Abstract
OBJECTIVES:
To describe the change in the management, and outcome of children with acute severe asthma (ASA) admitted to Pediatric Intensive Care Unit (PICU) at tertiary institute, as compared to previously published report in 2003.
METHODS:
This is a retrospective observational study. All consecutive pediatric ASA patients who were admitted to PICU during the study period were included. The data were extracted from PICU database and medical records. The Cohort in this study (2013 Cohort) was compared with the Cohort of ASA, which was published in 2003 from the same institution (2003 Cohort).
RESULTS:
In comparison to previous 2003 Cohort, current Cohort (2013) revealed higher mean age (5.5 vs. 3.6 years; P ≤ 0.001), higher rate of PICU admission (20.3% vs. 3.6%; P ≤ 0.007), less patients who received maintenance inhaled steroids (43.3% vs. 62.4%; P ≤ 0.03), less patients with pH <7.3 (17.9% vs. 42.9%; P ≤ 0.001). There were more patients in 2013 Cohort who received: Inhaled Ipratropium bromide (97% vs. 68%; P ≤ 0.001), intravenous magnesium sulfate (68.2% vs. none), intravenous salbutamol (13.6% vs. 3.6%; P ≤ 0.015), and noninvasive ventilation (NIV) (35.8% vs. none) while no patients were treated with theophylline (none vs. 62.5%). The median length of stay (LOS) was 2 days while mean LOS was half a day longer in the 2013 Cohort. None of our patients required intubation, and there was no mortality.
CONCLUSION:
We observed slight shift toward older age, considerably increased the rate of PICU admission, increased utilization of Ipratropium bromide, magnesium sulfate, and NIV as important modalities of treatment.
Keywords: Asthma, children, critical care, epidemiology, noninvasive ventilation, pediatric, Saudi, status asthmaticus
The prevalence of childhood asthma is increasing worldwide.[1,2] This is also true in Saudi Arabia, where it has increased from 8% to 23% in less than a decade.[3]
Status asthmaticus refers to an acute severe asthma (ASA) exacerbation, in which bronchial obstruction is severe and continues to worsen, or not improve, despite the institution of adequate standard therapy. Respiratory mucosal inflammation and bronchospasm result in dyspnea, increased work of breathing, hypoxemia, and hypercapnia that may progress to respiratory failure. Although the majority of acute asthma attacks are managed at the emergency department (ED) or general ward, admission to Pediatric Intensive Care Unit (PICU) for severe cases may be life-saving. Early and appropriate therapy of ASA result in improved outcome.[4,5,6,7] Over the last decade, there have been changes in treating acute asthma in view of recently published studies, moving more toward evidence-based medical practices.[6,8,9,10,11,12]
To the best of our knowledge, the only local study available to describe the clinical course and outcome of pediatric ASA patients who required admission to PICU was published 10 years ago.[13] The purpose of this current study is to describe the clinical course and outcome of children with ASA admitted to PICU, and to describe change of practice in their management at our institute compared to previously published report in 2003.
Methods
This is a retrospective observational quantitative study. The study was conducted at King Khalid University Hospital, a tertiary teaching hospital in Riyadh, Saudi Arabia. The pediatric service has more than 1400 inpatient admissions and more than 50,000 pediatric ED visits each year. The PICU consists currently of 13 beds, with more than 400 annual admissions.
All consecutive patients 14-year-old or younger with ASA, who were admitted to PICU during the period from November 2011 to October 2013, were included. The patients were either admitted directly to PICU from ED or transferred from pediatric inpatient ward. We identified children with ASA by reviewing the admission diagnosis to PICU. The admission criteria to PICU include one or more of the following: Worsening hypoxia or hypercarbia, requirement for intense (<2 h) or continuous nebulization therapy, exhaustion with shallow respiration, altered mental state, air leak syndrome, or respiratory failure. The criteria to transfer patient out of PICU include: Oxygen requirement <40% to maintain oxygen saturation equal or more than 92%, time between nebulization of 3 h or more, no requirement of noninvasive ventilation (NIV) support, absence of air leak syndrome.
The data were extracted from PICU database, and medical records using predesigned data collection sheet. The obtained information included age, gender, asthma maintenance medication, vital signs on admission, pediatric index of mortality II (PIM II),[14] pediatric respiratory assessment measure (PRAM) score[15,16] upon PICU admission, initial blood gas, Chest X-ray, need of invasive or NIV, medications, complication, length of stay (LOS), and mortality. The Cohort in this study (2013 Cohort) was compared to the Cohort of ASA, which was published in 2003 from our institution (2003 Cohort). The study was approved from the Institutional Review Board for Research at King Saud University.
