Abstract
Objective
To investigate risk factors for S1 screw loosening after lumbosacral fusion, including spinopelvic parameters and paraspinal muscles.
Methods
We studied with 156 patients with degenerative lumbar disease who underwent lumbosacral interbody fusion and pedicle screw fixation including the level of L5-S1 between 2005 and 2012. The patients were divided into loosening and non-loosening groups. Screw loosening was defined as a halo sign larger than 1 mm around a screw. We checked cross sectional area of paraspinal muscles, mean signal intensity of the muscles on T2 weight MRI as a degree of fatty degeneration, spinopelvic parameters, bone mineral density, number of fusion level, and the characteristic of S1 screw.
Results
Twenty seven patients showed S1 screw loosening, which is 24.4% of total. The mean duration for S1 screw loosening was 7.3±4.1 months after surgery. Statistically significant risk factors were increased age, poor BMD, 3 or more fusion levels (p<0.05). Among spinopelvic parameters, a high pelvic incidence (p<0.01), a greater difference between pelvic incidence and lumbar lordotic angle preoperatively (p<0.01) and postoperatively (p<0.05). Smaller cross-sectional area and high T2 signal intensity in both multifidus and erector spinae muscles were also significant muscular risk factors (p<0.05). Small converging angle (p<0.001) and short intraosseous length (p<0.05) of S1 screw were significant screw related risk factors (p<0.05).
Conclusion
In addition to well known risk factors, spinopelvic parameters and the degeneration of paraspinal muscles also showed significant effects on the S1 screw loosening.
Keywords: Lumbosacral region, Pedicle screws, Instrumentation, Muscle, Spinal fusion, Risk factors
INTRODUCTION
Many studies have reported frequent nonunion in the lumbosacral segment comparing to other levels2,8,9) and frequent sacral pedicle screw loosening in the cases of long level lumbosacral fusion18,19,24). The sacral screw loosening was reported to be occurred in about 15.6-41.9%10,16,34). Iliac screw, bicortical screw insertion, and cement augmentation have been attempted as preventative measures according to known risk factors related with techniques for S1 screw and bone quality1,27,29,30,33,36,37,44,48). Recently, spinal balance and paraspinal muscles are known to be closely related with hardware failure especially after long level fixation for spinal deformity5,25). In other words, spinal balance and paraspinal muscles may have effects on the mechanical stress or mechanical failure of S1 screw. However, to the best of our knowledge, there was no report studying their relationships directly.
In this study, we tried to investigate various risk factors for S1 screw loosening after lumbosacral fusion, including spinopelvic parameters and the degenerative changes of paraspinal muscles.
MATERIALS AND METHODS
Patients
Total 196 patients underwent spinal fusion operations including L5-S1 level for degenerative lumbar diseases between 2005 and 2012 in our hospital. All the enrolled patients were followed up for more than 24 months after surgery. Seven cases of revision surgery, a known risk factor for screw loosening5), were excluded from this study. Thirty-three patients received open pedicle screw fixation were also excluded. Finally, we conducted this study with 156 patients with 68 males and 88 females. The mean age at the time of surgery was 58.0±12.7 years. They were divided into two groups, loosening group with S1 screw loosening and non-loosening group without S1 screw loosening at 1 year after surgery.
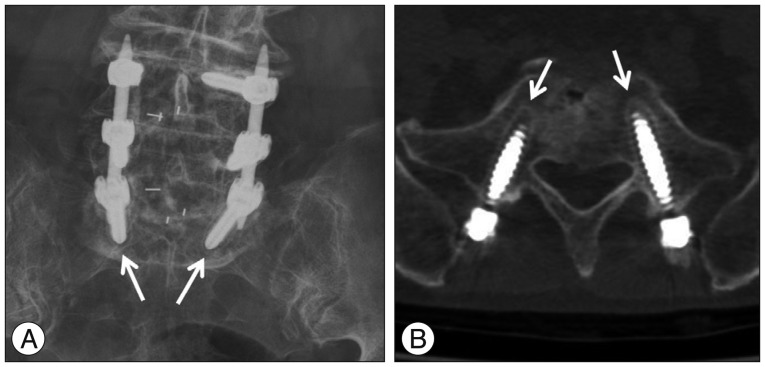
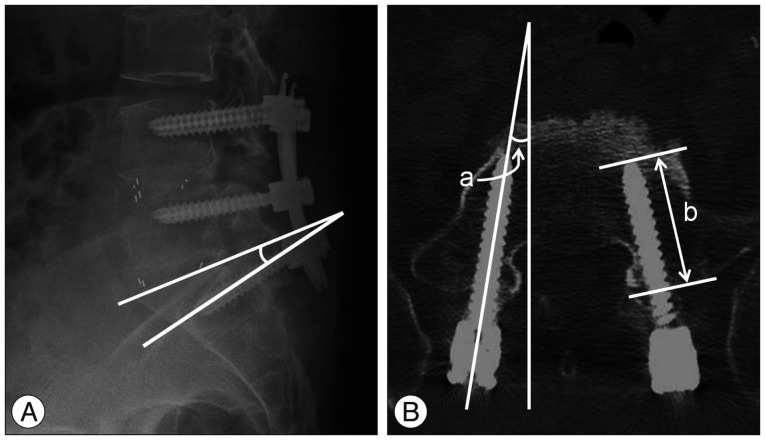
Preoperative diagnosis consisted of spinal stenosis in 144, spondylolisthesis in 100, degenerative scoliosis in 4, and discogenic pain in 2. There was no patient with sagittal imbalance on whole spine radiographic exam. All the patients received transforaminal lumbar interbody fusion (TLIF) with unilateral single interbody cage filled with autologous bone chips obtained from laminectomy and facetectomy. Numbers of fusion levels were 1-4 levels. Two percutaneous pedicle screw systems (Sextant and Longitude Systems; Medtronics, Memphis, TN, USA) were used for fixation. The diameter of S1 screw ranged 6.0-8.5 mm, and the length 35-50 mm. Screw loosening was defined as a halo sign showing a radiolucent line of ≥1 mm around the screw6,39) was found with simple radiographic films in one or both sides during 1 year after the surgery (Fig. 1).
