Abstract
Terminal erythroid differentiation occurs in the bone marrow, within specialized niches termed erythroblastic islands. These functional units consist of a macrophage surrounded by differentiating erythroblasts and have been described more than five decades ago but their function in the pathophysiology of erythropoiesis has remained unclear until recently. Here we propose that the central macrophage in the erythroblastic island contributes to the pathophysiology of anemia of inflammation. After introducing erythropoiesis and the interactions between the erythroblasts and the central macrophage within the erythroblastic islands, we will discuss the immunophenotypic characterization of this specific subpopulation of macrophages. We will then integrate these concepts into the currently known pathophysiological drivers of anemia of inflammation and address the role of the central macrophage in this disorder. Finally, as a means of furthering our understanding of the various concepts, we will discuss the differences between murine and rat models with regards to developmental and stress erythropoiesis in an attempt to define a model system representative of human pathophysiology.
Keywords: Erythroblastic Island, Anemia of Inflammation, Bone Marrow Macrophages, Terminal Erythroid Differentiation, Animal Models
Introduction
Anemia, defined by a decrease in the hemoglobin concentration, results from either increased peripheral destruction or decreased production of red blood cells (RBCs) or both. Anemia of inflammation is the second most common cause of anemia after iron deficiency [1] and is primarily an immune driven pathologic process that is frequently associated with various conditions, such as acute and chronic infections, sepsis, malignancies, autoimmune disorders, and chronic kidney disease [2]. Anemia of inflammation presents a clinical challenge as its consequences in the context of the aforementioned associated conditions leads to poorer prognosis, particularly in elderly patients with preexisting risk factors such as coronary artery disease, pulmonary disease, and chronic kidney disease [3]. In the most clinically dire cases such as in sepsis, the recommendation guidelines published by the Surviving Sepsis campaign [4] includes the usage of transfusions to obtain a hematocrit of 30%, which was found to be correlated with better patient outcomes than those who did not [5]. However, the limited clinical efficacy of repeated transfusions to correct anemia of inflammation suggests the need for an improvement in therapeutic strategies. In this context, increasing the red cell mass and thereby the hemoglobin concentration by stimulating red cell production remains appealing. Due to the complex nature of anemia of inflammation, a more complete understanding of erythropoiesis during both normal physiology and anemia of inflammation are warranted.
In the present review, we will first discuss erythropoiesis as a finely tuned cellular process. We will then introduce the erythroblastic island, the specialized niche within the bone marrow that support erythropoiesis; and expand on the known and putative roles played by bone marrow-derived macrophages at the center of these anatomic niches. We will integrate these concepts into the currently known pathophysiological drivers of anemia of inflammation and address areas requiring further research. Finally, as a means to answer these questions, we will discuss the differences between murine and rat models in regards to developmental erythropoiesis in an attempt to define a model system representative of human pathophysiology.
Erythropoiesis in the normal adult and its regulation by erythropoietin
From the hematopoietic stem cell to the red blood cell
Erythropoiesis in humans is an essential and highly regulated process that maintains the production of 2×1011 RBCs per day needed to maintain homeostatic oxygen delivery to tissues. In the bone marrow, red cell formation begins with the proliferation and commitment of the hematopoietic stem cell (HSC). Multipotent and minimally self-renewing short-term hematopoietic stem cells (ST-HSC) acquire hematopoietic lineage restricted transcription factors that drive differentiation to an erythroid/myeloid/megakaryocytic-forming progenitor, the common myeloid progenitor (CMP). The CMP expresses the transcription factors Tal1/SCL, GATA-2, NF-E2, GATA-1, C/EBPa, c-Myb, and PU.1 [6]. Further erythroid restriction to the megakaryocyte-erythroid progenitor (MEP) at the CMP stage requires the dominant expression of GATA-1, the master erythroid transcription factor, at the expense of PU.1 [7]. As hematopoietic progenitors progressively mature, they upregulate another erythroid-specific transcriptional factor, EKLF/KLF1, beginning as early as the CMP stage [8]. KLF1 itself is necessary for both the cell fate decisions at the MEP level and the transition from erythroid precursors (the Burst Forming Unit-Erythroid, BFU-E, and Colony Forming Unit-Erythroid, CFU-E) to the terminally differentiating erythroblasts. Indeed, overexpression of KLF1 induces greater levels of erythropoiesis than megakaryopoiesis from the MEP population with high numbers of developing erythroblasts [9]. Conversely, knockdown of KLF1 favors megakaryocyte formation and prevents the transition of CFU-E to the proerythroblasts [10], highlighting the central role of KLF-1 in lineage fate decisions.
Terminal erythroblast maturation marks the final stages of erythropoiesis, and takes place in a specialized erythroid microenvironment, the erythroblastic island, which will be discussed in greater details in this review. Proerythroblasts proceed through a number of subsequent mitoses to sequentially generate basophilic erythroblasts, polychromatic erythroblasts, and orthochromatic erythroblasts. This process is regulated notably by the concerted function of GATA-1, Tal1/SCL, LMO2, LDB1 and KLF1 [11]. Many of these regulatory proteins share overlapping areas of chromatin to modify gene expression (e.g. GATA-1 and KLF1) [12]. During terminal maturation, hemoglobin synthesis increases, cell size decreases, and the nucleus condenses. The condensed nucleus of the orthochromatic erythroblast is expelled through the intricate process of enucleation [13,14], and the central macrophage engulfs and degrades the newly released pyrenocyte, a pyknotic nucleus surrounded by a rim of cytoplasm and plasma membrane [15,16]. Recognized as a necessary step for mammalian erythropoiesis [17], the molecular mechanisms underlying enucleation are still not entirely clear. Nascent reticulocytes remain in the bone marrow for about 48 hours, and then enter the bloodstream where they mature for an additional 24 hours. Reticulocyte maturation completes erythropoiesis, with the elimination of the remnants of internal organelles [18–20] and extensive membrane remodeling [21,22]. Ultimately, mature erythrocytes survive for about 120 days in the blood stream. Figure 1 summarizes the different stages of erythropoiesis.
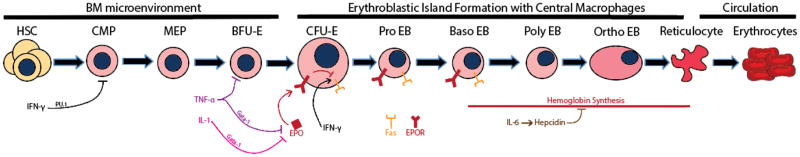
Figure 1. Erythropoiesis and its modulation by hormones and inflammatory cytokines.
Erythropoiesis begins with the hematopoietic stem cell which gives rise to the common myeloid progenitor (CMP), the megakaryocyte erythrocyte progenitor (MEP) and the Burst Forming Unit (BFU-E), which all develop sequentially within the microenvironment of the bone marrow. Starting at the Colony Forming Unit (CFU-E) stage, cells begin to attach and interact with the central macrophage to form the erythroblastic island and begin hemoglobin synthesis starting at the basophilic erythroblast stage until the formation of the reticulocyte, which then enters the circulation. Inflammatory cytokines interrupt the process of erythropoiesis at several stages of development. IFN-γ interferes at the CMP stage to push towards the megakaryocyte lineage, decreasing the numbers of MEP and BFU-E. IFN-γ also increases the number of Fas receptors leading to apoptosis of the EPO-R expressing stages of erythoid precursor cells. TNF-α and IL-1 together interact through GATA-1 to decrease the production of EPO. During stages of hemoglobin synthesis, the production of IL-6 and hepcidin prevent the availability of iron to the erythroblasts.
Regulation of erythropoiesis by erythropoietin
Of the many intrinsic and extrinsic factors that regulate red cell mass, the hormone erythropoietin (EPO) is the best studied and important in the context of anemia of inflammation. Decreased erythrocyte numbers and subsequent hypoxia stimulates EPO production by a heterogeneous population of peritubular interstitial fibroblast-like cells in the kidneys [23,24]. Crucial to the induction of EPO synthesis in these hypoxia-sensing cells is the regulation of intracellular hypoxia inducible factor-2α (HIF-2α) levels. Under normoxic conditions, the concerted function of prolyl hydroxylase and Von Hippel-Lindau target HIF-2α for degradation. However, hypoxia prevents hydroxylation of HIF-2α, and results in the stabilization of HIF-2α [25]. HIF-2α then translocates to the nucleus where it binds to regulatory elements upstream of the EPO gene to induce its expression and secretion [26]. EPO levels in the plasma then rise and the hormone acts on the bone marrow compartment where it stimulates red cell production. However, not all differentiating erythroid cells are sensitive to EPO (Figure 1). Indeed, the EPO receptor (EPO-R) is only expressed from the CFU-E to the basophilic erythroblast stages [27], as shown in Figure 1. At the molecular level, the signaling cascade leading to prevention of apoptosis of erythroblasts by Epo has been identified [28]. Once EPO binds to its receptor, its triggers phosphorylation of EPO-R, and subsequently, the activation of the STAT5, PI3-kinase/Akt, and MAP-ERK transduction pathways [29]. Ultimately, there is a decrease in the quantity of Fas membrane protein in response to EPO signaling, leading to a decrease in apoptosis [30]. Thus, EPO is a critical factor for erythroblast survival.
Erythroblastic Islands
Definition
The term erythroblastic island first appeared in the literature in 1958, when the French hematologist, Marcel Bessis, proposed it as “the functional unit of the bone marrow” [31]. In 1978, Mohandas and Prenant produced a three-dimensional reconstruction of the rat bone marrow, and confirmed Bessis’ original hypothesis [32]. These erythroblastic islands are specific to fetal and adult erythropoiesis and are not observed in the yolk sac [33]. As many as 30 to 48 developing erythroid cells, ranging from the CFU-E to the reticulocyte stage are found to be associated with macrophages also known as the central macrophage [31,34].
Interactions between differentiating erythroblasts and the central macrophage
Although erythroblasts can proliferate and enucleate in the absence of macrophages in vitro, this process is still relatively inefficient in comparison to the rates of erythropoiesis in vivo [35,36], highlighting the critical role for cell-cell interactions in physiological regulation of red cell production. Indeed, macrophages and erythroblasts share many cell-cell adhesion molecules. One of the first molecules identified in mediating the erythroblast-macrophage adhesive interactions was EMP (erythroblast macrophage protein, also known as macrophage erythroblast attacher, MAEA), which enables the interaction of developing erythroblasts with the macrophages via homophilic interactions [37]. Blockade of EMP using anti-EMP during in vitro studies resulted in decreased proliferation, maturation and enucleation [35], and Emp−/− mice presented with severe anemia and perinatal death [38]. Several other sets of critical adhesion molecules have been subsequently identified within the erythroblastic islands, such as α4β1-integrin on erythroblasts and vascular cell adhesion molecule-1 (VCAM-1) on the central macrophages [39]. Studies from Dr. Chasis’ group further showed that perturbing the interaction between the erythroid intercellular adhesion molecule-4 (ICAM-4) and macrophage αV-integrin resulted in the decreased formation of erythroblastic islands [40]. In addition, several additional surface markers have been identified on the central macrophage yet their counterpart receptors on erythroid precursors remain unknown. For example, ER-HR3, a rat monoclonal antibody was found to recognize a mouse antigen expressed by central macrophages in the mouse [41]. CD169, or sialoadhesin, was found on central macrophages and binds to an unidentified erythroblast sialylated glycoprotein within the erythroblastic island [42]. Further, CD163 was also identified as a macrophage adhesion glycoprotein and functions as a hemoglobin-haptoglobin complex receptor as well as being involved in increasing erythroid expansion [43].
