Abstract
Progressive multifocal leukoencephalopathy is a currently untreatable infection of the brain. Here, we demonstrate in 2 patients that treatment with interleukin 7, JC polyomavirus (JCV) capsid protein VP1, and a Toll-like receptor 7 agonist used as adjuvant, was well tolerated, and showed a very favorable safety profile and unexpected efficacy that warrant further investigation.
Keywords: progressive multifocal leukoencephalopathy, JC virus, IL-7, VP1
Progressive multifocal leukoencephalopathy (PML) is a life-threatening opportunistic infection of the brain caused by JC polyomavirus (JCV) [1] that occurs in various states of immunosuppression. The occurrence of PML in conditions of decreased CD4+ T-cell numbers or function with resolution following their restoration [2] and immunological studies from brain-infiltrating T-cells [3] strongly support the importance of these immune cells in controlling JCV infection. JCV-specific CD8+ cytotoxic T-cells also play an important role in controlling this infection and have been linked to recovery from PML [4]. The role of antibodies is less clear, as they are frequently present before and at onset of PML [5]. Currently, there is no specific antiviral or other drug to treat PML, and the only option is to restore protective immunity. The hematopoietic growth factor interleukin 7 (IL-7) is crucial for homeostatic T-cell proliferation [6] and restores T-cell function, including virus-specific immunity [7]. Because vaccines induce antigen-specific immune responses, we reasoned that a therapeutic vaccine against JCV along with IL-7 treatment for general immune restoration might be effective by preferentially expanding JCV-specific CD4+ T-cells over other specificities. We have treated 2 PML patients, who suffered from hereditary or acquired immunocompromise, with 3 subcutaneous injections of recombinant human IL-7 (rhIL-7 [CYT107]) and a therapeutic vaccine consisting of JCV VP1 protein in combination with a topically administered Toll-like receptor 7 (TLR7) agonist as adjuvant [8], and report the results herein.
METHODS
Ethics Statement
Both patients received the above-mentioned treatment as “Compassionate Use,” which refers to use of a nonapproved drug or biological/chemical compound outside the framework of a clinical trial. The physician acts here in the scope of her/his medical license and takes complete responsibility for the prescribed therapy. When using a nonapproved medication, the patient must be adequately informed and special authorization at the local Agency for Therapeutic Products obtained. Both patients were treated in full compliance with regulatory requirements in Germany and Switzerland. Patients and relatives were informed of the risks of the treatment, including death from PML immune reconstitution inflammatory syndrome (IRIS), and signed an informed consent.
Patients
Clinical information and neuroimaging (magnetic resonance imaging [MRI]), virological, and immunological findings are summarized in Supplementary Table 1. Both patients significantly deteriorated during the 12 months between diagnosis and treatment, and cerebrospinal fluid (CSF) JCV DNA remained positive during this time. Both patients were uninfected with human immunodeficiency virus (HIV).
Treatment Regimen and Follow-up
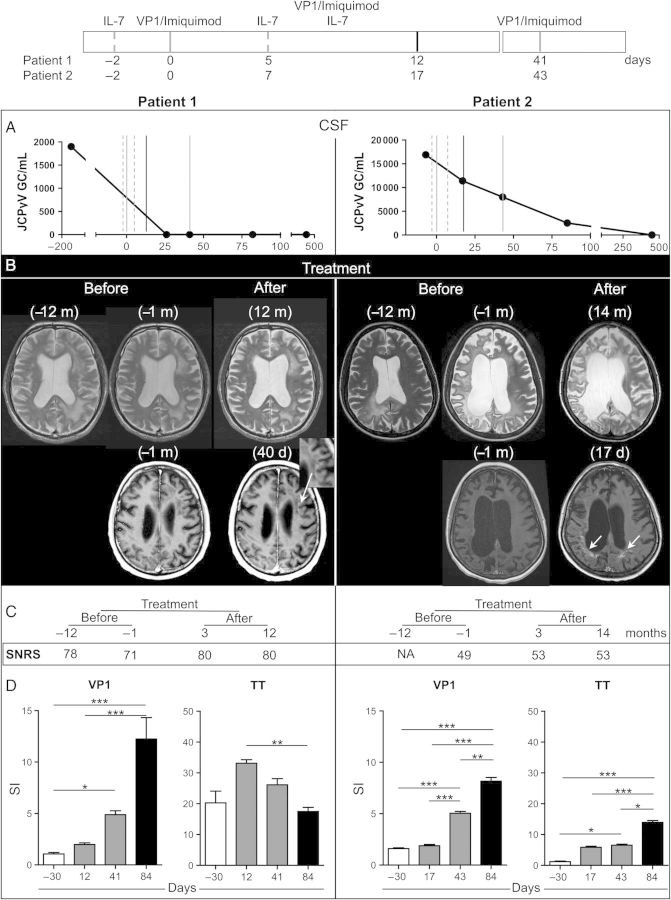
Patients were treated with 3 subcutaneous injections of glycosylated rhIL-7, 10 µg/kg body weight (CYT107, Cytheris S.A., Paris, France), 3 subcutaneous injections of 1 mg of recombinant JCV VP1 protein (Life Science Inkubator, Bonn, Germany), and topical imiquimod cream at the subcutaneous injection site (5%, Aldara, MEDA Pharm, Germany); a TLR7/8 agonist was used as adjuvant [8]. The treatment protocol is summarized in Figure 1.
