Abstract
Sleep is an important component of human life, yet many people do not understand the relationship between the brain and the process of sleeping. Sleep has been proven to improve memory recall, regulate metabolism, and reduce mental fatigue. A minimum of 7 hours of daily sleep seems to be necessary for proper cognitive and behavioral function. The emotional and mental handicaps associated with chronic sleep loss as well as the highly hazardous situations which can be contributed to the lack of sleep is a serious concern that people need to be aware of. When one sleeps, the brain reorganizes and recharges itself, and removes toxic waste byproducts which have accumulated throughout the day. This evidence demonstrates that sleeping can clear the brain and help maintain its normal functioning. Multiple studies have been done to determine the effects of total sleep deprivation; more recently some have been conducted to show the effects of sleep restriction, which is a much more common occurrence, have the same effects as total sleep deprivation. Each phase of the sleep cycle restores and rejuvenates the brain for optimal function. When sleep is deprived, the active process of the glymphatic system does not have time to perform that function, so toxins can build up, and the effects will become apparent in cognitive abilities, behavior, and judgment. As a background for this paper we have reviewed literature and research of sleep phases, effects of sleep deprivation, and the glymphatic system of the brain and its restorative effect during the sleep cycle.
Keywords: Glympathics, Sleep, Brain
Introduction
Every human being spends a significant amount of their life sleeping. Despite being such a huge component of human life, there is still a lot of mystery surrounding the relationship between the brain and the process of sleeping. In fact, sleeping influences each individual in numerous ways. Researchers and scientists alike have proven that sleeping improves memory recall and helps regulate the metabolism in the body and reduces mental fatigue [1]. Interestingly, scientists relate the dangers of chronic sleep loss to being similar to driving while intoxicated with alcohol. Sleeping is a basic physiological need, from the simple transitional period to the sleep stage. The emotional and mental handicap with chronic sleep loss as well as the highly hazardous situation which can be constrained by the lack of sleep is a serious concern that people need to be aware of. Sleeping is effortlessly important. In fact, for centuries no scientific evidence has authentically proven the significant reason for sleeping in a molecular level.
Until recently, the latest research developments have concluded that sleeping has much more impact in the brain than previously thought. More specifically, when one sleeps, the brain resets itself, removes toxic waste byproducts which may have accumulated throughout the day [2]. This new scientific evidence is important because it demonstrates that sleeping can clear “cobwebs” in the brain and help maintain its normal functioning. More importantly speaking, this paper illustrates the different principles of sleep; starting from the non-rapid eye movement (NREM) to the behavioral as well as mental patterns with chronic sleep loss as well as the importance of sleeping acting as a garbage disposal in the body.
Brain Activity During Sleep
Generally, sleeping is considered as an unconscious state, in which the one may be aroused [3]. This is why one dreams; we sometimes get the feeling of fear, shock, fatigue, and sorrow depending on what the brain was dreaming about. During sleep the brain is less responsive to external stimuli, which is why individuals do not respond while sleeping. One may wake up from the noise but can not hold a conscious conversation while asleep. Sleep is very important for the body to rest and restore its energy. It is an important cycle of resting, restoring energy and using it again. Often time lack of sleep causes day-to-day life disturbance. While resting our brain goes through different phases of sleep. These phases are important because during certain phase; if awakened, the sleep is disturbed and the brain may feel restless.
In a normal person; sleep is divided into two major phases, and each phase is further divided into cycles. The first phase is non-rapid eye movement (NREM) and the second is rapid eye movement (REM). The NREM phase is further divided into more stages as one goes into deeper sleep. These stages include N1, N2 and N3. During N3, one is considered to be in the deep or delta wave sleep. The REM sleep has tonic and phasic components to characterize its influence on sleep. The phasic part of rapid eye movement sleep has been identified as a sympathetically driven state, which characteristically consists of rapid eye movements as well as respiratory variability and muscle twitches [4]. During REM, the tonic phase is the para-sympathetically driven phase and there is no eye movement; the length and density of the eye movement in REM period increases throughout the sleep cycle. The sleep cycle first starts with NREM period and then followed by REM period [5]. During an 8-hour sleep the brain goes in and out of REM period about 4 to 5 times. This is the phase in which dreams generally occur.
