Antibody measurements were applied to estimate the rate of Salmonella infections in humans. Data obtained from 13 European countries correlated with the Salmonella prevalence in food animals and estimates of travel-associated Salmonella infections but not with the reported national incidence.
Keywords: nontyphoid Salmonella, seroepidemiology, incidence, food animals, surveillance
Abstract
We developed a model that enabled a back-calculation of the annual salmonellosis seroincidence from measurements of Salmonella antibodies and applied this model to 9677 serum samples collected from populations in 13 European countries. We found a 10-fold difference in the seroincidence, which was lowest in Sweden (0.06 infections per person-year), Finland (0.07), and Denmark (0.08) and highest in Spain (0.61), followed by Poland (0.55). These numbers were not correlated with the reported national incidence of Salmonella infections in humans but were correlated with prevalence data of Salmonella in laying hens (P < .001), broilers (P < .001), and slaughter pigs (P = .03). Seroincidence also correlated with Swedish data on the country-specific risk of travel-associated Salmonella infections (P = .001). Estimates based on seroepidemiological methods are well suited to measure the force of transmission of Salmonella to human populations, in particular relevant for assessments where data include notifications from areas, states or countries with diverse characteristics of the Salmonella surveillance.
Control of food-borne Salmonella infections in humans remain an important priority for public health. Although progress has been noted [1, 2] there are numerous challenges in quantifying progress [3]. Among these is the lack of an objective method to measure the incidence of salmonellosis in humans. Whereas animals and foods can be sampled and tested according to predefined schemes, the incidence of infections in humans is measured by passive laboratory-based surveillance, which is subject to limitations and biases often described as the “surveillance pyramid” [4]. This pyramid describes the chain of events that have to occur so that a case of salmonellosis in the population will become a reported case, including factors such as health-seeking behavior, clinical and laboratory practices regarding microbiological diagnostics, and, finally, reporting compliance. With increasing globalization of the food supply, food safety is more than ever an international issue. For these reasons, how the impact of food safety programs can be monitored and compared between countries, states, or areas has emerged as an important scientific question
We have previously proposed seroepidemiology as a method to measure the force of transmission of nontyphoid Salmonella infections in defined human populations independent of the sensitivity of public health surveillance [5–7]. Because this metric is different from the incidence of clinical infections, we have coined the term seroincidence. The seroincidence is calculated from the analysis of the levels of antibody classes against nontyphoid salmonellae in the general population, and the results of these examinations are converted into a single metric based on the kinetics of the antibody decay. In the present study, we determined the seroincidence of Salmonella in 13 European countries, compared the results with published data from baseline surveys of Salmonella prevalence in food animals across Europe and data from public health surveillance, and determined the relative risk of Salmonella infections in Europe by using Swedish travelers as sentinels.
MATERIALS AND METHODS
Calculation of National Estimates of Seroincidence
In a previous longitudinal study, we followed patients with culture-confirmed infections with Salmonella Typhimurium and Salmonella Enteritidis over time, and determined the decay of serum antibodies (immunoglobulin [Ig] G, A, and M) against Salmonella as measured with an indirect enzyme-linked immunosorbent assay (ELISA) method [8]. We thereby obtained parameters that predict the decay of antibodies as well as the individual variation of the antibody response to the Salmonella infection. These parameters were used in a Bayesian back-calculation model that converts data from the cross-sectional samples on measurements of IgG, IgA, and IgM into an estimation of time since infection [5]. This approach allows estimation of the seroincidence based on results obtained by analysis for antibodies against nontyphoid Salmonella in individuals representing the general population in a country (cross-sectional sample).
In the present study, 13 countries participated with 14 cross-sectional samples. Austria, England, Greece, Ireland, Spain, and the Netherlands (2006–2007) provided serum sample collections. We also recalculated the data from a published study in Denmark, Finland, France, Italy, the Netherlands (1998–2002), Romania, Poland, and Sweden [9]. The seroincidence estimates recalculated for the latter 8 countries vary marginally from the published results [9] owing to nature of the Bayesian approach and minor modifications of the model to increase the efficiency of estimation (details available from the authors). Table 1 provides a summary of the data; details on the cross-sectional samples from Austria, England, Greece, Ireland, and Spain are given below. In total, the 13 countries represent a population of 347 million inhabitants across Europe. We strove to include 500 samples from each country; this goal was based on simulation studies showing that this sample size would allow us to detect a 3-fold difference in seroincidence with 70% power (difference between 0.1 and 0.3 infections per year).
Table 1.