Figure 1.
Treatment protocol (upper scheme). Dotted gray lines represent time points of recombinant human interleukin 7 (rhIL-7) injection (patient 1: days –2 and 5; patient 2: days –2 and 7), solid gray lines represent time points of VP1 injection in combination with imiquimod (patient 1: days 0 and 41; patient 2: days 0 and 43), and black solid line represents simultaneous injection of VP1 and rhIL-7 in combination with imiquimod (patient 1: day 12; patient 2: day 17). Day 0 is the day of the first VP1 injection. Subtle differences in schedule between the 2 patients were due to an intercurrent urinary tract infection in patient 2. A, JC polyomavirus (JCV) load in cerebrospinal fluid from patient 1 (left) and patient 2 (right), before and at different time points during and after treatment. The y-axis represents viral load expressed as viral genome copies/mL and the x-axis shows time in days. B, T2 magnetic resonance imaging (MRI) from patient 1 (left top row) and patient 2 (right top row) before treatment and 12 or 14 months after treatment. Contrast-enhanced T1W MRI in patient 1 (left bottom row) and in patient 2 (right bottom row) performed before and 40 days (patient 1) or 17 days (patient 2) after first VP1 injection. White arrows point at gadolinium contrast enhancement indicative of neuroinflammation in the areas of progressive multifocal leukoencephalopathic lesions in both patients. The inset in the image of patient 1 focuses on the bandlike gadolinium-contrast-enhancing lesion. C, Scripps neurological rating scale before treatment and 3 months and 12 or 14 months after treatment. D, JCV VP1–specific and tetanus toxoid–specific CD4+ T-cell responses before (month –1, white histograms), during (patient 1: days 12 and 41; patient 2: days 17 and 43; gray histograms), and after (day 84, black histograms) rhIL-7/JCV VP1 vaccination treatment. Proliferative responses were measured by 3H-thymidine incorporation assay. Mean ± SEM and statistical significance are shown. *P < .05, **P < .01, ***P < .001. Abbreviations: CSF, cerebrospinal fluid; GC, genome copies; IL-7, interleukin 7; JCPyV, JC polyomavirus; NA, not available; SI, stimulation index; SNRS, Scripps neurological rating scale; TT, tetanus toxoid.
Tolerability and safety were assessed by clinical and laboratory adverse events (AEs) (Institute of Clinical Chemistry, University Medical Center Hamburg-Eppendorf, and the Institute of Clinical Chemistry, Hematology, and Neurology Clinics, University Hospital Zurich). Efficacy assessment included JCV DNA load, MRI, clinical observation, and immunological testing. Cranial MRI examinations (T1 pre- and postgadolinium, proton density/T2, fluid-attenuated inversion recovery, and diffusion-weighted images) were performed at the Department of Neuroradiology, University Medical Center Hamburg-Eppendorf, and the Institute for Neuroradiology, University Hospital Zurich. The Scripps neurological rating scale (SNRS) was used to assess the clinical status (100 = normal to 0 = dead).
Quantification of JCV Viral Load
Viral load was quantified in the CSF by quantitative polymerase chain reaction of JCV T antigen as previously described [9].
Proliferative Assays
Proliferative response of peripheral blood mononuclear cells (PBMCs) against VP1 (2 µg/mL [10]) and tetanus toxoid (TT, 10 µg/mL; Novartis Behring, Marburg, Germany) was tested in a 7-day 3H-thymidine incorporation assay, and stimulatory indices were calculated as follows: [mean counts per minute with protein / mean counts per minute unstimulated wells]. Proliferation was also determined by flow cytometry using CellTrace carboxyfluorescein succinimidyl ester (CFSE) kit (Invitrogen, Darmstadt, Germany) in PBMCs seeded with VP1 protein (2 µg/mL) for 6 days, labeled with CFSE, and restimulated or not with VP1. After 5 days, cells were stained with anti-CD4 (Biolegend, San Diego, California), anti-CD3 (eBioscience, San Diego, California), anti-CD25 (Biolegend), and anti-CD45RO (Biolegend). Samples were acquired using LSR-II and LSR-Fortessa flow cytometers (BD, Franklin Lakes, New Jersey) and data analyzed using FACSDiva Software (BD).
