Abstract
AIM
To evaluate the diagnostic efficiency of basic indicators and find characteristic indicators for keratoconus (KC) at adjacent stages, and to assess the progression pattern of KC.
METHODS
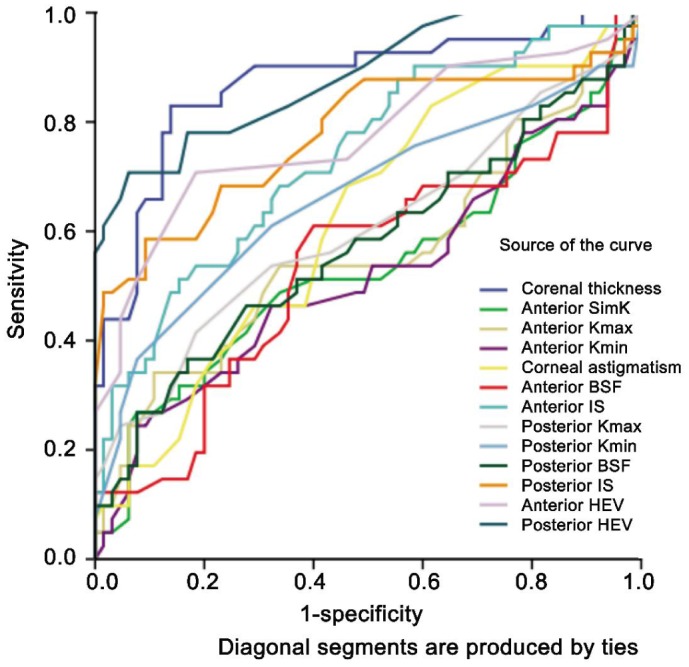
One hundred and eight (41 subclinical, 40 moderate, and 27 severe) keratoconic patients (108 eyes) and 105 myopic patients (105 eyes) as controls were recruited in this prospective, comparative case series study. Pentacam topography was performed. Receiver-operating-characteristic curves were used to get the characteristic indicators.
RESULTS
The most efficient distinguishing index between the subclinical KC and the controls was posterior elevation value (PEV, AUC=0.882), with the highest specificity being 93.8%. Corneal thickness (AUC=0.852) and posterior inferior-superior value (I-S) ranked second and third (AUC=0.776). When KC became moderate, PEV remained to be of the highest diagnostic efficiency (AUC=0.988), followed by the anterior elevation value (AUC=0.986) and other parameters of anterior surface. The diagnostic value increased significantly in the anterior curvature indices (all AUC>0.900) and appeared in the anterior best fitting sphere radius (AUC=0.919) when KC developed into the severe stage.
CONCLUSION
In the subclinical stage of KC, PEV, thickness, and posterior I-S had important diagnostic values, and elevation values remained most efficient when KC developed to the moderate stage. The anterior curvature indices were most characteristic when KC became severe. KC first appeared in the inferior cornea of posterior surface, but the feature of protrusion formed at the moderate stage.
Keywords: keratoconus, progression pattern, Pentacam, topography, diagnostic efficiency
INTRODUCTION
Keratoconus (KC) is a bilateral, noninflammatory, progressive eye disorder characterized by corneal thinning and anterior protrusion[1], with an incidence of 1/2000 in the general population. It is a major reason for corneal transplantation in developed countries[1]–[3]. There are many classification criteria of KC. According to the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) guidelines, KC is divided into early KC, moderate KC, and severe KC[4]. Different clinical management approaches could be offered depending on the exact stage of the disease.
Topography is the most useful tool for the early detection and progression monitoring of KC[5]–[8], although other new examination methods, such as wavefront aberration measurements and optical coherence tomography, are commonly used[9]–[11]. At the early stage of this ectatic disorder, topography using the Scheimpflug device like Pentacam seems to be much sensitive [5].
