Abstract
Objective:
To systematically investigate the effect of CT localizer radiograph acquisition on the tube current modulation and thus radiation dose of the subsequent diagnostic scan.
Methods:
Localizer radiographs of an abdominal section CT phantom were taken, and the resulting volume CT dose index (CTDIvol) for the diagnostic scan was recorded. Variables included tube potential, the phantom’s alignment within the CT scanner gantry in both the vertical and horizontal directions and the X-ray source angle at which the localizer was acquired.
Results:
Diagnostic scan CTDIvol decreased with increasing tube potential. Vertical (table height) movement was found to affect radiation dose more than horizontal movement, with ±50 mm table movement resulting in a standard deviation in the diagnostic scan CTDIvol of 4.4 mGy, compared with 2.5 mGy with ±50 mm horizontal movement. Correspondingly, localizer angles of 90° or 270° (3 o'clock and 9 o'clock X-ray source positions) were less sensitive overall to alignment errors, with a standard deviation of 2.5 mGy, compared with a 0° or 180° angle, which had a standard deviation of 3.8 mGy.
Conclusion:
To achieve a consistently optimized radiation dose, the localizer protocol should be paired with the diagnostic acquisition protocol. A final acquisition angle of 90° should be used when possible to minimize dose variation resulting from alignment errors.
Advances in knowledge:
Localizer parameters that affect radiation output were identified for this scanner system. The importance of tube potential and acquisition angle was highlighted.
Radiation exposure from medical imaging remains in the public awareness and has spurred the adoption of several technologies to minimize CT dose.1,2 A successful strategy for CT dose reduction is the use of tube current modulation (TCM), whereby the scanner adjusts tube current output along the z-axis and through the x- and y-axes according to estimates of patient attenuation. This TCM is used to achieve a consistent, pre-determined level of image quality.2 These preset levels vary by vendor in their exact definition, the terms noise index (GE Healthcare, Waukesha, WI), reference image (Philips Healthcare, Best, Netherlands), quality reference mAs (Siemens) and reference standard deviation (Toshiba Medical Systems Corp., Tokyo, Japan), and all have different functionality and dependencies.3–5
The estimates of patient attenuation used for TCM are based on the two-dimensional localizer radiograph, acquired prior to the diagnostic scan. The localizer, also known as the survey, pilot, scout (GE), surview (Philips), topogram (Siemens Healthcare, Erlangen, Germany) and scanogram (Toshiba), therefore plays a key role in determining patient dose, particularly in CT systems where online feedback is not used for TCM definition (i.e. the TCM relies solely on the localizer radiograph).6 Its importance is set to increase further, as manufacturers adopt automatic tube potential selection in addition to TCM, which is also based on the results from the localizer acquisition.7
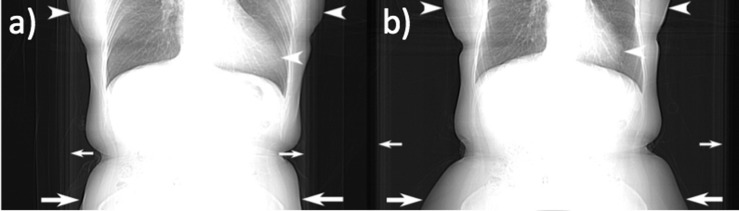
The TCM definition from localizer radiographs is known to be sensitive to patient miscentring errors, which represent a common procedural error. In a retrospective study of 273 adult body scans, an average patient centring error of −23 mm was found to exist in the vertical direction. This resulted in a mean dose increase of 33%, calculated via the change in tube current required to achieve a consistent image noise.8 Another study calculated vertical miscentring in 112 patients, finding a median error of 25–35 mm for different patient groups,9 while a third investigation found that patient centring was incorrect in 60 of 63 scans assessed.10 Incorrect TCM definition resulting from miscentring may be confounded by the apparent change in body morphology resulting from images taken using a 0°, anteroposterior (AP) source angle, and a 180°, posteroanterior (PA) source angle, both of which are commonly used clinically (Figure 1).
