Introduction
Premenstrual dysphoric disorder (PMDD), the most severe form of a menstrually related mood disorder (MRMD), afflicts 5-8% of women of reproductive age (Kroll & Rapkin, 2006). The prevalence of clinically significant premenstrual symptoms that are characterized by impairment, treatment seeking, and suicide risk, but do not meet DSM-IV requirement for the presence of five different symptoms, raises the percentage of afflicted women to 13–19% (Angst, Sellaro, Merikangas, & Endicott, 2001; Bunevicius, Leserman, & Girdler, 2012; Spitzer, Williams, Kroenke, Hornyak, & McMurray, 2000). PMDD is characterized by the cyclic recurrence of affective and somatic symptoms in the luteal phase of the menstrual cycle, resulting in luteal phase impairment equivalent to that of major depression, panic disorder, and post-traumatic stress disorder (PTSD) (Kroll & Rapkin, 2006; Lystyk & Gerrish, 2006). The most frequent core symptoms of PMDD are irritability, anger conflict, and emotional lability, and as mindfulness has demonstrated effectiveness in addressing similar symptoms in previous research (Greeson, 2009), we rationalized that mindfulness may be efficacious in treating women who suffer from impairment and distress due to symptoms of PMDD.
Despite the efficacy of SSRIs and a low-dose oral contraceptive in PMDD (Freeman et al., 2001; Steiner et al., 2006; Yonkers et al., 2005), non-response rates are ≥ 40% (Freeman, Rickels, Sondheimer, & Polansky, 1999; Halbreich, 2008; Steiner et al.,1995) and nearly 50% of MRMD women prescribed SSRIs do not take them or discontinue within six months (Sundstrom-Poromaa, 2000). Research on behavioral interventions in MRMD is sparse, with three randomized trials (Blake, Salkovskis, Gath, Day, & Garrod, 1998; Hunter et al., 2002; Morse, Dennerstein, Farrell, & Varnavides, 1991). These previous studies supported the efficacy of cognitive therapy as equivalent to fluoxetine, and superior to hormone therapy and relaxation, for alleviating PMDD symptoms; however these studies are more than ten years old, the behavioral interventions were not manualized or well described, and there was no attempt to investigate mechanisms of efficacy. Ideally, intervention approaches should both arise from an understanding of mechanisms and simultaneously inform about the pathophysiology of the disorder.
Women with a MRMD exhibit dysregulation in cardiovascular stress reactivity (Girdler, Pedersen, & Light, 1995; Girdler et al., 1998; Klatzkin, Lindgren, Forneris, & Girdler, 2010) and greater sensitivity to laboratory pain stimuli (Fillingim, 1995; Fleischman, Bunevicius, Leserman, & Girdler, 2013; Straneva et al., 2002) than controls. By extension, the theoretical framework driving the choice of mindfulness training as an intervention in MRMD is derived from the evidence for its ability to modulate stress, arousal and emotion regulation (Greeson, 2009), which are key challenges for women with PMDD. Mindfulness is defined as bringing one's awareness to moment-to-moment experiences without judgment (Kabat-Zinn, 1994). Mindfulness training decreases blood pressure (Nyklicek, Mommersteeg, Van Beugen, Ramakers, Van Boxtel, 2013; Hughes et al., 2013) and is efficacious in treating pain syndromes (Greeson, 2009; Reiner, Tibi, & Lipsitz, 2013). A consequence of mindfulness training is the realization that most thoughts and emotions fluctuate or are transient (Baer, 2003) and that these momentary experiences can be simply acknowledged as mental phenomena rather than reality, and allowed to pass. Such a perspective makes mindfulness training well suited to MRMD, since MRMD symptoms fluctuate with the hormones that drive them. The purpose of our pilot study was to assess recruitment, feasibility, adherence and potential mechanisms of efficacy associated with mindfulness training, and to support whether a randomized controlled trial (RCT) should be conducted in women with PMDD symptoms.
Method
Participants
After the University of North Carolina IRB approved the study, women were recruited through newspaper advertisements and flyers posted in the community; also, women were contacted who were originally enrolled in a prospective MRMD diagnostic study that served as a feeder study for other research studies (Bunevicius et al., 2012; Fleischman et al., 2013) and as a registry for future contact. Women were evaluated for medical and psychiatric histories using the MINI psychiatric interview (American Psychiatric Association & American Psychiatric Association Task Force on DSM-IV, 2000; Sheehan et al., 1998). All women were in good health, without chronic medical conditions or current psychiatric disorders. Women were then prospectively evaluated for two to three menstrual cycles to determine MRMD status.
MRMD diagnosis
The Daily Record of Severity of Problems (DRSP) allows for the quantification of the severity of physical, emotional and behavioral symptoms using a 6-point scale (Endicott, Nee, & Harrison, 2006). In order to discourage retrospective reporting, forms were mailed back weekly. Each woman met the following criteria: (1) at least a 30% decrease in emotional symptom severity between the seven luteal phase days preceding menses compared with follicular phase days 4–10; (2) a rating of emotional symptoms as moderate, severe or extreme on at least two of the seven premenstrual days; (3) remission of symptoms shortly after the onset of menses followed by a clear symptom-free period during the early-to-mid follicular phase and (4) criteria 1-3 met in at least two menstrual cycles (Endicott et al., 2006; Rubinow, Roy-Byrne, Hoban, Gold, & Post, 1984).
Twenty-eight women from the MRMD registry were invited to participate; 24 enrolled (80% recruitment rate), and 21 completed the MBSR class. Recent medical and psychiatric history were reviewed to determine if participants were still free of any current psychiatric disorder and chronic medical condition affecting eligibility. Additional eligibility required women to be 18-52 years of age with intact ovaries and not pregnant or nursing. After eligibility was established, the study was explained to women in detail by the study coordinator and women provided written consent. A brief, 11-item version of the DRSP form for PMDD symptoms was reviewed. Participants completed the daily ratings throughout the 12-week study period.
Data included in this manuscript are from two separate pilot studies (Pilot 1, n = 9; Pilot 2, n = 12). Procedures were identical in the two pilots except that two additional questionnaires were administered in the second pilot: the ruminative and reflection questionnaire (RRQ) and the self-compassion scale (SCS). Also, two different instructors taught the mindfulness intervention, both of whom were well trained and experienced in teaching the Mindfulness Based Stress Reduction (MBSR) curriculum as taught through the Center for Mindfulness at University of Massachusetts Medical Center.
Procedure
Daily Record of Severity of Problems (DRSP; Endicott et al., 2006)
Eleven items from this scale were used to evaluate the severity of core emotional (depression, hopelessness, worthlessness, anxiety, mood swings, sensitivity, irritability, conflict with others) and physical symptoms (sleeplessness, headache, and joint pain) of PMDD. The DRSP was completed daily and returned each week to the study coordinator.
