Abstract
Purpose:
The purpose of this study is to develop methods to identify glaucoma by examining the optic nerve head (ONH) of donor's eyes when information on the preexisting ocular disease is unavailable.
Materials and Methods:
The ONH of the donor's eyes was evaluated under a stereomicroscope for the cup-disc ratio (CDR) and focal retinal rim thinning. The vertical diameter of the cup and disc was also measured using a precalibrated eyepiece micrometer. The suspect eyes were subjected to histological analysis to confirm the presence of specific glaucomatous changes.
Results:
A total of 202 eyes from 119 donors (68 males and 51 females, aged 42–96) were evaluated for glaucoma. Among them, 190 (94%) eyes showing vertical CDR in the of 0.0–0.6 range were considered nonglaucomatous and the remaining eyes with >0.6 as glaucoma suspect. The calculated mean CDR of the two groups (0.3 ± 0.16, 0.62 ± 0.27) was highly significant (P = 0.0003). Of 12 eyes suspected of glaucoma, 7 eyes from 5 donors showed specific glaucomatous changes by histology. The prevalence of glaucoma was 4.2% among the donors studied.
Conclusions:
A simple method of screening fresh donor eyes for selecting those with glaucoma features using CDR and histological analysis was reported. This method helps to obtain biologically active human ocular tissue for glaucoma research on gene expression, ultrastructural/proteome changes, and outflow mechanism.
Keywords: Cup-disc ratio, donor eyes, glaucoma, glaucomatous changes, histopathology
Glaucoma is the second leading cause of blindness in the world. Primary open angle glaucoma (POAG) is the most predominant form of glaucoma the world over, accounting for 74% of those affected.[1] It has been estimated that 12% of global blindness is due to glaucoma and close to 11 million people will be bilaterally blind from glaucoma by the end of this decade. Based on the reported age and gender stratified prevalence estimates of the disease from several population-based studies, it is predicted that there are approximately 11.2 million persons aged 40 years and above with glaucoma in India.[2] Most of those with the disease are undiagnosed and there exist major challenges in the detection and treatment of this potentially blinding disease. Ocular research to understand the pathophysiology of glaucoma with the evolution of better therapeutic modalities to contain progressive optic nerve damage and visual field loss is crucial to prevent blindness.
The need for acquiring human ocular tissue to understand the pathophysiology and molecular mechanism of eye disease cannot be overemphasized. The comprehension of the biological basis of glaucoma has been advanced by the study of glaucoma models and ocular tissue that allow experimentation ordinarily not possible in living humans. Such in vitro studies on ocular tissue also facilitate testing of potential treatments as a “proof of principle” prior to human clinical trials. Although animal models exist for several of the eye diseases, some of the chronic diseases such as glaucoma cannot be comprehensively studied. It is difficult to mimic or induce several of the changes in the optic nerve head (ONH) or the trabecular meshwork characteristic of prolonged elevation of intraocular pressure (IOP) as observed in humans. There is a continued need to examine well-characterized human eye tissue in the light of new information from animal studies. Owing to the unique anatomy of the macula, the aqueous outflow tract and the ONH in humans, the study of human ocular tissue is expected to be the mainstay of ophthalmic research in the foreseeable future.[3]
The most practical method of obtaining human ocular tissue for research is from eyes procured postmortem from donors. Ocular tissue for glaucoma research could be obtained if families can confirm a prior diagnosis or treatment for glaucoma in the deceased. Such information from families in India is often unavailable since it has been known from several epidemiologic studies that more than 94% of glaucoma in the community is undetected. Moreover, the families may be unaware of preexisting glaucoma in the deceased. Thus, diseased cadaveric eye tissue of potential use in eye research go unnoticed by the Eye Bank staff.
According to the data available with the Eye Bank Association of India, merely 25% of the procured donor corneas are estimated to be suitable for corneal transplantation surgeries.[4] It is imperative that to obtain tissue for purposes of research in India where fresh human cadaver eyes are available, investigators have to evolve a reliable method to diagnose optic nerve damage characteristic of glaucoma by evaluation of the cadaver eyes, especially when the history of the disease in the donor is not available.
The diagnosis of glaucoma is often very challenging for the eye care practitioner. The assessment of the ONH changes in addition to IOP measurement and visual field defects are of paramount importance in the diagnosis and management of glaucoma in the clinical setting.[5] However, the diagnosis of characteristic changes in the ONH in donor's eyes is more challenging due to optic disc pallor and edema. Therefore, the objective of this study is to develop a method to identify the donor eyes with possible glaucoma by observing ONH changes under the stereomicroscope, followed by histological confirmation. This study was also extended to calculate the optic disc morphometric parameters for the South Indian donor eyes.
