Abstract
The aim of the current study was to examine the reliability and validity of a trait-based assessment of borderline personality disorder (BPD) using the NEO Five-Factor Inventory. Correlations between the Five-Factor Inventory-BPD composite (FFI-BPD) and explicit measures of BPD were examined across six samples, including undergraduate, community, and clinical samples. The median correlation was .60, which was nearly identical to the correlation between measures of BPD and a BPD composite generated from the full Revised NEO Personality Inventory (i.e., NEO-BPD; r =.61). Correlations between FFI-BPD and relevant measures of psychiatric symptomatology and etiology (e.g., childhood abuse, drug use, depression, and personality disorders) were also examined and compared to those generated using explicit measures of BPD and NEO-BPD. As expected, the FFI-BPD composite correlated most strongly with measures associated with high levels of Neuroticism, such as depression, anxiety, and emotion dysregulation, and the pattern of correlations generated using the FFI-BPD was highly similar to those generated using explicit measures of BPD and NEO-BPD. Finally, genetic analyses estimated that FFI-BPD is 44% heritable, which is comparable to meta-analytic research examining genetics associated with BPD, and revealed that 71% of the genetic influences are shared between FFI-BPD and a self-report measure assessing BPD (Personality Assessment Inventory – Borderline subscale; Morey, 1991). Generally, these results support the use of FFI-BPD as a reasonable proxy for BPD, which has considerable implications, particularly for potential gene-finding efforts in large, epidemiological datasets that include the NEO FFI.
Keywords: Borderline Personality Disorder, Genetics, five-factor model
Borderline personality disorder (BPD) is a personality disorder (PD) characterized by emotion dysregulation, impulsivity, interpersonal dysfunction, and identity disturbance. BPD is associated with considerable psychological distress (Ansell, Sanislow, McGlashan, & Grilo, 2007), functional impairment(Hill et al., 2008), risk of suicide (Pompili, Girardi, Ruberto, & Tatarelli, 2005), and treatment costs (Bender et al., 2001). Therefore, understanding etiological mechanisms involved in the development of BPD is of critical importance.
Trait based conceptualizations, assessments, and diagnosis of PDs like BPD have garnered growing support in the field due to evidence supporting the relative reliability, validity, and clinical utility of these approaches when compared to the existing categorical model (Clark, 2007; Widiger & Trull, 2007; Morey et al., 2012; Morey, Skodol, & Oldham, 2014; Widiger & Presnall, 2013) Given the substantial evidence supporting these dimensional trait models of PDs, a new diagnostic system for PDs was included in Section III (“emerging measures and model”) of the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) that is grounded, in large part, on a trait-based approach. Despite claims to the contrary (e.g., Gunderson, 2013), BPD is remarkably well-captured by both general and pathological trait approaches (e.g., Miller, Few, Lynam, & MacKillop, 2014; Trull, Widiger, Lynam, & Costa, 2003). Noteworthy, however, is that the Section III PD model is a hybrid categorical-dimensional model, meaning that the dimensional traits (Criterion B) can be used, along with assessment of impairment in personality functioning (Criterion A), to generate traditional, categorical diagnoses for 6 of the 10 PDs found in the main body of text, including BPD.
To date, the majority of the work examining dimensional models of PDs has been conducted from a Five-Factor Model (FFM) framework using measures such as the NEO Personality Inventory-Revised (NEO PI-R; Costa, & McCrae, 1992), which assesses five broad personality trait domains (e.g., Neuroticism) and 30 more specific facets (e.g., angry hostility). Using this model, researchers have developed FFM-based approaches to the assessment of PDs such as the prototype-matching and count techniques (see Miller, 2012, for a review). The prototype matching approach utilizes expert ratings of the prototypical individual with a given PD on the 30 facets of the FFM, which can then be compared with an individual’s score on a measure such as the NEO PI-R. The FFM BPD prototype has been shown to correlate strongly with explicit DSM-based measures of BPD as well as relevant external correlates, such as childhood sexual abuse (Trull et al., 2003). FFM PD count scores were developed (Miller, Bagby, Pilkonis, Reynolds, & Lynam, 2005) as an easier alternative to the prototype matching technique as they involve only the simple summation of scores across the most salient expert-rated facets. The FFM BPD count is generated using scores on nine facets rated as prototypical of BPD by experts, from the dimensions of Neuroticism, Openness, Agreeableness (reverse scored) and Conscientiousness (reverse scored) and demonstrates strong correlations with the prototype score and DSM based BPD measures. Miller, Morse, Nolf, Stepp, and Pilkonis (2012) demonstrated that BPD scores derived from the FFM BPD count and DSM-IV LEAD ratings were substantially related (r = .60; despite one being based on self-report data and the other using expert ratings of BPD symptoms) and manifested similar pattern of relations with key constructs from BPD’s nomological network (rICC = .84).
One of the pragmatic benefits of these trait approaches to PDs is that it may allow for considerably more research devoted to the epidemiology of PDs, in that many large datasets include general personality assessments but not explicit assessments of PDs. For instance, research focusing on genetic influences on BPD is limited due to a lack of adequate phenotype assessment in epidemiological datasets. The work that has been done estimates that 40% of the variance in BPD is due to genetic factors (Amad, Ramoz, Thomas, Jardri, & Gorwood, 2014); it is noteworthy that these genetic influences are shared with FFM traits (Distel et al., 2009; Few et al., 2014). Due to the heterogeneous nature of the BPD construct, Distel and colleagues (2010) also examined the covariance structure of four features of BPD (i.e., identity problems, affective instability, negative relationships, and self-harm). Heritability estimates ranged between 26% (self-harm) and 35% (negative relationships). Most importantly, however, they found that a common pathway model provided the best fit to the data, and concluded that “the four main features of BPD thus co-occur as a result of genetic and environmental factors that influence the four components in similar ways, through a latent predictor variable (the BPD construct)” (p.8). Despite the evidence in support of genetic influences on etiology, there has been minimal success in identifying specific genetic variants associated with BPD (Calati, Gressier, Balestri, & Serretti, 2013). Meta-analysis of 28 candidate gene studies reported null results in terms of the direct association between polymorphisms and BPD (Calati et al.). Furthermore, only one genome-wide association study (GWAS) of BPD has been conducted (Lubke et al., 2014), which identified seven single-nucleotide polymorphisms (SNPs) tagging the SERINC5 gene associated with a dimensional measure of borderline personality features. Importantly, however, these SNPs did not reach genome-wide significance (i.e., p<.5×10−8). The relative dearth of gene-finding studies is due again, in part, to the limited assessment of this phenotype in large epidemiological samples with rich genetic data.
In order to enhance gene-finding efforts directed at liability to BPD, significantly larger sample sizes will be needed. Based on strong genetic correlations between BPD and personality traits from twin studies, the use of trait based PD prototypes or count scores may significantly facilitate this progress, as numerous genetically informed studies routinely collect general personality, but not BPD data. However, a majority of such studies typically assess only domain level traits of the FFM with measures such as the NEO Five-Factor Inventory (NEO FFI; Costa & McCrae, 1992), making it impossible to generate the traditional BPD prototype or count scores based on the NEO PI-R. Therefore, the goal of the current study was to evaluate the utility of a NEO FFI composite representative of BPD liability (i.e., FFI-BPD), generated via summation of items assessing facets identified in meta-analytic research (Samuel & Widiger, 2008) and via academician (Lynam & Widiger, 2001) and clinician (Samuel & Widiger, 2004) ratings of prototypical BPD. We use the term “BPD liability” because the measure is not designed to explicitly assess diagnostic BPD symptoms, but rather variation in general personality traits that have been shown to associate with increased liability to BPD symptomatology. This endeavor is comparable to previous work using the self-report Multidimensional Personality Questionnaire-Brief Form (Patrick, Curtin, & Tellegen, 2002) to index BPD traits (Bornovalova, Hicks, Patrick, Iacono, & McGue, 2011), with the goal of being able to examine genetic influences and the longitudinal course of BPD in existing epidemiological datasets. The researchers developed a 19-item measure (Minnesota Borderline Personality Disorder Scale; MBPD) that demonstrated strong correlations with self-report measures of BPD and moderate correlations with categorical BPD diagnoses. The MBPD also correlated as expected with variables relevant to BPD, including substance abuse, childhood and adult trauma, and internalizing psychopathology.