There have been many clinical reports about topography for detection of KC [3],[8],[12]–[14]. Some researches provided compound indicators, such as the KC percentage index KISA%[7],corneal thickness spatial profile[15], and percentage thickness increase, which could screen forme fruste KC well; some investigated the change in topographic indicators of KC over a short period of time. However, neither evaluation of the diagnostic efficiency of indicators differentiating adjacent KC stages nor description about KC progressive pattern through the whole disease course is available. In this study, the diagnosing efficiency of indicators differentiating adjacent KC stages was investigated with the assistance of Pentacam topography. The most efficient indicators of each stage were connected in order and progressive pattern through the whole course was described. Basic indicators rather than compound indicators were used, so that the disease developing course can be easily understood, and the findings can be conveniently applied to daily clinical practice.
SUBJECTS AND METHODS
Patients
Patients with any history of other eye disease or surgery, or combined acute hydrops were excluded, and contact lens wearers were required to stop wearing for at least 3wk. Informed consent was obtained from all patients. This study was approved by the ethics committee of our institution, and all the procedures followed the tenets of the Declaration of Helsinki.
There are many criteria for diagnosis and severity grading of KC[4],[7],[14],[16]–[21]. The Massachusetts Eye and Ear Infirmary criteria (MEEI criteria)[16],[17] were used in this study to differentiate suspected and confirmed KC. According to the scoring, patients with at least one confirmed keratoconic eye were recruited. They were 45 females and 63 males, aged from 15 to 33y (mean, 20.7 ±5.5). The fellow eyes of 41 patients with unilateral KC were grouped as subclinical KC (41 eyes), and the 67 eyes of 67 patients with bilateral confirmed KC were further classified by severity based on the steep simulated K value. According to the CLEK guidelines[4],[18] , a steep simulated K of less than 45.00 D was classified as mild KC (0 eyes), 45.00 to 52.00 D as moderate KC (40 eyes), and more than 52.00 D as severe KC (27 eyes). Moreover, 105 patients (40 females and 65 males, 105 eyes) with myopia but no other eye diseases were used as controls, with an age of 17 to 38y (mean, 22.7 ±6.5). The cases of myopia were all axial, with normal corneas.
Pentacam Topography
The Pentacam system (Oculus Inc., Wetzlar, Germany) was used for topographic examination. The measurement results were checked under the quality specification (QS) window, and only the correct measurements (“QS” reads OK) were accepted.
Indexes
The elevation maps and sagittal curvature maps, as well as the corneal thickness, obtained using the Pentacam system, were evaluated. The float 8-mm best-fit-sphere calculated zone was selected; the maximum K (Kmax), minimum K (Kmin), mean simulated K (SimKm), corneal astigmatism (CA), best-fitting sphere radius (BFS), inferior-superior (I-S) value, elevation value of posterior/anterior surface (PEV/AEV), and minimum corneal thickness were recorded.
The I-S value was calculated by subtracting the superior value from the inferior value[7],and the superior/inferior value was calculated by averaging 5 data points along the superior /inferior cornea 3.0 mm from the center of the cornea at 30-degree intervals. The elevation value was acquired from the thinnest point of the elevation maps.
Statistical Analysis
The parameters were compared among the groups of severe KC, moderate KC, subclinical KC, and controls using the one-way ANOVA test or Mann-Whitney test. A Bonferroni correction was used to control the type 1 error (a=0.05).
Receiver operating characteristic (ROC) curves were used to find the parameters with high diagnosing efficiency for KC between two adjacent stages (subclinical KC vs controls, moderate KC vs subclinical KC, and severe KC vs moderate KC) according to the area under the curve (AUC). Then the characteristic parameters for KC in each stage were connected in a series, and progression pattern of this disease was obtained.
RESULTS
The distribution of posterior I-S in the controls was concentrated, with a mean of 0.1±0.1 D (95% confidence regions: 0.11 D to 0.17 D). The corneal thickness ranged from 449 µm to 577 µm in subclinical KC and from 485 µm to 635 µm in the controls (Table 1). The most characteristic index was PEV (AUC=0.882), followed by corneal thickness (AUC=0.852) and posterior I-S value (AUC=0.776) between the eyes with subclinical KC and the controls (Table 2; Figure 1). The PEV was 2.2±3.4 µm in the control group and 17.7±12.7 µm in the subclinical KC group. The cutoff value was 7.5 µm, with a sensitivity of 70.7% and a specificity of 93.8%.
