Abstract
A recent treatment option for non-vital immature teeth in young patients is revascularization with triple antibiotic paste (TAP). However, tooth discoloration was reported with the use of conventional minocycline-containing TAP. In this case report, amoxicillin-containing TAP was used for revascularization of non-vital immature teeth to prevent tooth discoloration. At the 1 yr follow up, the teeth were asymptomatic on clinical examination and showed slight discoloration of the crown due to mineral trioxide aggregate (MTA) filling rather than amoxicillin-containing TAP. Radiographic examination revealed complete resolution of the periapical radiolucency, and closed apex with obvious periodontal ligament space. However, the root growth was limited, and the treatment outcome was more like apexification rather than revascularization. These results may be due to unstable blood clot formation which could not resist the condensation force of MTA filling, whether or not a collagen matrix was in place. These cases showed that although revascularization was not successful, apexification could be expected, resulting in the resolution of the periapical radiolucency and the closure of the apex. Therefore, it is worthwhile attempting revascularization of non-vital immature teeth in young patients.
Keywords: Amoxicillin, Apexification, Immature teeth, Revascularization, Triple antibiotic paste
Introduction
Traditionally, the treatment plan for infected, non-vital, immature tooth is apexification with calcium hydroxide.1,2 The goal of apexification is to form an apical barrier for the filling materials to be compacted within the root canal space.3 Calcium hydroxide is usually used as an intra-canal medicament to control the infection and to induce an apical barrier. However, multiple visits to the dentist for lengthy time periods are required until the root canal is filled.4 To shorten the treatment period, mineral trioxide aggregate (MTA) is used instead of calcium hydroxide.3 Nonetheless, the root remains thin and weak after apexification.
Revascularization has recently been introduced. In 1992, Sato et al. reported disinfection of infected root canal using a mixture of antibacterial drugs.5 Because infection of the root canal is a polymicrobial infection consisting of both aerobic and anaerobic bacteria, the use of a mixture of ciprofloxacin, metronidazole, and minocycline was suggested for treating the teeth with necrotic pulps and infected root dentine.6,7,8,9,10,11,12 Revascularization procedure consists of three important stages, that is, elimination of bacteria from the root canal system, creation of a scaffold for the ingrowth of new tissue, and prevention of reinfection by creating a bacteria-tight seal.9,10,12,13,14,15,16 Through revascularization, the immature tooth shows continued root formation in length as well as in width, which is impossible to achieve through apexification.3
However, minocycline was reported to cause discoloration of teeth when triple antibiotic paste (TAP) is used as an intracanal medication.11,17,18,19,20 Thereafter, many efforts were made to reduce tooth discoloration when using TAP.10,11,18 Metal tip delivery system was used to prevent direct contact of TAP with the coronal dentin in the tooth.10,18 Also, application of a dentin bonding agent on the coronal dentin before TAP application could prevent tooth discoloration.11,18 On the other hand, substituting minocycline with an alternative antibiotic such as amoxicillin could reduce tooth discoloration and achieve effective disinfection of the root canal.5,15,18
The purpose of this paper was to report two cases in which revascularization of infected, non-vital, immature tooth was attempted using an amoxicillin-containing TAP that resulted in apexification rather than revascularization.
Case Reports
Case 1
A 20 year old female patient visited the Department of Conservative Dentistry in Chonnam National University Dental Hospital for treatment of the mandibular right second premolar. The patient complained of pain during mastication and swelling of the gingiva adjacent to the tooth.
On clinical examination, fractured dens evaginatus was suspected on the occlusal surface of the tooth (Figure 1a), and vestibular swelling was noted adjacent to the tooth. The tooth showed no response to electric pulp testing, and there was no mobility. The tooth was severely painful on percussion, and tender on palpation around the vestibule. Radiographic examination showed periapical radiolucency of the mandibular right second premolar with an open apex (Figure 1b). Based on these findings, the tooth was diagnosed with pulp necrosis and periapical abscess. Because the tooth had incomplete root formation with an open apex, revascularization was planned.
Figure 1. Clinical photographs and periapical radiographs of the mandibular right second premolar with an open apex. (a) Preoperative clinical photograph showing fractured dens evaginatus; (b) Preoperative periapical radiograph showing apical radiolucency and open apex; (c) Periapical radiograph after MTA filling showing limited blood clot space; (d) Clinical photograph at the 12 month follow-up showing slight grayish discoloration of the crown; (e) Periapical radiograph at the 12 month follow-up showing resolution of the apical radiolucency and limited root formation.