Descriptive statistics of all variables were expressed using median and inter-quartile ranges for continuous variables or mean ± standard deviation depending on the distribution of the variable. Ten years ago, the data from the current study was compared with our previous study. For categorical data, the Pearson Chi-squared test was used. For continuous data, the Mann–Whitney U-test or Student's t-test was used for nonparametric and parametric data, respectively. Logistic regression analysis was used to identify risk factors for mechanical ventilation (MV). Statistical significance was defined as P ≤ 0.05 and all computations were made using the Statistical Package for the Social Sciences (version 21.0; SPSS, Inc., Chicago, IL, USA).
Results
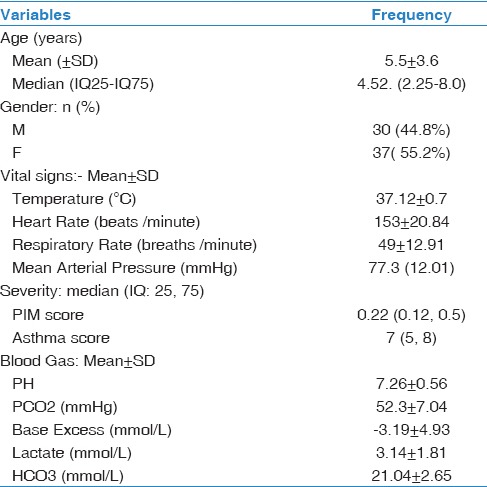
During the 2 years period (November 2011 to October 2013), 67 (20.3%) children were admitted to PICU out of 330 patients admitted to the pediatric ward with the diagnosis of ASA. The admission criteria to PICU were: Severe respiratory distress, hypoxemia, and requirement for frequent or continuous salbutamol nebulization therapy. For the current study Cohort, demographic and clinical profile data are presented in Table 1. These include: Age, gender, PIM II score, PRAM score, initial vital signs, and blood gas upon admission to PICU. Of 67 patients, 29 patients (46%) were on maintenance treatment with inhaled steroids upon admission while 34 (54%) patients were receiving inhaled salbutamol intermittently. Poor compliance to medication was documented in 36 (53.7%) patients. Sixteen patients (23.9%) had a history of previous PICU admission with a similar diagnosis.
Table 1.
Demographic and clinical profile data for current study (2013 Cohort)
Comorbidities were present in 19 (28.4%) patients and included: Type 1 diabetes mellitus, gastroesophageal reflux disease, ex-prematurity, cerebral palsy, seizure disorder, Down syndrome, food allergy, and obesity.
The median asthma score was 7, and the medians PIM II score was 0.5. Only one-third of patients 19 (28.8%) received antibiotics. Lung hyperinflation was the most common finding in chest X-ray 45 (67.2%) while other findings included: Infiltrations 9 (14.9%) or collapse 16 (23.9%). Spontaneous air leak syndromes were observed upon presentation in 3 cases; namely subcutaneous emphysema in two patients, and pneumomediastinum in one.
The number of patients who required NIV, such as bi-level positive airway pressure (BiPAP) or continuous positive airway pressure (CPAP) was 24 (35.8%). The median duration of BiPAP was 24.5 h while the CPAP was 48.1 h. Table 2 shows the multivariate logistic regression analysis for factors associated with NIV requirement. None of our patients required intubation, and there was no mortality. There were more cases admitted during fall and winter seasons, as compared to summer and spring. This seasonal variation is illustrated in Figure 1. Comparison between our previous 2003 Cohort and current Cohort (2013) is shown in Table 3.
Table 2.
Multivariate logistic regression analysis for factors associated with noninvasive ventilation requirement *B = Beta Coefficient
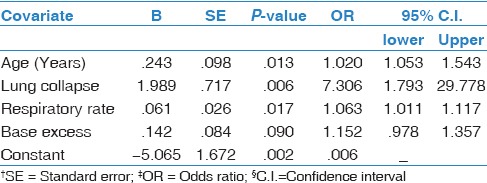
Figure 1.
