Abstract
Background
Although many people who inject drugs (PID) contend with comorbidities, including high rates of mental illness, limited attention has been given to the differences in comorbidities among men and women or the potential links between psychiatric disorders and HIV risk behaviours. We sought to longitudinally examine associations between depression and HIV-related sexual risk behaviours among PID, stratified by gender.
Methods
Data were derived from a prospective cohort of PID in Vancouver, Canada between December 2005 and November 2009. Using generalised estimating equations, we examined the relationship between depressive symptoms and two types of sexual HIV risk behaviours: engaging in unprotected sex; and having multiple sexual partners. All analyses were stratified by self-reported gender.
Results
Overall, 1017 PID participated in this study, including 331 (32.5%) women. At baseline, women reported significantly higher depressive symptoms than men (P < 0.001). In multivariate generalised estimating equations analyses, after adjustment for potential social, demographic and behavioural confounders, more severe depressive symptomology remained independently associated with engaging in unprotected sex [adjusted odds ratio (AOR) = 1.62, 95% confidence interval (CI): 1.18 – 2.23] and having multiple sexual partners (AOR = 1.54, 95% CI: 1.09 – 2.19) among women, but was only marginally associated with having multiple sexual partners among men (AOR = 1.18, 95% CI: 0.98 – 1.41).
Conclusions
These findings call for improved integration of psychiatric screening and treatment services within existing public health initiatives designed for PID, particularly for women. Efforts are also needed to address sexual risk-taking among female PID contending with clinically significant depression.
Keywords: HIV risk behaviours, injection drug use, prospective cohort study
INTRODUCTION
Over the past two decades, the comorbid presentation of psychiatric disorders and drug addiction has been well documented.1–6 Specifically, several systematic reviews and meta-analyses have suggested that some psychiatric disorders, including depression, anxiety disorders and antisocial personality behaviours, are more prevalent among people who use drugs than in general populations.7–10 For example, Goldner et al. reported that the incidence of depressive and anxiety symptoms were disproportionately high among populations who abused illicit drugs.7 Additionally, Perdue et al. found that 46.9% of male people who inject drugs (PID) in Seattle were diagnosed as having depressive symptoms.3 Given the increased risk of HIV transmission within this population, there is a need to consider the role that such psychiatric disorders may play in shaping HIV risk behaviours among PID.11–13
The effect of depression on sexual HIV risk behaviours among PID has received increasing attention, yet the results have been equivocal. Although some studies have shown that depression was associated with engaging in unprotected sexual intercourse, negative feelings regarding condom use, having sexual intercourse with three or more partners in the past 6 months, and having a greater number of lifetime sexual partners, a meta-analysis found little evidence to suggest that depressive symptoms predicted sexual risk behaviours.1–3,14–16 Further, most research to date has examined these associations using cross-sectional analyses,17 which may explain the discrepancies in the results and point to the need for longitudinal investigations of such relationships.
Few studies have investigated whether potential relationships between depression and sexual HIV risk behaviours differ between men and women, despite a body of research indicating important gender-based differences in vulnerability to depression and risks associated with sexual behaviours. Past research has suggested that among people who use drugs, women are far more likely to experience depression than men.18–20 Also, gender roles and relationship dynamics are known to predispose women to risky sexual behaviour.19 Therefore, this study sought to longitudinally investigate the relationship between depression and sexual HIV risk behaviours among male and female PID.
METHODS
Data for this study were derived from the Vancouver Injection Drug Users Study (VPIDS), which was initiated in May 1996. The VPIDS is an ongoing prospective cohort study that has previously been described in detail.21 Briefly, participants are eligible for inclusion in the study if they are 18 years or older, live in the Greater Vancouver region, have injected illicit drugs at least once in the past month, test seronegative for HIV infection, and provide written informed consent. At baseline and semiannually, participants provide blood samples for laboratory analysis and complete an interviewer-administered questionnaire. The questionnaire elicits a range of information, including demographic data, drug-use patterns, HIV risk behaviours, and access to drug treatment. Participants receive an honorarium of C$20 for each study visit. Ethical approval for VPIDS is obtained on an annual basis from the Providence Health Care/University of British Columbia Research Ethics Board. In the present study, data were abstracted and analysed from those who participated in baseline or follow-up visits between December 2005 and November 2009. The sample was further restricted to those who were sexually active at baseline.
