Abstract
Background
Epidemiologic studies of fecundability often use retrospectively-measured time-to-pregnancy (TTP), thereby introducing potential for recall error. Little is known about how recall error affects the bias and precision of the fecundability odds ratio (FOR) in such studies.
Methods
Using data from the Danish Snart-Gravid Study (2007–2012), we quantified error for TTP recalled in the first trimester of pregnancy relative to prospectively-measured TTP among 421 women who enrolled at the start of their pregnancy attempt and became pregnant within 12 months. We defined recall error as retrospectively-measured TTP minus prospectively-measured TTP. Using linear regression, we assessed mean differences in recall error by maternal characteristics. We evaluated the resulting bias in the FOR and 95% confidence interval (CI) using simulation analyses that compared corrected and uncorrected retrospectively-measured TTP values.
Results
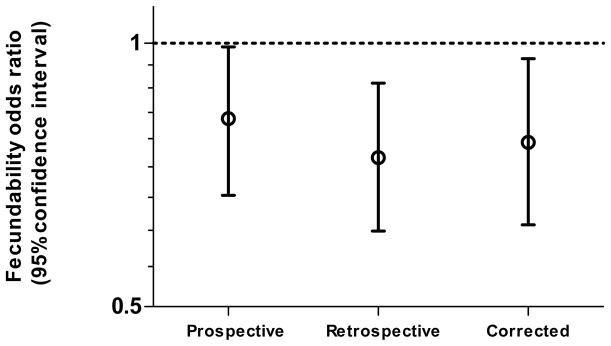
Recall error (mean=−0.11 months, 95% CI −0.25, 0.04) was not appreciably associated with maternal age, gravidity, or recent oral contraceptive use. Women with TTP>2 months were more likely to underestimate their TTP than women with TTP ≤2 months (unadjusted mean difference in error: −0.40 months, 95% CI −0.71, −0.09). FORs of recent oral contraceptive use calculated from prospectively-measured, retrospectively-measured, and corrected TTPs were 0.82 (95% CI 0.67, 0.99), 0.74 (95% CI 0.61, 0.90), and 0.77 (95% CI 0.62, 0.96), respectively.
Conclusions
Recall error was small on average among pregnancy planners who became pregnant within 12 months. Recall error biased the FOR of recent oral contraceptive use away from the null by 10%. Quantitative bias analysis of the FOR can help researchers quantify the bias from recall error.
INTRODUCTION
Studies investigating determinants of fecundability often use retrospectively-collected data on time-to-pregnancy (TTP) ascertained from already-pregnant women.1 Examples include the Danish National Birth Cohort2 and Norwegian Mother and Child Cohort Study.3 Systematic error in retrospectively-measured TTP can introduce bias in the fecundability odds ratio (FOR), defined as the ratio of the cycle-specific odds of pregnancy in the exposed relative to the unexposed population.4 Published investigations assessing systematic error in retrospectively-reported TTP compared with a prospective measure of TTP from the same population are scarce. In a validation study of TTP recalled during pregnancy and the first year postpartum, the gold standard of prospectively-measured TTP included data from participants who had already been attempting pregnancy for several months at enrollment.5
We quantified the error of TTP reported in months, recalled during the first trimester relative to prospectively-measured TTP, using data from Danish women participating in a prospective cohort study of TTP. We also assessed differences in error according to the following characteristics: prospectively-measured TTP (>2 vs. ≤2 months), maternal age (<30 vs. ≥30 years), gravidity, menstrual cycle regularity, and last contraceptive method. We conducted a quantitative bias analysis to correct the FOR estimated using retrospectively-measured TTP.