Materials and Methods
Human donor eyes
Fresh human donor eyes after the removal of the cornea for transplantation or the entire globe obtained from the Eye Bank of our hospital were handled in accordance with the Declaration of Helsinki. The prior permission was obtained from the Institutional Review Board of our hospital (IRB #. RES2011002BAS) and the written consent of the donor or next of kin were also obtained.
The donor eyes were enucleated within 4 h of death (mean elapsed time between death and enucleation was 3.19 ± 1.4 h), kept at 4°C and made available within 30 h (mean elapsed time between enucleation and analysis of ONH was 20.26 ± 9.11 h) for the study.
In this study, a total of 260 donor eyes from 141 donors (age ranging from 40 to 96 years) collected during 2011 were examined. Fifty-eight eyes were not suitable for ONH evaluation since they had severe disc edema, retina folded over the ONH, retinal detachment, staphyloma and/or vitreous condensation and hence excluded from the study. Remaining 202 eyes were obtained from 68 males and 51 females (paired eyes from 83 and single eyes from 36 donors).
Dissection of donor's eyes
Upon receipt of the donor's eyes from the Eye Bank, the cornea, lens and iris were gently removed without disturbing the retina under the dissecting microscope (Nikon, Japan). The right ONHs were oriented by keeping the macula on the left side of the observer and the left ONHs with the macula on the right side to simulate the physiological position. The right and left eyes were considered as per the information received from the Eye Bank. All eyes under study were screened for HIV, hepatitis A and C and syphilis and the positive cases were excluded from the study. Utmost care was taken during handling of the donor eyes.
Stereomicroscopic evaluation of optic nerve head
The ONH of each donor's eye was evaluated under the stereomicroscope with fiber optic illumination (Leica Stereomicroscope MS5, Texas, USA) and was graded as either nonglaucomatous or glaucoma-suspect based on the following criteria:
Nonglaucomatous: The ONH with vertical cup-disc ratio (CDR) ≤0.6 with no focal retinal rim thinning
Glaucoma-suspect: The ONH with vertical CDR ≥ 0.6 with focal retinal rim thinning, localized or diffuse neural rim loss, thinning or slope, generalized, or localized retinal nerve fiber thinning or defects and characteristic peripapillary atrophy suggestive of glaucomatous optic nerve damage (GOND).
The CDR is the diameter of the cup described as a fraction of the diameter of the disc.[6] All eyes were graded by a single observer. When the prior medical history of the donors was not available we utilized the estimation of vertical CDR and associated features such as loss of neuro retinal rim, retinal nerve fiber thinning (retinal nerve fiber layer [RNFL]) or peripapillary atrophy (PPA) as a measure of initial screening for glaucoma in donor eyes. All observed ONHs were pale and presented mild to moderate disc edema, although a significant increase in CDR could still be identified. Globes with the significant optic disc or posterior pole edema with ONHs that were not assessable by the ophthalmologist were excluded from the study. The cup was seen under stereomicroscope as three dimensional depressions in the disc that is devoid of neural tissue. In a population-based study in South India, it has been suggested that vertical CDR >0.5 should arouse suspicion of glaucoma since the median vertical CDR in the normal population has been observed to be 0.3 ± 0.2.[7] Hence in this study, we used a vertical CDR of ≥0.6 associated with focal/diffuse retinal rim thinning in the superior or inferior sector of the ONH as suspect glaucoma.
The vertical cup and disc diameter were also measured by using a precalibrated eye-piece micrometer of the stereomicroscope in 127 eyes. The schematic representation showing the method to accurately measure the vertical diameter of the ONH is shown in Fig. 1. A digital camera (Nikon Coolpix 8400, Japan) was used to take two-dimensional images of each ONH for documentation purposes.
Figure 1.