Similar to this approach, the goal of the current study was to develop an FFI-BPD measure to index BPD liability using several datasets with a variety of types of samples (e.g., undergraduate, outpatient clinical, epidemiological twin sample) and with both BPD and NEO FFI data. Like the MBPD study, the goal was not to develop another self-report measure of BPD, but rather, to develop a measure that enables the study of BPD liability in existing epidemiological datasets, particularly for genetic analyses. After creating the FFI-BPD, we first examined correlations between BPD and FFI-BPD and also compared these correlations to a BPD composite created using the full NEO PI-R (i.e., NEO-BPD). We then conducted a series of hierarchical regression analyses to test the extent to which FFI-BPD and NEO-BPD account for the same variance in explicit measures of BPD. Across five samples (i.e., undergraduate, community, clinical), convergent and discriminant validity were also examined by computing correlations between FFI-BPD and etiological risk factors (i.e., childhood abuse), measures of psychiatric symptomatology (i.e., emotion dysregulation, depression, anxiety, illicit drug use), and PDs and comparing them to those generated using explicit measures of BPD and NEO-BPD. BPD has previously demonstrated moderate correlations with childhood sexual abuse (Fossati, Madeddu, & Maffei, 1999; Bornovalova et al., 2013), and is associated with internalizing symptoms (i.e., anxiety, depression), emotion dysregulation, and substance use across a variety of samples (Eaton et al., 2011; Scott, Stepp, & Pilkonis, 2014). BPD is also highly comorbid with a number of other DSM-based PDs (e.g., Antisocial; Zimmerman, Rothschild, & Chelminski, 2005). In general, BPD tends to be more strongly associated with Cluster A and Cluster B PDs, but it is also highly comorbid with PDs from Clusters C (Tomko, Trull, Wood, & Sher, 2014). We expected similar results when examining correlations between these variables and FFI-BPD. Because we were primarily interested in the similarity of the patterns of correlations generated rather than the effect sizes, the correlational profiles generated by the three BPD measures across these external criteria were compared using both Pearson and intraclass correlations. We also computed correlations between FFI-BPD and the 30 FFM facets (with overlapping items from the NEO PI-R removed) and compared the profile of correlations to those generated using explicit measures of BPD. Finally, using classical twin modeling approaches, we examined the heritability of FFI-BPD and its genetic overlap with an explicit measure of BPD. Essentially, if there is substantial genetic overlap between these phenotypes, then the FFI-BPD composite could be used to index BPD liability, which would be useful in secondary data analyses with large, genetically informative epidemiological datasets.
Method
Participants
Sample 1
Participants were 358 undergraduate students (54% female; Mean age = 19.35; SD = 2.0) recruited from a research participant pool at a large Southeastern university who received research credit in exchange for participation. The majority of participants were Caucasian (82%); of the remaining participants, 10% were Asian and 6% were Black (see Maples, Guan, Carter, & Miller, 2014 for details).
Sample 2
The initial sample included 361 undergraduate students recruited from a research participant pool at a large Southeastern university who received research credit in exchange for participation, but 11 were excluded due to missing NEO PI-R data. The final sample included 350 participants (63% female; Mean age=19.11; SD=1.69). The majority of participants were Caucasian (89%); of the remaining participants, 4% were Black, 4% were Asian, and 3% chose “Other” for their racial/ethnic status (see Miller et al., 2010, for details).
Sample 3
The initial sample consisted of 3,348 twins from the Australian Twin Registry interviewed between 2005 and 2009 in a study primarily focusing on cannabis use. A subsample of these twins subsequently completed self-report questionnaires, and the final sample included 3,127 twins (66% female; Mean age=31.84; SD=2.48) with complete data for relevant study variables: (a) 948 monozygotic female twins (MZF: 382 pairs, 184 unpaired); (b) 444 monozygotic male twins (MZM: 153 pairs, 138 unpaired); (c) 716 dizygotic female twins (DZF: 288 pairs, 140 unpaired) (d) 330 dizygotic male twin (DZM: 95 pairs, 140 unpaired) and (e) 689 dizygotic opposite sex twins (DZOS: 198 pairs, 293 unpaired; see Lynskey et al., 2012, for details).
Sample 4
The initial sample comprised 1,630 individuals recruited from the St. Louis area in a study designed to examine the prevalence and impact of personality pathology in later life. Nineteen participants were excluded due to missing data, and the final sample included 1,611 participants (55% females; Mean age=59.54; SD=2.74). With regard to race and ethnic background, 65% were Caucasian, 32% were African-American, and 3% were from other groups (e.g., Asian, American, Indian; see Oltmanns, Rodrigues, Weinstein, & Gleason, 2014, for details).
Sample 5
The sample initially included 110 individuals currently receiving outpatient psychological or psychiatric treatment in a study designed to assess the reliability and validity of the DSM-5 Section III diagnostic model for PDs. Three participants were excluded due to missing NEO PI-R data, and the final sample included 107 participants (71% female; Mean age = 35.9; SD = 12.7). The majority of participants were White (91%); of the remaining participants, 6% were Black, and 3% were Asian (see Few et al., 2013, for details).
Sample 6
The initial sample consisted of 152 psychiatric outpatients meeting DSM-IV diagnostic criteria for BPD (N=93), major depressive disorder/dysthymic disorder without BPD (MDD-DYS; 34%) or another psychiatric diagnosis (N=7) in a study designed to examine affect and alcohol use among individuals with BPD. One participant was excluded due to missing NEO PI-R data. The sample included 151 participants (Mean age = 32.08; SD = 11.51), 85% were female and self-reported ethnicity was as follows: 83% Caucasian, 6% Black, 4% Asian, and 7% as Other (see Jahng et al., 2011, for details). An additional three participants did not have complete PD data, and therefore, only 148 participants were included in the analyses examining relations between the BPD measures/composites and PDs.
Measures
General Personality Measures
NEO Five-Factor Inventory (NEO FFI)
The NEO FFI (Costa, & McCrae, 1992) is a 60-item, self-report measure of the FFM personality domains used in Sample 3. Items are scored on a 1 (Strongly Disagree) to 5 (Strongly Agree) scale.
Revised NEO Personality Inventory (NEO PI-R)
The NEO PI-R (Costa, & McCrae, 1992) is a 240-item self-report measure of the FFM domains as well as the six lower-order facets subsumed by each domain. Eight items are used to assess each facet and are scored on a 0-4 scale (i.e., range: 0-32).
Personality Disorder Measures
Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II)
The SCID-II (First, Gibbon, Spitzer, Williams, & Benjamin, 1997) is a semi-structured interview used in Sample 5 that assesses the 10 DSM–IV PDs. Each PD criterion is scored using a 0 (i.e., absent), 1 (i.e., subclinical), or 2 (i.e., present) rating. Dimensional scores were utilized in the current study, which were generated via summation of ratings across criteria (e.g., Nine BPD criteria = 0-18 range). The alpha coefficient for BPD was .82, and for the remaining nine PDs, ranged from .68 (Obsessive-Compulsive PD) to .84 (Avoidant and Antisocial PDs).
Structured Clinical Interview for DSM-IV Axis II Personality Disorders – Personality Questionnaire (SCID-II P/Q)
The SCID-II P/Q (First et al., 1997) is a 119-item self-report questionnaire used in Samples 1 and 2 designed to assess the diagnostic criteria for the 10 DSM-IV PDs. The measure uses a forced-choice No/Yes response format. Only the BPD subscale was used in the current study and was scored by adding up “Yes” responses across 15 items (i.e., range: 0-15). Alpha coefficients were .74 and .73 for Samples 1 and 2, respectively.
Structured Interview for DSM-IV Personality (SIDP-IV)
The SIDP-IV (Pfohl, Bluhm, & Zimmerman, 1997) is a semi-structured interview used in Samples 4 and 6 that assesses criteria for the 10 DSM-IV PDs. It is organized by topic sections rather than disorders and assesses typical behavior within the past 5 years. Criteria are rated as follows: 0=absent; 1=subthreshold; 2=present; 3=strongly present. Dimensional scores were utilized in the current study, which were generated via summation of ratings across criteria for each PD (e.g., Nine BPD criteria = 0-27 range). In Sample 4, the alpha coefficient for BPD was .67, and for the remaining nine PDs, ranged from .52 (Schizotypal PD) to .82 (Avoidant PD). All PD variables in Sample 4, with the exception of Obsessive-Compulsive PD, were log-transformed prior to analyses to correct for non-normality. In Sample 6, the alpha coefficient for BPD was .83, and for the remaining nine PDs, ranged from .47 (Schizoid) to .84 (Avoidant). Only Antisocial and Narcissistic PDs were log-transformed due to skewness.
Personality Assessment Inventory– Borderline subscale (PAI-BOR)
The PAI-BOR (Morey, 1991) is a 24-item, self-report measure used in Samples 3 and 6 that generates a total score and scores on four subscales. Only the total scores (range= 0-72) were used in current analyses. Alpha coefficients were .88 and .87 for Samples 3 and 6, respectively.
Personality Diagnostic Questionnaire-4+ (PDQ-4+)
The PDQ-4+ (Hyler, 1994) is a 99-item self-report measure of DSM-IV PDs. Only the nine-item BPD subscale was used in the current study. The measure uses a True/False response format, and dimensional scores were created by summing the True responses across the nine items (i.e., range: 0-9; α=.55).
McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD)
The MSI-BPD (Zanarini et al., 2003) is a 10-item self-report measure of DSM-IV BPD used in Sample 2. Each item is rated as a “0” (absent) or “1” (present), and a dimensional score was created by summation across items (i.e., range: 0-10; α=.81).
Etiological Measures
Child Abuse and Trauma Scale (CATS)
The CATS (Sanders & Giolas, 1991) is a 38-item self-report measure of physical, verbal, emotional, and sexual abuse that was used in Sample 2. In the current study, a total score was utilized and generated using the 14 items identified in the Poythress, Skeem, and Lilienfeld analyses (2006). The alpha coefficient for the total score was .90. The variable was log-transformed prior to analyses to correct for non-normality.
Measures of Psychiatric Symptomatology
Brief Symptom Inventory (BSI)
The BSI (Derogatis & Melisaratos, 1983) is a 53-item self-report measure of psychological symptoms experienced during the past week that was used in Samples 2 and 5. The BSI includes specific symptom scales and a global severity scale. Only the anxiety and depression subscales (6 items each) were used in the current study. In Sample 2, alpha coefficients for the anxiety and depression subscales were .75 and .90, respectively. In Sample 5, alpha coefficients for the anxiety and depression subscales were .86 and .88,
Difficulties in Emotion Regulation Scale (DERS)
The DERS (Gratz & Roemer, 2004) is a 36-item self-report measure of problems with emotion regulation that was used in Sample 2. Only the total score was used in the current study (α=.92).
Computerized Diagnostic Interview Schedule (C-DIS-IV) screener
The C-DIS-IV screener (Robins & Helzer, 1994) was used in Sample 4 and is an assessment that was developed for non-clinicians to collect information that can generate DSM-IV diagnoses. In the current study, a dichotomous variable was used to identify individuals who reported a lifetime history of a major depressive disorder (0=no; 1=yes).
MINI-International Neuropsychiatric Interview (M.I.N.I.)
The M.I.N.I (Sheehan et al., 1998) is a brief structured interview that was used in Sample 4 to diagnose DSM-IV Axis I alcohol and drug use disorders. In the current study, dichotomous lifetime alcohol and drug dependence variables were utilized.
Illicit Substance Use
In Samples 2 and 5, participants were asked to report ever use of a variety of illicit substances (e.g., marijuana, crack/cocaine) in their lifetime. In Sample 2, five substances were assessed (Mean = 1.5; SD=1.07), and in Sample 5, eight substances were assessed (Mean=2.28; SD=2.21).
Data Analysis and Results
Scale development
In order to identify items to include in the FFI-BPD composite, clinician and academician ratings of prototypical BPD on the 30 FFM facets were examined, in addition to correlations between the FFM facets and BPD generated in meta-analytic research (Samuel & Widiger, 2008). The academician and clinician ratings used a 1 to 5 scale, and facets prototypically high (i.e., greater than or equal to 3.5) or prototypically low (i.e., less than or equal to 2.5), along with facets correlating with BPD at [.20] or greater, were considered. Only facets meeting these criteria from 2 out of 3 sources were selected. This yielded 16 facets (only 14 of which are assessed with at least one item in the NEO FFI) composed of 34 items on the NEO FFI: Neuroticism: anxiety (3 items), angry hostility (1 item), depression (4 items), impulsiveness (0 items), vulnerability (2 items); Extraversion: excitement seeking (1 item); Openness: feelings (1 item), actions (2 items); Agreeableness: trust (2 items), straightforwardness (1 item), altruism (5 items), compliance (3 items); Conscientiousness: order (3 items), dutifulness (3 items), self-discipline (3 items), deliberation (0 items). All items and facets considered low in relation to BPD were reverse scored prior to generating the composite (i.e., items assessing Agreeableness and Conscientiousness facets).
Given the unequal distribution of items across the facets, a maximum of two items per facet was retained in the final FFI-BPD composite. To do this, corrected inter-item correlations were generated, and items demonstrating the lowest correlations most consistently across the six datasets were removed from the composite (e.g., 3 of 5 items from the altruism facet were removed). The final FFI-BPD composite comprised 24 items assessing 14 of the 16 facets associated with BPD. Alpha coefficients (presented in Table 2) across the six samples ranged from .67 to .82 with a median of .78. The NEO-BPD composite was also generated in five of the six samples utilizing the NEO PI-R (Sample 3 does not include NEO PI-R data) and was computed via summation of the 16 facet scores, with Agreeableness and Conscientiousness facets reverse scored. Alpha coefficients, also presented in Table 2, ranged from .74 to .83 with a median of .79.
Table 2.
Means, standard deviations, and reliability coefficients for BPD measures
| BPD | FFI-BPD | NEO-BPD | |
|---|---|---|---|
|
| |||
| Sample 1: | |||
| SCID-II P/Q | 3.09 (2.68) α=.74 |
1.76 (0.44) α=.78 |
235.78 (42.85) α=.79 |
|
| |||
| Sample 2: | |||
| PDQ-4+ | 2.51 (1.70) α=.55 |
1.83 (0.43) α=.73 |
244.51 (38.70) α=.76 |
| MSI-BPD | 2.57 (2.60) α=.81 |
||
| SCID-II P/Q | 3.96 (2.92) α=.73 |
||
|
| |||
| Sample 3: | |||
| PAI-BOR | 17.39 (9.93) α=.88 |
1.52 (0.43) α=.81 |
- |
|
| |||
| Sample 4: | |||
| SIDP-IV | 1.13 (1.87) α=.67 |
1.35 (0.37) α=.78 |
194.26 (35.48) α=.81 |
|
| |||
| Sample 5: | |||
| SCID-II | 4.79 (4.23) α=.82 |
1.91 (0.51) α=.82 |
249.23 (48.26) α=.83 |
|
| |||
| Sample 6: | |||
| SIDP-IV PAI-BOR |
11.05 (5.56) α=.83 |
2.29 (0.39) α=.67 |
286.18 (38.22) α=.74 |
| 43.33 (11.55) α=.87 |
|||
Note: All descriptive statistics were generated prior to log transformations; SCID-II P/Q – Structured Clinical Interview for DSM-IV Axis II Personality Disorders – Personality Questionnaire; PDQ-4+ = Personality Diagnostic Questionnaire-4+; MSI-BPD = McLean Screening Instrument for Borderline Personality Disorder; SIDP-IV = Structured Interview for DSM-IV Personality; SCID-II = Structured Clinical Interview for DSM-IV Axis II Personality Disorders; PAI-BOR = Personality Assessment Inventory – Borderline subscale;
Phenotypic analyses and results
All phenotypic analyses were conducted in SPSS. Due to the number of analyses conducted and varying sample sizes, we focus on effect size as opposed to significance when reporting results. Based on Cohen (1988), we interpret correlations between .10 and .29 as “small,” .30-.49 as “medium,” and .50 and greater as “large.” Means, standard deviations and reliability coefficients for BPD measures in each sample are presented in Table 2. Correlations between BPD and the FFI-BPD composite within each sample are presented in Table 3. Medium to large effect sizes emerged, and correlations ranged from .35 (SIDP-IV in Sample 6) to .72 (PAI-BOR in Sample 3), with a median correlation of .60. Correlations between the NEO-BPD composite and BPD were nearly identical, ranging from .43 (SIDP-IV in Sample 4) to .67 (PAI-BOR in Sample 6) with a median correlation of .61.
Table 3.
Correlations between BPD and Five-Factor Model-BPD composites
| FFI-BPD | NEO-BPD | |
|---|---|---|
|
| ||
| Sample 1 | ||
|
| ||
| SCID-II P/Q | .63* | .63* |
|
| ||
| Sample 2 | ||
|
| ||
| PDQ-4 | .60* | .61* |
| SCID-II P/Q | .59* | .60* |
| MSI-BPD | .60* | .62* |
|
| ||
| Sample 3 | ||
|
| ||
| PAI-BOR | .72* | - |
|
| ||
| Sample 4 | ||
|
| ||
| SIDP-IV | .42* | .43* |
|
| ||
| Sample 5 | ||
|
| ||
| SCID-II | .55* | .59* |
|
| ||
| Sample 6 | ||
|
| ||
| SIDP-IV | .35* | .45* |
| PAI-BOR | .60* | .67* |
|
| ||
| Median correlation | .60 | .61 |
Note:
=p<.01; SCID-II P/Q – Structured Clinical Interview for DSM-IV Axis II Personality Disorders – Personality Questionnaire; PDQ-4+ = Personality Diagnostic Questionnaire-4+; MSI-BPD = McLean Screening Instrument for Borderline Personality Disorder; SIDP-IV = Structured Interview for DSM-IV Personality; SCID-II = Structured Clinical Interview for DSM-IV Axis II Personality Disorders; PAI-BOR = Personality Assessment Inventory – Borderline subscale;
Hierarchical linear regression was also utilized to examine whether NEO-BPD accounted for substantial unique variance in the explicit BPD measures beyond NEO-FFI. First, we entered the FFI-BPD composite at Step 1 and the NEO-BPD composite at Step 2. At Step 1, FFI-BPD accounted for between 13% (SIDP-IV in Sample 6) and 40% (SCID-II P/Q in Sample 1) of the variance in BPD, with an average R-squared of .29. At Step 2, NEO-BPD accounted for between 3% (SCID-II P/Q, MSI and PDQ, and SIDP-IV in Samples 1, 2, and 4, respectively) and 7% (SIDP-IV in Sample 6) of incremental variance with an average change in R-squared equal to .04.