METHODS
Study Population
The Snart-Gravid Study, conducted in Denmark from 2007–2012, enrolled 5,046 women who were aged 18–40 years, attempting pregnancy with a male partner, not using fertility treatments, and willing to provide their identification number for the Central Person Registry and email address.6 Participants provided informed consent and reported exposures, covariates, and pregnancy status using web-based questionnaires. Every two months, participants received an email invitation to complete a follow-up questionnaire, with non-respondents receiving up to two reminders. Active follow-up ended when participants reported they were pregnant, using fertility treatments, or no longer attempting pregnancy, or after they completed 12 months of follow up (i.e. six follow-up questionnaires), whichever came first. The study protocol was approved by the Institutional Review Boards of Boston University Medical Center and the Danish Data Protection Agency.
To obtain a prospective measure of TTP, we excluded from the analysis 4,293 women who enrolled after the first month of attempting pregnancy. We further excluded women who did not report that they were pregnant on a follow-up questionnaire (n=251), women with missing retrospectively-measured TTP (n=31), missing date of last menstrual period (LMP) at baseline (n=8), missing LMP in early pregnancy (n=1), missing exposure data (n=4), women who reported an LMP date that was <10 days before their report of pregnancy (n=3), and women who reported a retrospectively-measured TTP=1 after an interval >4 months between filling out questionnaires (n=4) because this could signify an intervening pregnancy loss. We further excluded 30 women who completed their early pregnancy questionnaire in the second trimester. After these exclusions, 421 women were included in the analysis.
Data Collection
The baseline questionnaire elicited data on length of the current pregnancy attempt in months, LMP date, menstrual cycle length and regularity, last method of contraception, body size, reproductive and medical histories, and lifestyle habits. The follow-up questionnaires collected information on LMP date and pregnancy status. For the current analysis, prospectively-measured TTP was defined as the interval in months from the beginning of the first menstrual cycle when the participant tried to become pregnant, to the middle of the menstrual cycle when she conceived a recognized pregnancy. Thus, we calculated prospectively-measured TTP in days and divided by 30.4 to convert days into months (365.25/30.4=12). The resultant continuous value of months was rounded to the nearest integer:
Retrospectively-measured TTP was defined using the question from the early pregnancy questionnaire, “How many months did it take you to get pregnant?” Retrospectively-measured TTP in months was reported as an integer ≥0. We interpreted a report of TTP = 0 as getting pregnant in the first month of trying (TTP = 1 month) and grouped these with reports of TTP=1 in the analysis, consistent with previous retrospective TTP studies.7
Cycle regularity was defined using the following question, “Within the past couple of years, has your menstrual period been regular during those time periods when you were not using hormonal contraceptives [if applicable]?” (yes or no). Last contraceptive method was reported from a multiple-choice question and categorized for analytic purposes as either oral contraceptives (OCs), barrier methods (condom, foam, gel, cream, sponge, suppository, or intrauterine device), or other method (hormone injection, patch, or ring; fertility awareness methods, withdrawal, or unspecified).
Statistical Analysis
We estimated the probability of under-estimating and over-estimating TTP, respectively, using prospectively-measured TTP as the benchmark. Recall error was quantified as the difference of retrospectively-measured TTP minus prospectivey-measured TTP. We further investigated systematic error by using linear regression to estimate recall error differences across categories of maternal characteristics that had consistent associations with TTP in the literature: age (≥30 vs. <30),8 cycle regularity (irregular vs. regular),9 and last contraceptive method (oral contraceptives vs. barrier methods).10 We also estimated the association of recall error with gravidity (gravid vs. nulligravid) and prospectively-measured TTP (>2 vs. ≤2), because longer TTP and gravidity were associated with underestimation of recalled TTP in a validation study of 10-year recall of TTP.11 We used diagnostic plots to verify the assumptions of linear regression. Linear regression models were adjusted for other potential predictors of misclassification including age, gravidity, cycle regularity, and last contraceptive method. Because adjustment for other predictors of misclassification did not change the results much, we present only the unadjusted estimates for mean difference in error.