The Process of Sleep in Adults
In adults the stage N1 of the NREM phase is considered to be the transition stage between wake and sleep. The stage N2 is light sleep which occurs throughout during the sleep period; during this stage, muscle relaxation occurs, the heart rate slows down and the temperature drops [6,7]. This is when the brain is preparing to enter into the deep sleep stage. Finally, the stage N3, can also called as the delta or slow wave sleep; which mostly takes place in the first third of the night sleep. The 3rd stage is more of deep sleep; if woken during this stage a person may feel disoriented for few minutes.
There are many consequences of lack of sleep on body as well as our well-being. But most importantly studies have shown lack of sleep can hinder memory recall in the brain as well as elevate stress levels. Sleep is needed to regenerate parts of the brain so that it can continue to function normally [8,9]. Lack of sleep or not enough sleep can cause some neurons in one’s brain to malfunction. If the neurons cannot function properly it affects the person’s behavior and has an impact on their performance. Certain stages of sleep are needed for the regeneration of neurons within the cerebral cortex while other stages of sleep seem to be used for forming new memories and generating new synaptic connections [10]. Since the brain is actively working all the hours when one’s awake, after certain time, the sleep neurons start to get tired. This affects the brain in many ways including trouble concentrating, difficulty focusing and having trouble remembering.
Clearing the Cobwebs out from the Brain
One of the great mysteries of sleep is how it connects with the brain. In fact, scientists have never concluded a precise reason for this relationship. Some of the most intriguing questions include: Why is sleep important? Why do human beings sleep? Recently, a study stated that when individuals sleep abundantly throughout the night, cellular waste byproducts which may have accumulated in the interstitial space and in the brain cells are thoroughly removed [11]. From this, it can be concluded that the fundamental purpose of sleep is to act like a garbage disposal for the brain. Essentially, sleeping acts as a garbage collector that comes during the night and removes the waste product left by the brain. This allows the brain to function normally the next day when one wakes up for slumber.
The Brain’s Garbage Disposal System
Recently research states that there is a fluid filled channel which eliminates the toxins in the brain that allows the brain to have a clean slate to work from after one engages in the act of sleeping [2]. This precise network is called the glympathic system. The glymphatic system is a waste clearance pathway, in layman’s terms, a plumbing system. Unlike the lymphatic system, the glymphatic system, dubbed after the combination of the words “lymphatic” and “glia” acts to flush out the cellular trash in the body just like a plumbing system would do. The glympathic system contains glial cells that are a particular type of neuro-functional cell in the human body.
Furthermore, this research study states that the brain contains glial cells which regulate the flow of the cerebrospinal fluid in the cell membrane [11]. These glial cells can be described as the brain’s motherboard as it acts as sustenance in the neurons in the central nervous system. As an example, if the channels in the glial cells are discarded, then the flow in the cerebrospinal fluid will be barricaded.
Moreover, it is stated that since the cell membrane requires adequate energy, the brain exclusively functions as a one way street [11]. For instance, the brain can be considered as a light switch, as it contains an “on” or “off” switch function. Meaning it can only perform one task at a time – whether it be clearing cellular waste products or processing sensory information, it cannot do both. This gives evidence for a theory that glymphatic system does exist and its function is to help remove the toxic metabolites from the brain. In the next section, the study in mice in connection with the brain and sleeping theory will be explored.
Experimental Study in Mice on the Effects of the Brain and Sleep
The substantial importance of sleeping can be scientifically proven in a newly profound research by the application of the two-photon microscope. It has been stated that the mice research with the two-photon microscope is significant to scientifically understand the core purpose of sleeping a molecular level [2]. In fact, the two-photon microscope depicts the relationship between the brain and sleeping with the help of distinguishing two dyes – red and green dyes injected in the mice into their living tissue. For instance, in the research, the mice are trained for consecutive two years to be in a state of consciousness and unconsciousness. The movement of the dyes in the mice shows the difference between the cerebrospinal fluid in the awake and sleep state.