Statistical analyses
We examined as our primary outcomes two types of sexual HIV risk behaviours occurring in the 6 months before participants’ interviews: (1) having sex with multiple partners; and (2) inconsistent condom use during vaginal or anal intercourse. To determine the number of sexual partners, participants were asked to report the number of different male and female partners with whom they had engaged in sexual activity within the previous 6 months, excluding those with whom they had engaged in sex for money, shelter, clothes, food, drugs, or favours. These outcome measures have successfully been used in a previous study.22 Inconsistent condom use was determined by asking participants how often a condom was used during vaginal and anal intercourse. Possible responses were: always, usually, sometimes, occasionally, and never. As in a previous study, this variable was dichotomised into ‘consistent’ (i.e. always) and ‘inconsistent’ (i.e. usually, sometimes, occasionally, or never) condom use.22 Those who reported engaging in vaginal and anal intercourse and reported discordant condom use were classified as inconsistent condom users.
Our primary explanatory variable of interest was severe depressive symptoms, which was ascertained by the Centre for Epidemiological Studies Depression Scale (CES-D) at each follow up. The CES-D scale is a 20-item survey measuring depressive symptoms and has been shown to be valid and reliable when administered to young people, homeless populations, and drug users.23–26 Consistent with past studies, scores of 22 or above were considered indicative of severe depressive symptoms and a probable diagnosis of depression.1,19,27 Building on previous studies that examined the relationship between depression and sexual HIV risk behaviours among PID, we also considered secondary explanatory variables of interest that might confound the relationship between depressive symptoms and sexual HIV risk behaviours.1–3 These included: age (per year older); identifying as lesbian, gay, bisexual or transgender (LGBT) (yes vs. no); ethnicity (Caucasian vs. others); living in unstable housing (yes vs. no); relationship status (legally married, common law or regular partner vs. others); non-injection crack use (≥ daily vs. < daily); non-injection crystal methamphetamine use (≥ daily vs. < daily); injection heroin use (≥ daily vs. < daily); injection cocaine use (≥ daily vs. < daily); injection crystal methamphetamine use (≥ daily vs. < daily); binge drug use, defined as a period of using injection or noninjection drugs more often than usual (yes vs. no); involvement in sex work (yes vs. no); and having been physically attacked or assaulted (yes vs. no). All behavioural variables referred to the 6-month period before the interview, and variable definitions are consistent with previous investigations.21–28
First, we compared CES-D scores at baseline between men and women using the Mann–Whitney test. We then examined bivariate and multivariate associations between the two outcomes and all explanatory variables, stratified by gender. Considering serial measures were available for each subject, we used generalised estimating equations (GEE) with a logit link function. GEE analyses allowed for consideration of factors associated with the two sexual risk behaviours over the full length of the study period, with standard errors calculated using an exchangeable correlation structure, adjusted by multiple observations for each individual. Since each individual could report having sex with multiple partners or inconsistent condom use during vaginal or anal intercourse during separate study visits, GEE analyses identified factors correlated with periods of HIV sexual risk behaviours both within and between individuals. GEE models are classified as a type of marginal longitudinal analysis and have been used to analyse datasets containing repeatedmeasures, such as longitudinal cohorts.29 To account for potential confounding with the primary variable of interest, multivariate GEE confounding models were fitted for each outcome using an a priori–defined modelling strategy proposed by Maldonado and Greenland.30 First, we fitted the full model containing the primary and secondary variables with P < 0.05 in the bivariate GEE analyses. Then, we constructed a series of reduced models by removing one secondary variable from the full model at a time. After comparing the coefficient associated with the primary variable of interest in the full model to the coefficient in each reduced model, we dropped the secondary variable associated with the smallest relative change. We repeated this iterative process until the smallest change exceeded 5%. All statistical analyses were performed using SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA). All P-values were two-sided.
RESULTS
In total, 1017 PID participated in this study, of whom 331 (32.5%) were women. In total, 331 women contributed 1410 observations, and 686 male participants contributed 3039 observations. The median age of women at baseline was 38 years [interquartile range (IQR): 30–45], whereas it was 43 years (IQR: 36–49) among men. The median CES-D score for the entire sample was 21 (IQR: 12–30). Overall, 197 (59.5%) women and 293 (42.7%) men had CES-D scores ≥ 22 at baseline. The difference in CES-D scores between women (median: 25, IQR: 15–33) and men (median: 19, IQR: 11–27; P < 0.001) was statistically significant.