ELISA for VP1-Specific Antibodies
VP1-specific immunoglobulin G titers in CSF/serum were determined as previously described [11]. Samples were preadsorbed with soluble BK virus VP1 to compete potentially cross-reactive antibodies. Virus-specific antibody indices (AI) were calculated as previously described [12]. AI values ≥1.5 indicate intrathecal antigen-specific antibody synthesis.
Statistical Analysis
Statistical analyses were performed with Prism 5.02 (GraphPad Software Inc, San Diego, California). Descriptive statistics are reported as mean ± SEM. Comparisons of ≥3 groups were assessed by 1-way analysis of variance with Bonferroni correction for multiple comparisons. P values <.05 were considered statistically significant.
RESULTS
Safety and Tolerability
Only patient 1 reported a mild AE (swelling and reddening at the rhIL-7 injection site). No hematological or blood chemistry abnormalities were observed, and all compounds were tolerated well.
Efficacy
A clear reduction in the CSF JCV load was observed in both patients (Figure 1A). JCV viral load testing remained negative during follow-up (12 months). Regarding MRI, no new T2 lesions were observed after treatment (Figure 1B). Contrast-enhancing lesions never occurred in either patient before treatment over a 12-month period. After treatment, we observed a subtle gadolinium-enhancing MRI lesion in patient 1, and clear enhancement in patient 2 indicative of an immune response in PML lesions (Figure 1B). Clinically, stabilization and/or amelioration of neurological findings after treatment was observed in both patients (see SNRS scores in Figure 1C). Patient 1 significantly deteriorated during the 12 months between diagnosis and treatment (SNRS score dropped from 78 to 71). At the time of treatment, he showed bilateral cerebellar signs of the lower limbs with gait ataxia and severe aphasia with leading comprehension deficits. Following treatment, he stabilized and perceptibly improved regarding cerebellar signs, speech, and cognitive functions while remaining stable during follow-up (SNRS score 80). Patient 2, who had steadily deteriorated before treatment, developing left-sided hemiplegia and becoming largely bedridden (SNRS score 49), stabilized clinically after treatment with signs of mild neuropsychological improvement regarding alertness (SNRS score 53). Finally, JCV VP1–specific CD4+ T-cell responses served as a mechanistic efficacy measure. Before treatment, PBMCs of both patients failed to respond to VP1 protein despite JCV infection. After treatment, proliferation of VP1-specific CD4+ T-cells rose significantly in both patients (Figure 1D). CFSE-labeled PBMCs from patient 1 after treatment and stimulated in vitro with VP1 confirmed that proliferating cells were mainly memory CD4+ T-cells, although CD8+ T-cell proliferation also rose (Supplementary Figure 1A). T-cell responses to the recall antigen TT were normal before treatment in patient 1 and remained unchanged at the end of treatment. In patient 2, TT-specific CD4+ T-cell responses were negative but turned positive after treatment, most likely as an effect of immune reconstitution by rhIL-7 (Figure 1D). Supporting this notion, the abnormally low CD4/CD8 ratio in both patients increased to normal levels after treatment (Supplementary Figure 1B). Intrathecal VP1-specific antibody responses were elevated before treatment in both patients and did not change after treatment (Supplementary Figure 1C).
DISCUSSION
PML is often fatal in immunocompromised patients, and there is currently no treatment. Only immune reconstitution with rhIL-7 (CYT107) represents an option based on preliminary data. Here, we performed 2 individual treatment attempts following ethical guidelines in 2 patients with PML, who suffered from hereditary or acquired CD4 lymphopenia. Although these 2 patients could be seen as not sufficiently representative as they showed a longer survival than the majority of untreated PML patients, they significantly deteriorated during the 12 months between diagnosis and treatment. Due to the often fatal outcome of PML, they were treated with subcutaneous injections of rhIL-7 (CYT107) with the aim to restore overall immune function. We have previously shown that JCV VP1–specific CD4+ T-cells are highly enriched in the brain during PML-IRIS and are probably critical for eliminating JCV from the central nervous system [3]. Because restoration of immune competence may not be sufficient to expand these JCV VP1–specific CD4+ T-cells even in the presence of JCV and VP1 in the brain, we decided to also vaccinate patients with JCV VP1 protein via an immunogenic route, that is, subcutaneously, in combination with a TLR7 agonist as adjuvant to assure boosting of VP1-specific CD4+ T-cell responses over other specificities. This PML treatment was not only well tolerated, but most importantly also appears to have long-lasting efficacy with respect to elimination of CSF JCV viral load, induction of MRI-proven inflammation at sites of PML lesions without prominent/classical PML-IRIS, and clinical stabilization with slight improvement. This efficacy means that the 2 aims of our treatment, to restore overall immune responsiveness and to boost JCV VP1–specific CD4+ T-cells, were accomplished. Immune restoration by rhIL-7 was evident in patient 2, who had a low response to the recall antigen TT and who regained responsiveness after treatment. Along this line, the peripheral CD4/CD8 ratio was also normalized after treatment in both patients. Furthermore, CD4+ JCV VP1–specific T-cell responses increased significantly, from previously negative in both patients. Despite these encouraging results, additional investigation of treatment efficacy in PML patients with more severe immunocompromise is warranted to discern the relative contribution of each compound and the putative role of VP1-specific CD8+ T-cells. Furthermore, although this therapeutic approach is not suitable for patients with HIV or with monoclonal antibody treatment–associated PML, in whom immune reconstitution is not the limiting factor, we believe that HIV patients or patients who will start on or are already treated with therapies that pose the risk of PML might benefit from a prophylactic vaccination with VP1.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online (http://cid.oxfordjournals.org). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. We thank Björn Zörner and Nikolai Pfender for assistance in clinical management, Brenda Reinhart for carefully reading the manuscript, and Magdalena Foege for preparation of regulatory documents, all at Neuroimmunology and Multiple Sclerosis Research, Department of Neurology, University of Zurich.
