Abstract
Corneal wound healing is a complex process involving cell death, migration, proliferation, differentiation, and extracellular matrix remodeling. Many similarities are observed in the healing processes of corneal epithelial, stromal and endothelial cells, as well as cell-specific differences. Corneal epithelial healing largely depends on limbal stem cells and remodeling of the basement membrane. During stromal healing, keratocytes get transformed to motile and contractile myofibroblasts largely due to activation of transforming growth factor-β system. Endothelial cells heal mostly by migration and spreading, with cell proliferation playing a secondary role. In the last decade, many aspects of wound healing process in different parts of the cornea have been elucidated, and some new therapeutic approaches have emerged. The concept of limbal stem cells received rigorous experimental corroboration, with new markers uncovered and new treatment options including gene and microRNA therapy tested in experimental systems. Transplantation of limbal stem cell-enriched cultures for efficient re-epithelialization in stem cell deficiency and corneal injuries has become reality in clinical setting. Mediators and course of events during stromal healing have been detailed, and new treatment regimens including gene (decorin) and stem cell therapy for excessive healing have been designed. This is a very important advance given the popularity of various refractive surgeries entailing stromal wound healing. Successful surgical ways of replacing the diseased endothelium have been clinically tested, and new approaches to accelerate endothelial healing and suppress endothelial-mesenchymal transformation have been proposed including Rho kinase (ROCK) inhibitor eye drops and gene therapy to activate TGF-β inhibitor SMAD7. Promising new technologies with potential for corneal wound healing manipulation including microRNA, induced pluripotent stem cells to generate corneal epithelium, and nanocarriers for corneal drug delivery are discussed. Attention is also paid to problems in wound healing understanding and treatment, such as lack of specific epithelial stem cell markers, reliable identification of stem cells, efficient prevention of haze and stromal scar formation, lack of data on wound regulating microRNAs in keratocytes and endothelial cells, as well as virtual lack of targeted systems for drug and gene delivery to select corneal cells.
Keywords: corneal epithelium, keratocyte, corneal endothelium, wound healing, gene therapy, stem cell
1. Introduction
Cornea is part of the eye exposed to the outer environment and thus most likely to sustain damage due to various insults. Therefore, corneal wound healing not only presents interest to basic science, but is also an important medical issue in need of management. Corneal wound healing is a significant clinical problem. This is due to frequent traumatic damage to the cornea and to the constantly increasing numbers of refractive surgeries. In USA only, over 40,000 corneal transplantations are made annually and the number of patients having received LASIK correction is approaching 20 million. Although the procedures are generally safe, even LASIK surgery generates at least 2% complications with abnormal wound healing, flap detachment, and ectasia. An estimated 20% of population suffers from an eye trauma in their lifetime. The rate of eye injuries in USA is estimated to be over one million annually. These increasingly high numbers illustrate the need for better understanding of corneal healing mechanisms and development of efficient ways to accelerate and improve wound healing.
This process comprises a complex of related events that have a common theme of wound repair by corneal cells. There are definite similarities in healing by epithelial, stromal and endothelial cells related to cell migration, dependence on growth factors and extracellular matrix (ECM) remodeling. Moreover, there is a well-documented cross-talk between healing of epithelial and stromal cells (Fig. 1), adding to the complexity of this process. At the same time, there are significant differences in healing scenarios of different corneal cells. The epithelium heals from itself, with frequent movement and differentiation of limbal stem cells, but it does not undergo transformation to different cell types. In contrast, stromal wounds heal with a sequence of transformation of stromal keratocytes to fibroblasts and myofibroblasts (Fig. 2), and significant participation of resident and circulating immune system cells. Corneal endothelium, unlike other cell types, mostly heals by cell migration and spreading, and may undergo epithelial-mesenchymal transformation in this process, but cell proliferation plays a secondary role. The goal of this review is thus to show the common themes as well as delineate the specifics of wound healing by major corneal cell types. Special emphasis is placed on recent progress in controlling the wound healing process using new biological modulators (including signaling inhibitors and microRNA), gene therapy, stem cells, and nanoformulations. Recent evidence related to using these new tools for addressing wound healing abnormalities related to diseases, such as diabetes, is also presented.
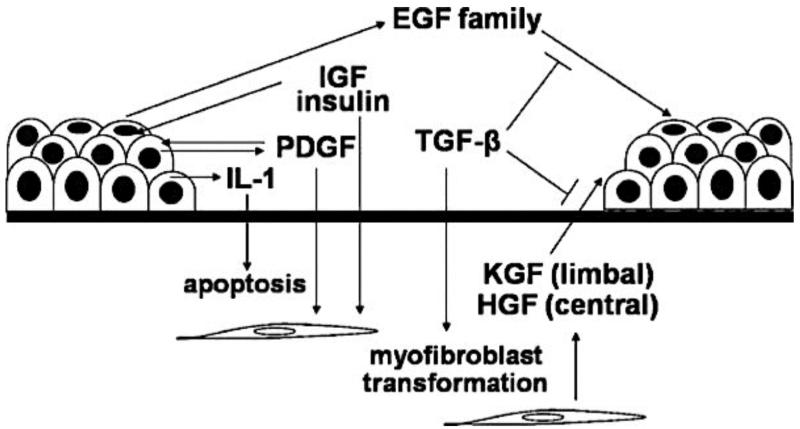
Figure 1.
Growth factors and epithelial wound healing. A multitude of growth factors and cytokines is released following an epithelial injury in the cornea. These factors play essential roles in epithelial–stromal interaction and in the successful healing of a wound. KGF and HGF are believed to be produced by keratocytes to influence epithelial behaviors, while IL-1 and PDGF may be master mediators secreted by the epithelium to modulate stromal response to injury. Others such as the EGF family, IGF, and TGF-β regulate both the epithelium and stromal cell transformation to myofibroblasts, and the cross-talk among various growth factors determines the outcome of an epithelial wound. Reproduced with permission from Yu et al., 2010b.
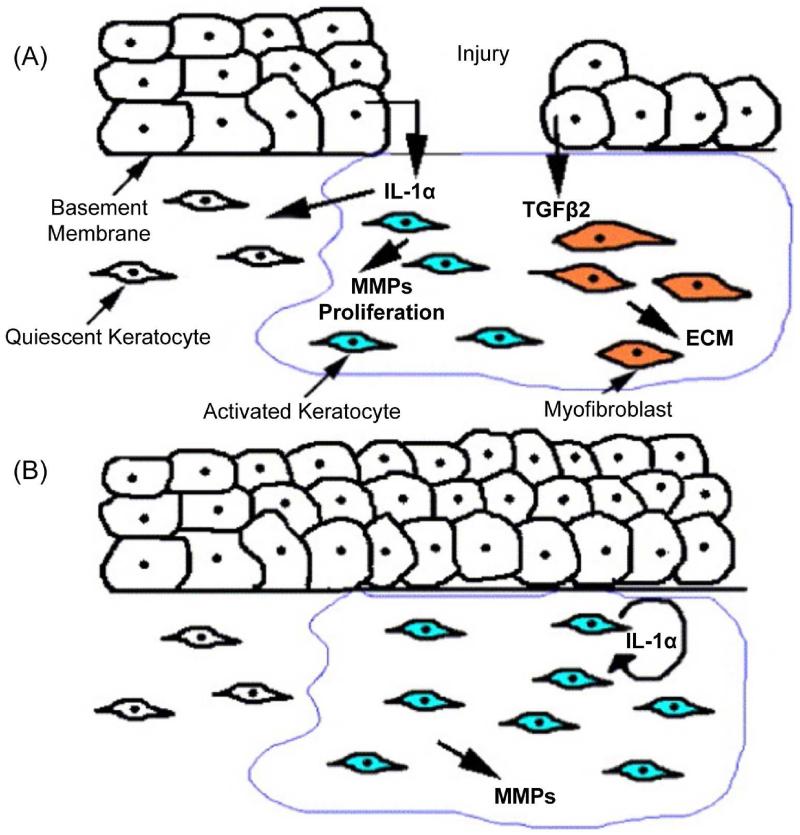
Figure 2.
Cellular interactions during corneal repair. (A) Upon corneal epithelial injury, IL-1α is released from the injured epithelium into the stroma. IL-1α induces some of the underlying stromal keratocytes to undergo cell death, while others are induced to proliferate, secrete MMPs, and transition from a quiescent to an activated phenotype. Due to the absence of a basement membrane, corneal epithelial cells also secrete TGF-β2 into the underlying stroma inducing a subpopulation of keratocytes to undergo transformation into myofibroblasts that secrete ECM. (B) The return of the basement membrane inhibits the release of TGF-β2 into the stroma and the myofibroblast phenotype is no longer observed. The activated keratocytes continue to secrete autocrine IL-1α and remodel the ECM. Reproduced with permission from West-Mays and Dwivedi, 2006.
The authors mainly focused on new published evidence, all the while trying to also reference significant older work in the corneal wound healing field.
2. Corneal epithelial wound healing
Corneal epithelium is a self-renewing tissue with stem cell niche residing in the corneoscleral junction, limbus, and providing a life-long supply of proliferating cells for epithelial regeneration (Di Girolamo, 2015; West et al., 2015). Various chemical, physical, and pathological insults damage the corneal epithelium resulting in disruption of its barrier function and wound formation. Proper wound healing is dynamic in order to maintain the integrity and health of corneal epithelial surface to preserve corneal transparency and vision. The healing of corneal epithelial wounds involves a number of concerted events including cell migration, proliferation, adhesion and differentiation with cell layer stratification. It involves growth factor/cytokine (Fig. 1) and extracellular matrix (ECM) signal-mediated interactions at the wound site to re-establish epithelial integrity and restore corneal homeostasis. The kinetics of epithelial wound healing includes two distinct phases: an initial latent phase and closure phase. The initial phase includes cellular and subcellular reorganization to trigger migration of the epithelial cells at the wound edge (Kuwabara et al., 1976; Crosson et al., 1986). The closure phase includes several continuous processes starting with cell migration, which is independent of cell mitosis (Anderson, 1977), followed by cell proliferation and differentiation and eventually, by stratification to restore the original multicellular epithelial layer (Crosson et al., 1986). Here we provide an overview of factors and mechanisms important for the control of corneal epithelial wound healing in normal and diseased states. Various ways of wounding corneal epithelium (epithelial debridement) for mechanistic studies have been reviewed in detail recently (Stepp et al., 2014).
2.1. Growth factors/cytokines in epithelial wound healing
Growth factors and cytokines are important regulators that stimulate growth, proliferation, migration, differentiation, adhesion, ECM deposition and proteinase regulation of cells involved in wound healing (Fig. 1). They mediate different cell functions including intracellular and intercellular signaling molecules. Corneal cells express many growth factors and cytokines that have specific effects on epithelial cells, such as epidermal growth factor (EGF), platelet-derived (PDGF) and transforming (TGF) growth factors α and β, acidic (FGF-1) and basic (FGF-2) fibroblast growth factors, insulin-like (IGF-I), keratinocyte (KGF), hepatocyte (HGF) growth factors, thymosin-β4,(Tβ4), interleukins (IL)-1, -6, and -10, and tumor necrosis factor (TNF)-α. Many of these factors are activated during wound healing (Lu et al., 2001; Yu et al., 2010b) and in corneal diseases such as diabetes (Gambaro and Baggio,1998; Hellmich et al., 2000; Keadle et al., 2000; Saghizadeh et al., 2005).
2.1.1. Epidermal growth factor family
EGF signaling comprises a major pathway that initiates cell migration and proliferation and stimulate corneal epithelial wound healing (Zieske et al., 2000; Lu et al., 2001; Nakamura et al., 2001). At early times of epithelial wound healing, cellular signaling initiated by EGF receptor (EGFR1/ErbB1 usually simply called EGFR) tyrosine kinase lead to activation of major downstream effectors, phosphatidylinositol-3-kinase (PI3-kinase)-Akt axis, and extracellular regulated kinase (ERK) (Zhang and Akhtar, 1997; Xu et al., 2009; Xu and Yu, 2011; Funari et al., 2013; Winkler et al., 2014). EGFR signaling activates an NF-κB pathway, which leads to transcriptional repressor CTCF activation and PAX6 downregulation (Li and Lu, 2005; Lu et al., 2010; Wang et al., 2012a) resulting in cell migration and proliferation in corneal epithelial cells (Imanishi et al., 2000). Recent studies (Wang et al., 2013) have demonstrated that in NF-κB p50 knockout mice, corneal epithelial wound healing is significantly delayed, suggesting that NF-κB signaling pathways play important roles in growth factor-promoted corneal epithelial self-renewal and wound healing. EGFR signaling also activates histone deacetylase 6 (HDAC6), which deacetylates α-tubulin, and promotes corneal epithelial cell migration and healing of debridement wounds. The effect on EGF-induced cell migration was verified by suppression of HDAC6 activity by trichostatin A or of its expression by siRNA (Wang et al., 2010a). Extending the duration of EGFR activity by inhibiting its negative regulator, E3 ubiquitin ligase (c-CbI), enhanced the rate of restoration of the corneal epithelial layer both in vitro and in vivo (Rush et al., 2014). In vivo studies in rats with type 1 diabetes mellitus (DM1) showed that a significant delay in corneal epithelial wound healing was correlated with altered EGFR signaling pathways through phosphatidylinositol 3-kinase (PI3K)–Akt and ERK, as well as their downstream BAD signaling pathways in migratory epithelium (Xu and Yu, 2011). shRNA-mediated suppression of matrix metalloproteinase (MMP)-10 and cathepsin F genes by adenoviral gene therapy of whole corneal epithelium or only of limbal cells normalized epithelial wound healing altered in human diabetic organ-cultured corneas with restoration of signaling pathways mediated by EGFR-Akt axis (Saghizadeh et al., 2013b; 2014). Moreover, in a DM1 mouse model, the application of substance P, a neuropeptide, promoted epithelial wound healing altered in diabetic mice, apparently by activating Akt, an EGFR downstream signaling molecule (Yang et al. 2014a). Furthermore, downregulation of phosphorylated and/or total EGFR by miR-146a or miR-424 led to a delayed wound healing in cultured telomerase-immortalized human corneal epithelial cells (Funari et al., 2013) and in primary limbal epithelial cells (Winkler et al., 2014). Therapeutic potential of human recombinant EGF for enhancing corneal epithelial wound healing has been reviewed (Márquez et al., 2011).
EGFRs comprise a family of four receptors, of which EGFR1 is the most studied in many cells and tissues including the cornea. EGFR2/ErbB2 has also been shown to promote corneal epithelial wound healing acting through ERK and PI3K (Xu et al., 2004b). EGFR3/ErbB3 is also expressed in the corneal epithelium, but its role in wound healing has not been investigated (Liu et al., 2001).
Beside EGF, there are several additional endogenous ligands known to bind EGFR1, such as heparin-binding EGF (HB-EGF) with an extra domain binding negatively charged glycans, transforming growth factor-α (TGF-α), betacellulin (BTC), amphiregulin (AR), and epiregulin (EPR). HB-EGF acting as both soluble and transmembrane protein increases epithelial wound healing through enhancing cellular attachment in vitro (Block et al., 2004; Xu et al., 2004a; Yoshioka et al., 2010). Since HB-EGF knockout mice die shortly after birth (Iwamoto et al., 2003), it was suggested that HB-EGF is the most important for growth and development among all the EGFR ligands. In addition, by establishing keratinocyte-specific HB-EGF-deficient (HB−/−) mice by Cre/loxP technology, it has been demonstrated that wound healing was significantly delayed in corneal epithelium (Yoshioka et al., 2010). Several studies also suggest that it stimulates better wound healing responses than EGF in corneal epithelial cells (Xu et al., 2004a; Tolino et al., 2011). The rates of EGFR downregulation by both EGF variants are relatively similar. However, HB-EGFR remains bound to cell much longer than EGF and has a lasting effect on wound healing after brief treatment, consistent with immobilized pool of HB-EGF on the cell surface and ECM providing continuous EGFR stimulation (Tolino et al., 2011). Another EGFR ligand, TGF-α, has been shown to enhance corneal epithelial migration and proliferation similar to EGF and HB-EGF, whereas it inhibited the expression of the differentiation-related corneal epithelial marker keratin 3 (Wilson et al., 1994). It has also been shown that mice that genetically lack TGF-α production have chronic corneal erosions (Mann et al., 1993). An in vitro study has demonstrated that TGF-α is a more potent activator of EGFR-mediated corneal wound healing than EGF via its ability to stimulate EGFR endocytosis and recycle it back to the plasma membrane where it can be re-stimulated (McClintock and Ceresa, 2010).
Epiregulin is upregulated in limbal epithelial basal cells compared to central cornea in mice. It increases corneal epithelial cell proliferation in vitro by activating EGFR and increasing the expression of HB-EGF and AR (Zhou et al., 2006; Morita et al., 2007), suggesting its role in maintaining the proliferative capacity of limbal basal cells. In vitro studies have shown that BTC was the most potent stimulator of corneal epithelial wound healing. However, out of six EGFR ligands, only EGF could promote wound healing in vivo, and it was the only ligand present at concentrations near the ligand’s Kd for the EGFR in human tears (Peterson et al., 2014). Importantly, EGFR can be transactivated through several effectors in addition to its own ligands to enhance migration and proliferation in wound healing (Lyu et al., 2006; Yang et al., 2010; Zhang et al., 2010).
2.1.2. Hepatocyte growth factor (HGF), or scatter factor
HGF is mainly produced by mesenchymal cells and targets epithelial cells in a paracrine manner via their cell surface receptor, c-met, a proto-oncogene expressed in epithelial cells (Bottaro et al., 1991; Rosen et al., 1994). It is expressed more in the central cornea than in the limbus by stromal cells. However, HGF and c-met mRNAs are found in all three major cell types of the human cornea including epithelial, stromal, and endothelial cells (Wilson et al., 1993), suggesting the existence of autocrine loops in corneal endothelium and epithelium. HGF regulates cell proliferation (Wilson et al., 1993), migration (Daniel et al., 2003; Saghizadeh et al., 2010a; 2011), and apoptosis (Kakazu et al. 2004) in corneal epithelial cells. After corneal epithelial wounding HGF expression is upregulated in keratocytes (Li et al., 1996) and epithelial cells (Kakazu et al., 2008; Saghizadeh et al., 2010a), which may contribute to the epithelial wound healing process. These data imply that, although corneal epithelial cells are stimulated mainly by exogenous HGF produced in lacrimal glands and present in tears, HGF may also function in intracrine and autocrine manners beside paracrine in regulating corneal wound healing (Wilson et al., 1993; Li et al., 1996). Our group and others have shown the contribution of altered growth factors including HGF–c-met system to basement membrane changes in diabetic cornea, and to the delayed epithelial wound healing (Ljubimov et al., 1998a; Saghizadeh et al., 2001a; 2001b; 2005; 2010a; 2011; Yu et al., 2010b). The important role of HGF–c-met in impaired diabetic corneal wound healing (Fig. 3) was confirmed in organ-cultured human diabetic corneas. Restoration of diabetes-decreased c-met levels in these corneas by gene therapy (Fig. 4) normalized wound healing dynamics, with downstream activation of p38 mitogen-activated protein (MAP) kinase (Sharma et al., 2003), as well as the expression of several stem cell markers (Saghizadeh et al., 2010a; 2011). Importantly, this positive effect was observed in organ-cultured corneas after gene therapy of either the whole epithelium or only limbal area (Figs. 4, 5) harboring stem cells (Saghizadeh et al., 2013b, 2014).
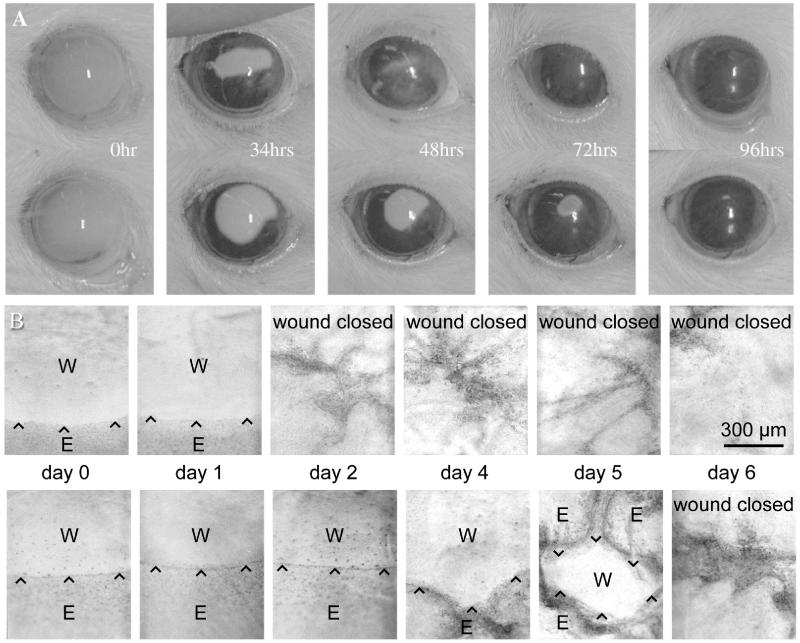
Figure 3.
Representative wound healing dynamics of normal and diabetic corneas. A, healing of rat epithelial scrape wounds. Upper panel, normal rat eye; lower panel, Goto-Kakizaki diabetic rat eye (DM2 model). Healing of diabetic cornea is clearly delayed. Reproduced with permission from Chikama et al., 2007.
B, healing of n-heptanol induced epithelial wounds in organ-cultured human corneas. Upper panel, normal cornea; lower panel, diabetic cornea. Healing of diabetic cornea is significantly delayed. Wound edges are marked by arrowheads. W, wound; E, epithelium. Reproduced with permission from Kabosova et al., 2003.
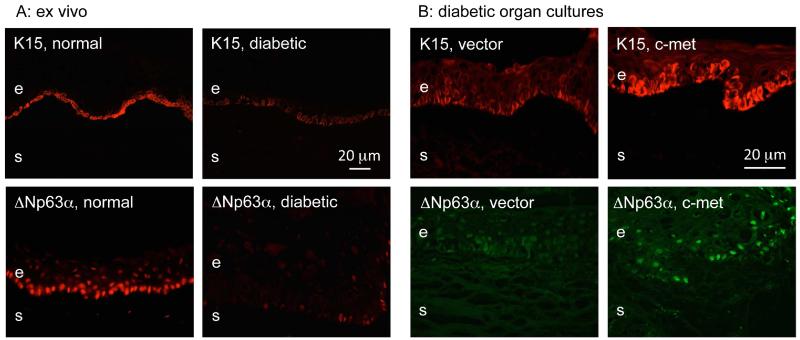
Figure 4.
Gene therapy-mediated upregulation of stem cell marker expression in diabetic corneas. A. Putative LESC marker expression patterns in normal and diabetic ex vivo limbus. Note a dramatic decrease in staining intensity and the number of positive basal epithelial cells for K15 and ΔNp63α in the diabetic limbus. B. Increased putative LESC marker expression in the diabetic limbus in organ culture upon c-met overexpression. c-Met gene transduction led to elevated and similar to normal expression of K15 and ΔNp63α in the limbus of organ-cultured diabetic corneas. e, epithelium, s, stroma. Bars = 20 μm. Reproduced from Saghizadeh et al., 2011.
Figure 5.
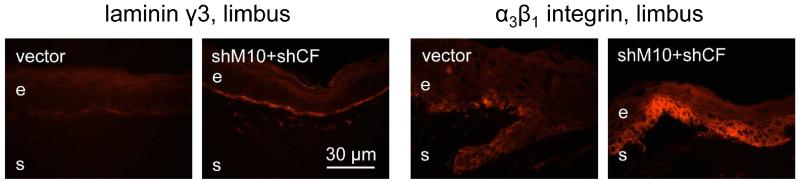
Increased expression of diabetic markers upon proteinase gene silencing in organ-cultured diabetic corneas. Left, limbal BM component laminin γ3 chain; a markedly increased staining and continuity is seen after shRNA silencing of MMP-10 (M10) and cathepsin F (CF) expression. Right, similar results obtained for a diabetes-downregulated marker α3β1 integrin. Bar = 30 μm. Reproduced from Saghizadeh et al., 2013b. © Association for Research in Vision and Ophthalmology.
2.1.3. Keratinocyte growth factor (KGF)
KGF is a member of the FGF family and is formally called fibroblast growth factor-7 (FGF-7). KGF functions in a similar fashion as HGF in corneal epithelial homeostasis and during wound healing (Wilson et al., 1998). KGF mRNA is expressed mainly by lacrimal gland and limbal fibroblasts, and its receptor, by limbal epithelial cells. It was suggested that KGF functions mainly in a paracrine fashion in the limbal epithelial homeostasis and during wound healing process (Wilson et al., 1993; Sotozono et al., 1994). KGF increased corneal epithelial wound healing in rabbit organ-cultured corneas (Chandrasekher et al., 2001) and enhanced cell proliferation in the limbal epithelium during regeneration of rabbit cornea in vivo (Sotozono et al., 1995). KGF promotes wound healing through MAP kinases and PI3K/p70 S6 signaling cascades in corneal epithelial cells (Chandrasekher et al., 2001; Sharma et al., 2003). In addition, the disruption of barrier function induced by hypoxia in human corneal epithelial cells was inhibited by KGF through ERK activation (Teranishi et al., 2008). Another member of the FGF family is KGF-2/FGF-10, which also functions in a paracrine fashion and has a role in regulation of corneal wound healing by stimulating epithelial stem cell proliferation (Wang et al., 2010b).
2.1.4. Insulin-like growth factors (IGFs)
IGFs have important roles in growth and energy metabolism, and regulate cell migration (Lee et al., 2006), differentiation (Trosan et al., 2012), proliferation, and survival (Yanai et al., 2006) in corneal epithelial cells through insulin receptor, and IGF receptors type I and type II. IGF-I and its receptors are expressed by both human corneal keratocytes and epithelial cells (Li and Tseng, 1995). In vivo studies have shown that rapid overexpression of IGF-I in wounded mouse cornea increased expression of IGF receptor in limbal cells and stimulated limbal cell differentiation, with no effects on limbal cell proliferation (Trosan et al., 2012). However, IGF-I can enhance proliferation and wound closure synergistically with substance P in-vivo (Nakamura et al., 1997), and in ex-vivo rabbit corneal epithelial cells (Nishida et al., 1996; Yamada et al., 2004). In addition, synergy of IGF-I with substance P in enhancing wound healing was observed in diseased corneas of diabetic rats (Nakamura et al., 2003) and in a rat model of neurotrophic keratopathy (Nagano et al., 2003). Another related key metabolic regulator present in tears is insulin. It is closely related to IGFs and enhances proliferation in corneal epithelial cells and wound healing through EGFR transactivation, ERK and PI3K activation (Shanley et al., 2004; Lyu et al., 2006). Interestingly, IGF-I mediates many growth-promoting effects of the growth hormone. However, growth hormone stimulation of corneal epithelial migration necessary for wound healing and mediated by STAT5 seems to occur independently of IGF-I suggesting a potential for combination therapy (Wirostko et al., 2015).
2.1.5. Transforming growth factor-β (TGF-β)
TGF-β isoforms, TGF-β1, TGF-β2 and TGF-β3, and their receptors are expressed by corneal epithelium and stromal keratocytes (Nishida et al., 1994). TGF-β isoforms are synthesized and secreted as inactive precursors with N-terminal latency-associated peptides, which are dissociated from TGF-β dimers during the activation process (Nishida et al., 1994). TGF-β1 and TGF-β2 can inhibit corneal epithelial cell proliferation in vitro (Pancholi et al., 1998; Haber et al., 2003), but have stimulatory effects on corneal stromal fibroblast proliferation (Andresen et al., 1997). Both TGF-β1 and TGF-β2 have antagonistic effects on EGF, HGF and KGF induced proliferation in vitro (Mishima et al., 1992; Honma et al., 1997). However, TGF-β2 can enhance corneal epithelial wound healing in rabbit corneas in vivo (Er and Uzmez, 1998). TGF-β stimulates corneal epithelial cell migration via integrin β1, which mediates p38 MAPK activation, ECM expression and epithelial-mesenchymal transformation (EMT) leading to increased cell mobility (Bhowmick et al., 2001; Saika et al., 2004a). Recent studies showed that corneal epithelial wound healing is delayed for 48 hours along with delay in p38 MAPK activation in mice lacking TGF-β signaling when its type II receptor is conditionally ablated (Terai et al., 2011). Along with impaired cell migration resulting from the delayed activation of p38 MAPK, the cell proliferation was suppressed at the leading wound edge probably via the alternative c-Jun N-terminal kinase (JNK) pathway (Saika et al., 2004b; Terai et al., 2011). Delayed activation of p38 MAPK in the absence of TGF-β receptor signaling suggests p38 MAPK is activated initially via the main TGF-β Smad signaling pathway and later, through another signaling cascade, possibly involving EGFR and other potential candidates (Saika et al., 2004b; Terai et al., 2011). Recent gene microarray analysis (Bettahi et al., 2014) revealed that both TGF-β1 and TGF-β3 were increased in response to wounding. In addition, the functional studies of TGF-β3 showed its contribution to wound healing in normal mouse and rat corneal epithelial cells (Bettahi et al., 2014). Further studies showed that TGF-β3, which was downregulated in rat DM1 and DM2, and in mouse DM1 models, enhanced epithelial wound closure in DM2 rat and DM1 mouse corneas via Smad and PI3K-Akt signaling pathways, and its target gene, PAI-1/Serpine1 (Bettahi et al., 2014). These data point to possible therapeutic potential of TGF-β3 for treating corneal and skin wounds in diabetic patients. Moreover, TGF-β3 can alleviate scar formation in the stroma due to TGF-β1 and -β2 activity (see Section 3).
2.1.6. Platelet-derived growth factors (PDGFs)
PDGF is made up of combination of four polypeptide chains, A, B, C, and D, as PDGF-AA, PDGF-BB, PDGF-AB, PDGF-CC, and PDGF-DD (Heldin, 2013). The first three PDGF isoforms are expressed by corneal epithelial cells and regulate migration and proliferation of keratocytes (Denk and Knorr, 1997; Kamiyama et al., 1998; Daniels and Khaw, 2000). PDGF-AB and PDGF-BB enhanced the migration of corneal fibroblasts in vitro, which could be blocked by respective antibodies (Kamiyama et al., 1998). Additionally, PDGF isoforms (PDGF-AA, PDGF-BB, and PDGF-AB), especially PDGF-AB, stimulated migration of rabbit corneal epithelial cells, but only in the presence of fibronectin (FN), which is part of provisional wound ECM (Kamiyama et al., 1998; Nishida et al., 2010).
2.1.7. Thymosin-β4 (Tβ4)
Tβ4 belongs to β-thymosin family of highly conserved 5 kDa peptides that primarily interact with G-actin and function as actin-sequestering proteins (Low et al., 1981; Dedova et al., 2006). Recent studies have revealed a wide range of biological activities by Tβ4, such as cell migration, angiogenesis, inflammation, and regeneration of damaged tissues including skin and cornea. Tβ4 promotes corneal re-epithelialization during healing, decreases inflammation and inhibits apoptosis both in vitro and in vivo using alkaline burn animal model. It also upregulates epithelial basement membrane (BM) component laminin-332, which mediates epithelial migration (Sosne et al., 2002; 2004; 2015). Tβ4 eye drops were able to improve wound healing in patients with chronic nonhealing neurotrophic corneal epithelial defects in a small clinical trial (Dunn et al., 2010). Tβ4 has been also successfully used in patients with dry eye syndrome (Sosne et al., 2012; 2015), and has shown protection of corneal endothelial cells from UVB-induced oxidative stress and apoptosis (Ho et al., 2010).
2.1.8. Interleukins 6 and 10 (IL-6 and IL-10)
Cytokines, such as IL-6 and IL-10, are secreted by epithelial cells or immune cells during wound healing, which is supposed to be beneficial for regeneration. IL-6 is an inflammatory cytokine elevated in tears of dry eye patients, which could be related to pain and tear film formation (Enriquez-de-Salamanca et al., 2010). Downstream IL-6 signaling pathway involves Janus kinase (JAK) self-phosphorylation leading to transcription regulator STAT3 activation (Sugaya et al., 2011). On the other hand, IL-10 is an anti-inflammatory cytokine elevated in patients with corneal graft rejection (van Gelderen et al., 2000). It has been shown that IL-6 enhances cell migration and wound healing of rabbit corneal epithelial cells (Nakamura and Nishida, 1999). More recently, the involvement of both IL-6 and IL-10 in wound healing response of human corneal epithelial cells has been demonstrated (Ebihara et al., 2011; Arranz-Valsero et al., 2014).
2.1.9. Nerve growth factor (NGF)
NGF is a member of the neurotrophin family of growth factors that is critical for the growth, maintenance, and survival of sympathetic and sensory neurons, and which also functions as a signaling molecule. Neurotrophin receptor p75 (NTR) and tropomyosin receptor kinase A (TrkA), a transmembrane tyrosine kinase, are NGF receptors present in both cornea and conjunctiva (You et al., 2000; Ríos et al., 2007). Several neuronal survival pathways are regulated by NGF signaling. The major pathway contributing to cell survival operates through NGF binding to TrkA leading to the activation PI3K-Akt. Another pathway works through MAPK-Ras-Raf and ribosomal S6 kinase (RSK) activation leading to transcriptional regulation. Recent studies have shown the role of NGF and its receptors TrkA and p75NTR in epithelial wound healing process in cornea and skin (Lambiase et al., 1998a; 2004; Micera et al., 2004). In patients with corneal ulcers, topical murine NGF eye drops ameliorated the rate of corneal epithelial healing and corneal sensitivity (Lambiase et al., 1998b; Bonini et al., 2000). In addition, NGF has beneficial effects on wound healing by modulating cell migration, keratocyte differentiation into myofibroblasts, and MMP-9 expression (Micera et al., 2006). More recent studies also showed the major role of NGF in epithelial and stromal healing where it stimulated cell migration by upregulation of MMP-9 and cleavage of integrin β4 (Blanco-Mezquita et al., 2013) and reduced haze formation (Anitua et al., 2013). These studies suggest that NGF has a potential to promote corneal wound healing in a clinical setting.