Quantitative bias analysis
To inform quantitative bias analyses in studies of fecundability that measure TTP retrospectively,12 we used our measures of recall error to impute probable, prospectively-measured (i.e., corrected) TTP values from retrospectively-measured TTP. First, we cross-tabulated prospectively-measured TTP and retrospectively-measured TTP. Next, to summarize the distribution of prospective TTP given the retrospective values, we fit one normal distribution to the observed prospectively-measured TTP values for each of the 12 values of retrospectively-measured TTP. We then imputed corrected TTP values (rounded to the nearest integer) for each subject by randomly sampling from the appropriate normal distribution given their retrospectively-measured value. We repeated this procedure 100,000 times to produce 100,000 imputed data sets. Observations with imputed TTP<1 were set to TTP=1, and observations with imputed TTP>12 months were censored at 12 months in keeping with standard analysis methods for TTP data.1 In the Appendix, we include SAS code that implements this procedure and shows the estimated mean and standard deviation of each normal distribution summarizing prospectively-measured TTP conditional on retrospectively-measured TTP. Fitting a normal distribution was intended to facilitate the application of these data to other cohorts by enhancing flexibility of the observed probabilities of prospectively-measured TTP conditional on retrospectively-measured TTP.
Bias analysis
We conducted a quantitative bias analysis that assessed the bias from recall error to the FOR of the association between oral contraceptive (OC) use as last method of contraception and fecundability.10 We estimated the FOR comparing OC use vs. all other contraceptive methods by fitting a discrete-time Cox proportional hazards model13 using the retrospectively-measured TTP (conventional analysis) as well as the prospectively-measured TTP. Then we proceeded as if we had no access to the prospectively-measured TTP data and estimated the FOR in each of the 100,000 data sets of corrected TTP. We incorporated the random error from the analysis of retrospectively-reported TTP by subtracting from each FOR the product of the standard error from the conventional analysis and a number drawn randomly from a standard normal distribution.14 The resulting distribution of 100,000 corrected FORs accounted for both the systematic and random error. We summarized this distribution using the median as the point estimate and the 2.5th and 97.5th percentile values to create 95% uncertainty intervals for the corrected FOR.14 All analyses were conducted in SAS version 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
Among the 421 women in the analytic sample, the median gestational age at report of TTP was 8 weeks (interquartile range: 6–10). These women tended to be under 30 years of age (62%, Table 1), lean (BMI<25 kg/m2: 74%), users of OCs as their last method of contraception (58%), and primigravid (53%). Compared with 4,625 women who were excluded from the analysis, included women had similar mean age (28.4 vs. 28.6 years), but they had a shorter median TTP (2 cycles vs. 9), lower mean BMI (23.4 vs. 24.5 kg/m2), and were more likely to have regular menstrual cycles (80% vs. 76%), to be non-smokers (88% vs. 80%), to have completed four years of higher education (66% vs. 57%), and have at least one child (39% vs. 32%).
Table 1.
Characteristics of 421 women who recalled their time-to-pregnancy in the first trimester: The Snart-Gravid Study, Denmark, 2007–2012.
| Characteristic | Percent |
|---|---|
| Gestational age, weeks (median) | 8 |
| Age <30 (%) | 62 |
| Body mass index, kg/m2 (%) | |
| <20 | 17 |
| 20–24 | 57 |
| 25–29 | 20 |
| ≥30 | 6 |
| Regular cycles (%) | 80 |
| Last method of contraception (%) | |
| Oral contraceptive pills | 58 |
| Barrier methods | 34 |
| Othera | 8 |
| Gravid (%) | 47 |
| Parous (%) | 39 |
| Current smoker (%) | 12 |
Includes withdrawal and fertility awareness methods.
Fifty-three percent of retrospective TTP reports agreed exactly with the prospective TTP measure, 26% were under-estimated, and 21% were over-estimated (Table 2). Recall error ≥ 2 months occurred in 12% of reports. The close agreement was evident in the cross-tabulation of prospectively- and retrospectively-measured TTP values (Table 3). There was no obvious digit preference for reporting. Recall error in months ranged from −6 to 18 months with a median of 0 and a mean of −0.11 months (95% CI −0.25, 0.04).
