically significant difference in mean operative times between the two groups (P = 0.3). Evaluation of the mean anastomosis times between the two groups was performed as this was the step of the operation that the robot was used for compared to the microscope. The mean anastomosis time for the MVR group was 64 min (n = 27) versus 74 min (n = 25) for the RAVR group. There was a statistically significant difference in the mean anastomosis times between the two groups (P = 0.009), with a 10 min longer mean anastomosis time with the robot-assisted group. A subgroup analysis of vasoepididymostomy patients reveals a mean anastomosis time of 74 min in the MVR group compared to a mean anastomosis time of 72 min in the RAVR group.
Table 2.
Mean sperm concentration and total motile count at 6 weeks postvasectomy reversal
DISCUSSION
For nearly a decade, the idea of applying the da Vinci® robotic system for VR has been explored. In 2004, ex-vivo vasal anastomoses were performed with the robot with the findings of tremor elimination and comparable patency rates.15 In 2005, improved stability and motion reduction during suturing was demonstrated while performing robot-assisted vasovasostomy and robot-assisted vasoepididymostomy in a rat model.16 A two-layer anastomosis was performed using robot assistance in an in vivo rabbit model in 2005.17 Ultimately, RAVR was applied to human surgery by Dr. Parekattil in 2010, with data suggesting shorter operative times and higher mean sperm counts in men undergoing RAVR.9,18
This current study demonstrates no statistically significant difference in patency rates between the two surgical techniques. However, in men who were in the 0–8 years obstructed interval, the robot-assisted technique had a 100% patency rate while the microsurgical technique had an 89% patency rate, which could arguably be a clinically significant difference. In contrast to previous human data, this data does not demonstrate a difference between sperm concentrations or total motile counts based on surgical instrumentation. Mean operative times were similar. As every patient's anatomy is different and there may be challenges in the setup of the vasal ends, or the vasal end to the epididymal tubule, for anastomosis depending on the vasectomist's technique or the tissue response, we thought it important to compare the actual anastomosis times between the two groups. The anastomosis is the only portion of the operation during which the robotic system is docked and used. Therefore, this was thought to be an important outcome to compare while eliminating variables of the time it may take to set up the vasal ends to prepare for the anastomosis with either technique. Although the mean robotic anastomosis time is statistically longer than the microsurgical anastomosis time, it is clinically a 10 min difference, which has debatable clinical significance. It should also be considered that there is a learning curve involved with robotic microsurgery, and this data is inclusive from the first RAVR performed by this surgeon with progression through the period reported. This surgeon is also fellowship trained in the traditional microsurgery. There has been shortening of operative and anastomotic robotic time with case volume and the practical difference between the two groups appears small. The question has arisen as to whether a surgeon formally trained in robotic surgery might have superior outcomes to one trained in microsurgery for RAVR. The author would argue that a surgeon trained in both disciplines is best suited for this operation, but as the data reveal, the transition from MVR to RAVR can be relatively seamless. In fact, the argument can be made that the principles of microsurgery are being applied to robot-assisted microsurgery and what is learned of tissue handling microsurgically is easily translated to robotic microsurgery. An understanding of the management of such patients and following semen parameters, and understanding when further intervention or assistance may be needed to assist the couple in conceiving is paramount for any surgeon caring for these patients. Therefore, training in the care for subfertile men is of great importance to provide this service.
The operative robot brings a new dynamic to microsurgery. It offers a number of potential advantages. These include elimination of tremor, improved stability, surgeon ergonomics/decreased surgeon fatigue, scalability of motion, three-dimensional high-definition visualization, the ability for the surgeon to manipulate three surgical instruments and the camera simultaneously, not requiring a specialty skilled microsurgical assistant, and the potential of improving operative times. The operative times have been reported as being shorter in a previous publication, and with experience, the surgeon from this study sees a similar trend.9 An additional advantage of the robotic platform is that during a difficult microsurgical case, if the surgeon backs away from the microscope for a moment and then re-engages, the surgical field has almost always invariably moved or changed. This is not the case with the robotic system, which allows for the surgeon to back out of the console, re-engage, and nothing in the field has changed.
Limitations to this study include the sample size, especially in men who are 15 years or greater from the time of vasectomy. Ultimately, prospective, randomized, control trials would give better data to elucidate the use of RAVR in comparison to traditional MVR.
CONCLUSION
Robot-assisted vasectomy reversal is an effective option with comparable outcomes.
COMPETING INTERESTS
The author declares no competing interests.