Laboratory testing
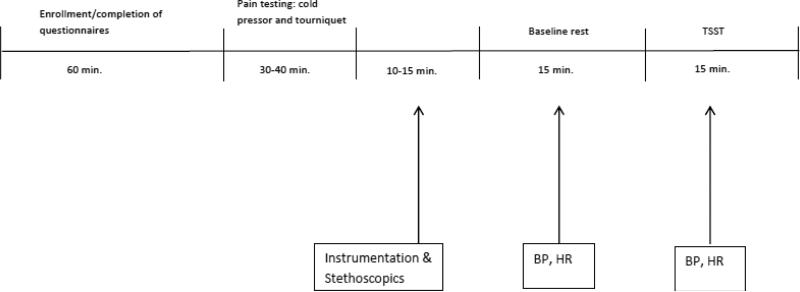
All participants were tested during the first two weeks before starting the MBSR program (weeks 1 and 2) and within two weeks after completing the MBSR intervention (weeks 11 and 12). Testing involved: 1) Pain Testing; 2) Instrumentation for blood pressure (BP) and heart rate (HR); 3) Recovery and Pre-stress Baseline Rest; and 4) Trier Social Stress Test (TSST; Fig. 1).
Fig. 1.
Laboratory Protocol
Pain Testing Procedures
Participants were exposed to two pain tests with a five-minute recovery imposed between tests. The cold pressor test was presented first, followed by the tourniquet procedure. Both tests have been shown to differentiate MRMD women from non-MRMD controls (Fleischman et al., 2013).
The hand cold pressor
A container was filled with ice and water maintained at 4° C. At the onset of the test, participants submerged their hand to their wrist and kept their hand still. The use of a water circulator prevented the water from warming near the participant's hand. Participants indicated when the sensations in their hand first became painful (pain threshold) and when they were no longer willing or able to tolerate the pain (pain tolerance). Immediately before removing their hand, participants rated the pain for intensity and unpleasantness using a visual analogue scale (0 – 100). A maximum time limit of five minutes was imposed though participants were not informed of this limit.
The submaximal effort tourniquet procedure
The participant's arm was raised for 30 seconds to promote venous drainage and then the tourniquet cuff positioned on the arm was rapidly inflated to 200 mmHg (via the Hokanson E20 Rapid Cuff Inflator) and the arm returned to the participant's side. To promote forearm ischemia, participants engaged in 20 handgrip exercises at 30% of maximum force with an inter-squeeze interval of two seconds. Participants verbally indicated when the sensations in their arm first become painful (pain threshold) and when they are no longer willing or able to tolerate the task (pain tolerance). Before deflating the cuff, participants rated both the intensity and the unpleasantness of the pain using the visual analogue scale. A maximum time limit of 20 minutes was imposed though participants were not informed of this limit.
Recovery and baseline rest
Participants sat quietly alone in a comfortable chair for 15 minutes. The first 10 minutes served as recovery from pain testing, while the last five minutes constituted the baseline from which to calculate cardiovascular reactivity to the stress test. BP and HR were taken at minutes 11, 13, and 15 and averaged.
The Trier social stress test (TSST; Kirschbaum, Pirke, & Hellhammer, 1993)
This is a well validated test that induces large BP and HR responses (Kirschbaum, Strasburger, & Langkrar, 1993; von Kanel, Kudielkac, Preckelb, Hanebuthb, & Fischerb, 2006) and involves the following components:
Pre-task instructions.
Participants were introduced to one or two people (the ‘selection committee’) after which the experimenter asked the participant to take over the role of a job applicant who was invited for a personnel interview with the company's staff managers (the selection committee). Participants were instructed that they would be tape-recorded and video-recorded and that the managers were trained to monitor nonverbal behavior.
Anticipation
The participant prepared her talk for five minutes in the presence of the committee. During this time, she was permitted to take notes.
Speech
The committee asked the participant to deliver her talk for five minutes. If the participant finished her talk before five minutes, the committee responded with prepared questions to ensure that the participant spoke for the entire time.
Serial subtraction
The committee then asked the participant to subtract the number seven from 2,000 as fast and as accurately as possible for five minutes. For each mistake, the participant was instructed to restart at 2,000.
BP and HR were taken at minutes 0, 2, 4, 6, and 9 during the baseline period, and at minutes 0, 2, and 4 during the anticipation, speech, and subtraction phases of the TSST. The values within each period were then averaged to establish a mean blood pressure and heart-rate value for each period. The Suntech Exercise BP monitor, Model 4240 (SunTech Medical Instruments, Inc., Raleigh, NC) was used to provide automated measurement of BP and HR. The Suntech Exercise BP monitor uses the auscultatory technique, with R-wave Gating, and is accurate within ±2 mmHg between 0 mmHg and 300 mmHg. Prior to initiating the initial rest period, three standard stethoscopic blood pressures were taken with the automated pressures in order to ensure correct microphone placement and cuff positioning.
Mindfulness based stress reduction (MBSR)
This program, developed by Jon Kabat-Zinn at the University of Massachusetts Medical Center, was implemented with minimal adaptation. It was conducted in a small group setting and delivered by trained MBSR instructors from the UNC Program on Integrative Medicine. The intervention included two-hour sessions for eight consecutive weeks plus a Saturday retreat near the end of the intervention. The Saturday retreat was modified from six hours to four hours.
Class 1: Introduction to the body scan, a practice to facilitate non-judgmental awareness of physical sensations, and an eating meditation that focused on differentiating physical sensations from thoughts.
Class 2: Introduction to sitting meditation with awareness of breathing as the primary object of attention.
Class 3: Introduction to gentle mindful yoga movements as a way of bringing awareness to subtle movements of the body.
Class 4: Introduction of walking meditation; the psychophysiology of the stress response was discussed.
Class 5: Sitting meditation was expanded to include awareness of thoughts arising and passing away, and discussion included the role of mindfulness in responding to stress in everyday life.
Class 6: Working with strong emotions was discussed as well as expanding the inner resources for emotional resilience.
Saturday Half-Day Retreat
Introduction to the concept of “functional silence”. Participants engaged in staff-led sitting meditation sessions, alternating with walking meditation, mindful yoga, and the body scan. Lunch was held in silence. In the afternoon, there was an introduction to loving-kindness meditation. Discussion at the end of the day allowed participants to share their experiences, challenges, and insights.
Class 7: Introduction to ‘choiceless awareness’ (a practice in which one is fully aware of the moment, yet not focused on any physical or mental image or object); awareness of how we nourish our bodies.
Class 8: A review of the course and cultivating resources for continued practice was discussed.
Measures
All questionnaires were completed both before and after the eight-week MBSR intervention.
Outcome Measures
Daily Record of Severity of Problems (DRSP; Endicott et al., 2006)
Eleven items from this scale were used to evaluate the severity of core emotional (depression, hopelessness, worthlessness, anxiety, mood swings, sensitivity, irritability, conflict with others) and physical symptoms (sleeplessness, headache, and joint pain) of PMDD.