Figure 1.
Clinical localizer imaging for body CT. (a) Exhibits relatively high magnification of the anterior soft tissues and heart in the chest (arrowheads) and a small area of pelvic subcutaneous soft tissues (large arrows) and CT table (small arrows) when compared with (b).
This study aimed to expand the current understanding of how localizer acquisition influences the radiation output of the diagnostic scan. This included phantom miscentring in both the vertical and horizontal directions and variation of the acquisition tube potential. No consensus exists among current studies for some trends, for instance, whether a 0°, 90° or 180° source angle affords the most consistent volume CT dose index (CTDIvol).11–13 This is probably owing to the many different combinations of CT scanner model, the body region scanned and the phantom type used. As this work used a previously untested phantom and scanner model, results were again likely to vary and add to the body of work in an important field. Unexplored aspects of localizer definition that were targeted included an investigation of all main source angles (0°, 90°, 180°) concurrently with variation in acquisition potential, and also the influence of extraneous objects in the acquisition field of view.
METHODS AND MATERIALS
The study was performed using an abdominal section water-based phantom, formed in polyethylene plastic from the abdominal cast of a 70-kg male adult. It measured 334 mm in the lateral, 275 mm in the AP and 150 mm in the z-direction. Three separate inserts to represent the two kidneys and the spine were filled with iodinated contrast agent (Omnipaque™ 350; GE Healthcare), with concentrations to reach approximately 200 HU for the kidneys and 400 HU for the spine at 120 kVp. The phantom was positioned at the centre of the CT gantry through the use of the laser sights and annotations on the phantom itself (Figure 2). It was then left in position for the majority of the scans until horizontal movement was required.
Figure 2.
Photograph showing the phantom positioned on the CT table in the gantry. Visible on the sides of the phantom are the markings used to ensure alignment (arrowheads). Also visible are the kidney and spine inserts, as well as three plugged holes that can accommodate simulated gastric tubing (not used in this study).
The scans were performed using a Discovery 750HD scanner (GE Healthcare). The precision of the system was tested through repetition of an identical localizer acquisition (0° source angle, 120 kVp potential, well-centred phantom) eight times and the measurement of variation in CTDIvol. All localizer radiographs in the study were obtained with a tube current of 10 mA and a scan length of 100 mm. This scan length was also used for the diagnostic scan definition.
Tube potentials of 80, 100, 120 and 140 kVp and X-ray source angles of 0°, 90°, 180° and 270° were investigated. Table positions of 50 mm above and 50 mm below the central plane were used in accordance with previous work,14 as were phantom positions 50 mm to the left and 50 mm to the right of the centreline. These horizontal positions were approximate as the phantom was moved by hand. Further localizer scans were acquired at vertical table increments of 10 mm above and below the central plane to allow a height sensitivity profile to be obtained. The incremental height radiographs were conducted using a tube potential of 120 kVp and source angles of 0° and 90°. Following this parametric investigation, additional objects were placed adjacent to the phantom to represent items that the patient neglected to remove prior to scanning, in order to test the corresponding increase in CTDIvol. These included a wallet, a set of keys, a mobile phone and a waist belt with a steel buckle.
The protocol for the hypothetical diagnostic acquisition was a contrast-enhanced, adult abdomen scan in routine practice at the institution. This involved a helical scan path with a pitch of 0.984, a tube potential of 120 kVp, auto mA and Smart mA both active with 150–800 mA limits, a noise index of 31.5, a display field of view of 360 mm and a prescribed image thickness of 1.25 mm. The CTDIvol of this scan was recorded following the acquisition of each localizer radiograph. Because GE scanners do not use any online feedback for TCM, there was no need to conduct the actual diagnostic scan.6
RESULTS
The eight identical localizer acquisitions displayed a standard deviation in prescribed CTDIvol of 0.23%, with all values lying within 1% of one another. This proved the scanner system to have a high level of precision; confirming the validity of the experimental procedure and results, where the smallest reported change in CTDIvol was 3%.