Fig. 1. Halo sign around S1 screws (arrows) on simple radiograph (A) and CT (B).
Risk factors and radiological evaluation
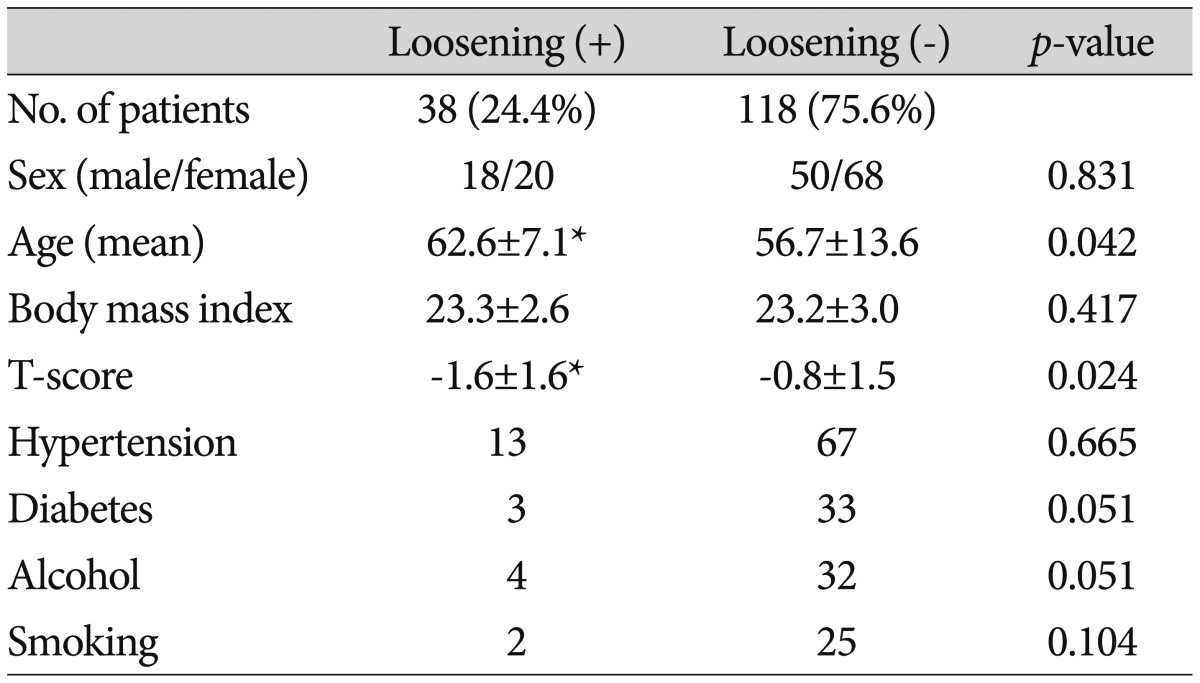
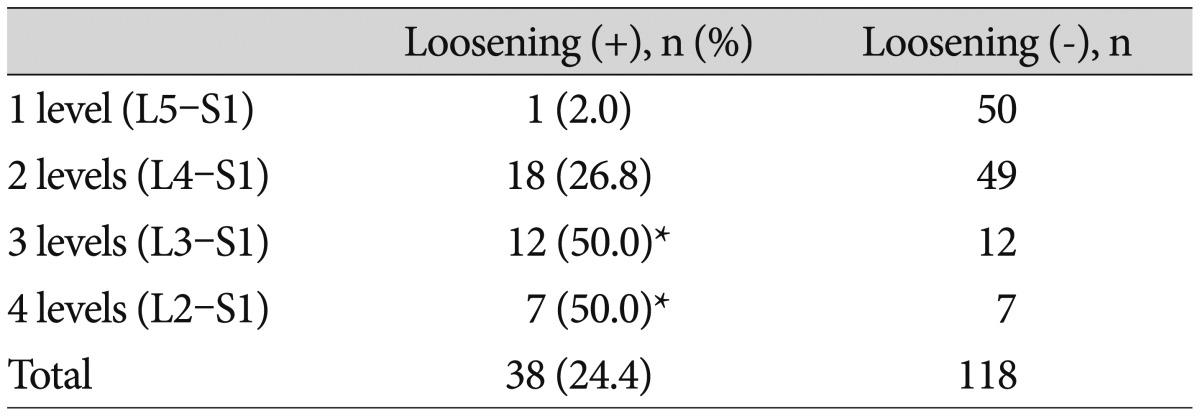
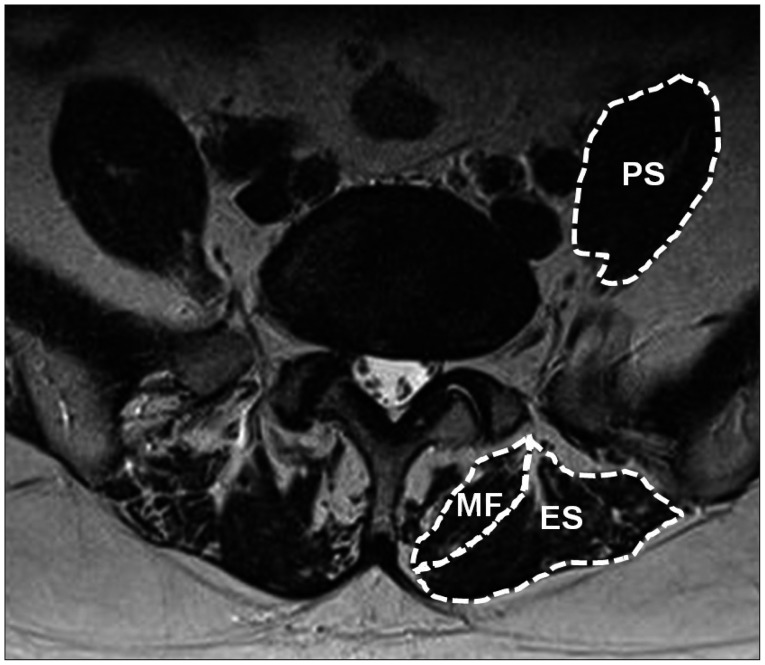
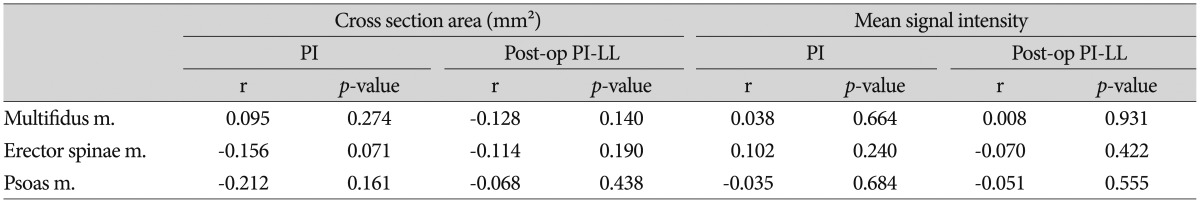
Patient's factors, sex, age, body mass index (BMI), bone mineral density (BMD), hypertension, diabetes, alcohol, and smoking, were checked (Table 1). Numbers of fusion levels were 1 (L5-S1), 2 (L4-S1), 3 (L3-S1), and 4 (L2-S1) levels (Table 2). T-score of lumbar spine was checked by measuring BMD with dual-energy radiograph absorptiometry (Lunar Prodigy; General Electric, Madison, WI, USA). Spinopelvic parameters, pre- and postoperative lumbar lordosis (LL), pelvic incidence (PI), sacral slope (SS), and difference between PI and LL (PI-LL) were measured with whole spine radiographic exam. As muscle related factors, cross sectional area (CSA) and mean signal intensity of paraspinal muscles were checked preoperatively at L5-S1 disc level with T2 weighted MRI axial images (Fig. 2). Axial and sagittal angles, diameter, length, and intraosseous length of S1 screws were checked with postoperative CT as screw related factors (Fig. 3).
Table 1. Patient profiles.
*p<.05
Table 2. Number of fusion levels and S1 screw loosening.
*p<.05
Fig. 2. Paraspinal muscles at L5-S1 level, multifidus muscle (MF), erector spinae muscle (ES), and psoas muscle (PS).
Fig. 3. A : Sagittal angle of S1 screw between screw and upper end plate of S1 vertebra on simple lateral radiograph. B : Axial angle of S1 screw between screw and vertical line (a) and intraosseous length of S1 screw as the length of intraosseous portion of the screw on postoperative CT (b).
