Abstract
AIM
To assess lens thickness measurements with anterior segment-optical coherence tomography (AS-OCT) in comparison with A-scan ultrasonography (A-scan US).
METHODS
There were 218 adult subjects (218 eyes) aged 59.2±9.2y enrolled in this prospective cross-sectional study. Forty-three eyes had open angles and 175 eyes had narrow angles. Routine ophthalmic exam was performed and nuclear opacity was graded using the Lens Opacities Classification System III (LOCS III). Lens thickness was measured by AS-OCT (Visante OCT, Carl Zeiss Meditec, Dublin, CA, USA). The highest quality image was selected for each eye and lens thickness was calculated using ImageJ software. Lens thickness was also measured by A-scan US.
RESULTS
Interclass correlations showed a value of 99.7% for intra-visit measurements and 95.3% for inter-visit measurements. The mean lens thickness measured by AS-OCT was not significantly different from that of A-scan US (4.861±0.404 vs 4.866±0.351 mm, P=0.74). Lens thickness values obtained from the two instruments were highly correlated overall (Pearson correlation coefficient=0.81, P<0.001), and in all LOCS III specific subgroups except in grade 5 of nuclear opacity. Bland-Altman analysis revealed a 95% limit of agreement from -0.45 to 0.46 mm. Lens thickness difference between the two instruments became smaller as the lens thickness increased and AS-OCT yielded smaller values than A-scan US in thicker lens (β=-0.29, P<0.001)
CONCLUSION
AS-OCT-derived lens thickness measurement is valid and comparable to the results obtained by A-scan US. It can be used as a reliable noncontact method for measuring lens thickness in adults with or without significant cataract.
Keywords: lens thickness, A-scan ultrasonography, anterior segment-optical coherence tomography, biometry, cataract
INTRODUCTION
Crystalline lens thickness can affect and be affected by different conditions such as aging, presbyopia, and myopia[1]–[3]. Thickening of the crystalline lens is considered an important predisposing factor for development of angle-closure glaucoma [4]. Therefore precise measurement of lens thickness can be of value in evaluating this condition.
A variety of techniques are used to measure lens thickness. A-scan ultrasonography (A-scan US) is the reference method for biometric measurements of lens thickness[5],[6]. Accommodation has been shown to increase the variability of A-scan US lens thickness measurements. Proper alignment of the probe requires expertise and office measurement can be difficult in young children as well[5].
The anterior segment-optical coherence tomography (AS-OCT; Visante OCT, Carl Zeiss Meditec, Dublin, CA, USA) is another method for obtaining measurements of structures in the anterior segment of the eye. AS-OCT is a fast, high resolution, non-contact imaging modality that is customized for anterior segment evaluation including for glaucoma and refractive surgery applications. It is also used for measurement of corneal thickness, anterior chamber depth (ACD), and anterior chamber width[7],[8]. Lens thickness can also be measured by using images captured by AS-OCT. The use of infrared light in the device does not change the pupil's size and may hence produce a more accurate lens thickness value[9].
The purpose of this study is to assess the validity of AS-OCT lens thickness measurements in comparison with A-scan US in adult participants.
SUBJECTS AND METHODS
In this prospective study, subjects with age greater than 40y were recruited as part of the Farabi Angle Closure Study, conducted at Farabi Eye Hospital, Tehran, Iran.
The study protocol was in accordance with the tenets of the Declaration of Helsinki and approved by the Farabi Hospital Research Ethics Committee (REC) and has been explained in detail previously [10],[11].
Patients referred to glaucoma or comprehensive clinic were enrolled in the study consequently. Exclusion criteria included: corneal opacity, any history of intraocular surgery, or ocular injury.
Written informed consent was obtained from each patient. Examination and testing included best-corrected visual acuity (BCVA), intraocular pressure (IOP) measurement by Goldmann applanation tonometry, complete slit-lamp and fundus examination, and gonioscopy. Cataract classification and grading was performed using the Lens Opacities Classification System III (LOCS III) [12].
After the initial examination, lens thickness and other biometric measures were determined by both A-scan US as the reference standard and AS-OCT. The measurements were performed in the same illumination conditions by two independent examiners who were masked to one another's results.