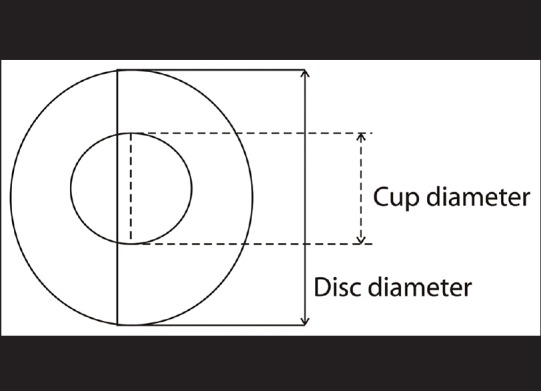
Schematic representation of optic nerve head. The vertical diameter of the optic disc and cup of donor eye was measured using a precalibrated eye piece micrometer in a stereomicroscope at ×16 magnification
Histological investigation
All the glaucoma-suspect and eight nonglaucomatous eyes were further evaluated histologically by a masked observer. Following fixation of eyes in a 10% buffered formaldehyde solution periodic acid-Schiff–eosin stained histological sections (8 µm thickness) were prepared using a standard protocol. The sagittal sections along with the optic nerve were analyzed for glaucomatous changes based on the following histological features: (a) Presence of peripapillary RNFL thinning, (b) axonal loss and (c) displacement and thinning of lamina cribrosa (LC). The RNFL thickness was measured in both glaucomatous and nonglaucomatous eyes to determine the extent of glaucomatous damage in the neural retina. The axonal loss was graded based on the extent of loss of optic nerve axons in ONH. The degree of ONH excavation was graded based on the central thickness of the LC in a representative histological section.
Results
Evaluation of cup and disc diameter
In this study, 202 eyes from 119 donors (68 males and 51 females with age ranging from 42 to 96 years) were examined. The evaluated ONHs were categorized as either nonglaucomatous or glaucoma-suspect based on the observed CDR [Fig. 2]. A total of 190 eyes out of 202 were found to have CDR ranging from 0.0 to 0.6 without focal neuro retinal rim thinning and hence they were graded as nonglaucomatous and the remaining eyes with more than 0.6 CDR with neural rim width changes as glaucoma-suspect. The mean CDR of nonglaucomatous eyes did not vary significantly between different age groups [Table 1]. The stereoscopic image of ONH of the nonglaucomatous eyes is given in Fig. 3. Among them, 28 paired eyes were found to have the same CDR in both eyes and 53 paired eyes showed different CDRs with no significant difference (P = 0.202, Wilcoxon signed-rank test). Among 202 eyes, 12 eyes were considered as glaucoma-suspect [Figs. 2, 4a and b] and therefore, further evaluated by histology.
Figure 2.
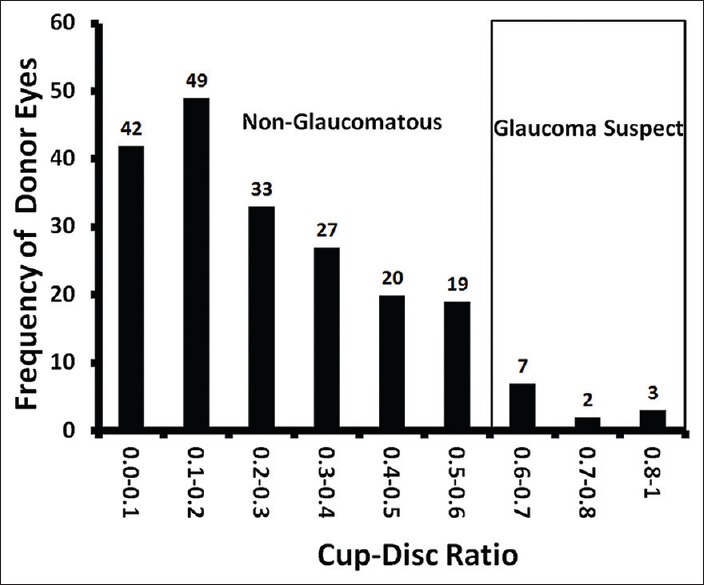
Histogram showing the distribution of cup-disc ratio of donor eyes. The optic nerve head of the donor eyes was classified either nonglaucomatous or glaucoma suspect based on cup-disc ratio. The diameters of the cup and the disc were evaluated under the stereomicroscope with fiber optic epi-illumination (Leica Stereomicroscope MS5, Texas, USA) at ×16. The distribution of cup-disc ratio for the total of 202 eyes is shown in this figure
Table 1.
Age-wise distribution of nonglaucomatous donor eyes
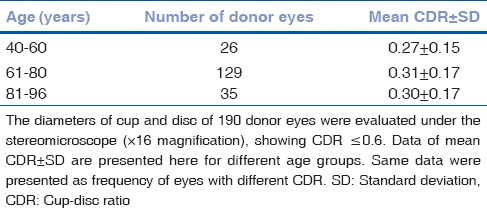
Figure 3.