Table 2.
Error in recalled time-to-pregnancy: 421 women in the first trimester, The Snart-Gravid Study, Denmark, 2007–2012.
| N | Under-estimateda % (95% CI) | Over-estimatedb % (95% CI) | Recall Error, monthsc
|
||
|---|---|---|---|---|---|
| Mean (95% CI) | Mean Differenced (95% CI) | ||||
| Entire population | 421 | 26 (95% CI 22, 30) | 21 (95% CI 17, 24) | −0.11 (95% CI −0.25, 0.04) | -- |
| Prospective TTP | |||||
| ≤2 | 219 | 13 (95% CI 8, 17) | 22 (95% CI 16, 27) | 0.11 (95% CI 0.03, 0.19) | 0.00 (reference) |
| >2 | 202 | 43 (95% CI 36, 49) | 18 (95% CI 13, 24) | −0.29 (95% CI −0.59, 0.01) | −0.40 (95% CI −0.71, −0.09) |
| Cycle Regularity | |||||
| Regular | 337 | 26 (95% CI 22, 31) | 22 (95% CI 18, 27) | −0.03 (95% CI −0.21, 0.15) | 0.00 (reference) |
| Irregular | 84 | 30 (95% CI 20, 40) | 12 (95% CI 5, 19) | −0.31 (95% CI −0.55, −0.07) | −0.28 (95% CI −0.58, 0.02) |
| Age | |||||
| <30 | 259 | 24 (95% CI 19, 29) | 20 (95% CI 14, 27) | −0.09 (95% CI −0.22, 0.04) | 0.00 (reference) |
| ≥30 | 162 | 32 (95% CI 25, 39) | 20 (95% CI 14, 27) | −0.07 (95% CI −0.41, 0.27) | 0.01 (95% CI −0.34, 0.38) |
| Gravidity | |||||
| Nulligravid | 221 | 27 (95% CI 21, 33) | 22 (95% CI 16, 27) | −0.07 (95% CI −0.19, 0.05) | 0.00 (reference) |
| Gravid | 200 | 27 (95% CI 21, 33) | 19 (95% CI 13, 24) | −0.10 (95% CI −0.38, 0.19) | −0.02 (95% CI −0.34,0.29) |
| Last contraceptive methode | |||||
| Barrier methods | 139 | 25 (95% CI 18, 32) | 16 (95% CI 10, 22) | −0.03 (95% CI −0.40, 0.35) | 0.00 reference) |
| Oral contraceptive | 247 | 26 (95% CI 20, 31) | 25 (95% CI 19, 30) | −0.07 (95% CI −0.20, 0.07) | −0.04 (95% CI −0.36, 0.28) |
TTP=time-to-pregnancy; CI=confidence interval
Under-estimated by ≥1 month
Over-estimated by ≥1 month
Recall error in months calculated as follows: Retrospectively-measured TTP – Prospectively-measured TTP
Mean difference in error was estimated from a simple linear regression model.
Analysis excluded 35 women whose last contraception was not oral contraceptives or barrier methods.
Table 3.
Frequency distribution of retrospectively-measured time-to-pregnancy conditional on prospectively-measured time-to-pregnancy in 421 women: The Snart-Gravid Study, Denmark, 2007–2012.