2.1.10. Opioid growth factor (OGF), or (Met5)-enkephalin
OGF is an autocrine and/or paracrine growth factor that binds to its ζ receptor (OGFR) to modulate DNA synthesis, cellular migration, and tissue organization of the corneal epithelium (Zagon et al., 1995; 1997). It is expressed in the epithelial basal and suprabasal layers and has an inhibitory effect on cellular proliferation through cyclin-dependent kinase inhibitors, p16 and/or p21 (McLaughlin et al., 2010). Opioid antagonist naltrexone (NTX) can disrupt OGF-OGFR interaction, which in the rabbit led to 30% to 72% increase in DNA synthesis in basal limbal and conjunctival epithelial cells with no effect on central corneal epithelium (Zagon et al., 1998a; 1998b). Conversely, OGF overexpression caused decreased DNA synthesis of basal epithelial cells in the peripheral cornea, limbus, and conjunctiva by 25% to 50%. Several studies have showed that both systemic injections and topical applications of NTX significantly accelerated corneal epithelial wound healing rate and re-epithelialization in rat, rabbit, and human (Zagon et al., 1998a; 1998b; 2000). Topical NTX application also normalized delayed wound healing, as well as tears production and corneal sensitivity in diabetic rodents (Klocek et al., 2009; Zagon et al., 2009). Topical application of opioid antagonist eye drops might be a promising novel therapy for corneal epithelial wound healing disorders.
2.2. Other molecular effectors in corneal epithelial wound healing
2.2.1. Purinergic receptors
The release of ATP induced within one minute after injury results in mobilization of intracellular calcium upon activation of purinergic receptors P2Y or P2X (Weinger et al., 2005; Lee et al., 2014). This activation appears to be one of the earliest events in the healing process (Lee et al., 2014). In the P2X7 knockout mice, corneal epithelial wound healing was compromised (Mayo et al., 2008). In addition, downregulation of the P2Y2 receptor using siRNA also inhibited wound healing in corneal epithelial cells in comparison to control cells transfected with scrambled sequence (Boucher et al., 2010). The release of nucleotides at the wound site not only activates purinergic receptor P2Y, but also leads to phosphorylation of site-specific residues on EGFR and its EGF-independent activation, suggesting possible cross-talk between purinergic receptors and EGFR in corneal epithelial cell migration and wound healing (Boucher et al., 2011). Most recent data show that the effects of P2X7 on wound healing may be mediated by a rearrangement of actin cytoskeleton enabling epithelial cells to better migrate (Minns et al., 2015).
2.2.2. Toll-like receptor 4 (TLR4)
TLRs also contribute to early corneal epithelial wound healing by enhancing cell migration and proliferation in vitro and in vivo (Eslani et al., 2014). TLRs are a family of proteins that play a major role in the innate immune system and modulate inflammation via several pathways such as nuclear factor κB (NF-κB), MAP kinases, and activator protein (AP)-1 (Pearlman et al., 2008; Kostarnoy et al., 2013). TLR4 signaling pathway is activated in response to its ligands such as pathogen-associated molecular patterns (viruses and bacteria), and damage-associated molecular patterns as a result of tissue injury. This leads to production of proinflammatory cytokines, adhesion molecules, and proteolytic enzymes during the inflammatory stage of wound healing (Pearlman et al., 2008; Kostarnoy et al., 2013), as well as to enhanced cell migration and proliferation. Human corneal epithelial cells (HCEC) treated with lipopolysaccharide (LPS) showed significant increase in wound closure. In these cells TLR4 mediated increase in cytokines such as IL-6, TNF-α, and CXCL8/IL-8, as well as enhanced phosphorylation of ERK1/2 and p38 MAP kinases (Eslani et al., 2014). Thus, TLR4 contributes to both inflammatory responses and epithelial migration and proliferation (Sharma et al., 2003; Eslani et al., 2014).
2.2.3. Rho-associated protein kinase (ROCK)
ROCK is a serine/threonine kinase, which is mainly involved in regulating cell movement through formation of actin stress fibers and focal adhesions (Leung et al., 1995; Ishizaki et al., 1996). ROCK1 and ROCK2 are major downstream effectors of the small Rho GTPases, the major regulators of the cytoskeleton. They are involved in many corneal cell functions such as epithelial differentiation (SundarRaj et al., 1998), proliferation (Yin et al., 2008), cell adhesion (Anderson et al. 2002), cytoskeleton reorganization (Kim and Petroll, 2007), and cell-matrix interactions (Kim et al., 2006). Both ROCK 1 and ROCK 2 are activated in response to wounding and HB-EGF stimulation. ROCK inhibitor Y-27632 accelerates wound healing mainly by modulating cell-ECM and cell-cell adhesion in HCECs, whereas Rho inhibitor C3 attenuates wound closure (Yin et al., 2008; Yin and Yu, 2008). ROCKs regulate cell-cell adhesion mediated by E-cadherin and β-catenin, as well as the formation and maintenance of barrier integrity (Yin and Yu, 2008). The mechanism of ROCK inhibitor influence on wound healing may be suggested from experiments with cardiac cells, where ROCK is induced by TGF-β and inhibits bone morphogenetic protein (BMP)-2 expression (Wang et al., 2012b). At the same time BMP-2 can mediate cell migration by inducing some ECM components (Inai et al., 2013). Therefore, ROCK inhibition may switch signaling from profibrotic TGF-β to pro-migratory BMP, and thus promote cell migration necessary for wound healing.
2.3. Cross-talk of signaling pathways in epithelial wound healing
Epithelial wound healing is mediated by various growth factors and cytokines that activate both parallel and sequential downstream signaling pathways. The growing evidence suggests the existence and importance of intracellular signaling cross-talk in the epithelial healing after injury. In the initial or lag phase of wound healing several parallel signaling pathways, which may also cross-talk, are activated to reorganize cellular and subcellular structures initiating cell migration, the first step of the healing process. These initial factors include IL-1 and TNF-α (Wilson et al., 1999), EGF and PDGF (Tuominen et al., 2001), which trigger a series of responses leading to epithelial cell migration through ERK, MAP kinases, and/or NF-κB pathway. Additionally, a number of transcription factors, such as c-fos, c-jun, jun-B, and fos-B, become activated during the lag phase of wound healing before the cells start to migrate (Oakdale et al., 1996). These initial factors can also lead to activation of other parallel pathways in underlying stroma, including IL-1-mediated keratocyte apoptosis via Fas/Fas ligand (Wilson et al., 1999), which leads to consecutive pathways of pro-inflammatory cascades in the first 24 hr following injury (Wilson et al., 2001). EGFR transactivation has been shown to enhance intracellular signaling in corneal epithelial wound healing in the presence of non-EGF ligands such as IGF, insulin, and HGF by activating ERK and PI3K/Akt pathways (Lyu et al., 2006; Spix et al., 2007). HGF and KGF, as well as pigment epithelium-derived factor (PEDF) signaling during wound healing converges on p38 and/or ERK1/2 pathways; the former mediates cell migration, whereas the latter induces proliferation (Sharma et al., 2003; Ho et al., 2013).
Another initial wound healing factor is the release of matrix metalloproteinases (MMPs), which triggers a series of processes to disengage cell-cell and cell-matrix adhesion. This further leads to initiation and facilitation of cell migration via cross-talk with integrins and the production of ECM proteins such as fibronectin, laminin and tenascin, in the wound area that act as a temporary scaffold for migratory cells (Tuft et al., 1993). The release of cellular nucleotides (e.g., ATP) upon epithelial injury is also implicated as an initial factor causing rapid activation of purinergic signaling and increase of intracellular Ca2+ levels leading to EGFR transactivation and cell migration, and eventually, epithelial wound healing with corneal nerve involvement (Weinger et al., 2005; Boucher et al., 2007; Yin et al., 2007; Lee et al., 2014). EGFR and purinergic signaling are also involved in the phosphorylation of paxillin needed for cell migration (Kimura et al., 2008; Mayo et al., 2008).
Cell migration during wound healing may also involve a cross-talk between growth factors and ECM. IGF-I was shown to induce cell migration directly through its receptor, as well as through stimulating the expression of corneal BM component laminin-332, which facilitates epithelial cell migration in vitro (Lee et al., 2006). IGF-I receptor can be also engaged in cross-talk with β1 chain-containing integrins important for corneal epithelial cell migration (Seomun and Joo, 2008) through their recruitment to lipid rafts (Salani et al., 2009). Overall, significant cross-talk in corneal wound healing has been revealed between several growth factors through transactivation of signaling pathways, and between growth factors and extracellular mediators of this process. This cross-talk underlines the complex nature of epithelial wound healing, and is a complicating factor in studies of this process using signaling inhibitors and activators.
2.4. Proteinases in epithelial wound healing
Proteinases, such as MMPs, cathepsins, and plasminogen activators are implicated in a wide range of physiological and pathological processes, including development, morphogenesis, angiogenesis, wound healing and tissue remodeling. MMPs form a large family of zinc-dependent endopeptidases that act on a variety of substrates, including ECM and BM proteins, proteinases, and their inhibitors, to activate growth factors, cytokines, receptors, and adhesion molecules (Sivak and Fini, 2002). Most MMPs are secreted as proenzymes and undergo proteolytic activation. MMP expression is also regulated by growth factors/cytokines (Girard et al., 1991; Kim et al., 2004). MMPs influence cell migration via extracellular matrix degradation or by modifying cellular adhesive properties and are elevated during corneal wound healing (Daniels et al., 2003; Blanco-Mezquita et al., 2013; Petznick et al., 2013; Mauris et al., 2014). They may also stimulate proliferation by altering the extracellular matrix microenvironment. In addition, MMPs may modulate the activity of growth factors/cytokines and receptors (Vu and Werb, 2000; Mott and Werb, 2004). Some MMPs, e.g., MMP-10 may delay corneal epithelial wound healing, possibly through downstream signaling (see below). The others, such as MMP-9, may play very complex roles in this process. On the one hand, galectin-3-induced MMP-9 facilitates corneal cell movement and wound healing by disrupting cell-cell contacts (Mauris et al., 2014), and respective knockout mice show delayed healing of skin wounds in vivo (Kyriakides et al., 2009). At the same time, its excessive production upon certain corneal injuries may dissolve epithelial BM and negatively impact healing (Fini et al., 1996; Ottino et al., 2002). Moreover, excessive MMP-9 cleavage of β4 chain of the hemidesmosomal component integrin α6β4 may lead to corneal epithelial erosions (Pal-Ghosh et al., 2011a). The final outcome may depend upon the availability and amounts of tissue inhibitors of MMPs (TIMPs) that are natural modulators of MMP activity (Nelson et al., 2000; Nagase and Brew, 2003). A comprehensive expression analysis of MMPs and TIMPs during corneal epithelial resurfacing in mice showed distinct MMP temporal-spatial profiles at different stages of regeneration (Gordon et al., 2011).
Urokinase-type plasminogen activator (uPA/PLAU) is upregulated in wounded corneal epithelial cells and may stimulate cell migration (Watanabe et al., 2003). Its influence on cell migration may be fine-tuned by its inhibitor (PAI-1/serpin E1/PLANH1) that is adhesive and chemotactic for corneal epithelium (Wang et al., 2005). The cathepsin family comprises lysosomal proteinases that may also be found on the cell surface or extracellularly and were implicated in ECM degradation, e.g., in keratoconus corneas (Maguen et al., 2008).
Abnormal MMP expression contributes to many pathological conditions, such as diabetic keratopathy and chronic wounds (Fini et al., 1996; Maguen et al. 1997; 2002; 2007; 2008; Nelson et al., 2000; Saghizadeh et al., 2001a; 2005; 2010a; Mohan et al., 2002; Kabosova et al., 2003; Toriseva and Kähäri, 2009). Our studies demonstrated increased expression of MMP-10 and cathepsin F in the human diabetic corneal epithelium, whereas diabetic keratocytes upregulated MMP-3 and MMP-10 (Saghizadeh et al., 2001a; 2005; 2010a; Kabosova et al., 2003). We also showed that overexpression of MMP-10 and cathepsin F in normal organ-cultured human corneas delayed wound healing and led to diabetic-like changes in basement membrane and integrin patterns (Saghizadeh et al., 2010a). Conversely, silencing of MMP-10 and cathepsin F genes using recombinant adenovirus-driven small hairpin RNA (shRNA) enhanced wound healing as well as increased epithelial and stem cell marker expression in organ-cultured human diabetic corneas through EGFR/Akt signaling pathway (Saghizadeh et al., 2013b; 2014). The data on MMP-10 were corroborated by in vivo studies of galactose-fed diabetic rats that also showed overexpression of MMP-10, which resulted in delayed wound healing. Whereas, suppression of MMP-10 expression by aldose reductase inhibitor normalized wound healing in diabetic animals (Tomomatsu et al., 2009; Takamura et al., 2013). Overall, some proteinases may facilitate wound healing, whereas the others inhibit it. Therefore, caution should be exerted when using broad-spectrum inhibitors, such as MMP inhibitor doxycycline (Li et al., 2003), to treat corneal problems associated with abnormal wound healing.
2.5. Extracellular matrix (ECM) in epithelial wound healing
Corneal epithelium makes its own ECM in the form of specialized epithelial BM that is apposed to underlying collagenous Bowman’s layer. It provides structural support and regulates through various receptors epithelial migration, proliferation, differentiation, adhesion and apoptosis (Azar et al., 1992; Kurpakus et al., 1992; Zieske et al., 1994; Ljubimov et al., 1995, 1996a; 1996b; Suzuki et al., 2003). Corneal BM components undergo considerable remodeling during embryonic and postnatal development (Kabosova et al., 2007). In the adult, they display regional heterogeneity among central part, limbus, and conjunctiva with respect to the distribution of type IV collagen and laminin isoforms, as well as of thrombospondin-1 (TSP-1), tenascin-C, fibrillin-1, and type XII collagen (Ljubimov et al. 1995; Kabosova et al., 2007; Schlötzer-Schrehardt et al., 2007). Corneal epithelial BM is composed of specialized networks of type IV collagens, laminins, nidogens, and perlecan as most BMs (Nakayasu et al. 1986; Martin and Timpl, 1987; Ljubimov et al., 1995; 1996a; Tuori et al. 1996; Kabosova et al., 2007; Schlötzer-Schrehardt et al., 2007), with additional components, such as TSP-1, matrilin-2, matrilin-4, types XV, XVII and XVIII collagen, and FN (Kabosova et al., 2007; Schlötzer-Schrehardt et al., 2007; Dietrich-Ntoukas et al., 2012). During epithelial wound healing, BM often undergoes degradation and subsequent resynthesis/reassembly and may regulate directed migration of epithelial cells into the wound, together with chemotactic factor gradients (Suzuki et al., 2000; Yu et al., 2010b). Several hours after the epithelial injury, a number of provisional ECM components, both BM-related, such as FN, and non-BM-related, such as fibrin (probably originating from tears), are laid down on the denuded area and/or overexpressed by the leading cells at the wound edge and subsequently by basal epithelial cells and keratocytes (Fujikawa et al., 1984; Tuft et al., 1993). This temporary ECM appears to be accumulated by a TGF-β-dependent mechanism (Leask and Abraham, 2004). At the early stage of migration, the cells at the wound edge upregulate FN receptor, integrin α5β1, to migrate over temporary ECM rich in FN (Nishida et al., 1990; Murakami et al., 1992). Subsequently, laminin and collagen types I and IV appear under the newly resurfaced epithelium, as the FN staining gradually decreases (Nakayasu et al., 1986; Murakami et al. 1992; Ljubimov et al. 1998a). Lumican is another ECM component that is transiently expressed during tissue repair in murine corneal epithelium; its absence inhibits epithelial resurfacing in organ culture and delays epithelial wound healing in vivo (Saika et al., 2002).
During corneal epithelial wounding the BM may or may not be damaged. Central epithelial debridement wounds experimentally inflicted with a dull blade leave BM intact and may heal without BM remodeling, but may lead to subsequent erosions. Wounds that damage or remove epithelial BM (inflicted by a rotating burr, such as Algerbrush) heal without erosions, although they damage more nerves and cause more pronounced keratocyte apoptosis; however, fewer immune cells are attracted (Pal-Ghosh et al., 2011b). When healing of debridement wounds takes longer than 24 hours (this usually happens with large wounds), epithelial BM shows clear signs of disruption (Sta Iglesia and Stepp, 2000). It may be suggested that activation of BM degradation is a result of transient amplifying cells (TACs) activity that heal the wound from corneal periphery to the center by centripetal movement similar to standard epithelial renewal. As they appear to have a different BM composition (Ljubimov et al., 1995) than the central epithelium, TACs and their progeny may need to remodel central BM for proper movement and healing without erosions.
Recently, the roles of biophysical and topographic cues intrinsic to cell microenvironment, including topographically patterned BM, substratum stiffness, and electric fields have been demonstrated in wound healing processes (Abrams et al., 2000; Gao et al., 2015a), including adhesion (Karuri et al., 2004), migration (Liliensiek et al., 2006), and proliferation (Diehl et al., 2005).
Epithelial BM integrity is often compromised during wounding, which may have consequences for healing of the whole cornea, rather than of the epithelium only. In normal conditions, the epithelial BM is thought to control the availability of epithelium-derived growth factors and cytokines, such as TGF-β1 and PDGF, to stromal cells and/or, in the opposite direction, the stromal-derived growth factors, such as KGF, to epithelium. Injury to epithelial BM allows access of stromal cells to the epithelial cytokines and vice versa. This is thought to cause keratocyte apoptosis (see Section 3) by IL-1, and keratocyte to myofibroblast transformation due to TGF-β and PDGF access to stroma (Chaurasia et al., 2009; Singh et al., 2011). Declined levels of TGF-β1 and PDGF in stroma due to reassembly of the epithelial BM appear to lead to the apoptosis of stromal myofibroblasts, which are dependent on TGF-β1 for survival (Netto et al., 2006; Kaur et al., 2009a; Singh et al., 2011).
The role of BM in corneal epithelial cell function and wound healing may be also inferred from studies of corneal diseases, such as diabetic keratopathy that typically displays delayed healing (Fig. 3). Decreased immunostaining and expression of several major epithelial BM components and laminin receptor α3β1/VLA-3 integrin, possibly due to degradation, have been documented in the human and rodent diabetic corneas, and upon epithelial cell treatment with high glucose (Ljubimov et al., 1998a; 1998b; Saghizadeh et al., 2001; Fujita et al., 2003; Takamura et al., 2013). These changes correlated with impaired epithelial wound healing in diabetic corneas (Kabosova et al., 2003). Moreover, specific gene therapy that normalized diabetic wound healing also increased the expression of affected BM components and α3β1 integrin (Fig. 5) suggesting their involvement in epithelial healing after debridement (Saghizadeh et al., 2010a; 2013a). Overall, epithelial BM plays a significant role in corneal epithelial healing, and its remodeling appears to be essential for this process.
2.6. Sensory innervation in epithelial wound healing
The sensory nerve fibers that originate and derived from the ophthalmic branch of the trigeminal ganglion enter the cornea peripherally and terminate in numerous fine endings among the epithelial cells. The integrity of nerve fibers is crucial for normal corneal function by sensing thermal, mechanical, and chemical stimuli leading to the release of essential neurotrophins for corneal homeostasis and wound healing (Göbbels et al., 1989). The trophic effect of sensory nerves on corneal epithelial wound healing appears to be mediated by neuropeptides such as substance P contained in nerve terminals (Gallar et al., 1990). Depletion of neuropeptides from sensory nerve terminals induced by topical application of neurotoxin capsaicin delayed the healing rate of corneal wound in rabbit (Gallar et al., 1990). Corneal nerve regeneration stimulated by docosahexaenoic acid and PEDF (DHA + PEDF) after nerve damage led to enhanced epithelial wound healing, which was related to the production of neuroprotectin D1 (Cortina et al., 2012). Substance P (SP) is another neuropeptide released from terminal sensory nerve fibers that plays a major role in the maintenance of corneal epithelium homeostasis and diabetic epithelial wound healing through the interaction with neurokinin receptor-1 (NK-1) (Yang et al., 2014a). SP–NK-1 receptor signaling activates several signaling pathways that are needed for epithelial wound healing, such as EGFR-Akt, and Sirt1, rescuing hyperglycemia-impaired corneal sensation, improving mitochondrial function, and decreasing reactive oxygen species accumulation (Yang et al., 2014a). Corneal diseases, such as diabetic and neurotrophic keratopathies, are associated with impaired function of corneal nerves and epithelial breakdown with the consequence of delayed epithelial wound healing and corneal neurotrophic ulceration (Lambiase et al., 1999). Improving nerve health and regeneration upon wounding may constitute an effective therapy for corneal healing abnormalities associated with diabetes.
2.7. Immune system in epithelial wound healing
The major function of corneal epithelium is to protect the eye interior by serving as a physical and chemical barrier against infection by tight junctions and sustaining the integrity and visual clarity of cornea. Wounded, damaged or infected epithelial cells secret the cytokine, IL-1α, which is stored in epithelial cells and released when the cell membrane is damaged by external insults. Secreted IL-1α can cause increased immune infiltration of the cornea leading to neovascularization, which may result in visual loss. However, IL-1α antagonist, IL-1RN, prevents leucocyte invasion of the cornea and suppresses neovascularization, which may help preserve vision (Stapleton et al., 2008). IL-1RN gene transfer in a rat model of corneal transplantation was able to inhibit graft rejection through the downregulation of immune mediators (Yuan et al., 2013). In animal models, corneal epithelial wounding prompts an acute inflammatory response in the limbal blood vessels leading to accumulation of leukocytes and neutrophils (Li et al., 2007; Yamagami et al., 2005), and migration of dendritic cells, macrophages and lymphocytes (Jin et al., 2007; Li et al., 2007; Gao et al. 2011) into the stroma and the wounded epithelium. Current evidence indicates that the innate inflammatory responses are necessary for corneal epithelial wound healing and nerve recovery (Li et al., 2006a; 2007; 2011; Gao et al., 2011). Platelets also accumulate in the limbus and migrate to the stroma in response to wounded epithelium, which is necessary for efficient re-epithelialization through cell adhesion molecules such as P-selectin (Li et al., 2006b; Lam et al., 2011). In fact, in P-selectin null mice, platelet accumulation in limbus, neutrophil emigration into wounded epithelium, and corneal epithelial wound closure were significantly reduced (Li et al., 2006b). In addition, epithelial cell division and basal cell density were also reduced, probably due to the absence of neutrophils, which were present in wild type mice within 12-18 hours of epithelial injury, the peak timing for wound coverage (Li et al., 2006a). These data are in agreement with a major role of immune system cells such as neutrophils in corneal epithelial wound healing, which might be due to their ability to release growth factors that impact the epithelium (Li et al., 2006a; 2006b). Recently, natural killer cells were also shown to be involved in epithelial wound healing by limiting an inflammatory reaction to corneal wounding (Liu et al., 2012). It should be noted that most data on immune cell participation in corneal wound healing have been obtained on animal models, whereas the information about human corneas is scarce.
2.8. Limbal epithelial stem cells in wound healing
Corneal epithelium is constantly renewed by limbal epithelial stem cells (LESC) that in many species including humans exclusively reside in the corneoscleral junction, limbus. The basal limbal epithelial cells are a diverse population with a small number of LESC predominantly located in the palisades of Vogt (Goldberg and Bron, 1982), and/or in the deeper stromal limbal crypts connected to the limbal epithelium (Dua et al., 2005). The existence of stem cells in the limbus was suggested initially in 1971 by Davanger and Evensen. It was most recently corroborated by elegant application of inducible tagging technology in vivo using keratin 14 promoter, which is expressed predominantly in the limbus. This technique allows tracking individual limbal cells, presumably LESC, and their migration to the center of the cornea, in accordance with the LESC hypothesis (Amitai-Lange et al., 2015; Di Girolamo, 2015; Di Girolamo et al., 2015). Similar data were also obtained using LacZ reporter mice (West et al., 2015). The association of the corneal epithelial tumors only with limbus also supports the LESC concept (Lee and Hirst, 1995). LESCs have a lifetime capacity for self-renewal, and the ability to generate TACs, which appear to make up most of the basal epithelium in the limbus and peripheral cornea. They are thought to migrate into the central cornea, proliferate rapidly afterwards and eventually terminally differentiate into central corneal epithelial cells. This process takes place during corneal homeostasis and wound healing (Lehrer et al. 1998; Ahmad et al., 2010; Ordonez et al. 2012; Amitai-Lange et al., 2015; Di Girolamo et al. 2015; West et al., 2015). In order to localize and identify the stem cells, several ways have been adopted including colony-forming assay for their proliferative potential, DNA label (BrdU) retaining ability due to their slow cycling nature, the presence of specific surface antigens, the lack of terminal differentiation markers, and the presence of the specific stromal niche cells (Barak et al., 1980; Lavker and Sun, 1983; Espana et al., 2003; Sun and Lavker, 2004; Yoon et al., 2014). Genetic or acquired deficiencies of or damage to LESC result in a clinical condition called limbal stem cell deficiency (LSCD). It may lead to serious corneal problems such as altered corneal wound healing, stromal neovascularization and in-growth of conjunctival cells, and eventually, to corneal opacity and visual loss (Biber et al., 2010).
2.8.1. Limbal epithelial stem cell markers
Because of small numbers of LESC in the cornea and some technical problems with their definition (by DNA label retaining, clonogenicity, etc.) there is still no consensus of their specific markers, which hampers their studies in normal corneal maintenance and wound healing. There have been only isolated attempts to identify proteins expressed in BrdU-retaining corneal cells in vivo, but all these potential markers were also found to be expressed in many limbal epithelial cells (reviewed in Joe and Yeung, 2014; Yoon et al., 2014). This uncertainty necessitates the use of several “putative” markers together, the most popular being ΔNp63α, ABCG2, C/EBPδ, Bmi-1, K15, and Notch 1, with exclusion of differentiated epithelial keratins K3 and K12 (Joe and Yeung, 2014). Most recently, a promising new marker ABCB5 was identified, with potential role in LESC quiescence and wound healing, as suggested by knockout mouse experiments (Ksander et al., 2014).
2.8.2. Limbal stem cells in epithelial renewal and wound healing
During corneal epithelial maintenance LESC divide occasionally in order to replace cells lost by terminal differentiation and eventually desquamation (Lehrer et al., 1998; Pellegrini et al. 1999). However, in response to injury the proliferative rate increases 8- to 9-fold in the limbus and about 2-fold in peripheral and central regions, which then returns to basal levels after 36-48 hrs in the limbus and after wound closure in peripheral/central regions (Cotsarelis et al., 1989; Lavker et al., 1998; Lehrer et al., 1998). Therefore, in response to wounding, LESC undergo few cycles and give rise to many TACs with high migratory and proliferative capacity. Their properties and transient amplification would then be modulated during centripetal migration in the course of wound healing in response to the changes in ECM, integrin receptors, growth factors and cytokines (Power et al., 1995; Trosan et al., 2012).
The essential role of LESC in wound healing is supported by a number of studies (Chen and Tseng, 1990; Tsai et al., 1990; Dua, 1998; Castro-Muñozledo, 2013; Amitai-Lange et al., 2015). When limbal cells are damaged or absent, wound healing in the cornea is altered or does not occur (Chen et al., 1990). Deficiencies of or damage to LESC result in partial or total LSCD. This leads to serious corneal problems, such as delayed wound healing, stromal neovascularization and ingrowth of conjunctival cells, which may cause corneal opacity and visual loss (Chen and Tseng, 1990; Lim et al., 2009). Limbal transplantation is able to restore wound healing (Tsai et al., 1990) and epithelial resurfacing of the entire corneal epithelium, and removal of the central epithelium leads to complete wound repopulation by limbal cells (Kenyon and Tseng, 1989; Chen and Tseng, 1990; Chung et al., 1995). It should be noted that central corneal cells significantly contribute to healing of small wounds, but large wounds show limbal cell involvement, although it may be delayed for several days (Amitai-Lange et al., 2015).
Signals triggering LESC-TAC activation, proliferation, and migration into the wound are not fully understood. It has been suggested that certain growth factors and cytokines (including those secreted by immigrating inflammatory cells), as well as chemotactic molecules including products of ECM degradation contribute to healing signals. Upon damage to the corneal epithelium, limbal fibroblasts markedly upregulate KGF expression and limbal epithelial cells show elevated expression of its receptor, suggesting the prominent role of KGF in limbal activation for wound healing (Wilson et al., 1999). CNTF, a well-known neuroprotective cytokine, has been shown recently to play a role in the activation of limbal epithelial stem/progenitor cells and wound healing of both normal and diabetic mouse corneal epithelium. Exogenous CNTF application enhanced wound healing by initiating of LESC activation, while its neutralizing antibody delayed healing (Zhou et al., 2015). Similar effects on epithelial healing were observed using FGF-2 eye drops in patients after photorefractive keratectomy (Meduri et al., 2012). We have observed that human diabetic corneas have upregulation of HGF but downregulation of its receptor c-met. These corneas also display delayed wound healing and markedly decreased expression of several putative LESC markers (Saghizadeh et al. 2011). Specific gene therapy to restore c-met levels normalized LESC marker expression in human diabetic organ-cultured corneas as well as wound healing (Saghizadeh et al., 2011; 2014). These data point to the importance of HGF–c-met signaling in LESC function and epithelial healing. In addition, gene therapy of limbal cells only produced similar effects, attesting to the major role of LESC in epithelial wound healing (Saghizadeh et al., 2014). Similar beneficial effects on diabetic corneal wound healing and LESC marker expression were observed upon shRNA-mediated inhibition of specific proteinases, MMP-10 and cathepsin F, that are upregulated in diabetic corneas (Saghizadeh et al., 2014). It remains to be established whether these effects were due to normalization of epithelial BM remodeling or to the concomitant activation of wound healing promoting EGFR-Akt signaling.
2.9. MicroRNAs in epithelial wound healing
MicroRNAs (miRNA) are small non-coding RNAs that can specifically bind to complementary sequences on 3′UTR of target mRNAs. If the sequence match is complete, the mRNA is slated for degradation; with a partial match, its function is inhibited. Overall, miRNA action usually results in gene silencing (Humphreys et al., 2005; Chendrimada et al., 2007). MiRNAs are natural and powerful gene expression regulators, and key mediators of basic biological processes in the organism including eye tissues (Li and Piatigorsky, 2009; Li et al., 2010). At the same time, their effects may not be easy to interpret because many miRNAs have more than one target (Bertero et al., 2011). Even if the primary target with complete sequence match with miRNA is identified, other proteins could also be affected by this miRNA or its inhibitor (antagomir). MiRNA effects may also be cell type-specific.
In the cornea, some miRNAs display topographical expression differences between central part, limbus, and adjacent conjunctiva (Xu, 2009; Karali et al., 2010; Saghizadeh et al., 2013a; Peng et al., 2015; Teng et al., 2015). Interestingly, several miRNAs with preferential limbal epithelial localization appear to play a role in delayed wound healing in diabetic corneas (Funari et al., 2013; Saghizadeh et al., 2013b; Winkler et al., 2014). The emerging evidence suggests the importance of miRNAs in many phases of corneal epithelial wound healing process, where some miRNAs promote healing, but others inhibit it (Funari et al., 2013; Lin et al., 2013; Winkler et al., 2014; An et al., 2015; Gao et al., 2015b). During migration and proliferation of corneal epithelial cells at the wound edge, upregulated miR-205 targets SH2-containing phosphoinositide-5-phosphatase (SHIP2), which in turn affects Akt signaling pathway and increases epithelial migration (Yu et al., 2010a). The upregulated miR-205 can additionally promote motility of epithelial cells through modification of F-actin organization (Yu et al., 2010a). It has been further shown that miR-205 facilitates wound healing process through inhibition of another target gene, KCNJ10 channel, in human corneal epithelial cells (Lin et al., 2013a). In skin keratinocytes, growth arrest at the final steps of re-epithelialization is regulated by miR-483-3p by acting on MK2 kinase and transcription factor YAP1 (Bertero et al., 2011).
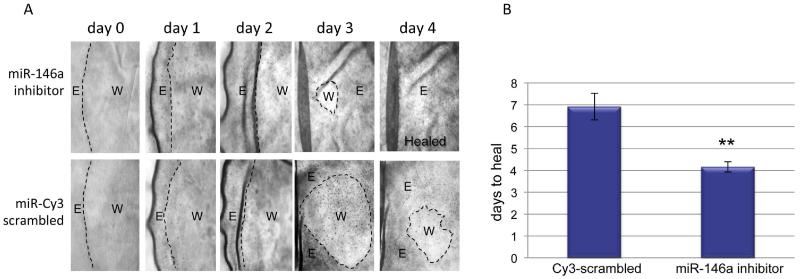
Several miRNAs appear to be responsible for delayed diabetic wound healing. MiR-146b and miR-21 have been implicated in altered wound healing in skin of diabetic mice (Madhyastha et al., 2012). MiR-204, which targets SIRT1 gene, was shown to impair cell cycle traverse of corneal epithelial cells in DM2 diabetic Akita mice (Gao et al., 2015b) and to inhibit cell migration (An et al., 2015). We have identified miR-146a and miR-424 as regulators of corneal epithelial wound healing (Funari et al., 2013). MiR-146a plays a major role as a modulator of the innate immune and inflammatory responses, and wound inflammation, and may repress proinflammatory genes within the wound (Roy and Sen, 2011; Xu et al., 2012a). It also inhibits cell migration by targeting EGFR and other signaling molecules such as IRAK1 and NF-κB (Kogo et al. 2011; Xu et al. 2012b; Chen et al. 2013; Funari et al. 2013). Both miR-146a and miR-424 suppressed, and conversely, their inhibitors enhanced, wound healing in transfected telomerase-immortalized HCEC in vitro. In cells transfected with miR-146a or miR-424 antagomir inhibitors, both EGFR and p38 were activated during wound closure. The mir-146a antagomir also enhanced wound healing (Fig. 6) in human diabetic organ-cultured corneas (Winkler et al. 2014). MiR-146a inhibited not only EGFR activation but also reduced the amount of total EGFR, which is its direct target (Funari et al. 2013). These recent data attest to the significance of miRNAs in regulating corneal wound closure, and provide novel insights into mechanisms of the wound healing process. Further investigations of their targets and affected pathways would help us understand normal epithelial healing, and its dysregulation in chronic wounds and diseased corneas.
Figure 6.
