Abstract
Background
Diabetes is the seventh leading cause of death in the United States and disproportionately affects racial and ethnic minorities. These disparities persist despite educational efforts to reduce the prevalence of diabetes. Receptiveness of educational efforts for Black men needs to be studied.
Objective
This study assesses Black men’s receptiveness to a barbershop-based program focused on diabetes prevention and awareness in a church-affiliated barbershop in Rochester, Minnesota.
Methods
The pastor and barber of a church-affiliated barbershop and academic medical researchers designed a community-engaged research study to determine Black men’s perception of diabetes. Recruitment for the 90-minute focus group included flyers (n=60), email, and in-person. Units of analysis included focus-group audio recording, transcripts, and field notes. Using traditional content analysis, we categorized data into themes and sub-themes.
Results
Thirteen Black men participated (Group 1, n=6; Group 2, n=7) having a mean age of 40.3 years (range 19 to 65), and employed full-time (77%). Themes included diabetes prevention, treatment, prevalence, risks, and health education. Participants identified diet and exercise as essential components of diabetes prevention. Additionally, participants mentioned that family history contributes to diabetes. Participants agreed that barbershops are an appropriate setting for data collection and health education on diabetes for Black men.
Discussion/Conclusion
Findings indicate that Black men are generally aware of diabetes. The community-engaged research process allowed for development of a culturally appropriate research study on diabetes. This study is the foundation for developing a culturally appropriate health education program on diabetes for Black men.
Keywords: Church, Black Men, Barbershop, Focus Group, Diabetes
INTRODUCTION
Diabetes is a leading cause of death in the United States (US), and the risk of death among people with diabetes is double than those without diabetes [1]. In relation to demographic distribution, the prevalence of diabetes is seven times higher among adults 65 years of age and older as compared to those 20-44 years old [2]. Racial and ethnic minority populations in the US have a higher prevalence of the disease than their non-Hispanic White counterparts [2]. Individuals living in areas with greater health disparities and less health equity have a higher risk of diabetes [3-5]. The epidemiological data on diabetes incidence, prevalence, morbidity and mortality in Minnesota mimics national trends [6]. Diabetes is the seventh leading cause of death in the state, which is the same as the United States population [6]. More than 250,000 individuals in Minnesota have been diagnosed with diabetes, and an estimated 25 % of adults in the state are pre-diabetic [6, 7]. Diabetes disproportionately affects racial and ethnic minorities in the US, who have more complications from diabetes, poorer health outcomes, and lower quality of care [4]. The prevalence of diabetes has dramatically increased in racial and ethnic minority communities [8, 9]. The incidence is higher for young non-Hispanic Blacks, who bear a disproportionate burden of the disease compared to their non-Hispanic White counterparts [8, 10]. For instance, Black adults in Minnesota are five times more likely than Whites to develop diabetes-related kidney failure [11]. The Black community is steadily growing in Olmsted County, and they represent nearly 6 percent of the population.[12]
Barbershop-based initiatives have been used successfully to engage and recruit Black men in health-research studies [13] . Historically, these initiatives utilized a combination of screening, education, and community capacity-building activities [14, 15]. Several studies have demonstrated that a barbershop-based health initiative is one of the easiest ways to reduce serious health conditions among Black men [16-18]. More importantly, through culturally specific programs, barbershops provide a venue for health education and promotion focused on chronic disease prevention [13, 19]. This study sought to assess Black men’s receptiveness to a barbershop-based program focused on diabetes prevention and awareness in Rochester and Olmsted County, Minnesota. Olmsted County is one of the fastest growing communities in Minnesota with Rochester being the third largest city in the state. Specifically, growth in the Black and Hispanic populations has increased in Rochester [20].
This study used a “barbershop for health” approach to assess Black men’s knowledge, attitudes, and behaviors regarding creation of a diabetes prevention program in Rochester and Olmsted County, Minnesota. We queried participants on the following: 1) their knowledge of diabetes causes, risk factors, and prevalence within their community; 2) their attitudes about prevention and treatment of the disease; and 3) the extent to which they practice behaviors helpful in reducing and preventing diabetes.