| Prospectively-measured time-to-pregnancy, months | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | >12 | Total | ||
| Retrospectively-measured time-to-pregnancy, months | 1 | 106 | 28 | 2 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 139 |
| 2 | 29 | 37 | 14 | 2 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 86 | |
| 3 | 1 | 18 | 30 | 19 | 5 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 77 | |
| 4 | 0 | 0 | 10 | 16 | 6 | 6 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 40 | |
| 5 | 0 | 0 | 4 | 3 | 14 | 6 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 28 | |
| 6 | 0 | 0 | 1 | 3 | 5 | 9 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 21 | |
| 7 | 0 | 0 | 0 | 0 | 1 | 3 | 4 | 2 | 0 | 0 | 0 | 0 | 0 | 10 | |
| 8 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 3 | 1 | 0 | 1 | 0 | 0 | 8 | |
| 9 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 3 | |
| 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 5 | 0 | 0 | 7 | |
| 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 12 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| >12 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | |
| Total | 136 | 83 | 61 | 45 | 33 | 30 | 10 | 8 | 4 | 3 | 6 | 0 | 0 | 421 | |
Under-estimation of retrospectively-measured TTP was more likely among those with longer prospectively-measured TTP (>2 vs. ≤2 months: mean difference in error=−0.40 months (95% CI −0.71, −0.09)). Women with irregular cycles tended to have more negative recall error than women with regular cycles (mean difference in error=−0.28 months (95% CI −0.58, 0.02)). There was little difference in recall error by age (≥30 versus <30 years: mean difference in error=0.01 months (95% CI −0.34, 0.38)) or gravidity (gravid versus nulligravid: mean difference in error =−0.02 months (95% CI −0.34, 0.29)). Recall error was not substantially different among women who used barrier methods and OCs as their last method of contraception (mean difference in error=−0.04 months, 95% CI −0.36, 0.28).
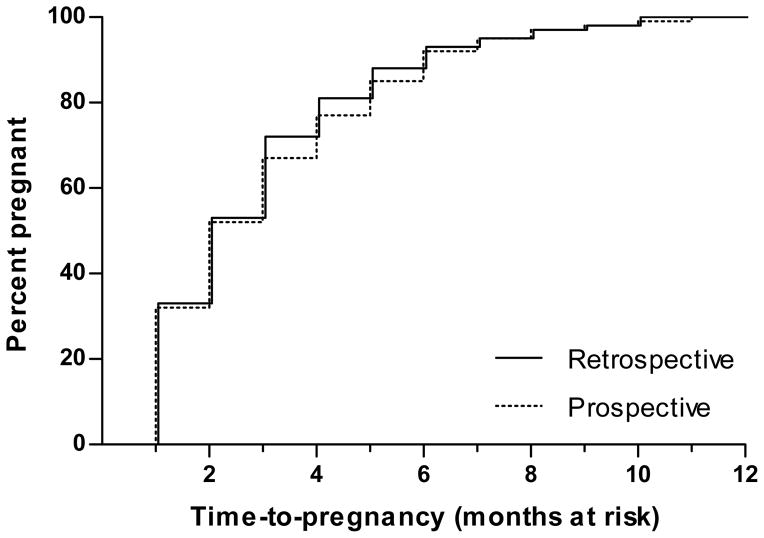
Because retrospectively-measured TTP tended to be under-estimated for prospectively-measured TTP values>2, the cumulative percent of pregnancy was slightly higher in months 3, 4, and 5 when it was calculated from retrospectively-measured TTP compared with prospectively-measured TTP (Figure 1).
Figure 1.
Cumulative percent pregnant according to prospectively-measured TTP and retrospectively-measured TTP: 421 women, The Snart-Gravid Study, Denmark, 2007–2012.
Sensitivity analyses
Women with irregular cycles, whose menstrual cycles often last >30 days, may become accustomed to thinking of menstrual cycles, not months, as the unit of attempt time. To investigate whether this phenomenon biased our data, we conducted a sensitivity analysis that compared the TTP reported by women with irregular cycles against prospectively-measured TTP in cycles. Among women with irregular cycles, using menstrual cycles instead of months as the metric of attempt time resulted in decreased error and a decreased mean difference in error relative to women with regular cycles, for whom the retrospective and prospective measures were still defined in months (underestimated TTP: 24% (95% CI 15%, 33%); over-estimated TTP=20% (95% CI 12%, 29%) ; mean difference in error=0.015 (95% CI −0.24, 0.27)).
Ninety-five percent of women analyzed completed the follow-up questionnaires every two months. A sensitivity analysis conducted among these women produced similar results to the overall analysis, as did a further sensitivity analysis that restricted to women having less than two intervening menstrual cycles between completed questionnaires (data not shown).