Local anesthesia was administered using 2% lidocaine with 1:100,000 epinephrine, and access cavity was prepared in the mandibular right second premolar under rubber dam isolation. The root canal was passively irrigated with 20 mL of 5.25% NaOCl using 31 gauge Endo-Eze irrigation needle tip (Ultradent, South Jordan, UT, USA) for 10 minutes. The needle tip was placed 2 mm away from the radiographic root end. Then, the root canal was irrigated with saline and dried with paper points.
TAP consisting of equal amounts of metronidazole (Flasinyl, CJ CheilJedang, Hwaseong, Korea), ciprofloxacin (Cyrocan, Hawon, Pyeongtaek, Korea), and amoxicillin (A-cillin, Boryung, Ansan, Korea) was mixed with saline on a glass slab. Using a lentulo spiral, amoxicillin-containing TAP was delivered to the dried root canal and filled to a level of 2 mm below the cemento-enamel junction. Then, the access cavity was temporarily sealed with Caviton (GC, Tokyo, Japan).
After three weeks, the patient's symptoms were relieved. The tooth was not painful on percussion, and the vestibular swelling had subsided. Tooth discoloration due to antibiotic was not observed. Under rubber dam isolation, the root canal was irrigated with saline to wash out the amoxicillin-containing TAP followed by a final rinse with 17% ethylenediaminetetraacetic acid (EDTA, Pulpdent, Watertown, MA, USA) and dried with paper points. To induce bleeding into the root canal, a size 10 K file was used to irritate the apical tissue. Then, ProRoot MTA (Dentsply, Tulsa, OK, USA) was applied with the aid of paper points up to the alveolar bone crest level followed by temporary filling with Caviton. Although MTA was carefully applied to the apical root canal, the blood-filled space underneath the MTA was hardly detected in the periapical radiograph (Figure 1c). On the following day, the tooth was restored permanently with a dual-cure composite resin (LuxaCore Z-Dual, DMG, Hamburg, Germany).
At the 1 year follow up, the tooth was asymptomatic. The tooth was mildly discolored with slight grayish color of the crown due to MTA filling (Figure 1d). Radiographic examination revealed complete resolution of the periapical radiolucency, and closed apex with obvious periodontal ligament space (Figure 1e). However, the root growth was limited, and the treatment outcome was more like apexification rather than revascularization.
Case 2
A 10 year old female patient presented with spontaneous pain in the mandibular right second premolar. On clinical examination, the tooth showed no response to electric pulp testing. The tooth had mobility with severe pain on percussion, and gingival swelling was observed around the involved tooth. Radiographic examination revealed large periapical radiolucency around the open apex of the mandibular right second premolar (Figure 2a). Based on these findings, the tooth was diagnosed with pulp necrosis and periapical abscess, and revascularization using an amoxicillin-containing TAP was planned.
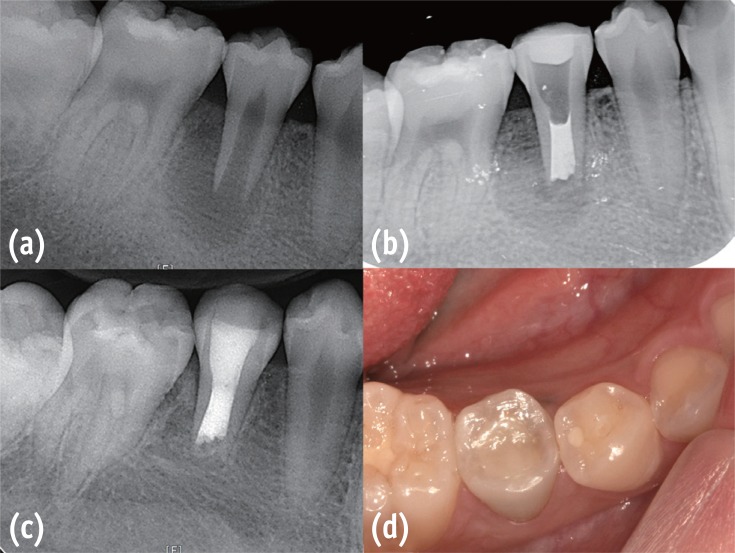
Figure 2. Periapical radiographs and clinical photograph of the mandibular right second premolar with an open apex. (a) Preoperative periapical radiograph showing apical radiolucency with underdeveloped root; (b) Periapical radiograph after MTA filling showing limited blood clot space despite using collagen matrix; (c) Periapical radiograph at the 12 month follow-up showing resolution of the apical radiolucency without further root formation; (d) Clinical photograph at the 12 month follow-up showing slight grayish discoloration of the crown due to MTA filling.