METHODS
Design
The pastor from Good News Church (alias used to protect confidentiality), with a predominantly Black congregation (African-American, Caribbean, and African decent), approached researchers at Mayo Clinic about conducting a barbershop-based health research program for Black men in Rochester. Good News Church operates the only Black barbershop in Rochester, Minnesota as an outreach ministry. This ministry provides a unique opportunity to connect with Black men through their outreach efforts. Many of the clients of the barbershop are not members of Good News Church but rather the greater Black male community.
Initial conversations with the church’s pastor and the lead barber indicated diabetes as a major health concern for the customers and church members. Following a comprehensive review of the literature and discussions with the pastor and barber, we created a focus-group script. The team chose a qualitative research approach with semi-structured focus groups. This provided an efficient method for gathering information from a variety of community members.
Focus Group Script Development
The semi-structured script used a theoretical framework adapted from constructs within the Health Belief Model (HBM), phases from the PRECEDE-PROCEED Model (PPM), and knowledge-attitude-behavior continuum (KAB). [21, 22] The HBM consists of six constructs that anticipate an individual’s health behaviors [22]: 1) Perceived Susceptibility refers to an individual’s understanding of risk and the prospect of being exposed to a certain disease or condition; 2) Perceived Severity examines the individual’s opinions on whether the disease or condition yields unfavorable health outcomes; 3) Perceived Benefits addresses participants’ acceptance that particular efforts either change the disease course or reduce risk; 4) Perceived Barriers describes the personal beliefs formulated around potential economic, psychosocial, and physical obstacles or costs associated with the ascribed intervention action; 5) Cues to Action assesses the internal and external factors affecting the individual’s motivation to adjust health behaviors; and 6) Self-Efficacy explores the individual’s belief that adopting these behaviors will yield desired outcomes.
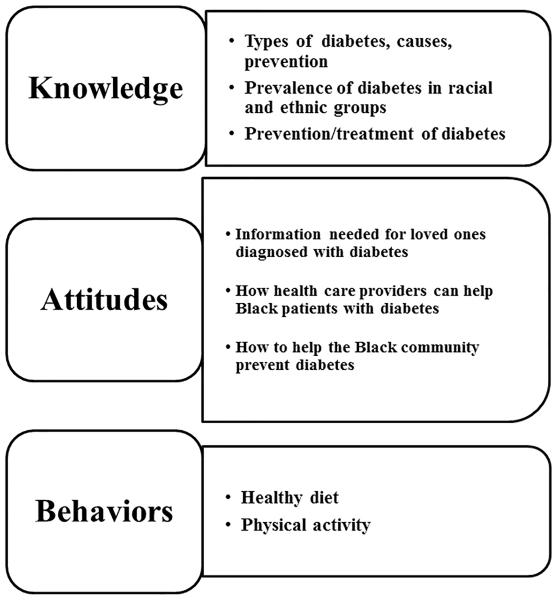
The use of PPM provided the opportunity for the pastor and barber to participate in the research study design. To gain a wider understanding of the target community, researchers engaged community members through qualitative research using focus groups. KAB seeks to increase the likelihood that an individual’s knowledge and attitudes will positively influence his behaviors [21]. The continuum takes into account behavior intention and information-processing model. We used HBM, PPM, and KAB to elicit participants’ thoughts on diabetes prevention and treatment. Figure 1 shows selected focus group topics as they relate to the constructs from KAB.
Barbershop Conversation Participant Recruitment
Men, 18 or older, who self-identified as Black, and lived in Olmsted County, Minnesota, were eligible for the study. The recruitment team included the pastor, barber, and staff from Mayo Clinic Center for Clinical and Translational Science Community Engagement Program. Mayo Clinic staff trained the study team on participant recruitment. Recruitment took place over a two-week period. Recruitment efforts included flyer distribution (n=60), mass e-mails, and in-person conversations at the barbershop site and other venues frequented by Black men. Potential participants received details for the focus group via email and telephone.