Wound healing in miR-146a inhibitor transfected human diabetic organ-cultured corneas. A. Transfection with miR-146a inhibitor enhanced wound healing compared to control transfected with labeled scrambled miR-Cy3. Transfected diabetic organ-cultured cornea with miR-146a inhibitor, upper row; with miR-Cy3-scrambled control, lower row. E, epithelium; W, wounded area. B. Quantitation of wound healing rates. The bar graph represents average ± SEM of pooled values (n=6) of days to heal. ** p<0.001 by paired two-tailed t test. Reproduced from Winkler et al., 2014.
2.10. Therapeutic approaches to enhance or normalize epithelial wound healing
2.10.1. Gene therapy
Gene therapy has a clear potential for treating human corneal diseases. Corneal immune-privileged nature and easy accessibility make it an easy target for gene therapy (Mohan et al., 2003; Liu et al., 2008). Gene delivery can be monitored visually by tagging a fluorescent protein to the target gene, and gene therapy reagents can be applied topically to the corneal surface. The major advantage is that the cornea can be maintained for several weeks in ex vivo organ culture, which allows us to improve the efficacy and safety of gene therapy by optimizing gene transfer. Here we will consider recent work on transgene delivery systems to the cornea in various in vivo and in vitro model systems.
2.10.1.1. Viral gene therapy
In recent years, viral gene therapy has been successfully applied for delivering specific genes into cornea producing rapid, high-level, expression of the target gene. Recombinant adenoviruses (rAV), adeno-associated viruses (rAAV), and lentiviruses are the major classes of viral vectors commonly used to transfect the cornea. The choice of viral vector depends on specific cell targeting, desired expression level, development of immune reactions, and choice of temporary vs. long-term expression of the target gene. Both rAV and rAAV can successfully deliver genes of interest into human corneas. rAAV appears to reach all three layers of corneal cells, epithelial, stromal and endothelial cells (Mohan et al. 2003; Liu et al., 2008). rAV transduction was seen only in epithelial and endothelial cells, and with considerably higher expression level of the green fluorescent protein (GFP) reporter than with rAAV transduction (Liu et al. 2008). Different rAAV serotype vectors also transduced corneal cells in rabbit corneas as well as human organ-cultured corneas to a different extent (Mohan et al., 2003, 2005; Liu et al., 2008; Buss, 2010). Our studies showed that rAAV1 and rAAV8 produced higher GFP staining intensities than rAAV2, rAAV5, and rAAV7 (Liu et al., 2008).
It is well established that diabetic corneas have slow wound healing. We have, therefore, used rAV-driven gene therapy to elucidate the functional role of several abnormally expressed target genes in wound healing of organ-cultured human diabetic corneas (Saghizadeh et al., 2010a; 2010b; 2011; 2013a; 2014). Central and limbal cells in these corneas were transduced with c-met gene to increase its expression, and/or shRNA to diabetes-upregulated MMP-10 and cathepsin F genes to decrease their expression (Saghizadeh et al., 2010a; 2010b; 2011; 2014). Transduction led to effective normalization of diabetic and stem cell marker patterns, as well as wound healing rates. This effect was also observed when only limbal cells were transduced before wounding the corneas (Saghizadeh et al., 2014). Several pathways including EGFR-Akt and p38 MAP kinase were suggested as gene therapy mechanisms. rAV-driven vasohibin-1 expression upon subconjunctival injection was also effective in inhibiting neovascularization upon mouse corneal alkaline burn (Zhou et al., 2010).
Corneal epithelial and endothelial cells have been also successfully transfected with lentiviral vectors for gene therapy purposes (Oliveira et al., 2010; Parker et al., 2010). These vectors can ensure long-term expression because of their integration into the host genome, but their random integration might result in side effects (Follenzi et al., 2007; Li and Huang, 2007). It remains to be established whether they would be useful for restoring abnormal wound healing in disease conditions. In this respect, transient transduction, e.g., with rAV or rAAV vectors could be preferable in order to provide wound healing enhancement, which may need to be only temporary.
2.10.1.2. Nanocarrier-based gene therapy
Nanotechnology is currently an area of great interest in ophthalmology due to a wide variety of potential applications in drug and gene delivery into the eye. Although viral-based therapies usually have better transduction efficiencies than nanocarriers (mostly represented by nanoparticles, NPs), the latter are relatively easy to synthesize and manipulate, have low production costs, can accommodate large size vectors, do not induce inflammatory responses, pose no risk of genomic insertion and mutation, and are amenable to targeting (Han et al. 2011; 2012). There are several types of NPs including metal-, lipid-, and polymer-based systems. They are different in size, charge, and structure but are all able to enter the cells, while avoiding the endosomes, and transfer the vector into the nucleus for gene expression (Adijanto and Naash, 2015). NPs allow combining several different plasmids in one particle to increase transgene expression (Klausner et al., 2010). The data on the use of NPs for corneal wound healing therapy are emerging. Inorganically-coated all-trans retinoic acid NPs have shown promise in enhancing corneal epithelial wound healing in cultured cells and a rabbit wound model (Hattori et al., 2012). Popular poly (lactide-co-glycolide) NPs loaded with antifibrotic drug pirfenidone also increased corneal re-epithelialization, as well as reduced collagen synthesis and prevented myofibroblast formation in a rabbit alkaline burn model (Chowdhury et al., 2013). Elastin-like polypeptide-based NPs bearing a mitogenic protein lacritin promoted corneal epithelial wound healing in non-obese diabetic mice (Wang et al., 2014). Overall, nanocarrier technologies have a potential for effective drug delivery and gene transfer for therapeutic approaches including wound healing promotion (Williams and Klebe, 2012), and their use may be expanded in the near future. At the same time, some industrially relevant engineered inorganic and organic NPs were shown to be toxic for corneal cells calling for proper toxicology studies (Zhou et al., 2014).
2.10.2. MicroRNA therapy
MiRNA therapy may either increase natural miRNAs that are underexpressed in cells using miRNA mimics or inhibit their expression with respective antagomirs when they are overexpressed. MiRNAs are known to have multi-targeted pattern of regulating many different genes across multiple pathways simultaneously, in contrast to other targeted therapies that affect only one or two genes or pathways. For instance, intravenous administration of miR-122 antagomir resulted in reduced level in plasma cholesterol by targeting simultaneously a number of cholesterol biosynthesis genes in mice and non-human primates (Elmen et al., 2008a, 2008b; Krützfeldt et al., 2005). This property may be advantageous in some cases, but may have unwanted or unpredictable side effects in others, calling for caution in using miRNAs for treatment.
The use of miRNA mimics or antagomirs is being investigated for therapeutic modulation of miRNAs in cancer (Huang et al., 2014), chronic inflammatory diseases (Worm et al., 2009), hepatitis C (Janssen et al., 2013), and herpetic stromal keratitis (Mulik et al., 2013). Studies in mice have demonstrated that antagomirs are efficient and specific silencers of endogenous miRNAs decreasing their levels in many organs (Krützfeldt et al., 2005). Since wound healing is a complex process involving a number of sequential and parallel pathways, miRNA multi-target regulation seems to be an attractive approach to mediating several processes simultaneously for treatment of healing problems in pathological conditions. We have recently applied antagomir-based therapy for successful normalization of epithelial wound healing alterations in human diabetic organ-cultured corneas. Treatment of diabetic organ-cultured cornea with miR-146a antagomir significantly enhanced cell migration, accompanied by increased phosphorylation of signaling intermediates EGFR and p38 (Funari et al., 2013; Winkler et al., 2014). Manipulating miRNA levels may provide a novel therapeutic tool for regulating corneal wound healing, as well as epithelial homeostasis and stem cell maintenance.
2.10.3. Stem cell therapy
The therapeutic use of LESC currently comprises an extremely dynamic area of research and clinical applications. LESC dysfunction or loss (LSCD) occurs in a wide variety of pathological conditions leading to abnormal epithelial self-renewal including hereditary disorders (e.g., aniridia or Stevens Johnson syndrome), autoimmune diseases, infections, inflammations, burns or diabetes (Daniels et al., 2006; Pellegrini et al., 2009; 2011; Rama et al., 2010; Saghizadeh et al., 2011; Hsu et al., 2014; Joe and Yeung, 2014). Loss (in LSCD) or dysfunction (in diabetes) of LESC causes alterations in epithelial renewal and thus, compromises wound healing as well. Therefore, restoration of LESC numbers and/or functions by transplantation or other approaches also normalizes the wound healing process including re-epithelialization after injuries (Tsai et al., 2000; Saghizadeh et al., 2011; 2014; Pellegrini et al., 2014).
Keratolimbal biopsy-based autografts for unilateral or allografts for bilateral LSCD are in clinical use for a number of years with about 30-45% success and 3-5-year graft survival (Kenyon and Tseng, 1989; Baylis et al., 2011). Both methods have drawbacks including sample limitation and possible damage at the autograft donor site or the risk of long-term immunosuppression in allograft therapy (Pellegrini et al., 1997; Liang et al., 2009). To circumvent these problems, ex vivo expansion of autologous and allogeneic LESC in culture was developed (Pellegrini et al., 1997) generating an epithelial cell sheet for transplanting onto the damaged eye of the patient. Human amniotic membrane (HAM), collagen shields, fibrin glue, denuded anterior lens capsule and temperature sensitive biopolymers with or without feeder cells have been used as supports for in vitro expansion of LESC for subsequent grafting onto the damaged eye, with an average 1-3 years success rate of up to 76% (Galal et al., 2007; Levis and Daniel 2009; Ahmad et al., 2010; Rama et al. 2010; Baylis et al. 2011; Vazirani et al., 2014). Recent efforts were focused on developing xenobiotic-free LESC cultures with no feeder cells or with human cells. Human autologous serum has been used to expand LESC on HAM (Shahdadfar et al., 2012) or on soft contact lenses (Bobba et al., 2015). The latter technique has been used in a clinical trial in 16 LSCD patients with reported success in 10 of 16 eyes (63%) at a median follow-up time of 2.5 years with the advantage of autologous transplantation (Bobba et al., 2015).
However, LESC can only be passaged several times in vitro (Shanmuganathan et al., 2006). Other drawbacks include relative low allograft survival, and potential contamination from still widely used mouse 3T3 cell feeder cells (Tseng et al., 2010). Therefore, attempts were made to substitute LESC with other stem cells, which would be especially advantageous in cases of total LSCD. One alternative source of autologous stem cell-based therapy is cultivated oral mucosal epithelium, which has shown up to 80% vision improvement after 1-2 years in a few clinical trials (Nakamura et al., 2011; Kolli et al., 2014; Sotozono et al., 2014). However, it often entails peripheral corneal neovascularization (Chen et al., 2012). Besides oral mucosa, conjunctival and epidermal epithelium, hair follicle, corneal epithelium-like cells differentiated from embryonic stem cells, etc. were tried as alternative sources of autologous stem cell-based therapy for corneal diseases and wound healing (Ono et al. 2007; Yang et al., 2008; Kumagai et al., 2010; Meyer-Blazejewska, et al. 2011; Yan et al., 2014). Adipose-derived, orbital fat-derived, and immature dental pulp stem cells have been used for successful re-epithelialization of chemically burned cornea (Monteiro et al., 2009; Lin et al., 2013b; Zeppieri et al., 2013). Additionally, mesenchymal stem cells (MSCs) were also considered as a source of corneal cells to treat burns and LSCD (Ma et al., 2006; Reinshagen et al., 2011; Pinarli et al., 2014). Interestingly, following the induction of epithelial corneal injury in mice by thermal cauterization, systemically administered MSCs homed to the injured epithelium causing its rapid regeneration (Lan et al., 2012).
The success of making lineage-specific differentiated cells from embryonic stem cells (ESC) or induced pluripotent stem cells (iPSC) (Aberdam et al., 2008; Noisa et al., 2012; Yamanaka, 2012) may lead to creation of other bankable and renewable sources of LESC for future transplantation needs. Both limbal- and fibroblast-derived iPSCs were generated and directed to limbal differentiation (Hayashi et al., 2012; Yu et al., 2013; Sareen et al., 2014; Casaroli-Marano et al., 2015). Since iPSCs are easily expandable, they are considered as an unlimited and renewable cell source. The present hurdle relates to optimization of their direct differentiation on optimal substrata with optimal factors/cytokines to the limbal cells and further to the stratified corneal cells. To date, several strategies have been developed to differentiate ESC/iPSC into limbal epithelial cells both in mouse and human (Casaroli-Marano et al., 2015). These techniques include using feeder cells (Aberdam et al., 2008), embryoid bodies (Bilousova et al., 2010), and stromal cell-derived inducing activity (SDIA) culture method (Sakurai et al., 2011; Yoshida et al., 2011). To date, protocols for making corneal epithelium from stem cells are not fully optimized. Our approach was to use natural substrata mimicking the native LESC niche, including feeder-less denuded HAM and de-epithelialized corneas, to direct iPSC to limbal differentiation. As a result, iPSC were differentiated into cells expressing a number of LESC markers (Sareen et al., 2014), and this protocol is being further tested and refined. The most promising approach to achieve reliable limbal epithelial differentiation may combine specific soluble factors given for select time periods, and the right extracellular niche. Recently, iPSCs were generated from mouse conjunctival cells (Yang et al., 2014b). Such cells may be readily obtained during ophthalmic surgeries or conjunctival biopsies and may constitute another source of limbal progenitor cells for autologous transplantation.
2.11. Concluding remarks
In the last decade there was a significant progress in the studies of corneal epithelial wound healing. Many signaling pathways responsible for healing stimulation, as well as their cross-talk have been unraveled. The feasibility of gene therapy for wound healing abnormalities has been demonstrated, along with the role of miRNA in the healing process. The limbal stem cell niche hypothesis has been verified by solid experimental data and new putative LESC markers have been described. New approaches for LESC transplantation have been worked out including xenobiotic-free culturing, and these cells are now used in several countries for efficiently fighting LSCD and various corneal injuries, with successful re-epithelialization. New sources for LESC replacement have been proposed and are being tested in animal models and in patients. There are still some unanswered questions and translational issues related to only partial knowledge of mechanisms of the complex wound healing process. Given the existence of signaling cross-talk among various effectors of epithelial healing, it may be advantageous to recur to combination therapies for acceleration of this process, but these studies are relatively scarce. The mechanisms of miRNA participation in wound healing are only beginning to be unraveled. Targeted drug delivery to stem cells is feasible (Chen et al., 2006) but is hampered by lack of fully specific LESC markers and by relative paucity of delivery vehicles including nanocarriers. There is still a significant problem with autologous LESC transplantation in severe burns and bilateral LSCD, and no ideal cell substitute has been proposed yet. Overall, recent identification of new players in the healing process, such as miRNA, and introduction of new technologies, including gene therapy, nanocarriers, new small molecule drugs, such as ROCK inhibitor, and renewable iPSC for LESC transplantation, may provide a boost for mechanistic studies of epithelial wound healing and for the development of optimized and streamlined xenobiotic-free treatments for various corneal wounds and autologous LESC replacement.
3. Corneal stromal wound healing
Corneal stromal wounds occur relatively often. They may result from traumas and various refractive surgeries meant to correct abnormal eyesight, e.g., myopia or hyperopia. These surgeries range from older radial keratotomy invented in the 1950’s and refined and propagated in the 1970′ by Fyodorov’s school, to photorefractive keratectomy (PRK), to modern and widespread laser in situ keratomileusis (LASIK), to the recent use of less damaging femtosecond lasers. In the United States alone about 700,000 LASIK surgeries are performed annually. Although most cases are uneventful, some patients develop complications of wound healing related to the formation of stromal haze with reduced corneal transparency after PRK, or related to flap detachment or failure with possible ectasia after LASIK. In many tissues, e.g., in skin fibrotic scar formation as a result of wound healing would not significantly affect tissue function. However, such scars can reduce corneal transparency and compromise vision. Upon proper healing, the corneal stroma gets remodeled fairly precisely, with its orderly arrays of collagen lamellae ensuring transparency and lack of vascularization (Fini and Stramer, 2005). Therefore, studies of stromal wound healing, its mechanisms and ways to prevent fibrotic and neovascular complications have enormous clinical significance.
It should be noted that stromal remodeling occurs not only upon direct damage to the stroma and its cells as exemplified by PRK and LASIK. The remodeling also happens upon death of stromal cells (keratocytes) caused by damage to or removal of corneal epithelium by various physical or chemical factors (Nakayasu, 1988; Szerenyi et al., 1994; Wilson et al., 1996; 2001; 2007). Such damage triggers a release of inflammatory cytokines from epithelial cells and/or tears (Maycock and Marshall, 2014), mainly IL-1 (α and β), that cause rapid apoptosis through Fas/Fas ligand system and later, necrosis of mainly anterior keratocytes. Interestingly, these cells die preferentially directly beneath the epithelial wounds, rather than also beyond their edges. This may argue against a diffusible factor as the main reason for cell depletion. Alternative mechanisms have not been explored and may include severance of intraepithelial nerves that may supply factors maintaining keratocytes’ health (Dr. Daniel Gibson, University of Florida, personal communication). The following stromal remodeling with replenishment of these cells from the areas adjacent to the depleted one (Zieske et al., 2001), also constitutes a wound healing process and may result in fibrotic changes, especially if the epithelial basement membrane was initially damaged (Stramer et al., 2003; Fini and Stramer, 2005; West-Mays and Dwivedi, 2006). This is a classical example of how stromal-epithelial interactions influence wound healing process by paracrine mediators.
3.1. Keratocyte conversion to fibroblasts and myofibroblasts during wound healing
Regulated changes of stromal cell phenotypes during wound healing (Fig. 2) have been a subject of a number of studies and excellent in-depth reviews; therefore, these will be only briefly reviewed here because they are important for the understanding of the whole stromal wound healing process. At the early stage of wound repair quiescent keratocytes at the wound edges change their properties to become activated to fibroblasts. These cells enter the cell cycle and acquire migratory properties necessary to repopulate and close the wound (West-Mays and Dwivedi, 2006). In culture, this transformation is mediated by some (FGF-2 and PDGF-AB, TGF-β) growth factors, whereas others (IL-1, IGF-1) only confer mitogenic activity (Jester and Ho-Cheng, 2003; Chen et al., 2009a). These cells remodel their actin cytoskeleton to acquire stress fibers and change their morphology from stellate to elongated one (Jester and Ho-Cheng, 2003). Fibroblasts downregulate the expression of differentiated keratocyte proteins, such as corneal crystallins (transketolase and aldehyde dehydrogenase 1A1), and keratan sulfate proteoglycans, and start producing proteinases (mostly MMPs), needed to remodel the wound ECM (Fini, 1999; Jester et al., 1999; Carlson et al., 2003; West-Mays and Dwivedi, 2006).
After they reach the wound bed, fibroblasts start expressing α-smooth muscle actin (α-SMA) and desmin, upregulate the expression of vimentin (Chaurasia et al., 2009), and become highly motile and contractile myofibroblasts needed to remodel wound ECM and contract the wound (Fig. 2). They also deposit provisional ECM rich in fibronectin and some other proteins including tenascin-C and type III collagen (Tervo et al., 1991; Fini, 1999). Myofibroblasts generate contractile forces to close the wound gap, and the expression of α-SMA directly correlates with corneal wound contraction (Jester et al., 1995). When the wound does not really contract as in the case of PRK or phototherapeutic keratectomy (PTK), the appearance of myofibroblasts is delayed, and they start accumulating as late as four weeks after irregular PTK (Barbosa et al., 2010). At least in this setting in a mouse model, the majority of myofibroblasts form not from activated corneal fibroblasts but from the immigrating bone marrow cells, as shown by adoptive transfer of green fluorescent protein (GFP)-labeled bone marrow (Barbosa et al., 2010). It is presently unclear whether massive participation of circulating cells in stromal myofibroblast formation also occurs in other species and in fast healing wounds.
It is generally accepted that myofibroblast transformation is triggered by TGF-β in vivo, which has been confirmed by numerous studies in vitro (Jester et al., 1999). More recent work has also implicated a potent mitogen, PDGF (both AA and BB) in this process, with a combination of TGF-β and PDGF being more potent than either factor alone (Kaur et al., 2009b; Singh et al., 2014). It should be noted that only TGF-β1 and TGF-β2 are active in this process, whereas TGF-β3 does not transform fibroblasts to myofibroblasts (Karamichos et al., 2011; 2014b). Interestingly, some data indicate that repopulation of keratocytes after epithelial debridement of mouse corneas occurs without the appearance of myofibroblasts (Matsuba et al., 2011), possibly through stimulation of keratocyte migration by aquaporin-1 water channel (Ruiz-Ederra and Verkman, 2009). Upon completion of wound healing, myofibroblasts apparently cease to express α-SMA. Their fate in vivo is not completely clear, although it was suggested that they might die by apoptosis and/or become scar keratocytes. Such cells are observed months after the wound has healed, and they are different from quiescent keratocytes by expressing some MMPs similar to fibroblasts (Fini, 1999). It remains unknown what signals trigger myofibroblast disappearance and healing completion. One hypothesis is that contact inhibition of proliferation would signal these cells to stop remodeling the wound.
Although myofibroblast appearance is widely considered as a necessary part of stromal wound healing, one should exert caution in using this marker in animal models of corneal injury. Recent data show that the numbers of myofibroblasts in the corneal stroma after PRK differ widely among various mouse strains (Singh et al., 2013).
3.2. Participation of immune system cells in stromal healing
Corneal injury in animal models entails an inflammatory response by immune system cells. They may include monocytes/macrophages, T cells, polymorphonuclear (PMN) leukocytes and natural killer (NK) cells (Gan et al., 1999; Wilson et al., 2001; 2004; Liu et al., 2012; Li et al., 2013). These infiltrating cells are usually defined by staining for CD11b, although in some studies a better characterization of these cells is provided (Wilson et al., 2001; Liu et al., 2012; Li et al., 2013). Immune cells may come to the injured cornea from the limbal area or mobilized from circulation (Wilson et al., 2001). A major attracting signal for such cells may be monocyte chemotactic protein-1 (MCP-1). This cytokine can be secreted by activated fibroblasts and triggered by IL-1 or TNF-α (Wilson et al., 2001). Another factor required for neutrophil influx following injury was identified as a stromal proteoglycan lumican (Hayashi et al., 2010). It is still unclear what are the magnitude, infiltrating cell repertoire and origin, as well as kinetics of the immune response to corneal injury in humans. A recent study identified increased numbers of CD11b-positive monocytes in the stroma following corneal incisions in an organ culture system (Mayer et al., 2014). Understandably, this study could only take into account the cells locally recruited from the limbus. Further characterization of these cells using human material would be important.
Functions of immune cells infiltrating injured corneas may be diverse. They may scavenge remnants of apoptotic keratocytes and protect the cornea from possible infection (Wilson et al., 2001). Some of these cells may become myofibroblasts (Barbosa et al., 2010) and thus participate in the wound contraction. Direct involvement of immune cells in the wound healing has been also suggested from recent studies. Blocking PMN entry into cornea by fucoidin (inhibitor of leucocyte adhesion to vascular endothelium) delayed wound healing after PRK in rabbits (Gan et al., 1999). Functional blocking of NK cells after epithelial abrasion and keratocyte loss inhibited healing and nerve regeneration (Liu et al., 2012). Macrophage depletion impaired wound healing after autologous corneal transplantation, with a decrease in wound myofibroblasts (Li et al., 2013). These studies emphasize the importance of local and systemic immunity in corneal wound healing, both epithelial and stromal.
3.3. Remodeling of stromal ECM during wound healing
As described in the previous sections, stromal wound healing is accompanied by several events that may be responsible for ECM changes in this location: death of keratocytes, secretion of proinflammatory and profibrotic cytokines including IL-1, TNF-α, and MCP-1, transient appearance of cells that do not normally form the stroma (PMNs, macrophages, myofibroblasts), and production of ECM-degrading enzymes by activated cells. All these factors contribute to ECM remodeling including its degradation, expression of ectopic components (provisional matrix formation by new cell types), and reassembly of the new ECM to form a more or less normal structure (reviewed in Zieske, 2001; Torricelli and Wilson, 2014). As a result, new ECM formed during wound healing often accumulates aberrant proteins, both in composition and structure. Over time, these proteins may form local scars persisting for a long time (Ishizaki et al., 1993; 1997; Maguen et al., 1997; Ljubimov et al., 1998; Maguen et al., 2002; 2007; Kato et al., 2003; Kamma-Lorger et al., 2009; Torricelli and Wilson, 2014). Because of slow turnover of ECM proteins, the unusual scar components may still be present around the healed wounds for years, especially in human corneas (Latvala et al., 1995a; Ljubimov et al., 1997; Alba et al., 1998; Maguen et al., 2002; 2007; 2008). These components, which are normally scarce in or absent from adult corneal stroma include type III, VIII, XIV, and XVIII collagen, limbal isoforms of type IV collagen, embryonic fibronectin isoforms, TSP-1, tenascin-C, fibrillin-1, and hevin (Saika et al., 1993; Melles et al., 1995; Nickeleit et al., 1996; Ishizaki et al., 1997; Maguen et al., 1997; Ljubimov et al., 1998; Zieske, 2001; Maguen et al., 2002; 2007; 2008; Kato et al., 2003; Javier et al., 2006; Matsuba et al., 2011; Chaurasia et al., 2013; Saika et al., 2013).
Although it is generally accepted that ECM components in the healing wounds may mostly serve structural functions, gene knockout experiments have suggested a deeper regulatory role of some of these proteins. One such component is glycophosphoprotein osteopontin that is also a cytokine modulating cell proliferation and macrophage activities. Osteopontin-null mice have delayed healing of incisional wounds, with less myofibroblasts and macrophages, and diminished expression of fibrogenic TGF-β1 (Miyazaki et al., 2008; Saika et al., 2013). Very similar changes were observed in wounded corneas of tenascin-C null mice (Sumioka et al., 2012; Saika et al., 2013). In case of TSP-1 that co-localizes with myofibroblasts in the healing stroma following incisional wounds (Matsuba et al., 2011), the changes in the healing process are even more pronounced when the respective gene is knocked out. TSP-1 null corneas remained edematous and non-transparent upon wounding and the wound could not contract, apparently due to great reduction in the numbers of myofibroblasts (Blanco-Mezquita et al., 2013). In this respect, it would be interesting to examine whether recruitment of bone marrow cells to the injured corneas would be also impaired in knockout animals.
3.4. Signaling pathways associated with stromal wound healing process
In order to pharmacologically control unwanted effects of wound healing process, e.g., fibrosis, that may lead to scar formation and decreased transparency, it is important to understand what growth factors and cytokines are involved at various stages of this process and what signaling intermediates are key to healing events. Keratocyte activation to fibroblasts is mediated by FGF-2, TGF-β, and PDGF, and their proliferation, by EGF, HGF, KGF, PDGF, IL-1 and IGF-I (Stern et al., 1995; Baldwin and Marshall, 2002; Jester and Ho-Cheng, 2003; Carrington and Boulton, 2005; Chen et al., 2009a). Although TGF-β is key to fibroblast to myofibroblast transformation, it actually inhibits keratocyte proliferation and migration (reviewed in Baldwin and Marshall, 2002). Stromal cellular infiltration upon injury was found to be stimulated by such cytokines as MCP-1 and platelet-activating factor (PAF) (Wilson et al., 2001; Kakazu et al., 2012). As noted above, TGF-β isoforms 1 and 2 (Torricelli and Wilson, 2014), as well as BMP-1 (Malecaze et al., 2014) may be responsible for the myofibroblast emergence, wound contraction and fibrotic scar formation. TGF-β also promotes deposition of excessive ECM in the wound bed that may result in scar formation. It can do it directly, as well as by stimulating production of other factors including connective tissue growth factor (CTGF) and IGF-I (Izumi et al., 2006; Shi et al., 2012; Karamichos et al., 2014b; Torricelli and Wilson, 2014). Therefore, attenuation of TGF-β expression and signaling may provide means to counteract fibrotic changes. For instance, topical rosiglitazone, ligand of peroxisome proliferator activated receptor γ (PPAR-γ) reduced α-SMA expression and scarring in cat corneas upon excimer laser ablation of anterior stroma without compromising wound healing. In corneal fibroblast cultures, it also counteracted TGF-β induced myofibroblast transformation (Huxlin et al., 2013). Similar effects were seen with neutralizing antibody to TGF-β (Møller-Pedersen et al., 1998). Inhibition of JNK signaling suppressed TGF-β induced CTGF expression and scarring in penetrating corneal wounds (Shi et al., 2012). Inhibitors of mTOR and p38 MAP kinase signaling were able to markedly reduce the expression of α-SMA and collagenase in corneal cells and injured corneas (Jung et al., 2007; Huh et al., 2009; Milani et al., 2013). In alkali-burned corneas, blocking of VEGF by neutralizing antibody bevacizumab also inhibited TGF-β expression and improved corneal transparency (Lee et al., 2009). With the widespread use of refractive surgeries, novel anti-TGF-β treatments such as approved for human use rosiglitazone (Huxlin et al., 2013), ROCK inhibitor (Chen et al., 2009a) or trichostatin A (Sharma et al., 2009) may become part of routine pharmacological management of wound healing.
3.5. Stromal wound healing complications upon refractive surgery
In most cases of PRK or LASIK or other corneal refractive surgeries the patients acquire better vision and the healing process does not present complications. However, there have been quite a few reports of lasting corneal opacity due stromal haze (thought to be a result of excessive stromal matrix accumulated during healing and/or persistence of residual wound healing cells) or corneal decompensation compromising vision and even requiring corneal transplantations in severe cases (Møller-Pedersen et al., 2000; Netto et al., 2005; 2006; Tomás-Juan et al., 2015).
3.5.1. Photorefractive keratectomy (PRK)
PRK entails removal of the epithelium with underlying Bowman’s layer and variable part of the anterior stroma (depending on the degree of correction needed) using a laser (Tomás-Juan et al., 2015). Then, the usual cascade of events with death of keratocytes, activation of stromal cells outside of the ablation zone, immune cell infiltration, and myofibroblast formation take place (Kaji et al., 2003). The epithelium regrows without Bowman’s layer and stroma increases in thickness, although the cornea flattens out changing its refractive properties to improve vision (Tomás-Juan et al., 2015). The initial epithelial coverage occurs fairly quickly, but the restoration of epithelial basement membrane, corneal nerve regeneration, and stromal remodeling usually take months to years. Haze occurs in all patients within a month postoperatively, then subsides except for infrequent persistence, and can be reduced by routinely used mitomycin C, although it is not effective in all cases (Fountain et al., 1994; Latvala et al., 1995b; Linne and Tervo, 1997; Erie, 2003; Lai et al., 2004; Netto et al., 2005; Dawson et al., 2008; Tomás-Juan et al., 2015). As the mechanisms of haze formation may be complex, involving TGF-β induced myofibroblasts and excessive ECM production during stromal remodeling, its prevention may require combined or novel therapies to deal with its various components. The ideal treatment should be fine tuned in order not to interfere with desired changes in corneal thickness that occur after surgery.
3.5.2. Laser in situ keratomileusis (LASIK)
LASIK is arguably the most popular type of refractive surgery largely used for myopia correction. It consists of forming an epithelial flap attached to the cornea at one end with microkeratome or laser, shaving a part of the anterior stroma, and placing the flap back to the cornea, where it strongly adheres back to the stroma. Contrary to PRK, LASIK does not involve significant stromal remodeling except at the flap margin, and haze is generally absent. Myofibroblasts also appear transiently mainly at the flap margin, where hypercellularity and epithelial ingrowth are usually noted even in uneventful cases (Ivarsen et al., 2003; Fournié et al., 2010). The flap margin also displays increased MMP production and long-term accumulation of fibrotic ECM consisting of several collagens, various basement membrane components and tenascin-C, apparently reinforcing flap adhesion (Azar et al., 1998; Pérez-Santonja et al., 1998; Wachtlin et al., 1999; Maguen et al., 2007; 2008; Esquenazi et al., 2009). Contrary to the flap margin with clearly fibrotic changes that persist in humans for years (Maguen et al., 2007), the flap interface presents a hypocellular scar with little deposition of fibrotic ECM (Wachtlin et al., 1999; Schmack et al., 2005; Priglinger et al., 2006; Maguen et al., 2007). The only ECM component surprisingly persisting at the flap interface is fibronectin (Priglinger et al., 2006; Maguen et al., 2007). The only other ECM change observed in this area was abnormal sulfation of stromal glycosaminoglycans (Zhang et al., 2006). Overall, LASIK procedure, except for complicated cases with pronounced stromal fibrosis (Maguen et al., 2002; 2007), does not require measures to reduce fibrotic ECM and does not produce significant haze, contrary to PRK. At the same time, LASIK flap may not completely heal for quite a long time as suggested by the presence of provisional ECM component fibronectin along the entire flap margin even in uneventful cases.
3.6. Emerging strategies for wound healing regulation
3.6.1. Viral and nanoparticle gene therapy for haze
Gene therapy is a powerful tool to change expression levels of one gene or a group of genes in a combination setting. Cornea offers a unique opportunity for gene therapy with possibilities of topical application of viruses or plasmids or injections either subconjunctivally or intrastromally. At the same time, this promising approach is only starting to be developed. Only a handful of stromal components and effectors have been manipulated so far by gene therapy to reduce corneal opacity and scarring. Knockdown of vimentin with injected shRNA was able to decrease stromal opacity in a penetrating wound model (Das et al., 2014). Mohan’s group successfully used overexpression of decorin, a natural inhibitor of TGF-β, to suppress fibrosis and myofibroblast formation induced by TGF-β. Decorin transduction was able to decrease α-SMA expression in cultured stromal fibroblasts by over 80% (Mohan et al., 2010). In a common rabbit model of haze upon −9 diopters PRK, adeno-associated virus-driven topical delivery of decorin gene effectively decreased myofibroblast and macrophage numbers and significantly reduced haze (Mohan et al., 2011). More recently, they have shown that BMP7 gene transfer into the stroma using gold NPs also effectively reduced haze upon PRK in vivo. The treatment decreased α-SMA expression and the numbers of infiltrating macrophages. BMP7 effectively counteracted TGF-β signaling in this model without noticeable immunogenicity or toxicity (Tandon et al., 2013). Similar data on haze inhibition were obtained with cationic NPs encapsulating a triple combination of siRNAs targeting TGF-β1, TGF-β receptor 2 and CTGF (Sriram et al., 2014). Poly (lactide-co-glycolide) NPs with encapsulated antifibrotic pirfenidone reduced stromal collagen production and myofibroblast formation (Chowdhury et al., 2013), and those with shRNA to VEGF-A inhibited neovascularization (Qazi et al., 2012) upon corneal alkaline burns in vivo. These data show great promise of gene therapy using either viral vectors or NPs to counteract excessive wound healing and ensuing haze or fibrosis in refractive surgery.