A-scan Ultrasonography
After instilling 1 drop of tetracaine for topical anesthesia, A-scan US (Echoscan, model U3300, Nidek Inc., Tokyo, Japan) was performed with the patient in a supine position and low ambient light. The patient was asked to fixate on a fixation light hanging in front of them. The 10 MHz probe was then placed on the center of the cornea perpendicularly, taking care to not indent the cornea. Using manual freezing of the scan, five consecutive measurements of lens thickness, ACD, and axial length (AL) were obtained. An average of 5 measures was used for analysis.
Anterior Segment-Optical Coherence Tomography
AS-OCT (Visante OCT; Carl Zeiss Meditec, Dublin, CA, USA) was performed for all patients in a dark environment by a single examiner. Scans were centered on the undilated pupil, along the horizontal axis with the patient fixated on the internal fixation target.
Raw image scanning in the “anterior segment single mode” (816×638 pixels exported image) was used to capture the crystalline lens. In order to obtain an image encompassing the entire lens thickness, the focus of the instrument was moved significantly posterior to the cornea until the reflection of the posterior lens surface became visible.
The image was considered acceptable when both reflections of the anterior and posterior surfaces of the lens were visible and on the line perpendicular to the lens surface. If the examiner could not ascertain the posterior or anterior border, he flagged it as a borderline image and excluded it.
To ensure that the scans were optically aligned, images were captured such that the corneal vertex reflex could be observed clearly.
To acquire images in a non-accommodative state, the patient's distance refraction was used to adjust the fixation target.
At least 3 consecutive images were captured, and the image with the best quality regarding alignment and visibility of the corneal vertex reflex, anterior and posterior lens surface reflexes was chosen for measurement and exported as a JPEG. The same protocol was followed at the second visit within two month for 50 cases to capture three additional images of the crystalline lens to evaluate intra-observer reproducibility.
Lens Thickness Measurement
Two observers (Moghimi S, Hamzeh N) performed AS-OCT measurements with the uncorrected exported raw images using ImageJ software (US National Institutes of Health, Bethesda, Maryland, USA). The method of calculation of lens thickness from raw images from Visante OCT (software version 2.0) has been discussed previously[5].
Briefly, in anterior segment mode the software assigns a refractive index of 1.000 (air) for all structures anterior to the anterior corneal boundary, 1.388 (cornea) for all structures within the corneal boundaries, and 1.343 (aqueous) for all structures posterior to the posterior corneal boundary. However, in raw image mode the entire image is set at a refractive index at 1.000. To eliminate this problem, the number of pixels from the anterior to the posterior boundary of the lens can be measured in the ImageJ processing software and divided by 1.388 (as the refractive index of crystalline lens). To summarize, the thickness of the crystalline lens was measured in pixels and converted to millimeters using the conversion 1 mm =51 pixels. The repeatability was measured with two sets of consecutive images in 20 eyes. The intra-observer and inter-observer reproducibility of the lens thickness measurements with the software were assessed using a random subset of 20 by the examiners within 1wk and showed an intra-observer correlation coefficient of 99.3% and inter-observer correlation coefficient of 97.5%.
Statistical Analysis
Statistical analysis was performed using SPSS for Windows software (version 17.0, SPSS, Inc.). Assuming r2= 0.2, we needed 50 cases detecting a significant correlation with a power of 80%. Only right eyes of the patients if they met the inclusion and exclusion criteria were included for statistical analysis. If the left eye was the only eye that met criteria, then the left eye was chosen for analysis.
All data were reported as means±standard deviations (SD). The differences were compared statistically using the Student's t-test. The Pearson correlation was used to assess the associations between AS-OCT and A-scan measurements. Bland-Altman plots were used to find a potential dependency between differences and A-scan measurements (as the reference standard)[13]. Intra-observer agreement was performed to assess the repeatability of lens thickness measurements. P values of less than 0.05 were considered to be statistically significant.
RESULTS
In this prospective study, 245 eyes of 245 subjects were enrolled. After excluding eyes, which had, AS-OCT images with unclear (n=18) or borderline (n=5) posterior or anterior capsules or variable A-scan (n=4), a total of 218 images were analyzed. Forty-three eyes had open angles and 175 were narrow angle. Forty-eight were male and 170 were female with a mean age of 59.2±9.1y (range: 35 years old and older). Interclass correlations were excellent with a value of 99.7% for intra-visit measurements and 95.3% for inter-visit measurements.