Participants selected one of two dates to attend a focus group. The barbershop served as the location for the 90-minute focus groups. The study was submitted and approved by the Mayo Clinic Institutional Review Board.
Data Collection and Remuneration
We conducted two focus groups, and all participants received a book (Mayo Clinic: The Essential Diabetes Book) as remuneration for their participation. Additionally, participants received a free meal during their focus-group session.
A Black male student intern trained in qualitative research moderated each group to maintain consistency and to create a comfortable environment for participants. The moderator followed a structured guide, obtained oral consent from the participants and asked open-ended questions to assess their knowledge, attitude, and behaviors about diabetes. The focus groups were audio recorded. Subsequently, the focus group recorders were transcribed verbatim. Another minority student from Mayo Clinic served as the note taker and observer during each focus group.
Data Analysis
Focus-group transcripts and field notes provided the units for analysis. The data analysis team consisted of five team members (JBB, SK, MVS, BS, and CW). We employed traditional content analysis [23]. Team members read the transcripts to become familiar with the data. One team member developed the coding taxonomy by reading the transcripts and creating preliminary themes and subthemes for a taxonomy. The taxonomy was based on HBM, PPM, and KAB, which contributed to the development of the focus-group script. Two other team members met with the primary coder, reviewed the created taxonomy, and began coding transcripts. A reflective process involved reviewing data and resolving discordant coding. The entire research team participated in interpreting the results. CW and BS created a document of the aggregated results and interpretations.
RESULTS
Participants
A total of n=13 Black male participated in the study. Group 1 included 6 men and Group 2 had 7 men. Participant ages ranged from 19 to 65 years with a mean of 40.3 years. Most participants reported having full-time employment (77%).
Themes
All participants held KABs about diabetes. Regardless of demographic characteristics, participants held thoughts about the prevalence of diabetes and their risk for developing diabetes. Across both focus groups, participants had suggestions for providing diabetes education to Black men in Rochester. Moreover, there was synergy when participants discussed family history, personal behaviors, and their culture as it relates to diabetes diagnosis, screening, education, and treatment as it relates to diabetes. Participants direct quotes are presented when appropriate under the themes.
Theme 1: KAB Regarding Diabetes Prevention and Treatment
The interview guide posed the question “What causes diabetes?”
Participants mentioned diet, physical activity, obesity, alcohol, and heredity as factors that can cause diabetes. Participants expressed a desire to learn more about diabetes.
“I just want people to talk about it…maybe work with other organizations…if you don’t learn about it in school, then how are you going to know?”
“[We need to] talk about a…fruit, vegetables, a…you know an appropriate diet…are we getting out there and …exercising? You know, when you take the stairs…when you get the opportunity to take the stairs …do we…you know…we don’t have to go out and run marathons, but…brisk walks each day; the type of things that we need to do in order to keep our heart healthy.”
Participants were asked to “explain the different types of diabetes.” One participant described diabetes in the following way:
“Type I [is the type] you’re born with, and you’ve done nothing wrong…not that anybody does anything wrong, just ones you are born with, and there’s the one [type II] you may acquire, which may have some heredity…some heredity to it, maybe more likely to get it if you have people in your family who have had it before, but it comes mainly from diet and exercise.”
Participants’ shared their attitudes and perceptions about diabetes prevention and education in the Black community. One participant discussed how community settings can be used to foster conversations on health.
He stated,
“In the traditional way, communities gather at a common [spot]…and that’s usually the best place to…get to talk, get talking about certain issues that we [Blacks] are facing…traditionally that’s been places of worship.”
Participants indicated that it is important to create messaging that is relevant, culturally sensitive and appropriate, and community-based. One participant stated,
“We are a population of African descent, and Black populations, and there are certain things that are very unique to our community but, in a certain extent, never to use or fall back on those without really realizing that every single person is the same. Within the same house, brothers and sisters may have completely different things, and so really looking at the individual, being sensitive about certain things that pertain to our community, but also not fall [into the habit of] under or over generalization[s].”