Muscle factors were measured for 3 paraspinal muscle groups, multifidus, erector spinae, and psoas muscles. The erector spinae muscles include both longissimus muscle and iliocostalis muscles at L5-S1 level. The signal intensity of muscle on T2 weighted MRI mainly reflects the amount of intramuscular fat content which is known to be related with muscle degeneration13,17). The cross sectional area and mean signal intensity of the muscle groups were measured with tools of PACS software (M-view, Infinitt Healthcare, Seoul, Korea). All the spinopelvic parameters, muscle factors, and screw factors were measured 2 times, and their mean values were used for analysis. The screw related factors were checked at both sides separately, and the total number of measured S1 screws was 268. All the data of screw factors in the loosening group were unexceptionally those of the loosened screws because all the patients in the group showed screw loosening bilaterally.
The sagittal angle of S1 screw was measured as the angle formed between S1 screw and S1 upper plate on simple lateral radiograph. The axial angle of S1 screw was measured as the angle between S1 screw and vertical line. The intraosseous length of S1 screw was measured as the length of intraosseous portion of the screw at S1 vertebra on postoperative CT.
To assess reliability of measurements, two authors measure the radiological parameters for 2 times with 2 weeks interval between the measurements. Statistical analysis was done with Student t-test, chi-square test, and Pearson's correlation coefficient. A p value less than 0.05 was considered to be statistically significant. The intraobserver and interobserver intraclass correlation coefficients (ICC) were calculated for LL, PI, SS, CSA and mean signal intensity of paraspinal muscles, angles (axial and sagittal angles) and intraosseous length of S1 screw.