To assess the overall effect of the tube potential, the CTDIvol was averaged between all localizer source angles and phantom positions for a given tube voltage. 80-kVp acquisitions resulted in a mean CTDIvol of 17.9 mGy, which decreased to 17.2, 14.5 and 14.1 mGy for the 100, 120 and 140 kVp images, respectively. With the 120 kVp as the baseline, these represent percentage differences of 24% for the 80-kVp, 19% for the 100-kVp and −3% for the 140-kVp scans.
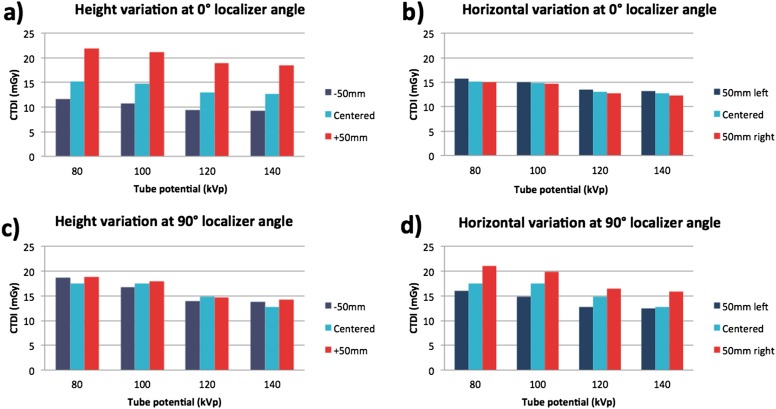
The greatest change in CTDIvol was observed for vertical movement with a localizer angle of 0° (Figure 3a). In this instance, the ±50 mm range caused a 100% variation in CTDIvol at 120 kVp. Vertical table movement with a 90° localizer angle showed the least variation, with the ±50 mm range corresponding to a 5% change in CTDIvol at 120 kVp (Figure 3c). The horizontal phantom movement resulted in intermediate differences, with changes in CTDIvol of 6% and 23% for the 0° and 90° angles, respectively (Figure 3b,d).
Figure 3.
Bar charts showing variation in volume CT dose index (CTDIvol) with localizer tube voltage and phantom position in the gantry. (a) Height variation at 0° localizer angle, (b) horizontal variation at 0° localizer angle, (c) height variation at 90° localizer angle, (d) horizontal variation at 90° localizer angle.
Collating results from all movements (vertical and horizontal), the 0°/180° localizer scans displayed a total standard deviation of 4.4 mGy, while the 90°/270° scans were less sensitive to phantom centring with a standard deviation of 2.5 mGy. Comparing the 0° with the 180° localizer angles with the phantom centred, the 180° localizer angle was found to result in a CTDIvol 14% higher than that of the 0° localizer angle.
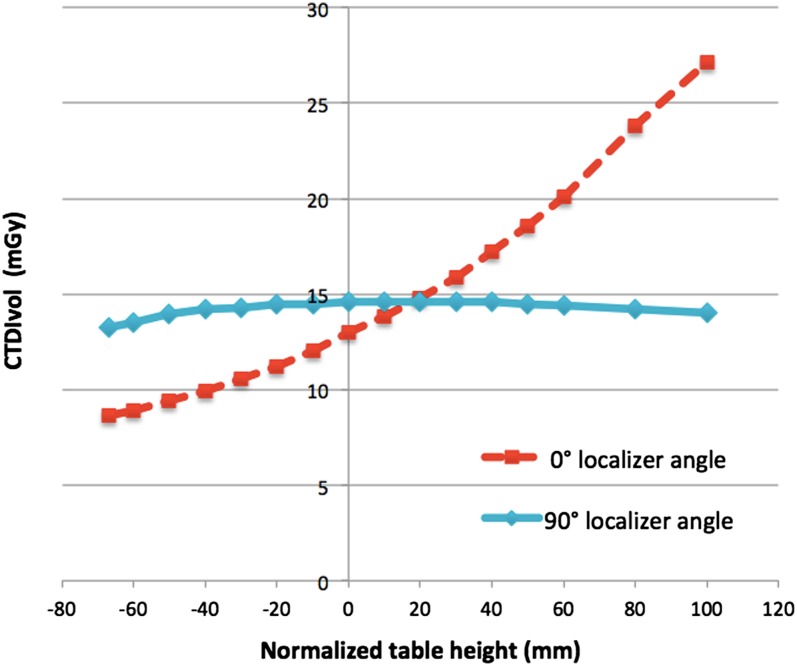
For the incremental variations in table height, the 0° localizer angle exhibited a relatively linear increase in CTDIvol with increasing table height, in agreement with previous work (Figure 4).9,14 This can be explained in terms of the phantom moving towards the X-ray source, thus having a greater magnification in the projection image and being interpreted by the scanner as a larger body requiring a higher tube current.14 The CTDIvol shows little dependence on table height for the 90° localizer plane, as although the phantom is moving vertically in these radiographs, its projected size remains largely unchanged.