Functionally, one of the most highly specific processes within the erythroblastic island performed by the central macrophage is the engulfment of the enucleated nucleus [44], and subsequent recycling of nucleotides after nuclei degradation [45]. Remarkably, the last division of the developing erythroblast is asynchronous, resulting in the formation of an enucleated reticulocyte and a pyrenocyte [15]. Both EMP and β1 integrin partition to the plasma membrane of the pyrenocyte, in order to facilitate its interaction with the central macrophage and subsequent phagocytosis [46]. Critical to the engulfment of the pyrenocyte is the macrophage expression of Mer tyrosine kinase receptor, which recognizes protein S that is bound to the phosphatidyl serine exposed by the pyrenocyte membrane [16,47].
While the factors governing the formation of erythroblastic islands remain to be fully elucidated, candidate genes are emerging. For example, KLF1 directly upregulates the expression of ICAM4, and KLF1 knockout studies result in significantly reduced levels of ICAM4 [8,48]. Furthermore, KLF1 has been shown induce the expression of macrophage DNase2a, a nuclease that leads to the digestion of the pyrenocyte [49]. These findings illustrate an important role of KLF1 in regulating multiple genes that facilitate erythroid precursor interactions with the central macrophage in erythroblastic islands. Another candidate gene identified for the formation of the erythroblastic island is Tropomodulin 3 (Tmod3), an actin-binding protein. Tmod3 is expressed by both erythroblasts and macrophages, and Tmod3−/− mice present with defective erythroblastic islands [50]. Clearly, further exploration is needed to identify the specific regulatory networks underlying the development of erythroblastic islands.
Immunophenotypic characterization of the central macrophage
A major challenge in the fields of erythropoiesis and macrophage biology has been the isolation and characterization of the specific functional population of central macrophages, as the bone marrow houses a widely heterogeneous population of macrophages. To date, it has not been possible to identify a unique surface protein that is exclusively expressed by the population of central macrophages. Initial isolation and immunocytochemical characterization of human central macrophages include CD4, CD11a, CD11c, CD18, CD31, HLA-DR, FcRI, FcRII, and FcRIII [51]. The F4/80 antigen and Forssman glycosphingolipid have been described as distinguishing markers of central macrophages but seem to be restricted to the mouse system [52,53].
Recent studies have begun to provide new insights into the phenotypic characterization of populations of macrophages that can be used to analyze the functions of central macrophages of erythroblastic islands. Using a combination of antibodies specific for CD169, VCAM-1, ER-HR3, CD11b, F4/80, and Ly-6G, adult mouse bone marrow and spleen macrophages were isolated via flow cytometry [54]. In the same study, CD169+ specific deletion using a simian diphtheria toxin receptor resulted in the loss of the CD11b+/F4/80+/VCAM1+/CD169+/ER-HR3+/Ly-6G+ macrophages as well as the loss of erythroblasts and reticulocytes from the bone marrow and the spleen. The increase in proerythroblasts, however, suggested a defect in maturation attributable to the disruption of the erythroblastic island. More interestingly, the same group observed that the administration of G-CSF to the mouse depleted the above-mentioned population of macrophages by 90% and reduced medullary erythropoiesis but also observed that G-CSF increased splenic erythropoiesis and erythroblastic island macrophages [54]. It remains to be seen how similar or different the populations of macrophages are that reside in the bone marrow compared to the populations found in the spleen and in the liver. This finding, along with the knowledge that, in humans, CD169 is expressed by macrophages in the bone marrow, splenic red-pulp, and liver macrophages [55] implies that CD169 specific depletion of macrophages is insufficient for the isolation of the bone marrow macrophages involved in definitive erythropoiesis. Indeed, in recent studies, splenectomized CD169+ macrophage depleted mice did not develop overt anemia, and the numbers of splenic red pulp macrophages and hepatic Kupffer macrophages decreased along with the number of bone marrow macrophages [56]. The authors reasoned that the number of macrophages involved in erythrocyte clearance is also decreased and thereby increased the overall life span of the erythrocytes accounting for the lack of anemia seen in the mice. While the panel of markers on human bone marrow aspirate may allow for an analysis of a subset of the population of central macrophages involved, it remains to be seen whether CD15−/CD163+/CD169+/VCAM1+ is sufficient for isolating a homogenous bone marrow macrophage population responsible for the formation of the erythroblastic islands in human bone marrow. However, it is an exciting start to determine if this population expresses the known specific cell adhesion molecules and which genetic transcription factors define it. Furthermore, differences in terms of tissue specific extramedullar erythropoietic response to anemia in mice and man have complicated the design of studies in terms of strategizing experimental strategies that enable the characterization of the specific functional population of central macrophages regulating erythropoiesis.
Pathophysiology of anemia of inflammation
At the core of the pathophysiology of anemia of inflammation is the production of the pro-inflammatory cytokines, IL-1, TNF-α, IFN-γ, and IL-6, which are inhibitory to the necessary and proper erythropoietic response in the face of anemia [57]. The systemic pathological processes include decreased EPO production and sensitivity [58], ineffective erythropoiesis, the dysregulation of iron homeostasis, and the shortened half-life of erythrocytes due to premature clearance.
Insufficient Bone Marrow Response to Erythropoietin
The insufficient bone marrow response to maintain steady-state erythropoiesis during anemia of inflammation can be partly explained by lower than expected EPO levels when compared to the levels observed in iron deficiency anemia [59]. In conditions such as rheumatoid arthritis, anemic patients display low levels of EPO in the plasma [60]. In addition, the reduced levels of EPO may have a contributing role in the sequestration of iron in macrophages, as EPO has been shown to negatively affect hepatic production of hepcidin [61], leading to hypoferremia, as discussed below. However patients with both hematologic malignancies and anemia of inflammation also have a blunted EPO response [62], suggesting signaling molecules beyond EPO might be at play.
In agreement, despite these findings of insufficient EPO production, the low levels of EPO are not the major mechanism behind anemia of inflammation, as the administration of EPO is insufficient to correct the anemia in patients [63]. Evidence supporting this theory is derived from the observation that patients with both renal disease and inflammation with a serum C-reactive protein (CRP) level of greater than 20 mg/L required higher doses of EPO than patients with primary EPO deficiency [64]. Furthermore, patients with CRP greater than 50 mg/L treated with high doses of EPO achieved hemoglobin concentrations less than that seen in a population of patients with CRP less than 50 mg/L treated with lower doses of EPO, indicating that the resistance to EPO during inflammation is partly responsible as well [63,65]. Experimentally, studies conducted with the EPO-producing cell line Hep3B, inflammatory cytokines TNF-α and IL-1 were shown to have an inhibitory effect on EPO production mainly through the effects of GATA-1 on the EPO promoter, and GATA-1 inhibitors were shown to reverse the suppression of EPO caused by TNF-α and IL-1 [66]. Accordingly, higher levels of EPO are needed to reconstitute the ability for the formation of CFU-E [67]. Other studies using TNF-α and IL-1 in vitro demonstrated that the effects of the cytokines are also due to the production of reactive oxygen species that interfere with the binding affinity of transcription factors that induce EPO expression [68]. An additional cytokine, IFN-γ has been identified as the major inflammatory cytokine involved in resistance to EPO response and has been shown to downregulate EPO receptors on erythroid precursors [69].
Hypoferremia and the role of hepcidin
The common response to systemic infection and inflammation is the production of IL-6, which stimulates hepatic production of hepcidin within hours of onset [70] (Figure 3). Hepcidin is the major regulator of circulating iron plasma levels and acts by binding to the membrane protein ferroportin, resulting in its internalization and subsequent degradation [70]. Pathologically excessive levels of hepcidin ultimately lead to a state of hypoferremia due to the decrease in iron export into the plasma from macrophages and hepatocytes [70]. The degradation of ferroportin also prevents the needed increased ability of duodenal enterocytes to absorb iron into the circulation [71] (Figure 3). Therefore, induction of hepcidin by inflammation and subsequent hypoferremia limit erythropoiesis.
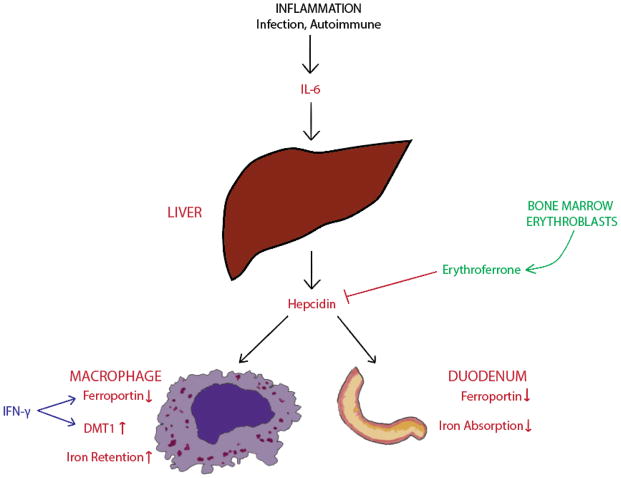
Figure 3. Hepcidin in anemia of inflammation.
The state of inflammation initiated by underlying causes such as overwhelming and/or chronic infection, autoimmune diseases, or malignancies lead to the production of IL-6 which act on the liver to produce hepcidin, ultimately decreasing ferroportin at both the enterocytes located at the duodenum and splenic macrophages. The increased iron retention by macrophages and decreased iron absorption by the enterocytes lead to a state of hypoferremia. Recently, an erythroid regulator called erythroferrone has been shown to inhibit the production of hepcidin. Iron retention by the macrophage is further regulated by IFN-γ.
The antagonist relationship between hepcidin and erythropoiesis was inferred when hepcidin levels were reduced in mouse models of anemia, following erythroid recovery [72]. Additionally, inhibition of hepcidin required proper production of EPO and a functioning bone marrow [73]. Recently, erythoferrone (ERFE) was identified as a new negative regulator of hepcidin. ERFE is produced by bone marrow erythroblasts and acts upon the liver to suppress hepcidin production [74] (Figure 3). Due to the fact that ERFE is elevated in β-thalassemia and is involved in the pathology of iron overload [75], perhaps simultaneous administration of ERFE and iron may be an exciting prospective strategy in alleviating the entrapment of iron associated with anemia of inflammation.