Estimated Salmonella Seroincidence in 13 European Countries, Incidence of Reported Cases, Risk of Salmonellosis for Swedish Travelers [10], and Data From European Baseline Surveys Conducted in Laying Hens, Broilers, and Slaughter Pigs [11–13]
| Country | Serum Samples, No. | Collection Period | Material | Estimated Seroincidence (Infections/Person-Year) (95% CI) | Reported Culture-Confirmed Cases, No./100 000 Population | Risk Per 100 000 Swedish Travelers | Laying Hen Holding Prevalence (2004–2005), % | Broiler Flock Prevalence (2005–2006), % | Prevalence in Slaughter Pigs (2006–2007), % |
|---|---|---|---|---|---|---|---|---|---|
| Austria | 219 | 2012 | Leftover sera | 0.119 (.028–.186) | 17.1 | 12.0 | 15.4 | 5.4 | 2 |
| Denmark | 1780 | 2006–2007 | Community-based study | 0.078 (.020–.139) | 30.7 | 3.8 | 2.7 | 1.6 | 7.7 |
| England | 500 | 2010 | Leftover sera | 0.095 (.028–.186) | 18.7 | 5.6 | 11.9 | 8.2 | 21.2 |
| Finland | 500 | 2000–2001 | Subsamples of serum banks | 0.071 (.020–.139) | 50.5 | 0.4 | 0.4 | 0.1 | 0 |
| France | 1010 | 2003–2004 | Routine free health checks | 0.387 (.296–.486) | 10 | 8.4 | 17.2 | 6.2 | 18.1 |
| Greece | 500 | 2011 | Blood donors and relatives of patients | 0.205 (.111–.317) | 4.2 | 39.2 | 49.3 | 24 | 24.8 |
| Ireland | 500 | 2009 | Pregnancy serum samples | 0.16 (.077–.258) | 7.5 | 3.2 | 1.4 | 27.6 | 16.1 |
| Italy | 516 | 2003–2004 | Persons consulting health service | 0.223 (.124–.344) | 11.1 | 12.8 | 29.2 | 28.3 | 16.5 |
| The Netherlands | 1065 | 1998–2002 | Subsamples of serum banks | 0.164 (.098–.239) | 20.6 | … | … | … | … |
| The Netherlands | 1053 | 2006–2007 | Subsamples of serum banks | 0.147 (.091–.212) | 15.7 | 4.6 | 15.4 | 7.5 | 8.5 |
| Poland | 500 | 2004 | Persons consulting health service | 0.549 (.382–.735) | 41.8 | 76.5 | 76.2 | 58.2 | 5.1 |
| Romania | 509 | 2007 | Persons consulting district medical service (nongastroenteritis) | 0.357 (.229–.502) | 2.9 | 68.9 | … | … | … |
| Spain | 500 | 2012 | Healthy population in Valencia region | 0.608 (.435–.798) | 32.5 | 72.0 | 73.2 | 41.2 | 29 |
| Sweden | 525 | 2007–2008 | Subsamples of serum banks | 0.056 (.011–.119) | 43.1 | … | 0 | 0 | 1.3 |
Abbreviation: CI, confidence interval.
England
The seroepidemiology program of Public Health England is based on a large collection of serum samples approximating the general population of England and Wales. Serum samples included are anonymized residues of specimens submitted for diagnostic testing. For this study, 500 serum samples collected during 2010 were selected, with 90 samples from each of 5 age groups (18–28, 29–38, 39–48, 49–58, and 59–68 years) and 50 samples from individuals aged >68 years. Within each age range, the samples were selected randomly.
Austria
The samples were collected from a single Austrian province, selected among all samples forwarded to one serological/virological institute. They were from adult patients without enteric or neurological symptoms (for example, patients with respiratory symptoms).
Greece
A total of 500 serum samples from blood donors or relatives of patients were included; they originated from 5 laboratories representing 5 regions: Athens, Thessaloniki, Ioannina, Larissa, and Alexandroupoli. These laboratories are spread across the country and are representative of the Greek blood donor population. Blood donors are aged 18–65 years and represent the healthiest part of the general population. About 80% of donors give blood repeatedly, and 20% are first-time donors.
Ireland
In Ireland, all pregnant women have a blood sample taken at antenatal consultation. From the entire blood bank collection, 500 serum samples were collected, including 50 serum samples each from women aged <20 and >44 years. In addition, 80 serum samples were selected from each of the following age ranges: 20–24, 25–29, 30–34, 35–39, and 40–44 years. Within each age range, the serum samples were selected at random.
Spain
The CSISP (Centro Superior de Investigación en Salud Pública) Biobank was established as a repository of biological samples (blood, serum, and DNA), representing the healthy population in the Valencia region. From this serum collection, 500 serum samples collected during 2012 were selected, with 90 samples from each of 5 age groups (18–28, 29–38, 39–48, 49–58, and 59–68 years) and 50 from individuals aged >68 years. Within each age group, the serum samples were selected randomly. All serum samples were analyzed at Statens Serum Institut using a mix ELISA with lipopolysaccharide from Salmonella serotypes Enteritidis and Typhimurium as the catching antigen, as described elsewhere [8, 9].