The mean crystalline lens thickness taken by AS-OCT was not significantly different from that of A-scan US (4.861±0.404 vs 4.866±0.351 mm, P=0.74). The same result was observed among different lens opacities when analyzing different LOCS subgroups (Table 1).
Table 1. The mean crystalline lens thickness taken by A-scan ultrasonography vs anterior segment optical coherence tomography.
| Subgroups | A-scan US | AS-OCT | P |
| LOCS 1 | 4.65±0.25 | 4.59±0.30 | 0.49 |
| LOCS 2 | 4.78±0.26 | 4.80±0.26 | 0.23 |
| LOCS 3 | 4.88±0.42 | 4.88±0.35 | 0.85 |
| LOCS 4 | 4.89±0.54 | 4.94±0.51 | 0.18 |
| LOCS 5 | 5.30±0.47 | 5.14±0.18 | 0.36 |
(x±s, mm)
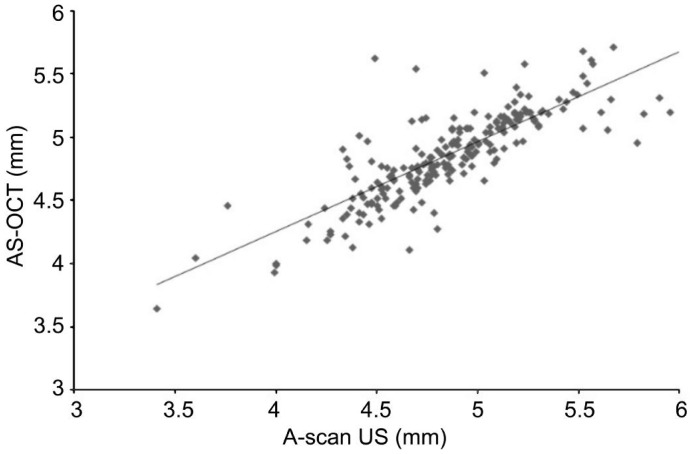
Figure 1 demonstrates the scatter diagram of lens thickness distribution measured with the two different methods. Measurements of lens thickness between the two instruments were highly correlated in all subjects (Pearson correlation coefficient =0.81, P <0.001). This is also true for all LOCS-specific subgroups except in LOCS 5 subgroup (Table 2).
Figure 1. Scatterplot of lens thickness data collected by AS-OCT and A-scan US shows a correlation coefficient of 0.81 (P<0.001).
Table 2. Comparison of measurements of lens thickness between the two instruments in specific subgroups.
| Subgroups | n | Correlation coefficient | P |
| LOCS 1 | 11 | 0.78 | 0.03 |
| LOCS 2 | 80 | 0.81 | <0.001 |
| LOCS 3 | 84 | 0.80 | <0.001 |
| LOCS 4 | 32 | 0.89 | <0.001 |
| LOCS 5 | 11 | 0.50 | 0.24 |
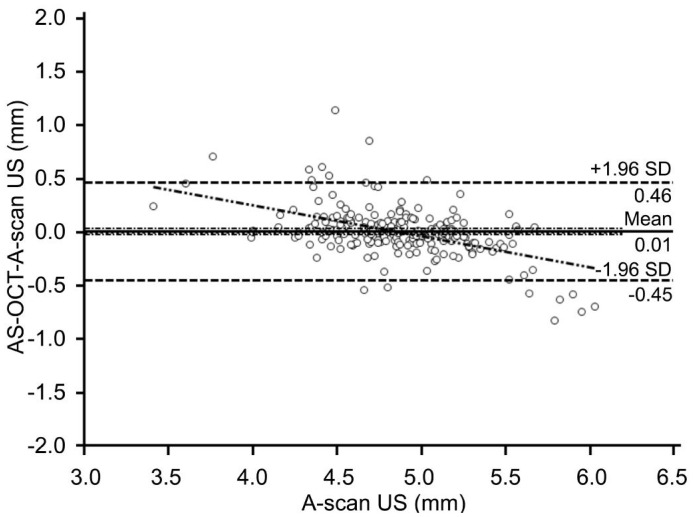
Figure 2 summarizes the results of Bland-Altman analysis for AS-OCT minus A-scan US vs A-scan US reference values. This analysis of individual pairs revealed a small bias of 0.005 (SD=0.23), with 95% limits of agreement from -0.45 to 0.46 mm. It revealed that the difference in the lens thickness between the two instruments (AS-OCT minus A-scan) became smaller as the lens thickness increased and AS-OCT yielded smaller numbers than A-scan US in thicker lens (β=-0.29, P<0.001).