After local anesthesia using 2% lidocaine with 1:100,000 epinephrine, the access cavity was prepared under rubber dam isolation. The root canal was passively irrigated with 20 mL of 5.25% NaOCl and dried with the aid of paper points. Amoxicillin-containing TAP was prepared as described above and delivered to the root canal using a lentulo spiral. TAP was filled to the level of 2 mm below cemento-enamel junction. The access cavity was temporarily sealed with Caviton and the patient was discharged.
After three weeks, the patient's symptoms were relieved. There was only slight pain on percussion without any mobility or gingival swelling. Tooth discoloration was not observed. Under rubber dam isolation, the root canal was gently irrigated with saline followed by final rinse with 17% EDTA. After the root canal was dried with paper points, bleeding was induced at the apical end with a size 10 K file. An absorbable atelocollagen sponge (Teruplug, Terumo, Tokyo, Japan) was cut into small sizes and delivered to the blood filled root end space to create an apical matrix. ProRoot MTA was applied with paper points to the root canal followed by a temporary filling with Caviton (Figure 2b). On the next day, the tooth was restored permanently with a dual-cure composite resin (LuxaCore Z-Dual).
At the 1 year follow up, the mandibular right second premolar was asymptomatic. The tooth was mildly discolored with slight grayish color of the crown by MTA filling similar to the first case (Figure 2d). Radiographic examination revealed complete resolution of the periapical radiolucency and a closed apex with obvious periodontal ligament space (Figure 2c). However, the root growth was limited, and the treatment outcome was apexification rather than pulp revascularization.
Discussion
An amoxicillin-containing TAP was used for disinfection of the root canals in both cases. Amoxicillin is a well-known broad spectrum antibiotic, and it is effective in eradicating most of the bacteria from the root canals.8,21,22 In a recent study, a total of 287 different bacterial strains were collected from 60 infected root canals with periapical abscess and all of the tested microorganisms were susceptible to amoxicillin.22 In accordance with the results of this study, the patients' symptoms were relieved and there were no signs of infection after three weeks of intracanal medication in the current cases.
Another advantage of using amoxicillin is that it causes less tooth discoloration than minocycline. Thompson and Kahler used an amoxicillin-containing TAP for revascularization and it resulted in a successful treatment outcome of an infected immature premolar without any discoloration.15 Akcay et al. reported that an amoxicillin-containing TAP caused less tooth discoloration than TAPs containing minocycline, doxycycline, or cefaclor.19 Severe color change was induced after 1 day by TAPs containing minocycline, doxycycline or cefaclor, compared to the color change after 1 week by amoxicillin-containing TAP. In the current case report, amoxicillin-containing TAP was placed for 3 weeks and tooth discoloration was not observed at the time when amoxicillin-containing TAP was removed. However, after 12 months, slight grayish tooth discoloration was observed. According to previous studies, tooth discoloration due to the use of TAP usually develops within the first 3 to 4 weeks as TAP is washed out during copious irrigation of the root canal.10,11,18,19 Therefore, this slight grayish discoloration might be due to the MTA filling rather than amoxicillin-containing TAP. A recent guideline for revascularization from American Association of Endodontists recommended that root end filling with MTA should be avoided in cases where there is an esthetic concern.23 The guideline suggested 3 to 4 mm of resin-modified glass ionomer cement (RMGIC) filling after inserting root end matrix material instead of MTA because of discolorations associated with it.23
We used 17% EDTA as a final rinse after washing out the amoxicillin-containing TAP with saline in both cases. Recent studies recommended the use of EDTA because of its chelating action on the root canal wall. Through decalcification, growth factors are released from the root canal dentin and they promote differentiation of cells into odontoblast-like cells.16,24,25
Hargreaves et al. summarized the essential factors for achieving a successful treatment outcome of revascularization.12 With respect to case selection, a wide and open apex is required for tissue ingrowth. Also, young patients have higher stem cell regenerative potential. During the clinical procedure, attention should be paid to avoid contact of the instrument with the canal walls, and sufficient use of sodium hypochlorite should be performed for effective irrigation. For disinfection of the root canal, TAP containing ciprofloxacin, metronidazole, and minocycline is effective for eliminating bacteria from the infected root canal system. Finally, the initiation of a blood clot is necessary as it acts as a protein scaffold that allows tissue regeneration.