External Data for Reference
Data on the official reported incidence of culture-confirmed cases of human infections with Salmonella were obtained from the joint reports of the European Food Safety Authority and the European Centre for Disease Prevention and Control (available at: http://www.efsa.europa.eu/). Data were used from the years in which collections of serum samples were started, (eg, data from Denmark were from 2006). In 2004–2005, the European Food Safety Agency (EFSA) conducted a baseline survey using a standardized method to assess the prevalence of Salmonella in holdings of laying hens in the European Union [11]. Similarly, data on Salmonella in broiler flocks were obtained in 2005–2006 [12]. Finally, the prevalence of Salmonella in slaughter pigs was determined by testing carcasses for Salmonella in lymph nodes in 2006–2007 [13].
In 2006, de Jong and Ekdahl [10] published a study where they used the risk of Salmonella infections in returning Swedish travelers to compare the disease burden in different European countries. They combined data from the Swedish database on notifiable communicable disease with data on frequency of foreign travel of Swedish residents obtained from telephone surveys in Sweden.
We used the Spearman rank correlation coefficient (Spearman ρ), a nonparametric measure, to examine the correlation between the estimated seroincidence and the external reference data (ie, officially reported incidences of human salmonellosis, risk per 100 000 Swedish travelers, and the data from the EFSA baseline surveys). Romania did not participate in the EFSA baseline surveys and was excluded from the assessment of the correlation with data from food animals.
RESULTS
The annual seroincidence of Salmonella ranged from 0.056 infections per person-year in Sweden to 0.61 in Spain. The 3 Nordic counties had comparably low incidences, whereas estimates obtained from the Netherlands, England, Austria, and Ireland ranged from 0.095 to 0.164. Estimates from Greece, Italy, Romania, France, Poland, and Spain ranged from 0.20 to 0.61 (Table 1).
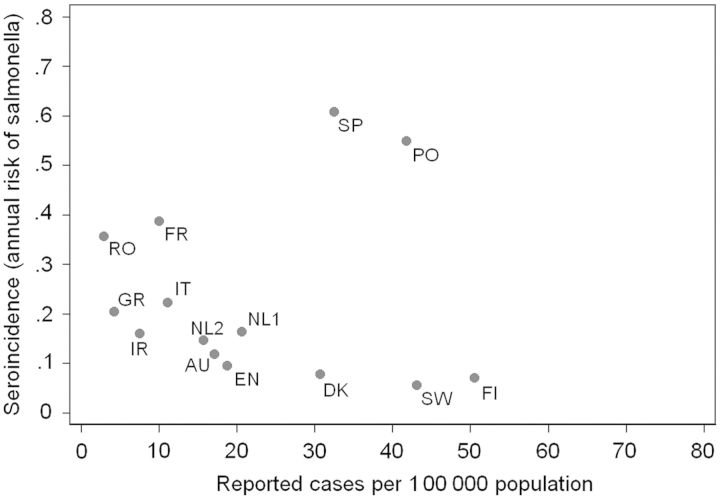
Figure 1 shows the seroincidence estimates plotted against the officially reported numbers of culture-confirmed infections. There was no significant correlation between these 2 parameters; if anything, there was a tendency toward an inverse correlation (Spearman ρ = −0.37; P = .20). Outliers were Spain and Poland. We found a high seroincidence in these 2 countries, which also report a relative high incidence of culture-confirmed cases.
Figure 1.
Salmonella seroincidence and the incidence of culture-confirmed cases reported to the European Union. Each point represents 1 country that took part in the study, except that the Netherlands is represented by 2 serum collections (1998–2002 [NL1] and 2006–2007 [NL2]) (Spearman ρ = −0.367; P = .20). Abbreviations: AU, Austria; DK, Denmark; EN, England; FI, Finland; FR, France; GR, Greece; IR, Ireland; IT, Italy; PO, Poland; RO, Romania; SP, Spain; SW, Sweden.