In recent years, autologous plasma rich in growth factors (PRGF), which is a pool of biologically active proteins, has been successfully used for treatment of corneal disorders including stromal haze and post-LASIK complications (Alio et al., 2007; 2012). PRGF can counteract TGF-β effects and influences a range of biological processes including proliferation, migration and differentiation (Anitua et al., 2011; 2013). Modern gene therapy, however, appears to have distinct advantages over PRGF in terms of defined target(s) and considerably longer effect, and may become a viable therapeutic alternative to PRGF.
3.6.2. Stem cell therapies
A decade ago, stromal stem cells expressing PAX6 and ABCG2 progenitor markers have been isolated as a side population from human limbal stroma and propagated using FGF-2 to differentiate into keratocytes (Du et al., 2005). CD133 progenitor marker-expressing cells were also isolated from human corneal stroma and successfully differentiated into keratocytes (Thill et al., 2007). Corneal stromal stem cells have been used to engineer stromal equivalents. In serum free-conditions, stromal stem cells were better suited for this goal than stromal fibroblasts, although in the presence of serum fibroblasts secreted a more abundant stromal-like ECM (Karamichos et al., 2014a; Wu et al., 2014a). Work by Funderburgh’s group has shown that injection of normal stromal stem cells into corneas of lumican-null mice with corneal opacity fully restored tissue transparency with increased production of stromal proteoglycans (Du et al., 2009). Exciting data were recently obtained by the same team on the use of limbal biopsy-derived human stromal stem cells that expressed a variety of progenitor markers and could differentiate into keratocytes in culture. When these cells were injected into wounded corneas, these cells prevented fibrotic scar formation and contributed to the regeneration of stromal ECM with lamellar structure and collagen organization typical for normal corneas (Basu et al., 2014). Overall, these studies open up new avenues for fibrosis treatment with a possibility for using autologous sources, such as limbal biopsies or adipose derived stem cells (Ma et al., 2013).
3.7. Corneal constructs and wound healing
Corneal blindness is a significant clinical problem, with close to 2 million cases of unilateral blindness reported annually. The supply of donor corneas for transplantation does not meet the demand in many countries. This prompted researchers to look for alternatives including corneal constructs or equivalents (Griffith and Harkin, 2014). In recent years, there was substantial progress in making corneal stromal constructs based on compressed collagen with or without stromal keratocytes or fibroblasts. Decellularized corneal stroma has also been used, as well as silk-fibroin or synthetic materials (Griffith and Harkin, 2014). Such constructs can be transplanted into a trephined bed in the stroma to replace damaged tissue, and some have entered clinical trials (Griffith and Harkin, 2014). The advantage of such constructs is that in many cases they could use autologous cells reducing possible complications.
Stromal constructs are usually well repopulated by recipient’s cells. The epithelium regrows well, and there are encouraging reports on keratocyte repopulation as well (Koulikovska et al., 2015). However, nerve regeneration has not been generally studied, partially due to short follow-up times. Stromal remodeling and myofibroblast appearance at the wound edge have not been studied in detail either. To make the stromal equivalents more biocompatible, they are covered by limbal epithelial cells and kept at the air-liquid interface to ensure their stratification (Mi and Connon, 2013; Kureshi et al., 2014; Wu et al., 2014b). The best results may be eventually obtained with constructs having all three main corneal types (Proulx et al., 2010), but these need to be thoroughly evaluated in vivo. Wound healing upon construct implantation in vivo also needs to be better studied.
3.8. Concluding remarks
Corneal stromal wound healing is a very important clinical problem due to phenomenal popularity of refractive corneal surgery. It is a very complex and orderly process with keratocyte death and repopulation, sequential transformation of keratocytes into fibroblasts and myofibroblasts, immigration of limbal and circulating immune cells and remodeling of the corneal ECM structure. As it is prone to excessive ECM accumulation causing fibrotic changes, molecular mechanisms of stromal wound healing are need to be unraveled in order to be able to prevent fibrosis and haze. An important outcome of these studies is the realization of the importance of epithelial-mesenchymal interactions triggering wound healing, stepwise transformation of corneal cells during healing, and the central role of TGF-β signaling in this process. New interventions based on TGF-β inhibition using gene therapy, introduction of specific ECM components, implantation of stromal equivalents, and nanotechnology for drug delivery are emerging. A promising approach is the use of stem cells that could control fibrosis and haze. A refinement of refractive surgery techniques with less damage to the stromal cells and haze, for example, using femtosecond laser for keratectomy and LASIK (Morishige et al., 2008; Petroll et al., 2008; Meltendorf et al., 2009), is also contributing to better control of corneal stromal wound healing.
4. Corneal endothelial wound healing
Due to relative inaccessibility of corneal endothelial layer, there are fewer studies of endothelial healing. This process mostly occurs as a consequence of various burns (Zhao et al., 2009) and surgeries meant to replace dysfunctional endothelial cells (Descemet’s stripping endothelial keratoplasty, DSEK) or endothelial cells with Descemet’s membrane (Descemet’s membrane endothelial keratoplasty, DMEK) (Melles et al., 2006; Price and Price, 2007; Caldwell et al., 2009; Dirisamer et al., 2011). The wound healing process of corneal endothelium has certain peculiarities. In many tissues, this process entails cell proliferation as a major mechanism of reducing and remodeling the wound bed. However, corneal endothelial cells, especially human, have very low proliferation rates (Mimura et al., 2013). It is generally considered that corneal endothelium closes the wound the gap mainly by migration and increased cell spreading. These two processes are pharmacologically separable and, depending on the wound nature, their relative contribution may vary (Joyce et al., 1990; Ichijima et al., 1993a; Gordon 1994; Mimura et al., 2013). Concerning cell division, some data suggest that during healing it remains very low (Lee and Kay, 2006), although this view is challenged by the fact that healing corneal endothelial cells mostly divide amitotically, with formation of binuclear cells (Landhsman et al., 1989). It should be noted that wounds and damage to the corneal endothelial cells are inflicted both directly, e.g., by alkaline burns, surgical replacement, corneal transplantation or even cataract surgery, as well as indirectly. In the latter case, the healing of keratectomy wound primarily affecting epithelial and stromal cells can also provoke endothelial cell apoptosis and ensuing healing (Li et al., 2000). Below, we will review the studies of endothelial healing mechanisms and emerging approaches to enhance this process.
4.1. Endothelial-mesenchymal transformation
Endothelial wound healing is associated with a transient acquisition of fibroblastic morphology and actin stress fibers by migrating cells, which is consistent with endothelial-mesenchymal transformation (EnMT) (Lee et al., 2004; Miyamoto et al., 2010). In a model of freeze injury, EnMT to myofibroblasts occurs at the migrating front, where cells lose tight junction protein ZO-1 and start expressing α-SMA (Petroll et al., 1997). Inducers of EnMT and fibrotic changes in the endothelial layer include FGF-2 that may come from PMNs migrating to the cornea during epithelial and stromal wound healing (Lee et al., 2004) or induced by IL-1β (Lee et al., 2012), and TGF-β (Sumioka et al., 2008). Because EnMT may lead to fibrotic complications of healing such as the formation of retrocorneal fibrous membrane (Ichijima et al., 1993b), some ways of attenuating EMT have been proposed. These include inhibiting the expression of connexin 43 (Nakano et al., 2008) and TGF-β type I receptor (Okumura et al., 2013). The latter technique also facilitates endothelial cell propagation in culture.
4.2. Factors and signaling pathways influencing endothelial healing
Migration and spreading of corneal endothelial cells during wound healing is stimulated by a number of factors. ECM proteins fibronectin and TSP-1 were shown to facilitate cell migration (Munjal et al., 1990; Gundorova et al., 1994; Blanco-Mezquita et al., 2013). Growth factors known to promote endothelial migration and wound healing include EGF, FGF-2, IL-1β, PDGF-BB, TGF-β2, and VEGF, whereas IGF-I and IGF-II are ineffective, and IL-4 reduces migration (Joyce et al., 1990; Raphael et al., 1993; Soltau and McLaughlin, 1993; Hoppenreijs et al., 1994a,b, 1996; Bednarz et al., 1996; Sabatier et al., 1996; Thalmann-Goetsch et al., 1997; Riek et al., 2001; Imanishi et al., 2000; Baldwin and Marshall, 2002; Lee and Heur, 2013; 2014). Signaling pathways downstream of these factors that are important for wound healing are diverse. Prostaglandin E2 acting through cAMP pathway, ERK1/2 and p38 MAP kinase have been shown to participate in endothelial migration and wound healing (Joyce and Mekir, 1994; Sumioka et al., 2008; Chen et al., 2009b; Joko et al., 2013). FGF-2 stimulates migration through several pathways including p38, PI3K/Akt, and protein kinase C/phospholipase A2 (Riek et al., 2001; Lee et al., 2004; Joko et al., 2013). IL-1β stimulates migration through induction of FGF-2 (Lee et al., 2012), as well as of Wnt5a that both activate Cdc42 and inactivate RhoA (Lee and Kay, 2006; Lee and Heur, 2013; 2014). In the previous section it was mentioned that IL-1 (both α and β) secreted by the damaged epithelium caused apoptosis of stromal keratocytes. However, in the endothelial cells this cytokine actually stimulates cell migration directly and indirectly. Overall, the mechanisms of endothelial healing need to be further investigated. At the same time, therapies are emerging that exploit already uncovered mechanisms of this process.
4.3. Therapeutic approaches to improve endothelial healing and regeneration
TGF-β can stimulate healing but at the same time it promotes fibrogenic changes including deposition of aberrant ECM (Sumioka et al., 2008; Miyamoto et al., 2010). To counteract the fibrogenic response, inhibition of TGF-β signaling has been attempted. Using viral-mediated overexpression of SMAD7, a natural TGF-β signaling inhibitor, it was shown that the expression of fibrosis-associated markers in corneal endothelial cells was suppressed without compromising the rate of wound healing (Sumioka et al., 2008). Additionally, SMAD7 gene transfer to rabbit endothelium suppressed the inhibitory action of TGF-β on cell proliferation, which was mediated by inhibition of SMAD2 phosphorylation and downregulation of p27Kip1 (Funaki et al., 2003; 2008). SMAD7 therapy is being currently considered as a treatment preventing the formation of retrocorneal fibrous membrane (Miyamoto et al., 2010).
Another promising approach for enhancing endothelial wound healing is the use of Rho kinase (ROCK) inhibition. Inactivation of RhoA mediates promotion of endothelial migration by IL-1β. As ROCK inhibitor (e.g., Y-27632) also downregulates RhoA kinase expression (Ji et al., 2014), it was reasonable to use this inhibitor to accelerate wound healing. In different models in vitro and in vivo (monkey and human eyes) Y-27632 promoted migration of corneal endothelial cells (Okumura et al., 2011; 2013; Pipparelli et al., 2013), although the data on stimulation of proliferation remain controversial (Pipparelli et al., 2013; Okumura et al., 2014). Recently, ROCK inhibitor eye drops have been tested for accelerating endothelial healing in a rabbit model and eyes of Fuchs’ endothelial dystrophy and bullous keratopathy patients that all underwent transcorneal freezing. The eye drops improved corneal clarity in patients with central corneal edema caused by Fuchs’ dystrophy and in rabbit eyes (Okumura et al., 2011; Koizumi et al., 2014). This method may prove to be efficient for treatment of edematous corneal disorders due to endothelial dysfunction and as a post-surgical management.
The use of stem cells to improve endothelial healing has also been considered. Corneal endothelial stem cells, unlike those in the epithelium or stroma, have not been definitively identified. However, the endothelial periphery contains cells with increased proliferative capacity, and it was suggested that this region could harbor endothelial stem cells (Winkelhart et al., 2005; Bartakova et al., 2014). Such cells, if identified, could eventually become a new therapeutic tool for wound healing and endothelial regeneration (Bartakova et al., 2014). Alternatively, some mesenchymal stem cells, e.g., from umbilical cord blood, could be potentially used for this purpose. In fact, such cells could home for wounded areas of endothelial sheets in vitro and could be altered towards endothelial phenotype (Joyce et al., 2012). Recently, reprogramming of corneal endothelium to neural crest-like progenitors was achieved by knockdown of p120 catenin to activate p120–ROCK signaling and canonical BMP pathway that links to the activation of the miR-302b-Oct4-Sox2-Nanog network. This approach allowed rapid expansion of endothelial cells with potential use for treatment (Zhu et al., 2014). Although this research area seems to be promising, more data need to be obtained to speculate about its possible therapeutic value.
4.4. Concluding remarks
Corneal endothelial cells heal wounds mainly by migration and spreading, making them substantially different from epithelial cells and keratocytes. They undergo EnMT during healing, which is mediated by TGF-β. Various growth factors and cytokines mediate endothelial wound healing through multiple signaling mechanisms. Recent progress in this field relates to new emerging therapeutics to accelerate endothelial healing, including SMAD7 gene therapy to suppress fibrotic changes, and ROCK inhibitor in the form of eye drops to enhance cell migration. With further refinement and increased use of surgical techniques to replace ailing endothelium, such biological treatments may become routine in corneal surgery and management of ocular burns affecting endothelial cells.
5. Conclusions and future directions
Corneal wound healing is a complex and regulated sequence of cellular reactions directed towards wound closure. As the healing process in other organs, it is a coordinated cascade of growth factor action, activation of various cross-talking signaling pathways, cell proliferation, migration, ECM remodeling, and return to quiescence. Three main types of cells, epithelial, stromal, and endothelial, are involved in corneal wound healing. Corneal nerves and immune system cells also play significant roles in this process. Corneal epithelium and stroma interact with each other during healing, as epithelial wounds cause keratocyte apoptosis, and stromal wounds invariably involve the epithelium (e.g., upon refractive surgery or burns). Endothelial cells are relatively less affected by the epithelial and stromal wounds. A number of molecular processes in healing of these cells are similar. However, one conclusion of corneal wound healing studies is that some key events in this process significantly differ in different cells. Epithelial cells heal through participation of limbal stem cells and their progeny under the action of a number of cross-talking growth factors and cytokines coming from cells and tears, and there is a significant involvement of the basement membrane proteolytic remodeling during healing. No cell transformation has been documented for this process. In contrast, keratocytes get transformed into activated fibroblasts and then to motile wound contracting and α-SMA expressing myofibroblasts under the influence of factors supplied by the epithelium, immigrating immune cells, and stromal cells themselves. The main signaling complex driving these processes in the stroma is TGF-β system. This system is tightly regulated, with profibrotic TGF-β1 and -β2, and antifibrotic TGF-β3. The result of their interplay is not always predictable, and excessive healing may occur leaving stromal haze and/or ECM scar, which are targets for various therapies that are being actively developed. Endothelial cell healing entails transformation to mesenchymal-type cells, migration and spreading, with less contribution from proliferation than in other corneal cells. Overall, the mechanisms of healing of different cells are not the same, calling for diversified means to modulate these processes depending on cell type.
Progress in epithelial wound healing studies is mainly related to the unraveling of signaling pathways mediating this process, identification of a number of markers expressed by limbal stem cells, and growing use of cultured LESCs for resurfacing of damaged or dysfunctional corneal epithelium by cell transplantation. The main effort in the latter area has been directed towards the development of xenobiotic-free cell cultures and for searches of cells suitable for autologous transplantation when LESCs are unavailable. Additionally, the importance of niche cells has been recently emphasized for the proper functioning of LESCs. In terms of clinical translation, stem cell transplants appear to be the most significant advance in repairing damaged corneal epithelium, be it the result of stem cell loss, mechanical (including surgical) trauma or burns. Another important area of new research relates to emerging gene and miRNA therapy accelerating wound healing in disease conditions, such as diabetes. Future efforts in the understanding of epithelial wound healing may be focused on several issues. The limbal stem cell niche hypothesis has been recently unequivocally proven by imaging the fate of single cells during corneal maintenance and wound healing. However, although many putative LESC markers have been identified, and some were shown to have clinical significance for transplantation, such as ΔNp63α and ABCG2, we still lack specific markers for LESC that could distinguish them from their progeny. The same general lack of specific markers applies to TACs. At the same time, monitoring the fate and specifically influencing the activity of LESCs and TACs may allow modulating wound healing, especially in disease states. Emerging new techniques for specific tracking of label retaining stem cells give hope that this problem would be solved soon.
Although many stem and progenitor cell types, such as oral mucosa cells, were tested as LESC substitutes for autologous transplantation in clinic, they are still inferior to limbal cells because of possible neovascularization or conjunctivalization. Recently, attempts were made to develop protocols for differentiating limbal cells from renewable and bankable sources, such as iPSCs or ESCs. Encouraging results in this area with the combined use of specific growth factors, signaling modulators (such as ROCK inhibitor), and limbal-like ECM supports allow anticipating that these new sources, which may be produced from autologous cells, would be developed for clinical translation in the near future.
Further, despite a previous interest in proteinase activity affecting ECM remodeling during epithelial healing, more recent studies on the role of select enzymes and their interplay in this process have become scarce. They may need to be expanded, in order to better understand potential ways of fine tuning proteinase expression and activity by gene, miRNA or inhibitor therapy for optimal healing.
Finally, corneal wound healing research and translation would benefit from the development of targeted viral vectors and/or nanosystems for delivery of drugs, genes, and miRNA/siRNA to specific cells including LESC. Cornea offers ideal conditions for using such delivery systems topically, which would significantly alleviate systemic toxicity concerns. Some work is already being performed in this very promising and clinically needed direction.
Progress in stromal wound healing and ways to control it is largely related to the growing success and popularity of refractive corneal surgery. The stromal healing is a very complex process comprising keratocyte apoptosis in the wound area due to cytokine secretion from the damaged epithelium, sequential transformation of remaining keratocytes into fibroblasts and contractile myofibroblasts, immigration of immune cells secreting various cytokines and proteinases, and remodeling of the corneal ECM structure. At the end of this process, myofibroblasts disappear and keratocytes become quiescent again. Not infrequently, this healing process becomes somewhat dysregulated, with excessive ECM accumulation leading to fibrotic changes. This occurs sometimes after PRK and always at the LASIK flap edge.
Fibrosis after healing appears to be due to unconcerted regulation of TGF-β system, which is central in the wound healing process. Therefore, it is important to uncover mechanisms of interactions of TGF-β isoforms, some of which are profibrotic, and some are antifibrotic. Directional shift of respective signaling may constitute a promising avenue of future research in this area. To attenuate fibrosis, gene therapy with decorin and BMP7, as well as the use of some approved drugs (rosiglitazone, trichostatin A, ROCK inhibitor) have already shown promise. Expansion of these studies may lead to rapid translation to clinical use. The main conclusion of this work is the necessity for better understanding and control of fibrotic changes in stromal wound healing mediated by TGF-β. Another potential area of future interest is pharmacological protection of keratocytes from apoptosis upon epithelial injury. Inhibition of cell death may be advantageous in order to ensure uneventful and fast healing of epithelial wounds with minimal stromal involvement. In this respect, introduction of future treatment agents based on gene expression manipulation and miRNA appears to be promising, although respective data are very scarce. These agents could be potentially used in conjunction with neurotrophic factors to enhance corneal nerve regeneration in order to accelerate wound healing.
Nanotechnology and stem cell therapies are beginning to be used to attenuate fibrotic changes during stromal healing. It may be too early to speculate about the future impact of these treatments, but even the first results are very encouraging. Technological advances in laser techniques used in refractive surgery with less damage to corneal cells, e.g., the use of femtosecond lasers for keratectomy and LASIK, may offer another future way of alleviating unwanted consequences of stromal healing.
Wound healing in the corneal endothelium recently attracted considerable interest due to increasing use of new endothelial transplantation techniques with or without Descemet’s membrane scaffold. As the endothelial healing does not involve significant cell proliferation, research efforts were directed towards accelerating cell migration and control of endothelial-mesenchymal transformation, which is mediated by TGF-β. Exciting data were obtained in recent years on successful use of SMAD7 gene therapy to curb fibrosis, and of ROCK inhibitor eye drops to enhance cell migration and healing rate. We can anticipate the expansion of these studies and future use of drug combinations for the most pronounced effect.
As discussed above, stem cell therapies for epithelial and stromal wound healing have already shown promise and some of them have entered clinical practice. Similar treatments to enhance endothelial healing have been seriously hampered by lack of information on endothelial stem cells. This avenue of research should be actively pursued in the future. At the same time, recent use of mesenchymal stem cells to cover endothelial wounds has shown promise for future applications. An exciting possibility of creating endothelial cell sheets upon transient reprogramming to neural crest-like progenitors is likely to yield another way of facilitating the healing process.
Overall, significant progress in studies and clinical applications related to healing of all main corneal cell types has been achieved in the last decade. Better understanding of cell type-specific healing mechanisms made it easier to design future treatment strategies. Based on the existing data, new promising translational areas may include gene, miRNA, and stem cell therapies, as well as antifibrotic and healing accelerating agents. More frequent use of combination therapies to enhance wound healing is also anticipated.
Highlights.
Epithelial, stromal and endothelial wounds heal by different mechanisms
Limbal stem cell transplantation markedly improves corneal re-epithelialization
Renewable autologous stem cell sources may improve transplantation outcomes
Gene therapy, miRNA and nanocarriers are emerging wound healing treatments
Antifibrotic agents appear to be promising treatments for stromal haze and scarring
Endothelial wound healing is improved by TGF-β suppression
Acknowledgements
Supported by NIH R01 EY13431, NIH R01 EY023429, NIH R21 EY022771, and Board of Governors Regenerative Medicine Institute grants. The funders had no role in any aspect of this work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflict of interest.
References
- Aberdam E, Barak E, Rouleau M, de LaForest S, Berrih-Aknin S, Suter DM, Krause KH, Amit M, Itskovitz-Eldor J, Aberdam D. A pure population of ectodermal cells derived from human embryonic stem cells. Stem Cells. 2008;26:440–444. doi: 10.1634/stemcells.2007-0588. [DOI] [PubMed] [Google Scholar]
- Abrams GA, Schaus SS, Goodman SL, Nealey PF, Murphy CJ. Nanoscale topography of the corneal epithelial basement membrane and Descemet’s membrane of the human. Cornea. 2000;19:57–64. doi: 10.1097/00003226-200001000-00012. [DOI] [PubMed] [Google Scholar]
- Adijanto J, Naash MI. Nanoparticle-based technologies for retinal gene therapy. Eur. J. Pharm. Biopharm. 2015;12:S0939–6411. doi: 10.1016/j.ejpb.2014.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad S, Kolli S, Lako M, Figueiredo F, Daniels JT. Stem cell therapies for ocular surface disease. Drug Discov. Today. 2010;15:306–313. doi: 10.1016/j.drudis.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Alio JL, Pastor S, Ruiz-Colecha J, Rodriguez A, Artola A. Treatment of ocular surface syndrome after LASIK with autologous platelet-rich plasma. J. Refract. Surg. 2007;23:617–619. doi: 10.3928/1081-597X-20070601-13. [DOI] [PubMed] [Google Scholar]
- Alio JL, Arnalich-Montiel F, Rodriguez AE. The role of “eye platelet rich plasma” (E-PRP) for wound healing in ophthalmology. Curr. Pharm. Biotechnol. 2012;13:1257–1265. doi: 10.2174/138920112800624355. [DOI] [PubMed] [Google Scholar]
- Amitai-Lange A, Altshuler A, Bubley J, Dbayat N, Tiosano B, Shalom-Feuerstein R. Lineage tracing of stem and progenitor cells of the murine corneal epithelium. Stem Cells. 2015;33:230–239. doi: 10.1002/stem.1840. [DOI] [PubMed] [Google Scholar]
- An J, Chen X, Chen W, Liang R, Reinach PS, Yan D, Tu L. MicroRNA expression profile and the role of miR-204 in corneal wound healing. Invest. Ophthalmol. Vis. Sci. 2015;56:3673–3683. doi: 10.1167/iovs.15-16467. [DOI] [PubMed] [Google Scholar]
- Anderson RR. Actin filaments in normal and migrating corneal epithelial cells. Invest. Ophthalmol. Vis. Sci. 1977;16:161–166. [PubMed] [Google Scholar]
- Anderson SC, Stone C, Tkach L, SundarRaj N. Rho and Rho-kinase (ROCK) signaling in adherens and gap junction assembly in corneal epithelium. Invest. Ophthalmol. Vis. Sci. 2002;43:978–986. [PubMed] [Google Scholar]
- Andresen JL, Ledet T, Ehlers N. Keratocyte migration and peptide growth factors: the effect of PDGF, bFGF, EGF, IGF-I, aFGF and TGF-β on human keratocyte migration in a collagen gel. Curr. Eye Res. 1997;16:605–613. doi: 10.1076/ceyr.16.6.605.5081. [DOI] [PubMed] [Google Scholar]
- Anitua E, Sanchez M, Merayo-Lloves J, De la Fuente M, Muruzabal F, Orive G. Plasma rich in growth factors (PRGF-Endoret) stimulates proliferation and migration of primary keratocytes and conjunctival fibroblasts and inhibits and reverts TGF-beta1-Induced myodifferentiation. Invest. Ophthalmol. Vis. Sci. 2011;52:6066–6073. doi: 10.1167/iovs.11-7302. [DOI] [PubMed] [Google Scholar]
- Anitua E, Muruzabal F, Alcalde I, Merayo-Lloves J, Orive G. Plasma rich in growth factors (PRGF-Endoret) stimulates corneal wound healing and reduces haze formation after PRK surgery. Exp Eye Res. 2013;115:153–61. doi: 10.1016/j.exer.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Arranz-Valsero I, Soriano-Romaní L, García-Posadas L, López-García A, Diebold Y. IL-6 as a corneal wound healing mediator in an in vitro scratch assay. Exp. Eye Res. 2014;25:183–192. doi: 10.1016/j.exer.2014.06.012. [DOI] [PubMed] [Google Scholar]
- Azar DT, Pluznik D, Jain S, Khoury JM. Gelatinase B and A expression after laser in situ keratomileusis and photorefractive keratectomy. Arch. Ophthalmol. 1998;116:1206–1208. doi: 10.1001/archopht.116.9.1206. [DOI] [PubMed] [Google Scholar]
- Azar DT, Spurr-Michaud SJ, Tisdale AS, Gipson IK. Altered epithelial-basement membrane interactions in diabetic corneas. Arch. Ophthalmol. 1992;110:537–40. doi: 10.1001/archopht.1992.01080160115045. [DOI] [PubMed] [Google Scholar]
- Baldwin HC, Marshall J. Growth factors in corneal wound healing following refractive surgery: A review. Acta. Ophthalmol. Scand. 2002;80:238–247. doi: 10.1034/j.1600-0420.2002.800303.x. [DOI] [PubMed] [Google Scholar]
- Barak Y, Karov Y, Levin S, Soroker N, Barash A, Lancet M, Nir E. Granulocyte-macrophage colonies incultures of human fetal liver cells: morphologic and ultrastructural analysis of proliferation and differentiation. Exp. Hematol. 1980;8:837–844. [PubMed] [Google Scholar]
- Barbosa FL, Chaurasia SS, Cutler A, Asosingh K, Kaur H, de Medeiros FW, Agrawal V, Wilson SE. Corneal myofibroblast generation from bone marrow-derived cells. Exp. Eye Res. 2010;91:92–96. doi: 10.1016/j.exer.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartakova A, Kunzevitzky NJ, Goldberg JL. Regenerative cell therapy for corneal endothelium. Curr. Ophthalmol. Rep. 2014;2:81–90. doi: 10.1007/s40135-014-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu S, Hertsenberg AJ, Funderburgh ML, Burrow MK, Mann MM, Du Y, Lathrop KL, Syed-Picard FN, Adams SM, Birk DE, Funderburgh JL. Human limbal biopsy-derived stromal stem cells prevent corneal scarring. Sci. Transl. Med. 2014;6:266ra172. doi: 10.1126/scitranslmed.3009644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylis O, Figueiredo F, Henein C, Lako M, Ahmad S. 13 years of cultured limbal epithelial cell therapy: a review of the outcomes. J. Cell Biochem. 2011;112:993–1002. doi: 10.1002/jcb.23028. [DOI] [PubMed] [Google Scholar]