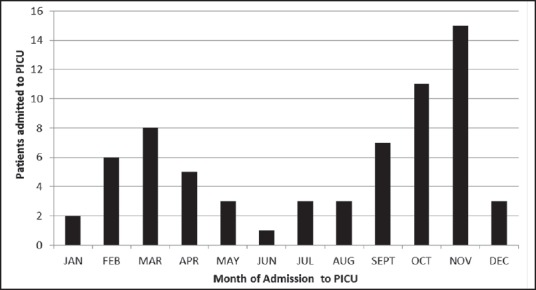
Monthly distribution of children admitted with asthma to Pediatric Intensive Care Unit
Table 3.
Comparison between our previous 2003 Cohort and current Cohort (2013)
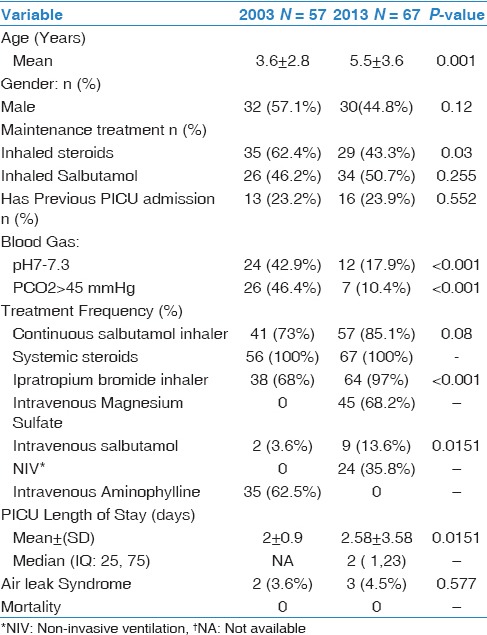
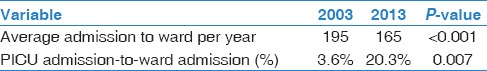
The mean age for 2013 Cohort is 5.5 years while it was 3.6 years in 2003 Cohort (P ≤ 0.001). The age distribution among patients in both groups is shown in Figure 2. There were less patients who received maintenance inhaled steroids, had lower pH and higher PCO2 in 2013 Cohort. Considering therapeutic options, there were more patients in 2013 Cohort who received inhaled Ipratropium bromide, intravenous magnesium sulfate, intravenous salbutamol, and NIV while no patients were treated with theophylline. In 2013 Cohort, the median and mean LOS was 2 and 2.5 days, respectively, compared to mean LOS of 2 days in 2003 Cohort. Average number of asthmatics admitted to ward and percentage of PICU admission for both Cohorts are shown in Table 4.
Figure 2.
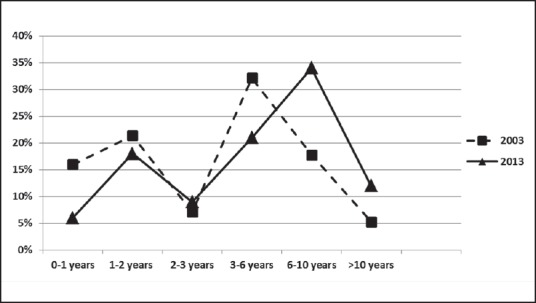
Percentage of age groups of asthmatic children admitted to the Pediatric Intensive Care Unit for both Cohorts (2003, 2013)
Table 4.