Bias Analysis
The bias analysis used data from all 421 women, of whom 247 (58.7%) used OCs as their last method of contraception. Using prospectively-measured TTP in months, OC use was associated with a lower fecundability relative to all other methods (FOR = 0.82 (95% CI 0.67, 0.99); Figure 2). Repeating this analysis using retrospectively-measured TTP yielded an FOR that was farther from the null (FOR=0.74 (95% CI 0.61, 0.90)). Using the corrected TTP values, the median FOR was 0.77, and the 95% uncertainty interval incorporating total study error (systematic and random) was (0.62, 0.96). The 95% uncertainty interval that accounted only for systematic error was (0.71, 0.84).
Figure 2.
Association of oral contraceptives for last contraceptive method with fecundability among 421 women: The Snart-Gravid Study, Denmark, 2007–2012.
COMMENTS
In this prospective study of pregnancy planners who were asked to recall their TTP in months during early pregnancy, recall error of TTP was on average small. Underestimation of TTP was greater among women with prospectively-measured TTP>2 relative to prospectively-measured TTP≤2, and among women with irregular cycles relative to regular cycles. Average recall error was similar across strata of age, gravidity, and last contraceptive method. Recall error biased the FOR of recent oral contraceptives use away from the null by 10% (0.74 vs. 0.82). A quantitative bias analysis produced a corrected FOR that more closely approximated the FOR from prospectively-measured TTP and an uncertainty interval that conveyed both systematic and random error.
This study was the first to compare TTP recalled in pregnancy with prospectively-measured TTP from the same participants. Baird et al.1 found the distribution of TTP ≤ 6 cycles recalled during the first six months of pregnancy nearly matched a distribution of prospectively-measured TTP from another study.15 Zielhuis et al. found little error on average in TTP recalled after 3–20 months among 100 women who had participated in a prospective study of early pregnancy loss5 (difference in retrospectively-measured and prospectively-measured TTP: mean =−0.6 months (95% CI −1.7, 0.5)). Notable differences between that study and ours are that the prospective measure of TTP in Zielhuis et al. included a period of time (“several months”) before enrollment, for an unreported but apparently substantial fraction of participants, and that study included women with TTP>12 months.5
Our finding that longer prospectively-measured TTP was associated with greater under-estimation of TTP agrees with results from a previous validation study of TTP recalled after 10 years11 and two reliability studies of TTP recalled after 1–4 years4 and 11–16 years.17 Cognitive psychology studies have reported that recalling the timing of past events is subject to a telescoping effect, in which the duration since a past event tends to be under-estimated.18 Another reason for this phenomenon is intuitive: larger values of TTP have more room for error.
Women with irregular menstrual cycles may give a somewhat less accurate report of TTP when the unit of time is months, not cycles. In planning their pregnancy, they might become accustomed to thinking of cycles as the unit of time, and their menstrual cycles may tend to last >30 days. These features could make it harder for them to understand the question and harder to recall their TTP in months. In support of this explanation, a sensitivity analysis found less error among women with irregular cycles when their retrospective report was interpreted as cycles rather than months. Questionnaire design may enhance reporting accuracy by eliciting retrospectively-measured TTP in cycles, in addition to months. A prospective cohort study that enrolls women who have already been attempting pregnancy may elicit the date of discontinuation of contraception, the most recent LMP date, and the number of cycles and months attempting pregnancy before the most recent LMP.
Retrospectively-measured TTP differed from prospectively-measured TTP by ≥1 month in 47% of responses, and by ≥ 2 months in only 12%. Although many women failed to recall their precise TTP, the great majority was able to recall its approximate value. There are alternative explanations for the preponderance of responses with a small amount of discrepancy between prospectively-measured and retrospectively-measured TTP. The discrepancy may reflect rounding error from reporting the number of months as an integer. Some women may have misunderstood the question and reported how many months they tried before the month when they got pregnant. Others may have reported TTP in cycles instead of months. Limitations in data collection by questionnaire may have resulted in counting a cycle when the participant was enrolled in the study but did not have sexual intercourse during the fertile period. In such a situation, the participant would have rightly subtracted one cycle from her TTP. Furthermore, prospectively-measured TTP was calculated from the LMP date on the baseline and follow-up questionnaires, and participants recalled these dates. The LMP date should be recalled highly accurately by someone planning pregnancy.