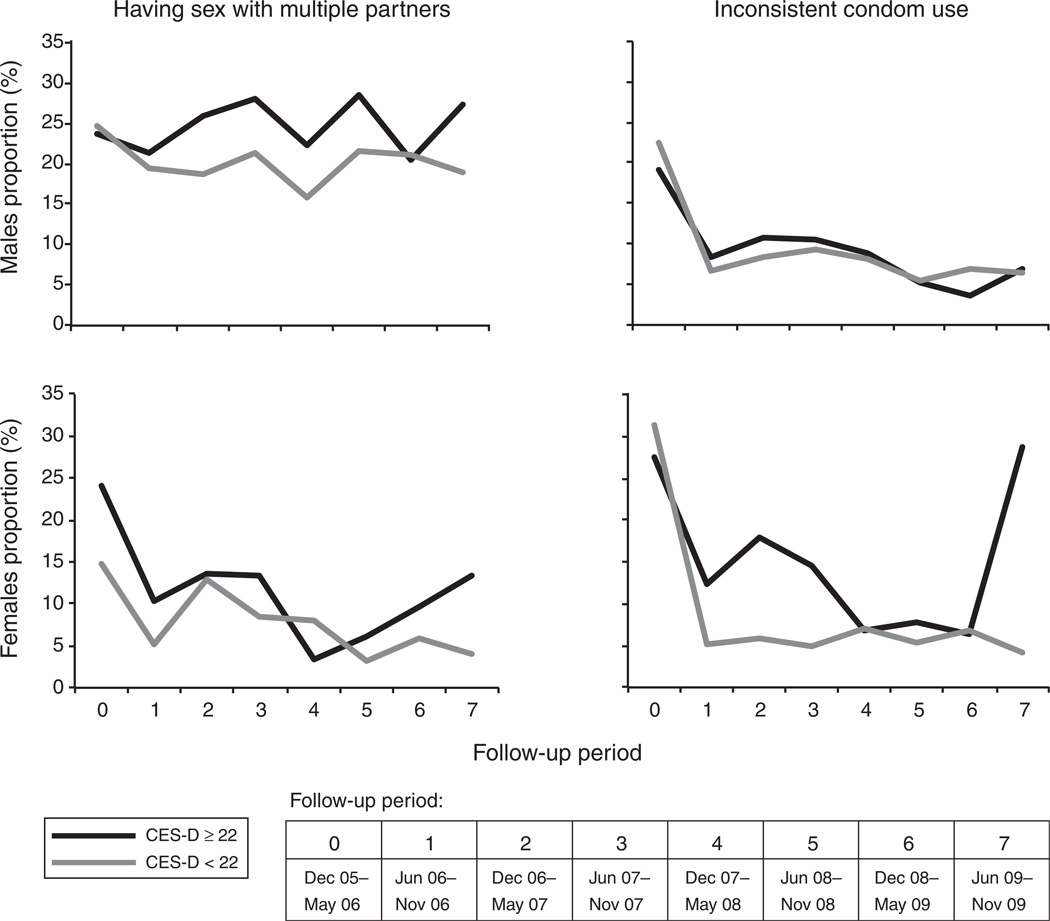
Comparisons of baseline demographic, social and behavioural characteristics between men and women are presented in Table 1. Women were more likely to identify as LGBT, report being in a stable relationship, report daily non-injection crack use, report sex work involvement, and have CES-D scores ≥ 22, whereas men were more likely to be older, Caucasian, and report living in unstable housing (all P < 0.05). The proportions of participants reporting sexual HIV risk behaviours by CES-D scores over the study period are shown in Fig. 1.
Table 1.
Baseline characteristics stratified by gender (n = 1017)
| Characteristic | Male 686 (67.5%) | Female 331 (32.5%) |
P-value |
|---|---|---|---|
| Median age (IQR) | 43 (36–49) | 38 (30–45) | <0.001 |
| LGBT | 28 (4) | 60 (18) | <0.001 |
| Caucasian | 481 (70) | 171 (52) | <0.001 |
| Unstable housing | 484 (71) | 199 (60) | <0.001 |
| In a stable relationshipA | 179 (26) | 147 (44) | <0.001 |
| ≥ Daily non-injection crack useB | 247 (36) | 175 (53) | <0.001 |
| ≥ Daily non-injection CM useB,C | 4 (1) | 3 (1) | 0.560 |
| ≥ Daily heroin injectionB,C | 199 (29) | 111 (34) | 0.142 |
| ≥ Daily cocaine injectionB,C | 57 (8) | 29 (9) | 0.808 |
| ≥ Daily CM injectionB | 21 (3) | 5 (2) | 0.142 |
| ≥ Daily binge drug useB | 227 (33) | 117 (35) | 0.476 |
| Sex work involvementB | 14 (2) | 134 (40) | <0.001 |
| Experience of violenceB | 165 (24) | 78 (24) | 0.864 |
| CES-D scores ≥ 22 | 293 (43) | 197 (60) | <0.001 |
Pearson χ2 test was used.
IQR, interquartile range; LGBT, lesbian/gay/bisexual/transgender; CM, crystal methamphetamine; CES-D, Centre for Epidemiological Studies Depression Scale
Legally married/common law/regular partner.
Refers to the 6-month period before the interview.
Fig. 1.
Proportion of people who inject drugs reporting sexual risk behaviours at follow-up, stratified by male and female with Centre for Epidemiological Studies Depression Scale (CES-D) ≥22 versus CES-D <22 (n = 1017).