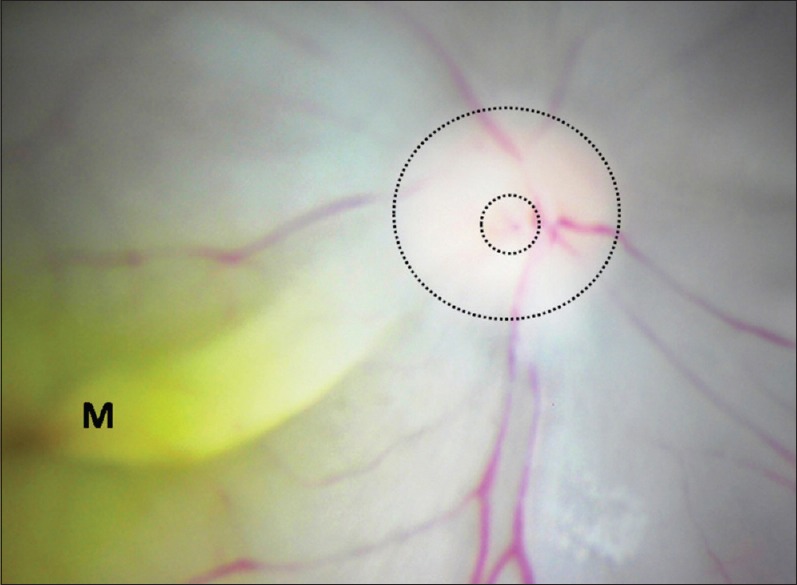
Image of the optic nerve head of nonglaucomatous donor eye. The image showing the right optic nerve head of the nonglaucomatous eye of a 63-year-old male donor with cup-disc ratio 0.2, graded under the stereomicroscope (×16). The margin of the optic disc and cup is shown as dotted circles. The glaucoma suggestive features such as focal retinal rim thinning, parapapillary atrophy and wide cupping are absent in this optic nerve head. M – Macula
Figure 4.
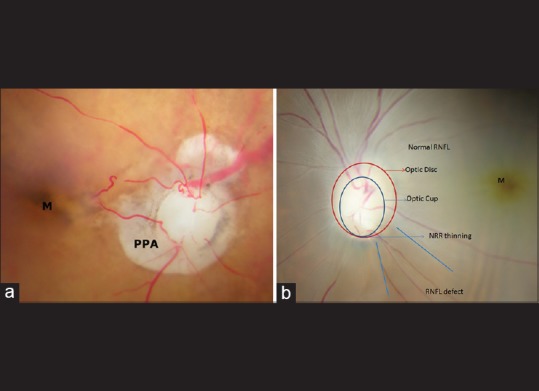
(a) Optic nerve head of donor eye with glaucoma suspect. The image showing the right optic nerve head of the glaucoma suspect donor eye of a 96-year-old female with cup-disc ratio 0.9 (serial number 3 in Table 3). The parapapillary atrophy (PPA) suggestive of glaucoma is seen around the optic disc (×16). (b) Optic nerve head of donor eye with glaucoma suspect. The image showing the left optic nerve head of the glaucoma suspect donor eye of a 75-year-old male with cup-disc ratio 0.6 (serial number 9 in [Table 3]). The retinal rim thinning and retinal nerve fiber layer defect suggestive of glaucoma are seen in the stereoscopic fundus image (×16)
Measurement of cup and disc diameter
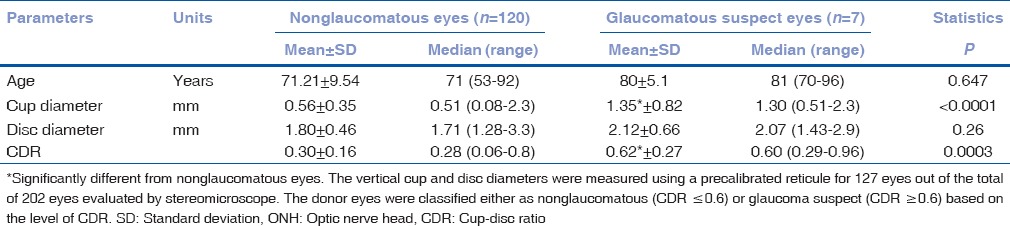
The ONH parameters were also measured accurately as described in Fig. 1 for 127 out of 202 eyes. The results are summarized in Table 2. Among them, paired eyes were from 50 and single eyes from 23 donors (40 males and 33 females). The mean vertical CDR of nonglaucomatous eyes and the glaucoma-suspect eyes was found to be 0.30 ± 0.16 and 0.62 ± 0.27 respectively and significantly different (P = 0.0003; Table 2). The mean optic cup diameter of glaucoma suspect eyes was found to be 2.4 higher than that of nonglaucomatous eyes [Table 2]. The mean vertical optic disc diameter between nonglaucomatous eyes (1.8 ± 0.46 mm) and glaucomatous eyes (2.12 ± 0.66 mm) was not significantly different (P = 0.26, Table 2). Further, the observed [Table 1] and calculated [Table 2] mean CDR for nonglaucomatous eyes was found to be 0.30 ± 0.17 and 0.30 ± 0.16 respectively and did not vary significantly.