Figure 2. Bland-Altman plot for AS-OCT minus A-scan US vs A-scan US reference values demonstrates a 95% limits of agreement from -0.45 to 0.46 mm.
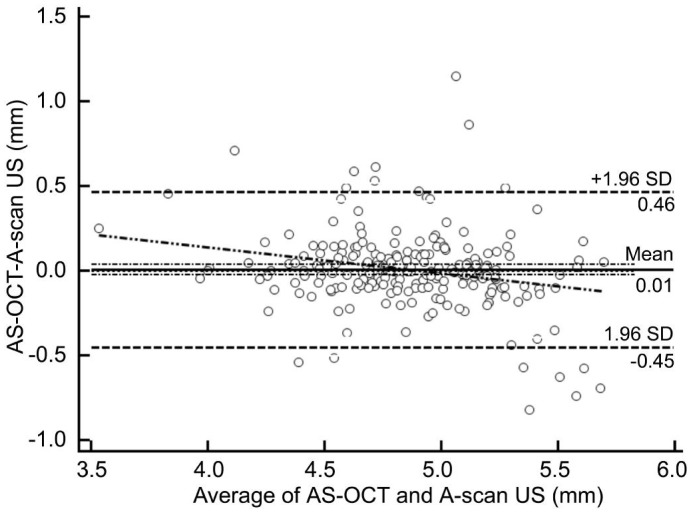
Figure 3 summarizes the results of Bland-Altman analysis for AS-OCT minus A-scan US vs mean of the A-scan and AS-OCT measurements with 95% limits of agreement from -0.45 to 0.46 mm. It revealed that the difference in the lens thickness between the two instruments (AS-OCT minus A-scan) varies according to lens thickness. (β=-0.154, P<0.001).
Figure 3. Bland-Altman plot for AS-OCT minus A-scan US vs mean of the A-scan and AS-OCT measurements demonstrates a 95% limits of agreement from -0.45 to 0.46 mm.
DISCUSSION
In this study we compared the lens thickness of 218 adults measured by AS-OCT to A-scan US, and demonstrated a high correlation between the two measurements. The values were not significantly different. This was also true in LOCS specific subgroups except in LOCS group 5.
Crystalline lens thickness is an important determining factor in conditions such as myopia, presbyopia, and angle-closure glaucoma[1],[2],[14]–[16]. It increases throughout life. Therefore accurate measurement of lens thickness is of great importance in studies related to development of refractive error, cataract surgery, and angle closure glaucoma[5].
A-scan US is currently used as the reference standard method for measuring lens thickness; however, it requires direct contact with the eye and local anesthesia. Furthermore, placing the probe in a proper position requires expertise; there is no precise landmark to align the instrument with the cornea in order to be ideally in line with the visual axis. Also corneal indention by the probe sometimes results in inaccurate measurements. Furthermore, A-scan US measurements may vary with accommodation. Because of these disadvantages, alternatives such as AS-OCT and optical A-scans including IOLMaster (CarlZeiss Meditec, Dublin, CA, USA) and Lenstar (Haag-Streit AG, Koeniz, Switzerland) are increasingly becoming adopted.
AS-OCT is a fast, simple to perform, non-contact method with a low learning curve. It uses infrared light, thus causing no alteration in pupil size, anterior chamber configuration, and perhaps lens thickness. Fixation on the internal target and accommodation can be controlled. Also there is a greater reproducibility for AS-OCT than other methods such as A-scan US and IOLMaster as reported in previous studies[3],[5],[17]–[19].
There are several studies that compared A-scan US and AS-OCT in measuring different anterior chamber parameters, but studies on lens thickness are uncommon.
In our study, we found that the AS-OCT lens thickness values did not significantly differ from the A-scan US values (P=0.74), and the two measurements highly correlated with each other. In a previous study on children, Lehman et al[5] showed that AS-OCT lens thickness measurements were significantly thinner than A-scan US (mean difference -0.045 mm). They explained the slightly thinner results by the greater refractive index used in AS-OCT than the one used in A-scan US. However, after excluding patients with AS-OCT images in which corneal reflex was not visible, the difference in lens thickness values was not significantly different, which was compatible with our results.