The demographic, social and behavioural characteristics associated with having multiple sexual partners in the bivariate and multivariate analyses are shown in Table 2. Among women having CES-D scores ≥ 22 remained independently associated with having multiple sexual partners after adjustment for potential social, demographic and behavioural confounders [adjusted odds ratio (AOR) = 1.54, 95% confidence interval (CI): 1.09 – 2.19]. In addition, age (AOR = 0.95, 95% CI: 0.92 – 0.97), identifying as LGBT (AOR = 2.56, 95% CI: 1.49 – 4.40), at least daily injection cocaine use (AOR = 0.33, 95% CI: 0.14 – 0.77), sex trade involvement (AOR = 2.58, 95% CI: 1.72 – 3.86), and experiencing violence (AOR = 2.19, 95% CI: 1.55 – 3.10) were independently associated with having multiple sexual partners. Among males, having CES-D scores ≥ 22 was marginally associated with having multiple sexual partners (AOR=1.18, 95% CI: 0.98 – 1.41). In addition, being in a stable relationship (AOR = 0.47, 95% CI: 0.35 – 0.62), at least daily non-injection crack use (AOR = 1.42, 95% CI: 1.16 – 1.72), at least daily non- injection crystal methamphetamine use (AOR = 2.75, 95% CI: 1.32 – 5.74), and sex trade involvement (AOR=2.68, 95% CI: 1.15 – 6.24) were independently associated with having multiple sexual partners.
Table 2.
Generalised estimating equations analyses of factors associated with having sex with multiple partners among people who use drugs in Vancouver, Canada (n = 1017)
| Male (n = 686) | Female (n = 331) | |||
|---|---|---|---|---|
| Characteristic | Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
| Age (per year older) | 0.99 (0.97 – 1.01) | – | 0.93 (0.91 – 0.96) | 0.95 (0.92 – 0.97) |
| LGBT (yes vs. no) | 2.22 (1.19 – 4.16) | – | 30.01 (1.78 – 5.10) | 2.56 (1.49 – 4.40) |
| Ethnicity (Caucasian vs. others) | 0.79 (0.58 – 1.07) | – | 10.02 (0.65 – 1.61) | – |
| Unstable housing (yes vs. no) | 1.22 (0.99 – 1.51) | – | 10.15 (0.78 – 1.70) | – |
| In a stable relationship (legally married/common law/regular partner vs. others) | 0.47 (0.35 – 0.61) | 0.47 (0.35 – 0.62) | 00.67 (0.47 – 0.98) | – |
| Non-injection crack useA (≥ daily vs. < daily) | 1.43 (1.18 – 1.73) | 1.42 (1.16 – 1.72) | 10.84 (1.25 – 2.71) | – |
| Non-injection CM useA(≥ daily vs. < daily) | 2.40 (1.23 – 4.67) | 2.75 (1.32 – 5.74) | 70.79 (1.17 – 51.91) | – |
| Injection heroin useA (≥ daily vs. < daily) | 1.00 (0.81 – 1.25) | – | 01.94 (1.30 – 2.91) | – |
| Injection cocaine useA (≥ daily vs. < daily) | 1.17 (0.84 – 1.62) | – | 0.44 (0.20 – 0.97) | 0.33 (0.14 – 0.77) |
| Injection CM useA (≥ daily vs. < daily) | 1.44 (0.86 – 2.40) | – | 2.20 (0.56 – 8.56) | – |
| Binge drug useA (yes vs. no) | 1.26 (1.07 – 1.49) | – | 0.82 (0.57 – 1.18) | – |
| Sex trade involvementA(yes vs. no) | 2.77 (1.19 – 6.44) | 2.68 (1.15 – 6.24) | 2.91 (1.94 – 4.36) | 2.58 (1.72 – |
| Experience of violenceA(yes vs. no) | 1.13 (0.93 – 1.36) | – | 2.34 (1.70 – 3.23) | 2.19 (1.55 – 3.10) |
| CES-D scores (≥22 vs. < 22) | 1.29 (1.08 – 1.55) | 1.18 (0.98 – 1.41) | 1.92 (1.39 – 2.65) | 1.54 (1.09 – 2.19) |
CES-D, Centre for Epidemiological Studies Depression Scale; CI, confidence interval; CM, crystal methamphetamine; LGBT, lesbian/gay/bisexual/transgender; OR, odds ratio; –, not applicable
Refers to the 6-month period before the interview.