Pain Sensitivity
For both the hand cold pressor (Mitchell, Macdonald, & Brodie, 2004) and submaximal effort tourniquet procedures (Moore, Duncan, Scott, Gregg, & Ghia, 1979), measures of pain threshold, tolerance, intensity and unpleasantness were assessed. Participants informed the task administrator when the onset of pain first occurred (threshold) and when pain could no longer be tolerated (tolerance), and number of seconds for each was noted. At the end of each task, participants rated pain on a visual analogue scale (0 being “no pain”, and 100 being “the worst pain imaginable”) for both pain intensity (the strength of the pain) and pain unpleasantness (the degree to which the pain was bothersome). Reliability and validity of both pain measures has been established (Edens & Gil, 1995).
Potential Mediators
Pain catastrophizing scale (PCS; Sullivan, Bishop, & Pivik, 1995) evaluates participants’ relationship to their pain. This scale assesses thoughts and feelings associated with pain in three domains: ruminating, magnifying, and hopelessness. Construct validity and temporal stability have been established (Sullivan, Bishop & Pivik, 1995).
Rumination and reflection questionnaire (RRQ; Trapnell & Campbell, 1999) differentiates between the rumination (anxious self-focus) and reflection (inquisitiveness self-focus) facets of private self-consciousness. The rumination and reflection subscales each contain 12 items and responses are given on a 5-point Likert scale. A Cronbach's alpha of .90 has been reported for the rumination subscale and .91 for the reflection subscale. Discriminant and concurrent validity have been established through comparisons with related scales (Trapnell & Campbell, 1999).
Five Facet Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) is a 39-item scale that measures the construct of mindfulness. Five facets compose the constructs: observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience. Items were rated on a 5-point scale ranging from 1 (never or very rarely true) to 5 (very often or always true). Higher scale scores indicate higher overall mindfulness. The five factors demonstrate good internal consistency with Cronbach alphas ranging from .72 - .92 (Baer et al., 2008; Christopher, Neuser, & Baitmangalkar, 2012), and construct validity has been established (Baer et al, 2008).
Self-compassion Scale (SCS; Neff, 2003) is a 26-item scale that measures self-compassion, defined as “holding one's feelings of suffering with a sense of warmth, connection, and concern” (Neff & McGehee, 2010, p. 226). This scale comprises the three facets of self-compassion measured as six subscales: mindfulness vs. over-identification, self-kindness vs. self-judgment, and common humanity vs. isolation. Internal consistency for this scale is excellent (Cronbach's alpha = .93; Neff, 2003) and construct validity has been established through positive associations with the Social Connectedness scale and three subscales of the Trait-Meta Mood Scale, and negative associations with the self-criticism subscale of the Depression Experience Questionnaire (Neff, 2003).
Beck Depression Inventory (BDI; Beck & Beamesdefer, 1974) is a widely used well-validated 21-item self-report measure that assesses depressive symptoms. A meta-analysis of internal consistency of this scale reported a reliability of .81 for non-psychiatric patients. Concurrent validity for non-psychiatric individuals with the Hamilton Psychiatric Rating Scale for Depression and clinical ratings were good; correlations with these measures were .74 and .60, respectively (Beck, Steer, & Carbin, 1988).
Spielberger State Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970) is a widely used 20-item self-report scale in which respondents rate their current levels of anxiety on a 4-point Likert scale, ranging from 1 (not at all) to 4 (very much so). Reported reliabilities range from .65 to.96 (Barnes, Harp, & Jung, 2002).
Process Evaluations
Stress Reduction Questionnaire was used at the end of the second laboratory session to evaluate whether participants used any stress reduction skills during the laboratory protocol. This five-item questionnaire created for this study asked questions such as: What stress reduction skills, if any, did you use during today's session? and Did you use these skills when you felt pain? If yes, to what extent did they help you to tolerate pain?
MBSR questionnaire was created for this study and administered during the last MBSR session to evaluate experiences during the MBSR program. On a Likert scale ranging from 1(not at all) to 5 (very much), participants were asked to respond to eight questions. Examples of these questions include: To what extent has participation in this course impacted your ability to manage your stress and PMDD symptoms? and To what extent have you made changes in your daily activities as a result of this course?
Compliance Measure
MBSR diary assessed the daily recorded number of minutes spent with each MBSR practice each day at home. Participants were also asked to indicate the amount of time spent on each type of activity (i.e., mindful breathing, yoga, loving-kindness meditation). These diaries were returned weekly to the study coordinator at each MBSR class session.
Historical Control Comparison Groups
Sixty-one women who had entered the MRMD diagnostic feeder study described above and met MRMD criteria were used as historical control groups. For a different protocol (Bunevicius et al., 2013; Klatzkin, Bunevicius, Forneris, & Girdler, 2014), these women had completed daily mood ratings using the DRSP over several months and 39 of the women had undergone pain testing with both pain tests on two occasions approximately eight weeks apart. However, these women had no intervention over the course of their participation. The 61 women provided a control for repeated symptom monitoring and the 39 woman subgroup served as the control for habituation to repeated pain testing. No significant differences existed between the MBSR group and the control group in age, minority distribution, or psychiatric histories (Table 1).
Table 1.
Demographics of Sample
| Mindfulness (n=21) | Historical Control for DRSP (n=61) | Historical Control for Pain Measures (n = 39) | |
|---|---|---|---|
| Mean Age | 38 | 34 | 35 |
| Race/Ethnicity (%) | |||
| Caucasian | 74 | 67 | 67 |
| African American | 22 | 23 | 23 |
| Hispanic | 4 | 5 | 5 |
| Asian | 0 | 3 | 3 |
| Native American | 0 | 2 | 3 |
| % Depression | 52 | 41 | 44 |
| % Anxiety | 10 | 8 | 8 |
| % PTSD | 10 | 10 | 8 |
| % Alcohol abuse | 7 | 11 | 10 |
| % Substance abuse | 0 | 8 | 10 |
Data Analyses
Mean luteal phase symptom severity derived from the DRSP instrument completed during the diagnostic study served as the baseline comparison from which to assess MBSR-related change. Paired t-tests were conducted for each of the 11 symptoms to assess change from pre to post MBSR. For the control group, DRSP measures for the same symptoms were assessed over an 8–12 week rating period. For each symptom, change scores were created (mean luteal phase severity level at the end of the ratings period – mean luteal phase severity level at the beginning of the rating period) and independent t-tests were conducted to assess group differences in the change in symptom severity over time.
For each pain measure (threshold, tolerance, intensity, unpleasantness), change scores were created (mean post intervention level – mean pre intervention level) and analyzed using independent t-tests. Similarly for the control group, change scores were created for each measure (mean week 8 pain level minus mean week 1 level) and independent t-tests were conducted to assess group differences in pain sensitivity over time.
For SBP, DBP, and HR, cardiovascular reactivity stress scores were created separately for the pre-intervention and post-intervention sessions (mean stressor level – mean baseline rest level). Then, pre- versus post-intervention differences in reactivity were analyzed separately for each cardiovascular measure and each stressor condition (anticipation, speech, and math) using paired t-tests.
Potential mediators (BDI, STAI, PCS, RRQ, SCS, FFMQ) were analyzed using paired t-tests. All analyses were conducted using SPSS 20.