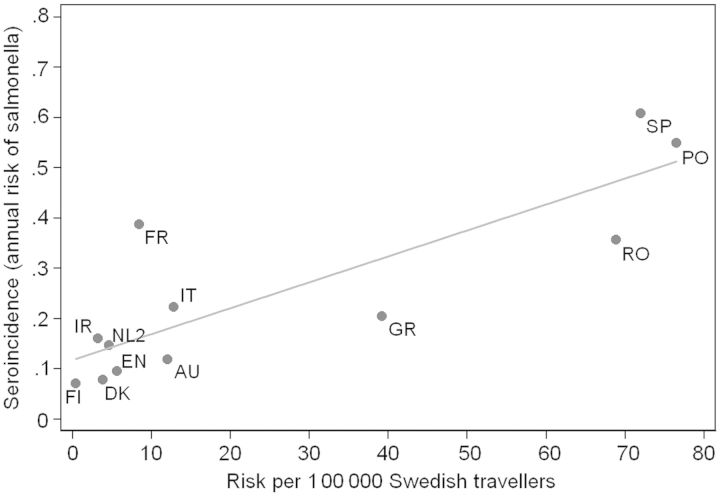
The seroincidence correlated with the risk of Salmonella infection in returning Swedish travelers (Figure 2). Spain, Poland, and Romania all had high estimates of seroincidence as well as a high risk of detecting a travel-associated Salmonella infection among residents of Sweden. France was an outlier with a relatively high seroincidence but a relative low risk of travel-associated Salmonella infections.
Figure 2.
Salmonella seroincidence and risk of Salmonella infection in Swedish travelers [10]. Each point represents 1 of 12 European countries (excluding Sweden and the Netherlands in 1998–2002) (Spearman ρ = 0.811; P = .001). Abbreviations: AU, Austria; DK, Denmark; EN, England; FI, Finland; FR, France; GR, Greece; IR, Ireland; IT, Italy; NL2, the Netherlands (2006–2007); PO, Poland; RO, Romania; SP, Spain.
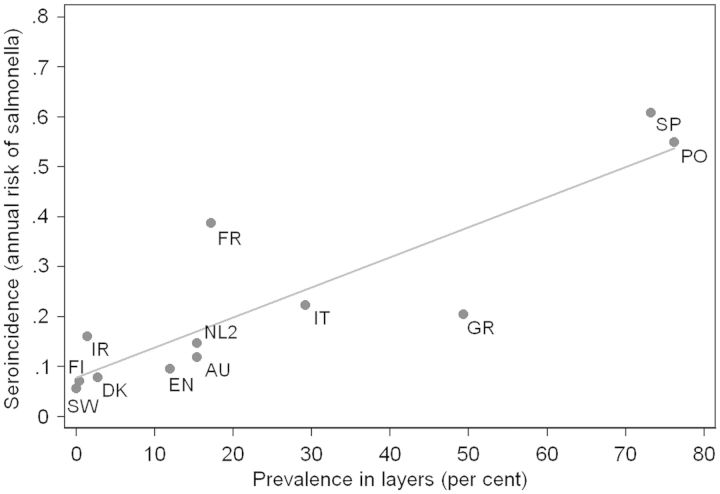
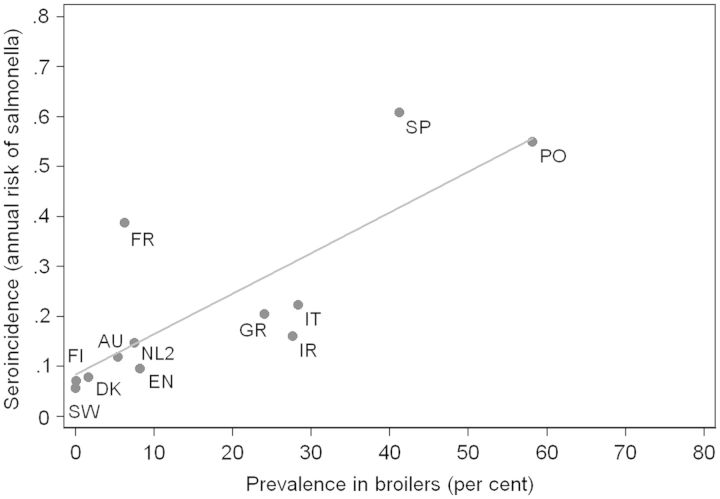
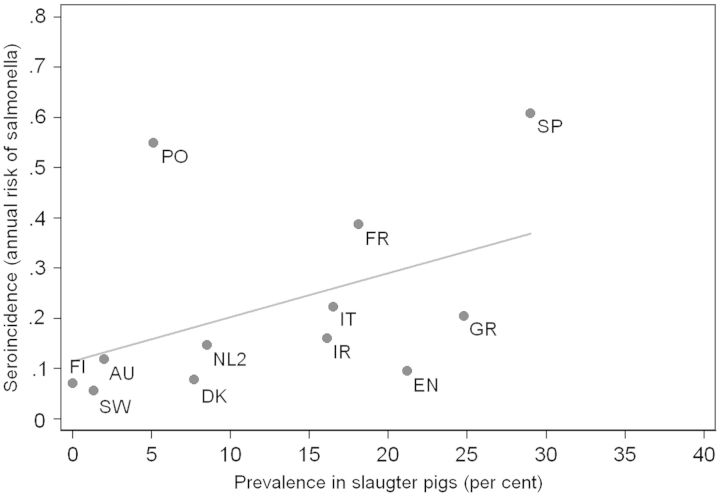
The seroincidence was strongly correlated with the observed prevalence of Salmonella-positive holdings of laying hens (Spearman ρ = 0.89; Figure 3). France seemed to be an outlier with a somehow higher seroincidence than predicted from the prevalence in laying hens alone, whereas Greece had a lower seroincidence. There was also a significant correlation with the prevalence of Salmonella in broiler flocks (Figure 4). France and Spain seemed to have a higher seroincidence in humans than could be predicted from the prevalence in broilers alone. Finally, Figure 5 shows that the seroincidence also correlated with the prevalence of Salmonella in slaughter pigs. Poland had a higher seroincidence than could be predicted from the prevalence in pigs alone, whereas England had low seroincidence in spite of a high prevalence of Salmonella in pigs (21%).