Because our study was limited to participants who became pregnant within ≤ 12 months, we were not able to assess recall error or digit preference for TTP>12 months, which would presumably have greater recall error. While we found no obvious digit preference in our retrospective measure of TTP, previous studies have shown evidence of digit preference at 1,11 6, 19 and 12 cycles.19 It is uncertain how recall error may differ by pregnancy outcome in our study, though validity of recalled TTP after 10 years did not depend on pregnancy outcome in a previous study.11
Our results would be applicable to pregnant women who planned their pregnancy because recalled TTP is usually not assessed for unplanned pregnancies. There are limitations to the generalizability of our findings due to certain features of the study and study population that may have improved recall. First, women who volunteer for a prospective study of TTP, especially in the first month of trying, may be more vigilant than women who do not volunteer for a prospective study of TTP, and this may translate to more accurate recall. Second, study participation was associated with high educational attainment, which may indicate more accurate recall.20 These two limitations would not greatly affect generalizability if inferences are limited to women who both plan their pregnancy and volunteer for epidemiologic studies. Pregnancy planning itself tends to be associated with greater socioeconomic advantage, in terms of marital status, education, and household income.21 Third, the participants completed questionnaires during their pregnancy attempt, which may have improved recall accuracy compared with that from a pregnant mother in a retrospective TTP study. Fourth, the recall interval was short. For all these reasons, the estimates of error in this study may be viewed as a “best case scenario” for the extent of the recall error in TTP ≤ 12 months.
Studies of fertility and pregnancy outcomes often rely on recalled TTP. This study provides evidence that TTP ≤ 12 months recalled during the first trimester of pregnancy has reasonable validity. In future studies, our method for quantitative bias analysis of the FOR can help researchers explore the effect of recall error on their results.
Supplementary Material
Acknowledgments
The authors thank Ms. Tina Christensen for supporting data collection and media relations, Dr. Kristen Hahn for assisting with data management, and Dr. Daniel Brooks for providing comments on previous versions of the manuscript.
This study was supported by the National Institutes of Health (R21-HD050264) and the Danish Medical Research Council (271-07-0338). RGR was supported by training grant T32-HD052458 and by an NIH Intramural Research Training Award. The content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
References
- 1.Baird DD, Wilcox AJ, Weinberg CR. Use of time to pregnancy to study environmental exposures. American Journal of Epidemiology. 1986;124:470–80. doi: 10.1093/oxfordjournals.aje.a114417. [DOI] [PubMed] [Google Scholar]
- 2.Olsen J, Melbye M, Olsen SF, Sorensen TI, Aaby P, Andersen AM, et al. The Danish National Birth Cohort--its background, structure and aim. Scandinavian Journal of Public Health. 2001;29:300–7. doi: 10.1177/14034948010290040201. [DOI] [PubMed] [Google Scholar]
- 3.Magnus P, Irgens LM, Haug K, Nystad W, Skjaerven R, Stoltenberg C. Cohort profile: the Norwegian Mother and Child Cohort Study (MoBa) International Journal of Epidemiology. 2006;35:1146–50. doi: 10.1093/ije/dyl170. [DOI] [PubMed] [Google Scholar]
- 4.Baird DD, Weinberg CR, Rowland AS. Reporting errors in time-to-pregnancy data collected with a short questionnaire. Impact on power and estimation of fecundability ratios. American Journal of Epidemiology. 1991;133:1282–90. doi: 10.1093/oxfordjournals.aje.a115840. [DOI] [PubMed] [Google Scholar]