Table 1. The basic data of four groups.
| Indicators | Severe KC | Moderate KC | Subclinical KC | Control |
| Anterior | ||||
| Kmax | 59.3±8.9 Dc | 47.0±2.1 Db | 43.3±1.7 D | 43.1±1.3 D |
| Kmin | 63.5±10.1 Dc | 48.7±2.2 Db | 44.0±1.9 D | 43.8±1.4 D |
| SimKm | 55.8±8.0 Dc | 45.4±2.2 Db | 42.5±1.6 D | 42.7±1.3 D |
| CA | 7.7±3.7 Dc | 3.3±1.6 Db | 1.5±0.7 D | 1.0±1.0 D |
| BSF | 7.1±0.5 mmc | 7.8±0.2 mmb | 7.9±0.3 mm | 7.9±0.2 mm |
| I-S | 5.9±4.8 D | 5.8±3.3 Db | 0.9±1.1 D | 0.1±0.7 D |
| AEV | 67.0±26.9 µmc | 30.0±10.3 µmb | 6.0±4.5µm | 2.3±1.9 µm |
| Posterior | ||||
| Kmax | -9.9±1.5 Dc | -7.4±0.5 Db | -6.6±0.3 D | -6.5±0.2 D |
| Kmin | -8.4±1.4 Dc | -6.6±0.5 Db | -6.1±0.3 D | -6.1±0.2 D |
| BSF | 6.0±0.4 mmc | 6.4±0.2 mmb | 6.5±0.3 mm | 6.4±0.2 mm |
| I-S | 1.1±1.3 Dc | 1.4±0.6 Db | 0.4±0.4 Da | 0.1±0.1 D |
| PEV | 143.1±52.1 µmc | 65.8±21.0 µmb | 17.7±12.7 µma | 2.2±3.4 µm |
| Thickness | 407.9±57.8 µmc | 454.8±33.4 µmb | 500.5±30.0 µma | 544.0±29.3 µm |
aSubclinical KC vs control, P<0.05; bModerate KC vs subclinical KC, P<0.05; cSevere KC vs moderate KC, P<0.05. Kmax: Maximum K; Kmin: Minimum K; SimKm: Mean simulated K; CA: Corneal astigmatism; BFS: Best-fitting sphere radius; I-S: Inferior-superior value; AEV: Anterior elevation value; PEV: Posterior elevation value.
Table 2. AUC and cutoff values of ROC curve in subclinical KC vs control eyes.
| Index | AUC | Cutoff value | Sensitivity (%) | Specificity (%) |
| PEV | 0.882 | 7.5 µm | 70.7 | 93.8 |
| Thickness | 0.852 | 523.5 µm | 78.1 | 81 |
| Posterior I-S | 0.776 | 0.35 D | 58.5 | 90.8 |
| AEV | 0.774 | 3.5 µm | 70.7 | 81.5 |
| Anterior I-S | 0.736 | 0.82 D | 51.2 | 84.6 |
PEV: Posterior elevation value; I-S: Inferior-superior value; AEV: Anterior elevation value; AUC: Area under curve.
Figure 1. ROC curve of subclinical KC vs control eyes.
Between the subclinical and moderate stages, the diagnostic efficiency of all characteristic indices increased significantly (all AUC≥0.9). The diagnostic efficiency of these indices decreased orderly from PEV, AEV, anterior Kmax, and anterior I-S to posterior I-S, and posterior Kmax. Between the two adjacent stages, the most characteristic index was still PEV (AUC=0.988), with a sensitivity of 95% and a specificity of 92.7%. The cutoff value was 37.0 µm in PEV and 15.0 µm in AEV. As for corneal thickness, its diagnostic efficiency (AUC=0.852) relatively declined compared to some other indexes (Table 3).