Financial support. The Institute for Neuroimmunology and Clinical Multiple Sclerosis Research was supported by the Gemeinnützige Hertie Stiftung. The Section of Neuroimmunology and Multiple Sclerosis Research is supported by the Clinical Research Priority Program on Multiple Sclerosis of the University of Zurich.
Potential conflicts of interest. T. C. is an employee of Cytheris, which produces rhIL-7 (CYT107). M. S., S. Y., I. J., S. S., and R. M. are coinventors of a patent application held by the University of Zurich. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Tan CS, Koralnik IJ. Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis. Lancet Neurol. 2010;9:425–37. doi: 10.1016/S1474-4422(10)70040-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cinque P, Pierotti C, Vigano MG, et al. The good and evil of HAART in HIV-related progressive multifocal leukoencephalopathy. J Neurovirol. 2001;7:358–63. doi: 10.1080/13550280152537247. [DOI] [PubMed] [Google Scholar]
- 3.Aly L, Yousef S, Schippling S, et al. Central role of JC virus-specific CD4+ lymphocytes in progressive multi-focal leucoencephalopathy-immune reconstitution inflammatory syndrome. Brain. 2011;134(pt 9):2687–702. doi: 10.1093/brain/awr206. [DOI] [PubMed] [Google Scholar]
- 4.Gheuens S, Bord E, Kesari S, et al. Role of CD4+ and CD8+ T-cell responses against JC virus in the outcome of patients with progressive multifocal leukoencephalopathy (PML) and PML with immune reconstitution inflammatory syndrome. J Virol. 2011;85:7256–63. doi: 10.1128/JVI.02506-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorelik L, Lerner M, Bixler S, et al. Anti-JC virus antibodies: implications for PML risk stratification. Ann Neurol. 2010;68:295–303. doi: 10.1002/ana.22128. [DOI] [PubMed] [Google Scholar]
- 6.Mackall CL, Fry TJ, Gress RE. Harnessing the biology of IL-7 for therapeutic application. Nat Rev Immunol. 2011;5:330–42. doi: 10.1038/nri2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pellegrini M, Calzascia T, Toe JG, et al. IL-7 engages multiple mechanisms to overcome chronic viral infection and limit organ pathology. Cell. 2011;144:601–13. doi: 10.1016/j.cell.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Feyeraband S, Stevanovic S, Gouttefangeas C, et al. Novel multi-peptide vaccination in HLA-A2+ hormone sensitive patients with biochemical relapse of prostate cancer. Prostate. 2009;69:917–27. doi: 10.1002/pros.20941. [DOI] [PubMed] [Google Scholar]
- 9.Pal A, Sirota L, Maudru T, Peden K, Lewis AM. Real-time quantitative PCR assays for the detection of virus-specific DNA in samples with mixed populations of polyomaviruses. J Virol Methods. 2006;135:32–42. doi: 10.1016/j.jviromet.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 10.Goldmann C, Petry H, Frye S, et al. Molecular cloning and expression of major structural protein VP1 of the human polyomavirus JC virus: formation of virus-like particles useful for immunological and therapeutic studies. J Virol. 1999;73:4465–9. doi: 10.1128/jvi.73.5.4465-4469.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weber T, Trebst C, Frye S, et al. Analysis of the systemic and intrathecal humoral immune response in progressive multifocal leukoencephalopathy. J Infect Dis. 1997;176:250–4. doi: 10.1086/514032. [DOI] [PubMed] [Google Scholar]
- 12.Reiber H, Lange P. Quantification of virus-specific antibodies in cerebrospinal fluid and serum: sensitive and specific detection of antibody synthesis in brain. Clin Chem. 1991;37:1153–60. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.