RESULTS
S1 screw loosening occurred in 38 of total 156 patients (24.4%). Mean age was significantly higher in loosening group (62.6±7.1) than non-loosening group (56.7±13.6) (p<0.05). The mean T-scores of BMD was significantly lower in loosening group (-1.6±1.6) than non-loosening group (-0.8±1.5) (p<0.05). There was no significant difference in gender, BMI, hypertension, diabetes, alcohol, and smoking history between the two groups (Table 1).
The mean duration for detection of screw loosening was 7.3±4.1 (2-15) months. The rate of S1 screw loosening according to the number of fusion levels were 2.0%, 26.8%, 50.0%, and 50.0% in 1, 2, 3, and 4 levels fusion groups. The rate of S1 screw loosening showed a significantly higher rate in 3 or 4 levels fusion comparing to 1 level fusion (p<0.05) (Table 2).
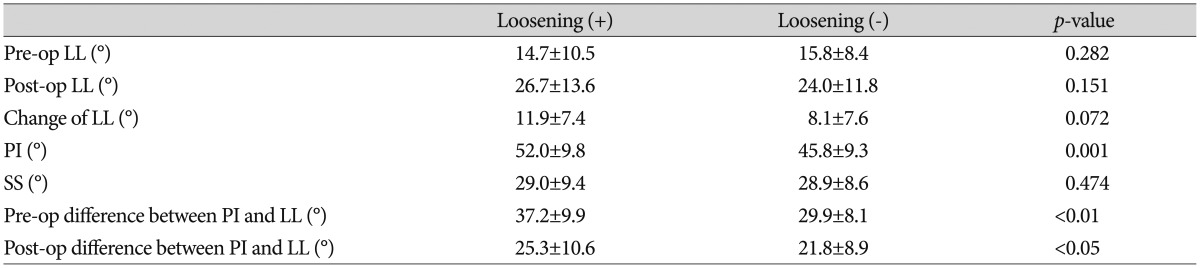
Mean pre- and postoperative LL values were 14.7±10.5° and 26.7±13.6° in the SL group, and 15.8±8.4° and 24.0±11.8° in the non SL group. Sacral slope angles were 29.0±9.4° and 28.9±8.6° in the loosening and non-loosening groups, respectively. The sacral slope, pre- and postoperative LL angles were not different between the two groups (Table 3). The change of LL angle after surgery was greater in the loosening group (11.9±7.4°) than and non-loosening group (8.1±7.6°), but there was no statistical significance (Table 3). Mean PI was significantly higher in the loosening group (52.0±9.8°) than those of non-loosening group (45.8±9.3°) (p<0.01) (Table 3). Pre- and postoperative PI-LL's were significantly greater, 37.2±9.9° (p<0.01) and 25.3±10.6° (p<0.05), in loosening group, comparing to those of non-loosening group, 29.9±8.1° and 21.8±8.9° (Table 3). The intraobserver ICC's were 0.97, 0.90, and 0.96 in LL, PI, and SS, respectively. The interobserver ICC's were 0.93, 0.84, and 0.94 in LL, PI, and SS, respectively.
Table 3. Comparison of spinopelvic parameters between the loosening and non-loosening groups.
LL : lumbar lordosis, PI : pelvic incidence, SS : sacral slope, change of LL : amount of LL corrected by surgery
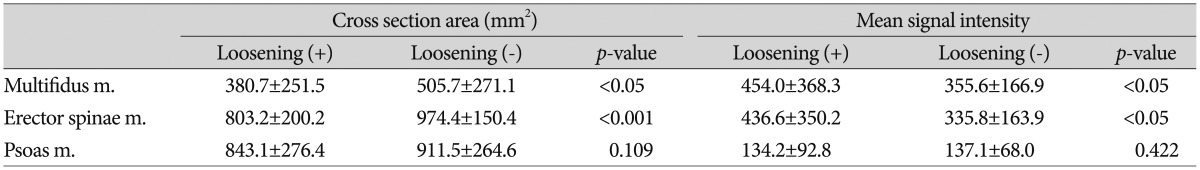
Mean CSA's of multifidus muscle, erector spinae muscle, and psoas muscle, checked at L5-S1 disc level, were 380.7±251.5 mm2, 803.2±200.2 mm2, and 843.1±276.4 mm2 in loosening group, and 905.7±271.1 mm2, 674.4±150.4 mm2, and 911.5±264.6 mm2 in non-loosening group (Table 4). CSA's of multifidus muscle (p<0.05) and erector spinae muscle (p<0.001) were significantly smaller in loosening group than non-loosening group. Mean signal intensity values on T2 MRI of the respective muscles were 454.0±368.3, 436.6±350.2, and 134.2±92.8 in loosening group, and 355.6±166.9, 335.8±163.9, and 137.1±68.0 in non-loosening group. The muscular signal intensities of multifidus and erector spinae muscles were significantly higher in loosening group (p<0.05) (Table 4). But psoas muscle didn't show any difference in both CSA and signal intensity between the two groups. There was no significant correlation between significant spinopelvic parameters (PI and postoperative PI-LL) and the degenerative changes (CSA and mean signal intensity) of paraspinal muscles according to Pearson correlation coefficient (p>0.05) (Table 5). The intraobserver ICC's were 0.90, 0.93, and 0.97 in CSA's of MF, ES, and PS. The intraobserver ICC's were 0.95, 0.97, and 0.98 in mean signal intensity values of MF, ES, and PS. The interobserver ICC's were 0.85, 0.85, and 0.90 in CSA's of MF, ES, and PS. The interobserver ICC's were 0.91, 0.90, and 0.94 in mean signal intensity values of MF, ES, and PS.