The Brain’s Glymphatic System
The cerebrospinal fluid travels first into the para-arterial space then into an interstitial space through the aquaporin 4 (APQ4) water channel pathway [11]. An exchange occurs between the cerebrospinal fluid as well as the interstitial fluid due to rhythmic vascular pulsations during the various stages of sleep. Moreover, waste products are then diverted away from the arteries to the veins and swiftly move along to the paravenous space [11]. To such degree, the glymphatic system acts accordingly in the same manner as the lymphatic system except for several particular situations – such as when the glymphatic system directs transport to the sites of excretion as well as recycling [12]. Nonetheless, deletion of the water channel pathway, aquaporin 4 (AQP4) would increase chances of excessive production of a peculiar metabolite. More so, the reasoning for the staggering increase of cerebrospinal fluid is due to the brain’s adapted ability to clear a specific metabolite in the body [1]. This precise metabolite is a peptide called beta-amyloid.
The functions of the glymphatic system differ in the awake and sleep state. It has been theorized that during the sleep state, the cerebrospinal fluid flows more profusely than during the day [2]. Equally important, in the sleeping state, the interstitial space increases roughly sixty percent and effectively clears toxic cellular trash. Thus, during the state of sleep, the cerebrospinal fluid removes the beta-amyloid metabolite in the brain [2]. As a matter of fact, it has been proven that beta amyloid accumulates during the day and can be the primarily reason for many of the neurodegenerative diseases such as Alzheimer’s disease and Dementia.
Undoubtedly, this study is important because it shows that the consequences of sleep deprivation can negatively manifest in motor functions, cognitive performances as well as behavioral patterns. The underlying mechanisms of these dysfunctions may be attributed to the excess accumulation of toxic metabolites like beta-amyloid. Overtime, the metabolite accumulations can lead to severe brain injury.
Sleep Deprivation
Many patients complain of times of insomnia, or that they do not get a sufficient amount of sleep. It has been often stated that eight hours of sleep per night is the required amount to be well rested and to be able to function at one’s best. The amount of sleep required to feel healthy and well rested is very individualized. There is not an exact number of hours or minutes of sleep that must be obtained for optimal health, but there does seem to be a range of sleep time needed for an individual to be cognitively aware of daily tasks and able to perform at one’s best.
Lack of sleep affects different parts of the brain, independently. For example, temporal lobe is associated with language processing, so lack of sleep often results in slurred speech because the brain’s inability to process the neuronal signal at optimum levels. Studies have shown that NREM sleep is important for turning off the norepinephrine, serotonin and histamine neurotransmitters, which in turn allows their receptors to “rest” and regain sensitivity [13]. This allows norepinephrine, serotonin and histamine to be more effective at naturally produced levels. During sleep, there are enzymes that repair brain cell damage caused by free radicals. In contrast, lack of sleep does not allow our brain to function normally because of the neurotransmitters, and neurons that are unable to rest or regenerate [13]. This becomes worse with people that are sleep deprived for days and their neurons start to degenerate because of constantly being actively at work. The neurons get worn out without having the time to regenerate and rest.
Aside from the physiological changes that the brain goes through with lack of sleep; sleep deprivation also have impact on the behavior, mood, cognitive performance, as well motor function of the body [10]. Studies have shown that motor vehicle accidents due to fatigue and lack of sleep are becoming more and more common. The consequences of not getting enough sleep are rather dangerous. It not only affects our mental and physical health as well as the cognitive performance but studies have proven that lack of sleep has negative effect on long-term memory, working memory, attention, higher order executive function, and various decision making processes [10]. It affects long-term memory due to the inability to consolidate learned tasks throughout the previous day as a result of the negative impact of early phase slow-wave (deep sleep), when normal memory consolidates learned tasks through neuronal synapses via encoding and memory storage. Simply put, with a lack of sleep neurons do not have a chance to create long-term memory and manifests itself as various clinical symptoms of behavioral, personality, cognitive, and physical complaints.
What are the consequences of sleep deprivation?
Many patients request their healthcare provider prescription of sleep aids, complaining about the inability to sleep. Some providers prescribe sleep aids to them, but many patients leave their office with a diagnosis of depression than a diagnosis of insomnia [14]. Many factors can affect one’s ability to get a full restful night of sleep. Depression, anxiety or stress may be a cause that inhibits the ability to fall asleep, or to stay sleeping through the night. Medical problems or sleep disorders may prevent a person from obtaining undisturbed sustained sleep, or from entering into all stages of sleep.