To examine the convergent and discriminant validity of the FFI-BPD composite, we examined its correlations with external variables assessing etiological risk factors (i.e., childhood abuse), psychiatric symptomatology (e.g., emotion dysregulation, anxiety, depression, illicit drug use), and PDs in relation to FFI-BPD, NEO-BPD, and explicit measures of BPD were compared in the five samples which were not utilized for genetic analyses (i.e., Samples 1, 2, 4, 5, and 6). Results are presented in Table 4. For explicit measures of BPD, correlations ranged from .07 (Schizoid PD in Sample 6) to .66 (Antisocial PD in Sample 5). For FFI-BPD, correlations ranged from .03 (Schizoid PD in Sample 6) to .61 (BSI Depression in Sample 5), and for NEO-BPD, correlations ranged from .02 (Schizoid PD in Samples 1 and 6) to .61 (BSI Depression in Sample 5).
Table 4.
Correlations between BPD, FFI-BPD, NEO-BPD and psychiatric variables
| BPD | FFI-BPD | NEO-BPD | |
|---|---|---|---|
|
| |||
| Sample 1 (N=358) | |||
| Illicit Drug Use Count | .15 | .19 | .27 |
| Paranoid PD | .52 | .42 | .36 |
| Schizoid PD | .18 | .11 | .02 |
| Schizotypal PD | .51 | .35 | .32 |
| Antisocial PD | .31 | .33 | .37 |
| Histrionic PD | .25 | .20 | .27 |
| Narcissistic PD | .42 | .34 | .33 |
| Avoidant PD | .32 | .33 | .21 |
| Dependent PD | .40 | .40 | .29 |
| Obsessive-Compulsive PD | .25 | .12 | .09 |
|
| |||
| Sample 2 (N=350) | |||
| BSI Anxiety | .46 | .47 | .41 |
| BSI Depression | .50 | .49 | .45 |
| Childhood Abuse | .39 | .41 | .36 |
| Illicit Drug Use Count | .25 | .19 | .25 |
| Emotion Dysregulation | .59 | .58 | .58 |
|
| |||
| Sample 4 (N=1611) | |||
| Lifetime MDD | .22 | .19 | .16 |
| Lifetime Alcohol Dependence | .25 | .18 | .18 |
| Lifetime Drug Dependence | .23 | .14 | .15 |
| Paranoid PD | .33 | .25 | .23 |
| Schizoid PD | .17 | .15 | .08 |
| Schizotypal PD | .25 | .19 | .17 |
| Antisocial PD | .40 | .25 | .25 |
| Histrionic PD | .29 | .15 | .18 |
| Narcissistic PD | .30 | .20 | .16 |
| Avoidant PD | .22 | .28 | .24 |
| Dependent PD | .26 | .25 | .20 |
| Obsessive-Compulsive PD | .20 | .18 | .15 |
|
| |||
| Sample 5 (N=107) | |||
| BSI Anxiety | .62 | .59 | .59 |
| BSI Depression | .61 | .61 | .61 |
| Illicit Drug Use Count | .36 | .37 | .34 |
| Paranoid PD | .57 | .46 | .48 |
| Schizoid PD | .17 | .24 | .16 |
| Schizotypal PD | .45 | .33 | .30 |
| Antisocial PD | .66 | .44 | .50 |
| Histrionic PD | .33 | .16 | .21 |
| Narcissistic PD | .35 | .33 | .31 |
| Avoidant PD | .33 | .39 | .38 |
| Dependent PD | .53 | .50 | .51 |
| Obsessive-Compulsive PD | .21 | .26 | .27 |
|
| |||
| Sample 6 (N=148) | |||
| Paranoid PD | .48 | .30 | .32 |
| Schizoid PD | .07 | .05 | .02 |
| Schizotypal PD | .33 | .09 | .16 |
| Antisocial PD | .53 | .29 | .37 |
| Histrionic PD | .46 | .22 | .30 |
| Narcissistic PD | .60 | .26 | .32 |
| Avoidant PD | .13 | .18 | .07 |
| Dependent PD | .30 | .19 | .18 |
| Obsessive-Compulsive PD | .27 | .20 | .20 |
Note:
=p<.01; p<.01; PD=Personality Disorder; BSI=Brief Symptom Inventory; MDD = Major Depressive Disorder;
To compare the pattern of correlations across the different measures of BPD, Pearson correlations and double-entry intraclass correlations (ICCDE) were computed (see McCrae, 2008 for a review). Although the relative similarity of correlations is of greater interest due to differences in methodology within and across samples, the ICCDE reflects not only similarity in shape, but also elevation and scatter (Furr, 2010). Large effect sizes emerged for both Pearson and intraclass correlations for the three profile comparisons. Of primary interest, the BPD and FFI-BPD Pearson correlation was .79 (ICCDE = .70), which is comparable to the .86 correlation that emerged between BPD and NEO-BPD (ICCDE = .74). The FFI-BPD and NEO-BPD Pearson correlation was .93 (ICCDE = .93), suggesting nearly identical profiles when using the NEO FFI rather than NEO PI-R to generate the BPD composite.
Lastly, to further test the convergent, discriminant, and criterion validity of the FFI-BPD scale, correlations were computed between FFI-BPD and the 30 FFM facets with the 24 overlapping items removed (Supplemental Table 1). The profile of correlations was compared to those generated using explicit measures of BPD. We provide averaged statistics across the five samples for both profile similarity and discriminant validity. First, a Fisher Z transformation was applied to all correlations. The average of these values for each of the 30 facets across the five samples was computed and then submitted to an inverse Fisher Z transformation. The profiles were then compared via Pearson and intraclass correlations. Very strong relative and absolute similarity between the FFM profiles for FFI-BPD and explicit measures of BPD emerged, as evidenced by the Pearson (r = .89.) and intraclass correlations (ICCDE = .89).
To obtain an overall average discriminant correlation, we focused on the association between the BPD measures (i.e., FFI-BPD and explicit measures of BPD) and the 14 FFM facets not included in the FFI-BPD composite. In all five samples, the absolute value of these correlations was computed, a Fisher Z transformation was applied, and then an average value (i.e., mean of 14 correlations for each BPD measure) was computed within each sample. The five sample values were then averaged for each BPD measure and an inverse Fisher Z transformation was applied to obtain an overall average discriminant correlation. Small effect sizes emerged for both FFI-BPD (average r = .23) and BPD (average r = .13), suggesting good discriminant validity with respect to associations with general personality traits.
Genetic analyses and results
Twin modeling of the FFI-BPD composite and BPD liability was conducted using data from Sample 3 in Mx (Neale, Boker, Xie, & HH, 2004) and full-information maximum-likelihood estimation. The PAI-BOR was used to assess BPD liability and the NEO-FFI was used to generate the FFI-BPD composite. Twin modeling enables estimation of additive genetic factors (A), non-additive genetic factors (or dominance; D) or shared environmental influences (C), and nonshared environmental factors (plus error variance; E) by examining the variance in and covariance between members of MZ and DZ twin pairs. MZ (rMZ) and DZ (rDZ) twin pair correlations were used to determine which variance components (A, C, D and E) should be modeled. Sex-averaged rMZ for BPD liability and FFI-BPD were .48 and .43, respectively. The corresponding rDZ for BPD liability and FFI-BPD were .30 and .26, respectively. Based on these correlations, additive genetic (A; rMZ>rDZ), shared environmental (C; rMZ>0.5*rDZ) and individual-specific environmental (E; rMZ≠1) influences were modeled.
FFI-BPD and BPD liability (as assessed using the PAI-BOR) were modeled in a bivariate (Cholesky decomposition) framework. Prior to twin modeling analyses, FFI-BPD and PAI-BOR scores were divided into approximately equal categories (4 and 5 categories, respectively) and tested for multivariate normality. Both ordinal variables satisfied the assumption of multivariate normality (ps > 0.05). An omnibus test of sex differences was utilized to investigate whether constraining variance components (A, C, E) but not thresholds, across sexes resulted in a significant deterioration of fit using the difference in −2 log likelihood fit which is distributed as a chi-square. Similarly, the role of C was examined by constraining it to zero. Due to the relatively small sample size and uneven distribution of same- versus opposite-sex DZ pairs, qualitative sex differences (rDZOS ≠0.5) were not explored.