Table 2.
ONH parameters of nonglaucomatous and glaucoma suspect donor eyes
Optic nerve head parameters of nonglaucomatous eyes by gender
The ONH parameters were calculated for 40 male (mean age 70.3 ± 9.8 years) and 33 female (mean age 72.2 ± 9.1 years) donors with nonglaucomatous eyes. The female donor eyes showed a mean vertical CDR of 0.32 ± 0.2 which was marginally high as compared to that of male donor eyes (0.25 ± 0.16). The mean optic disc diameters of male and female were 1.79 ± 0.46 and 1.82 ± 0.47 mm, and the mean optic cup diameter was 0.55 ± 0.37mm and 0.63 ± 0.44 mm respectively. The females had marginally higher values for these parameters compared to male donors though they were of the same age group.
Histological confirmation
The ONH histological features of nonglaucomatous eyes were confirmed as normal as evidenced by the absence of RNFL thinning, axonal loss, and ONH excavation [Fig. 5]. Among 12 glaucoma-suspect eyes (2 excluded due to the short optic nerve), 7 were confirmed as glaucomatous based on the criteria described in Table 3. The histology of a representative glaucomatous eye is shown in Fig. 6. The mean (±standard deviation) RNFL thickness and LC central thickness of glaucomatous eyes were 36.9 ± 13.7 µm and 54.7 ± 11.9 µm [Table 3] respectively. Both were significantly reduced (P > 0.0001) in glaucomatous as compared to nonglaucomatous eyes (RNFL thickness 259.9 ± 48.6 µm and LC central thickness 271 ± 74.8 µm). The remaining three eyes did not show any characteristic histological features of glaucoma though their CDR was 0.6–0.7 and hence graded as nonglaucomatous eyes.
Figure 5.
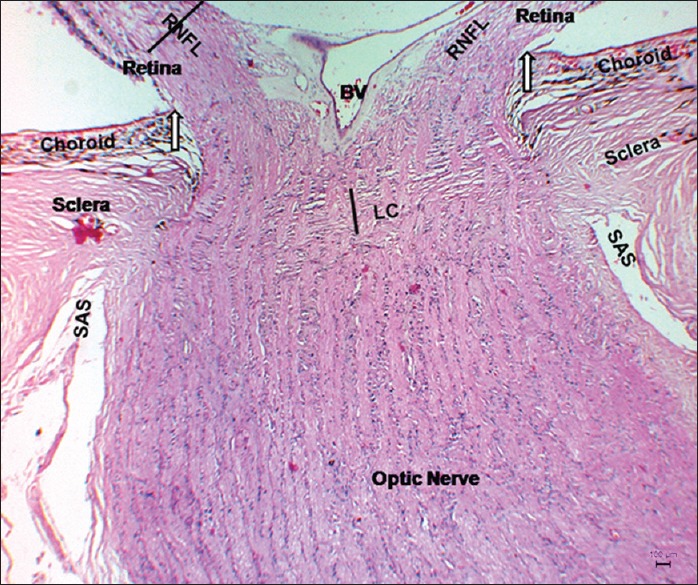
Micrograph of sagittal section of optic nerve head of nonglaucomatous eye. The median sagittal section of a nonglaucomatous optic nerve head showing the absence of RNFL thinning, LC displacement, optic nerve head cupping and axonal loss. The vertical line represents the central thickness of LC. White arrow indicates the end of Bruch's membrane. Note: The RNFL and LC central thickness were 201.9 µm and 259.5 µm respectively. BV: Blood vessel; LC: Lamina cribrosa; SAS: Sub-arachnoids’ space, RNFL: Retinal nerve fiber layer (periodic Schiff-eosin)
Table 3.