The average amount of sleep time for Americans as self-reported in a 2005 Gallup Poll survey of adults, 18 year-olds and older showed that 71% got less than eight hours of sleep per night on weekdays, and of those 16 % received less than 6 hours of sleep per night. The same population reported that they made up for some of the lost sleep time on the weekend, with 49 % stating that they obtained over eight hour of sleep and another 24 % (for a total of 73%) describing greater than seven. One classic study actually showed those hours of sleep on weekends [15].
Several scientific studies have been done to measure the physical and neurologic effects of total sleep deprivation, and now there is also scientific data available that evaluated the effects of restricted amount of sleep on neurobehavioral and physiologic function of a person that has been done that is reliable and reproducible. In two well controlled studies, healthy adults voluntarily were subjected to limited hours of sleep, randomized into 4, 6 and 8 hours of sleep. Caffeine use was carefully restricted as was sleep and wake time [14]. Neurobehavioral effects were tested using psychomotor vigilance tasks (PVT), which uses timed feedback for continued attention to measures the speed with which subjects respond to a visual stimulus [15]. Other tests included a computerized digital subtraction test, which was used to measure working memory.
Although there were not significant differences in baseline testing between the groups, after 14 continuous days of sleep restriction, the data showed significant changes in test result across the groups. As predicted, those with only 4 or 6 hour of sleep had lower scores on all testing, including lapses of attention, reduced cognitive thought, slowed working memory, depressed mood, and delayed reaction times [15]. However, those who obtained 7 hours of sleep or more had no significant difference in test scores, which may infer that 7 hours of nightly sleep may be all that is needed for optimal performance. After 3 days of sleep restriction of 4–6 hours, some of the subjects exhibited the same decreased reaction times and cognitive dysfunction as displayed in subjects that had been observed in testing total sleep deprivation. What is interesting is that at the end of the study, the sleep-deprived subjects did not reliably report feeling sleepy after chronic sleep restriction for 14 days. The authors felt that once sleep restriction becomes chronic, subjects were not able to reliably introspect with regard to their actual sleepiness; they were not self-aware of their deficiencies. The effects of sleep restriction raises concerns for occupations that require high level cognitive performance at critical times, especially in potentially dangerous or life threatening situations such as healthcare workers, military personnel, or space flight.
Medical Conditions Related to Sleep Deprivation
Restricted sleep or partial sleep deprivation is quite prevalent as a result of medical conditions -such as COPD; sleep disorders -such as sleep apnea or insomnia; and lifestyle, for example night shift-work, or medical school study hours. In the Journal of Sleep Medicine, Drs. Banks and Dinges (2007) describe sleep deprivation occurring in three different ways. The first is considered ‘sleep fragmentation’ in which the stages of sleep are disrupted to different degrees, resulting in less time of consolidated sleep in relation to the actual amount of time in bed. The second type of sleep deprivation involves the loss of the specific stages of sleep, and is described as ‘selective sleep restriction’. This is not as common as the other forms, and may occur in a person with sleep apnea who rarely enters REM sleep. The third type is explained as sleep restriction, or ‘sleep debt’.
Conclusion
In summary, the correlation between the brain and sleep serves multiple purposes and reasons in one’s life. Hence, its capacity to act as memory storage as well as its ability to process simple day to day tasks. Sleeping not only relieves stress and depression –but also prolongs alertness and memory recall. With the process of sleep, through the stages of non-rapid eye movement (NREM) to the rapid eye movement (REM); one can understand that sleeping is a necessity. From this one can see, that if an individual continually has insufficient amount of sleep; the repercussions could be hazardous both short and long term ones. Therefore, there is plenty of evidence indicating that sleep is crucial. In addition, with the discovery of the relationship between sleep and the brain’s health; one can conclude that sleeping clears the build-up of toxic waste products and may be of interest in investigating psychiatric illnesses. Moreover, the implications for warding off psychiatric disturbances are paramount, especially in Bipolar Disorder due to prodromal features often being lack of need for sleep. Similarly, patients suffering from Depression, Bipolar Disorder, Schizophrenia, and other maladies may want to consider proper sleep hygiene as part of the healing process as the brain’s glymphatic system clears out toxins, or may not be in certain psychiatric disturbances.