While the direct relationship between IL-6 and the induction of hepcidin explains the inadequate erythropoiesis by limiting iron availability for heme biosynthesis [70], other pro-inflammatory cytokines can also play a role in iron dysregulation. IFN-γ and TNF-α have been reported to increase the expression of divalent metal transporter 1 (DMT1) in macrophages thereby increasing iron uptake [76] (Figure 3). Furthermore, TNF-α, IL-1, IL-6 and IL-10 all stimulate the sequestration and storage of iron within macrophages by increasing ferritin expression.
Inflammatory Inhibition of Erythropoiesis
In addition to iron dysregulation, pro-inflammatory cytokines during anemia of inflammation have been involved in the process of proper proliferation and differentiation of erythroid precursors. TNF-α, IL-1, and IFN (both –α, -β, and –γ) have been shown to have inhibitory effects on the proper development of BFU-E and CFU-E to various extents [67]. Furthermore, IFN-γ has especially prominent negative effects on hemoglobin concentration and reticulocyte count and also affect the development of early EPO dependent stages of erythropoiesis, from the CFU-E to the basophilic erythoblast stages [77], by downregulating EPO receptors as well as decreasing expression of stem-cell factor [69]. Moreover, mouse studies have shown that IFN-γ can also directly block erythropoiesis by acting even earlier in developmental stages, at the CMP stage of hematopoiesis, by inducing the expression of the transcription factor PU.1 [78]. The effects of increased PU.1 expression results in a lineage switch at the CMP stage, resulting in an increased myeloid differentiation at the expense of erythroid differentiation, causing decreased numbers of erythroid precursors at the MEP and BFU-E stages [58]. In human in vitro studies, IFN-γ and other inflammatory cytokines heightened the sensitivity of EPO dependent erythroid precursors to undergo extrinsic apoptosis through increased expression of TNF superfamily receptors [79,80].
The other major inflammatory cytokine, TNF-α, can lead to erythrocyte damage induced by free radicals, resulting in an increase in erythrophagocytosis [81]. The interaction between TNF-α and erythroid precursors was further examined in the context of rheumatoid arthritis, in which up to 50% of patients exhibit anemia of chronic disease [82]. Increased TNF-α levels have been shown in vitro to inhibit the production of erythroid colony formation [83,84], and increased serum levels of TNF-α have been positively correlated with increasing degrees of anemia associated with rheumatoid arthritis [85]. Additionally, human bone marrow samples from these patients have decreased numbers of erythroid progenitor and precursor cells, low BFU-E colony formation, due to increased apoptosis in the erythroid precursor populations [86]. Further evidence in the same study supported the role of TNF-α in anemia of inflammation as the administration of anti-TNF-α antibody not only increased hemoglobin concentration, but also reduced the proportion of apoptotic cells in both the erythroid progenitor and precursor populations [86].
Erythroblastic Islands in Anemia of Inflammation
As mentioned earlier, the administration of recombinant erythropoietin remains as a useful but incomplete means of stimulating erythropoiesis in anemia of inflammation. Indeed, EPO administration increases hemoglobin concentration (and hematocrit) but does not reduce the number of red cell transfusions needed to correct the anemia [87]. Because recent studies have suggested a role for erythroblastic islands during stress erythropoiesis [56] and their involvement in supporting altered proliferation of erythroid precursor cells in a disease context such as polycythemia vera [88], increasing attention in the field is now focused on structural and molecular protein interactions between developing erythroblasts and central macrophages as well as the transcription factors that regulate these processes in the central macrophage. Our review not only recognizes these questions as crucial in understanding definitive erythropoiesis, but also extends the question to the role of these bone marrow central macrophages in the context of anemia of inflammation, particularly concerning the set of chemokines and cytokines that are produced both systemically and by the macrophages themselves that may have an effect on erythropoiesis per se.
Central to our question on macrophage function in the context of anemia of inflammation are the cytokines that are produced by these central macrophages within the erythroblastic island and their subsequent effects on erythropoiesis. Cellular interactions within the erythroblastic islands are complicated by a series of paracrine and autocrine signaling pathways. For example, Gas6 enhances Epo receptor signaling on erythroblasts and binds to its receptor on macrophages to reduce erythroid inhibitory factors [89]. Factors secreted by macrophages can also positively influence erythropoiesis such as insulin-like growth factor-1, which stimulates erythropoiesis at both the BFU-E and CFU-E stages [90]. While these positively regulating cytokines are important for the proper balance of erythropoiesis, much attention has also been diverted to the negatively regulating cytokines, especially those produced by underlying conditions such as autoimmune disorders or chronic infections that cause a systemic state of inflammation. However, as previously mentioned, local increased levels of TNF-α, IL-6, IFN-γ, and TGF-β in the bone marrow have also been associated with anemia of chronic inflammation [91]. TNF-α suppresses erythropoiesis through the caspase-activated cleavage of GATA-1, without which erythroid development is impaired and results in apoptosis [92] or in the disruption in proliferation of erythroid progenitors [93]. In addition, TNF-α has an effect on macrophages, causing a release of metalloproteases to disturb the adhesive interactions necessary for erythroblast island formation [94]. TGF-β activates Rho and Rac GTPases, altering the actin cytoskeleton that is finely tuned by cytoskeletal proteins within the erythroblasts, compromising the integrity of the cell membrane [95]. IFN-γ causes the secretion of TNF-related apoptosis inducing ligand (TRAIL) by both macrophages and erythroblasts, which activates ERK/MAPK to inhibit erythroblast differentiation [96,97] (Figure 2).
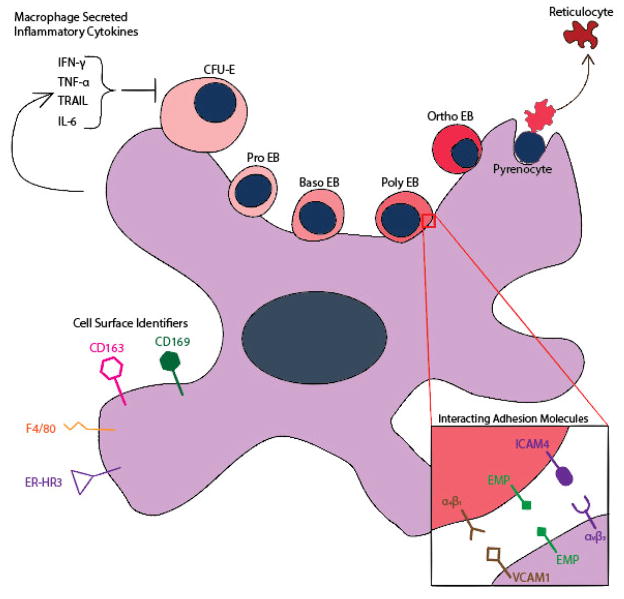
Figure 2. The erythroblastic island.
From the CFU-E stage to the formation of the reticulocyte, developing erythroblasts attach to a central macrophage located in the bone marrow through the use of α4β1, EMP, and ICAM4. The central macrophage mediates these interactions through VCAM1, EMP, αvβ3 respectively. Other cell surface identifiers expressed by the macrophage are CD163, CD169, F4/80, and ER-HR3. The inflammatory cytokines produced by the macrophages within the context of anemia of inflammation are known to inhibit erythropoiesis, particularly IFN-γ, TNF-α, TRAIL, and IL-6.
In addition to their identity, a related question is whether anemia of inflammation alters polarization of the central macrophage in the erythroblastic island and whether this process interferes with erythroblast development. Classically, activation of macrophages to the polarized M1 state is due to the production of reactive oxygen species and pro-inflammatory cytokines [98]. Conversely, the M2 polarization of macrophages is activated by IL-4, IL-13, TGF-β, and glucocorticoids and involves the regulation of the resolution phase of inflammation [99]. Upon comparison of gene expression profiles of genes related to iron homeostasis, over 60% of those genes were differentially expressed between M1 and M2 macrophages [100]. Whereas the M1 macrophages were shown to induce gene expression patterns that allow for iron sequestering, M2 macrophages not only downregulated expression of ferritin, but also actively exported iron through ferroportin [101]. One particularly interesting difference was the increased expression of CD163 by M2 macrophages, allowing for an increased ability to bind and internalize hemoglobin/haptoglobin complexes, a process necessary for the detoxification of heme associated iron [102]. Interestingly, CD163 was used as one of the cell surface markers used to isolate populations of bone marrow macrophages associated with erythroblastic islands that expressed both VCAM1 and CD169 [56]. It also seems that CD163 can act to mediate the binding of macrophages to erythroid precursors to induce proliferation and continued differentiation [43]. This suggests that the macrophage population supporting erythroblastic island formation exhibit gene expression profiles closer to the M2 polarization, but the degree of this overlap is still uncertain.
While the M1 and M2 classifications broadly describe the population that may include those of the central macrophages, a functional characterization guided by gene expression profiles is needed to validate and study a homogenous population of macrophages specific for the formation of erythroblastic islands. While our knowledge of the necessary transcription factors for these macrophages is incomplete, it is known that the retinoblastoma tumor (Rb) protein is crucial for the proper differentiation of these macrophages [103]. In Rb−/− mice, fetuses are severely anemic and die in utero from abnormal fetal liver erythropoiesis and failure of enucleation [104]. In addition to the role of Rb in erythroblasts [105,106], experimental evidence suggests a role of Rb in macrophages as well, since macrophages do not properly differentiate due to the inability of Rb to stop the inhibition of PU.1 by inhibitor of DNA-binding protein 2 (Id2) in Rb−/− mice [103]. Another example is the transcription factor c-Maf, which recognizes Maf recognition elements (MARE) or 5′ AT-rich half MARE in order to bind to DNA and regulate cellular proliferation and differentiation [107,108]. c-Maf was found to be expressed highly in fetal liver macrophages and necessary for the development of erythroblastic islands [109]. Further, it was found that the reduction of c-Maf resulted in decreased expression of VCAM-1, contributing to the defective interactions necessary for erythroblastic island development [109]. Other transcription factors that regulate specific cellular proteins and processes to the central macrophages remain unknown, particularly those that control the expression of EMP, αV-integrin, and the cytoskeletal-associated proteins that enable proper island formation and erythroblast enucleation.
Recently, the findings of KLF1 expression in macrophages has raised questions of not only the transcriptional machinery that regulates central macrophage function, but also on the ontogeny of the macrophages that comprise the erythroblastic islands [54,110]. The current dogma describes macrophages deriving from granulocyte-monocyte progenitors and erythroid cells from the MEP, with each progenitor population arising from the more developmentally immature population, the common myeloid progenitor, or CMP. In addition to this concept it is widely accepted that KLF1 is a transcription factor that is highly specific to the erythroid cell lineage [8]. A recent study challenges both these concepts by documenting that mouse embryonic stem cells could generate a clonal line giving rise to both erythroid cells and macrophages, which together formed physical structures that resembled that of erythroblastic islands [111]. It is still unknown, however, the correlation of these macrophages, anatomically and temporally to the erythroblastic islands, whether primitive, fetal, or bone marrow definitive [54].