Results
Twenty-eight participants were initially recruited for the study. Two withdrew prior to enrollment (one due to travel distance from the study, one due to an Axis 1 psychiatric diagnosis), two withdrew after enrollment but prior to the start of the intervention (one due to busy schedule, one for unknown reason), and three withdrew after week two of the intervention (one due to new job, one due to illness, and one due to heightened anxiety). Therefore, of those who began the mindfulness classes, 88% (n = 21) completed the classes and all post-intervention measures. The intervention covered eight classes (or 49 days, including the first and last class). Overall, participants engaged in some type of mindfulness practice at home 80% of the days, for a mean of 131 minutes per week.
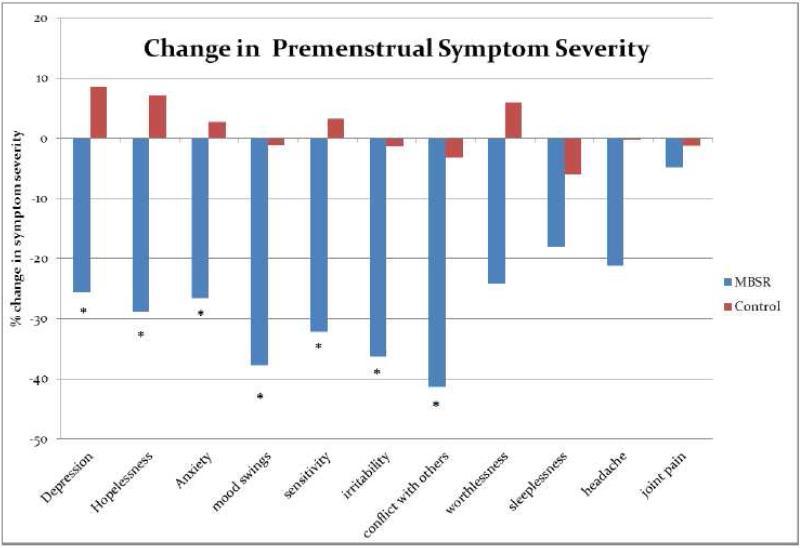
In relation to the DRSP, there was a significant decrease from pre- to post-MBSR training in premenstrual ratings of depression (t(19) = 3.27, p =.004), hopelessness (t(19) = 2.43, p =.025), anxiety (t(19) = 3.66, p =.002), mood swings (t(19) = 7.60, p < .001), sensitivity (t(19) = 3.39, p =.003), irritability (t(19) = 4.92, p < .001), and conflict with others (t(19) = 4.82, p < .001). The magnitude of symptom severity in worthlessness (t(19) = 1.70, ns), sleeplessness (t(19) = 1.42, ns), headache (t(19) = 1.61, ns), and joint pain (t(19) = 0.35, ns) did not decrease significantly. For the control group, no change was observed in any of the 11 symptom ratings over the eight-week period. Consequently, there was a significant difference in change scores between the two groups in depression (t(79) = 3.75, p < .001), hopelessness (t(79) = 3.02, p = .003), anxiety (t(79) = 2.88, p = .005), mood swings (t(79) = 4.53, p < .001), sensitivity (t(79) = 4.07, p < .001), irritability (t(79) = 3.76, p < .001), conflict with others (t(79) = 4.11, p < .001), and worthlessness (t(24) = 2.45, p = .017). There was no difference between the groups in change scores in sleep problems (t(79) = .95, ns) headaches (t(79) = .84, ns), and joint pain (t(25) = 0.36, ns) (see Table 2, Fig. 2).
Table 2.
Means and (SD) for Daily Symptom Ratings for MRMD Women Pre and Post MBSR Training
| Daily MRMD Symptoms | MBSR Intervention (n = 21) | Control (n = 61 for Daily Symptoms; n = 39 for Pain Symptoms) | ||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| depression** | 3.31 (1.14) | 2.47 (1.24) | 2.62 (1.00) | 2.84 (1.08) |
| hopelessness* | 2.28 (1.32) | 1.74 (1.06) | 2.06 (1.01) | 2.21 (1.14) |
| worthlessness | 2.39 (1.40) | 1.81 (1.22) | 2.13 (1.07) | 2.26 (1.31) |
| anxiety** | 3.80 (1.17) | 2.79 (1.14) | 3.08 (1.10) | 3.16 (1.04) |
| mood swings** | 3.85 (1.13) | 2.39 (1.05) | 3.04 (1.11) | 3.01 (1.05) |
| sensitivity** | 3.41 (1.30) | 2.20 (1.21) | 2.85 (1.10) | 2.94 (1.14) |
| irritability** | 4.03 (1.00) | 2.57 (1.18) | 3.30 (0.97) | 3.26 (.95) |
| conflict with others** | 3.47 (1.01) | 1.94 (0.97) | 2.76 (1.14) | 2.67 (1.08) |
| sleeplessness | 2.70 (1.41) | 2.21 (0.98) | 2.57 (1.22) | 2.41 (1.27) |
| headache | 1.96 (1.12) | 1.54 (1.07) | 1.97 (1.00) | 1.97 (1.04) |
| joint pain | 2.54 (1.32) | 2.42 (1.54) | 2.21 (1.12) | 2.24 (1.20) |
| Pain Sensitivity | ||||
| Cold pressor | ||||
| threshold | 14.10 (8.34) | 35.76 (63.29) | 24.49 (47.00) | 21.49 (46.90) |
| tolerance* | 68.14 (98.15) | 111.52 (120.08) | 75.08 (98.01) | 67.05 (102.47) |
| intensity | 45.24 (16.24) | 48.48 (20.22) | 54.95 (21.28) | 57.54 (23.60) |
| unpleasantness | 42.62 (20.35) | 50.00 (21.97) | 54.74 (23.60) | 61.18 (25.53) |
| Tourniquet | ||||
| threshold | 256.29 (286.77) | 293.76 (294.29) | 248.72 (273.31) | 187.17 (204.92) |
| tolerance | 512.10 (384.25) | 637.43 (407.50) | 480.03 (318.51) | 403.84 (351.25) |
| intensity | 40.25 (16.82) | 37.71 (22.94) | 40.26 (20.61) | 41.28 (18.13) |
| unpleasantness | 34.95 (24.00) | 43.57 (22.20) | 40.64 (17.63) | 46.36 (23.50) |
indicates significant difference in intervention group at the .05 level (2-tailed) pre to post in the MBSR group,
indicates significance pre to post at the .01 level. There were no significant pre-post differences in the control group.
Fig. 2.