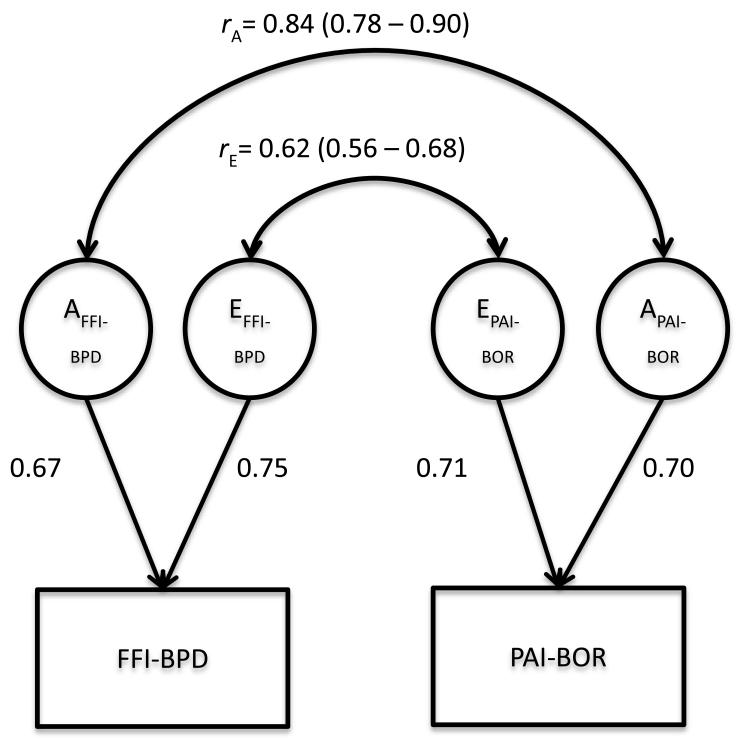
When variance components parameters were constrained to be equal across male and female twins, there was no decrement in model fit (Δχ2=2.63, 9 df; p=.98) and therefore, remaining models were estimated with variance components parameters (but not thresholds, which were estimated freely) equated across males and females. Additive genetic influences, however, could not be constrained to zero (Δχ2=15.05, 3 df, p<.01). In contrast, shared environmental influences (C) could be constrained to zero for both FFI-BPD and PAI-BOR (Δχ2=2.74, 3 df, p=0.43). The final model is presented in Figure 1. The resulting heritability (A) of FFI-BPD was estimated at 44% (95% CI: 0.37 – .0.51) with the remainder accounted for by individual-specific environmental factors (i.e., 56%; 95% CI: 0.49 – 0.63). The heritability of PAI-BOR was estimated at 49% (95% CI: 0.42 – 0.56) with individual-specific environmental factors accounting for the remaining 51% (95% CI: 0.44 – 0.58) of the variance. The phenotypic correlation between FFI-BPD and PAI-BOR was also attributable to both genetic and environmental influences. Specifically, the genetic correlation was .84 (95% CI: 0.78 – 0.90), suggesting that 71% (i.e., .842) of the genes contributing to variance in PAI-BOR overlap with those contributing to FFI-BPD. Although this correlation was substantial, the upper confidence limit was significantly lower than 1.0, indicating that there are additive genetic influences specific to PAI-BOR that are unshared with the FFI-BPD composite. The individual-specific environmental correlation was estimated at .62 (95% CI: 0.56 – 0.68).
Figure 1.
Bivariate Cholesky Model examining genetic overlap between FFI-BPD and PAI-BOR
Note: Standardized parameter estimates shown; FFI-BPD = Five-Factor Inventory Borderline Personality Disorder composite; PAI-BOR = BPD liability as assessed by the Personality Assessment Inventory – Borderline subscale; A=additive genetic influence; E=non-shared environmental influence; rA= genetic correlation between FFI-BPD and PAI-BOR; rE=non-shared environmental correlation between FFI-BPD and PAI-BOR.
Discussion
Substantial databases exist in which validated personality measures are embedded, which may allow for secondary data analyses that can inform our knowledge regarding biological influences on PD etiology as well as our understanding of PDs as they relate to issues such as comorbidity (Lynam & Widiger, 2001), sex differences (Lynam & Widiger, 2007) and changes over time (Wright, Hopwood, & Zanarini, 2015) Therefore, the current study examined the utility of a trait-based representation of BPD (FFI-BPD) generated using 24 items from the NEO FFI, a measure commonly included in large epidemiological datasets, that assess traits relevant to BPD (Lynam & Widiger, 2001; Samuel & Widiger, 2004; Samuel & Widiger, 2008).
As expected, scores on the FFI-BPD composite were higher in clinical samples relative to undergraduate and epidemiological samples, and highest in a clinical sample with 62% of participants having a DSM-IV BPD diagnosis (Sample 6). In terms of phenotypic relations between the FFI-BPD composite and explicit measures of BPD, the median correlation across studies was .60, which is as strong or stronger than the convergence often found between two explicit measures of BPD (Miller, Few, & Widiger, 2012). These findings indicate that the FFI-BPD composite is a reasonably good phenotypic proxy for BPD liability as measured using a variety of self-report and diagnostic interview assessments.
Beyond examining the correlations between BPD and FFI-BPD, we examined the association between explicit measures of BPD and NEO-BPD, which utilized 16 facet scores based on 128 items from the 240-item NEO PI-R. The goal of this analysis was to determine whether the NEO FFI omits critical information necessary in the trait-based assessment of BPD relative to the NEO PI-R. Importantly, the correlations between FFI-BPD and explicit BPD measures were nearly identical to those between the NEO-BPD composite and BPD measures (i.e., median r=.61 and .60, respectively). Additionally, the NEO-BPD accounted for relatively small amounts of incremental variance in explicit BPD measures beyond the NEO-FFI (i.e., 4% on average). This suggests that little is lost when using the NEO FFI to score BPD relative to the NEO PI-R, which is critically informative in that many existing epidemiological datasets utilize only the shorter NEO FFI.
In addition to correlations among BPD measures, relations between these measures and external variables assessing etiological risk factors, psychiatric symptomatology and other DSM-IV PDs were examined. In general, FFI-BPD correlated with these measures as expected. For example, a moderate correlation emerged between FFI-BPD and childhood abuse (r =.41), which is comparable to meta-analytic work that demonstrated a pooled correlation of .28 between BPD and childhood sexual abuse (Fossati, Madeddu, & Maffei, 1999). As expected, FFI-BPD was most strongly correlated with measures of psychiatric functioning associated with high levels of Neuroticism, such as depression, anxiety, and emotion dysregulation. With regard to PDs, the strongest correlations emerged for PDs characterized by high Neuroticism (e.g., Avoidant and Paranoid PD), low Agreeableness and Conscientiousness (e.g., Antisocial PD), whereas somewhat weaker correlations emerged for PDs characterized by Extraversion (i.e., Histrionic PD, Schizoid PD) and high Conscientiousness (i.e., Obsessive-Compulsive PD). Of greater importance than the magnitude of correlations between FFI-BPD and external variables was the observed similarity in the pattern of these correlations relative to those generated by explicit measures of BPD and the NEO-BPD composite. Strong similarity was observed across all three composites, again supporting the use of FFI-BPD as a proxy for BPD liability and suggesting high overlap between composites created from the short and long version of the NEO. Strong profile similarity between FFI-BPD and explicit measures of BPD was also demonstrated with regard to relations with the 30 FFM traits.
In general, both the FFI-BPD and explicit measures of BPD demonstrated only modest evidence of discriminant validity in terms of associations with other PDs. This is not entirely surprising as researchers have argued that PDs are largely comorbid due to shared underlying traits (Lynam & Widiger, 2001). Furthermore, there is little support for the clustering of PDs, and recent re-analysis of PD data in an epidemiological sample (Trull, Verges, Wood, & Sher, 2013) demonstrated that the structure of the ten DSM-IV PDs is better accounted for by a general PD factor rather than a three-cluster hierarchical structure shown in previous work (Cox, Clara, Worobec, & Grant, 2012). Despite this, evidence of discriminant validity was demonstrated when examining relations with FFM traits. Small average discriminant correlations emerged for FFI-BPD and explicit measures of BPD in relation to the 14 FFM traits (predominantly from the Extraversion and Openness domains) not included in the FFI-BPD composite. The correlation for FFI-BPD (r = .23) was somewhat larger than that generated from explicit measures of BPD (r = .13), although this is likely attributable to shared method variance.
With regard to genetic analyses and in line with previous studies of BPD (see Amad et al., 2014, for a review), the heritability estimates for BPD liability and the FFI-BPD composite were nearly identical (49% and 44%, respectively), with the remaining variance attributable to individual-specific environmental influences. These findings are consistent with theoretical explanations of BPD etiology suggesting that a temperamental predisposition (i.e., personality) in conjunction with invalidating environmental experiences can lead to the development of borderline symptomatology (Linehan, 1987).