Macrophages also play an important role in iron homeostasis. As mentioned earlier, hepcidin and the sequestration of iron in bone marrow macrophages play a pivotal role in contributing to the development of anemia of chronic inflammation. The recycling of iron begins as senescent and damaged erythrocytes are detected and engulfed by splenic red pulp macrophages [112]. Mechanisms in place for the surveillance of aging red cells are associated with the continual remodeling of the membrane as the erythrocytes circulate and are exposed to both oxidative and mechanical stress [113]. Other studies have described mechanistic details for the removal of aged erythrocytes, including those that describe the roles of band 3, phosphatidylserine, CD47, and complement receptor 1 [114–117]. After the ingestion of erythrocytes by macrophages into phagolysosomes, hemoglobin is degraded into heme and iron for recycling processes aided by heme-responsive gene 1 protein [118], and the cytosolic iron cations are further processed for transport by natural resistance associated macrophage protein (Nramp1) and divalent metal transporter 1 (DMT1) [119]. While the majority of the recycled iron supply is redistributed by transferrin molecules to return to developing erythroblasts to aid in the production of hemoglobin, some evidence suggests that macrophages may have a role in directly supplying iron to erythroid precursors, originally suggested by Marcel Bessis [120]. In co-culture experiments with human peripheral macrophages and erythroblasts grown in transferrin-free conditions, ferritin expression and evidence of exocytosis by the macrophages was documented [121]. However, the mechanisms by which macrophages, especially those that reside in the bone marrow, directly transfer iron into developing erythroblasts are still unknown. Therefore, a better understanding of iron metabolism in the erythroblastic island would certainly further our knowledge of the pathologic cellular events in the context of anemia of inflammation.
Of mice, rats and men: which model to study anemia of inflammation
Throughout the development of the hematopoietic system in vertebrates, the pool of progenitor populations giving rise to red cells occur not only in multiple temporal waves but at various anatomic sites throughout the body as well [122]. Similarly, it is likely that erythroblastic island macrophages and their progenitors reflect anatomical and developmental-specific populations. The laboratory mouse (Mus musculus) is a widely used model system in biology, and has been critical for the discovery of hematopoietic genes and our understanding of the ontogeny of the two distinct erythroid lineages, embryonically primitive and the adult definitive [123–125]. While these studies have provided a wealth of knowledge in understanding normal physiology of the human erythropoiesis, the differences between the species has complicated the direct relevance of the findings from the murine system to humans in the context of anemic disease and stress erythropoiesis, particularly concerning the role of the population of central macrophages. Therefore, by outlining the similarities and differences among mice, humans and rats we offer considerations for in vivo experiments aimed at understanding erythroblastic island physiology and pathology, and suggest that the rat is a better system for the study of erythroblastic islands.
Three developmental waves characterize the establishment of mammalian hematopoietic systems [126]. The first wave of hematopoiesis occurs at the site of the yolk sac, and together with macrophages and megakaryocytes, primitive erythrocytes (EryP) [127] are produced from hemangioblasts [128]. During the initial embryonic primitive phase of erythropoiesis, the EryP cells are characterized as large, nucleated cells and persist only for a transiently short period up until birth [129–132]. EryP cells retain their nucleus for the initial phase of their circulation during gestation until they also ultimately expel their nuclei as they mature within the circulation [132]. A subsequent transient wave from the yolk sac is then termed as the second wave, consisting of definitive erythroid cells (EryD), megakaryocyte, and myeloid lineage cells [129]. In contrast to EryP, these erythrocytes originate from BFU-Es that migrate to the fetal liver from the yolk sac and develop extravascularly to enucleate before entering the circulation [131]. The third and final wave arises from HSCs originating from the major embryonic arteries, which seed the fetal liver; later these definitive HSCs colonize the bone marrow [127,133,134]. In addition to their anatomic differences, it is currently proposed that definitive erythroid populations arise from discrete progenitors. Indeed, the first definitive erythroid population arises from the yolk sac erythroid myeloid progenitor population and the second wave of definitive erythroid population is seeded by the hematopoietic stem cell population arising from the major embryonic arteries [135]. Both phases of definitive erythropoiesis are characterized by extravascularly enucleated red cells and correlate with the formation of the erythroblastic island which have been observed in the fetal liver, bone marrow, and the red pulp of the spleen in the murine system [136]. Since these blood cells derive from separate progenitors, we may infer that the central island macrophage could originate from two distinct populations.
In contrast to developmental embryonic erythropoiesis, humans, mice, and rats possess divergent steady-state erythropoiesis in the adult. Unlike the human hematopoietic system, where erythropoiesis predominates in the bone marrow, the mouse spleen continually houses hematopoietic stem cells and remains a major organ contributing to erythropoiesis in response to anemia [137]. While bone marrow erythropoiesis in humans can generate 20-fold more red cells upon stimulation than at steady state, murine bone marrow erythropoiesis can increase red cell production less that 2-fold. Furthermore in rats, the shift of erythropoiesis from the spleen to the bone marrow is much more significant [138], with the adult rat spleen contributing less than 5% of its total erythropoietic activity and all of increased red cell production taking place in the bone marrow in response to anemia [139]. This is a much smaller fraction of splenic contribution of erythropoiesis than that occurs in the mouse [140]. Thus, erythropoiesis in the rat is highly reminiscent of human erythropoieisis.
An even greater difference among murine, rat, and human erythropoiesis is observed under anemic and/or hypoxic conditions, which activates a stress response to increase erythropoiesis, rapidly increasing the generation of replacing erythrocytes [141–143]. In mice, the spleen is the primary site for stress erythropoiesis [142,144–149], with the liver also involved as an extramedullary site for erythropoiesis [150,151]. It has also been well documented that spleen-derived stress erythroid progenitor cells of mice are distinct from the erythroid progenitor cells that are active during steady state erythropoiesis in the bone marrow [142]. Mechanistic insight from these studies detailed a distinct resident population of erythroid progenitors in the spleen of mice that utilize a BMP4-dependent stress erythropoiesis pathway and more importantly, the authors highlighted that such a pathway for human extramedullary stress erythropoiesis has not been identified. In fact, unless under pathologic conditions, splenic erythropoiesis is not a feature of stress erythropoiesis in humans except in case of myelofibrosis and other conditions in which the bone marrow space is exhausted for red cell production. Furthermore, the contribution of splenic erythropoiesis when recovering from anemic conditions was found to be minimal in rats [152]. Together, we conjecture that the populations of macrophages that provide a microenvironment for erythropoiesis correlate and differ accordingly based on anatomic location and because of this, likely influence the necessary capabilities of extramedullary stress erythropoiesis. Central to our understanding of the role of erythroblastic islands during pathologic conditions is the ability to study homologous systems. As rat and human adult definitive erythropoiesis share more commonalities than human and murine erythropoiesis, we propose that the rat hematopoietic system represents a more faithful in vivo model to study the role of erythroblastic islands in the context of anemia of inflammation.
Conclusions
A fuller understanding of the positive and negative regulators of central macrophage of the erythroblastic islands is vital for developing novel therapeutic strategies. As various pathologic inflammatory conditions disrupt the erythropoietic response via inflammatory cytokines, it is conceivable that these deleterious effects could be mitigated by the appropriate administration of antibodies that target purified populations of central macrophages must be reproducibly identified and isolated in a manner that allows for them to be studied using global approaches such as RNAseq and comprehensive proteomic analyses. Secondly, it is important to determine how each inflammatory cytokine, both independently and in concert with other cytokines, disrupts the integrity of the erythroblastic island. For example, what process of erythroblast enucleation is most compromised? What stage of erythroblast development is most vulnerable to the disruption of the erythroblastic island? Is the pathologic process an issue with the ratio of central macrophages to erythroblast precursors or an issue with the absolute number of central macrophages available in the bone marrow? Furthermore, a more complete understanding of erythroblastic islands will not only benefit our understanding of red blood cell pathologies, but also, the ability to differentiate sufficient numbers of red blood cells in vitro for transfusions using a universal donor derived progenitor cell at either the hematopoietic stem cell or pluripotent stem cell stage [153,154].
To our knowledge, there has yet to be a universal ex vivo system capable of producing sufficient numbers of fully mature and functional erythrocytes on an economic mass scale for the use of widespread clinical transfusions [155]. Perhaps a complete understanding of the interplay between central macrophages and erythroblasts may unravel novel strategies to provide such a method.
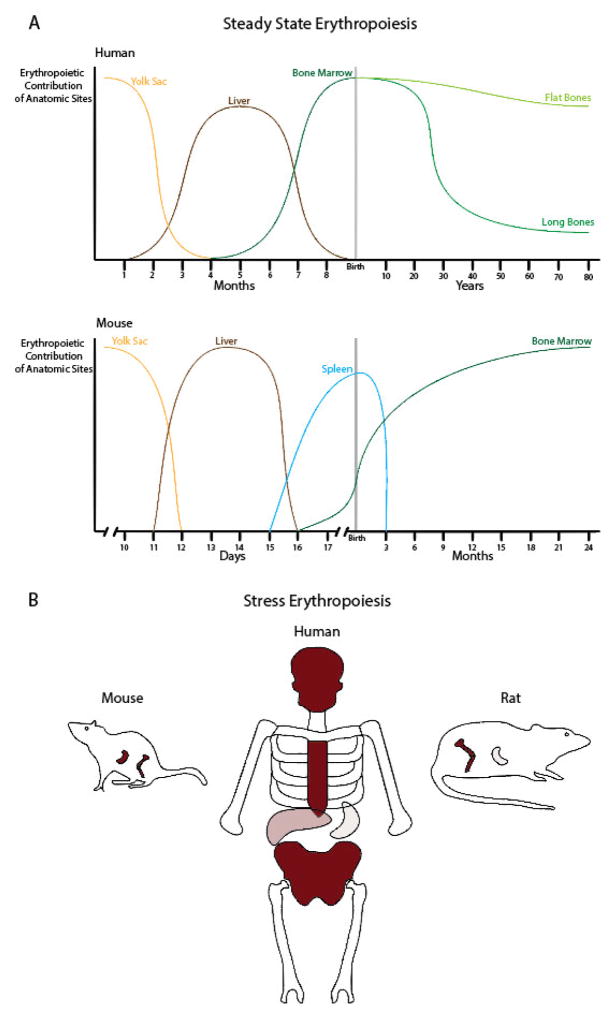
Figure 4. Anatomic sites of erythropoiesis in mammals during development and pathological conditions.