Change in Premenstrual Severity from pre- to post-MBSR intervention; * indicates p < .05
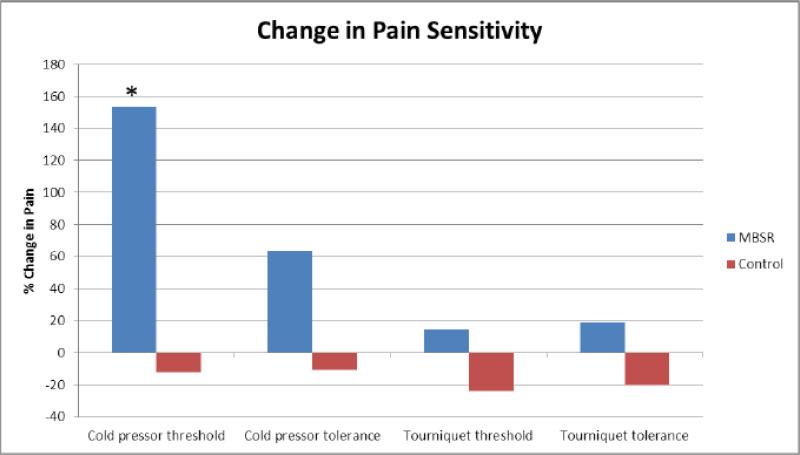
An increase in pain tolerance to the cold pressor task was observed from pre to post MBSR intervention (t (20) = −2.46, p = .02), which was significantly different from that of the control group (t (58) = −2.53, p = .02), for whom no change in cold pressor tolerance occurred over eight weeks (Fig. 3). No significant effects emerged for cold pressor pain threshold (t (20) = −1.64, ns), intensity (t (20) = −.98, ns) or unpleasantness ratings (t (20) = −1.70, ns) (Table 2). There were no significant effects for the submaximal effort tourniquet test.
Fig. 3.
Change in Pain Measures from pre- to post-MBSR intervention, * p < .05
Significant decreases were observed from pre to post intervention in the anticipation phase of the TSST for systolic BP and HR reactivity (t(20) = 2.16, p = .04 and t(20) = 2.71, p = .01, respectively) and a trend for reduced diastolic BP reactivity (t(20) = 1.90, p = .07). There was also a trend for reduced heart rate reactivity from pre to post intervention during the speech (t(20) = 1.90, p = .07) (Table 3).
Table 3.
Mean and (SD) for Potential Mediators and Laboratory Stress data (n = 21)
| Pre | Post | |
|---|---|---|
| TRIER | ||
| Preparation (mean - baseline) | ||
| Heart rate* | 13.68 (11.04) | 8.24 (5.83) |
| Systolic BP* | 10.76 (10.04) | 6.06 (6.00) |
| Diastolic BP | 6.94 (6.33) | 3.98 (5.73) |
| Speech (mean - baseline) | ||
| Heart rate | 15.41 (9.52) | 12.51 (8.31) |
| Systolic BP | 17.95 (8.46) | 15.79 (7.04) |
| Diastolic BP | 11.93 (5.58) | 11.04 (5.86) |
| Math (mean - baseline) | ||
| Heart rate | 10.26 (9.17) | 9.12 (7.35) |
| Systolic BP | 11.37 (7.12) | 11.35 (6.55) |
| Diastolic BP | 10.44 (4.96) | 8.37 (5.67) |
| Pain Catastrophizing Scale | ||
| Global | 12.70 (9.49) | 8.20 (10.38) |
| Rumination* | 5.80 (4.25) | 3.40 (4.01) |
| Magnification* | 2.60 (2.39) | 1.50 (2.04) |
| Rumination and Reflection Questionnaire | ||
| Rumination | 16.64 (6.62) | 18.89 (4.56) |
| Reflection | 13.85 (5.97) | 14.27 (3.75) |
| Self-compassion Scale | ||
| Self-kindness** | 2.71 (.87) | 3.35 (.95) |
| Self-judgment | 3.16 (1.00) | 2.97 (1.09) |
| Common humanity** | 3.43 (.81) | 3.95 (.81) |
| Isolation | 2.93 (1.07) | 2.80 (1.11) |
| Mindfulness | 3.30 (.59) | 3.50 (1.08) |
| Overidentification | 3.23 (1.03) | 3.02 (1.03) |
| Five facet Mindfulness Questionnaire | ||
| Observing* | 27.20 (4.32) | 30.45 (4.55) |
| Describing | 29.35 (7.15) | 29.65 (7.46) |
| Acting with Awareness* | 22.40 (5.93) | 24.90 (7.77) |
| Nonjudging** | 23.90 (6.77) | 29.30 (7.95) |
| Nonreacting | 19.30 (5.54) | 21.60 (6.36) |
| Beck Depression Inventory | 8.08 (5.11) | 6.58 (6.63) |
| Spielberger State Anxiety Scale | 44.53 (4.17) | 45.05 (3.89) |
| Spielberger Trait Anxiety Scale | 47.30 (4.27) | 47.20 (4.53) |
indicates significance at the .05 level (2-tailed),
indicates significance at the .01 level (2-tailed)
Reductions from pre to post MBSR were observed in ruminating on pain (t (19) = 2.43, p = .03) and magnifying pain (t (19) = 2.40, p = .03), while the global pain score only tended to decrease (t (19) = 1.95, p = .07). There was also no change in either the rumination or reflection subscale of the RRQ from pre to post MBSR: (t(10) = 1.34, p = ns; t (10) = −.76, p = ns; respectively). An increase from pre- to post-MBSR was observed in the subscales self-kindness (t (10) = −3.22, p = .009) and common humanity (t (10) = −3.20, p = .009) of the SCS, although there were no changes in self-judgment, isolation, mindfulness or over-identification. There was an increase from pre to post MBSR in the FFMQ facets of observing (t (19) = −2.77, p = .01), acting with awareness (t (19) = −2.28, p = .03), and non-judging inner-experience (t (19) = −3.93, p = .001), though not with describing and non-reacting to inner experience. There was no change in depression from pre to post MBSR (t (11) = .765, p = ns).There was also no change in either state or trait anxiety from pre to post (state: t(18) = −.592, p = ns); trait: t(19) = .122, p = ns) (Table 3).
Participants shared positive reflections on their experience of the MBSR course. Although one participant indicated her tentativeness with the practice, “[The course] was overall a good experience. I am unsure of my ability to relax and meditate”, the other participants felt the course had a profound impact on the way in which they experienced their lives, stating that it was “eye-opening” and that “It changed my life” and “[It gave me] ...tools to help manage my emotions and stress when I feel out of control; I can have control.”
All women indicated that they used one or more tools that they had learned in the MBSR course while undergoing the post stress and pain testing procedures. Ninety-five percent (n = 20) used a breathing technique, 62% (n = 13) used a body scan, 20% (n = 4) used observing physical sensations, 14% (n = 3) used noticing thoughts and letting them go or loving-kindness, and 5% (n = 1) employed visualization or stretching.
Discussion
The results of this pilot suggest that the standard MBSR course is acceptable, well-tolerated and potentially beneficial in women with a MRMD. Eighty-eight percent of the women who began the intervention completed not only the full program but also all post-intervention laboratory assessments. This rate is consistent with other reports of participants with mood disorders in MBSR classes (Lee et al., 2007; Ma & Teasdale, 2004; Vollestad, Sivertsen, & Nielsen, 2011). Similarly, self-reported rates of daily mindfulness practice were on par with other reports (Vettese, Toneatto, Stea, Nguyen, & Wang, 2009). The process measures obtained support the retention and compliance data in that the majority of women were employing one or more of the mindfulness-based techniques to reduce their stress in the laboratory. Additionally, data from the MBSR diary support that the women were also applying these skills in their lives.