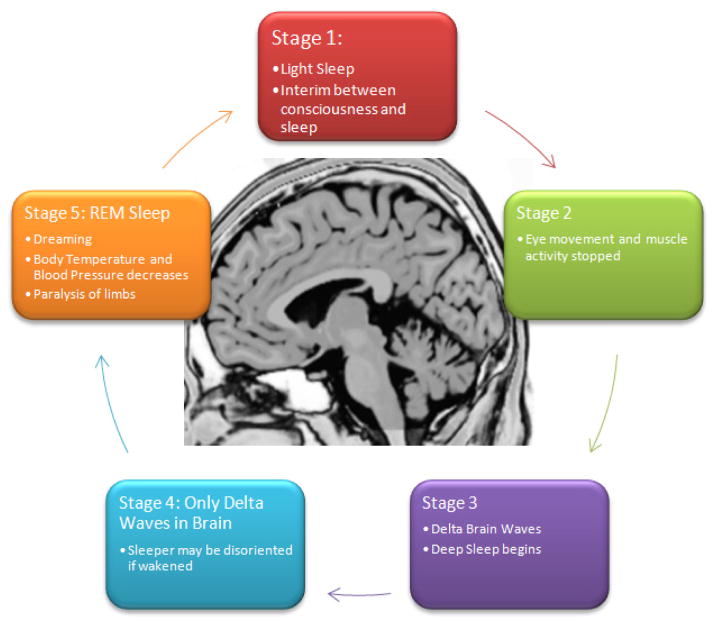
Figure 1.
Stages of the Sleep Cycle
Acknowledgments
Funding: Research reported in this publication was supported by National Institute of General Medical Sciences of the National Institutes of Health under award number T32 GM008685.
Footnotes
Conflicts of Interest
The authors declare no conflict of interest.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Herculano-Houzel S. Sleep It Out. Science (80– ) 2013;342:316–7. doi: 10.1126/science.1245798. [DOI] [PubMed] [Google Scholar]
- 2.Underwood E. Neuroscience. Sleep: the brain’s housekeeper? Science. 2013;342:301. doi: 10.1126/science.342.6156.301. [DOI] [PubMed] [Google Scholar]
- 3.Carskadon M, Dement W. Normal human sleep: an overview. Princ Pract Sleep Med. 1994;18:16–25. [Google Scholar]
- 4.Tsoukalas I. The origin of REM sleep: A hypothesis. Dreaming. 2012;22:253–83. doi: 10.1037/a0030790. [DOI] [Google Scholar]
- 5.Carskadon MA, Dement WC. Normal Human Sleep: An Overview. Princ Pract sleep Med. 2011;5:16–26. doi: 10.1016/B978-1-4160-6645-3.00002-5.. [DOI] [Google Scholar]
- 6. [accessed January 17, 2015];Sleep and Wakefulness, Kleitman. n.d http://www.press.uchicago.edu/ucp/books/book/chicago/S/bo3638082.html.
- 7.Murphy PJ, Campbell SS. Nighttime drop in body temperature: a physiological trigger for sleep onset? Sleep. 1997;20:505–11. doi: 10.1093/sleep/20.7.505. [DOI] [PubMed] [Google Scholar]
- 8.Hobson JA. Sleep is of the brain, by the brain and for the brain. Nature. 2005;437:1254–6. doi: 10.1038/nature04283. [DOI] [PubMed] [Google Scholar]
- 9.Cirelli C. Cellular consequences of sleep deprivation in the brain. Sleep Med Rev. 2006;10:307–21. doi: 10.1016/j.smrv.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Alhola P, Polo-Kantola P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr Dis Treat. 2007;3:553–67. [PMC free article] [PubMed] [Google Scholar]
- 11.Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–7. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nedergaard M. Garbage truck of the brain. Science. 2013;340:1529–30. doi: 10.1126/science.1240514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suntsova N, Szymusiak R, Alam MN, Guzman-Marin R, McGinty D. Sleep-waking discharge patterns of median preoptic nucleus neurons in rats. J Physiol. 2002;543:665–77. doi: 10.1113/jphysiol.2002.023085. PHY_023085 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 15.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]