Figure 3.
Salmonella seroincidence and the observed prevalence of Salmonella-positive holdings of laying hens in 12 European countries [11]. Each point represents 1 country (excluding Romania and the Netherlands in 1998–2002) (Spearman ρ = 0.893; P = .001). Abbreviations: AU, Austria; DK, Denmark; EN, England; FI, Finland; FR, France; GR, Greece; IR, Ireland; IT, Italy; NL2, the Netherlands (2006–2007); PO, Poland; SP, Spain; SW, Sweden.
Figure 4.
Salmonella seroincidence and the observed prevalence of Salmonella-positive holdings of broilers in 12 European countries [12]. Each point represents 1 country (excluding Romania and the Netherlands in 1998–2002) (Spearman ρ = 0.853; P = .004). Abbreviations: AU, Austria; DK, Denmark; EN, England; FI, Finland; FR, France; GR, Greece; IR, Ireland; IT, Italy; NL2, the Netherlands (2006–2007); PO, Poland; SP, Spain; SW, Sweden.
Figure 5.
Salmonella seroincidence and the observed prevalence of slaughter pigs infected with Salmonella in lymph nodes [13]. Each point represents 1 country (excluding Romania and the Netherlands in 1998–2002) (Spearman ρ = 0.629; P = .03). Abbreviations: AU, Austria; DK, Denmark; EN, England; FI, Finland; FR, France; GR, Greece; IR, Ireland; IT, Italy; NL2, the Netherlands (2006–2007); PO, Poland; SP, Spain; SW, Sweden.
DISCUSSION
There are considerable differences in the incidence of reported nontyphoid Salmonella infections in Europe, ranging in the present study from 2.9 per 100 000 population in Romania to 50.5 in Finland (Table 1). A pilot study indicated that these differences reflect the attributes of the surveillance pyramid rather than a true difference in the incidence of Salmonella infections [9]. In the present article, we describe our expansion of this study to include 13 countries representing a large part of the European Union. We found a 10-fold difference in the annual incidence of infections when comparing estimates from Spain and Poland with those from the Nordic countries where extensive Salmonella control programs in food animals have been established [14–16]. These findings are well in line with Finnish risk assessment models, wherein a scenario of 5 positive parent flocks was estimated to cause a 4.9–11.7-fold increase of human cases [14], but they are in striking contrast to reported incidences of Salmonella infections. If anything, there was a tendency toward an inverse correlation, which could indicate that case ascertainment and public health surveillance is more comprehensive in countries with a longer tradition and focus on Salmonella control. The data are indicative of major differences in Salmonella surveillance systems between European countries. Official numbers are misleading and cannot be used to compare the actual infection risk between countries. The data underscore the need to build a strong public health microbiology infrastructure in Europe and harmonize surveillance for food-borne bacteria, including nontyphoid Salmonella.
To validate our findings, we compared the seroincidence estimates with results from other studies that were independent of the sensitivity of public health surveillance. Although the serum samples were collected from 2000 to 2012, the seroincidence correlated very well with Salmonella prevalence in food animals [11–13] and with the risk of Salmonella infection in Swedish travelers returning from the respective countries [10]. The correlation was strongest with the prevalence in laying hens; this is not surprising, because eggs are an important cause of Salmonella infections in humans. Furthermore, there is extensive trade with meat from broilers and pork, whereas eggs usually are domestic owing to minor differences in production costs between European Union member states and logistical difficulties in trading shelled eggs [15]. In other words, trade of meat may dilute the associations. For example, England had a lower seroincidence than predicted from the prevalence of Salmonella in pork, which might be related to the fact that a large share of the pork in the United Kingdom is imported from countries with a lower prevalence of Salmonella in pork. National differences in cooking and consumption practices may play a role, which is difficult to quantify.