Although the self-report nature of the home-practice data may be viewed as a limitation, it is corroborated by the primary outcome data. There were clinically and statistically significant reductions in seven premenstrual emotional symptoms following MBSR training, and these reductions were significantly greater than changes seen in the historical control group, for which there was no change in symptom severity with daily ratings alone. The efficacy of MBSR to have beneficial effects on mood symptoms in controlled trials has been previously demonstrated (Greeson, 2009; Khoury et al., 2013), but this is the first demonstration that it may be efficacious for premenstrual symptoms using daily prospective ratings in a population who suffer from a MRMD.
In contrast, there was no evidence for improvement with MBSR in feelings of worthlessness, sleep, headache pain or joint pain severity. Lack of significant change in feelings of worthlessness is unexpected, given the finding of significant decrease in a similar variable, hopelessness; however, there were trends towards a decrease in sense of worthlessness. Small sample size and reduced statistical power may have contributed to the absence of an effect. Findings for lack of significant change in sleep, headache pain or joint pain severity are consistent with other literature showing greater MBSR-related improvements in psychological compared with physical domains of function (Khoury et al., 2013). In this case, the small sample size and reduced statistical power may have contributed to the absence of an effect for these measures, at least for sleep and headache.
Nonetheless, it was surprising that no effect of MBSR was seen for either headache or joint pain when MBSR was associated with significant reductions in pain sensitivity to the cold pressor test. The increase in cold pain tolerance was unlikely related to habituation since no effect of repeat testing on cold pain sensitivity was seen in the control group. Moreover, MBSR was not associated with a decrease in pain sensitivity to the tourniquet forearm ischemic pain test, suggesting that the ability of MBSR to beneficially modify pain sensitivity may depend, in part, on the pain modality. Indeed, three studies which utilized brief mindfulness interventions (Feuille & Pargament, 2013; Kingston, Chadwick, Meron, & Skinner, 2007; Liu, Wang, Chang, Chen, & Si, 2013) have reported that mindfulness practice decreases sensitivity to the cold pressor pain test. Evidence suggests that sensitivity to tourniquet-induced ischemic pain may involve endogenous opioid mechanisms (Frid, Singer, Oei, & Rana, 1981; Frid, Singer, & Rana, 1979), whereas sensitivity to cold pressor pain may be mediated by adrenergic mechanisms (Girdler et al., 2005). Thus, the possibility exists that different endogenous pain regulatory mechanisms may be differentially modulated by the MBSR intervention.
A number of controlled studies have reported that MBSR is associated with reductions in blood pressure responses to stress (Chen, Yang, Wang, & Zhang, 2013; Kingston et al., 2007; Nyklicek et al., 2013; Parswani, Sharma, & Iyengar, 2013), consistent with MBSR modulation of adrenergic physiology (e.g., blood pressure). This study also found that MBSR was associated with statistically significant reductions in heart rate and systolic blood pressure stress reactivity. Although the results are limited by the absence of a control group for habituation of cardiovascular reactivity, other studies with the Trier Social Stress Test show that although habituation is evident, stress reactivity continues to be significant even when the test occurs over five consecutive days (Kirschbaum, Pirke, & Hellhammer, 1993).
In addition to any MBSR-related reductions in cardiovascular stress reactivity that may serve as a potential mediator to the observed beneficial changes in symptoms and cold pain sensitivity, we also identified other potential mediators in this population to be tested in subsequent research. These include the mindfulness characteristics of observing, acting with awareness and non-judging inner-experiences; the self-kindness and common humanity components of self-compassion; and pain rumination and magnification. Of interest, there was no evidence in this cohort that general rumination changed with MBSR, nor did depressive or anxious symptoms unrelated to the menstrual cycle.
Conclusion
This pilot study supports testing the efficacy of the standard MBSR program for women with a MRMD in a controlled trial. Should it prove to be efficacious, investigating other interventions which incorporate mindfulness as a component, such as Mindful Self-Compassion, is warranted. These would provide alternative viable behavioral interventions for a disorder for which current available treatment options are limited. Although this study suffers from the usual limitations inherent in pilot research, such as a small sample size and lack of an active control comparator group, the feasibility and adherence data are encouraging and the availability of the historical control groups for symptom and laboratory pain measures reported herein strengthens the reliability of the primary outcome findings. Moreover, this study identified potential mediators of MBSR-related improvement. Future studies of biological and psychological mediators of MBSR-related benefit, not only in women with a MRMD but in other patient populations, would advance our understanding of mechanisms by which MBSR ameliorates psychological and medical suffering as well as further our understanding of the pathophysiology of stress-related disorders.
Acknowledgements
Funding was provided in part by grant number T32AT003378-04 from the National Center on Complementary and Alternative Medicine (NCCAM) and grant number R01 MH099076 from the National Institute of Mental Health (NIMH) at the National Institutes of Health (NIH). Analyses and conclusions are the responsibility of the authors rather than the funders.
Contributor Information
Karen Bluth, Program on Integrative Medicine, Department of Physical Medicine and Rehabilitation, School of Medicine, University of North Carolina-Chapel Hill, Chapel Hill, NC.
Susan Gaylord, Program on Integrative Medicine, Department of Physical Medicine and Rehabilitation, School of Medicine, University of North Carolina-Chapel Hill, Chapel Hill, NC.
Khanh Nguyen, Department of Psychiatry, School of Medicine, University of North Carolina-Chapel Hill, Chapel Hill, NC.
Adomas Bunevicius, Lithuanian University of Health Science, Institute of Neurosciences, Laboratory of Clinical Research, Kaunas, Lithuania.