In a study on adult subjects, it was found that AS-OCT yielded lens thickness values significantly greater than A-scan US (0.135 mm in the elderly and 0.101 mm in young subjects), although measurements highly correlated with each other[3]. Differences in the physical principles of the two measurement methods may be the reason for the small difference. Also they explained that the difference might be the result of accommodation on A-scan US measurements, as their subjects had to fixate on the probe. In contrast, AS-OCT is not or minimally affected by accommodation.
There is substantial evidence that AS-OCT measurements such as corneal thickness, anterior chamber depth, anterior chamber angles are greatly reproducible[9].
We showed an excellent interclass correlation for lens thickness, which indicate that AS-OCT could also provide a reliable measurement of lens thickness.
Zeng et al[3] also found a high inter- and intra-observer correlation for both AS-OCT and A-scan US and demonstrated that agreement tends to be better with AS-OCT. Another study also demonstrated an excellent repeatability for lens thickness measurement by AS-OCT which was better than the best reported repeatability of A-scan US in the literature[5]. They suggested to include the corneal reflex in crystalline lens images captured by the Visante OCT to maximize excellent repeatability it already had.
Refractive index of the lens changes as the lens become denser, and lenses with different densities have different refractive indices. However, lens thickness measurements with AS-OCT presumed a constant refractive index for lens. It is the same with A-scan, which assumes a constant velocity of sound independent of lens density. Drexler et al[20] suggested that the effect of greater lens density on lens thickness measurements is more in ultrasound method than optical methods. In our study A-scan and AS-OCT values were not significantly different in LOCS subgroups and they were highly correlated except in LOCS III of No.5. The reason might be small sample of cases in the No.5 group.
The Bland-Altman plot showed that the AS-OCT/A-scan US lens thickness difference becomes smaller as the lens thickness increases; and AS-OCT yielded smaller numbers than A-scan US in thicker lens. This was the same in lenses with higher lens opacity. As a cataract progresses, the lens becomes thicker and denser and refractive index increases. As a result the measurement by AS-OCT may be an underestimation of the lens thickness[5]. Larger sample size or a study of clear lenses or very thick lens may help to identify this relationship more precisely.
There were some limitations to our study. All of our subjects were Iranian and most of them had senile cataract with high lens thickness. Moreover we didn't compare the results to the new non-contact methods like Lenstar that also uses OCT. This is especially important in thick lenses in which measurement might be more distorted using US.
In summary, AS-OCT provides lens thickness measurements in adults that are comparable to A-scan US. It can be used as a convenient non-contact and reproducible method for measuring lens thickness in adults with or without significant cataract. Since the results were not significantly different with A-scan US measurement, as the gold standard method, it may be used alternatively for lens thickness measurement. This is specially useful when lens thickness should be measured along with other anterior segment parameters, obviating the use of another instrument.
Acknowledgments
Conflicts of Interest: Hamzeh N, None; Moghimi S, None; Latifi G, None; Mohammadi M, None; Khatibi N, None; Lin SC, None.
REFERENCES
- 1.García-Domene MC, Díez-Ajenjo MA, Gracia V, Felipe A, Artigas J. A simple description of age-related changes in crystalline lens thickness. Eur J Ophthalmol. 2011;21(5):597–603. doi: 10.5301/EJO.2011.6253. [DOI] [PubMed] [Google Scholar]
- 2.Mutti DO, Zadnik K, Fusaro RE, Friedman NE, Sholtz RI, Adams AJ. Optical and structural development of the crystalline lens in childhood. Invest Ophthalmol Vis Sci. 1998;39(1):120–133. [PubMed] [Google Scholar]
- 3.Zeng Y, Liu Y, Liu X, Chen C, Xia Y, Lu M, He M. Comparison of lens thickness measurements using the anterior segment optical coherence tomography and a-scan ultrasonography. Invest Ophthalmol Vis Sci. 2009;50(1):290–294. doi: 10.1167/iovs.07-1216. [DOI] [PubMed] [Google Scholar]