Figure 4.
Line plot showing the resulting volume CT dose index (CTDIvol) change from incremental 10-mm movements in table height. The −68 mm lower limit corresponds to the physical limit of the table movement.
The extraneous objects, when included adjacent to the phantom, caused generally modest increases in the scan CTDIvol. These increases, averaged between the 0° and 90° angles, were 4% for the keys, 6% for the wallet, 14% for the phone and a more substantial 32% for the belt. When comparing the 0° and 90° acquisition angles, the increase was more substantial from the angle where the projected area of the object was larger: for the keys, wallet and phone that were placed at the side of the phantom, the 90° angle showed the greater CTDIvol increase, while for the belt with its steel buckle on the anterior surface, this was true for the 0° angle.
DISCUSSION
A key finding was the decrease in scan CTDIvol observed for increasing localizer tube potentials for this scanner system and phantom combination. It can be accounted for by the scanner interpreting the body as being less dense in the high tube voltage images owing to lower attenuation, and therefore prescribing a lower tube current. This result implies that users should be aware of the localizer acquisition tube voltage and ensure that it remains paired with a given diagnostic protocol in order to maintain consistent image quality.
For the two vertical localizer angles, 0° gave lower radiation output than did 180° for the diagnostic scan. This is in accordance with one previous study15 and contrary to another that found that the two were equivalent.13 It is owing perhaps to the smaller projected area of the CT table, although it has also been suggested that the greater magnification of the spine in the PA view plays a role.15 The 90° localizer angle was found to offer lower radiation output than did both 0° and 180° localizer angles. Again there is no consensus among previous research for this finding, with studies that both corroborate it12,13 and find the contrary.11 A reason for this discrepancy, with both studies conducted using GE scanner systems, may be that the previous study included the chest region or that it investigated only the z-axis component of TCM.
The study further consolidates previous research, finding a strong dependence of the prescribed CTDIvol on patient location within the gantry.8,9,14 Another trend observed was the increased sensitivity of the 0° localizer angle to phantom movement compared with 90° localizer angle, supporting previous research.9 One would expect the 0° localizer angle to be more sensitive to vertical movement as the projected area of the phantom changes, and correspondingly, the 90° localizer angle to be more sensitive to horizontal movement. This was confirmed, although when accounting for all vertical and horizontal movement, greater variations in the CTDIvol were observed for the 0° source angle acquisitions. This is perhaps owing to the concave shape of the CT table, which results in a physical tilting of the phantom when moved laterally, which may offset some movement. In clinical practice, it could also be argued that centring inaccuracies are more likely in the vertical direction, as the curved table implies that patients should naturally be relatively well centred horizontally. For these reasons, the authors would recommend using a 90° localizer angle where possible. When multiple localizer images are taken, this scanner system uses only the most recently acquired radiograph for TCM definition.11,12 In this instance, the 90° localizer image should be taken last to provide the most consistent dose. Recent research using a Siemens scanner has, however, shown that TCM definition is affected and improved by the acquisition of multiple localizer scans.13 Users should therefore be aware of the dependencies of their scanner and of further developments in the future.