Susan Girdler, Department of Psychiatry, School of Medicine, University of North Carolina-Chapel Hill, Chapel Hill, NC.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders : DSM-IVTR. 4th ed American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Angst J, Sellaro R, Merikangas KR, Endicott J. The epidemiology of perimenstrual psychological symptoms. Acta Psychiatrica Scandinavica. 2001;104(2):110–116. doi: 10.1034/j.1600-0447.2001.00412.x. doi: acp412. [DOI] [PubMed] [Google Scholar]
- Baer R. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology Science and Practice. 2003;10:125–143. [Google Scholar]
- Baer R, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JM. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;3:329–42. doi: 10.1177/1073191107313003. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Barnes LLB, Harp D, Jung WS. Reliability generalizations of scores on the Spielberger state-trait anxiety inventory. Educational and Psychological Measurement. 2002;62:603–615. [Google Scholar]
- Beck AT, Beamesdefer A. Assessment of depression: The depression inventory. In: Pichot P, editor. Psychological Measurements in Psychopharmacology: Modern Problems in Pharmacopsychiatry. Vol. 7. Basel; Paris, Karger: 1974. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Blake F, Salkovskis P, Gath D, Day A, Garrod A. Cognitive therapy for premenstrual syndrome: a controlled trial. Journal of Psychosomatic Research. 1998;45(4):307–318. doi: 10.1016/s0022-3999(98)00042-7. doi: S0022399998000427. [DOI] [PubMed] [Google Scholar]
- Bunevicius A, Leserman J, Girdler SS. Hypothalamic-pituitary-thyroid axis function in women with a menstrually related mood disorder: association with histories of sexual abuse. Psychosomatic Medicine. 2012;74(8):810–816. doi: 10.1097/PSY.0b013e31826c3397. doi: 10.1097/PSY.0b013e31826c3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunevicius A, Rubinow DR, Calhoun A, Leserman J, Richardson E, Rozanski K, Girdler SS. The association of migraine with menstrually related mood disorders and childhood sexual abuse. Journal of Womens Health (Larchmont) 2013;22(10):871–876. doi: 10.1089/jwh.2013.4279. doi: 10.1089/jwh.2013.4279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Yang X, Wang L, Zhang X. A randomized controlled trial of the effects of brief mindfulness meditation on anxiety symptoms and systolic blood pressure in Chinese nursing students. Nurse Education Today. 2013;33(10):1166–1172. doi: 10.1016/j.nedt.2012.11.014. doi: 10.1016/j.nedt.2012.11.014. [DOI] [PubMed] [Google Scholar]
- Christopher MS, Neuser MJ, Baitmangalkar A. Exploring the psychometric properties of the five facet mindfulness questionnaire. Mindfulness. 2012;3:124–131. [Google Scholar]
- Edens JL, Gil KM. Experimental induction of pain: Utility in the study of clinical pain. Behavior Therapy. 1995;26:197–216. [Google Scholar]
- Endicott J, Nee J, Harrison W. Daily Record of Severity of Problems (DRSP): reliability and validity. Archives of Womens Ment al Health. 2006;9(1):41–49. doi: 10.1007/s00737-005-0103-y. [DOI] [PubMed] [Google Scholar]
- Feuille M, Pargament K. Pain, mindfulness, and spirituality: A randomized controlled trial comparing effects of mindfulness and relaxation on pain-related outcomes in migraineurs. Journal of Health Psychology. 2013 doi: 10.1177/1359105313508459. doi: 10.1177/1359105313508459. [DOI] [PubMed] [Google Scholar]
- Fillingim RB, Girdler SS, Booker DK, Light KC, Harris MB, Maixner W. Pain sensitivity in women with premenstrual dysphoric disorder: A preliminary report. Journal of Womens Health (Larchmt) 1995;4:367–374. [Google Scholar]
- Fleischman DS, Bunevicius A, Leserman J, Girdler SS. Menstrually Related Mood Disorders and a History of Abuse: Moderators of Pain Sensitivity. Health Psychology. 2013 doi: 10.1037/a0031900. doi: 10.1037/a0031900. [DOI] [PubMed] [Google Scholar]
- Freeman EW, Kroll R, Rapkin A, Pearlstein T, Brown C, Parsey K, Foegh M. Evaluation of a unique oral contraceptive in the treatment of premenstrual dysphoric disorder. Journal of Womens Health Gender Based Medicine. 2001;10(6):561–569. doi: 10.1089/15246090152543148. [DOI] [PubMed] [Google Scholar]
- Freeman EW, Rickels K, Sondheimer SJ, Polansky M. Differential response to antidepressants in women with premenstrual syndrome/premenstrual dysphoric disorder: a randomized controlled trial. Archives of General Psychiatry. 1999;56(10):932–939. doi: 10.1001/archpsyc.56.10.932. [DOI] [PubMed] [Google Scholar]
- Frid M, Singer G, Oei T, Rana C. Reactions to ischemic pain: interactions between individual, situational and naloxone effects. Psychopharmacology (Berl) 1981;73(2):116–119. doi: 10.1007/BF00429200. [DOI] [PubMed] [Google Scholar]
- Frid M, Singer G, Rana C. Interactions between personal expectations and naloxone: effects on tolerance to ischemic pain. Psychopharmacology (Berl) 1979;65(3):225–231. doi: 10.1007/BF00492208. [DOI] [PubMed] [Google Scholar]
- Girdler SS, Maixner W, Naftel HA, Stewart PW, Moretz RL, Light KC. Cigarette smoking, stress-induced analgesia and pain perception in men and women. Pain. 2005;114(3):372–385. doi: 10.1016/j.pain.2004.12.035. doi: 10.1016/j.pain.2004.12.035. [DOI] [PubMed] [Google Scholar]
- Girdler SS, Pedersen CA, Light KC. Thyroid axis function during the menstrual cycle in women with premenstrual syndrome. Psychoneuroendocrinology. 1995;20(4):395–403. doi: 10.1016/0306-4530(94)00068-9. doi: 0306453094000689. [DOI] [PubMed] [Google Scholar]
- Girdler SS, Pedersen CA, Straneva PA, Leserman J, Stanwyck CL, Benjamin S, Light KC. Dysregulation of cardiovascular and neuroendocrine responses to stress in premenstrual dysphoric disorder. Psychiatry Research. 1998;81(2):163–178. doi: 10.1016/s0165-1781(98)00074-2. doi: S0165178198000742 . [DOI] [PubMed] [Google Scholar]
- Greeson JM. Mindfulness Research Update: 2008. Complementary Health Practice Review. 2009;2009;14(10):10–18. doi: 10.1177/1533210108329862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbreich U. Selective serotonin reuptake inhibitors and initial oral contraceptives for the treatment of PMDD: effective but not enough. CNS Spectrums. 2008;13(7):566–572. doi: 10.1017/s1092852900016849. [DOI] [PubMed] [Google Scholar]
- Hughes JW, Fresco DM, Myerscough R, van Dulmen MH, Carlson LE, Josephson R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosomatic Medicine. 2013;75(8):721–8. doi: 10.1097/PSY.0b013e3182a3e4e5. doi: 10.1097/PSY.0b013e3182a3e4e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter MS, Ussher JM, Browne SJ, Cariss M, Jelley R, Katz M. A randomized comparison of psychological (cognitive behavior therapy), medical (fluoxetine) and combined treatment for women with premenstrual dysphoric disorder. Journal of Psychosomatic Obstetrics and Gynaecology. 2002;23(3):193–199. doi: 10.3109/01674820209074672. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness in Everyday Life. Hyperion; New York: 1994. [Google Scholar]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, Hofmann SG. Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review. 2013;33(6):763–771. doi: 10.1016/j.cpr.2013.05.005. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- Kingston J, Chadwick P, Meron D, Skinner TC. A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. Journal of Psychosomatic Research. 2007;62(3):297–300. doi: 10.1016/j.jpsychores.2006.10.007. doi: 10.1016/j.jpsychores.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, Hellhammer DH. The 'Trier Social Stress Test'--a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28(1-2):76–81. doi: 10.1159/000119004. doi: 119004. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Strasburger CJ, Langkrar J. Attenuated cortisol response to psychological stress but not to CRH or ergometry in young habitual smokers. Pharmacology, Biochemistry, and Behavior. 1993;44(3):527–531. doi: 10.1016/0091-3057(93)90162-m. [DOI] [PubMed] [Google Scholar]