Of primary interest in the current study, however, was the extent to which BPD liability and the FFI-BPD composite are influenced by the same genes, with the goal of determining whether the FFI-BPD composite can be used as a genetic proxy for BPD liability in existing epidemiological datasets with limited explicit assessment of BPD. Results of bivariate twin modeling suggested that 71% of the genes influencing BPD liability (as assessed using the PAI-BOR) are shared with the FFI-BPD composite. The strong genetic correlation (.84) is promising in that a large percentage of genetic influences on BPD liability would be captured in genetic analyses using the FFI-BPD composite. For example, genome-wide association studies (GWAS) have examined personality traits such as Neuroticism, individually, using meta-analytic methods (Amin et al., 2013) – such studies can be easily extended to study configurations of traits, such as FFI-BPD. The results could further be examined for overlap with existing results from the GWAS of BPD (Lubke et al., 2014), and this molecular genetic overlap could be formally quantified by creating polygenic scores and predicting, say, variance in BPD from scores derived from large meta-analyses of the FFI-BPD composite. Importantly, however, there are genes specific to BPD liability assessed using the PAI-BOR that are unshared with the FFI-BPD composite, as evidenced by the 95% confidence interval not including 1.0. Therefore, using the FFI-BPD composite as a genetic proxy for BPD liability, although useful, would not capture all of the genetic influences on BPD (at least as dimensionally assessed using the PAI-BOR).
There are several strengths of the current study, including the use of multiple datasets with rich FFM personality data and BPD data assessed using both self-report and interview-based measures. Additionally, a wide range of samples was utilized, including undergraduates, older adults, and clinical outpatients, which enabled a more comprehensive characterization of the phenotypic relationship between BPD liability and FFI-BPD, as well as between FFI-BPD and other measures of etiological risk and psychiatric symptomatology, and enhances the generalizability of findings. Notably, FFI-BPD exhibited a very reasonable degree of consistency in correlations with these clinical covariates across samples. The genetic analyses also provide initial support for the intended application of this measure, which is to utilize this measure in existing genetic datasets. Despite these strengths, there were limitations, most notably the use of self-reported BPD in the genetic analyses, which may have inflated the genetic and environmental correlations with self-reported FFI-BPD due to common method variance. Examination of the genetic correlation between FFI-BPD and alternative, interview-based measures of BPD would provide further support for the validity of the FFI-BPD composite. Several of the external variables were also derived via self-report methodology, such as childhood sexual abuse. Similar to the limitations of assessing life stress that have been articulated (Monroe, 2008), retrospective self-report assessment of childhood trauma is susceptible to memory and recall bias (Hardt & Rutter, 2004). However, it should be noted that the purpose of these analyses was to demonstrate a similar pattern of correlations for FFI-BPD and explicit measures of BPD rather than characterize the magnitude of the relationship between BPD and these external variables. Other limitations include small sample sizes, particularly in the clinical populations, and the lack of a second twin study to replicate the genetic findings.
There are additional conceptual limitations worth mention. First, there is considerable debate surrounding the construct validity of BPD. Several studies using confirmatory factor analysis have found that the DSM BPD diagnostic criteria are unidimensional (e.g., Clifton & Pilkonis, 2007; Johansen, Karterud, Pedersen, Gude, & Falkum, 2004). However, exploratory factory analytic studies have identified between two and four factors that explain the BPD criteria (e.g., Sanislow et al., 2002; Becker, McGlashan, & Grilo, 2006) highlighting the potential heterogeneity of BPD, which has been a longstanding criticism of the construct (Tyrer, 1999). Thus, one might argue that trait-based measures, while advantageous in their ability to account for heterogeneity, should not be used to recreate potentially invalid diagnostic categories. While we understand this rationale, there are both practical and empirical reasons for using trait-based measures that can be used to assess PDs. From a practical standpoint, the current diagnostic manual (DSM-5) continues to utilize a categorical model of diagnosis, and furthermore, the Section III model for future research employs a hybrid categorical-dimensional model of PD assessment and classification. Researchers have indicated that this retention of PD categories or constructs has persisted in order to maintain continuity in clinical practice (Skodol, Morey, Bender, & Oldham, 2013). This approach has also received empirical support, with more recent research demonstrating a hybrid categorical-dimensional model of BPD criteria (Hallquist & Pilkonis, 2012) and genetic research identifying support for the heritability of BPD features and a latent BPD construct, through which genetic and environmental factors influence these features (Distel et al., 2010). Therefore, the use of trait-based measures to assess PD constructs, in essence, embodies the zeitgeist of the field’s theoretical, empirical, and practical approach to PD assessment. Furthermore, genetic studies focus on a liability continuum, and trait-based measures (as opposed to dichotomous case-control outcomes) facilitate analyses by increasing the total variability in a phenotype.
Secondly, it is necessary to encourage some caution regarding the use of the NEO FFI as a substitute for explicit measures of BPD or as a preferable alternative to the longer NEO PI-R. Although FFI-BPD may serve as a reasonable approximation of BPD in existing datasets with limited personality data, brief measures often have limitations. For example, as has been the case in the literature regarding the assessment of expressed emotion (Hooley & Richters, 1991), shorter measures, although strongly correlated with the original construct, may be limited in their predictive validity. Thus, explicit measures of BPD and more robust trait-based assessments of BPD (e.g., FFM BPD count; Miller et al., 2005), which have considerably greater empirical support to date, should be used when feasible.
In conclusion, results of this study provide preliminary support for the validity of a 24-item composite of BPD liability generated using the NEO FFI. This FFI-BPD composite demonstrates moderate to strong convergence with explicit measures of BPD and correlates as expected with a number of relevant psychiatric variables, including childhood abuse, depression, anxiety, emotion dysregulation, and PDs. Furthermore, heritability estimates for FFI-BPD and an explicit measure of BPD liability were nearly identical, and the genetic correlation indicated that 71% of the genetic influences between these two phenotypes are shared. Importantly, our goal with the presentation of the genetic analyses was to demonstrate that our trait-based conceptualization of BPD is heritable and that this heritability roughly captures a substantial proportion of additive genetic variance in an explicit measure of BPD. This will allow future GWAS to aggregate data on the more commonly assessed FFI BPD. Results also provide further support for trait-based conceptualization and assessment of PDs, and suggest that trait-based composites may be utilized to further understanding of the epidemiology of PDs in datasets that are limited to brief, general measures of personality traits.
Supplementary Material
Table 1.
Description of samples and measures used in the current study
| Size | Population | FFM Measure |
BPD measure | Validity Measures | |
|---|---|---|---|---|---|
| Sample 1 | 358 | undergraduate students |
NEO PI-R | SCID-II P/Q | SCID-II P/Q Illicit Drug Use |
| Sample 2 | 350 | undergraduate students |
NEO PI-R | SCID II P/Q PDQ-4+ MSI-BPD |
BSI CATS DERS Illicit Drug Use |
| Sample 3 | 3127 | adult Australian twins |
NEO FFI | PAI-BOR | |
| Sample 4 | 1611 | older adult community |
NEO PI-R | SIDP-IV | SIDP-IV C-DIS-IV M.I.N.I |
| Sample 5 | 107 | adult outpatient: general clinical |
NEO PI-R | SCID-II | SCID-II BSI Illicit Drug Use |
| Sample 6 | 151 | adult outpatient: BPD (62%) and MDD/DYS (34%) |
NEO PI-R | SIDP-IV PAI-BOR |
SIDP-IV |
Note: FFM = Five-Factor Model; BPD = Borderline Personality Disorder; MDD/DYS = Major Depressive Disorder/Dysthymia; NEO PI-R = NEO Personality Inventory-Revised; NEO FFI = NEO Five Factor Inventory; SCID-II P/Q – Structured Clinical Interview for DSM-IV Axis II Personality Disorders – Personality Questionnaire; PDQ-4+ = Personality Diagnostic Questionnaire-4+; MSI-BPD = McLean Screening Instrument for Borderline Personality Disorder; SIDP-IV = Structured Interview for DSM-IV Personality; SCID-II = Structured Clinical Interview for DSM-IV Axis II Personality Disorders; PAI-BOR = Personality Assessment Inventory – Borderline subscale; BSI = Brief Symptom Inventory; CATS = Child Abuse and Trauma Scale; DERS = Difficulties in Emotion Regulation Scale; C-DIS-IV = Computerized Diagnostic Interview Schedule screener; M.I.N.I. = MINI-International Neuropsychiatric Interview;
Acknowledgments
This research was funded by National Institute on Drug Abuse (NIDA) grants: DA18267 (ML; data collection); DA23668 & DA32573 (AA; analysis), National Institute on Alcohol Abuse and Alcoholism (NIAAA) grants: AA023693 (LF), and National Institute of Mental Health (NIMH) grants: MH077840 (TO; sample 5); MH069472 (TT; sample 6); collection of sample 3 was facilitated through access to the Australian Twin Registry, a national resource supported by an Enabling Grant (ID 628911) from the National Health & Medical Research Council.