In case 1, the apex of the second premolar was not adequately open and the root was already formed to the length similar to the first premolar. Also, the age of the patient was 20 years compared to the other case reports in which the age of the patients was less than 18 years.9,12,14 These factors could have influenced the treatment outcome. More importantly, the disinfected root canal should have been filled with blood clot to obtain the regenerative potential of apical stem cells. However, in this case, there was little space for the blood clot, and the major part of the root canal was filled with MTA (Figure 1). It could be suspected that the time for blood clot formation was not sufficient and MTA occupied the blood filled space before clot formation. Jung et al. reported that they waited for 15 minutes for blood clot formation.26 Albeit, the blood clot was still fragile and some of the MTA extruded into the apical third of the root canal. Therefore, more than 15 minutes would be needed for formation and stabilization of the blood clot. Blood clots in the root canal are supposed to act as scaffolds, rich in many growth-factors.9 Previous studies showed that root canals containing blood clots after disinfection had better treatment outcomes than those without blood clots in the apical part.13,27 Also, Ding et al. reported that in their cases, unfavorable revascularization outcomes were related to the failure to induce bleeding into the root canal.9 The resolution of inflammation in the apical region, as well as the use of local anesthetics with epinephrine could be one of the reasons.
In case 2, the mandibular second premolar showed a wide and open apex for sufficient tissue ingrowth and the patient was as young as 10 years. After irritation of the apical tissue for inducing bleeding, an apical matrix was inserted to retain blood in the root canal before clot formation. Then, the canal was filled with MTA. However, minimum blood-filled space was observed on the periapical radiograph even though an apical matrix was introduced into the root canal. Lack of blood clot formation might have limited the growth potential of the root. Literatures suggested that a resorbable collagen matrix should be placed before filling the disinfected root canal with MTA or glass ionomers to preserve the blood filled space.23,26 It might be possible that, in this case, cutting the apical matrix into small pieces had little effect on maintaining the blood filled space in the apical part. Also, even with the apical matrix, sufficient time would be needed for formation and stabilization of the blood clot.
In the current cases, revascularization of non-vital immature teeth was attempted using amoxicillincontaining TAP and resulted in limited root formation in length as well as in width possibly due to insufficient blood clot formation. However, as long as the root canal is disinfected, apexification could be expected, resulting in the resolution of the radiolucency with apical closure of the root.
Conclusions
Revascularization of infected, non-vital, immature teeth was attempted using amoxicillin-containing TAP. Tooth discoloration was limited to the minimum. However, insufficient blood clot formation due to the extrusion of MTA into the apical root canal limited the tissue ingrowth and resulted in apexification. These cases showed that although revascularization was not successful, apexification could be expected, resulting in the resolution of the periapical radiolucency with apical closure. Therefore, it would be worthwhile to attempt revascularization of non-vital immature teeth.
Acknowledgement
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2013R1A1A2008051).
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Dominguez Reyes A, Muñoz Muñoz L, Aznar Martín T. Study of calcium hydroxide apexification in 26 young permanent incisors. Dent Traumatol. 2005;21:141–145. doi: 10.1111/j.1600-9657.2005.00289.x. [DOI] [PubMed] [Google Scholar]
- 2.Ghose LJ, Baghdady VS, Hikmat YM. Apexification of immature apices of pulpless permanent anterior teeth with calcium hydroxide. J Endod. 1987;13:285–290. doi: 10.1016/s0099-2399(87)80045-6. [DOI] [PubMed] [Google Scholar]
- 3.Huang GT. Apexification: the beginning of its end. Int Endod J. 2009;42:855–866. doi: 10.1111/j.1365-2591.2009.01577.x. [DOI] [PubMed] [Google Scholar]
- 4.Rafter M. Apexification: a review. Dent Traumatol. 2005;21:1–8. doi: 10.1111/j.1600-9657.2004.00284.x. [DOI] [PubMed] [Google Scholar]
- 5.Sato I, Ando-Kurihara N, Kota K, Iwaku M, Hoshino E. Sterilization of infected root-canal dentine by topical application of a mixture of ciprofloxacin, metronidazole and minocycline in situ. Int Endod J. 1996;29:118–124. doi: 10.1111/j.1365-2591.1996.tb01172.x. [DOI] [PubMed] [Google Scholar]
- 6.Baumgartner JC, Falkler WA., Jr Bacteria in the apical 5 mm of infected root canals. J Endod. 1991;17:380–383. doi: 10.1016/s0099-2399(06)81989-8. [DOI] [PubMed] [Google Scholar]