A. During the course of embryonic development in human and mice, the yolk sac is the first source of erythrocytes to provide the fetus with oxygen. Throughout development, fetal liver contributes as the main source of erythropoiesis with the yolk sac regressing. At the time of birth, the bone marrow emerges as the main source of erythropoiesis with the seeding of the hematopoietic stem cells. However, a notable difference is the contribution to erythropoiesis of the spleen in the mouse till 3 months of age. In humans, the sites of erythropoiesis change over time as red blood cell production recedes in the long bones (tibia, femur) and persists in the flat bones (sternum, skull, ribs, pelvis). B. During stress erythropoiesis, the sites of erythropoiesis in the adult human are primarily the flat bones of the skull, sternum, and pelvis with minor contributions from the liver and less so from the spleen. Contributions from the liver and the spleen do not normally occur unless under pathologic disease states. In the mouse system, splenic erythropoiesis is a main feature of stress erythropoiesis with erythroid progenitors in the spleen having being well studied and described. Conversely in the rat, the spleen is a minor contributor of erythropoiesis during times of stress.
Acknowledgments
We apologize for being unable to cite numerous studies due to space restrictions.
This work was supported by NIH (DK26263 to NM) and the Pediatric Cancer Foundation (LB). BMD is a recipient of an American Society of Hematology Physician-Scientist Career Development Award. LB is the recipient of an Allied World St. Baldrick’s Scholar Award.
References
- 1.Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352:1011–23. doi: 10.1056/NEJMra041809. [DOI] [PubMed] [Google Scholar]
- 2.Weiss G. Pathogenesis and treatment of anaemia of chronic disease. Blood Rev. 2002;16:87–96. doi: 10.1054/blre.2002.0193. [DOI] [PubMed] [Google Scholar]
- 3.Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC, Dc W. Prevalence of anemia in persons 65 years and older in the United States : evidence for a high rate of unexplained anemia. Blood. 2004;104:2263–8. doi: 10.1182/blood-2004-05-1812. [DOI] [PubMed] [Google Scholar]
- 4.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;34:17–60. doi: 10.1007/s00134-007-0934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 6.Zhu J, Emerson SG. Hematopoietic cytokines, transcription factors and lineage commitment. Oncogene. 2002;21:3295–313. doi: 10.1038/sj.onc.1205318. [DOI] [PubMed] [Google Scholar]
- 7.Orkin SH, Zon LI. Hematopoiesis: An Evolving Paradigm for Stem Cell Biology. Cell. 2008;132:631–44. doi: 10.1016/j.cell.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siatecka M, Bieker JJ. The multifunctional role of EKLF / KLF1 during erythropoiesis. Blood. 2011;118:2044–54. doi: 10.1182/blood-2011-03-331371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olopade OI, Thangavelu M, Larson Ra, Mick R, Kowal-Vern A, Schumacher HR, et al. Clinical, morphologic, and cytogenetic characteristics of 26 patients with acute erythroblastic leukemia. Blood. 1992;80:2873–82. [PubMed] [Google Scholar]
- 10.Frontelo P, Manwani D, Galdass M, Karsunky H, Lohmann F, Gallagher PG, et al. Novel role for EKLF in megakaryocyte lineage commitment. Blood. 2007;110:3871–80. doi: 10.1182/blood-2007-03-082065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hattangadi SM, Wong P, Zhang L, Flygare J, Lodish HF. From stem cell to red cell: Regulation of erythropoiesis at multiple levels by multiple proteins, RNAs, and chromatin modifications. Blood. 2011;118:6258–68. doi: 10.1182/blood-2011-07-356006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tallack MR, Whitington T, Yuen WS, Kassouf MT, Hughes JR, Taylor S, et al. A global role for KLF1 in erythropoiesis revealed by ChIP-seq in primary erythroid cells. Genome Res. 2010;20:1052–63. doi: 10.1101/gr.106575.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koury ST, Koury MJ, Bondurant MC. Cytoskeletal distribution and function during the maturation and enucleation of mammalian erythroblasts. J Cell Biol. 1989;109:3005–13. doi: 10.1083/jcb.109.6.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skutelsky E, Danon D. An Electron Microscopic Study of Nuclear Elimination From the Late Erythroblast. J Cell Biol. 1967;33:625–35. doi: 10.1083/jcb.33.3.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGrath KE, Kingsley PD, Koniski AD, Porter RL, Bushnell TP, Palis J. Enucleation of primitive erythroid cells generates a transient population of “pyrenocytes” in the mammalian fetus. Blood. 2008;111:2409–17. doi: 10.1182/blood-2007-08-107581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshida H, Kawane K, Koike M, Mori Y, Uchiyama Y, Nagata S. Phosphatidylserine-dependent engulfment by macrophages of nuclei from erythroid precursor cells. Nature. 2005;437:754–8. doi: 10.1038/nature03964. [DOI] [PubMed] [Google Scholar]
- 17.Tavassoli M, Crosby WH. Fate of the Nucleus of the Marrow Erythroblast. Science (80- ) 1973;179:912–3. doi: 10.1126/science.179.4076.912. [DOI] [PubMed] [Google Scholar]
- 18.Leyen K, Van Duvoisin RM, Engelhardt H, Wiedmann M. A function for lipoxygenase in programmed organelle degradation. Nature. 1998;395:392–5. doi: 10.1038/26500. [DOI] [PubMed] [Google Scholar]
- 19.Pan BT, Johnstone RM. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: selective externalization of the receptor. Cell. 1983;33:967–78. doi: 10.1016/0092-8674(83)90040-5. [DOI] [PubMed] [Google Scholar]
- 20.Ney Pa. Normal and disordered reticulocyte maturation. Curr Opin Hematol. 2011;18:152–7. doi: 10.1097/MOH.0b013e328345213e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu J, Guo X, Mohandas N, Chasis Ja, An X. Membrane remodeling during reticulocyte maturation. Blood. 2010;115:2021–7. doi: 10.1182/blood-2009-08-241182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blanc L, Vidal M. Reticulocyte membrane remodeling: contribution of the exosome pathway. Curr Opin Hematol. 2010;17:177–83. doi: 10.1097/MOH.0b013e328337b4e3. [DOI] [PubMed] [Google Scholar]
- 23.Lacombe C, Da Silva JL, Bruneval P, Fournier JG, Wendling F, Casadevall N, et al. Peritubular cells are the site of erythropoietin synthesis in the murine hypoxic kidney. J Clin Invest. 1988;81:620–3. doi: 10.1172/JCI113363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Semenza GL, Koury ST, Nejfelt MK, Gearhart JD, Antonarakis SE. Cell-type-specific and hypoxia-inducible expression of the human erythropoietin gene in transgenic mice. Proc Natl Acad Sci U S A. 1991;88:8725–9. doi: 10.1073/pnas.88.19.8725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kapitsinou PP, Liu Q, Unger TL, Rha J, Davidoff O, Keith B, et al. Hepatic HIF-2 regulates erythropoietic responses to hypoxia in renal anemia. Blood. 2010;116:3039–48. doi: 10.1182/blood-2010-02-270322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scortegagna M, Morris Ma, Oktay Y, Bennett M, Garcia Ja. The HIF family member EPAS1 / HIF-2a is required for normal hematopoiesis in mice. Blood. 2003;102:1634–40. doi: 10.1182/blood-2003-02-0448. [DOI] [PubMed] [Google Scholar]
- 27.Gregory CJ. Erythropoietin sensitivity as a differentiation marker in the hemopoietic system: studies of three erythropoietic colony responses in culture. J Cell Physiol. 1976;89:289–301. doi: 10.1002/jcp.1040890212. [DOI] [PubMed] [Google Scholar]
- 28.Koury MJ, Bondurant MC. Erythropoietin retards DNA breakdown and prevents programmed death in erythroid progenitor cells. Science. 1990;248:378–81. doi: 10.1126/science.2326648. [DOI] [PubMed] [Google Scholar]
- 29.Richmond TD, Chohan M, Barber DL. Turning cells red: Signal transduction mediated by erythropoietin. Trends Cell Biol. 2005;15:146–55. doi: 10.1016/j.tcb.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 30.Rubiolo C, Piazzolla D, Meissl K, Beug H, Huber JC, Kolbus A, et al. Abalance between Raf-1 and Fas expression sets the pace of erythroid differentiation. Blood. 2006;108:152–9. doi: 10.1182/blood-2005-09-3866. [DOI] [PubMed] [Google Scholar]
- 31.BESSIS M. Erythroblastic island, functional unity of bone marrow. Rev Hematol. 1958;13:8–11. [PubMed] [Google Scholar]
- 32.Mohandas N, Prenant M. Three-dimensional model of bone marrow. Blood. 1978;51:633–43. [PubMed] [Google Scholar]
- 33.Dzierzak E, Philipsen S. Erythropoiesis : Development and Differentiation. Cold Spring Harb Perspect Med. 2013;3:1–16. doi: 10.1101/cshperspect.a011601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chasis JA, Mohandas N. Erythroblastic islands: Niches for erythropoiesis. Blood. 2008;112:470–8. doi: 10.1182/blood-2008-03-077883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanspal M, Smockova Y, Uong Q. Molecular identification and functional characterization of a novel protein that mediates the attachment of erythroblasts to macrophages. Blood. 1998;92:2940–50. [PubMed] [Google Scholar]
- 36.Rhodes MM, Kopsombut P, Bondurant MC, Price JO, Koury MJ. Adherence to macrophages in erythroblastic islands enhances erythroblast proliferation and increases erythrocyte production by a different mechanism than erythropoietin. Blood. 2008;111:1700–8. doi: 10.1182/blood-2007-06-098178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hanspal M, Hanspal JS. The association of erythroblasts with macrophages promotes erythroid proliferation and maturation: a 30-kD heparin-binding protein is involved in this contact. Blood. 1994;84:3494–504. [PubMed] [Google Scholar]
- 38.Soni S, Bala S, Gwynn B, Sahr KE, Peters LL, Hanspal M. Absence of erythroblast macrophage protein (Emp) leads to failure of erythroblast nuclear extrusion. J Biol Chem. 2006;281:20181–9. doi: 10.1074/jbc.M603226200. [DOI] [PubMed] [Google Scholar]