Average number of asthmatics yearly admitted to ward and percentage of Pediatric Intensive Care Unit admission for both Cohorts
Discussion
ASA is a life-threatening condition that can lead to death in severe cases. Thus, it necessitates management in acute care settings, such as ED or PICU. This study demonstrates significant findings when compared to our previous report that was published in 2003. Despite a decrease in the number of asthmatics who were admitted to our pediatric ward, there was a noticeable increase in the number of patients who required PICU admission. The lack of significant increase in other severity indicators, such as rate of PICU readmission, complications, rate of intubation, or mortality, makes it difficult to explain such increment in PICU admission based solely on increased severity of the disease overtime. In addition, this finding may indicate improvement in ED management of ASA, leading to less in-patient admission, and only severe cases were admitted. On the other hand, a lower threshold for PICU admission might be a contributing factor to the increase in PICU admission rate. A similar observation was reported by Hartman et al. upon review of asthma cases at New Jersey. They found a decrease in hospital admission by half but associated with tripled rate of PICU admission.[17] Both of our 2003 and 2013 Cohorts, demonstrated similar peaks for PICU admission:First peak during the second year of life and the second, relatively higher peak, was among the preschool age group. However, our current study showed a mean age of children requiring PICU admission of 5.5 years, as compared to a mean of 3.6 years in 2003 Cohort from our institution.[13] This may indicate a slight shift toward higher age in children with ASA requiring PICU admission. However, there is a need to evaluate this finding in other Cohorts and centers across the region. On the other hand, most of other recent studies reported mean or median age of admission to PICU in the range of 6-11 years.[17,18,19,20]
There were similar seasonal variation in both Cohorts, with more ASA patients being admitted to PICU between November and March, leading to peak admission rate during fall and winter. Pendergraft et al. observed a similar increase in hospitalization, ICU admission, and ED visit of asthma patients during the winter. This is likely to be due to the increase in the prevalence of respiratory viral infections, the most common trigger for acute asthma exacerbation.[21,22] In contrast, countries without significant seasonal variation in climate showed the unremarkable prevalence of asthma admission to PICU during the winter season.[18] This study also demonstrates a similar finding to the 2003 Cohort, where almost one-quarter of our patients had previous PICU admission. Other studies reported readmission to PICU in the range of 12-63% of patients.[19,20,23] Although results are variable, but readmission to PICU with ASA may alert healthcare providers about possible suboptimum outpatient follow-up and compliance. This is further supported by our observation that less than half of our current Cohort were prescribed inhaled steroid prior to their study period admission, and only half of them had good compliance. These were common findings among asthmatics that required PICU admission in other published results.[18,19] Thus, such risk factors should be considered in the evaluation of sick asthmatics. Implementation of educational programs and efforts to improve compliance of asthma prophylaxis may be an essential tool to improve outpatient follow-up and medication compliance among these children. Other reported risk factors included poor asthma control, parental history of allergic disease, and the usage of steroids during the first admission, and ventilation at admission.
In our study, the presence of hyperinflation and segmental or lobar lung collapse were the most frequent findings on chest radiographs. These findings correlate with the pathophysiology of asthma, that includes increased airway resistance and mucus plugs formation. Although routine radiologic evaluation is not recommended for all acute exacerbation of asthma, it remains an important diagnostic tool in these subgroup of patients requiring PICU admission, to rule out complications, such as air-leak syndrome or major lung collapse, or if other diagnosis is considered. Narayanan et al. in a recent review of patients, who were hospitalized for asthma reported that out of 44% of patients who had chest X-ray, only 10% of patient had modified treatment plan after the chest X-ray.[24]
The lack of severity scores and vital signs in 2003 Cohort report put some limitations on interpreting the reported lower pH and higher PCO2 at PICU admission as compared to our current Cohort. The improvement in blood gas findings in our current Cohort may be partially due to having lower threshold for admission to PICU, or due to truly better initial stabilization at ED in view of recent modification of management of ASA.[6,11,12,25]
Systemic steroids and inhaled salbutamol remained the cornerstone in the management of ASA.[8,9,10,26] All patients during the study period from both Cohorts received both medications. Among our current Cohort, we found that the majority of patients were treated initially with continuous salbutamol nebulization rather than intermittent doses, with no adverse complication reported. Papo et al. has reported that the use of continuous salbutamol nebulization showed improvement in outcomes and better cost effectiveness than intermittent therapy.[27] However, the use of such approach should be carefully accompanied by close monitoring for potential side effects. Sarnaik et al. reported that diastolic hypotension and tachycardia are dose-dependent side effects of high dose β2-agonist, and may be associated with increased troponin levels in high-risk patients, a marker of myocardial injury.[28] In addition, transient intrapulmonary shunting associated with β2-agonist therapy may contribute to arterial hypoxemia.[29]
On the other hand, we observed changes in other therapies in our current Cohort as compared to 2003 Cohort. These changes included: Trends toward increased use of Ipratropium bromide nebulization and intravenous salbutamol infusion. Furthermore, we observed the emergence of intravenous magnesium sulfate as a second-line treatment, with a significant decline in the use of Aminophylline. These trends are correlating with the changes in asthma management guidelines during the 10 years period between the two Cohorts.[8,9,30] The optimum intravenous bronchodilator has been an area of debate, with concerns about effectiveness, safety, and cost. This controversy has been a focus for many publications.[31,32,33,34,35,36,37] The use of intravenous magnesium sulfate in ASA, when the initial management fails, can reduce hospitalization and improve outcome.[12,25,30,38,39,40] In contrast, use of methylxanthines in treatment of ASA has decreased, probably due to lack of proven superiority to intravenous magnesium sulfate or β2-agonist in the literature, in addition to unfavorable side effects and narrow therapeutic window.[6,32,37,41,42] Nevertheless, its use in refractory cases is variably considered.[36,43,44,45,46]
NIV was used in 35.8% of our patient. Its use was safe, and none of our 2013 Cohort patients required invasive ventilation. Furthermore, there was no associated complication or air leak syndrome among these patients. The multivariate logistic regression analysis for factors associated with NIV requirement revealed: older age, the presence of lung collapse on chest X-ray, and higher respiratory rate. In contrast, NIV was not used in 2003 Cohort. The main indication for its use is to improve the work of breathing and facilitate gas exchange. Basnet et al. published his prospective randomized controlled trial that reported a safe profile and favorable outcome for asthmatic children treated with NIV.[47] Therefore, NIV became a popular tool to minimize the need for tracheal intubation. However, in severe and progressive cases, intubation and MV are inevitable.