ONH features of glaucoma suspect donor eyes
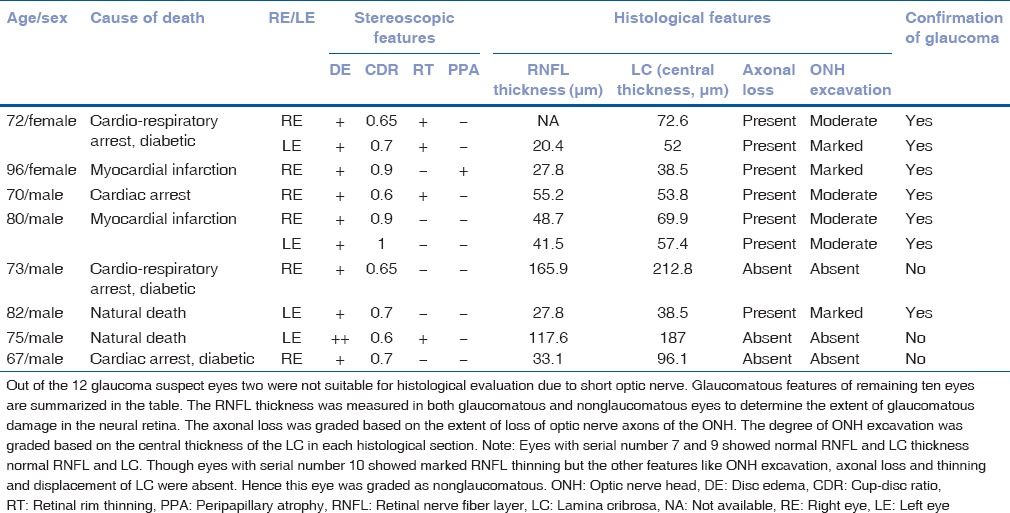
Figure 6.
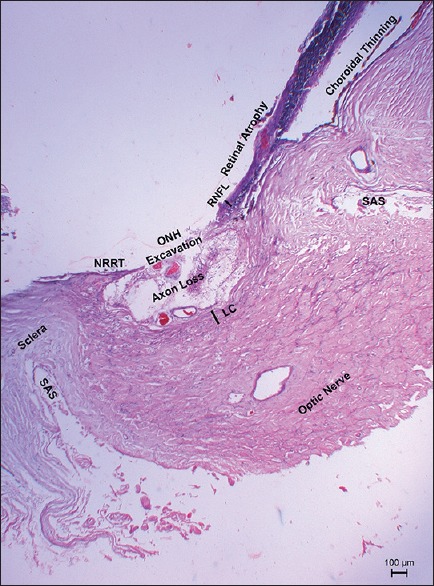
Micrograph of sagittal section of optic nerve head of glaucomatous eye. The median sagittal section of a glaucomatous optic nerve head showing thinning of RNFL, LC, deep excavation of optic nerve head and axonal loss. In addition, severe choroidal thinning, marked neural retinal rim thinning and retinal atrophy were noted. The vertical line represents the central thickness of LC. Note: The RNFL and LC central thickness were 27.8 µm and 38.5 µm respectively. Both thicknesses were reduced significantly as compared to nonglaucomatous eye. LC: Lamina cribrosa; NRRT: Neural rim retinal thinning; SAS: Sub-Arachnid's space; RNFL: Retinal nerve fiber layer (periodic Schiff-eosin staining)
Discussion
The CDR measurement in postmortem eyes has already been used as a means of differentiating normal from glaucomatous eyes in spite of the presence of postmortem changes (swelling) in the ONH.[8,9] Clinical estimation of CDR has been found to correlate well with that in cadaver eyes.[10] Varma et al. have demonstrated glaucomatous ONH damage in cadaver eyes using a reliable histological evaluation of RNFL ONH and retinal architecture in cadaver eyes. In this study, the eyes were considered normal based on the absence of a clinical history of glaucoma, normal retina and ONH on light microscopic examination.[11]
Frenkel et al. described the following histological features discriminating glaucoma from normal eyes based on the study of healthy and glaucomatous donor eyes and animal models: Ganglion cell body counts, optic nerve axonal counts, ONH morphometry, RNFL thickness, and RNFL axonal counts.[12] Although the RNFL axonal count is considered to be the gold standard to discriminate glaucoma from normal donor eyes (unaffected by postmortem and fixation artifacts), we relied on study of optic nerve morphometry and histological confirmation by RNFL thinning to detect glaucoma since such a method proved to be relatively simple and practicable.