Table 4. Comparison of the muscular factors between the loosening and non-loosening groups.
Table 5. Pearson correlation coefficients between spinopelvic parameters and the degenerative changes of paraspinal muscles.
PI-LL : difference between pelvic incidence and lumbar lordosis, r : Pearson correlation coefficients
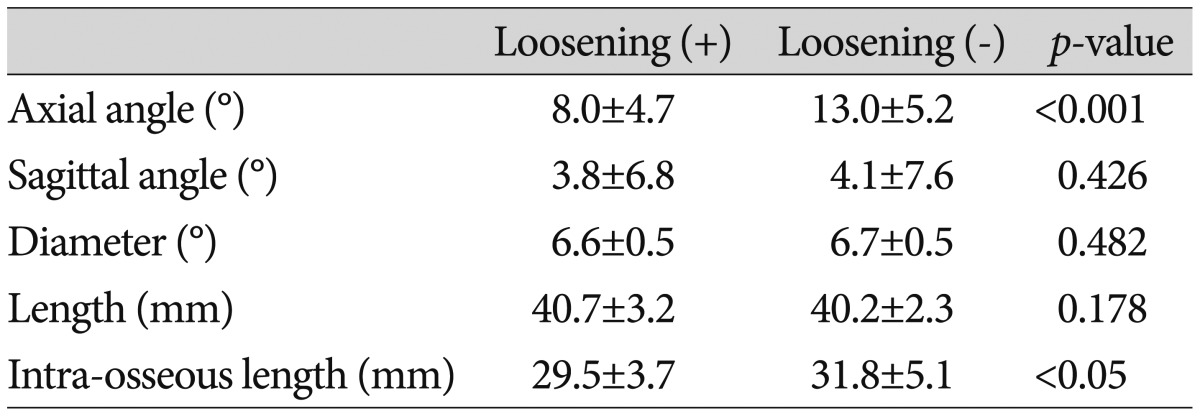
The mean axial angle of S1 screw was 8.0±4.7° in loosening group, which was significantly lower than those of non-loosening group, 13.0±5.2° (p<0.001) (Table 6). Other screw related factors including sagittal angle, diameter, and length of S1 screw were similar between the two groups. Even though the whole length of S1 screw was not so meaningful, intraosseous length of S1 screw was significantly longer, 31.8±5.1 mm, in non-loosening group than loosening group, 29.5±3.7 mm (p<0.05) (Table 6). The intraobserver ICC's were 0.98, 0.95, and 0.90 in axial angle, sagittal angle, and intra-osseous length of S1 screw, respectively. The interobserver ICC's were 0.90, 0.88, and 0.85 in axial angle, sagittal angle, and intra-osseous length of S1 screw, respectively.
Table 6. Comparison of S1 screw profile between the loosening and non-loosening groups.
DISCUSSION
Among the patients underwent spinal fusion operation including S1, the loosening rate of S1 screw had been reported about 15.6-46.5%10,16,34). Screw loosening rate of lumbar spine was reported to be about 10-20%, which is, in general, lower than S1 screw loosening rate45). There is a tendency of decreased fusion rate at lumbosacral level due to increased pseudoarthrosis4,35). In our study, S1 screw loosening occurred in 24.4%, which was relatively high level comparable with other reports.
This is because the sacrum is composed primarily of cancellous bone, and receives a greater mechanical load than other segments28). The anatomical characteristics of the S1 pedicle, a larger diameter and shorter length than lumbar pedicles, indicate that S1 screw loosening occurs more frequently due to the structural weakness of the S1 body and pedicle31). Other factors that reportedly contribute to sacral screw failure include inappropriate direction or depth of screw insertion, and large cantilever bending moments loaded by long level instrumentation2,34,43). In relation to the fusion length there was no specified criteria for the use of S1 protective procedures according to the number of fusion levels. Our data showed 3 or more levels (L3-S1 or L2-S1) significantly increased the risk of the S1 screw loosening, which seemed to suggest the need for use of S1 protective procedures in the cases with 3 or more fusion levels.
There have been various techniques for the protection of S1 screw including sacropelvic fixation1,30,37,44,48), bicortical or tricortical insertion of S1 screw27,29), and cement augmentation33,36). We also used these techniques as preventive methods in selected patients with high risk of screw loosening, osteoporosis or old age, which were proved as risk factors for the S1 screw loosening, who were not enrolled in this study. Although the techniques must have a strong preventive effect for S1 screw loosening, we could not analyze their effects because of their selective use for high risk patients.
Differences in fusion methods also appear to influence screw loosening. Some reports indicated TLIF showed a lower screw loosening rate than posterior lumbar interbody fusion (PLIF)14,47). Xu et al.46) reported the mechanical difference between TLIF and PLIF by proving the difference in screw stress, which might be related with increased possibility of S1 screw loosening. However, we could not find a study directly reporting S1 screw loosening after TLIF operation. Considering the different biomechanical effect on pedicle screw between TLIF and PLIF, a separate study on risk factors of S1 screw loosening for both types of fusion seems to be necessary. In this study, we selected patients underwent TLIF for investigation of S1 screw loosening.