Table 3. AUC and cutoff values of ROC curve in moderate KC vs subclinical KC eyes.
| Index | AUC | Cutoff value | Sensitivity (%) | Specificity (%) |
| PEV | 0.988 | 37.0 µm | 95.0 | 92.7 |
| AEV | 0.986 | 15.0 µm | 91.3 | 96.3 |
| Anterior Kmax | 0.939 | 46.75 D | 85.0 | 92.7 |
| Anterior I-S | 0.938 | 2.31 D | 87.5 | 92.7 |
| Posterior I-S | 0.916 | 0.68 D | 92.5 | 91.2 |
| Posterior Kmax | 0.916 | -6.95 D | 90.0 | 82.9 |
| Thickness | 0.852 | 464.5 µm | 92.9 | 71.5 |
PEV: Posterior elevation value; AEV: Anterior elevation value; Kmax: Maximum K; AUC: Area under curve.
The anterior BFS was 7.9±0.2 mm, 7.9±0.3 mm, 7.8±0.2 mm, and 7.1±0.5 mm in the controlled, subclinical KC, moderate KC, and severe KC eyes, respectively. When KC became severe, the diagnostic efficiency of characteristic indices decreased from the anterior Kmax, posterior Kmax, anterior SimKm, anterior Kmin to PEV, anterior BFS, and AEV orderly, all being high (all AUC>0.9; Table 4).
Table 4. AUC and cutoff values of ROC curve in severe KC vs moderate KC eyes.
| Index | AUC | Cutoff value | Sensitivity (%) | Specificity (%) |
| Anterior Kmax | 1.00 | 52.15 D | 100 | 100 |
| Posterior Kmax | 0.988 | -7.90 D | 100 | 87.5 |
| Anterior SimKm | 0.972 | 50.75 D | 84.6 | 100 |
| Anterior Kmin | 0.925 | 48.95 D | 84.6 | 92.5 |
| PEV | 0.923 | 92.50 µm | 84.6 | 95.0 |
| Anterior BFS | 0.919 | 7.53 µm | 87.5 | 85.2 |
| AEV | 0.913 | 46.00 µm | 76.9 | 97.5 |
| Thickness | 0.795 | 422.50 µm | 85.0 | 65.4 |
Kmax: Maximum K; Kmin: Minimum K; SimKm: Mean simulated K; BFS: Best-fitting sphere radius; PEV: Posterior elevation value; AEV: Anterior elevation value; AUC: Area under curve.
DISCUSSION
The pathogenesis of primary KC remains unclear. Early screening and diagnosis of this disease [3], [6]–[10],[12]were investigated in recent years. The progression course was also detected by topography, but the follow-up period was not long [8],[18]–[20]. Li et al[21] calculated that approximately 50% of clinically normal fellow eyes of patients with unilateral KC would develop KC within 16y. It is indeed difficult to continuously follow so many patients through the whole disease course. In our study, the differentiating indices between two adjacent stages were found, and the indices with high diagnosing efficiency were determined as the manifestation of KC progression from one stage to the next, then the progression pattern of KC was speculated, in the optical point of view.
Elevation
The traditional diagnostic criteria of KC mainly include clinical signs and indices of curvature maps by topography, but the diagnostic value of elevation maps has drawn increasing attention [3],[5],[12],[17],[22],[23]. Elevation value is often measured as the maximum value above the BFS in the central 5 mm of the cornea, which is suitable for centrally protruded KC (advanced KC), but not for very early KC and normal eyes. The incorporation of astigmatic elevation into the calculation of average normal elevation artificially can inflate the normal elevation measurements and reduce their screening utility[23]. In our study, the elevation value was acquired from the thinnest point as reported by Khachikian and Belin[23]. In their report, the PEV at the thinnest point was 3.6±4.7 µm for normal eyes and 9.4±5.4 µm for eyes with subclinical KC, in proximity to our measure results. Other new elevation-acquisition methods were also taken recently. Kamiya et al[14] used the enhanced BFS (with exclusion of a 3.5-mm optical zone in the thinnest portion of the cornea), and Smadja et al[24] used best-fit toric and aspheric reference surface to get elevation value in order to improve screening efficiency.