- 39.Sadahira Y, Yoshino T, Monobe Y. Very late activation antigen 4-vascular cell adhesion molecule 1 interaction is involved in the formation of erythroblastic islands. J Exp Med. 1995;181:411–5. doi: 10.1084/jem.181.1.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee G, Lo A, Short Sa, Mankelow TJ, Spring F, Parsons SF, et al. Targeted gene deletion demonstrates that the cell adhesion molecule ICAM-4 is critical for erythroblastic island formation. Blood. 2006;108:2064–71. doi: 10.1182/blood-2006-03-006759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Jong JP, Voerman JS, van der Sluijs-Gelling AJ, Willemsen R, Ploemacher RE. A monoclonal antibody (ER-HR3) against murine macrophages. I. Ontogeny, distribution and enzyme histochemical characterization of ER-HR3-positive cells. Cell Tissue Res. 1994;275:567–76. doi: 10.1007/BF00318825. [DOI] [PubMed] [Google Scholar]
- 42.Morris L, Crocker PR, Fraser I, Hill M, Gordon S. Expression of a divalent cation-dependent erythroblast adhesion receptor by stromal macrophages from murine bone marrow. J Cell Sci. 1991;99 ( Pt 1):141–7. doi: 10.1242/jcs.99.1.141. [DOI] [PubMed] [Google Scholar]
- 43.Fabriek BO, Polfliet MMJ, Vloet RPM, Van Der Schors RC, Ligtenberg AJM, Weaver LK, et al. The macrophage CD163 surface glycoprotein is an erythroblast adhesion receptor. Blood. 2007;109:5223–9. doi: 10.1182/blood-2006-08-036467. [DOI] [PubMed] [Google Scholar]
- 44.Skutelsky E, Danon D. On the expulsion of the erythroid nucleus and its phagocytosis. Anat Rec. 1972;173:123–6. doi: 10.1002/ar.1091730111. [DOI] [PubMed] [Google Scholar]
- 45.Kawane K, Fukuyama H, Kondoh G, Takeda J, Ohsawa Y, Uchiyama Y, et al. Requirement of DNase II for definitive erythropoiesis in the mouse fetal liver. Science. 2001;292:1546–9. doi: 10.1126/science.292.5521.1546. [DOI] [PubMed] [Google Scholar]
- 46.Lee JCM, Gimm JA, Lo AJ, Koury MJ, Krauss SW, Mohandas N, et al. Mechanism of protein sorting during erythroblast enucleation: Role of cytoskeletal connectivity. Blood. 2004;103:1912–9. doi: 10.1182/blood-2003-03-0928. [DOI] [PubMed] [Google Scholar]
- 47.Toda S, Segawa K, Nagata S. MerTK-mediated engulfment of pyrenocytes by central macrophages in erythroblastic islands. Blood. 2014;123:3963–71. doi: 10.1182/blood-2014-01-547976. [DOI] [PubMed] [Google Scholar]
- 48.Tallack MR, Magor GW, Dartigues B, Sun L, Huang S, Fittock JM, et al. Novel roles for KLF1 in erythropoiesis revealed by mRNA-seq. Genome Res. 2012;22:2385–98. doi: 10.1101/gr.135707.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Porcu S, Manchinu MF, Marongiu MF, Sogos V, Poddie D, Asunis I, et al. Klf1 Affects DNase II-Alpha Expression in the Central Macrophage of a Fetal Liver Erythroblastic Island: a Non-Cell-Autonomous Role in Definitive Erythropoiesis. Mol Cell Biol. 2011;31:4144–54. doi: 10.1128/MCB.05532-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sui Z, Nowak RB, Bacconi A, Kim NE, Liu H, Li J, et al. Tropomodulin3-null mice are embryonic lethal with anemia due to impaired erythroid terminal differentiation in the fetal liver. Blood. 2014;123:758–67. doi: 10.1182/blood-2013-03-492710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee SH. Isolation and immunocytochemical characterization of human bone marrow stromal macrophages in hemopoietic clusters. J Exp Med [Internet] 1988;168:1193–8. doi: 10.1084/jem.168.3.1193. Available from: http://www.jem.org/cgi/doi/10.1084/jem.168.3.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McKnight AJ, Macfarlane AJ, Dri P, Turley L, Willis AC, Gordon S. Molecular cloning of F4/80, a murine macrophage-restricted cell surface glycoprotein with homology to the G-protein-linked transmembrane 7 hormone receptor family. J Biol Chem. 1996;271:486–9. doi: 10.1074/jbc.271.1.486. [DOI] [PubMed] [Google Scholar]
- 53.Sadahira Y, Yasuda T, Kimoto T. Regulation of Forssman antigen expression during maturation of mouse stromal macrophages in haematopoietic foci. Immunology. 1991;73:498–504. [PMC free article] [PubMed] [Google Scholar]
- 54.Jacobsen RN, Perkins AC, Levesque J-P. Macrophages and regulation of erythropoiesis. Curr Opin Hematol [Internet] 2015;22:1. doi: 10.1097/MOH.0000000000000131. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00062752-900000000-99569. [DOI] [PubMed] [Google Scholar]
- 55.Hartnell A, Steel J, Turley H, Jones M, Jackson DG, Crocker PR. Characterization of human sialoadhesin, a sialic acid binding receptor expressed by resident and inflammatory macrophage populations. Blood. 2001;97:288–96. doi: 10.1182/blood.v97.1.288. [DOI] [PubMed] [Google Scholar]
- 56.Chow A, Huggins M, Ahmed J, Hashimoto D, Lucas D, Kunisaki Y, et al. CD169+ macrophages provide a niche promoting erythropoiesis under homeostasis and stress. Nat Med [Internet] Nature Publishing Group. 2013;19:429–36. doi: 10.1038/nm.3057. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3983996&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Means RT. Recent developments in the anemia of chronic disease. Curr Hematol Rep. 2003;2:116–21. [PubMed] [Google Scholar]
- 58.Koury MJ. Blood Rev. Vol. 28. Elsevier B.V; 2014. Abnormal erythropoiesis and the pathophysiology of chronic anemia; pp. 49–66. [Internet] Available from: http://dx.doi.org/10.1016/j.blre.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 59.Baer AN, Dessypris EN, Goldwasser E, Krantz SB. Blunted erythropoietin response to anaemia in rheumatoid arthritis. Br J Haematol. 1987;66:559–64. doi: 10.1111/j.1365-2141.1987.tb01344.x. [DOI] [PubMed] [Google Scholar]
- 60.Hochberg MC, Arnold CM, Hogans BB, Spivak JL. Serum immunoreactive erythropoietin in rheumatoid arthritis: impaired response to anemia. Arthritis Rheum. 1988;31:1318–21. doi: 10.1002/art.1780311016. [DOI] [PubMed] [Google Scholar]
- 61.Ganz T. Hepcidin and iron regulation. Blood. 2014;117:4425–33. doi: 10.1182/blood-2011-01-258467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miller CB, Jones RJ, Piantadosi S, Abeloff MD, Spivak JL. Decreased erythropoietin response in patients with the anemia of cancer. N Engl J Med. 1990;322:1689–92. doi: 10.1056/NEJM199006143222401. [DOI] [PubMed] [Google Scholar]
- 63.Macdougall IC, Cooper AC. Erythropoietin resistance: the role of inflammation and pro-inflammatory cytokines. Nephrol Dial Transplant. 2002;17 (Suppl 1):39–43. doi: 10.1093/ndt/17.suppl_11.39. [DOI] [PubMed] [Google Scholar]
- 64.Bárány P. Inflammation, serum C-reactive protein, and erythropoietin resistance. Nephrol Dial Transplant. 2001:224–7. doi: 10.1093/ndt/16.2.224. [DOI] [PubMed] [Google Scholar]
- 65.Ganz T. Anemia of Chronic Disease. In: Lichtman M, Kipps T, Seligsohn U, Kaushansky K, Prchal J, editors. Williams Hematol. 8. New York, NY: McGraw-Hill; 2010. [Google Scholar]
- 66.Imagawa S, Nakano Y, Obara N, Suzuki N, Doi T, Kodama T, et al. A GATA-specific inhibitor (K-7174) rescues anemia induced by IL-1beta, TNF-alpha, or L-NMMA. FASEB J. 2003;17:1742–4. doi: 10.1096/fj.02-1134fje. [DOI] [PubMed] [Google Scholar]
- 67.Means RT, Krantz SB. Inhibition of human erythroid colony-forming units by gamma interferon can be corrected by recombinant human erythropoietin. Blood. 1991;78:2564–7. [PubMed] [Google Scholar]
- 68.Jelkmann W. Proinflammatory cytokines lowering erythropoietin production. J Interferon Cytokine Res. 1998;18:555–9. doi: 10.1089/jir.1998.18.555. [DOI] [PubMed] [Google Scholar]
- 69.Taniguchi S, Dai CH, Price JO, Krantz SB. Interferon gamma downregulates stem cell factor and erythropoietin receptors but not insulin-like growth factor-I receptors in human erythroid colony-forming cells. Blood. 1997;90:2244–52. [PubMed] [Google Scholar]
- 70.Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science (80- ) 2004;306:2090–3. doi: 10.1126/science.1104742. [DOI] [PubMed] [Google Scholar]
- 71.Pietrangelo A. Physiology of iron transport and the hemochromatosis gene. Am J Physiol Gastrointest Liver Physiol. 2002;282:G403–14. doi: 10.1152/ajpgi.00404.2001. [DOI] [PubMed] [Google Scholar]
- 72.Nicolas G, Chauvet C, Viatte L, Danan JL, Bigard X, Devaux I, et al. The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J Clin Invest. 2002;110:1037–44. doi: 10.1172/JCI15686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pak M, Lopez MA, Gabayan V, Ganz T, Rivera S. Suppression of hepcidin during anemia requires erythropoietic activity. Blood. 2006;108:3730–5. doi: 10.1182/blood-2006-06-028787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kautz L, Jung G, Valore EV, Rivella S, Nemeth E, Ganz T. Identification of erythroferrone as an erythroid regulator of iron metabolism. Nat Genet [Internet] Nature Publishing Group. 2014;46:678–84. doi: 10.1038/ng.2996. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24880340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kautz L, Jung G, Du X, Gabayan V, Chapman J, Nasoff M, et al. Erythroferrone contributes to hepcidin suppression and iron overload in a mouse model of -thalassemia. Blood. 2015 doi: 10.1182/blood-2015-07-658419. [Internet] Available from: http://www.bloodjournal.org/cgi/doi/10.1182/blood-2015-07-658419. [DOI] [PMC free article] [PubMed]
- 76.Ludwiczek S, Aigner E, Theurl I, Weiss G. Cytokine-mediated regulation of iron transport in human monocytic cells. Blood. 2003;101:4148–54. doi: 10.1182/blood-2002-08-2459. [DOI] [PubMed] [Google Scholar]
- 77.Wang CQ, Udupa KB, Lipschitz DA. Interferon-gamma exerts its negative regulatory effect primarily the earliest stages of murine erythroid progenitor cell development. J Cell Physiol. 1995;162:134–8. doi: 10.1002/jcp.1041620116. [DOI] [PubMed] [Google Scholar]