In general, the addition of extraneous objects within the field of view was not overly detrimental to the prescribed TCM. In the present study, keys increased the CTDIvol by only 4%. This could in part be attributed to the relatively large size of the phantom; the effects for smaller patient sizes are likely to be more pronounced. The fact that the belt had the greatest effect shows that less dense material that covers a larger area is of more concern than small, high attenuation objects such as keys. This has implications for the presence of heavy clothing and blankets. In general, it is recommended that localizer images be reacquired following the discovery of any extraneous objects, whatever their form. It is inadvisable to remove any objects without the reacquisition of the localizer. This would result in higher patient dose since their shielding effect, which was factored in the TCM calculation, will be absent.
A final point not investigated in the present work but known through prior studies is to ensure that the body segments to be scanned are included in the localizer. If the localizer does not encompass the entirety of the scanned length of the patient, the software will compensate erratically based on the limited localizer data that are available.16 This could either result in a falsely high or low tube current. For example, if only the abdomen is included in the localizer, extension of the CT scan through the pelvis will likely result in under-radiation of the pelvis and high image noise.
Some factors were not explored in the present work, as they have been well characterized elsewhere. First, it was assumed that the actual modulation prescribed was consistent between different localizer acquisitions, as observed previously using a similar CT system.11 Second, the image noise in the diagnostic scan resulting from the variations in localizer acquisition has been investigated previously, with noise shown to increase for decreasing prescribed CTDIvol.11,12,14 Another factor not within the scope of the project was the direct measurement of radiation dose to the phantom. Radiation output in the form of CTDIvol was considered a fair surrogate, as it has been shown through simulation that patient dose is closely proportional to the console CTDIvol value.17 Finally, variation of the localizer tube current was not performed. For a similar scanner system, however, this did not influence the CTDIvol of the diagnostic scan.11
The study had several limitations. Most notable of these was the use of a single GE scanner system. As the other vendors prescribe TCM in different ways, the scan CTDIvol resulting from the localizer image is likely to vary significantly. Dose distribution was not considered. It has been observed that a 30-mm error in patient centring can result in a 12–18% increase in surface dose, while a 60-mm error can cause a 41–49% increase.10 This has important implications for sensitive, near-surface organs such as the breast, which would receive higher radiation dose than did deeper organs. A final limitation was the absence of investigation into the effect of the patients’ arms in the localizer field of view, which can occur in body imaging if the patient is unable to raise their arms above their head. If the patients’ arms remained in the field of view, the overall localizer attenuation and thus prescribed radiation output would likely be significantly higher.
The research highlights the need to set localizer tube voltage and source angles for a given protocol in order to ensure successful TCM definition. This not only provides correct patient dose but also allows the radiology team at an institution to base image quality and dose strategies on a known and consistent set of scans. As in prior studies, acquisition of two localizer radiographs is recommended to ensure accurate centring in both directions;9,13 in this instance, with a final localizer acquisition angle of 90°. In combination with diligence in patient centring and care to remove all overlying objects from the patient, these techniques help to ensure consistent TCM, image quality and radiation dose.