ACKNOWLEDGMENTS
St. David's South Austin Medical Center robotic surgery team: Charlie Harlan, C.S.T., Tara Buck, R.N., B.S.N., C.N.O.R., and Thomas Butz, R.N. who were integral in the establishment and surgical assistance of the robotic vasectomy reversal program.
REFERENCES
- 1.Sheynkin YR, Ye Z, Menendez S, Liotta D, Veeck LL, et al. Controlled comparison of percutaneous and microsurgical sperm retrieval in men with obstructive azoospermia. Hum Reprod. 1998;13:3086–9. doi: 10.1093/humrep/13.11.3086. [DOI] [PubMed] [Google Scholar]
- 2.Sandlow JI, Nagler HM. Vasectomy and vasectomy reversal: important issues. Preface. Urol Clin North Am. 2009;36:xiii–xiv. doi: 10.1016/j.ucl.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Belker AM, Thomas AJ, Jr, Fuchs EF, Konnak JW, Sharlip ID. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. J Urol. 1991;145:505–11. doi: 10.1016/s0022-5347(17)38381-7. [DOI] [PubMed] [Google Scholar]
- 4.Kolettis PN, Sabanegh ES, Nalesnik JG, D’Amico AM, Box LC, et al. Pregnancy outcomes after vasectomy reversal for female partners 35 years old or older. J Urol. 2003;169:2250–2. doi: 10.1097/01.ju.0000063780.74931.d6. [DOI] [PubMed] [Google Scholar]
- 5.Lipshultz LI. Vasectomy reversal-predicting outcomes. J Urol. 2004;171:310. doi: 10.1097/01.ju.0000102200.69922.bf. [DOI] [PubMed] [Google Scholar]
- 6.Brannigan RE. Vasectomy reversal: indications and outcomes. J Urol. 2012;187:385–6. doi: 10.1016/j.juro.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Hsiao W, Goldstein M, Rosoff JS, Piccorelli A, Kattan MW, et al. Nomograms to predict patency after microsurgical vasectomy reversal. J Urol. 2012;187:607–12. doi: 10.1016/j.juro.2011.10.044. [DOI] [PubMed] [Google Scholar]
- 8.Kim HH, Goldstein M. History of vasectomy reversal. Urol Clin North Am. 2009;36:359–73. doi: 10.1016/j.ucl.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Parekattil SJ, Atalah HN, Cohen MS. Video technique for human robot-assisted microsurgical vasovasostomy. J Endourol. 2010;24:511–4. doi: 10.1089/end.2009.0235. [DOI] [PubMed] [Google Scholar]
- 10.Boccard GD. Geneva Foundation for Medical Research; 2006. Robotic vasectomy reversal. [Google Scholar]
- 11.De Nayer PV, Schatteman P, Fonteyne E, Mottrie A. Robotic assistance in urological microsurgery: initial report of successful in-vivo robot-assisted vasovasostomy. J Robot Surg. 2007;1:161–2. doi: 10.1007/s11701-007-0025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Boccard G. Robotic two plane microsurgical vasectomy reversal with 11/0 and 10/1 sutures. Econ Robot Surg Newsl. 2009:7. [Google Scholar]
- 13.De Boccard G, Mottrie A. Robotic surgery in male infertility. In: Hemal AK, Menon M, editors. Robotics in Genitourinary Surgery. London: Springer-Verlag; 2011. pp. 617–23. [Google Scholar]
- 14.Berger RE. Triangulation end-to-side vasoepididymostomy. J Urol. 1998;159:1951–3. doi: 10.1016/S0022-5347(01)63205-1. [DOI] [PubMed] [Google Scholar]
- 15.Kuang W, Shin PR, Matin S, Thomas AJ., Jr Initial evaluation of robotic technology for microsurgical vasovasostomy. J Urol. 2004;171:300–3. doi: 10.1097/01.ju.0000098364.94347.02. [DOI] [PubMed] [Google Scholar]
- 16.Schiff J, Li PS, Goldstein M. Robotic microsurgical vasovasostomy and vasoepididymostomy in rats. Int J Med Robot. 2005;1:122–6. doi: 10.1002/rcs.21. [DOI] [PubMed] [Google Scholar]
- 17.Kuang W, Shin PR, Oder M, Thomas AJ., Jr Robotic-assisted vasovasostomy: a two-layer technique in an animal model. Urology. 2005;65:811–4. doi: 10.1016/j.urology.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 18.Parekattil SJ, Gudeloglu A, Brahmbhatt J, Wharton J, Priola KB. Robotic assisted versus pure microsurgical vasectomy reversal: technique and prospective database control trial. J Reconstr Microsurg. 2012;28:435–44. doi: 10.1055/s-0032-1315788. [DOI] [PubMed] [Google Scholar]