- 5.Zielhuis GA, Hulscher ME, Florack EI. Validity and reliability of a questionnaire on fecundability. International Journal of Epidemiology. 1992;21:1151–6. doi: 10.1093/ije/21.6.1151. [DOI] [PubMed] [Google Scholar]
- 6.Mikkelsen EM, Hatch EE, Wise LA, Rothman KJ, Riis A, Sorensen HT. Cohort profile: the Danish Web-based Pregnancy Planning Study--’Snart-Gravid’. International Journal of Epidemiology. 2009;38:938–43. doi: 10.1093/ije/dyn191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joffe M, Key J, Best N, Keiding N, Scheike T, Jensen TK. Studying time to pregnancy by use of a retrospective design. American Journal of Epidemiology. 2005;162:115–24. doi: 10.1093/aje/kwi172. [DOI] [PubMed] [Google Scholar]
- 8.Larsen U, Vaupel JW. Hutterite fecundability by age and parity: strategies for frailty modeling of event histories. Demography. 1993;30:81–102. [PubMed] [Google Scholar]
- 9.Jensen TK, Scheike T, Keiding N, Schaumberg I, Grandjean P. Fecundability in relation to body mass and menstrual cycle patterns. Epidemiology. 1999;10:422–8. doi: 10.1097/00001648-199907000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Mikkelsen EM, Riis AH, Wise LA, Hatch EE, Rothman KJ, Sorensen HT. Pre-gravid oral contraceptive use and time to pregnancy: a Danish prospective cohort study. Human Reproduction. 2013;28:1398–405. doi: 10.1093/humrep/det023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooney MA, Buck Louis GM, Sundaram R, McGuiness BM, Lynch CD. Validity of self-reported time to pregnancy. Epidemiology. 2009;20:56–9. doi: 10.1097/EDE.0b013e31818ef47e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye X, Skjaerven R, Basso O, Baird DD, Eggesbo M, Uicab LA, et al. In utero exposure to tobacco smoke and subsequent reduced fertility in females. Human Reproduction. 2010;25:2901–6. doi: 10.1093/humrep/deq235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cox DR, Oakes D. Analysis of Survival Data. New York: Chapman & Hall; 1984. [Google Scholar]
- 14.Fox MP, Lash TL, Greenland S. A method to automate probabilistic sensitivity analyses of misclassified binary variables. International Journal of Epidemiology. 2005;34:1370–6. doi: 10.1093/ije/dyi184. [DOI] [PubMed] [Google Scholar]
- 15.Tietze C. Fertility after discontinuation of intrauterine and oral contraception. International Journal of Fertility. 1968;13:385. [PubMed] [Google Scholar]
- 16.Greenland S, Lash TL. Bias Analysis. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. pp. 345–80. [Google Scholar]
- 17.Joffe M, Villard L, Li Z, Plowman R, Vessey M. A time to pregnancy questionnaire designed for long term recall: validity in Oxford, England. Journal of Epidemiology & Community Health. 1995;49:314–9. doi: 10.1136/jech.49.3.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tourangeau R, Rips LJ, Rasinski K. The Psychology of Survey Response. Cambridge, U.K: Cambridge University Press; 2000. The Role of Memory in Survey Responding; pp. 62–99. [Google Scholar]
- 19.Ridout MS, Morgan BJ. Modelling digit preference in fecundability studies. Biometrics. 1991;47:1423–33. [PubMed] [Google Scholar]
- 20.Unsworth N. Variation in working memory capacity, fluid intelligence, and episodic recall: A latent variable examination of differences in the dynamics of free recall. Memory & Cognition. 2009;37:837–49. doi: 10.3758/MC.37.6.837. [DOI] [PubMed] [Google Scholar]
- 21.Rasch V, Knudsen LB, Wielandt H. Pregnancy planning and acceptance among Danish pregnant women. Acta Obstet Gynecol Scand. 2001;80:1030–5. doi: 10.1034/j.1600-0412.2001.801111.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.