Another mentioned,
“I think we’re more “hands-on” [community] … It’s not what you say, ‘cause most us grew up with coming in…going in one ear and out the other, instead of what…actually, what you been through. And I think, you know, it has to be more hands-on things done with the Black community then rather than just saying do things.”
Participants were asked, “Is diabetes more prevalent in Blacks or people in the White population? How common is diabetes for each of these groups?”
Participants agreed that diabetes was more prevalent in Blacks than in non-Blacks. A few of the participants came to this conclusion of a higher prevalence in Blacks because of personal experiences with family, or conversations with peers or friends. Upon further examination of the prevalence of diabetes, participants affirmed that they were at risk for diabetes.
“I think we all are at some risk, ‘cause I don’t think we’re “risk free”. I guess it all depends on… you know…just your life-style promotes a greater risk.”
Moreover, some believed in myths like temperature affecting individuals’ susceptibility to diabetes.
“Cold makes the blood difficult to circulate…so warmer climate may be a little bit better as far as blood circulation is concerned.”
Even participants who did not know the cause of diabetes realized that it has higher prevalence in their community. For example, one participant says,
“It’s not in my family like that, but at the same time I just know it’s something that revolves around the community…the Black community and stuff like that, so. I don’t know if it’s in the food or what.”
It was frequently stated that diabetes “runs in my family.” Participants considered diet and lifestyle as factors increasing the risk of developing diabetes.
“I think it was due more so to the food…the types of foods they were eating, and lack of exercise”.
One participant stated,
“With the correct diet and exercise, I believe that you can prevent diabetes.”
When probed about their current eating habits, participants mentioned eating fried foods and foods with a high sugar and/or fat content like “soul food”.
Theme 2: Trust of Health Care Providers
Participants indicated they trust family, friends, colleagues, and church leaders for health information. However, most participants felt most comfortable with health care providers giving them health information. One participant had this to say about Black male health care providers:
“Ideally I would like a Black male. Someone who can like relate to me more-so.”
Another participant agreed and share he would feel more comfortable with a Black male provider. “It won’t make a difference, but I think I’ll listen more if it’s a male and he’s from the same background as me.”
Eventually participants agreed that the ideal health provider gives clear and concise information that helps to establish trust. For instance, it was summed up by one participant as “I have had very positive experiences with male, female, African-American, Caucasian, Hispanic doctors…just a very caring doctor…somebody who cares, who’s honest, who’s open to… listening to what I have to say and who’s not judgmental.”
Participants indicated that health providers needed to employ appropriate methods of communication in order to reach Blacks with diabetes. They agreed that providers may actually need to visit the Black community (i.e., in barbershops, churches or, in the case of younger Black males, in secondary schools). Although relying on media was less effective than one-on-one counseling, they noted that television was more effective than print and that Facebook and Twitter might better serve the younger audience. Participants suggested that health providers give information on causes, prevention, and treatment of diabetes.
“Right, tell us what the cure is, what we got to do to end this mad human drama this I hear; this diabetes thing. How do we cure this? What do we have to do to maintain that level of not to get it so serious that you have to get cut on, and get ampted [amputated] off and all that type of stuff.”
There was agreement that people need to discuss health choices and especially diabetes, “it’s affecting the Black community real bad, and so we need to talk about it more.”
One participant had this to say about consequences of having diabetes, “If you didn’t take corrective action that they could go blind, lose legs…die.”
Participants reported that the lack of insurance, limited insurance, or fear of receiving a bill prevented Blacks with diabetes from visiting the doctor on a regular basis. Participants gave personal accounts of receiving high bills after visiting doctors for routine care, “I go to the doctor and…just get a prescription for blood pressure pills, and … you owe eight hundred- something bucks.” Some participants discussed the difficulty of dealing with insurance providers or understanding coverage.
Theme 3: Health Education for Diabetes
Participants expressed interest in learning more about diabetes. Here is how a participant indicates his interest in additional education:
“I think there is definitely one approach that I think that at this point, folks may not know exactly what diabetes is, you know, but they know that it exists, and they know that you get limbs cut off and you die, and stuff like that. And I think what’s important is to start teaching folks sort of the alternatives to how you deal with it.”