- Klatzkin RR, Bunevicius A, Forneris CA, Girdler S. Menstrual mood disorders are associated with blunted sympathetic reactivity to stress. Journal of Psychosomatic Research. 2014;76(1):46–55. doi: 10.1016/j.jpsychores.2013.11.002. doi: 10.1016/j.jpsychores.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatzkin RR, Lindgren ME, Forneris CA, Girdler SS. Histories of major depression and premenstrual dysphoric disorder: Evidence for phenotypic differences. Biological Psychology. 2010;84(2):235–247. doi: 10.1016/j.biopsycho.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroll R, Rapkin AJ. Treatment of premenstrual disorders. Journal of Reproductive Medicine. 2006;51(4):359–370. [PubMed] [Google Scholar]
- Lee SH, Ahn SC, Lee YJ, Choi TK, Yook KH, Suh SY. Effectiveness of a meditation-based stress management program as an adjunct to pharmacotherapy in patients with anxiety disorder. Journal of Psychosomatic Research. 2007;62(2):189–195. doi: 10.1016/j.jpsychores.2006.09.009. doi: 10.1016/j.jpsychores.2006.09.009. [DOI] [PubMed] [Google Scholar]
- Liu X, Wang S, Chang S, Chen W, Si M. Effect of brief mindfulness intervention on tolerance and distress of pain induced by cold-pressor task. Stress Health. 2013;29(3):199–204. doi: 10.1002/smi.2446. doi: 10.1002/smi.2446. [DOI] [PubMed] [Google Scholar]
- Lystyk, Gerrish SW. Premenstrual syndrome and premenstrual dysphoric disorder: Issues of quality of life, stress and exercise. In: Preedy VR, Watson RR, editors. Handbook of Disease Burdens and Quality of Life Measures. Springer; New York: 2006. [Google Scholar]
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology. 2004;72(1):31–40. doi: 10.1037/0022-006X.72.1.31. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- Mitchell LA, Macdonald RAR, Brodie EE. Temperature and the cold pressor test. The Journal of Pain. 2004;5:233–237. doi: 10.1016/j.jpain.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Moore PA, Duncan GH, Scott DS, Gregg JM, Ghia JN. The submaximal effort tourniquet test: Its use in evaluating experimental and chronic pain. Pain. 1979;6:375–382. doi: 10.1016/0304-3959(79)90055-1. [DOI] [PubMed] [Google Scholar]
- Morse CA, Dennerstein L, Farrell E, Varnavides K. A comparison of hormone therapy, coping skills training, and relaxation for the relief of premenstrual syndrome. Journal of Behavioral Medicine. 1991;14(5):469–489. doi: 10.1007/BF00845105. [DOI] [PubMed] [Google Scholar]
- Neff KD. The development and validation of a scale to measure self-compassion. Self and Identity. 2003;2:223–250. doi: 10.1080/15298860390209035. [Google Scholar]
- Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self and Identity. 2010;9(3):225–240. doi: 10.1080/15298860902979307. [Google Scholar]
- Nyklicek I, Mommersteeg PM, Van Beugen S, Ramakers C, Van Boxtel GJ. Mindfulness-based stress reduction and physiological activity during acute stress: a randomized controlled trial. Health Psychology. 2013;32(10):1110–1113. doi: 10.1037/a0032200. doi: 10.1037/a0032200. [DOI] [PubMed] [Google Scholar]
- Parswani MJ, Sharma MP, Iyengar S. Mindfulness-based stress reduction program in coronary heart disease: A randomized control trial. International Journal of Yoga. 2013;6(2):111–117. doi: 10.4103/0973-6131.113405. doi: 10.4103/0973-6131.113405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiner K, Tibi L, Lipsitz JD. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Medicine. 2013;14(2):230–242. doi: 10.1111/pme.12006. doi: 10.1111/pme.12006. [DOI] [PubMed] [Google Scholar]
- Rubinow DR, Roy-Byrne P, Hoban MC, Gold PW, Post RM. Prospective assessment of menstrually related mood disorders. American Journal of Psychiatry. 1984;141(5):684–686. doi: 10.1176/ajp.141.5.684. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Supplement 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- Spielberger C, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press, Inc.; Palo Alto, CA: 1970. [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American Journal of Obstetrics and Gynecology. 2000;183(3):759–769. doi: 10.1067/mob.2000.106580. doi: S0002-9378(00)78686-8. [DOI] [PubMed] [Google Scholar]
- Steiner M, Pearlstein T, Cohen LS, Endicott J, Kornstein SG, Roberts C, Yonkers K. Expert guidelines for the treatment of severe PMS, PMDD, and comorbidities: the role of SSRIs. Journal of Womens Health (Larchmont) 2006;15(1):57–69. doi: 10.1089/jwh.2006.15.57. [DOI] [PubMed] [Google Scholar]
- Steiner M, Steinberg S, Stewart D, Carter D, Berger C, Reid R, Streiner D. Fluoxetine in the treatment of premenstrual dysphoria. Canadian Fluoxetine/Premenstrual Dysphoria Collaborative Study Group. New England Journal of Medicine. 1995;332(23):1529–1534. doi: 10.1056/NEJM199506083322301. [DOI] [PubMed] [Google Scholar]
- Straneva PA, Maixner W, Light KC, Pedersen CA, Costello NL, Girdler SS. Menstrual cycle, beta-endorphins, and pain sensitivity in premenstrual dysphoric disorder. Health Psychology. 2002;21(4):358–367. [PubMed] [Google Scholar]
- Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and Validation. Psychological Assessment. 1995;7(4):524–532. [Google Scholar]
- Sundstrom-Poromaa I, Bixo M, Bjorn I, Nordh O. Compliance to antidepressant drug therapy for treatment of premenstrual syndrome. Journal of Psychosomatic Obstetrics and Gynecology. 2000;21:205–211. doi: 10.3109/01674820009085589. [DOI] [PubMed] [Google Scholar]
- Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: distinguishing rumination from reflection. Journal of Personality and Social Psychology. 1999;76(2):284–304. doi: 10.1037//0022-3514.76.2.284. [DOI] [PubMed] [Google Scholar]
- Vettese LC, Toneatto T, Stea JN, Nguyen L, Wang JJ. Do Mindfulness Meditation Participants Do Their Homework? And Does It Make a Difference? A Review of the Empirical Evidence. Journal of Cognitive Psychotherapy. 2009;23(3):198–225. doi: 10.1891/0889-8391.23.3.198. [Google Scholar]
- Vollestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behavior Research Therapy. 2011;49(4):281–288. doi: 10.1016/j.brat.2011.01.007. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- von Kanel R, Kudielkac BM, Preckelb D, Hanebuthb D, Fischerb JE. Delayed response and lack of habituation in plasma interleukin-6 to acute mental stress in men. Brain, Behavior, Immunity. 2006;20(1):40–48. doi: 10.1016/j.bbi.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Brown C, Pearlstein TB, Foegh M, Sampson-Landers C, Rapkin A. Efficacy of a new low-dose oral contraceptive with drospirenone in premenstrual dysphoric disorder. Obstetrics and Gynecology. 2005;106(3):492–501. doi: 10.1097/01.AOG.0000175834.77215.2e. [DOI] [PubMed] [Google Scholar]