- 78.Libregts SF, Gutiérrez L, De Bruin AM, Wensveen FM, Papadopoulos P, Van Ijcken W, et al. Chronic IFN-γ production in mice induces anemia by reducing erythrocyte life span and inhibiting erythropoiesis through an IRF-1/PU axis. Blood. 2011;118:2578–88. doi: 10.1182/blood-2010-10-315218. [DOI] [PubMed] [Google Scholar]
- 79.Dai CH, Price JO, Brunner T, Krantz SB. Fas ligand is present in human erythroid colony-forming cells and interacts with Fas induced by interferon gamma to produce erythroid cell apoptosis. Blood. 1998;91:1235–42. [PubMed] [Google Scholar]
- 80.Felli N, Pedini F, Zeuner A, Petrucci E, Testa U, Conticello C, et al. Multiple members of the TNF superfamily contribute to IFN-gamma-mediated inhibition of erythropoiesis. J Immunol. 2005;175:1464–72. doi: 10.4049/jimmunol.175.3.1464. [DOI] [PubMed] [Google Scholar]
- 81.Moldawer LL, Marano MA, Wei H, Fong Y, Silen ML, Kuo G, et al. Cachectin/tumor necrosis factor-alpha alters red blood cell kinetics and induces anemia in vivo. FASEB J. 1989;3:1637–43. doi: 10.1096/fasebj.3.5.2784116. [DOI] [PubMed] [Google Scholar]
- 82.Jongen-Lavrencic M, Peeters HR, Wognum A, Vreugdenhil G, Breedveld FC, Swaak AJ. Elevated levels of inflammatory cytokines in bone marrow of patients with rheumatoid arthritis and anemia of chronic disease. J Rheumatol. 1997;24:1504–9. [PubMed] [Google Scholar]
- 83.Katevas P, Andonopoulos AP, Kourakli-Symeonidis A, Manopoulou E, Lafi T, Makri M, et al. Peripheral blood mononuclear cells from patients with rheumatoid arthritis suppress erythropoiesis in vitro via the production of tumor necrosis factor alpha. Eur J Haematol. 1994;53:26–30. doi: 10.1111/j.1600-0609.1994.tb00175.x. [DOI] [PubMed] [Google Scholar]
- 84.Voulgari PV, Kolios G, Papadopoulos GK, Katsaraki A, Seferiadis K, Drosos AA. Role of cytokines in the pathogenesis of anemia of chronic disease in rheumatoid arthritis. Clin Immunol. 1999;92:153–60. doi: 10.1006/clim.1999.4736. [DOI] [PubMed] [Google Scholar]
- 85.Vreugdenhil G, Löwenberg B, Van Eijk HG, Swaak AJ. Tumor necrosis factor alpha is associated with disease activity and the degree of anemia in patients with rheumatoid arthritis. Eur J Clin Invest. 1992;22:488–93. doi: 10.1111/j.1365-2362.1992.tb01495.x. [DOI] [PubMed] [Google Scholar]
- 86.Papadaki Ha, Kritikos HD, Valatas V, Boumpas DT, Eliopoulos GD. Anemia of chronic disease in rheumatoid arthritis is associated with increased apoptosis of bone marrow erythroid cells: improvement following anti-tumor necrosis factor-alpha antibody therapy. Blood. 2002;100:474–82. doi: 10.1182/blood-2002-01-0136. [DOI] [PubMed] [Google Scholar]
- 87.Heuser M, Ganser A. Recombinant human erythropoietin in the treatment of nonrenal anemia. Ann Hematol. 2006:69–78. doi: 10.1007/s00277-005-1086-5. [DOI] [PubMed] [Google Scholar]
- 88.Ramos P, Casu C, Gardenghi S, Breda L, Crielaard BJ, Guy E, et al. Macrophages support pathological erythropoiesis in polycythemia vera and β-thalassemia. Nat Med [Internet] Nature Publishing Group. 2013;19:437–45. doi: 10.1038/nm.3126. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23502961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Angelillo-Scherrer A, Burnier L, Lambrechts D, Fish RJ, Tjwa M, Plaisance S, et al. Role of Gas6 in erythropoiesis and anemia in mice. J Clin Invest. 2008;118:583–96. doi: 10.1172/JCI30375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sawada K, Krantz SB, Dessypris EN, Koury ST, Sawyer ST. Human colony-forming units-erythroid do not require accessory cells, but do require direct interaction with insulin-like growth factor I and/or insulin for erythroid development. J Clin Invest. 1989;83:1701–9. doi: 10.1172/JCI114070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Means RT. Hepcidin and cytokines in anaemia. Hematology. 2004;9:357–62. doi: 10.1080/10245330400018540. [DOI] [PubMed] [Google Scholar]
- 92.De Maria R, Zeuner A, Eramo A, Domenichelli C, Bonci D, Grignani F, et al. Negative regulation of erythropoiesis by caspase-mediated cleavage of GATA-1. Nature. 1999;401:489–93. doi: 10.1038/46809. [DOI] [PubMed] [Google Scholar]
- 93.Dai C, Chung IJ, Jiang S, Price JO, Krantz SB. Reduction of cell cycle progression in human erythroid progenitor cells treated with tumour necrosis factor alpha occurs with reduced CDK6 and is partially reversed by CDK6 transduction. Br J Haematol. 2003;121:919–27. doi: 10.1046/j.1365-2141.2003.04367.x. [DOI] [PubMed] [Google Scholar]
- 94.Flores-Figueroa E, Gutiérrez-Espíndola G, Montesinos JJ, Arana-Trejo RM, Mayani H. In vitro characterization of hematopoietic microenvironment cells from patients with myelodysplastic syndrome. Leuk Res. 2002;26:677–86. doi: 10.1016/s0145-2126(01)00193-x. [DOI] [PubMed] [Google Scholar]
- 95.Maddala R, Reddy VN, Epstein DL, Rao V. Growth factor induced activation of Rho and Rac GTPases and actin cytoskeletal reorganization in human lens epithelial cells. Mol Vis. 2003;9:329–36. [PubMed] [Google Scholar]
- 96.Zamai L, Secchiero P, Pierpaoli S, Bassini A, Papa S, Alnemri ES, et al. TNF-related apoptosis-inducing ligand (TRAIL) as a negative regulator of normal human erythropoiesis. Blood. 2000;95:3716–24. [PubMed] [Google Scholar]
- 97.Secchiero P, Melloni E, Heikinheimo M, Mannisto S, Di Pietro R, Iacone A, et al. TRAIL regulates normal erythroid maturation through an ERK-dependent pathway. Blood. 2004;103:517–22. doi: 10.1182/blood-2003-06-2137. [DOI] [PubMed] [Google Scholar]
- 98.Martinez FO, Helming L, Gordon S. Alternative activation of macrophages: an immunologic functional perspective. Annu Rev Immunol. 2009;27:451–83. doi: 10.1146/annurev.immunol.021908.132532. [DOI] [PubMed] [Google Scholar]
- 99.Sica A, Mantovani A. Macrophage plasticity and polarization: In vivo veritas. J Clin Invest. 2012:787–95. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Recalcati S, Locati M, Marini A, Santambrogio P, Zaninotto F, De Pizzol M, et al. Differential regulation of iron homeostasis during human macrophage polarized activation. Eur J Immunol. 2010;40:824–35. doi: 10.1002/eji.200939889. [DOI] [PubMed] [Google Scholar]
- 101.Gammella E, Buratti P, Cairo G, Recalcati S. Macrophages: central regulators of iron balance. Metallomics [Internet] 2014;6:1336–42. doi: 10.1039/c4mt00104d. Available from: http://pubs.rsc.org/en/content/articlelanding/2014/mt/c4mt00104d\nhttp://pubs.rsc.org/en/Content/ArticleLanding/2014/MT/C4MT00104D\nhttp://pubs.rsc.org/en/content/articlepdf/2014/mt/c4mt00104d. [DOI] [PubMed] [Google Scholar]
- 102.Vallelian F, Schaer CA, Kaempfer T, Gehrig P, Duerst E, Schoedon G, et al. Glucocorticoid treatment skews human monocyte differentiation into a hemoglobin-clearance phenotype with enhanced heme-iron recycling and antioxidant capacity. Blood. 2010;116:5347–56. doi: 10.1182/blood-2010-04-277319. [DOI] [PubMed] [Google Scholar]
- 103.Iavarone A, King ER, Dai X-M, Leone G, Stanley ER, Lasorella A. Retinoblastoma promotes definitive erythropoiesis by repressing Id2 in fetal liver macrophages. Nature. 2004;432:1040–5. doi: 10.1038/nature03068. [DOI] [PubMed] [Google Scholar]
- 104.Clarke AR, Maandag ER, van Roon M, van der Lugt NM, van der Valk M, Hooper ML, et al. Requirement for a functional Rb-1 gene in murine development. Nature. 1992;359:328–30. doi: 10.1038/359328a0. [DOI] [PubMed] [Google Scholar]
- 105.Clark AJ, Doyle KM, Humbert PO. Cell-intrinsic requirement for pRb in erythropoiesis. Blood. 2004;104:1324–6. doi: 10.1182/blood-2004-02-0618. [DOI] [PubMed] [Google Scholar]
- 106.Sankaran VG, Orkin SH, Walkley CR. Rb intrinsically promotes erythropoiesis by coupling cell cycle exit with mitochondrial biogenesis. Genes Dev. 2008;22:463–75. doi: 10.1101/gad.1627208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kataoka K, Noda M, Nishizawa M. Maf nuclear oncoprotein recognizes sequences related to an AP-1 site and forms heterodimers with both Fos and Jun. Mol Cell Biol. 1994;14:700–12. doi: 10.1128/mcb.14.1.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yoshida T, Ohkumo T, Ishibashi S, Yasuda K. The 5′-AT-rich half-site of Maf recognition element: A functional target for bZIP transcription factor Maf. Nucleic Acids Res. 2005;33:3465–78. doi: 10.1093/nar/gki653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kusakabe M, Hasegawa K, Hamada M, Nakamura M, Ohsumi T, Suzuki H, et al. c-Maf plays a crucial role for the definitive erythropoiesis that accompanies erythroblastic island formation in the fetal liver. Blood. 2011;118:1374–85. doi: 10.1182/blood-2010-08-300400. [DOI] [PubMed] [Google Scholar]
- 110.Yien Y, Bieker JJ. EKLF/KLF1: a tissue-restricted integrator of transcriptional control, chromatin remodeling, and lineage determination. Mol Cell Biol. 2013;33:4–13. doi: 10.1128/MCB.01058-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xue L, Galdass M, Gnanapragasam MN, Manwani D, Bieker JJ. Extrinsic and intrinsic control by EKLF (KLF1) within a specialized erythroid niche. Development [Internet] 2014;141:2245–54. doi: 10.1242/dev.103960. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24866116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mebius RE, Kraal G. Structure and function of the spleen. Nat Rev Immunol. 2005;5:606–16. doi: 10.1038/nri1669. [DOI] [PubMed] [Google Scholar]
- 113.Piomelli S, Seaman C. Mechanism of red blood cell aging: Relationship of cell density and cell age. Am J Hematol. 1993:46–52. doi: 10.1002/ajh.2830420110. [DOI] [PubMed] [Google Scholar]
- 114.Lutz HU. Innate immune and non-immune mediators of erythrocyte clearance. Cell Mol Biol (Noisy-le-grand) 2004:107–16. [PubMed] [Google Scholar]