Based on the striking correlations, we propose that seroepidemiology is well suited to evaluate the impact of Salmonella control programs in food animals on the Salmonella incidence in the human population. This novel method is an objective way of comparing the force of transmission, that is, the rate at which humans (independent of the clinical outcome of the infection) acquire salmonellosis, between different countries and over time. The tool is independent of the artifacts and biases in passive laboratory-based public health surveillance. This point is well illustrated by our data, showing low seroincidence in countries that established Salmonella control programs many years ago, such as Finland and Sweden, which have received a special permission from the European Union to implement stricter Salmonella control measures than regulated by the European Zoonoses Directive [17, 18].
The Netherlands provided 2 data sets. Over time, the seroincidence decreased by 10%, whereas the incidence of notified cases declined by 23% from 1998 to 2006, albeit with large confidence intervals (Table 1). A previous study in Denmark, using serum collections from 1983, 1986, 1992, and 1999, showed that the seroincidence of Salmonella increased almost parallel to the rise in culture-confirmed cases, owing to the emergence of Salmonella Enteritidis [19]. These tendencies support the usefulness of seroepidemiology for monitoring changes in the force of transmission.
Our study is subject to a number of limitations. Seroincidence is not a measure of clinical illness and does as such not measure the actual burden of illness. It is rather an attempt to measure the frequency of exposures to Salmonella that are recognized by the immune system and followed by antibody response. We do not know how many of the seroincident infections are cases with clinical disease. The disease-to-infection ratio may differ between populations, and there may be a nonlinear correlation between estimated seroincidence and disease-to-infection ratio owing to (partial) immunity. A 10-fold difference in seroincidence between Sweden and Spain, in other words, does not necessarily pan out as a 10-fold difference in burden of illness. Further studies should explore these matters. Nonetheless, it is worth noticing that the actual magnitudes of the seroincidence estimates are much higher than community estimates of salmonellosis incidence derived from studies analyzing the various steps of the surveillance pyramid and from prospective population cohort studies [20–26]. It is therefore possible that Salmonella infections, whether symptomatic or asymptomatic, are common events in industrialized countries. This notion is corroborated by a review suggesting that asymptomatic fecal shedding of Salmonella was common in the United States in the 1980s [27].
Although we aimed to include serum samples from representative community serosurveys, this proved difficult. The samples obtained represent different compromises to some degree and may introduce biases. Studies exploring to what extent the inclusion serum samples from blood donors or pregnant women or residual sera from patients with no gastrointestinal disease provide seroincidence estimates similar to those from the general population are warranted. Results from such studies will help in the design of practical sampling plans, allowing the use of seroepidemiology as a routine tool to monitor the impact of control programs for Salmonella (or other pathogens).
We estimated seroincidence based on the antibody decay profile determined in a longitudinal study of Danish patients with culture-confirmed Salmonella gastroenteritis [8]. It is conceivable that the decay profile is different in a high-incidence country and that this introduces uncertainty in the model. Ideally, such follow-up studies should be repeated in settings with different levels of endemicity. Furthermore, for practical and ethical reasons, we did not attempt to obtain serum samples from children to determine antibody decay in this age group, so it was not meaningful to include children in the cross-sectional data. However, a high proportion of the reported cases of culture-confirmed Salmonella infections are in children, and it is therefore of interest to estimate the seroincidence and the disease-to-infection ratio in child populations as well. Furthermore, inclusion of the elderly varied between countries. Elderly person are at increased risk for nontyphoid Salmonella infections, which could affect the differences in incidence data. Nonetheless, we do not regard this issue as a major limitation in the application of seroepidemiology as a tool to measure the force of infection in a population as a whole.
Although commercial immunoassays are available to detect subunit antigens for Salmonella Typhi, there is no international consensus on similar tests for nontyphoid salmonellosis. We developed and validated an in-house ELISA [8, 28], and methodological variations were not an issue because all tests were run in the same laboratory and included the same controls. The ELISA was based on antigens from serotypes Enteritidis (serogroup D1) and Typhimurium (serogroup B). These 2 serotypes represent 70% of human Salmonella infections in the European Union. Cross-reactions to related serotypes within group B and D are expected, whereas the ability to detect seroresponse to more distantly related serotypes have not been examined.
Without ignoring the limitations, we suggest that estimates of Salmonella infection incidence based on the seroepidemiological method are better suited than reported numbers of culture-confirmed cases to measure the force of infection at the population level and thus to monitor the effect of Salmonella control programs. This is particularly relevant for international assessments, which include areas or countries with diverse characteristics of the Salmonella surveillance pyramids.