RNFL was significantly thinner in glaucomatous eyes (40 ± 18 µm) than that of normal eyes (215 ± 70 mm).[13] Thinner RNFL in human eyes hence can be used as a histological surrogate for optic nerve damage to confirm glaucoma. A direct correlation has also been found between CDR estimate and RNFL thickness in experimental glaucoma models.[14] Based on these observations, we have proposed a method to distinguish glaucomatous from nonglaucomatous donor eyes in the absence of prior clinical history. Initial evaluation of the posterior pole of donor's eyes by an experienced glaucoma specialist identified glaucoma suspect eyes based on a CDR estimate of 0.6 or higher, associated with neural rim thinning. Subsequently, histological confirmation of RNFL thinning confirmed the presence of glaucoma.
Our finding on the mean CDR in nonglaucomatous eyes (0.30 ± 0.16, Figure 2) and in glaucoma suspect eyes (0.62 ± 0.27) was comparable to the observed CDR in normal and in those with definitive glaucoma in South Indian population.[7,15,16] Moreover, we have demonstrated that the mean vertical CDR (0.78 ± 0.15) [Table 3] of donor eyes with confirmed glaucoma features were significantly higher (P = 0.003) than that of nonglaucomatous eyes [Fig. 2].
Three eyes suspected of glaucoma based on ONH evaluation failed to reveal any histological features suggestive of glaucoma [Table 3]. Therefore, confirmation by histopathology is important, especially when the donor history was unknown. Increased CDR may also be due to causes other than glaucoma such as ischemic optic neuropathies, compressive optic neuropathies, disc colobomas and traumatic optic neuropathy or disc changes following hypotensive shock. None of these conditions are, however, characterized by asymmetric thinning of the neuroretinal rim of the optic disc as in glaucoma. Moreover, all donor eyes suspected of glaucoma based on ONH examination and confirmed as glaucoma did not show hemorrhage, ischemic necrosis, infarcts, thrombosis inside vessels, inflammatory cell or macrophage infiltration, features which help to differentiate GOND from ischemic optic neuropathies as described by Knox et al.[17] Thinner RNFL found in glaucoma suspected eyes in the present study (36.9 ± 13.7 µm) correlates well with the findings of Dichtl et al. and is evidence in support of GOND in cadaver eyes.
It is possible that this method of identifying glaucoma in the donor eyes could have missed early glaucomatous damage in some donors owing to difficulty in estimation of CDR and would have identified only those eyes with significant glaucomatous cupping. But the objective of this study was to identify eyes with glaucoma for obtaining ocular tissue for research and not determining the prevalence/existence of glaucomatous damage in the donor's eyes. The method of identification of glaucomatous eyes in the present study is designed for eyes with a wide cup in the large disc. Other procedure may have to be designed for eyes with the smaller disc. We were unable to classify the type of a POAG or primary angle closure glaucoma (PACG) since histological examination of the angle of the anterior chamber had not been performed. A careful stereomicroscopic dissection and histological evaluation of the anterior segment of donor's eyes would allow further classification of glaucoma into POAG and PACG.
The major strength of the current study is to have utilized a large cohort of freshly obtained Indian donor eyes without ocular disease history. More recently, it was possible for Goldhagen et al. to identify typical glaucomatous pathologic changes on the basis of optic nerve cupping and atrophy of retinal ganglion cell layer, even though the medical history of the donor was not available.[18] In the same study, the authors have demonstrated a statistically significant increase in RhoA levels in ONH of eyes with glaucoma when compared with age-matched controls. Such a strategy could be used along with histological confirmation to distinguish glaucomatous from nonglaucomatous donor eyes so that well defined fresh human ocular tissues are available to study the molecular mechanism involved in the pathogenesis of glaucoma.
Conclusion
We have described a two-step method to screen fresh donor eyes in order to select those with glaucomatous features, especially when the prior history of ocular diseases of the donors is not available. This approach would likely to yield ocular tissues for glaucoma research on gene expression, proteome profiling, ultrastructural changes in the trabecular meshwork and patho-physiologic mechanisms governing trabecular outflow.
Financial support and sponsorship
Aravind Medical Research Grant - In-house Funding, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge the Rotary International Eye Bank, Aravind Eye Hospital, Madurai for providing donor eyes. We also acknowledge Mrs. Bala, Laboraotry Assistant, Department of Ocular Pharmacology, AMRF; Mrs. Papathi, Laboratory Technician, Department of Pathology, AEH, Madurai for their assistance in histological preparation and Mr. Vijayakumar, Biostatistician for his assistance in statistical analysis.