- Bednarz J, Thalmann-Goetsch A, Richard G, Engelmann K. Influence of vascular endothelial growth factor on bovine corneal endothelial cells in a wound-healing model. Ger. J. Ophthalmol. 1996;5:127–31. [PubMed] [Google Scholar]
- Bertero T, Gastaldi C, Bourget-Ponzio I, Imbert V, Loubat A, Selva E, Busca R, Mari B, Hofman P, Barbry P, Meneguzzi G, Ponzio G, Rezzonico R. miR-483-3p controls proliferation in wounded epithelial cells. FASEB J. 2011;25:3092–105. doi: 10.1096/fj.10-168401. [DOI] [PubMed] [Google Scholar]
- Bettahi I, Sun H, Gao N, Wang F, Mi X, Chen W, Liu Z, Yu FS. Genome-wide transcriptional analysis of differentially expressed genes in diabetic, healing corneal epithelial cells: hyperglycemia-suppressed TGFβ3 expression contributes to the delay of epithelial wound healing in diabetic corneas. Diabetes. 2014;63:715–727. doi: 10.2337/db13-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhowmick NA, Zent R, Ghiassi M, McDonnell M, Moses HL. Integrin β1 signaling is necessary for transforming growth factor-β activation of p38MAPK and epithelial plasticity. J. Biol. Chem. 2001;276:46707–46713. doi: 10.1074/jbc.M106176200. [DOI] [PubMed] [Google Scholar]
- Biber JM, Holland EJ, Neff KD. Management of ocular stem cell disease. Int. Ophthalmol. Clin. 2010;50:25–34. doi: 10.1097/IIO.0b013e3181e20d64. [DOI] [PubMed] [Google Scholar]
- Bilousova G, Chen J, Roop DR. Differentiation of mouse induced pluripotent stem cells into a multipotent keratinocyte lineage. J. Invest. Dermatol. 2010;131:857–864. doi: 10.1038/jid.2010.364. [DOI] [PubMed] [Google Scholar]
- Blanco-Mezquita T, Martinez-Garcia C, Proença R, Zieske JD, Bonini S, Lambiase A, Merayo-Lloves J. Nerve growth factor promotes corneal epithelial migration by enhancing expression of matrix metalloprotease-9. Invest. Ophthalmol. Vis. Sci. 2013a;54:3880–3890. doi: 10.1167/iovs.12-10816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco-Mezquita JT, Hutcheon AE, Zieske JD. Role of thrombospondin-1 in repair of penetrating corneal wounds. Invest. Ophthalmol. Vis. Sci. 2013b;54:6262–6268. doi: 10.1167/iovs.13-11710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block ER, Matela AR, SundarRaj N, Iszkula ER, Klarlund JK. Wounding induces motility in sheets of corneal epithelial cells through loss of spatial constraints: role of heparin-binding epidermal growth factor-like growth factor signaling. J. Biol. Chem. 2004;279:24307–24312. doi: 10.1074/jbc.M401058200. [DOI] [PubMed] [Google Scholar]
- Bobba S, Chow S, Watson S, Di Girolamo N. Clinical outcomes of xeno-free expansion and transplantation of autologous ocular surface epithelial stem cells via contact lens delivery: a prospective case series. Stem Cell Res. Ther. 2015;6:23. doi: 10.1186/s13287-015-0009-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonini S, Lambiase A, Rama P, Capriogli G, Aloe L. Topical treatment with nerve growth factor for neurotrophic keratitis. Ophthalmology. 2000;107:1347–1352. doi: 10.1016/s0161-6420(00)00163-9. [DOI] [PubMed] [Google Scholar]
- Bottaro DP, Rubin JS, Faletto DL, Chan AM, Kmiecik TE, Vande Woude GF, Aaronson SA. Identification of the hepatocyte growth factor receptor as the c-met proto-oncogene product. Science. 1991;251:802–804. doi: 10.1126/science.1846706. [DOI] [PubMed] [Google Scholar]
- Boucher I. Injury and nucleotides induce phosphorylation of epidermal growth factor receptor: MMP and HB-EGF dependent pathway. Exp. Eye Res. 2007;85:130–141. doi: 10.1016/j.exer.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boucher I, Rich C, Lee A, Marcincin M, Trinkaus-Randall V. The P2Y2 receptor mediates the epithelial injury response and cell migration. Am. J. Physiol. Cell Physiol. 2010;299:C411–C421. doi: 10.1152/ajpcell.00100.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boucher I, Kehasse A, Marcincin M, Rich C, Rahimi N, Trinkaus-Randall V. Distinct activation of epidermal growth factor receptor by UTP contributes to epithelial cell wound repair. Am. J. Pathol. 2011;178:1092–1105. doi: 10.1016/j.ajpath.2010.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss DG, Giuliano E, Sharma A, Mohan RR. Gene delivery in the equine cornea: a novel therapeutic strategy. Vet. Ophthalmol. 2010;13:301–306. doi: 10.1111/j.1463-5224.2010.00813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell MC, Afshari NA, Decroos FC, Proia AD. The histology of graft adhesion in Descemet stripping with endothelial keratoplasty. Am. J. Ophthalmol. 2009;148:277–281. doi: 10.1016/j.ajo.2009.03.025. [DOI] [PubMed] [Google Scholar]
- Carlson EC, Wang IJ, Liu CY, Brannan P, Kao CW, Kao WW. Altered KSPG expression by keratocytes following corneal injury. Mol. Vis. 2003;9:615–623. [PubMed] [Google Scholar]
- Carrington LM, Boulton M. Hepatocyte growth factor and keratinocyte growth factor regulation of epithelial and stromal corneal wound healing. J. Cataract Refract. Surg. 2005;31:412–423. doi: 10.1016/j.jcrs.2004.04.072. [DOI] [PubMed] [Google Scholar]
- Casaroli-Marano RP, Nieto-Nicolau N, Martínez-Conesa EM, Edel M, Álvarez-Palomo AB. Potential role of induced pluripotent stem cells (iPSCs) for cell-based therapy of the ocular surface. J. Clin. Med. 2015;4:318–342. doi: 10.3390/jcm4020318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro-Muñozledo F. Review: corneal epithelial stem cells, their niche and wound healing. Mol. Vis. 2013;24:1600–1613. [PMC free article] [PubMed] [Google Scholar]
- Chandrasekher G, Kakazu AH, Bazan HE. HGF- and KGF-induced activation of PI-3K/p70 S6 kinase pathway in corneal epithelial cells: its relevance in wound healing. Exp. Eye Res. 2001;73:191–202. doi: 10.1006/exer.2001.1026. [DOI] [PubMed] [Google Scholar]
- Chaurasia SS, Kaur H, de Medeiros FW, Smith SD, Wilson SE. Reprint of “Dynamics of the expression of intermediate filaments vimentin and desmin during myofibroblast differentiation after corneal injury”. Exp. Eye Res. 2009;89:590–596. doi: 10.1016/S0014-4835(09)00247-4. [DOI] [PubMed] [Google Scholar]
- Chaurasia SS, Perera PR, Poh R, Lim RR, Wong TT, Mehta JS. Hevin plays a pivotal role in corneal wound healing. PLoS One. 2013;8:e81544. doi: 10.1371/journal.pone.0081544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JJ, Tseng SC. Corneal epithelial wound healing in partial limbal deficiency. Invest. Ophthalmol. Vis. Sci. 1990;31:1301–1314. [PubMed] [Google Scholar]
- Chen J, Guerriero E, Sado Y, SundarRaj N. Rho-mediated regulation of TGF-β1- and FGF-2-induced activation of corneal stromal keratocytes. Invest. Ophthalmol. Vis. Sci. 2009a;50:3662–3670. doi: 10.1167/iovs.08-3276. [DOI] [PubMed] [Google Scholar]
- Chen WL, Lin CT, Li JW, Hu FR, Chen CC. ERK1/2 activation regulates the wound healing process of rabbit corneal endothelial cells. Curr. Eye Res. 2009b;34:103–111. doi: 10.1080/02713680802621741. [DOI] [PubMed] [Google Scholar]
- Chen Z, Mok H, Pflugfelder SC, Li DQ, Barry MA. Improved transduction of human corneal epithelial progenitor cells with cell-targeting adenoviral vectors. Exp. Eye Res. 2006;83:798–806. doi: 10.1016/j.exer.2006.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G, Umelo IA, Lv S, Teugels E, Fostier K, Kronenberger P, Dewaele A, Sadones J, Geers C, De Grève J. miR-146a inhibits cell growth, cell migration and induces apoptosis in non-small cell lung cancer cells. PLoS One. 2013;8:e60317. doi: 10.1371/journal.pone.0060317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HC, Yeh LK, Tsai YJ, Lai CH, Chen CC, Lai JY, Sun CC, Chang G, Hwang TL, Chen JK, Ma DH. Expression of angiogenesis-related factors in human corneas after cultivated oral mucosal epithelial transplantation. Invest. Ophthalmol. Vis. Sci. 2012;17:5615–23. doi: 10.1167/iovs.11-9293. [DOI] [PubMed] [Google Scholar]
- Chendrimada TP, Finn KJ, Ji X, Baillat D, Gregory RI, Liebhaber SA, Pasquinelli AE, Shiekhattar R. MicroRNA silencing through RISC recruitment of eIF6. Nature. 2007;447:823–828. doi: 10.1038/nature05841. [DOI] [PubMed] [Google Scholar]
- Cheng CC, Wang DY, Kao MH, Chen JK. The growth-promoting effect of KGF on limbal epithelial cells is mediated by upregulation of ΔNp63α through the p38 pathway. J. Cell Sci. 2009;122:4473–4480. doi: 10.1242/jcs.054791. [DOI] [PubMed] [Google Scholar]
- Chikama T, Wakuta M, Liu Y, Nishida T. Deviated mechanism of wound healing in diabetic corneas. Cornea. 2007;26(Suppl 1):S75–81. doi: 10.1097/ICO.0b013e31812f6d8e. [DOI] [PubMed] [Google Scholar]
- Chowdhury S, Guha R, Trivedi R, Kompella UB, Konar A, Hazra S. Pirfenidone nanoparticles improve corneal wound healing and prevent scarring following alkali burn. PLoS One. 2013;8:e70528. doi: 10.1371/journal.pone.0070528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung EH, DeGregorio PG, Wasson M, Zieske JD. Epithelial regeneration after limbus-to-limbus debridement. Expression of α-enolase in stem and transient amplifying cells. Invest. Ophthalmol. Vis. Sci. 1995;36:1336–1343. [PubMed] [Google Scholar]
- Cortina MS, He J, Li N, Bazan NG, Bazan HE. Recovery of corneal sensitivity, calcitonin gene-related peptide-positive nerves, and increased wound healing induced by pigment epithelial-derived factor plus docosahexaenoic acid after experimental surgery. Arch Ophthalmol. 2012;130:76–83. doi: 10.1001/archophthalmol.2011.287. [DOI] [PubMed] [Google Scholar]
- Cotsarelis G, Cheng SZ, Dong G, Sun TT, Lavker RM. Existence of slow-cycling limbal epithelial basal cells that can be preferentially stimulated to proliferate: implications on epithelial stem cells. Cell. 1989;57:201–209. doi: 10.1016/0092-8674(89)90958-6. [DOI] [PubMed] [Google Scholar]
- Crosson CE, Klyce SD, Beuerman RW. Epithelial wound closure in the rabbit cornea. A biphasic process. Invest. Ophthalmol. Vis. Sci. 1986;27:464–473. [PubMed] [Google Scholar]
- Daniels JT, Khaw PT. Temporal stimulation of corneal fibroblast wound healing activity by differentiating epithelium in vitro. Invest. Ophthalmol. Vis. Sci. 2000;41:3754–3762. [PubMed] [Google Scholar]
- Daniels JT, Harris AR, Mason C. Corneal epithelial stem cells in health and disease. Stem Cell Rev. 2006;2:247–254. doi: 10.1007/s12015-006-0053-4. [DOI] [PubMed] [Google Scholar]
- Daniels JT, Limb GA, Saarialho-Kere U, Murphy G, Khaw PT. Human corneal epithelial cells require MMP-1 for HGF-mediated migration on collagen I. Invest. Ophthalmol. Vis. Sci. 2003;44:1048–1055. doi: 10.1167/iovs.02-0442. [DOI] [PubMed] [Google Scholar]
- Davanger M, Evensen A. Role of the pericorneal papillary structure in renewal of corneal epithelium. Nature. 1971;229:560–561. doi: 10.1038/229560a0. [DOI] [PubMed] [Google Scholar]
- Dawson DG, Grossniklaus HE, McCarey BE, Edelhauser HF. Biomechanical and wound healing characteristics of corneas after excimer laser keratorefractive surgery: is there a difference between advanced surface ablation and sub-Bowman’s keratomileusis? J Refract Surg. 2008;24:S90–99. doi: 10.3928/1081597X-20080101-16. [DOI] [PubMed] [Google Scholar]
- Dedova IV, Nikolaeva OP, Safer D, De La Cruz EM, dos Remedios CG. Thymosin β4 induces a conformational change in actin monomers. Biophys. J. 2006;90:985–992. doi: 10.1529/biophysj.105.063081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denk PO, Knorr M. The in vitro effect of platelet-derived growth factor isoforms on the proliferation of bovine corneal stromal fibroblasts depends on cell density. Graefes Arch. Clin. Exp. Ophthalmol. 1997;235:530–534. doi: 10.1007/BF00947012. [DOI] [PubMed] [Google Scholar]
- Di Girolamo N. Moving epithelia: tracking the fate of mammalian limbal epithelial stem cells. Prog. Ret. Eye Res. 2015 doi: 10.1016/j.preteyeres.2015.04.002. In press. [DOI] [PubMed] [Google Scholar]
- Di Girolamo N, Bobba S, Raviraj V, Delic NC, Slapetova I, Nicovich PR, Halliday GM, Wakefield D, Whan R, Lyons GJ. Tracing the fate of limbal epithelial progenitor cells in the murine cornea. Stem Cells. 2015;33:157–169. doi: 10.1002/stem.1769. [DOI] [PubMed] [Google Scholar]
- Diehl KA, Foley JD, Nealey PF, Murphy CJ. Nanoscale topography modulates corneal epithelial cell migration. J. Biomed. Mater. Res. Part A. 2005;75A:603–611. doi: 10.1002/jbm.a.30467. [DOI] [PubMed] [Google Scholar]
- Dietrich-Ntoukas T, Hofmann-Rummelt C, Kruse FE, Schlötzer-Schrehardt U. Comparative analysis of the basement membrane composition of the human limbus epithelium and amniotic membrane epithelium. Cornea. 2012;31:564–569. doi: 10.1097/ICO.0b013e3182254b78. [DOI] [PubMed] [Google Scholar]
- Dirisamer M, Dapena I, Ham L, van Dijk K, Oganes O, Frank LE, van der Wees J, Melles GR. Patterns of corneal endothelialization and corneal clearance after Descemet membrane endothelial keratoplasty for Fuchs endothelial dystrophy. Am. J. Ophthalmol. 2011;152:543–555. doi: 10.1016/j.ajo.2011.03.031. [DOI] [PubMed] [Google Scholar]
- Du Y, Funderburgh ML, Mann MM, SundarRaj N, Funderburgh JL. Multipotent stem cells in human corneal stroma. Stem Cells. 2005;23:266–1275. doi: 10.1634/stemcells.2004-0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y, Carlson EC, Funderburgh ML, Birk DE, Pearlman E, Guo N, Kao WW, Funderburgh JL. Stem cell therapy restores transparency to defective murine corneas. Stem Cells. 2009;27:1635–1642. doi: 10.1002/stem.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua HS. The conjunctiva in corneal epithelial wound healing. Br. J. Ophthalmol. 1998;82:1407–11. doi: 10.1136/bjo.82.12.1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua HS, Shanmuganathan VA, Powell-Richards AO, Tighe PJ, Joseph A. Limbal epithelial crypts: a novel anatomical structure and a putative limbal stem cell niche. Br. J. Ophthalmol. 2005;89:529–532. doi: 10.1136/bjo.2004.049742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn SP, Heidemann DG, Chow CY, Crockford D, Turjman N, Angel J, Allan CB, Sosne G. Treatment of chronic nonhealing neurotrophic corneal epithelial defects with thymosin β4. Ann. N. Y. Acad. Sci. 2010;1194:199–206. doi: 10.1111/j.1749-6632.2010.05471.x. [DOI] [PubMed] [Google Scholar]
- Ebihara N, Matsuda A, Nakamura S, Matsuda H, Murakami A. Role of the IL-6 classic- and trans-signaling pathways in corneal sterile inflammation and wound healing Invest. Ophthalmol. Vis. Sci. 2011;52:8549–8557. doi: 10.1167/iovs.11-7956. [DOI] [PubMed] [Google Scholar]
- Elmén J, Lindow M, Schütz S, Lawrence M, Petri A, Obad S, Lindholm M, Hedtjärn M, Hansen HF, Berger U, Gullans S, Kearney P, Sarnow P, Straarup EM, Kauppinen S. LNA-mediated microRNA silencing in non-human primates. Nature. 2008a;452:896–899. doi: 10.1038/nature06783. [DOI] [PubMed] [Google Scholar]
- Elmén J, Lindow M, Silahtaroglu A, Bak M, Christensen M, Lind-Thomsen A, Hedtjarn M, Hansen JB, Hansen HF, Straarup EM, McCullagh K, Kearney P, Kauppinen S. Antagonism of microRNA-122 in mice by systemically administered LNA-antimiR leads to up-regulation of a large set of predicted target mRNAs in the liver. Nucleic Acids Res. 2008b;36:1153–116. doi: 10.1093/nar/gkm1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enríquez-de-Salamanca A, Castellanos E, Stern ME, Fernández I, Carreño E, García-Vázquez C, Herreras JM, Calonge M. Tear cytokine and chemokine analysis and clinical correlations in evaporative-type dry eye disease. Mol. Vis. 2010;16:862–873. [PMC free article] [PubMed] [Google Scholar]
- Er H, Uzmez E. Effects of transforming growth factor-β2, interleukin 6 and fibronectin on corneal epithelial wound healing. Eur. J. Ophthalmol. 1998;8:224–229. doi: 10.1177/112067219800800404. [DOI] [PubMed] [Google Scholar]
- Erie JC. Corneal wound healing after photorefractive keratectomy: a 3-year confocal microscopy study. Trans. Am. Ophthalmol. Soc. 2003;101:293–333. [PMC free article] [PubMed] [Google Scholar]
- Eslani M, Movahedan A, Afsharkhamseh N, Sroussi H, Djalilian AR. The role of toll-like receptor 4 in corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2014;55:6108–6115. doi: 10.1167/iovs.14-14736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espana EM, Kawakita T, Romano A, Di Pascuale M, Smiddy R, Liu CY, Tseng SC. Stromal niche controls the plasticity of limbal and corneal epithelial differentiation in a rabbit model of recombined tissue. Invest. Ophthalmol. Vis. Sci. 2003;44:5130–5135. doi: 10.1167/iovs.03-0584. [DOI] [PubMed] [Google Scholar]
- Esquenazi S, Esquenazi I, Grunstein L, He J, Bazan H. Immunohistological evaluation of the healing response at the flap interface in patients with LASIK ectasia requiring penetrating keratoplasty. J. Refract Surg. 2009;25:739–746. doi: 10.3928/1081597x-20090707-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fini ME, Parks WC, Rinehart WB, Girard MT, Matsubara M, Cook JR, West-Mays JA, Sadow PM, Burgeson RE, Jeffrey JJ, Raizman MB, Kruegerm RR, Zieskem JD. Role of matrix metalloproteinases in failure to re-epithelialize after corneal injury. Am. J. Pathol. 1996;149:1287–1301. [PMC free article] [PubMed] [Google Scholar]
- Fini ME, Parks WC, Rinehart WB, Girard MT, Matsubara M, Cook JR, West-Mays JA, Sadow PM, Burgeson RE, Jeffrey JJ, Raizman MB, Krueger RR, Zieske JD. Role of matrix metalloproteinases in failure to re-epithelialize after corneal injury. Am. J. Pathol. 1996;149:1287–1302. [PMC free article] [PubMed] [Google Scholar]
- Fini ME. Keratocyte and fibroblast phenotypes in the repairing cornea. Prog. Retin. Eye Res. 1999;18:529–551. doi: 10.1016/s1350-9462(98)00033-0. [DOI] [PubMed] [Google Scholar]
- Fini ME, Stramer BM. How the cornea heals: cornea-specific repair mechanisms affecting surgical outcomes. Cornea. 2005;24(Suppl 1):S2–S11. doi: 10.1097/01.ico.0000178743.06340.2c. [DOI] [PubMed] [Google Scholar]
- Follenzi A, Santambrogio L, Annoni A. Immune responses to lentiviral vectors. Curr. Gene Ther. 2007;7:306–315. doi: 10.2174/156652307782151515. [DOI] [PubMed] [Google Scholar]
- Fountain TR, de la Cruz Z, Green WR, Stark WJ, Azar DT. Reassembly of corneal epithelial adhesion structures after excimer laser keratectomy in humans. Arch. Ophthalmol. 1994;112:967–972. doi: 10.1001/archopht.1994.01090190115030. [DOI] [PubMed] [Google Scholar]
- Fournié PR, Gordon GM, Dawson DG, Malecaze FJ, Edelhauser HF, Fini ME. Correlation between epithelial ingrowth and basement membrane remodeling in human corneas after laser-assisted in situ keratomileusis. Arch. Ophthalmol. 2010;128:426–436. doi: 10.1001/archophthalmol.2010.23. [DOI] [PubMed] [Google Scholar]
- Freire V, Andollo N, Etxebarria J, Duran JA, Morales MC. In vitro effects of three blood derivatives on human corneal epithelial cells. Invest. Ophthalmol. Vis. Sci. 2012;53:5571–5578. doi: 10.1167/iovs.11-7340. [DOI] [PubMed] [Google Scholar]
- Fujikawa LS, Foster CS, Gipson IK, Colvin RB. Basement membrane components in healing rabbit corneal epithelial wounds: immunofluorescence and ultrastructural studies. J. Cell Biol. 1984;98:128–138. doi: 10.1083/jcb.98.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita H, Morita I, Takase H, Ohno-Matsui K, Mochizuki M. Prolonged exposure to high glucose impaired cellular behavior of normal human corneal epithelial cells. Curr. Eye Res. 2003;27:197–203. doi: 10.1076/ceyr.27.4.197.16598. [DOI] [PubMed] [Google Scholar]
- Funaki T, Ebihara N, Murakami A, Nakao A. Ex vivo transfer of Smad7 decreases damage to the corneal endothelium after penetrating keratoplasty. Jpn. J. Ophthalmol. 2008;52:204–210. doi: 10.1007/s10384-007-0526-2. [DOI] [PubMed] [Google Scholar]
- Funaki T, Nakaom A, Ebihara N, Setoguchi Y, Fukuchi Y, Okumura K, Ra C, Ogawa H, Kanai A. Smad7 suppresses the inhibitory effect of TGF-β2 on corneal endothelial cell proliferation and accelerates corneal endothelial wound closure in vitro. Cornea. 2003;22:153–159. doi: 10.1097/00003226-200303000-00015. [DOI] [PubMed] [Google Scholar]
- Funari VA, Winkler M, Brown J, Dimitrijevich SD, Ljubimov AV, Saghizadeh M. Differentially expressed wound healing-related microRNAs in the human diabetic cornea. PLoS One. 2013;8:e84425. doi: 10.1371/journal.pone.0084425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galal A, Perez-Santonja JJ, Rodriguez-Prats JL. Human anterior lens capsule as a biologic substrate for the ex vivo expansion of limbal stem cells in ocular surface reconstruction. Cornea. 2007;26:473–478. doi: 10.1097/ICO.0b013e318033bd0f. [DOI] [PubMed] [Google Scholar]
- Gallar J, Pozo MA, Rebollo I, Belmonre C. Effects of capsaicin on corneal wound healing. Invest. Ophthalmol. Vis. Sci. 1990;31:1968–1974. [PubMed] [Google Scholar]
- Gambaro G, Baggio B. Growth factors and the kidney in diabetes mellitus. Crit. Rev. Clin. Lab. Sci. 1998;35:117–151. doi: 10.1080/10408369891234174. [DOI] [PubMed] [Google Scholar]
- Gan L, Fagerholm P, Kim HJ. Effect of leukocytes on corneal cellular proliferation and wound healing. Invest. Ophthalmol. Vis. Sci. 1999;40:575–581. [PubMed] [Google Scholar]
- Gao N, Yin J, Yoon GS, Mi QS, Yu FS. Dendritic cell-epithelium interplay is a determinant factor for corneal epithelial wound repair. Am. J. Pathol. 2011;179:2243–53. doi: 10.1016/j.ajpath.2011.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J, Raghunathan VK, Reid B, Wei D, Diaz RC, Russell P, Murphy CJ, Zhao M. Biomimetic stochastic topography and electric fields synergistically enhance directional migration of corneal epithelial cells in a MMP-3-dependent manner. Acta Biomater. 2015a;12:102–112. doi: 10.1016/j.actbio.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao JN, Wang Y, Zhao X, Chen P, Xie L. MicroRNA-204-5p-mediated regulation of SIRT1 contributes to the delay of epithelial cell-cycle traversal in diabetic corneas. Invest. Ophthalmol. Vis. Sci. Invest. Ophthalmol. Vis. Sci. 2015b;56:1493–1504. doi: 10.1167/iovs.14-15913. [DOI] [PubMed] [Google Scholar]
- Girard MT, Matsubara M, Fini ME. Transforming growth factor-β and interleukin-1 modulate metalloproteinase expression by corneal stromal cells. Invest. Ophthalmol. Vis. Sci. 1991;32:2441–2454. [PubMed] [Google Scholar]
- Griffith M, Harkin DG. Recent advances in the design of artificial corneas. Curr. Opin. Ophthalmol. 2014;25:240–247. doi: 10.1097/ICU.0000000000000049. [DOI] [PubMed] [Google Scholar]
- Göbbels M, Spitznas M, Oldendoerp J. Impairment of corneal epithelial barrier function in diabetics. Graefes Arch. Clin. Exp. Ophthalmol. 1989;227:142–144. doi: 10.1007/BF02169787. [DOI] [PubMed] [Google Scholar]
- Goldberg MF, Bron AJ. Limbal palisades of Vogt. Trans. Am. Ophthalmol. Soc. 1982;80:155–171. [PMC free article] [PubMed] [Google Scholar]
- Gordon SR. Cytological and immunocytochemical approaches to the study of corneal endothelial wound repair. Prog. Histochem. Cytochem. 1994;28:1–64. doi: 10.1016/s0079-6336(11)80033-1. [DOI] [PubMed] [Google Scholar]
- Gordon GM, Austin JS, Sklar AL, Feuer WJ, LaGier AJ, Fini ME. Comprehensive gene expression profiling and functional analysis of matrix metalloproteinases and TIMPs, and identification of ADAM-10 gene expression, in a corneal model of epithelial resurfacing. J. Cell Physiol. 2011;226:1461–70. doi: 10.1002/jcp.22306. [DOI] [PubMed] [Google Scholar]
- Gundorova RA, Brikman IV, Ibadova SI, Issaeva RT. Stimulation of penetrating corneal wound healing by exogenous fibronectin. Eur. J. Ophthalmol. 1994;4:202–210. doi: 10.1177/112067219400400403. [DOI] [PubMed] [Google Scholar]
- Haber M, Cao Z, Panjwani N, Bedenice D, Li WW, Provost PJ. Effects of growth factors (EGF, PDGF-BB and TGF-β1) on cultured equine epithelial cells and keratocytes: implications for wound healing. Vet. Ophthalmol. 2003;6:211–217. doi: 10.1046/j.1463-5224.2003.00296.x. [DOI] [PubMed] [Google Scholar]
- Han Z, Conley SM, Naash MI. AAV and compacted DNA nanoparticles for the treatment of retinal disorders: challenges and future prospects. Invest. Ophthalmol. Vis. Sci. 2011;52:3051–3059. doi: 10.1167/iovs.10-6916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Z, Conley SM, Makkia R, Guo J, Cooper MJ, Naash MI. Comparative analysis of DNA nanoparticles and AAVs for ocular gene delivery. PLoS One. 2012;7:e52189. doi: 10.1371/journal.pone.0052189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattori M, Shimizu K, Katsumura K, Oku H, Sano Y, Matsumoto K, Yamaguchi Y, Ikeda T. Effects of all-trans retinoic acid nanoparticles on corneal epithelial wound healing. Graefes Arch. Clin. Exp. Ophthalmol. 2012;250:557–563. doi: 10.1007/s00417-011-1849-8. [DOI] [PubMed] [Google Scholar]
- Hayashi Y, Call MK, Chikama T, Liu H, Carlson EC, Sun Y, Pearlman E, Funderburgh JL, Babcock G, Liu CY, Ohashi Y, Kao WW. Lumican is required for neutrophil extravasation following corneal injury and wound healing. J. Cell Sci. 2010;123:2987–2995. doi: 10.1242/jcs.068221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi R, Ishikawa Y, Ito M, Kageyama T, Takashiba K, Fujioka T, Tsujikawa M, Miyoshi H, Yamato M, Nakamura Y, Nishida K. Generation of corneal epithelial cells from induced pluripotent stem cells derived from human dermal fibroblast and corneal limbal epithelium. PLoS One. 2012;7:e45435. doi: 10.1371/journal.pone.0045435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heldin CH. Targeting the PDGF signaling pathway in tumor treatment. Cell Commun. Signal. 2013;11:97. doi: 10.1186/1478-811X-11-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellmich B, Schellner M, Schatz H, Pfeiffer A. Activation of transforming growth factor-β1 in diabetic kidney disease. Metabolism. 2000;49:353–359. doi: 10.1016/s0026-0495(00)90264-6. [DOI] [PubMed] [Google Scholar]
- Ho TC, Chen SL, Wu JY, Ho MY, Chen LJ, Hsieh JW, Cheng HC, Tsao YP. PEDF promotes self-renewal of limbal stem cell and accelerates corneal epithelial wound healing. Stem Cells. 2013;31:1775–1784. doi: 10.1002/stem.1393. [DOI] [PubMed] [Google Scholar]
- Ho JH, Su Y, Chen KH, Lee OK. Protection of thymosin β-4 on corneal endothelial cells from UVB-induced apoptosis. Chin. J. Physiol. 2010;53:190–195. doi: 10.4077/cjp.2010.amh091. [DOI] [PubMed] [Google Scholar]
- Honma Y, Nishida K, Sotozono C, Kinoshita S. Effect of transforming growth factor-β1 and -β2 on in vitro rabbit corneal epithelial cell proliferation promoted by epidermal growth factor, keratinocyte growth factor, or hepatocyte growth factor. Exp. Eye Res. 1997;65:391–396. doi: 10.1006/exer.1997.0338. [DOI] [PubMed] [Google Scholar]
- Hoppenreijs VP, Pels E, Vrensen GF, Treffers WF. Basic fibroblast growth factor stimulates corneal endothelial cell growth and endothelial wound healing of human corneas. Invest. Ophthalmol. Vis. Sci. 1994a;35:931–944. [PubMed] [Google Scholar]
- Hoppenreijs VP, Pels E, Vrensen GF, Treffers WF. Effects of platelet-derived growth factor on endothelial wound healing of human corneas. Invest. Ophthalmol. Vis. Sci. 1994b;35:150–161. [PubMed] [Google Scholar]
- Hoppenreijs VP, Pels E, Vrensen GF, Treffers WF. Corneal endothelium and growth factors. Surv Ophthalmol. 1996;41:155–164. doi: 10.1016/s0039-6257(96)80005-1. [DOI] [PubMed] [Google Scholar]
- Hsu CC, Peng CH, Hung KH, Lee YY, Lin TC, Jang SF, Liu JH, Chen YT, Woung LC, Wang CY, Tsa CY, Chiou SH, Chen SJ, Chang YL. Stem cell therapy for corneal regeneration medicine and contemporary nanomedicine for corneal disorders. Cell Transplant. 2015 doi: 10.3727/096368914X685744. In press. [DOI] [PubMed] [Google Scholar]
- Huang YH, I CC, Kuo CH, Hsu YY, Lee FT, Shi GY, Tseng SH, Wu HL. Thrombomodulin promotes corneal epithelial wound healing. PLoS One. 2015;10:e0122491. doi: 10.1371/journal.pone.0122491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Lyu H, Wang J, Liu B. MicroRNA regulation and therapeutic targeting of survivin in cancer. Am. J. Cancer Res. 2014;5:20–31. [PMC free article] [PubMed] [Google Scholar]
- Huh MI, Kim YH, Park JH, Bae SW, Kim MH, Chang Y, Kim SJ, Lee SR, Lee YS, Jin EJ, Sonn JK, Kang SS, Jung JC. Distribution of TGF-β isoforms and signaling intermediates in corneal fibrotic wound repair. J. Cell Biochem. 2009;108:476–488. doi: 10.1002/jcb.22277. [DOI] [PubMed] [Google Scholar]
- Humphreys DT, Westman BJ, Martin DI, Preiss T. MicroRNAs control translation initiation by inhibiting eukaryotic initiation factor 4E/cap and poly(A) tail function. Proc. Natl. Acad. Sci. U.S.A. 2005;102:16961–16966. doi: 10.1073/pnas.0506482102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxlin KR, Hindman HB, Jeon KI, Bühren J, MacRae S, DeMagistris M, Ciufo D, Sime PJ, Phipps RP. Topical rosiglitazone is an effective anti-scarring agent in the cornea. PLoS One. 2013;8:e70785. doi: 10.1371/journal.pone.0070785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichijima H, Petroll WM, Barry PA, Andrews PM, Dai M, Cavanagh HD, Jester JV. Actin filament organization during endothelial wound healing in the rabbit cornea: comparison between transcorneal freeze and mechanical scrape injuries. Invest. Ophthalmol. Vis. Sci. 1993a;34:2803–28012. [PubMed] [Google Scholar]
- Ichijima H, Petroll WM, Jester JV, Barry PA, Andrews PM, Dai M, Cavanagh HD. In vivo confocal microscopic studies of endothelial wound healing in rabbit cornea. Cornea. 1993b;12:369–378. doi: 10.1097/00003226-199309000-00001. [DOI] [PubMed] [Google Scholar]
- Imanishi J, Kamiyama K, Iguchi I, Kita M, Sotozono C, Kinoshita S. Growth factors: importance in wound healing and maintenance of transparency of the cornea. Prog Retin Eye Res. 2000;19:113–129. doi: 10.1016/s1350-9462(99)00007-5. [DOI] [PubMed] [Google Scholar]
- Inai K, Burnside JL, Hoffman S, Toole BP, Sugi Y. BMP-2 induces versican and hyaluronan that contribute to post-EMT AV cushion cell migration. PLoS One. 2013;8:e77593. doi: 10.1371/journal.pone.0077593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa T, del Cerro M, Liang FQ, Loya N, Aquavella JV. Corneal sensitivity and nerve regeneration after excimer laser ablation. Cornea. 1994;13:225–231. doi: 10.1097/00003226-199405000-00006. [DOI] [PubMed] [Google Scholar]
- Ishizaki T, Maekawa M, Fujisawa K, Okawa K, Iwamatsu A, Fujita A, Watanabe N, Saito Y, Kakizuka A, Morii N, Narumiya S. The small GTP-binding protein Rho binds to and activates a 160 kDa Ser/Thr protein kinase homologous to myotonic dystrophy kinase. EMBO J. 1996;15:1885–1893. [PMC free article] [PubMed] [Google Scholar]
- Ishizaki M, Shimoda M, Wakamatsu K, Ogro T, Yamanaka N, Kao CW, Kao WW. Stromal fibroblasts are associated with collagen IV in scar tissues of alkali-burned and laceraed corneas. Curr. Eye Res. 1997;16:339–348. doi: 10.1076/ceyr.16.4.339.10684. [DOI] [PubMed] [Google Scholar]
- Ishizaki M, Zhu G, Haseba T, Shafer SS, Kao WW. Expression of collagen I, smooth muscle alpha-actin, and vimentin during the healing of alkali-burned and lacerated corneas. Invest. Ophthalmol. Vis. Sci. 1993;34:3320–3328. [PubMed] [Google Scholar]