Subclinical Keratoconus vs Controls
The most characteristic index was PEV between the eyes with subclinical KC and the controls. This was in accordance with report of de Sanctis et al[3]. In their study, posterior elevation showed high predictive accuracy for subclinical KC compared to the controls (AUC=0.93), and the optimal cutoff point was 29 µm, with a sensitivity of 68% and a specificity of 90.8%. Because of the difference of acquiring points, our cutoff value (7.5 µm) was much smaller, but with an approximate sensitivity (70.7%) and specificity (93.8%).
The second efficient diagnostic index was corneal thickness (0.852), with the highest sensitivity in all indices; it meant that the cornea getting thinner was the most sensitive alteration at the subclinical KC stage. This important role related to corneal thickness in early stage of KC was also reported by Mihaltz et al[25].They reported that posterior and anterior elevation showed the best predictive accuracy, followed by minimal and central pachymetry (0.89 and 0.88) between KC (mild and moderate) and the controls. In our study, KC was divided by severity. The diagnostic value of corneal thickness was high in the early stage, but declined when KC became moderate from the subclinical stage.
The third characteristic index was posterior I-S value. In the classic diagnostic criteria of KC, the anterior I-S value played a very important part[1],[4],[16], and our result indicated that it was the same to the posterior I-S, even more important in the very early stage.
The cornea of the subclinical keratoconic eyes would protrude from the inferior periphery of posterior surface, showing an elevation and a larger inferior curvature on the posterior surface, without obvious protrusion of the anterior surface. Our finding is consistent with the report from Pinero et al[22]. They did not find any significant difference in the central corneal curvature on posterior surface between the subclinical KC and the control.
Moderate Keratoconus vs Subclinical Keratoconus
The leading characteristic index of moderate KC was also PEV, which increased significantly from 17.7±12.7 µm (subclinical stage) to 65.8±21.0 µm (moderate stage). This demonstrated that the continuous development of corneal ectasia in the posterior surface remained to be the most significant feature when KC developed from the subclinical to moderate stage.
With the highest specificity of 96.3% and a sensitivity of 91.3%, AEV was another characteristic index. It indicated that from the moderate stage the ectasia of anterior surface was obvious, not just the posterior surface cone. The feature of corneal protrusion centrally formed. The finding is partly consistent with the report of Mihaltz et al[25] in which posterior and anterior elevation showed the best predictive accuracy (AUC: 0.97 and 0.96, respectively) between eyes with KC (mild and moderate) and the controls.
Besides elevation, other indices of anterior surface, such as anterior Kmax (AUC: 0.939) and anterior I-S (AUC: 0.938), began to change markedly. The diagnostic efficiency of all characteristic indices increased obviously in the moderate stage, indicating a rapid development of KC. In contrast, the relative diagnostic value of thickness at this stage (AUC: 0.852) relatively declined.
Severe Keratoconus vs Moderate Keratoconus
All AUCs of the characteristic indices were larger than 0.9 in the comparison of severe KC and moderate KC. Not only the Kmax (AUC=1.0) but also the SimKm and Kmin changed dramatically. It indicated the cornea protruded to a wider range.
The diagnostic efficiency of anterior BFS at the severe stage became obvious. Anterior BFS values in normal eyes, subclinical KC and moderate KC eyes were close, but became much smaller in severe KC eyes. In some reports, KC was classified with the index of anterior BFS. Our results showed that the diagnostic value of anterior BFS was little at previous stages, only being improved to the severe stage. Although new reference surface such as toric and aspheric surface can be used to improve screening efficiency, the BFS was the most often used reference surface in daily practice.
In the process from moderate KC to severe KC, accompanied with the thinning of cornea, the diagnostic value increased in anterior curvature indices and appeared in anterior BFS, but declined in the I-S value. All the changes indicated that when KC developed to the severe stage, the cornea appeared entirely protruding.