The United States also has regional variations in the reported incidence of human Salmonella cases. FoodNet was established as a network for the active surveillance of food-borne infections, including Salmonella infections. It was originally based on surveillance in 5 sites, but later more states and sites were included, and differences in the baseline incidence of Salmonella infection became evident [3, 4]. It is not understood to which extent the difference in baseline incidence reflects a surveillance artifact due to differences in the surveillance pyramid, or whether it reflects true differences in the incidence of salmonellosis [4]. Seroepidemiological studies may provide more insights into these differences.
Notes
Acknowledgments. We thank the following persons for excellent collaboration over many years and for assistance in providing access to serum sample collections: Wilfrid van Pelt, Peter Teunis, and Yvonne T. H. P. van Duynhoven, Centre for Infectious Disease Control, National Institute for Public Health and the Environment, Bilthoven, the Netherlands; Sandra Jelovcan, Austrian Agency for Health and Food Safety, Institute for Medical Microbiology and Hygiene–Centre for Food-Related Infectious Diseases, Graz, Austria; Allan Linneberg, Research Centre for Prevention and Health, Glostrup, Denmark; Richard Pebody, Public Health England, Colindale, London, United Kingdom; Markku Kuusi, National Institute for Health and Welfare, Helsinki, Finland; Henriette de Valk, Infectious Diseases Department, Institut de Veille Sanitaire, Saint Maurice, France; Kassiani Mellou, Department of Epidemiological Surveillance and Intervention, Center of Disease Control, Attica, Greece; Martin Cormican, University College Hospital, Galway, Ireland; Maria Cristiana Rota, Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute, Istituto Superiore di Sanità, Roma, Italy; Malgorzata Sadowska-Todys, Department of Epidemiology, National Institute of Public Health–National Institute of Hygiene, Warsaw, Poland; Lavinia Zota, National Center for Surveillance and Control of Communicable Diseases, National Institute of Public Health, Bucharest, Romania; Jacobo Martínez, Centro Superior de Investigación en Salud Pública Biobank, Valencia, Spain; Cecilia Jernberg, Public Health Agency of Sweden, Solna; and Andrea Ammon, European Centre for Disease Prevention and Control, Stockholm, Sweden. We also acknowledge the contributions of Katrin Kuhn, Mette Strid, Bjørn Kantsø, Tina H. Ceper, and Daniel Silla Jatta, from the Division of Microbiological Diagnostics and Infection Control, Statens Serum Institut, Copenhagen, Denmark.
Financial support. This work was cofunded by Med-Vet-Net, a “Network of Excellence” for research on the prevention and control of zoonoses, funded by the European Commission within the Sixth Framework Programme (contract 506122) and by the European Centre for Disease Control and Prevention (project OJ/2009/06/03-PROC/2009/021).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Eurosurveillance editorial team. The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2011 has been published. Euro Surveill. 2013;18 20449. [PubMed] [Google Scholar]
- 2.O'Brien SJ. The “decline and fall” of nontyphoidal Salmonella in the United Kingdom. Clin Infect Dis. 2013;56:705–10. doi: 10.1093/cid/cis967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Incidence and trends of infection with pathogens transmitted commonly through food—Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 1996–2012. Morb Mortal Wkly Rep MMWR. 2013;62:283–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Hardnett FP, Hoekstra RM, Kennedy M, Charles L, Angulo FJ. Epidemiological issues in study design and data analysis related to FoodNet activities. Clin Infect Dis. 2004;38(suppl 3):S121–6. doi: 10.1086/381602. [DOI] [PubMed] [Google Scholar]
- 5.Simonsen J, Mølbak K, Falkenhorst G, Krogfelt KA, Linneberg A, Teunis PFM. Estimation of incidences of infectious diseases based on antibody measurements. Stat Med. 2009;28:1882–95. doi: 10.1002/sim.3592. [DOI] [PubMed] [Google Scholar]
- 6.Simonsen J, Teunis P, Van Pelt W, et al. Usefulness of seroconversion rates for comparing infection pressures between countries. Epidemiol Infect. 2011;139:636–43. doi: 10.1017/S0950268810000750. [DOI] [PubMed] [Google Scholar]
- 7.Teunis PFM, Van Eijkeren JCH, Ang CW, et al. Biomarker dynamics: estimating infection rates from serological data. Stat Med. 2012;31:2240–8. doi: 10.1002/sim.5322. [DOI] [PubMed] [Google Scholar]
- 8.Falkenhorst G, Ceper TH, Strid MA, Mølbak K, Krogfelt KA. Serological follow-up after non-typhoid Salmonella infection in humans using a mixed lipopolysaccharide ELISA. Int J Med Microbiol. 2013;303:533–8. doi: 10.1016/j.ijmm.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Falkenhorst G, Simonsen J, Ceper TH, et al. Serological cross-sectional studies on Salmonella incidence in eight European countries: no correlation with incidence of reported cases. BMC Public Health. 2012;12:523. doi: 10.1186/1471-2458-12-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Jong B, Ekdahl K. The comparative burden of salmonellosis in the European Union member states, associated and candidate countries. BMC Public Health. 2006;6:1–9. doi: 10.1186/1471-2458-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Report of the Task Force on Zoonoses Data Collection on the analysis of the baseline study on the prevalence of Salmonella in holdings of laying hen flocks of Gallus gallus . EFSA J. 2007 97:1–84. [Google Scholar]
- 12.Report of the Task Force on Zoonoses Data Collection on the analysis of the baseline survey on the prevalence of Salmonella in broiler flocks of Gallus gallus, Part A. EFSA J. 2007;98:1–85. [Google Scholar]
- 13.Report of the Task Force on Zoonoses Data Collection on the analysis of the baseline study on the prevalence of Salmonella in slaughter pigs, in the EU, 2006-2007. Part A: Salmonella prevalence estimates. EFSA J. 2008;135:1–111. [Google Scholar]
- 14.Maijala R, Ranta J, Seuna E, Peltola J. The efficiency of the Finnish Salmonella control programme. Food Control. 2005;16:669–75. [Google Scholar]
- 15.Health poultry. Report from the project “Development of new integrated strategies for prevention, control and monitoring of epizootic poultry diseases.”. Available at: http://www.healthy-poultry.org/ Accessed 14 August 2014.