Demographic, social and behavioural characteristics associated with inconsistent condom use in bivariate and multivariate analyses are shown in Table 3. As shown in multivariate analyses, having CES-D scores ≥ 22 remained independently associated with inconsistent condom use among females (AOR = 1.62, 95% CI: 1.18–2.23). In addition, age (AOR=0.95, 95% CI: 0.93–0.97), unstable housing (AOR=0.58, 95% CI: 0.41–0.83), and experiencing violence (AOR = 1.76, 95% CI: 1.17–2.66) were independently associated with inconsistent condom use. Among men, having CES-D scores ≥ 22 was not significantly associated with the outcome in the bivariate analysis (OR = 1.13, 95% CI: 0.86–1.50), and therefore we did not fit a multivariate GEE model for this outcome in men.
TABLE 3.
Generalised estimating equations analyses of factors associated with inconsistent condom use among people who use in Vancouver, Canada (n = 1017)
| Male (n = 686) | Female (n = 331) | |||
|---|---|---|---|---|
| Characteristic | Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
| Age (per year older) | 0.96 (0.94 – 0.98) | – | 0.95 (0.93 – 0.97) | 0.95 (0.93 – 0.97) |
| LGBT (yes vs. no) | 1.47 (0.69 – 3.15) | – | 1.69 (1.01 – 2.85) | – |
| Ethnicity (Caucasian vs. others) | 0.66 (0.49 – 0.90) | – | 1.15 (0.78 – 1.70) | – |
| Unstable housing (yes vs. no) | 0.89 (0.69 – 1.16) | – | 0.70 (0.50 – 0.97) | 0.58 (0.41 – 0.83) |
| In a stable relationship (legally married/common law/regular partner vs. others) | 1.98 (1.49 – 2.63) | – | 1.52 (1.08 – 2.13) | – |
| Non-injection crack useA (≥ daily vs. < daily) | 1.12 (0.85 – 1.47) | – | 0.95 (0.66 – 1.36) | – |
| Non-injection CM useA(≥ daily vs. < daily) | 2.27 (0.91 – 5.66) | – | 1.80 (0.13 – 24.58) | – |
| Injection heroin useA (≥ daily vs. < daily) | 1.39 (1.04 – 1.85) | – | 2.11 (1.48 – 3.00) | – |
| Injection cocaine useA (≥ daily vs. < daily) | 0.99 (0.63 – 1.56) | – | 1.06 (0.61 – 1.82) | – |
| Injection CM useA (≥ daily vs. < daily) | 2.76 (1.52 – 5.00) | – | 0.49 (0.10 – 2.28) | – |
| Binge drug useA (yes vs. no) | 0.98 (0.77 – 1.25) | – | 1.00 (0.73 – 1.36) | – |
| Sex trade involvementA (yes vs. no) | 3.62 (1.85 – 7.12) | – | 1.70 (1.18 – 2.45) | 1.45 (0.99 – 2.13) |
| Experience of violenceA (yes vs. no) | 0.96 (0.71 – 1.30) | – | 1.87 (1.24 – 2.82) | 1.76 (1.17 – 2.66) |
| CES-D scores (≥ 22 vs. < 22) | 1.13 (0.86 – 1.50) | – | 1.82 (1.33 – 2.50) | 1.62 (1.18 – 2.23) |
CES-D, Centre for Epidemiological Studies Depression Scale; CI, confidence interval; CM, crystal methamphetamine; LGBT, lesbian/gay/bisexual/transgender; OR, odds ratio; –, not applicable
Refers to the 6-month period before the interview.
DISCUSSION
In the present analysis, we observed high rates of depressive symptoms amongst PID in Vancouver, Canada, with more female PID reporting high CES-D scores than male. We also found that female PID presenting with high depressive symptoms were more likely to engage in unprotected sex and have multiple sexual partners, whereas male PID presenting with high depressive symptoms were more likely to report having multiple sexual partners, although this relationship did not meet conventional statistical significance.