The importance of surgical recovery of lumbar lordosis has been reported in many papers, and insufficient lumbar lordotic angle seem to be associated with lower back pain and functional loss20,22,23). During spinal fusion, it is more important to correct lumbar lordotic angle within its physiological range, usually greater than PI16,40). Accordingly, larger preoperative PI demands greater lumbar lordotic angle during surgery40). Decreased lordotic angle can cause increased load to the adjacent segments7,12). According to our data, the preoperative PI, difference between PI and lumbar lordotic angle was significantly greater in the screw loosening group comparing to the non-loosening group. When the patients had high preoperative PI-LL difference, 37.2±9.9°, the risk S1 screw loosening increased significantly. This insufficient correction of a lordotic angle, still high postoperative PI-LL difference, 25.3±10.6°, seems to increase the risk of S1 screw loosening due to more bending moment and mechanical stress to the screw. Both pre- and postoperative PI-LL's seem to be important risk factors. But we think the postoperative PI-LL is a more important factor because it can be reduced by surgery.
Paraspinal muscles play an important role in maintaining segmental, regional, and global stability25). The indicators of degenerative change in the paraspinal muscles include cross-sectional area and fatty changes. Degeneration in the cross-sectional area appears as muscle atrophy15,26); fatty changes in muscles are also a form of degeneration, which is closely associated with functional decrease11,26,32,41). Lee et al.25) indicated that the fat content of the paraspinal muscles was the factor with the greatest influence on the result of lumbosacral fusion operation. According to our results, smaller cross-sectional areas and greater fatty changes in multifidus and erector spinae muscles may affect clinical result of fusion operation by way of increasing S1 screw loosening.
The spinopelvic parameters with significant effect on S1 screw loosening, PI and postoperative PI-LL, were selected to test correlation with muscular degenerative indices, CSA and mean signal intensity. But, there was no significant correlation between the spinopelvic parameters and degenerative indices of paraspinal muscles. This suggests the two types of risk factors, spinopelvic parameters and muscular degeneration, may have their own effects on S1 screw loosening and can have synergistic effect. We didn't analyze their synergistic effect, it seems to need further study investigating their independency or synergistic effect on the development of S1 screw loosening.
Screw angulation strengthens the resistance to straight pullout. Many studies have shown that two angulated screws have greater resistance to pullout than parallel ones3,38,42,49). Krag et al.21) performed biomechanical testing on pedicle screws, and indicated that angulated screws are stronger due to a 'toe nail' effect. Our results also confirmed that the S1 screw axial angle, not the sagittal angle, was important to protect S1 screw. In addition, the long intraosseous length of screw, not the diameter or whole length of screw, was noted to reduce the risk of S1 screw loosening significantly.
A retrospective study with a small number of patients was a limitation of our study. Although a study on sacropelvic parameters was conducted, a direct relationship with sagittal balance was not fully investigated because our study didn't enroll any patient with sagittal imbalance. The data of cross sectional area and fatty degeneration of paraspinal muscles could not explain actual muscle function. Moreover, our data were based on radiological findings, which did not reflect clinical outcomes directly. Therefore, additional studies related to these subjects are deemed to be necessary in the future.
CONCLUSION
Most of the risk factors for S1 screw loosening, including age, osteoporosis, number of fusion levels, toe nail effect of screw, were proved to be related with S1 screw loosening, which were comparable with other reports. But we focused on the additional two types of possible risk factors, spinopelvic parameters and back muscle degeneration. The high PI and high PI-LL were proved to be significant risk factors, suggesting the importance of making sagittal balance during surgery. Back muscle weakness represented by CSA and fat degeneration was also proved to be a risk factor, which shows the importance of preoperative evaluation for paraspinal muscles and postoperative back muscle rehabilitation program.
References
- 1.Allen BL, Jr, Ferguson RL. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine (Phila Pa 1976) 1984;9:388–394. doi: 10.1097/00007632-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Balderston RA, Winter RB, Moe JH, Bradford DS, Lonstein JE. Fusion to the sacrum for nonparalytic scoliosis in the adult. Spine (Phila Pa 1976) 1986;11:824–829. doi: 10.1097/00007632-198610000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Barber JW, Boden SD, Ganey T, Hutton WC. Biomechanical study of lumbar pedicle screws : does convergence affect axial pullout strength? J Spinal Disord. 1998;11:215–220. [PubMed] [Google Scholar]