- Ivarsen A, Laurberg T, Møller-Pedersen T. Characterisation of corneal fibrotic wound repair at the LASIK flap margin. Br. J. Ophthalmol. 2003;87:1272–1278. doi: 10.1136/bjo.87.10.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto R, Yamazaki S, Asakura M, Takashima S, Hasuwa H, Miyado K, Adachi S, Kitakaze M, Hashimoto K, Raab G, Nanba D, Higashiyama S, Hori M, Klagsbrun M, Mekada E. Heparin-binding EGF-like growth factor and ErbB signaling is essential for heart function. Proc. Natl. Acad. Sci. U S A. 2003;100:3221–3226. doi: 10.1073/pnas.0537588100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izumi K, Kurosaka D, Iwata T, Oguchi Y, Tanaka Y, Mashima Y, Tsubota K. Involvement of insulin-like growth factor-I and insulin-like growth factor binding protein-3 in corneal fibroblasts during corneal wound healing. Invest. Ophthalmol. Vis. Sci. 2006;47:591–598. doi: 10.1167/iovs.05-0097. [DOI] [PubMed] [Google Scholar]
- Janssen HL, Reesink HW, Lawitz EJ, Zeuzem S, Rodriguez-Torres M, Patel K, van der Meer AJ, Patick AK, Chen A, Zhou Y, Persson R, King BD, Kauppinen S, Levin AA, Hodges MR. Treatment of HCV infection by targeting microRNA. N. Engl. J. Med. 2013;368:1685–1694. doi: 10.1056/NEJMoa1209026. [DOI] [PubMed] [Google Scholar]
- Javier JA, Lee JB, Oliveira HB, Chang JH, Azar DT. Basement membrane and collagen deposition after laser subepithelial keratomileusis and photorefractive keratectomy in the leghorn chick eye. Arch. Ophthalmol. 2006;124:703–709. doi: 10.1001/archopht.124.5.703. [DOI] [PubMed] [Google Scholar]
- Jester JV, Petroll WM, Barry PA, Cavanagh HD. Expression of alpha-smooth muscle (α-SM) actin during corneal stromal wound healing. Invest. Ophthalmol. Vis. Sci. 1995;36:809–819. [PubMed] [Google Scholar]
- Jester JV, Petroll WM, Cavanagh HD. Corneal stromal wound healing in refractive surgery: the role of myofibroblasts. Prog. Retin. Eye Res. 1999;18:311–356. doi: 10.1016/s1350-9462(98)00021-4. Review. [DOI] [PubMed] [Google Scholar]
- Jester JV, Ho-Chang J. Modulation of cultured corneal keratocyte phenotype by growth factors/cytokines control in vitro contractility and extracellular matrix contraction. Exp. Eye Res. 2003;77:581–592. doi: 10.1016/s0014-4835(03)00188-x. [DOI] [PubMed] [Google Scholar]
- Ji H, Tang H, Lin H, Mao J, Gao L, Liu J, Wu T. Rho/Rock cross-talks with transforming growth factor-β/Smad pathway participates in lung fibroblast-myofibroblast differentiation. Biomed. Rep. 2014;2:787–792. doi: 10.3892/br.2014.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y, Shen L, Chong EM, Hamrah P, Zhang Q, Chen L, Dana MR. The chemokine receptor CCR7 mediates corneal antigen-presenting cell trafficking. Mol. Vis. 2007;13:626–634. [PMC free article] [PubMed] [Google Scholar]
- Joko T, Shiraishi A, Akune Y, Tokumaru S, Kobayashi T, Miyata K, Ohashi Y. Involvement of P38MAPK in human corneal endothelial cell migration induced by TGF-β2. Exp. Eye Res. 2013;108:23–32. doi: 10.1016/j.exer.2012.11.018. [DOI] [PubMed] [Google Scholar]
- Joe AW, Yeung SN. Concise review: identifying limbal stem cells: classical concepts and new challenges. Stem Cells Trans. Med. 2014;3:318–322. doi: 10.5966/sctm.2013-0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce NC, Harris DL, Markov V, Zhang Z, Saitta B. Potential of human umbilical cord blood mesenchymal stem cells to heal damaged corneal endothelium. Mol. Vis. 2012;18:547–564. [PMC free article] [PubMed] [Google Scholar]
- Joyce NC, Meklir B, Neufeld AH. In vitro pharmacologic separation of corneal endothelial migration and spreading responses. Invest. Ophthalmol. Vis. Sci. 1990;31:1816–1826. [PubMed] [Google Scholar]
- Joyce NC, Meklir B. PGE2: a mediator of corneal endothelial wound repair in vitro. Am. J. Physiol. 1994;266:C269–275. doi: 10.1152/ajpcell.1994.266.1.C269. [DOI] [PubMed] [Google Scholar]
- Jung JC, Huh MI, Fini ME. Constitutive collagenase-1 synthesis through MAPK pathways is mediated, in part, by endogenous IL-1α during fibrotic repair in corneal stroma. J. Cell Biochem. 2007;102:453–462. doi: 10.1002/jcb.21309. [DOI] [PubMed] [Google Scholar]
- Kabosova A, Kramerov AA, Aoki AM, Murphy G, Zieske JD, Ljubimov AV. Human diabetic corneas preserve wound healing, basement membrane, integrin and MMP-10 differences from normal corneas in organ culture. Exp. Eye Res. 2003;77:211–217. doi: 10.1016/s0014-4835(03)00111-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabosova A, Azar DT, Bannikov GA, Campbell KP, Durbeej M, Ghohestani RF, Jones JC, Kenney MC, Koch M, Ninomiya Y, Patton BL, Paulsson M, Sado Y, Sage EH, Sasaki T, Sorokin LM, Steiner-Champliaud MF, Sun TT, Sundarraj N, Timpl R, Virtanen I, Ljubimov AV. Compositional differences between infant and adult human corneal basement membranes. Invest. Ophthalmol. Vis. Sci. 2007;48:4989–4999. doi: 10.1167/iovs.07-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaji Y, Yamashita H, Oshika T. Corneal wound healing after excimer laser keratectomy. Semin. Ophthalmol. 2003;18:11–16. doi: 10.1076/soph.18.1.11.14075. [DOI] [PubMed] [Google Scholar]
- Kakazu A, Chandrasekher G, Bazan HE. HGF protects corneal epithelial cells from apoptosis by the PI-3K/Akt-1/Bad- but not the ERK1/2-mediated signaling pathway. Invest. Ophthalmol. Vis. Sci. 2004;45:3485–3492. doi: 10.1167/iovs.04-0372. [DOI] [PubMed] [Google Scholar]
- Kakazu A, He J, Kenchegowda S, Bazan HE. Lipoxin A inhibits platelet-activating factor inflammatory response and stimulates corneal wound healing of injuries that compromise the stroma. Exp. Eye Res. 2012;103:9–16. doi: 10.1016/j.exer.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakazu A, Sharma G, Bazan HE. Association of protein tyrosine phosphatases (PTPs)-1B with c-Met receptor and modulation of corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2008;49:2927–35. doi: 10.1167/iovs.07-0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamiyama K, Iguchi I, Wang X, Imanishi J. Effects of PDGF on the migration of rabbit corneal fibroblasts and epithelial cells. Cornea. 1998;17:315–325. [PubMed] [Google Scholar]
- Kamma-Lorger CS, Boote C, Hayes S, Albon J, Boulton ME, Meek KM. Collagen ultrastructural changes during stromal wound healing in organ cultured bovine corneas. Exp. Eye Res. 2009;88:953–959. doi: 10.1016/j.exer.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Karali M, Peluso I, Gennarino VA, Bilio M, Verde R, Lago G, Dollé P, Banfi S. miRNeye: a microRNA expression atlas of the mouse eye. BMC Genomics. 2010;11:715. doi: 10.1186/1471-2164-11-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamichos D, Funderburgh ML, Hutcheon AE, Zieske JD, Du Y, Wu J, Funderburgh JL. A role for topographic cues in the organization of collagenous matrix by corneal fibroblasts and stem cells. PLoS One. 2014a;9:e86260. doi: 10.1371/journal.pone.0086260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamichos D, Hutcheon AE, Zieske JD. Reversal of fibrosis by TGF-β3 in a 3D in vitro model. Exp. Eye Res. 2014b;124:31–36. doi: 10.1016/j.exer.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karuri NW, Liliensiek S, Teixeira AI, Abrams G, Campbell S, Nealey PF, Murphy CJ. Biological length scale topography enhances cell-substratum adhesion of human corneal epithelial cells. J. Cell Sci. 2004;117:3153–3164. doi: 10.1242/jcs.01146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato T, Chang JH, Azar DT. Expression of type XVIII collagen during healing of corneal incisions and keratectomy wounds. Invest. Ophthalmol. Vis. Sci. 2003;44:78–85. doi: 10.1167/iovs.01-1257. [DOI] [PubMed] [Google Scholar]
- Kaur H, Chaurasia SS, Agrawal V, Suto C, Wilson SE. Corneal myofibroblast viability: opposing effects of IL-1 and TGF-β1. Exp. Eye Res. 2009a;89:152–158. doi: 10.1016/j.exer.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur H, Chaurasia SS, de Medeiros FW, Agrawal V, Salomao MQ, Singh N, Ambati BK, Wilson SE. Corneal stroma PDGF blockade and myofibroblast development. Exp Eye Res. 2009b;88:960–965. doi: 10.1016/j.exer.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keadle TL, Usui N, Laycock KA, Miller JK, Pepose JS, Stuart PM. IL-1 and TNF-α are important factors in the pathogenesis of murine recurrent herpetic stromal keratitis. Invest. Ophthalmol. Vis. Sci. 2000;41:96–102. [PubMed] [Google Scholar]
- Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96:709–722. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- Kim HS, Shang T, Chen Z, Pflugfelder SC, Li DQ. TGF-β 1 stimulates production of gelatinase (MMP-collagenases (MMP-1, -13) and stromelysins (MMP-3, -10, -11) by human corneal epithelial cells. Exp. Eye Res. 2004;79:263–274. doi: 10.1016/j.exer.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Kim A, Lakshman N, Petroll WM. Quantitative assessment of local collagen matrix remodeling in 3-D culture: the role of Rho kinase. Exp. Cell Res. 2006;312:3683–3692. doi: 10.1016/j.yexcr.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim A, Petroll WM. Microtubule regulation of corneal fibroblast morphology and mechanical activity in 3-D culture. Exp. Eye Res. 2007;85:546–556. doi: 10.1016/j.exer.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura K, Teranishi S, Yamauchi J, Nishida T. Role of JNK-dependent serine phosphorylation of paxillin in migration of corneal epithelial cells during wound closure. Invest. Ophthalmol. Vis. Sci. 2008;49:125–132. doi: 10.1167/iovs.07-0725. [DOI] [PubMed] [Google Scholar]
- Klausner EA, Zhang Z, Chapman RL, Multack RF, Volin MV. Ultrapure chitosan oligomers as carriers for corneal gene transfer. Biomaterials. 2010;31:1814–1820. doi: 10.1016/j.biomaterials.2009.10.031. [DOI] [PubMed] [Google Scholar]
- Klocek MS, Sassani JW, McLaughlin PJ, Zagon IS. Naltrexone and insulin are independently effective but not additive in accelerating corneal epithelial healing in type I diabetic rats. Exp. Eye Res. 2009;89:686–92. doi: 10.1016/j.exer.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogo R, Mimori K, Tanaka F, Komune S, Mori M. Clinical significance of miR-146a in gastric cancer cases. Clin. Cancer Res. 2011;17:4277–4284. doi: 10.1158/1078-0432.CCR-10-2866. [DOI] [PubMed] [Google Scholar]
- Koizumi N, Okumura N, Ueno M, Kinoshita S. New therapeutic modality for corneal endothelial disease using Rho-associated kinase inhibitor eye drops. Cornea. 2014;33(Suppl 11):S25–31. doi: 10.1097/ICO.0000000000000240. [DOI] [PubMed] [Google Scholar]
- Kolli S, Ahmad S, Mudhar HS, Meeny A, Lako M, Figueiredo FC. Successful application of ex vivo expanded human autologous oral mucosal epithelium for the treatment of total bilateral limbal stem cell deficiency. Stem Cell. 2014;32:2135–2146. doi: 10.1002/stem.1694. [DOI] [PubMed] [Google Scholar]
- Kostarnoy AV, Gancheva PG, Logunov DY, Verkhovskaya LV, Bobrov MA, Scheblyakov DV, Tukhvatulin AI, Filippova NE, Naroditsky BS, Gintsburg AL. Topical bacterial lipopolysaccharide application affects inflammatory response and promotes wound healing. J. Interferon Cytokine Res. 2013;33:514–522. doi: 10.1089/jir.2012.0108. [DOI] [PubMed] [Google Scholar]
- Koulikovska M, Rafat M, Petrovski G, Veréb Z, Akhtar S, Fagerholm P, Lagali N. Enhanced regeneration of corneal tissue via a bioengineered collagen construct implanted by a nondisruptive surgical technique. Tissue Eng. Part A. 2015;21:1116–30. doi: 10.1089/ten.TEA.2014.0562. [DOI] [PubMed] [Google Scholar]
- Krutzfeldt J, Rajewsky N, Braich R, Rajeev KG, Tuschl T, Manoharan M, Stoffel M. Silencing of microRNAs in vivo with ‘antagomirs’. Nature. 2005;438:685–689. doi: 10.1038/nature04303. [DOI] [PubMed] [Google Scholar]
- Ksander BR, Kolovou PE, Wilson BJ, Saab KR, Guo Q, Ma J, McGuire SP, Gregory MS, Vincent WJ, Perez VL, Cruz-Guilloty F, Kao WW, Call MK, Tucker BA, Zhan Q, Murphy GF, Lathrop KL, Alt C, Mortensen LJ, Lin CP, Zieske JD, Frank MH, Frank NY. ABCB5 is a limbal stem cell gene required for corneal development and repair. Nature. 2014;511:353–357. doi: 10.1038/nature13426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumagai Y, Kurokawa MS, Ueno H, Kayama M, Tsubota K, Nakatsuji N, Kondo Y, Ueno S, Suzuki N. Induction of corneal epithelium–like cells from cynomolgus monkey embryonic stem cells and their experimental transplantation to damaged cornea. Cornea. 2010;29:432–438. doi: 10.1097/ICO.0b013e3181b9ffcc. [DOI] [PubMed] [Google Scholar]
- Kureshi AK, Drake RA, Daniels JT. Challenges in the development of a reference standard and potency assay for the clinical production of RAFT tissue equivalents for the cornea. Regen. Med. 2014;9:167–177. doi: 10.2217/rme.13.92. [DOI] [PubMed] [Google Scholar]
- Kurpakus MA, Stock EL, Jones JC. The role of the basement membrane in differential expression of keratin proteins in epithelial cells. Dev. Biol. 1992;150:243–255. doi: 10.1016/0012-1606(92)90239-d. [DOI] [PubMed] [Google Scholar]
- Kuwabara T, Perkins DS, Coggan DG. Sliding of the epithelium in experimental corneal wounds. Invest. Ophthalmol. 1976;15:4–14. [PubMed] [Google Scholar]
- Kyriakides TR, Wulsin D, Skokos EA, Fleckman P, Pirrone A, Shipley JM, Senior RM, Bornstein P. Mice that lack matrix metalloproteinase-9 display delayed wound healing associated with delayed reepithelization and disordered collagen fibrillogenesis. Matrix Biol. 2009;28:65–73. doi: 10.1016/j.matbio.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai YH, Wang HZ, Lin CP, Chang SJ. Mitomycin C alters corneal stromal wound healing and corneal haze in rabbits after argon-fluoride excimer laser photorefractive keratectomy. J. Ocul. Pharmacol. Ther. 2004;20:129–138. doi: 10.1089/108076804773710803. [DOI] [PubMed] [Google Scholar]
- Lam FW, Burns AR, Smith CW, Rumbaut RE. Platelets enhance neutrophil transendothelial migration via P-selectin glycoprotein ligand-1. Am. J Physiol. Heart Circ. Physiol. 2011;300:H468–H475. doi: 10.1152/ajpheart.00491.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambiase A, Bonini S, Micera A, Rama P, Bonini S, Aloe L. Expression of nerve growth factor receptors on the ocular surface in healthy subjects and during manifestation of inflammatory diseases. Invest. Ophthalmol. Vis. Sci. 1998a;39:1272–1275. [PubMed] [Google Scholar]
- Lambiase A, Rama P, Bonini S, Caprioglio G, Aloe L. Topical treatment with nerve growth factor for corneal neurotrophic ulcers. N. Eng. J. Med. 1998b;338:1174–1180. doi: 10.1056/NEJM199804233381702. [DOI] [PubMed] [Google Scholar]
- Lambiase A, Rama P, Aloe L, Bonini S. Management of neurotrophic keratopathy. Curr. Opin. Ophthalmol. 1999;10:270–276. doi: 10.1097/00055735-199908000-00009. [DOI] [PubMed] [Google Scholar]
- Lambiase A, Micera A, Sgrilletta R, Bonini S, Bonini S. Nerve growth factor and the immune system: old and new concepts in the cross-talk between immune and resident cells during pathophysiological conditions. Curr. Opin. Allergy Clin. Immunol. 2004;4:425–430. doi: 10.1097/00130832-200410000-00015. [DOI] [PubMed] [Google Scholar]
- Lan Y, Kodati S, Lee HS, Omoto M, Jin Y, Chauhan SK. Kinetics and function of mesenchymal stem cells in corneal injury. Invest. Ophthalmol. Vis. Sci. 2012;53:3638–3644. doi: 10.1167/iovs.11-9311. [DOI] [PubMed] [Google Scholar]
- Landshman N, Solomon A, Belkin M. Cell division in the healing of the corneal endothelium of cats. Arch. Ophthalmol. 1989;107:1804–1808. doi: 10.1001/archopht.1989.01070020886032. [DOI] [PubMed] [Google Scholar]
- Latvala T, Tervo K, Mustonen R, Tervo T. Expression of cellular fibronectin and tenascin in the rabbit cornea after excimer laser photorefractive keratectomy: a 12 month study. Br. J. Ophthalmol. 1995a;79:65–69. doi: 10.1136/bjo.79.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latvala T, Tervo K, Tervo T. Reassembly of the α6β4 integrin and laminin in rabbit corneal basement membrane after excimer laser surgery: a 12-month follow-up. CLAO J. 1995b;21:125–129. [PubMed] [Google Scholar]
- Lavker RM, Sun TT. Epidermal stem cells. J. Invest. Dermatol. 1983;81:121s–7s. doi: 10.1111/1523-1747.ep12540880. [DOI] [PubMed] [Google Scholar]
- Lavker RM, Wei ZG, Sun TT. Phorbol ester preferentially stimulates mouse fornical conjunctival and limbal epithelial cells to proliferate in vivo. Invest. Ophthalmol. Vis. Sci. 1998;39:301–307. [PubMed] [Google Scholar]
- Leask A, Abraham DJ. TGF-beta signaling and the fibrotic response. FASEB J. 2004;18:816–827. doi: 10.1096/fj.03-1273rev. [DOI] [PubMed] [Google Scholar]
- Lee A, Derricks K, Minns M, Ji S, Chi C, Nugent MA, Trinkaus-Randall V. Hypoxia-induced changes in Ca2+ mobilization and protein phosphorylation implicated in impaired wound healing. Am. J. Physiol. Cell. Physiol. 2014;306:C972–985. doi: 10.1152/ajpcell.00110.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JG, Heur M. Interleukin-1β enhances cell migration through AP-1 and NF-κB pathway-dependent FGF2 expression in human corneal endothelial cells. Biol. Cell. 2013;105:175–189. doi: 10.1111/boc.201200077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JG, Heur M. Interleukin-1β-induced Wnt5a enhances human corneal endothelial cell migration through regulation of Cdc42 and RhoA. Mol. Cell Biol. 2014;34:3535–3545. doi: 10.1128/MCB.01572-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee GA, Hirst LW. Ocular surface squamous neoplasia. Surv. Ophthalmol. 1995;39:429–450. doi: 10.1016/s0039-6257(05)80054-2. [DOI] [PubMed] [Google Scholar]
- Lee JG, Kay EP. FGF-2-induced wound healing in corneal endothelial cells requires Cdc42 activation and Rho inactivation through the phosphatidylinositol 3-kinase pathway. Invest. Ophthalmol. Vis. Sci. 2006;47:1376–1386. doi: 10.1167/iovs.05-1223. [DOI] [PubMed] [Google Scholar]
- Lee JG, Ko MK, Kay EP. Endothelial mesenchymal transformation mediated by IL-1β-induced FGF-2 in corneal endothelial cells. Exp. Eye Res. 2012;95:35–39. doi: 10.1016/j.exer.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Lee HT, Lee JG, Na M, Kay EP. FGF-2 induced by interleukin-1 beta through the action of phosphatidylinositol 3-kinase mediates endothelial mesenchymal transformation in corneal endothelial cells. J. Biol. Chem. 2004;279:32325–32332. doi: 10.1074/jbc.M405208200. [DOI] [PubMed] [Google Scholar]
- Lee HK, Lee JH, Kim M, Kariya Y, Miyazaki K, Kim EK. Insulin-like growth factor-1 induces migration and expression of laminin-5 in cultured human corneal epithelial cells. Invest. Ophthalmol. Vis. Sci. 2006;47:873–882. doi: 10.1167/iovs.05-0826. [DOI] [PubMed] [Google Scholar]
- Lee SH, Leem HS, Jeong SM, Lee K. Bevacizumab accelerates corneal wound healing by inhibiting TGF-β2 expression in alkali-burned mouse cornea. BMB Rep. 2009;42:800–805. doi: 10.5483/bmbrep.2009.42.12.800. [DOI] [PubMed] [Google Scholar]
- Lehrer MS, Sun TT, Lavker RM. Strategies of epithelial repair: modulation of stem cell and transit. amplifying cell proliferation. J. Cell Sci. 1998;111:2867–2875. doi: 10.1242/jcs.111.19.2867. [DOI] [PubMed] [Google Scholar]
- Leung T, Manser E, Tan L, Lim L. A novel serine/threonine kinase binding the Ras-related RhoA GTPase which translocates the kinase to peripheral membranes. J. Biol. Chem. 1995;270:29051–29054. doi: 10.1074/jbc.270.49.29051. [DOI] [PubMed] [Google Scholar]
- Levis H, Daniels JT. New technologies in limbal epithelial stem cell transplantation. Curr. Opin. Biotechnol. 2009;20:593–597. doi: 10.1016/j.copbio.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Li DQ, Tseng SC. Three patterns of cytokine expression potentially involved in epithelial-fibroblast interactions of human ocular surface. J. Cell. Physiol. 1995;163:61–79. doi: 10.1002/jcp.1041630108. [DOI] [PubMed] [Google Scholar]
- Li Q, Weng J, Mohan RR, Bennett GL, Schwall R, Wang ZF, Tabor K, Kim J, Hargrave S, Cuevas KH, Wilson SE. Hepatocyte growth factor and hepatocyte growth factor receptor in the lacrimal gland, tears, and cornea. Invest. Ophthalmol. Vis. Sci. 1996;37:727–39. [PubMed] [Google Scholar]
- Li Q, Ashraf MF, Bekoe NA, Stark WJ, Chan CC, O’Brien TP. The role of apoptosis in the early corneal wound healing after excimer laser keratectomy in the rat. Graefes Arch. Clin. Exp. Ophthalmol. 2000;238:853–860. doi: 10.1007/s004170000182. [DOI] [PubMed] [Google Scholar]
- Li T, Lu L. Epidermal growth factor-induced proliferation requires down-regulation of Pax6 in corneal epithelial cells. J. Biol. Chem. 2005;280:12988–91295. doi: 10.1074/jbc.M412458200. [DOI] [PubMed] [Google Scholar]
- Li SD, Huang L. Non-viral is superior to viral gene delivery. J. Control Release. 2007;123:181–183. doi: 10.1016/j.jconrel.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Li Z, Burns AR, Rumbaut RE, Smith CW. γδ T cells are necessary for platelet and neutrophil accumulation in limbal vessels and efficient epithelial repair after corneal abrasion. Am. J. Pathol. 2007a;171:838–845. doi: 10.2353/ajpath.2007.070008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Burns AR, Smith CW. Lymphocyte function-associated antigen-1-dependent inhibition of corneal wound healing. Am. J. Pathol. 2006a;169:1590–600. doi: 10.2353/ajpath.2006.060415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Rumbaut RE, Burns AR, Smith CW. Platelet response to corneal abrasion is necessary for acute inflammation and efficient re-epithelialization. Invest. Ophthalmol. Vis. Sci. 2006b;47:4794–4802. doi: 10.1167/iovs.06-0381. [DOI] [PubMed] [Google Scholar]
- Li J, Bia H, Zhu Y, Wang XY, Wang F, Zhang JW, Lavker RM, Yu J. Antagomir dependent microRNA-205 reduction enhances adhesion ability of human corneal epithelial keratinocytes. Chinese Med. Sci. J. 2010;25:65–70. doi: 10.1016/s1001-9294(10)60024-7. [DOI] [PubMed] [Google Scholar]
- Li Z, Burns AR, Han L, Rumbaut RE, Smith CW. IL-17 and VEGF are necessary for efficient corneal nerve regeneration. Am. J. Pathol. 2011;178:1106–1116. doi: 10.1016/j.ajpath.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Li B, Jiang H, Wang Y, Qu M, Duan H, Zhou Q, Shi W. Macrophage depletion impairs corneal wound healing after autologous transplantation in mice. PLoS One. 2013;8:e61799. doi: 10.1371/journal.pone.0061799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L, Sheha H, Li J, Tseng SC. Limbal stem cell transplantation: new progresses and challenges. Eye. 2009;23:1946–1953. doi: 10.1038/eye.2008.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liliensiek SJ, Campbell S, Nealey PF, Murphy CJ. The scale of substratum topographic features modulates proliferation of corneal epithelial cells and corneal fibroblasts. J. Biomed. Mater. Res. A. 2006;79:185–192. doi: 10.1002/jbm.a.30744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim P, Fuchsluger TA, Jurkunas UV. Limbal stem cell deficiency and corneal neovascularization. Sem. Ophthalmol. 2009;24:139–148. doi: 10.1080/08820530902801478. [DOI] [PubMed] [Google Scholar]
- Lin D, Halilovic A, Yue P, Bellner L, Wang K, Wang L, Zhang C. Inhibition of miR-205 impairs the wound-healing process in human corneal epithelial cells by targeting KIR4.1 (KCNJ10) Invest. Ophthalmol. Vis. Sci. 2013a;54:6167–6178. doi: 10.1167/iovs.12-11577. [DOI] [PubMed] [Google Scholar]
- Lin KJ, Loi MX, Lien GS, Cheng CF, Pao HY, Chang YC, Ji AT, Ho JH. Topical administration of orbital fat-derived stem cells promotes corneal tissue regeneration. Stem Cell Res. Ther. 2013b;4:72. doi: 10.1186/scrt223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linna T, Tervo T. Real-time confocal microscopic observations on human corneal nerves and wound healing after excimer laser photorefractive keratectomy. Curr. Eye Res. 1997;16:640–649. doi: 10.1076/ceyr.16.7.640.5058. [DOI] [PubMed] [Google Scholar]
- Liu Z, Carvajal M, Carraway CA, Carraway K, Pflugfelder SC. Expression of the receptor tyrosine kinases, epidermal growth factor receptor, ErbB2, and ErbB3, in human ocular surface epithelia. Cornea. 2001;20:81–85. doi: 10.1097/00003226-200101000-00016. [DOI] [PubMed] [Google Scholar]
- Liu J, Saghizadeh M, Tuli SS, Kramerov AA, Lewin AS, Bloom DC, Hauswirth WW, Castro MG, Schultz GS, Ljubimov AV. Different tropism of adenoviruses and adeno-associated viruses to corneal cells: implications for corneal gene therapy. Mol. Vis. 2008;14:2087–2096. [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Smith CW, Zhang W, Burns AR, Li Z. NK Cells Modulate the Inflammatory Response to Corneal Epithelial Abrasion and Thereby Support Wound Healing. J. Pathol. 2012;181:452–462. doi: 10.1016/j.ajpath.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljubimov AV, Burgeson RE, Butkowski RJ, Michael AF, Sun TT, Kenney MC. Human corneal basement membrane heterogeneity: topographical differences in the expression of type IV collagen and laminin isoforms. Lab Invest. 1995;72:461–473. [PubMed] [Google Scholar]
- Ljubimov AV, Burgeson RE, Butkowski RJ, Couchman JR, Wu RR, Ninomiya Y, Sado Y, Maguen E, Nesburn AB, Kenney MC. Extracellular matrix alterations in human corneas with bullous keratopathy. Invest. Ophthalmol. Vis. Sci. 1996a;37:997–1007. [PubMed] [Google Scholar]
- Ljubimov AV, Burgeson RE, Butkowski RJ, Couchman JR, Zardi L, Ninomiya Y, Sado Y, Huang ZS, Nesburn AB, Kenney MC. Basement membrane abnormalities in human eyes with diabetic retinopathy. J Histochem Cytochem. 1996b;44:1469–1479. doi: 10.1177/44.12.8985139. [DOI] [PubMed] [Google Scholar]
- Ljubimov AV, Huang ZS, Huang GH, Burgeson RE, Gullberg D, Miner JH, Ninomiya Y, Sado Y, Kenney MC. Human corneal epithelial basement membrane and integrin alterations in diabetes and diabetic retinopathy. J Histochem Cytochem. 1998a;46:1033–1041. doi: 10.1177/002215549804600907. [DOI] [PubMed] [Google Scholar]
- Ljubimov AV, Alba SA, Burgeson RE, Ninomiya Y, Sado Y, Sun TT, Nesburn AB, Kenney MC, Maguen E. Extracellular matrix changes in human corneas after radial keratotomy. Exp. Eye Res. 1998b;67:265–272. doi: 10.1006/exer.1998.0511. [DOI] [PubMed] [Google Scholar]
- Low TL, Hu SK, Goldstein AL. Complete amino acid sequence of bovine thymosin beta 4: a thymic hormone that induces terminal deoxynucleotidyltransferase activity in thymocyte populations. Proc. Natl. Acad. Sci. U. S. A. 1981;78:1162–1166. doi: 10.1073/pnas.78.2.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L, Reinach P, Kao WW. Corneal epithelial wound healing. Exp. Biol. Med. 2001;226:653–664. doi: 10.1177/153537020222600711. [DOI] [PubMed] [Google Scholar]
- Lu L, Wang L, Li T, Wang J. NF-κB subtypes regulate CCCTC binding factor affecting corneal epithelial cell fate. J. Biol. Chem. 2010;285:9373–9382. doi: 10.1074/jbc.M109.094425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu J, Lee KS, Joo CK. Transactivation of EGFR mediates insulin-stimulated ERK1/2 activation and enhanced cell migration in human corneal epithelial cells. Mol. Vis. 2006;12:1403–1410. [PubMed] [Google Scholar]
- Ma Y, Xu Y, Xiao Z, Yang W, Zhang C, Song E, Du Y, Li L. Reconstruction of chemically burned rat corneal surface by bone marrow-derived human mesenchymal stem cells. Stem Cells. 2006;24:315–321. doi: 10.1634/stemcells.2005-0046. [DOI] [PubMed] [Google Scholar]
- Ma XY, Bao HJ, Cui L, Zou J. The graft of autologous adipose-derived stem cells in the corneal stromal after mechanic damage. PLoS One. 2013;8:e76103. doi: 10.1371/journal.pone.0076103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhyastha R, Madhyastha H, Nakajima Y, Omura S, Maruyama M. MicroRNA signature in diabetic wound healing: promotive role of miR-21 in fibroblast migration. Int. Wound J. 2012;9:355–361. doi: 10.1111/j.1742-481X.2011.00890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen E, Alba SA, Burgeson RE, Butkowski RJ, Michael AF, Kenney MC, Nesburn AB, Ljubimov AV. Alterations of corneal extracellular matrix after multiple refractive procedures: a clinical and immunohistochemical study. Cornea. 1997;16:675–682. [PubMed] [Google Scholar]
- Maguen E, Zorapapel NC, Zieske JD, Ninomiya Y, Sado Y, Kenney MC, Ljubimov AV. Extracellular matrix and matrix metalloproteinase changes in human corneas after complicated laser-assisted in situ keratomileusis (LASIK) Cornea. 2002;21:95–100. doi: 10.1097/00003226-200201000-00020. [DOI] [PubMed] [Google Scholar]
- Maguen E, Maguen B, Regev L, Ljubimov AV. Immunohistochemical evaluation of two corneal buttons with post-LASIK keratectasia. Cornea. 2007;26:983–991. doi: 10.1097/ICO.0b013e3180de1d91. [DOI] [PubMed] [Google Scholar]
- Maguen E, Rabinowitz YS, Regev L, Saghizadeh M, Sasaki T, Ljubimov AV. Alterations of extracellular matrix components and proteinases in human corneal buttons with INTACS for post-laser in situ keratomileusis keratectasia and keratoconus. Cornea. 2008;27:565–573. doi: 10.1097/ICO.0b013e318165b1cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malecaze F, Massoudi D, Fournié P, Tricoire C, Cassagne M, Malbouyres M, Hulmes DJ, Moali C, Galiacy SD. Upregulation of bone morphogenetic protein-1/mammalian tolloid and procollagen C-proteinase enhancer-1 in corneal scarring. Invest. Ophthalmol. Vis. Sci. 2014;55:6712–6721. doi: 10.1167/iovs.13-13800. [DOI] [PubMed] [Google Scholar]
- Mann GB, Fowler KJ, Gabriel A, Nice EC, Williams RL, Dunn AR. Mice with a null mutation of the TGF alpha gene have abnormal skin architecture, wavy hair, and curly whiskers and often develop corneal inflammation. Cell. 1993;73:249–261. doi: 10.1016/0092-8674(93)90227-h. [DOI] [PubMed] [Google Scholar]
- Márquez EB, De Ortueta D, Royo SB, Martínez-Carpio PA. Epidermal growth factor receptor in corneal damage: update and new insights from recent reports. Cutan. Ocul. Toxicol. 2011;30:7–14. doi: 10.3109/15569527.2010.498398. [DOI] [PubMed] [Google Scholar]
- Martin GR, Timpl R. Laminin and other basement membrane components. Annu. Rev. Cell Biol. 1987;3:57–85. doi: 10.1146/annurev.cb.03.110187.000421. [DOI] [PubMed] [Google Scholar]
- Matsuba M, Hutcheon AE, Zieske JD. Localization of thrombospondin-1 and myofibroblasts during corneal wound repair. Exp. Eye Res. 2011;93:534–540. doi: 10.1016/j.exer.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauris J, Woodward AM, Cao Z, Panjwani N, Argüeso P. Molecular basis for MMP9 induction and disruption of epithelial cell-cell contacts by galectin-3. J. Cell Sci. 2014;127:3141–3148. doi: 10.1242/jcs.148510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maycock NJ, Marshall J. Genomics of corneal wound healing: a review of the literature. Acta Ophthalmol. 2014;92:e170–84. doi: 10.1111/aos.12227. [DOI] [PubMed] [Google Scholar]
- Mayo C, Ren R, Rich C, Stepp MA, Trinkaus-Randall V. Regulation by P2X7: epithelial migration and stromal organization in the cornea. Invest. Ophthalmol. Vis. Sci. 2008;49:4384–4391. doi: 10.1167/iovs.08-1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClintock JL, Ceresa BP. Transforming growth factor-α enhances corneal epithelial cell migration by promoting EGFR recycling. Invest. Ophthalmol. Vis. Sci. 2010;51:3455–3461. doi: 10.1167/iovs.09-4386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin P, Sassani JW, Klocek MS, Zagon IS. Diabetic keratopathy and treatment by modulation of the opioid growth factor (OGF) – OGF receptor (OGFr) axis with naltrexone: A review. Brain Res. Bull. 2010;81:236–247. doi: 10.1016/j.brainresbull.2009.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meduri A, Aragona P, Grenga PL, Roszkowska AM. Effect of basic fibroblast growth factor on corneal epithelial healing after photorefractive keratectomy. J. Refract. Surg. 2012;28:220–223. doi: 10.3928/1081597X-20120103-02. [DOI] [PubMed] [Google Scholar]