Our results corroborate past studies that suggest depressive symptoms are higher among PID compared with the general population.17,31 The CES-D scores in our cohort were high, with a median of 21 at baseline, whereas CES-D scores among general population samples average around 8.31 Moreover, 293 (43%) men and 197 (60%) women had CES-D scores ≥ 22, which is indicative of significant depressive symptomology. However, CES-D scores among our cohort were comparable to CESPage 11 of 26 D scores reported in other studies investigating depression among PID in Baltimore and Seattle.3,31
Consistent with past studies, we found that women were more likely to report having severe depressive symptoms than men.20,32–33 Some previous gender-based investigations of depression and associated risk behaviours have focused on hormonal differences between men and women, and how such differences might impact psychological reactions to adverse events.34–35 However, other studies have argued that there is an interaction between gender and social factors.19,32,36 For example, one potential hypothesis suggests that in most societies, women traditionally have less social power, which increases their vulnerability to traumatic events such as violence and sexual abuse.36 Indeed, past work undertaken in Vancouver has documented adverse gender-based power relations among local drug users as well as the extreme violence that many women in this community face.37–38 Increased exposure to traumatising experiences can potentially alter females’ biological and psychological stress responses, which may subsequently compromise their problem solving and coping mechanisms when experiencing stressful situations.32,36
Although previous studies have suggested that depression is linked with HIV risk behaviours among PID, to our knowledge, this is the first prospective cohort study that has conducted a longitudinal gender-based analysis focused on the relationship between depression and sexual HIV risk behaviours.1–4 Multiple cross-sectional studies and one longitudinal study have found that depression is associated with a variety of sexual HIV risk behaviours.1–3 Other authors have argued that associations between depression and sexual risk behaviours may result from impaired cognitive functioning secondary to depression, which may lead to individuals engaging in potentially risky behaviours such as having a greater number of lifetime sex partners and reporting three or more sex partners in the past 6 months.1,3 One other possible interpretation is that depression is a multifaceted disorder influenced by several psychosocial risk factors and structural exposures, including incarceration.3
Our findings highlight the need for integrated screening, counselling, and treatment options to address psychiatric disorders within existing HIV-prevention programs designed for PID. Currently, these interventions are not included in the World Health Organisation or other United Nations agencies’ recommended HIV-prevention interventions for PID.39 Our findings also indicate the need for intervention strategies to be multifaceted and gender-specific. Given that female PID are more likely to experience traumatic events (e.g. sexual abuse) and depression, there is a critical need for social support and mental health treatment interventions tailored to female victims of abuse and violence.32,40 Moreover, female adolescents exhibiting depressive symptomology may be more likely to use illicit substances and engage in risky sexual behaviours, thus there may be a need to develop gender-specific mental health programs targeting at-risk youth, particularly females.1,19 Given the known barriers to healthcare among PID, efforts should be made to offer such programs in lowthreshold initiatives, including drop-in centres where nurses and healthcare practitioners can make referrals to other primary care services.41–42
The present study has several limitations. First, as our study sample was not randomly recruited, our findings may not be generalisable to PID in other settings. Second, we relied on self-reported data, thus our findings may be subject to response biases. However, several other studies have demonstrated self-reporting amongst PID is generally valid and reliable.43–44 We were also unable to infer causality from the findings due to the observational nature of our study. Finally, we ascertained depressive symptoms through the use of the CES-D scores. As such, we were unable to identify participants who were clinically diagnosed with depression.
In summary, we found that higher depressive symptom scores were independently associated with sexual HIV risk behaviours among women and were marginally associated with having multiple sexual partners among men. These results point to a need for improved integration of psychiatric testing, screening, and counselling services within existing public health initiatives for PID. These results also underscore the importance of gender differences and support the need for gender-specific HIV prevention interventions. Ultimately, gender-specific prevention and treatment strategies should be an integral component among initiatives addressing HIV transmission amongst PID.
SUMMARY.
Although many people who inject drugs (PID) contend with comorbidities, including high rates of mental illness, limited attention has been given to the differences in comorbidities among men and women or the potential links between psychiatric disorders and HIV risk behaviours. We sought to longitudinally examine associations between depression and HIV-related sexual risk behaviours among PID, stratified by gender. In multivariate analyses, after adjustment for potential social, demographic and behavioural confounders, more severe depressive symptomology remained independently associated with engaging in unprotected sex and having multiple sexual partners among women, but was only marginally associated with having multiple sexual partners among men. These findings call for improved integration of psychiatric screening and treatment services within existing public health initiatives designed for PID, particularly for women.
Acknowledgements
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. The study was supported by the US National Institutes of Health (R01DA011591). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports Dr Evan Wood. Kanna Hayashi is supported by the Canadian Institutes of Health Research.
Footnotes
Conflicts of interest
None declared.