Participants mentioned the importance of creating a specific, personalized message for the intended audience. One participant suggested pictograms a helpful in health education tool. This led to a discussion of having Black-tailored diabetes health-education materials.
For instance, one participant said,
“I think we often times make assumptions about different people, from a racial standpoint, from gender stand points… you have to kind of, you know, take each case as it comes.”
Participants supported the idea of having culturally appropriate diabetes-education materials.
“I think that the curriculum has to be culture sensitive.”
They felt that mass media advertisements would be a good approach to communicate health promotion and prevention of diabetes. A participant stated,
“Maybe if they start having commercials and stuff, you know, people watch a lot of TV at home and have a lot of advertising, so I guess if they start showing risks of diabetes like they do about cancer and smoking, I think it would be a good awareness of everybody else that watch TV.”
Still, participants agreed that mass media should not replace direct contact with Black men at risk for developing diabetes. In particular, participants singled out printed materials as an ineffective method of education:
“Everybody’s gonna get a pamphlet, you know, Black people don’t read including me.”
Participants also agreed that messages should be age-appropriate with a special focus on secondary school audiences. For example, one participant suggested face-to-face meetings in a study-hall setting:
“It will never get off the ground if they [health providers] don’t periodically meet in a classroom. I mean like…even if you have to force it on them, doing a study hall or we just have to speak…like we doin’ now.”
Additionally, participants felt that it was important to hear from individuals living a diabetic lifestyle so they could relate and gain knowledge about diabetes treatment and progression.
DISCUSSION
Findings from these focus groups show that Black men have a general awareness of diabetes. However, there are conceptual gaps in knowledge about risk factors and susceptibility. Participants strongly agreed that culturally appropriate barbershop-based initiatives could have meaningful impact by offering a diabetes self-care and monitoring program [16, 18, 24-27]. Previous research studies have failed to identify a single modifiable risk factor for diabetes in Black communities. A previous study estimates that as many as one in three adults living in the United States could have diabetes by 2050 [28]. Findings from this and similar studies among Blacks suggest that factors such as socioeconomic status may contribute to higher incidence of diabetes [9, 29]. This multidimensional concept of socioeconomic status relates to a person’s education, income, occupation as well as diet and access to exercise facilities and healthcare services [5, 18]. Diabetes impacts a broad spectrum; nearly 12% of men ≥ 20 years in the United States may have confirmed or undiagnosed diabetes [30]. The prevalence of diabetes in Minnesota has increased from 5.0 percent in 1994 to 6.7 percent in 2010 [31, 32].
Recognizing the importance of the barbershop in the Black community, development of a culturally appropriate diabetes-prevention program is consistent with a community-engaged research model. Moreover, these approach can, utilize principles of HBM, PPM, and KAB. The primary value of barbershop setting is its ability to empower both community members (specifically Black men) and researchers jointly to address health disparities in the community at the grassroots level [33]. Parallels exist in barbershop for health promotion programs with Black men and similar programs in the church. For instance, the church also educates the Black community about health and well-being [34]. Research partnerships between churches and academic institutions have provided opportunities for marginalized communities to engage in the research process [35]. This engagement is the result of the churches’ established relationships as institutional leaders for change that evoke sense of sense of mutual understanding and respect that serves as protection for the Black community [35-38].
Barbershops are a sort of “country club for Black men” [24]. They are an important channel for health outreach and health promotion targeting Black men [16, 18]. Davis maintained that “the barbershop is one of the few places where African-American men gather and do not feel threatened as Black men” [19]. This realization is not lost because the barbershop provides an opportunity to distinguish the sociocultural constructs of what it means to be Black men compared to being a man in the greater American community [19].
Many researchers and medical institutions have partnered with communities to focus efforts outside of the traditional clinical setting to address the health disparities of preventable diseases such as diabetes that disproportionately impact Black men [16, 18, 25, 27, 33]. Historically, barbers play an important role in the American culture as some of the first entrepreneurs in our country who influenced the health of the community they served [13]. Barbers’ strategic role as leaders in the community has proven successful in motivating and engaging Black men in health promotion [25]. The barbershop is a “sacred” institution that serves as a solid infrastructure in the Black community to introduce health promotion and research to an underserved population.