References
- 1.Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004;82:887–8. [PMC free article] [PubMed] [Google Scholar]
- 2.George R, Ve RS, Vijaya L. Glaucoma in India: Estimated burden of disease. J Glaucoma. 2010;19:391–7. doi: 10.1097/IJG.0b013e3181c4ac5b. [DOI] [PubMed] [Google Scholar]
- 3.Curcio CA. Research Tissue Acquisition Working Group. Declining availability of human eye tissues for research. Invest Ophthalmol Vis Sci. 2006;47:2747–9. doi: 10.1167/iovs.05-0978. [DOI] [PubMed] [Google Scholar]
- 4.The Rotary Aravind International Eye Bank. Madurai: Aravind Eye Care System; c2001. [Last cited on 2012 Jan 14]. Available from: http://www.aravind.org/EyeBanks.aspx . [Google Scholar]
- 5.Hancox OD. Optic disc size, an important consideration in glaucoma. Clin Eye Vis Care. 1999;11:59–62. [Google Scholar]
- 6.Armaly MF. Cup-disc ratio in early open-angle glaucoma. Doc Ophthalmol. 1969;26:526–33. doi: 10.1007/BF00944008. [DOI] [PubMed] [Google Scholar]
- 7.Ramakrishnan R, Nirmalan PK, Krishnadas R, Thulasiraj RD, Tielsch JM, Katz J, et al. Glaucoma in a rural population of southern India: The Aravind comprehensive eye survey. Ophthalmology. 2003;110:1484–90. doi: 10.1016/S0161-6420(03)00564-5. [DOI] [PubMed] [Google Scholar]
- 8.Yücel YH, Gupta N, Kalichman MW, Mizisin AP, Hare W, de Souza Lima M, et al. Relationship of optic disc topography to optic nerve fiber number in glaucoma. Arch Ophthalmol. 1998;116:493–7. doi: 10.1001/archopht.116.4.493. [DOI] [PubMed] [Google Scholar]
- 9.Jonas JB, Hayreh SS. Localised retinal nerve fibre layer defects in chronic experimental high pressure glaucoma in rhesus monkeys. Br J Ophthalmol. 1999;83:1291–5. doi: 10.1136/bjo.83.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quigley HA, Brown AE, Morrison JD, Drance SM. The size and shape of the optic disc in normal human eyes. Arch Ophthalmol. 1990;108:51–7. doi: 10.1001/archopht.1990.01070030057028. [DOI] [PubMed] [Google Scholar]
- 11.Varma R, Skaf M, Barron E. Retinal nerve fiber layer thickness in normal human eyes. Ophthalmology. 1996;103:2114–9. doi: 10.1016/s0161-6420(96)30381-3. [DOI] [PubMed] [Google Scholar]
- 12.Frenkel S, Morgan JE, Blumenthal EZ. Histological measurement of retinal nerve fibre layer thickness. Eye (Lond) 2005;19:491–8. doi: 10.1038/sj.eye.6701569. [DOI] [PubMed] [Google Scholar]
- 13.Dichtl A, Jonas JB, Naumann GO. Retinal nerve fiber layer thickness in human eyes. Graefes Arch Clin Exp Ophthalmol. 1999;237:474–9. doi: 10.1007/s004170050264. [DOI] [PubMed] [Google Scholar]
- 14.Quigley HA, Coleman AL, Dorman-Pease ME. Larger optic nerve heads have more nerve fibers in normal monkey eyes. Arch Ophthalmol. 1991;109:1441–3. doi: 10.1001/archopht.1991.01080100121056. [DOI] [PubMed] [Google Scholar]
- 15.Vijaya L, George R, Paul PG, Baskaran M, Arvind H, Raju P, et al. Prevalence of open-angle glaucoma in a rural south Indian population. Invest Ophthalmol Vis Sci. 2005;46:4461–7. doi: 10.1167/iovs.04-1529. [DOI] [PubMed] [Google Scholar]
- 16.Dandona L, Dandona R, Srinivas M, Mandal P, John RK, McCarty CA, et al. Open-angle glaucoma in an urban population in southern India: The Andhra Pradesh eye disease study. Ophthalmology. 2000;107:1702–9. doi: 10.1016/s0161-6420(00)00275-x. [DOI] [PubMed] [Google Scholar]
- 17.Knox DL, Kerrison JB, Green WR. Histopathologic studies of ischemic optic neuropathy. Trans Am Ophthalmol Soc. 2000;98:203–20. [PMC free article] [PubMed] [Google Scholar]
- 18.Goldhagen B, Proia AD, Epstein DL, Rao PV. Elevated levels of RhoA in the optic nerve head of human eyes with glaucoma. J Glaucoma. 2012;21:530–8. doi: 10.1097/IJG.0b013e318241b83c. [DOI] [PubMed] [Google Scholar]