- 115.Fernandez-Boyanapalli RF, Frasch SC, McPhillips K, Vandivier RW, Harry BL, Riches DWH, et al. Impaired apoptotic cell clearance in CGD due to altered macrophage programming is reversed by phosphatidylserine-dependent production of IL-4. Blood. 2009;113:2047–55. doi: 10.1182/blood-2008-05-160564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Oldenborg PA, Zheleznyak A, Fang YF, Lagenaur CF, Gresham HD, Lindberg FP. Role of CD47 as a marker of self on red blood cells. Science. 2000;288:2051–4. doi: 10.1126/science.288.5473.2051. [DOI] [PubMed] [Google Scholar]
- 117.Melhorn MI, Brodsky AS, Estanislau J, Khoory JA, Illigens B, Hamachi I, et al. CR1-mediated ATP release by Human red blood cells promotes CR1 clustering and modulates the immune transfer process. J Biol Chem. 2013;288:31139–53. doi: 10.1074/jbc.M113.486035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.White C, Yuan X, Schmidt PJ, Bresciani E, Samuel TK, Campagna D, et al. HRG1 Is Essential for Heme Transport from the Phagolysosome of Macrophages during Erythrophagocytosis. Cell Metab [Internet] 2013;17:261–70. doi: 10.1016/j.cmet.2013.01.005. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1550413113000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Soe-Lin S, Sheftel AD, Wasyluk B, Ponka P. Nramp1 equips macrophages for efficient iron recycling. Exp Hematol. 2008;36:929–37. doi: 10.1016/j.exphem.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 120.Bessis MC, Breton-Gorius J. Iron metabolism in the bone marrow as seen by electron microscopy: a critical review. Blood. 1962;19:635–63. [PubMed] [Google Scholar]
- 121.Leimberg MJ, Prus E, Konijn AM, Fibach E. Macrophages function as a ferritin iron source for cultured human erythroid precursors. J Cell Biochem. 2008;103:1211–8. doi: 10.1002/jcb.21499. [DOI] [PubMed] [Google Scholar]
- 122.Baron MH, Isern J, Fraser ST. The embryonic origins of erythropoiesis in mammals. Blood. 2012;119:4828–37. doi: 10.1182/blood-2012-01-153486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bradley A. Mining the mouse genome. Nature. 2002;420:512–4. doi: 10.1038/420512a. [DOI] [PubMed] [Google Scholar]
- 124.Mikkola HKA, Orkin SH. Gene targeting and transgenic strategies for the analysis of hematopoietic development in the mouse. Methods Mol Med. 2005;105:3–22. doi: 10.1385/1-59259-826-9:003. [DOI] [PubMed] [Google Scholar]
- 125.Paigen K. One hundred years of mouse genetics: an intellectual history II. The molecular revolution (1981–2002) Genetics. 2003;163:1227–35. doi: 10.1093/genetics/163.4.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Palis J. Ontogeny of erythropoiesis. Curr Opin Hematol. 2008;15:155–61. doi: 10.1097/MOH.0b013e3282f97ae1. [DOI] [PubMed] [Google Scholar]
- 127.Tavian M, Péault B. Embryonic development of the human hematopoietic system. Int J Dev Biol. 2005;49:243–50. doi: 10.1387/ijdb.041957mt. [DOI] [PubMed] [Google Scholar]
- 128.Tober J, Koniski A, McGrath KE, Vemishetti R, Emerson R, De Mesy-Bentley KKL, et al. The megakaryocyte lineage originates from hemangioblast precursors and is an integral component both of primitive and of definitive hematopoiesis. Blood. 2007;109:1433–41. doi: 10.1182/blood-2006-06-031898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Palis J, Robertson S, Kennedy M, Wall C, Keller G. Development of erythroid and myeloid progenitors in the yolk sac and embryo proper of the mouse. Development. 1999;126:5073–84. doi: 10.1242/dev.126.22.5073. [DOI] [PubMed] [Google Scholar]
- 130.Isern J, He Z, Fraser ST, Nowotschin S, Ferrer-Vaquer A, Moore R, et al. Single-lineage transcriptome analysis reveals key regulatory pathways in primitive erythroid progenitors in the mouse embryo. Blood. 2011;117:4924–34. doi: 10.1182/blood-2010-10-313676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fraser ST, Isern J, Baron MH. Maturation and enucleation of primitive erythroblasts during mouse embryogenesis is accompanied by changes in cell-surface antigen expression. Blood. 2007;109:343–52. doi: 10.1182/blood-2006-03-006569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kingsley PD, Malik J, Fantauzzo KA, Palis J. Yolk sac-derived primitive erythroblasts enucleate during mammalian embryogenesis. Blood. 2004;104:19–25. doi: 10.1182/blood-2003-12-4162. [DOI] [PubMed] [Google Scholar]
- 133.Kumaravelu P, Hook L, Morrison AM, Ure J, Zhao S, Zuyev S, et al. Quantitative developmental anatomy of definitive haematopoietic stem cells/long-term repopulating units (HSC/RUs): role of the aorta-gonad-mesonephros (AGM) region and the yolk sac in colonisation of the mouse embryonic liver. Development. 2002;129:4891–9. doi: 10.1242/dev.129.21.4891. [DOI] [PubMed] [Google Scholar]
- 134.Cumano A, Godin I. The Ontogeny of the Hematopoietic System. Annu Rev Immunol. 2007;25:745–85. doi: 10.1146/annurev.immunol.25.022106.141538. [DOI] [PubMed] [Google Scholar]
- 135.McGrath KE, Frame JM, Fromm GJ, Koniski AD, Kingsley PD, Little J, et al. A transient definitive erythroid lineage with unique regulation of the Beta-globin locus in the mammalian embryo. Blood. 2011;117:4600–8. doi: 10.1182/blood-2010-12-325357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Allen TD, Dexter TM. Ultrastructural aspects of erythropoietic differentiation in long-term bone marrow culture. Differentiation. 1982;21:86–94. doi: 10.1111/j.1432-0436.1982.tb01201.x. [DOI] [PubMed] [Google Scholar]
- 137.Brodsky I, Dennis LH, Kahn SB, Brady LW. Normal mouse erythropoiesis I. The role of the spleen in mouse erythropoiesis. Cancer Res. 1966;26:198–201. [PubMed] [Google Scholar]
- 138.Vacek A, Bartonickova A, Tkadlecek L. Age dependence of the number of the stem cells in haemopoietic tissues of rats. Cell Tissue Kinet. 1976;9:1–8. doi: 10.1111/j.1365-2184.1976.tb01248.x. [DOI] [PubMed] [Google Scholar]
- 139.GARCIA JF. Changes in blood, plasma and red cell volume in the male rat, as a function of age. Am J Physiol. 1957;190:19–24. doi: 10.1152/ajplegacy.1957.190.1.19. [DOI] [PubMed] [Google Scholar]
- 140.Seifert MF, Marks SC. The regulation of hemopoiesis in the spleen. Experientia. 1985;41:192–9. doi: 10.1007/BF02002613. [DOI] [PubMed] [Google Scholar]
- 141.Socolovsky M. Molecular insights into stress erythropoiesis. Curr Opin Hematol. 2007;14:215–24. doi: 10.1097/MOH.0b013e3280de2bf1. [DOI] [PubMed] [Google Scholar]
- 142.Lenox LE, Perry JM, Paulson RF. BMP4 and Madh5 regulate the erythroid response to acute anemia. Blood. 2005;105:2741–8. doi: 10.1182/blood-2004-02-0703. [DOI] [PubMed] [Google Scholar]
- 143.Paulson RF, Shi L, Wu D-C. Stress erythropoiesis: new signals and new stress progenitor cells. Curr Opin Hematol. 2011;18:139–45. doi: 10.1097/MOH.0b013e32834521c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Maekawa S, Iemura H, Kato T. Enhanced erythropoiesis in mice exposed to low environmental temperature. J Exp Biol [Internet] 2013;216:901–8. doi: 10.1242/jeb.076760. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23155089. [DOI] [PubMed] [Google Scholar]
- 145.Bauer A, Tronche F, Wessely O, Kellendonk C, Reichardt HM, Steinlein P, et al. The glucocorticoid receptor is required for stress erythropoiesis. Genes Dev. 1999;13:2996–3002. doi: 10.1101/gad.13.22.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Broudy VC, Lin NL, Priestley GV, Nocka K, Wolf NS. Interaction of stem cell factor and its receptor c-kit mediates lodgment and acute expansion of hematopoietic cells in the murine spleen. Blood. 1996;88:75–81. [PubMed] [Google Scholar]
- 147.Millot S, Andrieu V, Letteron P, Lyoumi S, Hurtado-Nedelec M, Karim Z, et al. Erythropoietin stimulates spleen BMP4-dependent stress erythropoiesis and partially corrects anemia in a Mouse model of generalized inflammation. Blood. 2010;116:6072–81. doi: 10.1182/blood-2010-04-281840. [DOI] [PubMed] [Google Scholar]
- 148.Perry JM, Harandi OF, Paulson RF. BMP4, SCF, and hypoxia cooperatively regulate the expansion of murine stress erythroid progenitors. Blood. 2007;109:4494–502. doi: 10.1182/blood-2006-04-016154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lenox LE, Shi L, Hegde S, Paulson RF. Extramedullary erythropoiesis in the adult liver requires BMP-4/Smad5-dependent signaling. Exp Hematol. 2009;37:549–58. doi: 10.1016/j.exphem.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ploemacher RE, van Soest PL. Morphological investigation on phenylhydrazine-induced erythropoiesis in the adult mouse liver. Cell Tissue Res. 1977;178:435–61. doi: 10.1007/BF00219567. [DOI] [PubMed] [Google Scholar]
- 151.Ploemacher RE, van Soest PL, Vos O. Kinetics of erythropoiesis in the liver induced in adult mice by phenylhydrazine. Scand J Haematol. 1977;19:424–34. doi: 10.1111/j.1600-0609.1977.tb01497.x. [DOI] [PubMed] [Google Scholar]
- 152.Nagai, Hirofumi, Chatani, Fumio, Sasaki, Satoshi, Miyajima H. Negligible contribution of splenic erythropoiesis to recovery from anemia in rats. J Toxicol Pathol. 1993;6:241–9. [Google Scholar]
- 153.Migliaccio AR, Whitsett C, Papayannopoulou T, Sadelain M. The potential of stem cells as an in vitro source of red blood cells for transfusion. Cell Stem Cell [Internet] Elsevier Inc. 2012;10:115–9. doi: 10.1016/j.stem.2012.01.001. Available from: http://dx.doi.org/10.1016/j.stem.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Douay L, Andreu G. Ex vivo Production of Human Red Blood Cells From Hematopoietic Stem Cells: What Is the Future in Transfusion? Transfus. Med Rev. 2007;21:91–100. doi: 10.1016/j.tmrv.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 155.Giarratana M-C, Kobari L, Lapillonne H, Chalmers D, Kiger L, Cynober T, et al. Ex vivo generation of fully mature human red blood cells from hematopoietic stem cells. Nat Biotechnol. 2005;23:69–74. doi: 10.1038/nbt1047. [DOI] [PubMed] [Google Scholar]