This study had the advantage of working with both a local Black church with an affiliated barbershop. Through this outreach effort, we were able to engage in a dialogue about diabetes. The focus-group participants perceived family history and diet to be primary factors in development of diabetes; most participants expressed a lack of confidence in their level of knowledge and understanding of diabetes. Participants’ comments indicated that limited knowledge makes it difficult to address deficiencies and misperceptions around diabetes. Participants mentioned their personal or families’ experience as a motivating factor for learning more about diabetes.
Some participants felt that a family history of diabetes increased their risk of acquiring the disease. Overwhelmingly, there were suggestions that an unhealthy diet and lack of exercise contribute to the higher incidence of diabetes in Blacks. Participants reported that “some” of their acquaintances, including family and friends, could benefit from diabetes prevention and education given the current culture, habits, and values of the Black community.
Participants commented on the confusion resulting from inconsistent or often-changing messages from family members and healthcare providers. Therefore, diabetes-prevention approaches targeted to Black men should be culturally appropriate and concise. When probed about the media’s effectiveness in preventing diabetes, many participants felt that commercials increase knowledge of diabetes risk. Age should be a consideration in designing diabetes-based health-promotion messages; for example, participants felt that Twitter and Facebook would be effective in reaching younger Black men. In addition to designing effective health-promotion materials, healthcare providers may need to go beyond the traditional methods and identify ‘safe spaces’ (traditional community gathering places) to provide education; these could include barbershops, community centers, schools and places of worship.
There are some potential limitations to this study. First, the study is a small sampling (n=13) of men who self-identified as Black and lived in Olmsted County, Minnesota, which means the findings may not be generalized to other Black men in other communities. Secondly, one church and its affiliated barbershop were involved in the recruitment for this project. This may have limited the catchment area of potential study participants. Lastly, there was a short timeframe to collect data. If the project timeline had been longer, more men could have participated in the conversations. This study supports existing research on barbershop-based health education and prevention. It expands on the literature because it includes participants from a small number of immigrant communities in addition to African-Americans.
This project demonstrates a successful community engagement in research collaboration with an academic medical center and a church-affiliated barbershop. The effort successfully identified and recruited Black men to determine the feasibility of this research process in Rochester and Olmsted County, Minnesota. Study participants were aware that a combination of a well-balanced diet and regular exercise could possibly prevent diabetes. Furthermore, the findings indicate that a tailored, culturally appropriate message with clarity for the targeted audience may be an effective approach to diabetes education and awareness. Administering a health-promotion program in a barbershop setting can positively influence health behavior choices of Black men. Future research should focus on how to engage Black barbershops in health- promotion activities. This study allowed us the opportunity to explore the emerging health disparities that impact Black men and to determine ways to discuss health in an environment familiar to them. This type of study takes into account the historical, cultural, and spiritual aspects that shape the development of sustainable health interventions with Black men [13, 19].
Acknowledgements
The authors would like to thank the Mayo Clinic Center for Clinical and Translational Science Activities Community Engagement Program and Mayo Clinic College of Medicine Office of Diversity. Special thanks to Good News Church (Alias) and Good News Barbershop (Alias) for their help with designing and implement the study.
This publication was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS) and Grant Number HL092621 from the National Heart, Lung, and Blood Institute, components of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Footnotes
Conflict of Interest
JBB, CW, SK, AC, EAM, IB, MVS, BS, MH, JK, LD and OID declare that they have no conflict of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants included in the study.