- 7.Windley W, 3rd, Teixeira F, Levin L, Sigurdsson A, Trope M. Disinfection of immature teeth with a triple antibiotic paste. J Endod. 2005;31:439–443. doi: 10.1097/01.don.0000148143.80283.ea. [DOI] [PubMed] [Google Scholar]
- 8.Pinheiro ET, Gomes BP, Drucker DB, Zaia AA, Ferraz CC, Souza-Filho FJ. Antimicrobial susceptibility of Enterococcus faecalis isolated from canals of root filled teeth with periapical lesions. Int Endod J. 2004;37:756–763. doi: 10.1111/j.1365-2591.2004.00865.x. [DOI] [PubMed] [Google Scholar]
- 9.Ding RY, Cheung GS, Chen J, Yin XZ, Wang QQ, Zhang CF. Pulp revascularization of immature teeth with apical periodontitis: a clinical study. J Endod. 2009;35:745–749. doi: 10.1016/j.joen.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds K, Johnson JD, Cohenca N. Pulp revascularization of necrotic bilateral bicuspids using a modified novel technique to eliminate potential coronal discolouration: a case report. Int Endod J. 2009;42:84–92. doi: 10.1111/j.1365-2591.2008.01467.x. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Kim Y, Shin SJ, Park JW, Jung IY. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod. 2010;36:1086–1091. doi: 10.1016/j.joen.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 12.Hargreaves KM, Giesler T, Henry M, Wang Y. Regeneration potential of the young permanent tooth: what does the future hold? J Endod. 2008;34:S51–S56. doi: 10.1016/j.joen.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 13.Thibodeau B, Teixeira F, Yamauchi M, Caplan DJ, Trope M. Pulp revascularization of immature dog teeth with apical periodontitis. J Endod. 2007;33:680–689. doi: 10.1016/j.joen.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Shah N, Logani A, Bhaskar U, Aggarwal V. Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth: a pilot clinical study. J Endod. 2008;34:919–925. doi: 10.1016/j.joen.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Thomson A, Kahler B. Regenerative endodonticsbiologically-based treatment for immature permanent teeth: a case report and review of the literature. Aust Dent J. 2010;55:446–452. doi: 10.1111/j.1834-7819.2010.01268.x. [DOI] [PubMed] [Google Scholar]
- 16.Law AS. Considerations for regeneration procedures. J Endod. 2013;39:S44–S56. doi: 10.1016/j.joen.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Dodd MA, Dole EJ, Troutman WG, Bennahum DA. Minocycline-associated tooth staining. Ann Pharmacother. 1998;32:887–889. doi: 10.1345/aph.17397. [DOI] [PubMed] [Google Scholar]
- 18.Kim B, Song MJ, Shin SJ, Park JW. Prevention of tooth discoloration associated with triple antibiotics. Restor Dent Endod. 2012;37:119–122. [Google Scholar]
- 19.Akcay M, Arslan H, Yasa B, Kavrik F, Yasa E. Spectrophotometric analysis of crown discoloration induced by various antibiotic pastes used in revascularization. J Endod. 2014;40:845–848. doi: 10.1016/j.joen.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Cheek CC, Heymann HO. Dental and oral discolorations associated with minocycline and other tetracycline analogs. J Esthet Dent. 1999;11:43–48. doi: 10.1111/j.1708-8240.1999.tb00375.x. [DOI] [PubMed] [Google Scholar]
- 21.Sabrah AH, Yassen GH, Gregory RL. Effectiveness of antibiotic medicaments against biofilm formation of Enterococcus faecalis and Porphyromonas gingivalis. J Endod. 2013;39:1385–1389. doi: 10.1016/j.joen.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Sousa EL, Gomes BP, Jacinto RC, Zaia AA, Ferraz CC. Microbiological profile and antimicrobial susceptibility pattern of infected root canals associated with periapical abscesses. Eur J Clin Microbiol Infect Dis. 2013;32:573–580. doi: 10.1007/s10096-012-1777-5. [DOI] [PubMed] [Google Scholar]
- 23.American Association of Endodontists. Considerations for Regenerative Procedures. [updated 2013 July 31]. Available from: www.aae.org/Dental_Professionals/Considerations_for_Regenerative_Procedures.aspx.
- 24.Galler KM, D'Souza RN, Federlin M, Cavender AC, Hartgerink JD, Hecker S, Schmalz G. Dentin conditioning codetermines cell fate in regenerative endodontics. J Endod. 2011;37:1536–1541. doi: 10.1016/j.joen.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 25.Wigler R, Kaufman AY, Lin S, Steinbock N, Hazan-Molina H, Torneck CD. Revascularization: a treatment Park HB et al. for permanent teeth with necrotic pulp and incomplete root development. J Endod. 2013;39:319–326. doi: 10.1016/j.joen.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Jung IY, Lee SJ, Hargreaves KM. Biologically based treatment of immature permanent teeth with pulpal necrosis: a case series. J Endod. 2008;34:876–887. doi: 10.1016/j.joen.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 27.Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004;30:196–200. doi: 10.1097/00004770-200404000-00003. [DOI] [PubMed] [Google Scholar]