- 4.Bernhardt M, Swartz DE, Clothiaux PL, Crowell RR, White AA., 3rd Posterolateral lumbar and lumbosacral fusion with and without pedicle screw internal fixation. Clin Orthop Relat Res. 1992;(284):109–115. [PubMed] [Google Scholar]
- 5.Cho W, Mason JR, Smith JS, Shimer AL, Wilson AS, Shaffrey CI, et al. Failure of lumbopelvic fixation after long construct fusions in patients with adult spinal deformity : clinical and radiographic risk factors : clinical article. J Neurosurg Spine. 2013;19:445–453. doi: 10.3171/2013.6.SPINE121129. [DOI] [PubMed] [Google Scholar]
- 6.Dakhil-Jerew F, Jadeja H, Cohen A, Shepperd JA. Inter-observer reliability of detecting Dynesys pedicle screw using plain X-rays : a study on 50 post-operative patients. Eur Spine J. 2009;18:1486–1493. doi: 10.1007/s00586-009-1071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dekutoski MB, Schendel MJ, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976) 1994;19:1745–1751. doi: 10.1097/00007632-199408000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Devlin VJ, Boachie-Adjei O, Bradford DS, Ogilvie JW, Transfeldt EE. Treatment of adult spinal deformity with fusion to the sacrum using CD instrumentation. J Spinal Disord. 1991;4:1–14. [PubMed] [Google Scholar]
- 9.Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity : luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976) 2002;27:776–786. doi: 10.1097/00007632-200204010-00017. [DOI] [PubMed] [Google Scholar]
- 10.Finger T, Bayerl S, Onken J, Czabanka M, Woitzik J, Vajkoczy P. Sacropelvic fixation versus fusion to the sacrum for spondylodesis in multilevel degenerative spine disease. Eur Spine J. 2014;23:1013–1020. doi: 10.1007/s00586-014-3165-6. [DOI] [PubMed] [Google Scholar]
- 11.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;(304):78–83. [PubMed] [Google Scholar]
- 12.Herkowitz HN. Lumbar spinal stenosis : indications for arthrodesis and spinal instrumentation. Instr Course Lect. 1994;43:425–433. [PubMed] [Google Scholar]
- 13.Huang Y, Majumdar S, Genant HK, Chan WP, Sharma KR, Yu P, et al. Quantitative MR relaxometry study of muscle composition and function in Duchenne muscular dystrophy. J Magn Reson Imaging. 1994;4:59–64. doi: 10.1002/jmri.1880040113. [DOI] [PubMed] [Google Scholar]
- 14.Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976) 2001;26:567–571. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 15.Jorgensen MJ, Marras WS, Gupta P. Cross-sectional area of the lumbar back muscles as a function of torso flexion. Clin Biomech (Bristol, Avon) 2003;18:280–286. doi: 10.1016/s0268-0033(03)00027-5. [DOI] [PubMed] [Google Scholar]
- 16.Kim EH, Kim HJ. Long segment fusion to L5 vertebra and sacral vertebra in degenerative lumbar spine. J Korean Soc Spine Surg. 2002;9:216–222. [Google Scholar]
- 17.Kim HK, Laor T, Horn PS, Racadio JM, Wong B, Dardzinski BJ. T2 mapping in Duchenne muscular dystrophy : distribution of disease activity and correlation with clinical assessments. Radiology. 2010;255:899–908. doi: 10.1148/radiol.10091547. [DOI] [PubMed] [Google Scholar]
- 18.Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC, 2nd, Rinella AS. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am. 2006;88:721–728. doi: 10.2106/JBJS.E.00550. [DOI] [PubMed] [Google Scholar]
- 19.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum : prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976) 2006;31:2329–2336. doi: 10.1097/01.brs.0000238968.82799.d9. [DOI] [PubMed] [Google Scholar]
- 20.Kostuik JP, Hall BB. Spinal fusions to the sacrum in adults with scoliosis. Spine (Phila Pa 1976) 1983;8:489–500. doi: 10.1097/00007632-198307000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Krag MH, Beynnon BD, Pope MH, Frymoyer JW, Haugh LD, Weaver DL. An internal fixator for posterior application to short segments of the thoracic, lumbar, or lumbosacral spine. Design and testing. Clin Orthop Relat Res. 1986;(203):75–98. [PubMed] [Google Scholar]
- 22.La Grone MO. Loss of lumbar lordosis. A complication of spinal fusion for scoliosis. Orthop Clin North Am. 1988;19:383–393. [PubMed] [Google Scholar]
- 23.Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B, et al. Sagittal alignment in lumbosacral fusion : relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lebwohl NH, Cunningham BW, Dmitriev A, Shimamoto N, Gooch L, Devlin V, et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine (Phila Pa 1976) 2002;27:2312–2320. doi: 10.1097/00007632-200211010-00003. [DOI] [PubMed] [Google Scholar]
- 25.Lee CS, Chung SS, Choi SW, Yu JW, Sohn MS. Critical length of fusion requiring additional fixation to prevent nonunion of the lumbosacral junction. Spine (Phila Pa 1976) 2010;35:E206–E211. doi: 10.1097/BRS.0b013e3181bfa518. [DOI] [PubMed] [Google Scholar]
- 26.Lee JC, Cha JG, Kim Y, Kim YI, Shin BJ. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis : comparison with the normal controls. Spine (Phila Pa 1976) 2008;33:318–325. doi: 10.1097/BRS.0b013e318162458f. [DOI] [PubMed] [Google Scholar]