- Melles GR, Ong TS, Ververs B, van der Wees J. Descemet membrane endothelial keratoplasty (DMEK) Cornea. 2006;25:987–990. doi: 10.1097/01.ico.0000248385.16896.34. [DOI] [PubMed] [Google Scholar]
- Melles GR, SundarRaj N, Binder PS, van der Weiden MM, Wijdh RH, Beekhuis WH, Anderson JA. Immunohistochemical analysis of unsutured and sutured corneal wound healing. Curr. Eye Res. 1995;14:809–817. doi: 10.3109/02713689508995803. [DOI] [PubMed] [Google Scholar]
- Meltendorf C, Burbach GJ, Ohrloff C, Ghebremedhin E, Deller T. Intrastromal keratotomy with femtosecond laser avoids profibrotic TGF-β1 induction. Invest. Ophthalmol. Vis. Sci. 2009;50:3688–3695. doi: 10.1167/iovs.08-2699. [DOI] [PubMed] [Google Scholar]
- Meyer-Blazejewska EA, Call MK, Yamanaka O, Liu H, Schlötzer-Schrehardt U, Kruse FE, Kao WW. From hair to cornea: toward the therapeutic use of hair follicle-derived stem cells in the treatment of limbal stem cell deficiency. Stem Cells. 2011;29:57–66. doi: 10.1002/stem.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mi S, Connon CJ. The formation of a tissue-engineered cornea using plastically compressed collagen scaffolds and limbal stem cells. Methods Mol. Biol. 2013;1014:143–155. doi: 10.1007/978-1-62703-432-6_9. [DOI] [PubMed] [Google Scholar]
- Micera A, Lambiase A, Aloe L, Bonini S, Levi-Schaffer F, Bonini S. Nerve growth factor involvement in the visual system: implications in allergic and neurodegenerative diseases. Cytokine Growth Factor Rev. 2004;15:411–417. doi: 10.1016/j.cytogfr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Micera A, Lambiase A, Puxeddu I, Aloe L, Stampachiacchiere B, Levi-Schaffer F, Bonini S, Bonini S. Nerve growth factor effect on human primary fibroblastic-keratocytes: Possible mechanism during corneal healing. Exp. Eye Res. 2006;83:747–757. doi: 10.1016/j.exer.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Milani BY, Milani FY, Park DW, Namavari A, Shah J, Amirjamshidi H, Ying H, Djalilian AR. Rapamycin inhibits the production of myofibroblasts and reduces corneal scarring after photorefractive keratectomy. Invest. Ophthalmol. Vis. Sci. 2013;54:7424–7430. doi: 10.1167/iovs.13-12674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimura T, Yamagami S, Amano S. Corneal endothelial regeneration and tissue engineering. Prog. Retin. Eye Res. 2013;35:1–17. doi: 10.1016/j.preteyeres.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Mishima H, Nakamura M, Murakami J, Nishida T, Otori T. Transforming growth factor-beta modulates effects of epidermal growth factor on corneal epithelial cells. Curr. Eye Res. 1992;11:691–696. doi: 10.3109/02713689209000742. [DOI] [PubMed] [Google Scholar]
- Miyamoto T, Sumioka T, Saika S. Endothelial mesenchymal transition: a therapeutic target in retrocorneal membrane. Cornea. 2010;29(Suppl 1):S52–56. doi: 10.1097/ICO.0b013e3181efe36a. [DOI] [PubMed] [Google Scholar]
- Miyazaki K, Okada Y, Yamanaka O, Kitano A, Ikeda K, Kon S, Uede T, Rittling SR, Denhardt DT, Kao WW, Saika S. Corneal wound healing in an osteopontin-deficient mouse. Invest. Ophthalmol. Vis. Sci. 2008;49:1367–1375. doi: 10.1167/iovs.07-1007. [DOI] [PubMed] [Google Scholar]
- Mohan R, Chintala SK, Jung JC, Villar WV, McCabe F, Russo LA, Lee Y, McCarthy BE, Wollenberg KR, Jester JV, Wang M, Welgus HG, Shipley JM, Senior RM, Fini ME. Matrix metalloproteinase gelatinase B (MMP-9) coordinates and effects epithelial regeneration. J. Biol. Chem. 2002;277:2065–2072. doi: 10.1074/jbc.M107611200. [DOI] [PubMed] [Google Scholar]
- Mohan RR, Gupta R, Mehan MK, Cowden JW, Sinha S. Decorin transfection suppresses profibrogenic genes and myofibroblast formation in human corneal fibroblasts. Exp. Eye Res. 2010;91:238–245. doi: 10.1016/j.exer.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohan RR, Schultz GS, Hong JW, Mohan RR, Wilson SE. Gene transfer into rabbit keratocytes using AAV and lipid-mediated plasmid DNA vectors with a lamellar flap for stromal access. Exp Eye Res. 2003;76:373–383. doi: 10.1016/s0014-4835(02)00275-0. [DOI] [PubMed] [Google Scholar]
- Mohan RR, Sharma A, Netto MV, Sinha S, Wilson SE. Gene therapy in the cornea. Prog. Retin. Eye Res. 2005;24:537–59. doi: 10.1016/j.preteyeres.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Mohan RR, Tandon A, Sharma A, Cowden JW, Tovey JC. Significant inhibition of corneal scarring in vivo with tissue-selective, targeted AAV5 decorin gene therapy. Invest. Ophthalmol. Vis. Sci. 2011a;52:4833–4841. doi: 10.1167/iovs.11-7357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Møller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV. Neutralizing antibody to TGFβ modulates stromal fibrosis but not regression of photoablative effect following PRK. Curr. Eye Res. 1998;17:736–747. [PubMed] [Google Scholar]
- Møller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV. Stromal wound healing explains refractive instability and haze development after photorefractive keratectomy: a 1-year confocal microscopic study. Ophthalmology. 2000;107:1235–1245. doi: 10.1016/s0161-6420(00)00142-1. [DOI] [PubMed] [Google Scholar]
- Monteiro BG, Serafim RC, Melo GB, Silva MC, Lizier NF, Maranduba CM, Smith RL, Kerkis A, Cerruti H, Gomes JA, Kerkis I. Human immature dental pulp stem cells share key characteristic features with limbal stem cells. Cell Prolif. 2009;42:587–594. doi: 10.1111/j.1365-2184.2009.00623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morishige N, Kesler-Diaz A, Wahlert AJ, Kurtz RM, Juhasz T, Sarayba M, Jester JV. Corneal response to femtosecond laser photodisruption in the rabbit. Exp. Eye Res. 2008;86:835–843. doi: 10.1016/j.exer.2008.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morita S, Shirakata Y, Shiraishi A, Kadota Y, Hashimoto K, Higashiyama S, Ohashi Y. Human corneal epithelial cell proliferation by epiregulin and its cross-induction by other EGF family members. Mol. Vis. 2007;13:2119–2128. [PubMed] [Google Scholar]
- Mott JD, Werb Z. Regulation of matrix biology by matrix metalloproteinases. Curr. Opin. Cell Biol. 2004;16:558–564. doi: 10.1016/j.ceb.2004.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulik S, Bhela S, Rouse BT. Potential function of miRNAs in herpetic stromal keratitis. Invest. Ophthalmol. Vis. Sci. 2013;54:563–573. doi: 10.1167/iovs.12-11094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munjal ID, Crawford DR, Blake DA, Sabet MD, Gordon SR. Thrombospondin: biosynthesis, distribution, and changes associated with wound repair in corneal endothelium. Eur. J. Cell Biol. 1990;52:252–263. [PubMed] [Google Scholar]
- Murakami J, Nishida T, Otori T. Coordinated appearance of beta 1 integrins and fibronectin during corneal wound healing. J. Lab. Clin. Med. 1992;120:86–93. [PubMed] [Google Scholar]
- Nagano T, Nakamura M, Nakata K, Yamaguchi T, Takase K, Okahara A, Ikuse T, Nishida T. Effects of substance P and IGF-1 in corneal epithelial barrier function and wound healing in a rat model of neurotrophic keratopathy. Invest. Ophthalmol. Vis. Sci. 2003;44:3810–3815. doi: 10.1167/iovs.03-0189. [DOI] [PubMed] [Google Scholar]
- Nagase H, Brew K. Designing TIMP (tissue inhibitor of metalloproteinases) variants that are selective metalloproteinase inhibitors. Biochem. Soc. Symp. 2003;70:201–212. doi: 10.1042/bss0700201. [DOI] [PubMed] [Google Scholar]
- Nakamura M, Ofuji K, Chikama T, Nishida T. Combined effects of substance P and insulin-like growth factor-1 on corneal epithelial wound closure of rabbit in vivo. Curr. Eye Res. 1997;16:275–278. doi: 10.1076/ceyr.16.3.275.15409. [DOI] [PubMed] [Google Scholar]
- Nakamura M, Nishida T. Differential effects of epidermal growth factor and interleukin 6 on corneal epithelial cells and vascular endothelial cells. Cornea. 1999;18:452–458. doi: 10.1097/00003226-199907000-00011. [DOI] [PubMed] [Google Scholar]
- Nakamura Y, Sotozono C, Kinoshita S. The epidermal growth factor receptor (EGFR): role in corneal wound healing and homeostasis. Exp. Eye Res. 2001;72:511–517. doi: 10.1006/exer.2000.0979. [DOI] [PubMed] [Google Scholar]
- Nakamura M, Kawahara M, Morishige N, Chikama T, Nakata K, Nishida T. Promotion of corneal epithelial wound healing in diabetic rats by the combination of a substance P-derived peptide (FGLM-NH2) and insulin-like growth factor-1. Diabetologia. 2003;46:839–842. doi: 10.1007/s00125-003-1105-9. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Takeda K, Inatomi T, Sotozono C, Kinoshita S. Long-term results of autologous cultivated oral mucosal epithelial transplantation in the scar phase of severe ocular surface disorders. Br. J. Ophthalmol. 2011;95:942–946. doi: 10.1136/bjo.2010.188714. [DOI] [PubMed] [Google Scholar]
- Nakano Y, Oyamada M, Dai P, Nakagami T, Kinoshita S, Takamatsu T. Connexin43 knockdown accelerates wound healing but inhibits mesenchymal transition after corneal endothelial injury in vivo. Invest. Ophthalmol. Vis. Sci. 2008;49:93–104. doi: 10.1167/iovs.07-0255. [DOI] [PubMed] [Google Scholar]
- Nakayasu K. Stromal changes following removal of epithelium in rat cornea. Jpn. J. Ophthalmol. 1988;32:113–125. [PubMed] [Google Scholar]
- Nakayasu K, Tanaka M, Konomi H, Hayashi T. Distribution of types I, II, III, IV and V collagen in normal and keratoconus corneas. Ophthalmic Res. 1986;18:1–10. doi: 10.1159/000265406. [DOI] [PubMed] [Google Scholar]
- Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM. Matrix metalloproteinases: Biologic activity and clinical implications. J. Clin. Oncol. 2000;18:1135–1149. doi: 10.1200/JCO.2000.18.5.1135. [DOI] [PubMed] [Google Scholar]
- Netto MV, Mohan RR, Ambrósio R, Jr., Hutcheon AE, Zieske JD, Wilson SE. Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy. Cornea. 2005;24:509–522. doi: 10.1097/01.ico.0000151544.23360.17. [DOI] [PubMed] [Google Scholar]
- Netto MV, Mohan RR, Sinha S, Sharma A, Dupps W, Wilson SE. Stromal haze, myofibroblasts, and surface irregularity after PRK. Exp. Eye Res. 2006;82:788–797. doi: 10.1016/j.exer.2005.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickeleit V, Kaufman AH, Zagachin L, Dutt JE, Foster CS, Colvin RB. Healing corneas express embryonic fibronectin isoforms in the epithelium, subepithelial stroma, and endothelium. Am. J. Pathol. 1996;149:549–558. [PMC free article] [PubMed] [Google Scholar]
- Nishida T. Translational research in corneal epithelial wound healing. Eye Contact Lens. 2010;36:300–304. doi: 10.1097/ICL.0b013e3181f016d0. [DOI] [PubMed] [Google Scholar]
- Nishida T, Nakamura M, Mishima H, Otori T. Differential modes of action of fibronectin and epidermal growth factor on rabbit corneal epithelial migration. J. Cell Physiol. 1990;145:549–554. doi: 10.1002/jcp.1041450323. [DOI] [PubMed] [Google Scholar]
- Nishida K, Kinoshita S, Yokoi N, Kaneda M, Hashimoto K, Yamamoto S. Immunohistochemical localization of transforming growth factor-β1, -β2, and -β3 latency-associated peptide in human cornea. Invest. Ophthalmol. Vis. Sci. 1994;35:3289–3294. [PubMed] [Google Scholar]
- Nishida T, Nakamura M, Ofuji K, Reid TW, Mannis MJ, Murphy CJ. Synergistic effects of substance P with insulin-like growth factor-1 on epithelial migration of the cornea. J. Cell. Physiol. 1996;169:159–166. doi: 10.1002/(SICI)1097-4652(199610)169:1<159::AID-JCP16>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Noisa P, Ramasamy TS, Lamont FR, Yu JS, Sheldon MJ, Russell A, Jin X, Cui W. Identification and characterisation of the early differentiating cells in neural differentiation of human embryonic stem cells. PLoS One. 2012;7:e37129. doi: 10.1371/journal.pone.0037129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okadal Y, Saika S, Hashizume l.N., Kobatal S, Yamanaka O, Ohnishi Y, Senba E. Expression of fos family and jun family proto-oncogenes during corneal epithelial wound healing. Curr. Eye Res. 1996;15:824–832. doi: 10.3109/02713689609017623. [DOI] [PubMed] [Google Scholar]
- Okumura N, Koizumi N, Ueno M, Sakamoto Y, Takahashi H, Hamuro J, Kinoshita S. The new therapeutic concept of using a rho kinase inhibitor for the treatment of corneal endothelial dysfunction. Cornea. 2011a;30(Suppl 1):S54–59. doi: 10.1097/ICO.0b013e3182281ee1. [DOI] [PubMed] [Google Scholar]
- Okumura N, Koizumi N, Ueno M, Sakamoto Y, Takahashi H, Hirata K, Torii R, Hamuro J, Kinoshita S. Enhancement of corneal endothelium wound healing by Rho-associated kinase (ROCK) inhibitor eye drops. Br. J. Ophthalmol. 2011b;95:1006–1009. doi: 10.1136/bjo.2010.194571. [DOI] [PubMed] [Google Scholar]
- Okumura N, Koizumi N, Kay EP, Ueno M, Sakamoto Y, Nakamura S, Hamuro J, Kinoshita S. The ROCK inhibitor eye drop accelerates corneal endothelium wound healing. Invest. Ophthalmol. Vis. Sci. 2013a;54:2493–2502. doi: 10.1167/iovs.12-11320. [DOI] [PubMed] [Google Scholar]
- Okumura N, Kay EP, Nakahara M, Hamuro J, Kinoshita S, Koizumi N. Inhibition of TGF-β signaling enables human corneal endothelial cell expansion in vitro for use in regenerative medicine. PLoS One. 2013b;8:e58000. doi: 10.1371/journal.pone.0058000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura N, Nakano S, Kay EP, Numata R, Ota A, Sowa Y, Sakai T, Ueno M, Kinoshita S, Koizumi N. Involvement of cyclin D and p27 in cell proliferation mediated by ROCK inhibitors Y-27632 and Y-39983 during corneal endothelium wound healing. Invest. Ophthalmol. Vis. Sci. 2014;55:318–329. doi: 10.1167/iovs.13-12225. [DOI] [PubMed] [Google Scholar]
- Oliveira LA, Kim C, Sousa LB, Schwab IR, Rosenblatt MI. Gene transfer to primary corneal epithelial cells with an integrating lentiviral vector. Arq. Bras. Oftalmol. 2010;73:447–453. doi: 10.1590/s0004-27492010000500012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ono K, Yokoo S, Mimura T, Usui T, Miyata K, Araie M, Yamagami S, Amano S. Autologous transplantation of conjunctival epithelial cells cultured on amniotic membrane in a rabbit model. Mol. Vis. 2007;13:1138–1143. [PMC free article] [PubMed] [Google Scholar]
- Ordonez P, Di Girolamo N. Limbal epithelial stem cells: role of the niche microenvironment. Stem Cells. 2012;30:100–107. doi: 10.1002/stem.794. [DOI] [PubMed] [Google Scholar]
- Ottino P, Taheri F, Bazan HE. Platelet-activating factor induces the gene expression of TIMP-1, -2, and PAI-1: imbalance between the gene expression of MMP-9 and TIMP-1 and -2. Exp. Eye Res. 2002;74:393–402. doi: 10.1006/exer.2001.1135. [DOI] [PubMed] [Google Scholar]
- Pal-Ghosh S, Blanco T, Tadvalkar G, Pajoohesh-Ganji A, Parthasarathy A, Zieske JD, Stepp MA. MMP9 cleavage of the β4 integrin ectodomain leads to recurrent epithelial erosions in mice. J. Cell Sci. 2011a;124:2666–2675. doi: 10.1242/jcs.085480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal-Ghosh S, Pajoohesh-Ganji A, Tadvalkar G, Stepp MA. Removal of the basement membrane enhances corneal wound healing. Exp. Eye Res. 2011b;93:927–936. doi: 10.1016/j.exer.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pancholi S, Tullo A, Khaliq A, Foreman D, Boulton M. The effects of growth factors and conditioned media on the proliferation of human corneal epithelial cells and keratocytes. Graefes Arch. Clin. Exp. Ophthalmol. 1998;236:1–8. doi: 10.1007/s004170050034. [DOI] [PubMed] [Google Scholar]
- Parker DG, Coster DJ, Brereton HM, Hart PH, Koldej R, Anson DS, Williams KA. Lentivirus-mediated gene transfer of interleukin 10 to the ovine and human cornea. Clin. Exp. Ophthalmol. 2010;38:405–413. doi: 10.1111/j.1442-9071.2010.02261.x. [DOI] [PubMed] [Google Scholar]
- Pearlman E, Johnson A, Adhikary G, Sun Y, Chinnery HR, Fox T, Kester M, McMenamin PG. Toll-like receptors at the ocular surface. Ocul. Surf. 2008;6:108–116. doi: 10.1016/s1542-0124(12)70279-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini G, Traverso CE, Franzi AT, Zingirian M, Cancedda R, De Luca M. Lancet. 1997;349:990–993. doi: 10.1016/S0140-6736(96)11188-0. [DOI] [PubMed] [Google Scholar]
- Pellegrini G, Golisano O, Paterna P, Lambiase A, Bonini S, Rama P, De Luca M. Location and clonal analysis of stem cells and their differentiated progeny in the human ocular surface. J. Cell Biol. 1999;145:769–82. doi: 10.1083/jcb.145.4.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini G, Rama P, Mavilio F, De Luca M. Epithelial stem cells in corneal regeneration and epidermal gene therapy. J. Pathol. 2009;217:217–228. doi: 10.1002/path.2441. [DOI] [PubMed] [Google Scholar]
- Pellegrini G, Rama P, De Luca M. Vision from the right stem. Trends Mol. Med. 2011;17:1–7. doi: 10.1016/j.molmed.2010.10.003. [DOI] [PubMed] [Google Scholar]
- Pellegrini G, Rama P, Di Rocco A, Panaras A, De Luca M. Concise review: hurdles in a successful example of limbal stem cell-based regenerative medicine. Stem Cells. 2014;32:26–34. doi: 10.1002/stem.1517. [DOI] [PubMed] [Google Scholar]
- Peng H, Park JK, Katsnelson J, Kaplan N, Yang W, Getsios S, Lavker RM. microRNA-103/107 family regulates multiple epithelial stem cell characteristics. Stem Cells. 2015;33:1642–1656. doi: 10.1002/stem.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Santonja JJ, Linna TU, Tervo KM, Sakla HF, Alió y Sanz JL, Tervo TM. Corneal wound healing after laser in situ keratomileusis in rabbits. J. Refract Surg. 1998;14:602–609. doi: 10.3928/1081-597X-19981101-06. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Phelps ED, Doll MA, Schaal S, Ceresa BP. The role of endogenous epidermal growth factor receptor ligands in mediating corneal epithelial homeostasis. Invest. Ophthalmol. Vis. Sci. 2014;55:2870–2880. doi: 10.1167/iovs.13-12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petroll WM, Barry-Lane PA, Cavanagh HD, Jester JV. ZO-1 reorganization and myofibroblast transformation of corneal endothelial cells after freeze injury in the cat. Exp. Eye Res. 1997;64:257–267. doi: 10.1006/exer.1996.0211. [DOI] [PubMed] [Google Scholar]
- Petroll WM, Bowman RW, Cavanagh HD, Verity SM, Mootha VV, McCulley JP. Assessment of keratocyte activation following LASIK with flap creation using the IntraLase FS60 laser. J. Refract Surg. 2008;24:847–849. doi: 10.3928/1081597x-20081001-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petznick A, Madigan MC, Garrett Q, Sweeney DF, Evans MD. Contributions of ocular surface components to matrix-metalloproteinases (MMP)-2 and MMP-9 in feline tears following corneal epithelial wounding. PLoS One. 2013;8:e7194. doi: 10.1371/journal.pone.0071948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinarli FA, Okten G, Beden U, Fişgin T, Kefeli M, Kara N, Duru F, Tomak L. Keratinocyte growth factor-2 and autologous serum potentiate the regenerative effect of mesenchymal stem cells in cornea damage in rats. Int. J. Ophthalmol. 2014;7:211–219. doi: 10.3980/j.issn.2222-3959.2014.02.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pipparelli A, Arsenijevic Y, Thuret G, Gain P, Nicolas M, Majo F. ROCK inhibitor enhances adhesion and wound healing of human corneal endothelial cells. PLoS One. 2013;8:e62095. doi: 10.1371/journal.pone.0062095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power WJ, Kaufman AH, Merayo-Lloves J, Arrunategui-Correa V, Foster CS. Expression of collagens I, III, IV and V mRNA in excimer wounded rat cornea: analysis by semi-quantitative PCR. Curr. Eye Res. 1995;14:879–886. doi: 10.3109/02713689508995127. [DOI] [PubMed] [Google Scholar]
- Price MO, Price FW. Descemet’s stripping endothelial keratoplasty. Curr. Opin. Ophthalmol. 2007;18:290–294. doi: 10.1097/ICU.0b013e3281a4775b. 2007. [DOI] [PubMed] [Google Scholar]
- Priglinger SG, May CA, Alge CS, Wolf A, Neubauer AS, Haritoglou C, Kampik A, Welge-Lussen U. Immunohistochemical findings after LASIK confirm in vitro LASIK model. Cornea. 2006;25:331–335. doi: 10.1097/01.ico.0000183535.99651.7b. [DOI] [PubMed] [Google Scholar]
- Proulx S, d’Arc Uwamaliya J, Carrier P, Deschambeault A, Audet C, Giasson CJ, Guérin SL, Auger FA, Germain L. Reconstruction of a human cornea by the self-assembly approach of tissue engineering using the three native cell types. Mol Vis. 2010;16:2192–201. [PMC free article] [PubMed] [Google Scholar]
- Qazi Y, Stagg B, Singh N, Singh S, Zhang X, Luo L, Simonis J, Kompella UB, Ambati BK. Nanoparticle-mediated delivery of shRNA. VEGF-A plasmids regresses corneal neovascularization. Invest. Ophthalmol. Vis. Sci. 2012;53:2837–2844. doi: 10.1167/iovs.11-9139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Y, Chi W, Hua X, Deng R, Li J, Liu Z, Pflugfelder SC, Li DQ. Unique expression pattern and functional role of periostin in human limbal stem cells. PLoS One. 2015;10:e0117139. doi: 10.1371/journal.pone.0117139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael B, Kerr NC, Shimizu RW, Lass JH, Crouthamel KC, Glaser SR, Stern GA, McLaughlin BJ, Musch DC, Duzman E. Enhanced healing of cat corneal endothelial wounds by epidermal growth factor. Invest. Ophthalmol. Vis. Sci. 1993;34:2305–2312. [PubMed] [Google Scholar]
- Rama P, Matuska S, Paganoni G, Spinelli A, De Luca M, Pellegrini G. Limbal stem-cell therapy and longterm corneal regeneration. N. Engl. J. Med. 2010;363:147–155. doi: 10.1056/NEJMoa0905955. [DOI] [PubMed] [Google Scholar]
- Reinshagen H, Auw-Haedrich C, Sorg RV, Boehringer D, Eberwein P, Schwartzkopff J, Sundmacher R, Reinhard T. Corneal surface reconstruction using adult mesenchymal stem cells in experimental limbal stem cell deficiency in rabbits. Acta Ophthalmol. 2011;89:741–8. doi: 10.1111/j.1755-3768.2009.01812.x. [DOI] [PubMed] [Google Scholar]
- Rieck PW, Cholidis S, Hartmann C. Intracellular signaling pathway of FGF-2-modulated corneal endothelial cell migration during wound healing in vitro. Exp. Eye Res. 2001;73:639–650. doi: 10.1006/exer.2001.1067. [DOI] [PubMed] [Google Scholar]
- Ríos JD, Ghinelli E, Gu J, Hodges RR, Dartt DA. Role of neurotrophins and neurotrophin receptors in rat conjunctival goblet cell secretion and proliferation. Invest. Ophthalmol. Vis. Sci. 2007;48:1543–1551. doi: 10.1167/iovs.06-1226. [DOI] [PubMed] [Google Scholar]
- Rosen EM, Nigam SK, Goldberg ID. Scatter factor and the c-met receptor: a paradigm for mesenchymal/epithelial interaction. J. Cell Biol. 1994;127:1783–1787. doi: 10.1083/jcb.127.6.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy S, Sen CK. MiRNA in innate immune responses: novel players in wound inflammation. Physiol Genomics. 2011;43:557–565. doi: 10.1152/physiolgenomics.00160.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush JS, Boeving MA, Berry WL, Ceresa BP. Antagonizing c-Cbl enhances EGFR-dependent corneal epithelial homeostasis. Invest. Ophthalmol. Vis. Sci. 2014;55:4691–4699. doi: 10.1167/iovs.14-14133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Ederra J, Verkman AS. Aquaporin-1-facilitated keratocyte migration in cell culture and in vivo corneal wound healing models. Exp. Eye Res. 2009;89:159–165. doi: 10.1016/j.exer.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatier P, Rieck P, Daumer ML, Courtois Y, Pouliquen Y, Hartmann C. Effects of human recombinant basic fibroblast growth factor on endothelial wound healing in organ culture of human cornea. J. Fr. Ophtalmol. 1996;19:200–207. [PubMed] [Google Scholar]
- Saghizadeh M, Brown DJ, Castellon R, Chwa M, Huang GH, Ljubimova JY, Rosenberg S, Spirin KS, Stolitenko RB, Adachi W, Kinoshita S, Murphy G, Windsor LJ, Kenney MC, Ljubimov AV. Overexpression of matrix metalloproteinase-10 and matrix metalloproteinase-3 in human diabetic corneas: a possible mechanism of basement membrane and integrin alterations. Am. J. Pathol. 2001a;158:723–734. doi: 10.1016/S0002-9440(10)64015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saghizadeh M, Chwa M, Aoki A, Lin B, Pirouzmanesh A, Brown DJ, Ljubimov AV, Kenney MC. Altered expression of growth factors and cytokines in keratoconus, bullous keratopathy and diabetic human corneas. Exp. Eye Res. 2001b;73:179–189. doi: 10.1006/exer.2001.1028. [DOI] [PubMed] [Google Scholar]
- Saghizadeh M, Kramerov AA, Tajbakhsh J, Aoki AM, Wang C, Chai NN, Ljubimova JY, Sasaki T, Sosne G, Carlson MR, Nelson SF, Ljubimov AV. Proteinase and growth factor alterations revealed by gene microarray analysis of human diabetic corneas. Invest. Ophthalmol. Vis. Sci. 2005;46:3604–3615. doi: 10.1167/iovs.04-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saghizadeh M, Kramerov AA, Yu FS, Castro MG, Ljubimov AV. Normalization of wound healing and diabetic markers in organ cultured human diabetic corneas by adenoviral delivery of c-met gene. Invest. Ophthalmol Vis. Sci. 2010a;51:1970–1980. doi: 10.1167/iovs.09-4569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saghizadeh M, Kramerov AA, Yaghoobzadeh Y, Hu J, Ljubimova JY, Black KL, Castro MG, Ljubimov AV. Adenovirus-driven overexpression of proteinases in organ-cultured normal human corneas leads to diabetic-like changes. Brain Res. Bull. 2010b;81:262–272. doi: 10.1016/j.brainresbull.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saghizadeh M, Soleymani S, Harounian A, Bhakta B, Troyanovsky SM, Brunken WJ, Pellegrini G, Ljubimov AV. Alterations of epithelial stem cell marker patterns in human diabetic corneas and effects of c-met gene therapy. Mol Vis. 2011;17:2177–2190. [PMC free article] [PubMed] [Google Scholar]
- Saghizadeh M, Brown J, Ljubimov AV, Funari VA. miRNA expression profiling in central and limbal diabetic and normal human corneas using deep sequencing. Invest. Ophthalmol. Vis. Sci. 2013a;54:3229. EAbstract. [Google Scholar]
- Saghizadeh M, Dib CM, Brunken WJ, Ljubimov AV. Normalization of wound healing and stem cell marker patterns in organ-cultured human diabetic corneas by gene therapy of limbal cells. Exp. Eye Res. 2014;129:66–73. doi: 10.1016/j.exer.2014.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saghizadeh M, Epifantseva I, Hemmati DM, Ghiam CA, Brunken WJ, Ljubimov AV. Enhanced wound healing, kinase and stem cell marker expression in diabetic organ-cultured human corneas upon MMP-10 and cathepsin F gene silencing. Invest. Ophthalmol. Vis. Sci. 2013b;54:8172–8180. doi: 10.1167/iovs.13-13233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saika S, Kobata S, Hashizume N, Okada Y, Yamanaka O. Epithelial basement membrane in alkali-burned corneas in rats. Immunohistochemical study. Cornea. 1993;12:383–390. doi: 10.1097/00003226-199309000-00003. [DOI] [PubMed] [Google Scholar]
- Saika S, Ohnishi Y, Ooshima A, Liu CY, Kao WW. Epithelial repair: roles of extracellular matrix. Cornea. 2002;21(Suppl 1):S23–29. doi: 10.1097/00003226-200203001-00006. [DOI] [PubMed] [Google Scholar]
- Saika S, Kono-Saika S, Ohnishi Y, Sato M, Muragaki Y, Ooshima A, Flanders KC, Yoo J, Anzano M, Liu CY, Kao WW, Roberts AB. Smad3 signaling is required for epithelial–mesenchymal transition of lens epithelium after injury. Am. J. Pathol. 2004a;164:651–663. doi: 10.1016/S0002-9440(10)63153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saika S, Okada Y, Miyamoto T, Yamanaka O, Ohnishi Y, Ooshima A, Liu CY, Weng D, Kao WW. Role of p38 MAP kinase in regulation of cell migration and proliferation in healing corneal epithelium. Invest. Ophthalmol. Vis. Sci. 2004b;45:100–109. doi: 10.1167/iovs.03-0700. [DOI] [PubMed] [Google Scholar]
- Saika S, Sumioka T, Okada Y, Yamanaka O, Kitan A, Miyamoto T, Shirai K, Kokado H. Wakayama symposium: modulation of wound healing response in the corneal stroma by osteopontin and tenascin-C. Ocul. Surf. 2013;11:12–15. doi: 10.1016/j.jtos.2012.09.002. [DOI] [PubMed] [Google Scholar]
- Sakurai M, Hayashi R, Kageyama T, Yamato M, Nishida K. Induction of putative stratified epithelial progenitor cells in vitro from mouse-induced pluripotent stem cells. J. Artif. Organs. 2011;14:58–66. doi: 10.1007/s10047-010-0547-3. [DOI] [PubMed] [Google Scholar]
- Salani B, Briatore L, Contini P, Passalacqua M, Melloni E, Paggi A, Cordera R, Maggi D. IGF-I induced rapid recruitment of integrin β1 to lipid rafts is caveolin-1 dependent. Biochem. Biophys. Res. Commun. 2009;380:489–492. doi: 10.1016/j.bbrc.2009.01.102. [DOI] [PubMed] [Google Scholar]
- Sareen D, Saghizadeh M, Ornelas L, Winkler MA, Narwani K, Sahabian A, Funari VA, Tang J, Spurka L, Punj V, Maguen E, Rabinowitz YS, Svendsen CN, Ljubimov AV. Differentiation of human limbal-derived induced pluripotent stem cells into limbal-like epithelium. Stem Cells Transl. Med. 2014;3:1002–1012. doi: 10.5966/sctm.2014-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schermer A, Galvin S, Sun TT. Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. J. Cell Biol. 1986;103:49–62. doi: 10.1083/jcb.103.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlötzer-Schrehardt U, Dietrich T, Saito K, Sorokin L, Sasaki T, Paulsson M, Kruse FE. Characterization of extracellular matrix components in the limbal epithelial stem cell compartment. Exp. Eye Res. 2007;85:845–60. doi: 10.1016/j.exer.2007.08.020. [DOI] [PubMed] [Google Scholar]
- Schmack I, Dawson DG, McCarey BE, Waring GO, 3rd, Grossniklaus HE, Edelhauser HF. Cohesive tensile strength of human LASIK wounds with histologic, ultrastructural, and clinical correlations. J. Refract. Surg. 2005;21:433–445. doi: 10.3928/1081-597X-20050901-04. [DOI] [PubMed] [Google Scholar]
- Seomun Y, Joo CK. Lumican induces human corneal epithelial cell migration and integrin expression via ERK 1/2 signaling. Biochem. Biophys. Res. Commun. 2008;372:221–225. doi: 10.1016/j.bbrc.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Shahdadfar A, Haug K, Pathak M, Drolsum L, Olstad OK, Johnsen EO, Petrovski G, Moe MC, Nicolaissen B. Ex vivo expanded autologous limbal epithelial cells on amniotic membrane using a culture medium with human serum as single supplement. Exp. Eye Res. 2012;97:1–9. doi: 10.1016/j.exer.2012.01.013. [DOI] [PubMed] [Google Scholar]
- Shanley LJ, McCaig CD, Forrester JV, Zhao M. Insulin, not leptin, promotes in vitro cell migration to heal monolayer wounds in human corneal epithelium. Invest. Ophthalmol. Vis. Sci. 2004;45:1088–1094. doi: 10.1167/iovs.03-1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanmuganathan VA, Rotchford AP, Tullo AB, Joseph A, Zambrano I, Dua HS. Epithelial proliferative potential of organ cultured corneoscleral rims; implications for allo-limbal transplantation and eye banking. Br. J. Ophthalmol. 2006;90:55–58. doi: 10.1136/bjo.2005.071910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma GD, He J, Bazan HE. p38 and ERK1/2 coordinate cellular migration and proliferation in epithelial wound healing: evidence of cross-talk activation between MAP kinase cascades. J. Biol. Chem. 2003;278:21989–21997. doi: 10.1074/jbc.M302650200. [DOI] [PubMed] [Google Scholar]
- Shi L, Chang Y, Yang Y, Zhang Y, Yu FS, Wu X. Activation of JNK signaling mediates connective tissue growth factor expression and scar formation in corneal wound healing. PLoS One. 2012;7:e32128. doi: 10.1371/journal.pone.0032128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh V, Barbosa FL, Torricelli AA, Santhiago MR, Wilson SE. Transforming growth factor β and platelet-derived growth factor modulation of myofibroblast development from corneal fibroblasts in vitro. Exp. Eye Res. 2014;120:152–160. doi: 10.1016/j.exer.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh V, Santhiago MR, Barbosa FL, Agrawal V, Singh N, Ambati BK, Wilson SE. Effect of TGFβ and PDGF-B blockade on corneal myofibroblast development in mice. Exp. Eye Res. 2011;93:810–817. doi: 10.1016/j.exer.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh V, Torricelli AA, Nayeb-Hashemi N, Agrawal V, Wilson SE. Mouse strain variation in SMA(+) myofibroblast development after corneal injury. Exp. Eye Res. 2013;115:27–30. doi: 10.1016/j.exer.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivak JM, Fini ME. MMPs in the eye: emerging roles for matrix metalloproteinases in ocular physiology. Prog. Retin. Eye Res. 2002;21:1–14. doi: 10.1016/s1350-9462(01)00015-5. [DOI] [PubMed] [Google Scholar]