Previously, many researchers just evaluated changes of KC at one particular stage or mixed stages over a short period of time. Kim and Joo[19] observed the progression of KC over 3y using Orbscan II, and found the rate of keratometric change was 0.78±0.99 D/half-year, with a rate of keratometric change of 1.37±1.08 D/half-year in the eyes exhibiting progression and 0.15±0.15 D/half-year in the eyes exhibiting no apparent progression; eye rubbing and inferior steepening were observed to be associated with progression after diagnosis. Taneja et al[18] investigated changes using Orbscan in patients with KC and vernal keratoconjunctivitis over 1y, and reported that in patients with progression (8/22), a statistically significant change was found in posterior float curvature, SimK astigmatism, and maximum astigmatism. The whole progression course of KC is very long. Choi and Kim[20] revealed that progression occurred in approximately 50% of patients with mild KC, with an increased central K of 1.50 D during 12y. In this study, the characteristic indicators were involved to describe the whole development course of KC.
In conclusion, PEV seemed to be the most characteristic index of KC in the subclinical and moderate stages. In the subclinical stage, PEV, I-S, and thickness had important diagnostic values, but were replaced by PEV, AEV, and parameters of anterior surface when KC became moderate. The diagnostic value increased significantly in anterior curvature indices and appeared in anterior BFS, but declined in the I-S value when moderate KC developed into severe KC. It may be speculated that accompanied with the thinning of cornea, keratoconic eyes usually have slight protrusion of posterior surface from inferior periphery first. Besides further elevation of posterior surface, anterior surface would protrude significantly, and the feature of central protrusion forms at the moderate stage of KC. When KC becomes severe, the curvature increased dramatically, and the cornea protrudes wholly.
Acknowledgments
Conflicts of Interest: Du XL, None; Chen M, None; Xie LX, None.
REFERENCES
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Wilson SE, Klyce SD. Screening for corneal topographic abnormalities before refractive surgery. Ophthalmology. 1994;101(1):147–152. doi: 10.1016/s0161-6420(94)31372-8. [DOI] [PubMed] [Google Scholar]
- 3.de Sanctis U, Loiacono C, Richiardi L, Turco D, Mutani B, Grignolo FM. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminating keratoconus/subclinical keratoconus. Ophthalmology. 2008;115(9):1534–1539. doi: 10.1016/j.ophtha.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 4.Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, Shin JA, Sterling JL, Wagner H, Gordon MO. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39(13):2537–2546. [PubMed] [Google Scholar]
- 5.Hashemi H, Mehravaran S. Day to day clinically relevant corneal elevation, thickness, and curvature parameters using the Orbscan II Scanning Slit Topographer and the Pentacam Scheimpflug Imaging Device. Middle East Afr J Ophthalmol. 2010;17(1):44–55. doi: 10.4103/0974-9233.61216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ucakhan OO, Cetinkor V, Ozkan M, Kanpolat A. Evaluation of Scheimpflug imaging parameters in subclinical keratoconus, keratoconus, and normal eyes. J Cataract Refract Surg. 2011;37(6):1116–1124. doi: 10.1016/j.jcrs.2010.12.049. [DOI] [PubMed] [Google Scholar]
- 7.Li X, Yang H, Rabinowitz YS. Keratoconus: classification scheme based on videokeratography and clinical signs. J Cataract Refract Surg. 2009;35(9):1597–1603. doi: 10.1016/j.jcrs.2009.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahin A, Yildirim N, Basmak H. Two-year interval changes in Orbscan II topography in eyes with keratoconus. J Cataract Refract Surg. 2008;34(8):1295–1299. doi: 10.1016/j.jcrs.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 9.Qin B, Chen S, Brass R, Li Y, Tang M, Zhang X, Wang X, Wang Q, Huang D. Keratoconus diagnosis with optical coherence tomography-based pachymetric scoring system. J Cataract Refract Surg. 2013;39(12):1864–1871. doi: 10.1016/j.jcrs.2013.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buhren J, Kook D, Yoon G, Kohnen T. Detection of subclinical keratoconus by using corneal anterior and posterior surface aberrations and thickness spatial profiles. Invest Ophthalmol Vis Sci. 2010;51(7):3424–3432. doi: 10.1167/iovs.09-4960. [DOI] [PubMed] [Google Scholar]