REFERENCES
- 1.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care. 2009 Feb;32(2):287–94. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . Diabetes Report Card 2012. Centers for Disease Control and Prevention, Services UDoHaH; Atlanta, GA: 2012. [Google Scholar]
- 3.Betancourt JR, Corbett J, Bondaryk MR. Addressing disparities and achieving equity: cultural competence, ethics, and health-care transformation. Chest. 2014 Jan;145(1):143–8. doi: 10.1378/chest.13-0634. [DOI] [PubMed] [Google Scholar]
- 4.Betancourt JR, Duong JV, Bondaryk MR. Strategies to reduce diabetes disparities: an update. Curr Diab Rep. 2012 Dec;12(6):762–8. doi: 10.1007/s11892-012-0324-1. [DOI] [PubMed] [Google Scholar]
- 5.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007 Oct;64(5 Suppl):101S–56S. doi: 10.1177/1077558707305409. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minnesota Diabetes Program . Diabetes and Prediabetes in Minnesota 2012: Facts for Providers, Researchers, and Diabetes Adovates. Minnesota Department of Health; St. Paul, MN: 2014. [cited 2014 November 20, 2014]; Available from: http://www.health.state.mn.us/diabetes/pdf/DiabetesPrediabetesMinnesotaFactSheet2012.pdf. [Google Scholar]
- 7.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013 Apr;36(4):1033–46. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Menke A, Rust KF, Fradkin J, Cheng YJ, Cowie CC. Associations between trends in race/ethnicity, aging, and body mass index with diabetes prevalence in the United States: a series of cross-sectional studies. Ann Intern Med. 2014 Sep 2;161(5):328–35. doi: 10.7326/M14-0286. [DOI] [PubMed] [Google Scholar]
- 9.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med. 2014 Apr 15;160(8):517–25. doi: 10.7326/M13-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davidson MB, Duran P, Lee ML. Community screening for pre-diabetes and diabetes using HbA1c levels in high-risk African Americans and Latinos. Ethn Dis. 2014 Spring;24(2):195–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Renal Network 11. ERDS 2011 Available from: http://www.esrdnet11.org/assets/pdf/2011_annual_report_data_tables.pdf.
- 12.Minnesota Olmsted County Demographics and Census Data. 2015 Available from: http://www.co.olmsted.mn.us/yourgovernment/demographics/Pages/default.aspx.
- 13.Davis OI. (Re)framing Health Literacy: Transforming the Culture of Health in the Black Barbershop. The Western Journal of Black Studies. 2011 Fall 2011. [Google Scholar]
- 14.Hart A, Jr., Bowen DJ. The feasibility of partnering with African-American barbershops to provide prostate cancer education. Ethn Dis. 2004 Spring;14(2):269–73. [Research Support, U.S. Gov't, P.H.S.] [PubMed] [Google Scholar]
- 15.Hart A, Jr., Underwood SM, Smith WR, Bowen DJ, Rivers BM, Jones RA, et al. Recruiting African-American barbershops for prostate cancer education. J Natl Med Assoc. 2008 Sep;100(9):1012–20. doi: 10.1016/s0027-9684(15)31437-1. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 16.Jones DK. Promoting cancer prevention through beauty salons and barbershops. N C Med J. 2008 Jul-Aug;69(4):339–40. [PubMed] [Google Scholar]
- 17.Li J, Linnan L, Rose J, Hooker E, Boswell M, D'Angelo H, et al. Promoting men's health within barbershops: barber/owner survey results and implications for intervention planning. Prev Med. 2011 Sep;53(3):207–8. doi: 10.1016/j.ypmed.2011.06.001. [Letter Research Support, N.I.H., Extramural] [DOI] [PubMed] [Google Scholar]
- 18.Linnan LA, Reiter PL, Duffy C, Hales D, Ward DS, Viera AJ. Assessing and promoting physical activity in African American barbershops: results of the FITStop pilot study. Am J Mens Health. 2011 Jan;5(1):38–46. doi: 10.1177/1557988309360569. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis OI. Barbershop Cuisine: African American Foodways and Narratives of Health in the Black Barbershop. Int J Mens Health. 2013;12(2):138–49. [Google Scholar]