- Soltau JB, McLaughlin BJ. Effects of growth factors on wound healing in serum-deprived kitten corneal endothelial cell cultures. Cornea. 1993;12:208–215. doi: 10.1097/00003226-199305000-00005. [DOI] [PubMed] [Google Scholar]
- Sosne G, Szliter EA, Barrett R, Kernacki KA, Kleinman H, Hazlett LD. Thymosin β4 promotes corneal wound healing and decreases inflammation in vivo following alkali injury. Exp. Eye Res. 2002;74:293–299. doi: 10.1006/exer.2001.1125. [DOI] [PubMed] [Google Scholar]
- Sosne G, Siddiqi A, Kurpakus-Wheater M. Thymosin β-4 inhibits corneal epithelial cell apoptosis after ethanol exposure in vitro. Invest. Ophthalmol. Vis. Sci. 2004;45:1095–1100. doi: 10.1167/iovs.03-1002. [DOI] [PubMed] [Google Scholar]
- Sosne G, Qiu P, Ousler GW, 3rd, Dunn SP, Crockford D. Thymosin β4: a potential novel dry eye therapy. Ann. N. Y. Acad Sci. 2012;1270:45–50. doi: 10.1111/j.1749-6632.2012.06682.x. [DOI] [PubMed] [Google Scholar]
- Sotozono C, Inatomi T, Nakamura M, Kinoshita S. Keratinocyte growth factor accelerates corneal epithelial wound healing in vivo. Invest. Ophthalmol. Vis. Sci. 1995;36:1524–1529. [PubMed] [Google Scholar]
- Sotozono C, Inatomi T, Nakamura T, Koizumi N, Yokoi N, Ueta M, Matsuyama K, Kaneda H, Fukushima M, Kinoshita S. Cultivated oral mucosal epithelial transplantation for persistent epithelial defect in severe ocular surface diseases with acute inflammatory activity. Acta Ophthalmol. 2014;92:e447–453. doi: 10.1111/aos.12397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotozono C, Kinoshita S, Kita M, Imanishi J. Paracrine role of keratinocyte growth factor in rabbit corneal epithelial cell growth. Exp. Eye Res. 1994;59:385–391. doi: 10.1006/exer.1994.1122. [DOI] [PubMed] [Google Scholar]
- Spix JK, Chay EY, Block ER, Klarlund JK. Hepatocyte growth factor induces epithelial cell motility through transactivation of the epidermal growth factor receptor. Exp. Cell Res. 2007;313:3319–3325. doi: 10.1016/j.yexcr.2007.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spurlin JW, III, Lwigale PY. Wounded embryonic corneas exhibit nonfibrotic regeneration and complete innervation. Invest. Ophthalmol. Vis. Sci. 2013;54:6334–6344. doi: 10.1167/iovs.13-12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriram S, Gibson DJ, Robinson P, Pi L, Tuli S, Lewin AS, Schultz G. Assessment of anti-scarring therapies in ex vivo organ cultured rabbit corneas. Exp. Eye Res. 2014;125:173–182. doi: 10.1016/j.exer.2014.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sta Iglesia DD, Stepp MA. Disruption of the basement membrane after corneal débridement. Invest. Ophthalmol. Vis. Sci. 2000;41:1045–1053. [PubMed] [Google Scholar]
- Stapleton WM, Chaurasia SS, Medeiros FW, Mohan RR, Sinha S, Wilson SE. Topical interleukin-1 receptor antagonist inhibits inflammatory cell infiltration into the cornea. Exp. Eye Res. 2008;86:753–757. doi: 10.1016/j.exer.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern ME, Waltz KM, Beurerman RW, Ghosn CR, Mantras CE, Nicolson M, Assouline M, Stern KL, Wheeler LA. Effect of platelet-derived growth factor on rabbit corneal wound healing. Wound Repair Regen. 1995;3:59–65. doi: 10.1046/j.1524-475X.1995.30111.x. [DOI] [PubMed] [Google Scholar]
- Stramer BM, Zieske JD, Jung JC, Austin JS, Fini ME. Molecular mechanisms controlling the fibrotic repair phenotype in cornea: implications for surgical outcomes. Invest. Ophthalmol. Vis. Sci. 2003;44:4237–4246. doi: 10.1167/iovs.02-1188. [DOI] [PubMed] [Google Scholar]
- Sugaya S, Sakimoto T, Shoji J, Sawa M. Regulation of soluble interleukin-6 (IL-6) receptor release from corneal epithelial cells and its role in the ocular surface. Jpn. J. Ophthalmol. 2011;55:277–282. doi: 10.1007/s10384-011-0002-x. [DOI] [PubMed] [Google Scholar]
- Sumioka T, Ikeda K, Okada Y, Yamanaka O, Kitano A, Saika S. Inhibitory effect of blocking TGF-β/Smad signal on injury-induced fibrosis of corneal endothelium. Mol. Vis. 2008;14:2272–2281. [PMC free article] [PubMed] [Google Scholar]
- Sumioka T, Kitano A, Flanders KC, Okada Y, Yamanaka O, Fujita N, Iwanishi H, Kao WW, Saika S. Impaired cornea wound healing in a tenascin C-deficient mouse model. Lab Invest. 2013;93:207–217. doi: 10.1038/labinvest.2012.157. [DOI] [PubMed] [Google Scholar]
- Sun TT, Lavker RM. Corneal epithelial stem cells: past, present, and future. J. Invest. Dermatol. Symp. Proc. 2004;9:202–207. doi: 10.1111/j.1087-0024.2004.09311.x. [DOI] [PubMed] [Google Scholar]
- SundarRaj N, Kinchington PR, Wessel H, Goldblatt B, Hassell J, Vergnes JP, Anderson SC. A Rho-associated protein kinase: differentially distributed in limbal and corneal epithelia. Invest. Ophthalmol. Vis. Sci. 1998;39:1266–1272. [PubMed] [Google Scholar]
- Suzuki K, Tanaka T, Enoki M, Nishida T. Coordinated reassembly of the basement membrane and junctional proteins during corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2000;41:2495–2500. [PubMed] [Google Scholar]
- Suzuki K, Saito J, Yanai R, Yamada N, Chikama T, Seki K, Nishida T. Cell-matrix and cell-cell interactions during corneal epithelial wound healing. Prog. Retin. Eye Res. 2003;22:113–133. doi: 10.1016/s1350-9462(02)00042-3. [DOI] [PubMed] [Google Scholar]
- Szerenyi KD, Wang X, Gabrielian K, McDonnell PJ. Keratocyte loss and repopulation of anterior corneal stroma after de-epithelialization. Arch. Ophthalmol. 1994;112:973–976. doi: 10.1001/archopht.1994.01090190121031. [DOI] [PubMed] [Google Scholar]
- Takamura Y, Matsumoto T, Tomomatsu T, Matsumura T, Takihara Y, Inatani M. Aldose reductase inhibitor counteracts the enhanced expression of matrix metalloproteinase-10 and improves corneal wound healing in galactose-fed rats. Mol. Vis. 2013;19:2477–2486. [PMC free article] [PubMed] [Google Scholar]
- Tandon A, Sharma A, Rodier JT, Klibanov AM, Rieger FG, Mohan RR. BMP7 gene transfer via gold nanoparticles into stroma inhibits corneal fibrosis in vivo. PLoS One. 2013;8:e66434. doi: 10.1371/journal.pone.0066434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng Y, Wong HK, Jhanji V, Chen JH, Young AL, Zhang M, Choy KW, Mehta JS, Pang CP, Yam GH. Signature microRNAs in human cornea limbal epithelium. Funct. Integr. Genomics. 2015;15:277–294. doi: 10.1007/s10142-014-0417-9. [DOI] [PubMed] [Google Scholar]
- Terai K, Call MK, Liu H, Saika S, Liu CY, Hayashi Y, Chikama T, Zhang J, Terai N, Kao CW, Kao WW. Crosstalk between TGF-β and MAPK signaling during corneal wound healing. Invest. Ophthalmol. Vis. Sci. 2011;52:8208–8215. doi: 10.1167/iovs.11-8017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teranishi S, Kimura K, Kawamoto K, Nishida T. Protection of human corneal epithelial cells from hypoxia-induced disruption of barrier function by keratinocyte growth factor. Invest. Ophthalmol. Vis. Sci. 2008;49:2432–2437. doi: 10.1167/iovs.07-1464. [DOI] [PubMed] [Google Scholar]
- Tervo K, van Setten GB, Beuerman RW, Virtanen I, Tarkkanen A, Tervo T. Expression of tenascin and cellular fibronectin in the rabbit cornea after anterior keratectomy. Immunohistochemical study of wound healing dynamics. Invest. Ophthalmol. Vis. Sci. 1991;32:2912–2918. [PubMed] [Google Scholar]
- Thalmann-Goetsch A, Engelmann K, Bednarz J. Comparative study on the effects of different growth factors on migration of bovine corneal endothelial cells during wound healing. Acta. Ophthalmol. Scand. 1997;75:490–495. doi: 10.1111/j.1600-0420.1997.tb00134.x. [DOI] [PubMed] [Google Scholar]
- Thill M, Schlagner K, Altenähr S, Ergün S, Faragher RG, Kilic N, Bednarz J, Vohwinkel G, Rogiers X, Hossfeld DK, Richard G, Gehling UM. A novel population of repair cells identified in the stroma of the human cornea. Stem Cells Dev. 2007;16:733–745. doi: 10.1089/scd.2006.0084. [DOI] [PubMed] [Google Scholar]
- Thomas PB, Liu YH, Zhuang FF, Selvam S, Song SW, Smith RE, Trousdale MD, Yiu SC. Identification of Notch-1 expression in the limbal basal epithelium. Mol. Vis. 2007;13:337–344. [PMC free article] [PubMed] [Google Scholar]
- Tolino MA, Block ER, Klarlund JK. Brief treatment with heparin-binding EGF-like growth factor, but not with EGF, is sufficient to accelerate epithelial wound healing. Biochim. Biophys. Acta. 2011;1810:875–878. doi: 10.1016/j.bbagen.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomás-Juan J, Murueta-Goyena Larrañaga A, Hanneken L. Corneal regeneration after photorefractive keratectomy: a review. J. Optom. 2015;8:149–169. doi: 10.1016/j.optom.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomomatsu T, Takamura Y, Kubo E, Akagi Y. Aldose reductase inhibitor counteracts the attenuated adhesion of human corneal epithelial cells induced by high glucose through modulation of MMP-10 expression. Diabetes Res. Clin. Pract. 2009;86:16–23. doi: 10.1016/j.diabres.2009.07.007. [DOI] [PubMed] [Google Scholar]
- Torricelli AA, Wilson SE. Cellular and extracellular matrix modulation of corneal stromal opacity. Exp. Eye Res. 2014;129:151–160. doi: 10.1016/j.exer.2014.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toriseva M, Kähäri VM. Proteinases in cutaneous wound healing. Cell Mol. Life Sci. 2009;66:203–224. doi: 10.1007/s00018-008-8388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trosan P, Svobodova E, Chudickova M, Krulova M, Zajicova A, Holan V. The key role of insulin-like growth factor I in limbal stem cell differentiation and the corneal wound-healing process. Stem Cells Dev. 2012;21:3341–3350. doi: 10.1089/scd.2012.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai RJ, Sun TT, Tseng SC. Comparison of limbal and conjunctival autograft transplantation in corneal surface reconstruction in rabbits. Ophthalmology. 1990;97:446–455. doi: 10.1016/s0161-6420(90)32575-7. [DOI] [PubMed] [Google Scholar]
- Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N. Engl. J. Med. 2000;343:86–93. doi: 10.1056/NEJM200007133430202. [DOI] [PubMed] [Google Scholar]
- Tseng SC. Regulation and clinical implications of corneal epithelial stem cells. Mol. Biol. Rep. 1996;23:47–58. doi: 10.1007/BF00357072. [DOI] [PubMed] [Google Scholar]
- Tseng SC, Chen SY, Shen YC, Chen WL, Hu FR. Critical appraisal of ex vivo expansion of human limbal epithelial stem cells. Curr. Mol. Med. 2010;10:841–850. doi: 10.2174/156652410793937796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuft SJ, Gartry DS, RaweI M, Meek KM. Photorefractive keratectomy: implications of corneal wound healing. Br. J. Ophthalmol. 1993;77:243–247. doi: 10.1136/bjo.77.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuominen IS, Tervo TM, Teppo AM, Valle TU, Grönhagen-Riska C, Vesaluoma MH. Human tear fluid PDGF-BB, TNF-α and TGF-β1 vs corneal haze and regeneration of corneal epithelium and subbasal nerve plexus after PRK. Exp. Eye Res. 2001;72:631–641. doi: 10.1006/exer.2001.0999. [DOI] [PubMed] [Google Scholar]
- Tuori A, Uusitalo H, Burgeson RE, Terttunen J, Virtanen I. The immunohistochemical composition of the human corneal basement membrane. Cornea. 1996;15:286–294. doi: 10.1097/00003226-199605000-00010. [DOI] [PubMed] [Google Scholar]
- van Gelderen BE, Van Der Lelij A, Peek R, Broersma L, Treffers WF, Ruijter JM, van Der Gaag R. Cytokines in aqueous humour and serum before and after corneal transplantation and during rejection. Ophthalmic Res. 2000;32:157–164. doi: 10.1159/000055607. [DOI] [PubMed] [Google Scholar]
- Vu TH, Werb Z. Matrix metalloproteinases: effectors of development and normal physiology. Genes Dev. 2000;14:2123–2133. doi: 10.1101/gad.815400. [DOI] [PubMed] [Google Scholar]
- Wachtlin J, Langenbeck K, Schründer S, Zhang EP, Hoffmann F. Immunohistology of corneal wound healing after photorefractive keratectomy and laser in situ keratomileusis. J. Refract Surg. 1999;15:451–458. doi: 10.3928/1081-597X-19990701-11. [DOI] [PubMed] [Google Scholar]
- Wang L, Deng SX, Lu L. Role of CTCF in EGF-induced migration of immortalized human corneal epithelial cells. Invest. Ophthalmol. Vis Sci. 2012a;53:946–951. doi: 10.1167/iovs.11-8747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Despanie J, Shi P, Edman-Woolcott MC, Lin YA, Cui H, Heur JM, Fini ME, Hamm-Alvarez SF, MacKay JA. Lacritin-mediated regeneration of the corneal epithelia by protein polymer nanoparticles. J. Mater. Chem. B. Mater. Biol Med. 2014;2:8131–8141. doi: 10.1039/C4TB00979G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Lin A, Lu L. Effect of EGF-induced HDAC6 activation on corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2010a;51:2943–2948. doi: 10.1167/iovs.09-4639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Sun A, Li L, Zhao G, Jia J, Wang K, Ge J, Zou Y. Up-regulation of BMP-2 antagonizes TGF-β1/ROCK-enhanced cardiac fibrotic signalling through activation of Smurf1/Smad6 complex. J. Cell Mol. Med. 2012b;16:2301–2310. doi: 10.1111/j.1582-4934.2012.01538.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Wu X, Shi T, Lu L. Epidermal growth factor (EGF)-induced corneal epithelial wound healing through nuclear factor κB subtype-regulated CCCTC binding factor (CTCF) activation. J. Biol. Chem. 2013;288:24363–24371. doi: 10.1074/jbc.M113.458141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Zhou X, Ma J, Tian H, Jiao Y, Zhang R, Huang Z, Xiao J, Zhao B, Qian H, Li X. Effects of keratinocyte growth factor-2 on corneal epithelial wound healing in a rabbit model of carbon dioxide laser injury. Biol. Pharm. Bull. 2010b;33:971–976. doi: 10.1248/bpb.33.971. [DOI] [PubMed] [Google Scholar]
- Watanabe M, Yano W, Kondo S, Hattori Y, Yamada N, Yanai R, Nishida T. Up-regulation of urokinase-type plasminogen activator in corneal epithelial cells induced by wounding. Invest. Ophthalmol. Vis. Sci. 2003;44:3332–3338. doi: 10.1167/iovs.02-1280. [DOI] [PubMed] [Google Scholar]
- Weinger I, Klepeis V, Trinkaus-Randall V. Tri-nucleotide receptors play a critical role in epithelial cell wound repair. Purinerg. Signal. 2005;1:281–292. doi: 10.1007/s11302-005-8132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West JD, Dorà NJ, Collinson JM. Evaluating alternative stem cell hypotheses for adult corneal epithelial maintenance. World J. Stem Cells. 2015;7:281–299. doi: 10.4252/wjsc.v7.i2.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West-Mays JA, Dwivedi DJ. The keratocyte: corneal stromal cell with variable repair phenotypes. Int. J. Biochem. Cell Biol. 2006;38:1625–1631. doi: 10.1016/j.biocel.2006.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whikehart DR, Parikh CH, Vaughn AV, Mishler K, Edelhauser HF. Evidence suggesting the existence of stem cells for the human corneal endothelium. Mol Vis. 2005;11:816–824. [PubMed] [Google Scholar]
- Williams KA, Klebe S. Gene therapy for corneal dystrophies and disease, where are we? Curr. Opin. Ophthalmol. 2012;23:276–279. doi: 10.1097/ICU.0b013e3283541eb6. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Chaurasia SS, Medeiros FW. Apoptosis in the initiation, modulation and termination of the corneal wound healing response. Exp. Eye Res. 2007;85:305–311. doi: 10.1016/j.exer.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SL, El Haj AJ, Yang Y. Control of scar tissue formation in the cornea: strategies in clinical and corneal tissue engineering. J. Funct. Biomater. 2012;3:642–687. doi: 10.3390/jfb3030642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SE, He YG, Weng J, Li Q, McDowall AW, Vital M, Chwang EL. Epithelial injury induces keratocyte apoptosis: hypothesized role for the interleukin-1 system in the modulation of corneal tissue organization and wound healing. Exp. Eye Res. 1996;62:325–327. doi: 10.1006/exer.1996.0038. [DOI] [PubMed] [Google Scholar]
- Wilson SE, He YG, Weng J, Zieske JD, Jester JV, Schultz GS. Effect of epidermal growth factor, hepatocyte growth factor, and keratinocyte growth factor, on proliferation, motility and differentiation of human corneal epithelial cells. Exp. Eye Res. 1994;59:665–678. doi: 10.1006/exer.1994.1152. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Li Q, Mohan RR, Tervo T, Vesaluoma M, Bennett GL, Schwall R, Tabor K, Kim J, Hargrave S, Cuevas KH. Lacrimal gland growth factors and receptors: lacrimal fibroblastic cells are a source of tear HGF. Adv. Exp. Med. Biol. 1998;438:625–628. doi: 10.1007/978-1-4615-5359-5_88. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Liu JJ, Mohan RR. Stromal-epithelial interactions in the cornea. Prog. Retin. Eye Res. 1999;18:293–309. doi: 10.1016/s1350-9462(98)00017-2. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Mohan RR, Mohan RR, Ambrosio R, Jr, Hong J, Lee J. The corneal wound healing response: cytokine mediated interaction of the epithelium, stroma, and inflammatory cells. Prog. Retin. Eye Res. 2001;20:625–637. doi: 10.1016/s1350-9462(01)00008-8. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Mohan RR, Netto M, Perez V, Possin D, Huang J, Kwon R, Alekseev A, Rodriguez-Perez JP. RANK, RANKL, OPG, and M-CSF expression in stromal cells during corneal wound healing. Invest. Ophthalmol. Vis. Sci. 2004;45:2201–2211. doi: 10.1167/iovs.03-1162. [DOI] [PubMed] [Google Scholar]
- Wilson SE, Walker JW, Chwang EL, He YG. Hepatocyte growth factor, keratinocyte growth factor, their receptors, fibroblast growth factor receptor-2, and the cells of the cornea. Invest. Ophthalmol. Vis. Sci. 1993;34:2544–2561. [PubMed] [Google Scholar]
- Winkler MA, Dib C, Ljubimov AV, Saghizadeh M. Targeting miR-146a to treat delayed wound healing in human diabetic organ-cultured corneas. PLoS One. 2014;9:e114692. doi: 10.1371/journal.pone.0114692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirostko B, Rafii M, Sullivan DA, Morelli J, Ding J. Novel therapy to treat corneal epithelial defects: a hypothesis with growth hormone. Ocul Surf. 2015 doi: 10.1016/j.jtos.2014.12.005. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worm J, Stenvang J, Petri A, Frederiksen KS, Obad S, Elmén J, Hedtjärn M, Straarup EM, Hansen JB, Kauppinen S. Silencing of microRNA-155 in mice during acute inflammatory response leads to derepression of C/EBP β and down-regulation of G-CSF. Nucleic Acids Res. 2009;37:5784–5792. doi: 10.1093/nar/gkp577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J, Du Y, Mann MM, Funderburgh JL, Wagner WR. Corneal stromal stem cells versus corneal fibroblasts in generating structurally appropriate corneal stromal tissue. Exp. Eye Res. 2014a;120:71–81. doi: 10.1016/j.exer.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Zhou Q, Duan H, Wang X, Xiao J, Duan H, Li N, Li C, Wan P, Liu Y, Song Y, Zhou C, Huang Z, Wang Z. Reconstruction of auto-tissue-engineered lamellar cornea by dynamic culture for transplantation: a rabbit model. PLoS One. 2014b;9:e93012. doi: 10.1371/journal.pone.0093012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S. MicroRNA expression in the eyes and their significance in relation to functions. Prog. Retin. Eye Res. 2009;28:87–116. doi: 10.1016/j.preteyeres.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Xu KP, Ding Y, Ling J, Dong Z, Yu FS. Wound-induced HB-EGF ectodomain shedding and EGFR activation in corneal epithelial cells. Invest. Ophthalmol. Vis. Sci. 2004a;45:813–820. doi: 10.1167/iovs.03-0851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu KP, Li Y, Ljubimov AV, Yu FS. High glucose suppresses epidermal growth factor receptor/phosphatidylinositol 3-kinase/Akt signaling pathway and attenuates corneal epithelial wound healing. Diabetes. 2009;58:1077–1085. doi: 10.2337/db08-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu KP, Riggs A, Ding Y, Yu FS. Role of ErbB2 in corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2004b;45:4277–4283. doi: 10.1167/iovs.04-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu B, Wang N, Wang X, Tong N, Shao N, Tao J, Li P, Niu X, Feng N, Zhang L, Hua L, Wang Z, Chen M. MiR-146a suppresses tumor growth and progression by targeting EGFR pathway and in a p-ERK-dependent manner in castration-resistant prostate cancer. Prostate. 2012b;72:1171–1178. doi: 10.1002/pros.22466. [DOI] [PubMed] [Google Scholar]
- Xu J, Wu W, Zhang L, Dorset-Martin W, Morris MW, Mitchell ME, Liechty KW. The role of microRNA-146a in the pathogenesis of the diabetic wound-healing impairment: correction with mesenchymal stem cell treatment. Diabetes. 2012a;61:2906–2912. doi: 10.2337/db12-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu K, Yu FS. Impaired epithelial wound healing and EGFR signaling pathways in the corneas of diabetic rats. Invest. Ophthalmol. Vis. Sci. 2011;52:3301–3308. doi: 10.1167/iovs.10-5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada N, Yanai R, Nakamura M, Inui M, Nishida T. Role of the C domain of IGFs in synergistic promotion, with a substance P-derived peptide, of rabbit corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2004;45:1125–1131. doi: 10.1167/iovs.03-0626. [DOI] [PubMed] [Google Scholar]
- Yamagami S, Hamrah P, Miyamoto K, Miyazaki D, Dekaris I, Dawson T, Lu B, Gerard C, Dana MR. CCR5 chemokine receptor mediates recruitment of MHC class II-positive Langerhans cells in the mouse corneal epithelium. Invest. Ophthalmol. Vis. Sci. 2005;46:1201–1207. doi: 10.1167/iovs.04-0658. [DOI] [PubMed] [Google Scholar]
- Yamanaka S. Induced pluripotent stem cells: past, present, and future. Cell Stem Cell. 2012;10:678–684. doi: 10.1016/j.stem.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Yan L, Jiang D, He J, Wong DSH, Lian Q. Limbal stem cells and corneal epithelial regeneration: current status and prospectives. J. Ocular Biol. 2014;2:10. [Google Scholar]
- Yanai R, Yamada N, Inui M, Nishida T. Correlation of proliferative and anti-apoptotic effects of HGF, insulin, IGF-1, IGF-2, and EGF in SV40-transformed human corneal epithelial cells. Exp. Eye Res. 2006;83:76–83. doi: 10.1016/j.exer.2005.10.033. [DOI] [PubMed] [Google Scholar]
- Yang X, Moldovan NI, Zhao Q. Reconstruction of damaged cornea by autologous transplantation of epidermal adult stem cells. Mol. Vis. 2008;14:1064–1070. [PMC free article] [PubMed] [Google Scholar]
- Yang H, Wang Z, Capó-Aponte JE, Zhang F, Pan Z, Reinach PS. Epidermal growth factor receptor transactivation by the cannabinoid receptor (CB1) and transient receptor potential vanilloid 1 (TRPV1) induces differential responses in corneal epithelial cells. Exp. Eye Res. 2010;91:462–471. doi: 10.1016/j.exer.2010.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Di G, Qi X, Qu M, Wang Y, Duan H, Danielson P, Xie L, Zhou Q. Substance P promotes diabetic corneal epithelial wound healing through molecular mechanisms mediated via the neurokinin-1 receptor. Diabetes. 2014a;63:4262–4274. doi: 10.2337/db14-0163. [DOI] [PubMed] [Google Scholar]
- Yang J, Li Y, Erol D, Wu WH, Tsai YT, Li XR, Davi RJ, Tsang SH. Generation of induced pluripotent stem cells from conjunctiva. Graefes Arch. Clin. Exp. Ophthalmol. 2014b;252:423–431. doi: 10.1007/s00417-014-2575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin J, Xu K, Zhang J, Kumar A, Yu FS. Wound-induced ATP release and EGF receptor activation in epithelial cells. J. Cell Sci. 2007;120:815–825. doi: 10.1242/jcs.03389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin J, Lu J, Yu FS. Role of small GTPase Rho in regulating corneal epithelial wound healing. Invest. Ophthalmol. Vis. Sci. 2008;49:900–909. doi: 10.1167/iovs.07-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin J, Yu FS. Rho kinases regulate corneal epithelial wound healing. Am. J. Physiol. Cell Physiol. 2008;295:C378–387. doi: 10.1152/ajpcell.90624.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JJ, Ismail S, Sherwin T. Limbal stem cells: central concepts of corneal epithelial homeostasis. World J. Stem Cells. 2014;6:391–403. doi: 10.4252/wjsc.v6.i4.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida S, Yasuda M, Miyashita H, Ogawa Y, Yoshida T, Matsuzaki Y, Tsubota K, Okano H, Shimmura S. Generation of stratified squamous epithelial progenitor cells from mouse induced pluripotent stem cells. PLoS One. 2011;6:e28856. doi: 10.1371/journal.pone.0028856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshioka R, Shiraishi A, Kobayashi T, Morita S, Hayashi Y, Higashiyama S, Ohashi Y. Corneal epithelial wound healing impaired in keratinocyte-specific HB-EGF-deficient mice in vivo and in vitro. Invest. Ophthalmol. Vis. Sci. 2010;51:5630–5639. doi: 10.1167/iovs.10-5158. [DOI] [PubMed] [Google Scholar]
- You L, Kruse FE, Völcker HE. Neurotrophic factors in the human cornea. Invest. Ophthalmol. Vis. Sci. 2000;41:692–702. [PubMed] [Google Scholar]
- Yu J, Peng H, Ruan Q, Fatima A, Getsios S, Lavker RM. MicroRNA-205 promotes keratinocyte migration via the lipid phosphatase SHIP2. FASEB J. 2010a;24:3950–3959. doi: 10.1096/fj.10-157404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu FS, Yin J, Xu K, Huang J. Growth factors and corneal epithelial wound healing. Brain Res. Bull. 2010b;81:229–235. doi: 10.1016/j.brainresbull.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu D, Chen M, Sun X, Ge J. Differentiation of mouse induced pluripotent stem cells into corneal epithelial-like cells. Cell Biol. Int. 2013;37:87–94. doi: 10.1002/cbin.10007. [DOI] [PubMed] [Google Scholar]
- Yuan J, Liu Y, Huang W, Zhou S, Ling S, Chen J. The experimental treatment of corneal graft rejection with the interleukin-1 receptor antagonist (IL-1ra) gene. PLoS One. 2013;8:e60714. doi: 10.1371/journal.pone.0060714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagon IS, Sassani JW, McLaughlin PJ. Opioid growth factor modulates corneal epithelial outgrowth in tissue culture. Am. J. Physiol. 1995;268:R942–R950. doi: 10.1152/ajpregu.1995.268.4.R942. [DOI] [PubMed] [Google Scholar]
- Zagon IS, Sassani JW, Kane ER, McLaughlin PJ. Homeostasis of ocular surface epithelium in the rat is regulated by opioid growth factor. Brain Res. 1997;759:92–102. doi: 10.1016/s0006-8993(97)00238-2. [DOI] [PubMed] [Google Scholar]
- Zagon IS, Sassani JW, McLaughlin PJ. Reepithelialization of the rat cornea is accelerated by blockade of opioid receptors. Brain Res. 1998a;798:254–60. doi: 10.1016/s0006-8993(98)00427-2. [DOI] [PubMed] [Google Scholar]
- Zagon IS, Sassani JW, McLaughlin PJ. Reepithelialization of the rabbit cornea is regulated by opioid growth factor. Brain Res. 1998b;803:61–68. doi: 10.1016/s0006-8993(98)00610-6. [DOI] [PubMed] [Google Scholar]
- Zagon IS, Sassani JW, McLaughlin PJ. Reepithelialization of the human cornea is regulated by endogenous opioids. Invest. Ophthalmol. Vis. Sci. 2000;41:73–81. [PubMed] [Google Scholar]
- Zagon IS, Klocek MS, Sassani JW, McLaughlin PJ. Dry eye reversal and corneal sensation restoration with topical naltrexone in diabetes mellitus. Arch. Ophthalmol. 2009;127:1468–1473. doi: 10.1001/archophthalmol.2009.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeppieri M, Salvetat ML, Beltrami AP, Cesselli D, Bergamin N, Russo R, Cavaliere F, Varano GP, Alcalde I, Merayo J, Brusini P, Beltrami CA, Parodi PC. Human adipose-derived stem cells for the treatment of chemically burned rat cornea: preliminary results. Curr. Eye Res. 2013;38:451–463. doi: 10.3109/02713683.2012.763100. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Akhtar RA. Epidermal growth factor stimulation of phosphatidylinositol 3-kinase during wound closure in rabbit corneal epithelial cells. Invest. Ophthalmol. Vis. Sci. 1997;38:1139–1148. [PubMed] [Google Scholar]
- Zhang Y, Schmack I, Dawson DG, Grossniklaus HE, Conrad AH, Kariya Y, Suzuki K, Edelhauser HF, Conrad GW. Keratan sulfate and chondroitin/dermatan sulfate in maximally recovered hypocellular stromal interface scars of postmortem human LASIK corneas. Invest. Ophthalmol. Vis. Sci. 2006;47:2390–2396. doi: 10.1167/iovs.05-1559. [DOI] [PubMed] [Google Scholar]
- Zhang F, Yang H, Pan Z, Wang Z, Wolosin JM, Gjorstrup P, Reinach PS. Dependence of resolvin-induced increases in corneal epithelial cell migration on EGF receptor transactivation. Invest. Ophthalmol. Vis. Sci. 2010;51:5601–5609. doi: 10.1167/iovs.09-4468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao B, Ma A, Martin FL, Fullwood NJ. An investigation into corneal alkali burns using an organ culture model. Cornea. 2009;28:541–546. doi: 10.1097/ICO.0b013e3181901e08. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Chen P, Di G, Zhang Y, Wang Y, Qi X, Duan H, Xie L. Ciliary neurotrophic factor promotes the activation of corneal epithelial stem/progenitor cells and accelerates corneal epithelial wound healing. Stem Cells. 2015;33:1566–1576. doi: 10.1002/stem.1942. [DOI] [PubMed] [Google Scholar]
- Zhou M, Li XM, Lavker RM. Transcriptional profiling of enriched populations of stem cells versus transient amplifying cells. A comparison of limbal and corneal epithelial basal cells. J. Biol. Chem. 2006;281:19600–19609. doi: 10.1074/jbc.M600777200. [DOI] [PubMed] [Google Scholar]
- Zhou EH, Watson C, Pizzo R, Cohen J, Dang Q, Ferreira de Barros PM, Park CY, Chen C, Brain JD, Butler JP, Ruberti JW, Fredberg JJ, Demokritou P. Assessing the impact of engineered nanoparticles on wound healing using a novel in vitro bioassay. Nanomedicine (Lond) 2014;9:2803–2815. doi: 10.2217/nnm.14.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou SY, Xie ZL, Xiao O, Yang XR, Heng BC, Sato Y. Inhibition of mouse alkali burn induced-corneal neovascularization by recombinant adenovirus encoding human vasohibin-1. Mol. Vis. 2010;16:1389–1398. [PMC free article] [PubMed] [Google Scholar]
- Zhu YT, Li F, Han B, Tighe S, Zhang S, Chen SY, Liu X, Tseng SC. Activation of RhoA-ROCK-BMP signaling reprograms adult human corneal endothelial cells. J. Cell Biol. 2014;206:799–811. doi: 10.1083/jcb.201404032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zieske JD. Extracellular matrix and wound healing. Curr Opin Ophthalmol. 2001;12:237–41. doi: 10.1097/00055735-200108000-00001. [DOI] [PubMed] [Google Scholar]
- Zieske JD, Guimarães SR, Hutcheon AE. Kinetics of keratocyte proliferation in response to epithelial debridement. Exp. Eye Res. 2001;72:33–39. doi: 10.1006/exer.2000.0926. [DOI] [PubMed] [Google Scholar]
- Zieske JD, Mason VS, Wasson ME, Meunier SF, Nolte CJ, Fukai N, Olse BR, Parenteau NL. Basement membrane assembly and differentiation of cultured corneal cells: importance of culture environment and endothelial cell interaction. Exp. Cell Res. 1994;214:621–633. doi: 10.1006/excr.1994.1300. [DOI] [PubMed] [Google Scholar]
- Zieske JD, Takahashi H, Hutcheon AE, Dalbone AC. Activation of epidermal growth factor receptor during corneal epithelial migration. Invest. Ophthalmol. Vis. Sci. 2000;41:1346–1355. [PubMed] [Google Scholar]