- 4.Lim MC, Lim LS, Gazzard G, Husain R, Chan YH, Seah SK, Aung T. Lens opacity, thickness, and position in subjects with acute primary angle closure. J Glaucoma. 2006;15(3):260–263. doi: 10.1097/01.ijg.0000212212.10395.76. [DOI] [PubMed] [Google Scholar]
- 5.Lehman BM, Berntsen DA, Bailey MD, Zadnik K. Validation of OCT-based crystalline lens thickness measurements in children. Optom Vis Sci. 2009;86(3):181–187. doi: 10.1097/OPX.0b013e318198198d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lam AK, Chan R, Pang PC. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt. 2001;21(6):477–483. doi: 10.1046/j.1475-1313.2001.00611.x. [DOI] [PubMed] [Google Scholar]
- 7.Baikoff G, Lutun E, Ferraz C, Wei J. Static and dynamic analysis ofthe anterior segment with optical coherence tomography. J Cataract Refract Surg. 2004;30(9):1843–1850. doi: 10.1016/j.jcrs.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 8.Nemeth G, Vajas A, Tsorbatzoglou A, Kolozsvari B, Modis L, Jr, Berta A. Assessment and reproducibility of anterior chamber depth measurement with anterior segment optical coherence tomography compared with immersion ultrasonography. J Cataract Refract Surg. 2007;33(3):443–447. doi: 10.1016/j.jcrs.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Wong AL, Leung CK, Weinreb RN, Cheng AK, Cheung CY, Lam PT, Pang CP, Lam DS. Quantitative assessment of lens opacities with anterior segment optical coherence tomography. Br J Ophthalmol. 2009;93(1):61–65. doi: 10.1136/bjo.2008.137653. [DOI] [PubMed] [Google Scholar]
- 10.Latifi G, Moghimi S, Eslami Y, Fakhraie G, Zarei R, Lin S. Effect of phacoemulsification on drainage angle status in angle closure eyes with or without extensive peripheral anterior synechiae. Eur J Ophthalmol. 2012 Aug 30; doi: 10.5301/ejo.5000191. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Moghimi S, Vahedian Z, Fakhraie G, Ghaffari R, Eslami Y, Jabarvand M, Zarei R, Mohammadi M, Lin S. Ocular biometry in the subtypes of angle closure: an anterior segment optical coherence tomography study. Am J Ophthalmol. 2013;155(4):664–673. doi: 10.1016/j.ajo.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Chylack LT, Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111(6):831–836. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 13.Bland JM, Altman DG. Altman Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 14.Saxena S, Agrawal PK, Pratap VB, Nath R. Anterior chamber depth and lens thickness in primary angle-closure glaucoma: a case-control study. Indian J Ophthalmol. 1993;41(2):71–73. [PubMed] [Google Scholar]
- 15.Schachar RA, Pierscionek BK, Abolmaali A, Le T. The relationshipbetween accommodative amplitude and the ratio of central lens thickness to its equatorial diameter in vertebrate eyes. Br J Ophthalmol. 2007;91(6):812–817. doi: 10.1136/bjo.2006.107524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yip LW, Aquino MC, Chew PT. Measurement of anterior lens growth after acute primary angle-closure glaucoma. Can J Ophthalmol. 2007;42(2):321–322. [PubMed] [Google Scholar]
- 17.Baikoff G, Jodai H, Bourgeon G. Measurement of the internal diameter and depth of the anterior chamber: IOLMaster versusanterior chamber optical coherence tomographer. J Cataract Refract Surg. 2005;31(9):1722–1728. doi: 10.1016/j.jcrs.2005.02.030. [DOI] [PubMed] [Google Scholar]
- 18.O'Donnell C, Hartwig A, Radhakrishnan H. Comparison of central corneal thickness and anterior chamber depth measured using LenStar LS900, Pentacam, and Visante AS-OCT. Cornea. 2012;31(9):983–988. doi: 10.1097/ICO.0b013e31823f8e2f. [DOI] [PubMed] [Google Scholar]
- 19.Yazici AT, Bozkurt E, Alagoz C, Alagoz N, Pekel G, Kaya V, Yilmaz OF. Central corneal thickness, anterior chamber depth, and pupil diameter measurements using Visante OCT, Orbscan, and Pentacam. J Refract Surg. 2010;26(2):127–133. doi: 10.3928/1081597X-20100121-08. [DOI] [PubMed] [Google Scholar]
- 20.Drexler W, Findl O, Menapace R, Rainer G, Vass C, Hitzenberger CK, Fercher AF. Partial coherence interferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol. 1998;126(4):524–534. doi: 10.1016/s0002-9394(98)00113-5. [DOI] [PubMed] [Google Scholar]