References
- Amad A, Ramoz N, Thomas P, Jardri R, Gorwood P. Genetics of borderline personality disorder: Systematic review and proposal of an integrative model. Neuroscience and Biobehavioral Reviews. 2014 doi: 10.1016/j.neubiorev.2014.01.003. doi:10.1016/j.neubiorev.2014.01.003. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association DSM 5. American Journal of Psychiatry. 2013:991. doi:10.1176/appi.books.9780890425596.744053. [Google Scholar]
- Amin N, Hottenga J-J, Hansell NK, Janssens ACJW, de Moor MHM, Madden PAF, van Duijn CM. Refining genome-wide linkage intervals using a meta-analysis of genome-wide association studies identifies loci influencing personality dimensions. European Journal of Human Genetics : EJHG. 2013;21(8):876–82. doi: 10.1038/ejhg.2012.263. doi:10.1038/ejhg.2012.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansell EB, Sanislow CA, McGlashan TH, Grilo CM. Psychosocial impairment and treatment utilization by patients with borderline personality disorder, other personality disorders, mood and anxiety disorders, and a healthy comparison group. Comprehensive Psychiatry. 2007;48:329–336. doi: 10.1016/j.comppsych.2007.02.001. doi: 10.1016/j.comppsych.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Becker DF, McGlashan TH, Grilo CM. Exploratory factor analysis of borderline personality disorder criteria in hospitalized adolescents. Comprehensive Psychiatry. 2006;47:99–105. doi: 10.1016/j.comppsych.2005.07.003. 10.1016/j.comppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Gunderson JG. Treatment utilization by patients with personality disorders. American Journal of Psychiatry. 2001;158:295–302. doi: 10.1176/appi.ajp.158.2.295. doi:10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Patrick CJ, Iacono WG, McGue M. Development and validation of the Minnesota borderline personality disorder scale. Assessment. 2011;18:234–252. doi: 10.1177/1073191111398320. doi: 10.1177/1073191111398320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono W. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: a longitudinal discordant twin design. Journal of Abnormal Psychology. 2013;122:180–194. doi: 10.1037/a0028328. doi: 10.1037/a0028328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calati R, Gressier F, Balestri M, Serretti A. Genetic modulation of borderline personality disorder: Systematic review and meta-analysis. Journal of Psychiatric Research. 2013 doi: 10.1016/j.jpsychires.2013.06.002. doi:10.1016/j.jpsychires.2013.06.002. [DOI] [PubMed] [Google Scholar]
- Clark LA. Assessment and diagnosis of personality disorder: perennial issues and an emerging reconceptualization. Annual Review of Psychology. 2007;58:227–57. doi: 10.1146/annurev.psych.57.102904.190200. doi:10.1146/annurev.psych.57.102904.190200. [DOI] [PubMed] [Google Scholar]
- Clifton A, Pilkonis PA. Evidence for a single latent class of Diagnostic and Statistical Manual of Mental Disorders borderline personality pathology. Comprehensive Psychiatry. 2007;48:70–78. doi: 10.1016/j.comppsych.2006.07.002. doi: 10.1016/j.comppsych.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Costa, McCrae RR. Neo PI-R professional manual. Vol. 396. Psychological Assessment Resources; Odessa, FL: 1992. [Google Scholar]
- Cox BJ, Clara IP, Worobec LM, Grant BF. An empirical evaluation of the structure of DSM-IV personality disorders in a nationally representative sample: results of confirmatory factor analysis in the National Epidemiologic Survey on Alcohol and Related Conditions Waves 1 and 2. Journal of Personality Disorders. 2012;26:890–901. doi: 10.1521/pedi.2012.26.6.890. doi: 10.1521/pedi.2012.26.6.890. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. Psychological Medicine. 1983;13(3):595–605. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6622612. [PubMed] [Google Scholar]
- Distel MA, Trull TJ, Willemsen G, Vink JM, Derom CA, Lynskey M, Boomsma DI. The Five-Factor Model of Personality and Borderline Personality Disorder: A Genetic Analysis of Comorbidity. Biological Psychiatry. 2009;66:1131–1138. doi: 10.1016/j.biopsych.2009.07.017. doi:10.1016/j.biopsych.2009.07.017. [DOI] [PubMed] [Google Scholar]
- Distel MA, Willemsen G, Ligthart L, Derom CA, Martin NG, Neale MC, et al. Genetic covariance structure of the four main features of borderline personality disorder. Journal of Personality Disorders. 2010;24:427–444. doi: 10.1521/pedi.2010.24.4.427. doi: 10.1521/pedi.2010.24.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, et al. Borderline personality disorder co-morbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Few LR, Grant JD, Trull TJ, Statham DJ, Martin NG, Lynskey MT, Agrawal A. Genetic variation in personality traits explains genetic overlap between borderline personality features and substance use disorders. Addiction (Abingdon, England) 2014 doi: 10.1111/add.12690. doi:10.1111/add.12690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Few LR, Miller JD, Rothbaum AO, Meller S, Maples J, Terry DP, MacKillop J. Examination of the Section III DSM-5 diagnostic system for personality disorders in an outpatient clinical sample. Journal of Abnormal Psychology. 2013;122(4):1057–69. doi: 10.1037/a0034878. doi:10.1037/a0034878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer R, Williams J, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) American Psychiatric Press, Inc.; 1997. [Google Scholar]
- Fossati A, Madeddu F, Maffei C. Borderline Personality Disorder and childhood sexual abuse: a meta-analytic study. Journal of Personality Disorders. 1999;13(3):268–80. doi: 10.1521/pedi.1999.13.3.268. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10498039. [DOI] [PubMed] [Google Scholar]
- Furr RM. The double-entry intraclass correlation as an index of profile similarity: meaning, limitations, and alternatives. Journal of Personality Assessment. 2010;92:1–15. doi: 10.1080/00223890903379134. doi: 10.1080/00223890903379134. [DOI] [PubMed] [Google Scholar]
- Gratz K, Roemer L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gunderson JG. Seeking clarity for future revisions of the personality disorders in DSM-5. Personality Disorders. 2013;4(4):368–76. doi: 10.1037/per0000026. doi:10.1037/per0000026. [DOI] [PubMed] [Google Scholar]
- Hallquist MN, Pilkonis PA. Refining the phenotype of borderline personality disorder: Diagnostic criteria and beyond. Personality Disorders: Theory, Research, and Treatment. 2012;3:228–246. doi: 10.1037/a0027953. doi: 10.1037/a0027953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hill J, Pilkonis P, Morse J, Feske U, Reynolds S, Hope H, Broyden N. Social domain dysfunction and disorganization in borderline personality disorder. Psychological Medicine. 2008;38:135–146. doi: 10.1017/S0033291707001626. doi:10.1017/S0033291707001626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM, Richters JE. Alternative measures of expressed emotion: a methodological and cautionary note. Journal of Abnormal Psychology. 1991;100(1):94–7. doi: 10.1037//0021-843x.100.1.94. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2005278. [DOI] [PubMed] [Google Scholar]
- Hyler S. PDQ-4 and PDQ-4+ instructions for use. New York State Psychiatric Institute; New York: 1994. [Google Scholar]
- Jahng S, Solhan MB, Tomko RL, Wood PK, Piasecki TM, Trull TJ. Affect and alcohol use: an ecological momentary assessment study of outpatients with borderline personality disorder. Journal of Abnormal Psychology. 2011;120(3):572–84. doi: 10.1037/a0024686. doi:10.1037/a0024686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen M, Karterud S, Pedersen G, Gude T, Falkum E. An investigation of the prototype validity of the borderline DSM-IV construct. Acta Psychiatrica Scandinavica. 2004;109:289–298. doi: 10.1046/j.1600-0447.2003.00268.x. [DOI] [PubMed] [Google Scholar]
- Linehan M. Dialectical Behavior Therapy for borderline personality disorder: Theory and method. Bulletin of the Menninger Clinic. 1987;51:261–276. [PubMed] [Google Scholar]
- Lubke GH, Laurin C, Amin N, Hottenga JJ, Willemsen G, van Grootheest G, Boomsma DI. Genome-wide analyses of borderline personality features. Molecular Psychiatry. 2014;19(8):923–9. doi: 10.1038/mp.2013.109. doi:10.1038/mp.2013.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR, Widiger TA. Using the five-factor model to represent the DSM-IV personality disorders: an expert consensus approach. Journal of Abnormal Psychology. 2001;110(3):401–12. doi: 10.1037//0021-843x.110.3.401. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11502083. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Widiger TA. Using a general model of personality to understand sex differences in the personality disorders. Journal of Personality Disorders. 2007;21:583–602. doi: 10.1521/pedi.2007.21.6.583. doi:10.1521/pedi.2007.21.6.583. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Agrawal A, Henders A, Nelson EC, Madden PAF, Martin NG. An Australian twin study of cannabis and other illicit drug use and misuse, and other psychopathology. Twin Research and Human Genetics : The Official Journal of the International Society for Twin Studies. 2012;15(5):631–41. doi: 10.1017/thg.2012.41. doi:10.1017/thg.2012.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maples JL, Guan L, Carter NT, Miller JD. A Test of the International Personality Item Pool Representation of the Revised NEO Personality Inventory and Development of a 120-Item IPIP-Based Measure of the Five-Factor Model. Psychological Assessment. 2014 doi: 10.1037/pas0000004. doi:10.1037/pas0000004. [DOI] [PubMed] [Google Scholar]