REFERENCES
- 1.Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish PH, Iritani B. Adolescent depression and suicide risk: association with sex and drug behavior. Am J Prev Med. 2004;27:224–231. doi: 10.1016/j.amepre.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Hutton HE, Lyketsos CG, Zenilman JM, Thompson RE, Erbelding EJ. Depression and HIV risk behaviors among patients in a sexually transmitted disease clinic. Am J Psychol. 2004;161:912–914. doi: 10.1176/appi.ajp.161.5.912. [DOI] [PubMed] [Google Scholar]
- 3.Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among Seattle-area injection drug users and young men who have sex with men. AIDS Educ Prev. 2003;15:81–92. doi: 10.1521/aeap.15.1.81.23842. [DOI] [PubMed] [Google Scholar]
- 4.Rohde P, Noell J, Ochs L, Seeley J. Depression, suicidal ideation and STD-related risk in homeless older adolescents. J Adolesc. 2001;24:447–460. doi: 10.1006/jado.2001.0382. [DOI] [PubMed] [Google Scholar]
- 5.Brady K, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. Am J Psychol. 2005;162:1483. doi: 10.1176/appi.ajp.162.8.1483. [DOI] [PubMed] [Google Scholar]
- 6.Brooner R, King V, Kidorf M, Schmidt C, Bigelow G. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- 7.Goldner E, Lusted A, Roerecke M, Rehm J, Fischer B. Prevalence of Axis-1 psychiatric (with focus on depression and anxiety) disorder and symptomatology among non-medical prescription opioid users in substance use treatment: systematic review and meta-analyses. Addict Behav. 2014;39:520–531. doi: 10.1016/j.addbeh.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 8.Hawkins E. A tale of two systems: co-occurring mental health and substance abuse disorders treatment for adolescents. Annu Rev Psychol. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- 9.Malta M, Strathdee S, Magnanini M, Bastos F. Adherence to antiretroviral therapy for human immunodeficiency virus/acquired immune deficiency syndrome among drug users: a systematic review. Addiction. 2008;103:1242–1257. doi: 10.1111/j.1360-0443.2008.02269.x. [DOI] [PubMed] [Google Scholar]
- 10.Rogers D. The harmful effects of recreation ecstasy: a systematic review of observational evidence. Health Technol Assess. 2009;13:xxi-338. doi: 10.3310/hta13050. [DOI] [PubMed] [Google Scholar]
- 11.Craib K, Spittal P, Wood E, Laliberte N, Hogg R, Li K, Heath K, Tyndall M, O’Shaughnessy M, Schecter M. Risk factors for elevated HIV incidence among aboriginal injection drug users in Vancouver. CMAJ. 2003;168:19–24. [PMC free article] [PubMed] [Google Scholar]
- 12.Joint United Nations Programme on HIV/AIDS. United Nations. [[verified 15 November 2014]];2006 Available online at: http://data.unaids.org/pub/epireport/2006/2006_epiupdate_en.pdf. [Google Scholar]
- 13.Karon J, Fleming P, Steketee R, De Cock K. HIV in the United States at the turn of the century: an epidemic in transition. Am J Public Health. 2001;91:1060–1068. doi: 10.2105/ajph.91.7.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychol. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- 15.Kalichman S, Weinhardt L. Negative affect and sexual risk behavior: comment on Crepaz and Marks. Health Psychol. 2001;20:300–301. [PubMed] [Google Scholar]
- 16.Valverde E, Purcell D, Waldrop-Valverde D, Malow R, Knowlton A, Gomez C, Farrell N. Correlates of depression among HIV-positive women and men who inject drugs. J Acquir Immune Defic Syndr. 2007;46(Suppl 2):S96–S100. doi: 10.1097/QAI.0b013e318157683b. [DOI] [PubMed] [Google Scholar]
- 17.Williams C, Latkin C. The role of depressive symptoms in predicting sex with multiple and high-risk partners. J Acquir Immune Defic Syndr. 2005;38:69–73. doi: 10.1097/00126334-200501010-00013. [DOI] [PubMed] [Google Scholar]
- 18.Sordo L, Chahua M, Bravo M, Barrio G, Brugal M, Domingo-Salvany A, Molist G, Fuente L. Depression among regular heroin users: the influence of gender. Addict Behav. 2012;37:148–152. doi: 10.1016/j.addbeh.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Hallfors D, Waller M, Bauer D, Ford C, Halpern C. Which comes first in adolescence – sex and drugs or depression? Am J Prev Med. 2005;29:163–170. doi: 10.1016/j.amepre.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Abulseoud O, Karpyak V, Schneekloth T, Hall-Flavin D, Loukianova L, Geske J, Biernacka J, Mrazek D, Frye M. A retrospective study of gender differences in depressive symptoms and risk of relapse in patients with alcohol dependence. Am J Addiction. 2013;22:437–442. doi: 10.1111/j.1521-0391.2013.12021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wood E, Tyndall M, Spittal P, Li K, Kerr T, Hogg R, Montaner J, O’Shaugnessy M, Schechter M. Unsafe injection practices in a cohort of injection drug users in Vancouver: could safer injecting rooms help? CMAJ. 2001;165:405–410. [PMC free article] [PubMed] [Google Scholar]