- 11.Lo W, Chen WL, Hsueh CM, Ghazaryan AA, Chen SJ, Ma DH, Dong CY, Tan HY. Fast Fourier transform-based analysis of second-harmonic generation image in keratoconic cornea. Invest Ophthalmol Vis Sci. 2012;53(7):3501–3507. doi: 10.1167/iovs.10-6697. [DOI] [PubMed] [Google Scholar]
- 12.Schlegel Z, Hoang-Xuan T, Gatinel D. Comparison of and correlation between anterior and posterior corneal elevation maps in normal eyes and keratoconus-suspect eyes. J Cataract Refract Surg. 2008;34(5):789–795. doi: 10.1016/j.jcrs.2007.12.036. [DOI] [PubMed] [Google Scholar]
- 13.Kanellopoulos AJ, Asimellis G. Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol. 2013;7:1539–1548. doi: 10.2147/OPTH.S44741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamiya K, Ishii R, Shimizu K, Igarashi A. Evaluation of corneal elevation, pachymetry and keratometry in keratoconic eyes with respect to the stage of Amsler-Krumeich classification. Br J Ophthalmol. 2014;98(4):459–463. doi: 10.1136/bjophthalmol-2013-304132. [DOI] [PubMed] [Google Scholar]
- 15.Ambrosio R, Jr, Alonso RS, Luz A, Coca Velarde LG. Corneal-thickness spatial profile and corneal-volume distribution: tomographic indices to detect keratoconus. J Cataract Refract Surg. 2006;32(11):1851–1859. doi: 10.1016/j.jcrs.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 16.Melki SA, Azar DT. LASIK complications: etiology, management, and prevention. Surv Ophthalmol. 2001;46(2):95–116. doi: 10.1016/s0039-6257(01)00254-5. [DOI] [PubMed] [Google Scholar]
- 17.Prakash G, Agarwal A, Mazhari AI, Kumar G, Desai P, Kumar DA, Jacob S, Agarwal A. A new, pachymetry-based approach for diagnostic cutoffs for normal, suspect and keratoconic cornea. Eye(Lond) 2012;26(5):650–657. doi: 10.1038/eye.2011.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taneja M, Ashar JN, Mathur A, Vaddavalli PK, Rathi V, Sangwan V, Murthy S. Measure of keratoconus progression in patients with vernal keratoconjunctivitis using scanning slit topography. Cont Lens Anterior Eye. 2013;36(1):41–44. doi: 10.1016/j.clae.2012.10.067. [DOI] [PubMed] [Google Scholar]
- 19.Kim H, Joo CK. Measure of keratoconus progression using Orbscan II. J Refract Surg. 2008;24(6):600–605. doi: 10.3928/1081597X-20080601-08. [DOI] [PubMed] [Google Scholar]
- 20.Choi JA, Kim MS. Progression of keratoconus by longitudinal assessment with corneal topography. Invest Ophthalmol Vis Sci. 2012;53(2):927–935. doi: 10.1167/iovs.11-8118. [DOI] [PubMed] [Google Scholar]
- 21.Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology. 2004;111(3):440–446. doi: 10.1016/j.ophtha.2003.06.020. [DOI] [PubMed] [Google Scholar]
- 22.Pinero DP, Alio JL, Aleson A, Escaf Vergara M, Miranda M. Corneal volume, pachymetry, and correlation of anterior and posterior corneal shape in subclinical and different stages of clinical keratoconus. J Cataract Refract Surg. 2010;36(5):814–825. doi: 10.1016/j.jcrs.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 23.Khachikian SS, Belin MW. Posterior elevation in keratoconus. Ophthalmology. 2009;116(4) doi: 10.1016/j.ophtha.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Smadja D, Santhiago MR, Mello GR, Krueger RR, Colin J, Touboul D. Influence of the reference surface shape for discriminating between normal corneas, subclinical keratoconus, and keratoconus. J Refract Surg. 2013;29(4):274–281. doi: 10.3928/1081597X-20130318-07. [DOI] [PubMed] [Google Scholar]
- 25.Mihaltz K, Kovacs I, Takacs A, Nagy ZZ. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with pentacam. Cornea. 2009;28(9):976–980. doi: 10.1097/ICO.0b013e31819e34de. [DOI] [PubMed] [Google Scholar]