- McCrae RR. A note on some measures of profile agreement. Journal of Personality Assessment. 2008;90:105–109. doi: 10.1080/00223890701845104. doi: 10.1080/00223890701845104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JD. Five-Factor Model Personality Disorder Prototypes: A Review of Their Development, Validity, and Comparison to Alternative Approaches. Journal of Personality. 2012;80:1565–1591. doi: 10.1111/j.1467-6494.2012.00773.x. doi:10.1111/j.1467-6494.2012.00773.x. [DOI] [PubMed] [Google Scholar]
- Miller JD, Bagby RM, Pilkonis PA, Reynolds SK, Lynam DR. A simplified technique for scoring DSM-IV personality disorders with the Five-Factor Model. Assessment. 2005;12:404–415. doi: 10.1177/1073191105280987. doi:10.1177/1073191105280987. [DOI] [PubMed] [Google Scholar]
- Miller JD, Dir A, Gentile B, Wilson L, Pryor LR, Campbell WK. Searching for a vulnerable dark triad: comparing Factor 2 psychopathy, vulnerable narcissism, and borderline personality disorder. Journal of Personality. 2010;78(5):1529–64. doi: 10.1111/j.1467-6494.2010.00660.x. doi:10.1111/j.1467-6494.2010.00660.x. [DOI] [PubMed] [Google Scholar]
- Miller JD, Few LR, Lynam DR, MacKillop J. Pathological personality traits can capture DSM-IV personality disorder types. Personality Disorders: Theory, Research, and Treatment. 2014;6 doi: 10.1037/per0000064. doi: 10.1037/per0000064. [DOI] [PubMed] [Google Scholar]
- Miller JD, Few L, Widiger T. Assessment of Personality Disorders and Related Traits: Bridging DSM-IV-TR and DSM-5. In: Widiger T, editor. Oxford Handbook of Personality Disorder. Oxford University Press; New York: 2012. pp. 108–140. Retrieved from http://www.ljemail.org/reference/ReferencesPapers.aspx?ReferenceID=1302317. [Google Scholar]
- Miller JD, Morse JQ, Nolf K, Stepp SD, Pilkonis PA. Can DSM–IV Borderline Personality Disorder Be Diagnosed via Dimensional Personality Traits? Implications for the DSM-5 Personality Disorder Proposal. Journal of Abnormal Psychology. 2012 doi: 10.1037/a0027410. doi:10.1037/a0027410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Annual Review of Clinical Psychology. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Morey LC. Personality Assessment Inventory, Professional Manual. Psychological Assessment Resources, Inc.; Lutz, FL: 1991. [Google Scholar]
- Morey LC, Hopwood CJ, Markowitz JC, Gunderson JG, Grilo CM, McGlashan TH, Skodol AE. Comparison of alternative models for personality disorders, II: 6-, 8- and 10-year follow-up. Psychological Medicine. 2012;42(8):1705–13. doi: 10.1017/S0033291711002601. doi:10.1017/S0033291711002601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC, Skodol AE, Oldham JM. Clinician judgments of clinical utility: A comparison of DSM-IV-TR personality disorders and the alternative model for DSM-5 personality disorders. Journal of Abnormal Psychology. 2014;123:398–405. doi: 10.1037/a0036481. doi:10.1037/a0036481. [DOI] [PubMed] [Google Scholar]
- Neale M, Boker S, Xie G, HH M. Mx: Statistical modeling. 6th ed. Department of Psychiatry; Richmond, VA: VCU Box 900126: 2004. [Google Scholar]
- Oltmanns TF, Rodrigues MM, Weinstein Y, Gleason MEJ. Prevalence of Personality Disorders at Midlife in a Community Sample: Disorders and Symptoms Reflected in Interview, Self, and Informant Reports. Journal of Psychopathology and Behavioral Assessment. 2014;36(2):177–188. doi: 10.1007/s10862-013-9389-7. doi:10.1007/s10862-013-9389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14:150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Bluhm N, Zimmerman M. Structured Interview for DSM-IV Personality: SIDP-IV. American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Pompili M, Girardi P, Ruberto A, Tatarelli R. Suicide in borderline personality disorder: a meta-analysis. Nordic Journal of Psychiatry. 2005;59:319–324. doi: 10.1080/08039480500320025. doi:10.1080/08039480500320025. [DOI] [PubMed] [Google Scholar]
- Poythress NG, Skeem JL, Lilienfeld SO. Associations among early abuse, dissociation, and psychopathy in an offender sample. Journal of Abnormal Psychology. 2006;115(2):288–97. doi: 10.1037/0021-843X.115.2.288. doi:10.1037/0021-843X.115.2.288. [DOI] [PubMed] [Google Scholar]
- Robins L, Helzer A. The half-life of a structured interview: The NIMH Diagnostic Interview Schedule (DIS) International Journal of Methods in Psychiatric Research. 1994:95–102. [Google Scholar]
- Ruocco AC, Lam J, McMain SF. Subjective cognitive complaints and functional disability in patients with borderline personality disorder and their nonaffected first-degree relatives. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 2014;59(6):335–44. doi: 10.1177/070674371405900607. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25007408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel DB, Widiger TA. Clinicians’ personality descriptions of prototypic personality disorders. Journal of Personality Disorders. 2004;18:286–308. doi: 10.1521/pedi.18.3.286.35446. doi: 10.1521/pedi.18.3.286.35446. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: a facet level analysis. Clinical Psychology Review. 2008;28(8):1326–42. doi: 10.1016/j.cpr.2008.07.002. doi:10.1016/j.cpr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, et al. Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: findings from the collaborative longitudinal personality disorders study. American Journal of Psychiatry. 2002;159:284–290. doi: 10.1176/appi.ajp.159.2.284. [DOI] [PubMed] [Google Scholar]
- Scott LN, Stepp SD, Pilkonis PA. Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Personality Disorders: Theory, Research, and Treatment. 2014;5:278–288. doi: 10.1037/per0000070. doi: 10.1037/per0000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry. 1998;59(Suppl 2):22–33. quiz 34–57. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9881538. [PubMed] [Google Scholar]
- Skodol AE, Morey LC, Bender DS, Oldham JM. The ironic fate of the personality disorders in DSM-5. Personality Disorders: Theory, Research, and Treatment. 2013;4:342–349. doi: 10.1037/per0000029. doi: 10.1037/per0000029. [DOI] [PubMed] [Google Scholar]
- Tomko RL, Trull TJ, Wood PK, Sher KJ. Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. Journal of Personality Disorders. 2014;28:734–750. doi: 10.1521/pedi_2012_26_093. doi: 10.1521/pedi_2012_26_093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Widiger TA, Lynam DR, Costa PT. Borderline personality disorder from the perspective of general personality functioning. Journal of Abnormal Psychology. 2003;112:193–202. doi: 10.1037/0021-843x.112.2.193. doi:10.1037/0021-843X.112.2.193. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Verges A, Wood PK, Sher KJ. The structure of DSM-IV-TR personality disorder diagnoses in NESARC: a reanalysis. Journal of Personality Disorders. 2013;27:727–734. doi: 10.1521/pedi_2013_27_107. doi: 10.1521/pedi_2013_27_107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer P. Borderline personality disorder: a motley diagnosis in need of reform. Lancet. 1999;354:2095–2096. doi: 10.1016/S0140-6736(99)00401-8. doi: 10.1016/S0140-6736(99)00401-8. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Presnall JR. Clinical application of the five-factor model. Journal of Personality. 2013;81:515–527. doi: 10.1111/jopy.12004. doi: 10.1111/jopy.12004. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: shifting to a dimensional model. The American Psychologist. 2007;62(2):71–83. doi: 10.1037/0003-066X.62.2.71. doi:10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Wright AG, Hopwood CJ, Zanarini MC. Associations netween changes in normal personality traits and borderline personality disorder symptoms over 16 years. Personality Disorders: Theory, Research, and Treatment. 2015;6:1–11. doi: 10.1037/per0000092. doi: 10.1037/per0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) Journal of Personality Disorders. 2003;17:568–573. doi: 10.1521/pedi.17.6.568.25355. doi:10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Rothschild L, Chelminski I. The prevalence of DSM-IV personality disorders in psychiatric outpatients. American Journal of Psychiatry. 2005;162:1911–1918. doi: 10.1176/appi.ajp.162.10.1911. doi: 10.1176/appi.ajp.162.10.1911. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.