- 22.Marshall B, Kerr T, Shoveller J, Montaner J, Wood E. Structural factors associated with an increased risk of HIV and sexually transmitted infection transmission among street-involved youth. BMC Public Health. 2009;9:7. doi: 10.1186/1471-2458-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fitzpatrick K, Irwin J, Lagory M, Ritchey F. Just thinking about it: social capital and suicide ideation among homeless persons. J Health Psychol. 2007;12:750–760. doi: 10.1177/1359105307080604. [DOI] [PubMed] [Google Scholar]
- 24.Radloff L. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 25.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 26.Weissman M, Sholomskas D, Pottenger M, Prusoff B, Locke B. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 27.Hadland S, Marshall B, Kerr T, Qi J, Montaner J, Wood E. Depressive symptoms and patterns of drug use among street youth. J Adolesc Health. 2011;48:585–590. doi: 10.1016/j.jadohealth.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marshall B, Kerr T, Shoveller J, Patterson T, Buxton J, Wood E. Homelessness and unstable housing associated with an increased risk of HIV and STI transmission among street-involved youth. Health Place. 2009;15:783–790. doi: 10.1016/j.healthplace.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wood E, Kerr T, Lloyd-Smith E, Buchner C, Marsh DC, Montaner J, Tyndall MW. Methodology for evaluating Insite: Canada’s first medically supervised safer injection facility for injection drug users. Harm Reduct J. 2004;1:1–9. doi: 10.1186/1477-7517-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- 31.Hasin D, Glick H. Depressive symptoms and DSM-III-R alcohol dependence: general population results. Addiction. 1993;88:1431–1436. doi: 10.1111/j.1360-0443.1993.tb02030.x. [DOI] [PubMed] [Google Scholar]
- 32.Parker G, Brotchie H. Gender differences in depression. Int Rev Psychiatry. 2010;22:429–436. doi: 10.3109/09540261.2010.492391. [DOI] [PubMed] [Google Scholar]
- 33.Sagud M, Hotujac L, Mihaljević-Peles A, Jakovljević M. Gender differences in depression. Coll Antropol. 2002;26:149–157. [PubMed] [Google Scholar]
- 34.Costello E, Pine D, Hammen C, March J, Plotsky P, Weissman M, Biederman J, Goldsmith H, Kaufman J, Lewinsohn P, Hellander M, Hoagwood K, Koretz D, Nelson C, Leckman J. Development and natural history of mood disorders. Biol Psychiatry. 2002;52:529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- 35.Graber J, Seeley J, Brooks-Gunn J, Lewinsohn P. Is pubertal timing associated with psychopathology in young adulthood? J Am Acad Child Adolesc Psychiatry. 2004;43:718–726. doi: 10.1097/01.chi.0000120022.14101.11. [DOI] [PubMed] [Google Scholar]
- 36.Nolen-Hoeksema S. Gender differences in depression. Curr Dir Psychol Sci. 2001;10:173–176. [Google Scholar]
- 37.Shannon K, Kerr T, Allinott S, Chettiar J, Shoveller J, Tyndall M. Social and structural violence and power relations in mitigating HIV risk of drug-using women in survival sex work. Soc Sci Med. 2008;66:911–921. doi: 10.1016/j.socscimed.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Fairbairn N, Small W, Shannon K, Wood E, Kerr T. Seeking refuge from violence in street-based drug scenes: women’s experience in North America’a first supervised injection facility. Soc Sci Med. 2008;67:817–823. doi: 10.1016/j.socscimed.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organisation, United Nations Office on Drugs and Crime, Joint United Nations Programme on HIV/AIDS. Geneva: WHO; 2012. WHO, UNODC, UNAIDS technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users. http://apps.who.int/iris/bitstream/10665/77969/1/9789241504379_eng.pdf. [Google Scholar]
- 40.Braitstein P, Li K, Tyndall M, Spittal P, O’Shaugnessy M, Schilder A, Johnston C, Hogg R, Schechter M. Sexual violence among a cohort of injection drug users. Soc Sci Med. 2003;57:561–569. doi: 10.1016/s0277-9536(02)00403-3. [DOI] [PubMed] [Google Scholar]
- 41.Edlin B, Kresina T, Raymond D, Carden M, Gourevitch M, Rich J, Cheever L, Cargill V. Overcoming barriers to prevention, care, and treatment of hepatitis C in illicit drug users. Clin Infect Dis. 2005;40:S276–S285. doi: 10.1086/427441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kerr T, Wood E, Grafstein E, Ishida T, Shannon K, Lai C, Montaner J, Tyndall M. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health. 2005;27:62–66. doi: 10.1093/pubmed/fdh189. [DOI] [PubMed] [Google Scholar]
- 43.Goldstein M, Friedman S, Neaigus A, Jose B, Ildefonso G, Curtis R. Self-reports of HIV risk behavior by injecting drug users: Are they reliable? Addiction. 1995;90:1097–1104. doi: 10.1046/j.1360-0443.1995.90810978.x. [DOI] [PubMed] [Google Scholar]
- 44.Petry N. Reliability of drug users’ self-reported HIV risk behaviors using a brief, 11-item scale. Subst Use Misuse. 2001;36:1731–1747. doi: 10.1081/ja-100107576. [DOI] [PubMed] [Google Scholar]