- 20.Minnesota Department of Administration . Minnesota State Demographic Center. Minnesota Department of Adminstration; St. Paul, Minnesota: 2014. [cited 2014 November 20, 2014]; Available from: http://mn.gov/admin/demography/ [Google Scholar]
- 21.Bettinghaus EP. Health promotion and the knowledge-attitude-behavior continuum. Prev Med. 1986;15(5):475–91. doi: 10.1016/0091-7435(86)90025-3. [DOI] [PubMed] [Google Scholar]
- 22.Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. Jossey-Bass; San Francisco, CA: 2008. [Google Scholar]
- 23.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005 Nov;15(9):1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 24.Baker JL, Brawner B, Cederbaum JA, White S, Davis ZM, Brawner W, et al. Barbershops as venues to assess and intervene in HIV/STI risk among young, heterosexual African American men. Am J Mens Health. 2012 Sep;6(5):368–82. doi: 10.1177/1557988312437239. [DOI] [PubMed] [Google Scholar]
- 25.Hess PL, Reingold JS, Jones J, Fellman MA, Knowles P, Ravenell JE, et al. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. 2007 May;49(5):1040–6. doi: 10.1161/HYPERTENSIONAHA.106.080432. [Evaluation Studies Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 26.Luque JS, Rivers BM, Gwede CK, Kambon M, Green BL, Meade CD. Barbershop communications on prostate cancer screening using barber health advisers. Am J Mens Health. 2011 Mar;5(2):129–39. doi: 10.1177/1557988310365167. [Research Support, N.I.H., Extramural] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Releford BJ, Frencher SK, Jr., Yancey AK, Norris K. Cardiovascular disease control through barbershops: design of a nationwide outreach program. J Natl Med Assoc. 2010 Apr;102(4):336–45. doi: 10.1016/s0027-9684(15)30606-4. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gambert SR, Pinkstaff S. Emerging Epidemic: Diabetes in Older Adults: Demography, Economic Impact, and Pathophysiology. Diabetes Spectrum. 2006;19(4):221–8. [Google Scholar]
- 29.Rust KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, Bainbridge KE, et al. Prevalence of Diabetes and High Risk for Diabetes Using A1C Criteria in the U.S. Population in 1988-2006. Diabetes Care. 2010;33(3):7p. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention BRFSS. 2010 Available from: http://apps.nccd.cdc.gov/brfss/display.asp.
- 31.American Diabetes Association The Burden of Diabetes in Minnesota. 2010 Available from: http://www.diabetes.org/assets/pdfs/advocacy/states/minnesota-state-fact-sheet.pdf.
- 32.Centers for Disease Control and Prevention MN Fact Sheet. 2012 Available from: http://www.cdc.gov/nchs/pressroom/states/MN_2012.pdf.
- 33.Releford BJ, Frencher SK, Jr., Yancey AK. Health promotion in barbershops: balancing outreach and research in African American communities. Ethn Dis. 2010 Spring;20(2):185–8. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.] [PMC free article] [PubMed] [Google Scholar]
- 34.Rowland ML, Isaac-Savage EP. As I see it: a study of African American pastors' views on health and health education in the black church. J Relig Health. 2014 Aug;53(4):1091–101. doi: 10.1007/s10943-013-9705-2. [DOI] [PubMed] [Google Scholar]
- 35.De Marco M, Weiner B, Meade SA, Hadley M, Boyd C, Goldmon M, et al. Assessing the readiness of black churches to engage in health disparities research. J Natl Med Assoc. 2011 Sep-Oct;103(9-10):960–7. doi: 10.1016/s0027-9684(15)30453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Butler-Ajibade P, Booth W, Burwell C. Partnering with the black church: recipe for promoting heart health in the stroke belt. ABNF J. 2012 Spring;23(2):34–7. [PubMed] [Google Scholar]
- 37.Das A, Nairn S. Race differentials in partnering patterns among older U.S. men: influence of androgens or religious participation? Arch Sex Behav. 2013 Oct;42(7):1119–30. doi: 10.1007/s10508-013-0096-y. [DOI] [PubMed] [Google Scholar]
- 38.Goldmon MV, Roberson JT., Jr Churches, academic institutions, and public health: partnerships to eliminate health disparities. N C Med J. 2004 Nov-Dec;65(6):368–72. [PubMed] [Google Scholar]