REFERENCES
- 1.Thrall JH. Radiation exposure in CT scanning and risk: where are we? Radiology 2012; 264: 325–8. doi: 10.1148/radiol.12121137 [DOI] [PubMed] [Google Scholar]
- 2.Coakley FV, Gould R, Yeh BM, Arenson RL. CT radiation dose: what can you do right now in your practice? AJR Am J Roentgenol 2011; 196: 619–25. doi: 10.2214/AJR.10.5043 [DOI] [PubMed] [Google Scholar]
- 3.Solomon JB, Li X, Samei E. Relating noise to image quality indicators in CT examinations with tube current modulation. AJR Am J Roentgenol 2013; 200: 592–600. doi: 10.2214/AJR.12.8580 [DOI] [PubMed] [Google Scholar]
- 4.Lee CH, Goo JM, Ye HJ, Ye SJ, Park CM, Chun EJ, et al. Radiation dose modulation techniques in the multidetector CT era: from basics to practice. Radiographics 2008; 28: 1451–9. doi: 10.1148/rg.285075075 [DOI] [PubMed] [Google Scholar]
- 5.Söderberg M, Gunnarsson M. Automatic exposure control in computed tomography—an evaluation of systems from different manufacturers. Acta Radiol 2010; 51: 625–34. doi: 10.3109/02841851003698206 [DOI] [PubMed] [Google Scholar]
- 6.McCollough CH, Bruesewitz MR, Kofler JM, Jr. CT dose reduction and dose management tools: overview of available options. Radiographics 2006; 26: 503–12. [DOI] [PubMed] [Google Scholar]
- 7.Grant K, Schmidt B. Care kV: automated dose-optimized selection of X-ray tube voltage. Forcheim, Germany: Siemens Healthcare; 2011. [Google Scholar]
- 8.Toth T, Ge Z, Daly MP. The influence of patient centering on CT dose and image noise. Med Phys 2007; 34: 3093–101. [DOI] [PubMed] [Google Scholar]
- 9.Kaasalainen T, Palmu K, Reijonen V, Kortesniemi M. Effect of patient centering on patient dose and image noise in chest CT. AJR Am J Roentgenol 2014; 203: 123–30. doi: 10.2214/AJR.13.12028 [DOI] [PubMed] [Google Scholar]
- 10.Li J, Udayasankar UK, Toth TL, Seamans J, Small WC, Kalra MK. Automatic patient centering for MDCT: effect on radiation dose. AJR Am J Roentgenol 2007; 188: 547–52. [DOI] [PubMed] [Google Scholar]
- 11.Brisse HJ, Madec L, Gaboriaud G, Lemoine T, Savignoni A, Neuenschwander S, et al. Automatic exposure control in multichannel CT with tube current modulation to achieve a constant level of image noise: experimental assessment on pediatric phantoms. Med Phys 2007; 34: 3018–33. [DOI] [PubMed] [Google Scholar]
- 12.Papadakis AE, Perisinakis K, Damilakis J. Automatic exposure control in pediatric and adult multidetector CT examinations: a phantom study on dose reduction and image quality. Med Phys 2008; 35: 4567–76. [DOI] [PubMed] [Google Scholar]
- 13.Singh S, Petrovic D, Jamnik E, Aran S, Pourjabbar S, Kave ML, et al. Effect of localizer radiograph on radiation dose associated with automatic exposure control: human cadaver and patient study. J Comput Assist Tomogr 2014; 38: 293–8. doi: 10.1097/RCT.0000000000000035 [DOI] [PubMed] [Google Scholar]
- 14.Matsubara K, Koshida K, Ichikawa K, Suzuki M, Takata T, Yamamoto T, et al. Misoperation of CT automatic tube current modulation systems with inappropriate patient centering: phantom studies. AJR Am J Roentgenol 2009; 192: 862–5. doi: 10.2214/AJR.08.1472 [DOI] [PubMed] [Google Scholar]
- 15.Moro L, Panizza D, D’Ambrosio D, Carne I. Considerations on an automatic computed tomography tube current modulation system. Radiat Prot Dosimetry 2013; 156: 525–30. doi: 10.1093/rpd/nct095 [DOI] [PubMed] [Google Scholar]
- 16.Söderberg M. Automatic exposure control in CT an investigation between different manufacturers considering radiation dose and image quality. Master of Science Thesis. Lund, Sweden: Lund University; 2008.
- 17.Turner AC, Zankl M, DeMarco JJ, Cagnon CH, Zhang D, Angel E, et al. The feasibility of a scanner-independent technique to estimate organ dose from MDCT scans: using CTDIvol to account for differences between scanners. Med Phys 2010; 37: 1816–25. [DOI] [PMC free article] [PubMed] [Google Scholar]