- 27.Lehman RA, Jr, Kuklo TR, Belmont PJ, Jr, Andersen RC, Polly DW., Jr Advantage of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation : a biomechanical analysis. Spine (Phila Pa 1976) 2002;27:806–811. doi: 10.1097/00007632-200204150-00006. [DOI] [PubMed] [Google Scholar]
- 28.Leong JC, Lu WW, Zheng Y, Zhu Q, Zhong S. Comparison of the strengths of lumbosacral fixation achieved with techniques using one and two triangulated sacral screws. Spine (Phila Pa 1976) 1998;23:2289–2294. doi: 10.1097/00007632-199811010-00008. [DOI] [PubMed] [Google Scholar]
- 29.Luk KD, Chen L, Lu WW. A stronger bicortical sacral pedicle screw fixation through the s1 endplate : an in vitro cyclic loading and pull-out force evaluation. Spine (Phila Pa 1976) 2005;30:525–529. doi: 10.1097/01.brs.0000154649.55589.bf. [DOI] [PubMed] [Google Scholar]
- 30.McCarthy RE, Bruffett WL, McCullough FL. S rod fixation to the sacrum in patients with neuromuscular spinal deformities. Clin Orthop Relat Res. 1999;(364):26–31. doi: 10.1097/00003086-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 31.McLachlin SD, Al Saleh K, Gurr KR, Bailey SI, Bailey CS, Dunning CE. Comparative assessment of sacral screw loosening augmented with PMMA versus a calcium triglyceride bone cement. Spine (Phila Pa 1976) 2011;36:E699–E704. doi: 10.1097/BRS.0b013e3181fb73ea. [DOI] [PubMed] [Google Scholar]
- 32.Mengiardi B, Schmid MR, Boos N, Pfirrmann CW, Brunner F, Elfering A, et al. Fat content of lumbar paraspinal muscles in patients with chronic low back pain and in asymptomatic volunteers : quantification with MR spectroscopy. Radiology. 2006;240:786–792. doi: 10.1148/radiol.2403050820. [DOI] [PubMed] [Google Scholar]
- 33.Moore DC, Maitra RS, Farjo LA, Graziano GP, Goldstein SA. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine (Phila Pa 1976) 1997;22:1696–1705. doi: 10.1097/00007632-199708010-00003. [DOI] [PubMed] [Google Scholar]
- 34.Pihlajämaki H, Myllynen P, Böstman O. Complications of transpedicular lumbosacral fixation for non-traumatic disorders. J Bone Joint Surg Br. 1997;79:183–189. doi: 10.1302/0301-620x.79b2.7224. [DOI] [PubMed] [Google Scholar]
- 35.Rechtine GR, Sutterlin CE, Wood GW, Boyd RJ, Mansfield FL. The efficacy of pedicle screw/plate fixation on lumbar/lumbosacral autogenous bone graft fusion in adult patients with degenerative spondylolisthesis. J Spinal Disord. 1996;9:382–391. [PubMed] [Google Scholar]
- 36.Renner SM, Lim TH, Kim WJ, Katolik L, An HS, Andersson GB. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine (Phila Pa 1976) 2004;29:E212–E216. doi: 10.1097/00007632-200406010-00020. [DOI] [PubMed] [Google Scholar]
- 37.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;(203):7–17. [PubMed] [Google Scholar]
- 38.Ruland CM, McAfee PC, Warden KE, Cunningham BW. Triangulation of pedicular instrumentation. A biomechanical analysis. Spine (Phila Pa 1976) 1991;16(6 Suppl):S270–S276. doi: 10.1097/00007632-199106001-00019. [DOI] [PubMed] [Google Scholar]
- 39.Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Joint Surg Br. 2004;86:457–461. doi: 10.1302/0301-620x.86b3.14323. [DOI] [PubMed] [Google Scholar]
- 40.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 41.Seo JB, Yoo JS, Jang HS, Kim JS. Correlation of clinical symptoms and function with fatty degeneration of infraspinatus in rotator cuff tear. Knee Surg Sports Traumatol Arthrosc. 2015;23:1481–1488. doi: 10.1007/s00167-014-2857-0. [DOI] [PubMed] [Google Scholar]
- 42.Skinner R, Maybee J, Transfeldt E, Venter R, Chalmers W. Experimental pullout testing and comparison of variables in transpedicular screw fixation. A biomechanical study. Spine (Phila Pa 1976) 1990;15:195–201. doi: 10.1097/00007632-199003000-00007. [DOI] [PubMed] [Google Scholar]
- 43.Soini J, Laine T, Pohjolainen T, Hurri H, Alaranta H. Spondylodesis augmented by transpedicular fixation in the treatment of olisthetic and degenerative conditions of the lumbar spine. Clin Orthop Relat Res. 1993;(297):111–116. [PubMed] [Google Scholar]
- 44.Winter RB, Pinto WC. Pelvic obliquity. Its causes and its treatment. Spine (Phila Pa 1976) 1986;11:225–234. [PubMed] [Google Scholar]
- 45.Wu JC, Huang WC, Tsai HW, Ko CC, Wu CL, Tu TH, et al. Pedicle screw loosening in dynamic stabilization : incidence, risk, and outcome in 126 patients. Neurosurg Focus. 2011;31:E9. doi: 10.3171/2011.7.FOCUS11125. [DOI] [PubMed] [Google Scholar]
- 46.Xu H, Tang H, Guan X, Jiang F, Xu N, Ju W, et al. Biomechanical comparison of posterior lumbar interbody fusion and transforaminal lumbar interbody fusion by finite element analysis. Neurosurgery. 2013;72(1 Suppl Operative):21–26. doi: 10.1227/NEU.0b013e3182742a69. [DOI] [PubMed] [Google Scholar]
- 47.Yan DL, Pei FX, Li J, Soo CL. Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J. 2008;17:1311–1316. doi: 10.1007/s00586-008-0739-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zahi R, Vialle R, Abelin K, Mary P, Khouri N, Damsin JP. Spinopelvic fixation with iliosacral screws in neuromuscular spinal deformities : results in a prospective cohort of 62 patients. Childs Nerv Syst. 2010;26:81–86. doi: 10.1007/s00381-009-0966-8. [DOI] [PubMed] [Google Scholar]
- 49.Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;(203):99–112. [PubMed] [Google Scholar]