- 16.Wegener HC, Hald T, Lo Fo Wong D, et al. Salmonella control programs in Denmark. Emerg Infect Dis. 2003;9:774–80. doi: 10.3201/eid0907.030024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Regulation (EC) No 1688/2005 of 14 October 2005 implementing Regulation (EC) No 853/2004 of the European Parliament and of the Council as regards special guarantees concerning Salmonella for consignments to Finland and Sweden of certain meat and eggs. Official J European Union. 2005 L 271:17–28. [Google Scholar]
- 18.Directive 2003/99/EC of the European Parliament and of the Council of 17 November 2003 on the monitoring of zoonoses and zoonotic agents, amending Council Decision 90/424/EEC and repealing Council Directive 92/117/EEC. Official J European Union. 2003 L 325:31–40. [Google Scholar]
- 19.Simonsen J, Strid MA, Mølbak K, Krogfelt KA, Linneberg A, Teunis P. Sero-epidemiology as a tool to study the incidence of Salmonella infections in humans. Epidemiology Infect. 2008;136:895–902. doi: 10.1017/S0950268807009314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas MK, Majowicz SE, Sockett PN, et al. Estimated numbers of community cases of illness due to Salmonella, Campylobacter and verotoxigenic Escherichia coli: pathogen-specific community rates. Can J Infect Dis Med Microbiol. 2006;17:229–34. doi: 10.1155/2006/806874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall G, Yohannes K, Raupach J, Becker N, Kirk M. Estimating community incidence of Salmonella, Campylobacter, and Shiga toxin-producing Escherichia coli infections, Australia. Emerg Infect Dis. 2008;14:1601–9. doi: 10.3201/eid1410.071042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis. 2011;17:7–15. doi: 10.3201/eid1701.P11101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wheeler JG, Sethi D, Cowden JM, et al. Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance. BMJ. 1999;318:1046–50. doi: 10.1136/bmj.318.7190.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Wit MA, Koopmans MP, Kortbeek LM, et al. Sensor, a population-based cohort study on gastroenteritis in the Netherlands: incidence and etiology. Am J Epidemiol. 2001;154:666–74. doi: 10.1093/aje/154.7.666. [DOI] [PubMed] [Google Scholar]
- 25.Tam CC, Rodrigues LC, Viviani L, et al. IID2 Study Executive Committee. Longitudinal study of infectious intestinal disease in the UK (IID2 study): incidence in the community and presenting to general practice. Gut. 2012;61:69–77. doi: 10.1136/gut.2011.238386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kemmeren JM, Mangen MJ, van Duynhoven YT, Havelaar AH. Priority setting of foodborne pathogens. Bilthoven, the Netherlands: National Institute for Public Health and the Environment; 2006:55–7. Report 33008001/2006. [Google Scholar]
- 27.Chalker RB, Blaser MJ. A review of human salmonellosis: III. Magnitude of Salmonella infection in the United States. Rev Infect Dis. 1988;10:111–24. doi: 10.1093/clinids/10.1.111. [DOI] [PubMed] [Google Scholar]
- 28.Kuhn KG, Falkenhorst G, Ceper TH, et al. Detecting non-typhoid Salmonella in humans by ELISAs: a literature review. J Med Microbiol. 2012;61:1–7. doi: 10.1099/jmm.0.034447-0. [DOI] [PubMed] [Google Scholar]