In this study, we found that the PICU LOS of our patients was variable, with a mean of 2.58 days. Although this may indicate change toward slightly higher LOS as compared to a mean of 2 days in 2003 Cohort, but this could be due to skewed distribution curve with outliers. This assumption is supported by the fact that the two-third of patients stayed for 2 days or less and the computed median for this Cohort is 2 days. On the other hand, due to lack of severity scores in 2003 Cohort, it will be difficult to adjust LOS for the severity to make it clinically meaningful. Nevertheless, despite using PICU discharge criteria, it remains vulnerable to assessing physician's subjectivity. Our findings are consistent with reported LOS in the literature in the range of 1-3 days.[17,18,19,20,23,48]
The presence of air leak syndrome was observed in both Cohorts upon admission before the initiation of treatment, and they were probably related to the air trapping pathophysiology and disease severity. Fortunately, all patients in both Cohorts had a smooth recovery, without the need of intercostals tube drainage. A previous study revealed that 8% of asthmatic children admitted to PICU developed complications and needed a longer stay. Bronchopneumonia, aspiration pneumonia, ventilator-associated pneumonia, pneumo-mediastinum, pneumothorax, and hemodynamic compromise were the most encountered adverse events.[18,49]
There was no mortality in both Cohorts from our institution. The outcome of childhood ASA is relatively good, with low mortality, ranging from 0% to 4%.[2,18,20,50,51] The need for MV has been significantly associated with higher mortality. Rampa et al. described in hospital mortality of 4% for those with MV, as compared to 0.03% for those without MV.[48] Furthermore, delay in arrival to ED is consistently associated with increased morbidity and mortality.[6,7]
The limitation of our study lies mainly in the design of retrospective analysis from a single center experience. However, it highlights the changes over one decade in the population and clinical management practices of ASA requiring admission to PICU. Further prospective studies with larger number of patients representing multicenter experience are recommended.
In summary, we observed slight shift toward older age for children with ASA, who required admission to PICU, with peak admission at fall and winter. Although the rate of ward admission due to acute asthma has decreased, the rate of PICU admission has considerably increased. The clinical course and outcomes of patients with ASA, who required PICU admission varied according to the severity. This study demonstrates an increase in utilization of magnesium sulfate and NIV as important modalities of treatment. On the other hand, there is a significant decrease in the use of aminophylline in severe asthmatics. This study also reports low rate of complications and no mortality among these asthmatic children in our institute.
Financial support and sponsorship
College of Medicine Health Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Anandan C, Nurmatov U, van Schayck OC, Sheikh A. Is the prevalence of asthma declining.Systematic review of epidemiological studies? Allergy. 2010;65:152–67. doi: 10.1111/j.1398-9995.2009.02244.x. [DOI] [PubMed] [Google Scholar]
- 2.Strid JM, Gammelager H, Johansen MB, Tønnesen E, Christiansen CF. Hospitalization rate and 30-day mortality among patients with status asthmaticus in Denmark: A 16-year nationwide population-based cohort study. Clin Epidemiol. 2013;5:345–55. doi: 10.2147/CLEP.S47679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wahabi HA, Alziedan RA. Reasons behind non-adherence of healthcare practitioners to pediatric asthma guidelines in an emergency department in Saudi Arabia. BMC Health Serv Res. 2012;12:226. doi: 10.1186/1472-6963-12-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009;123(Suppl 3):S131–45. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 5.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: Prevalence, health care utilization, and mortality. Pediatrics. 2002;110(2 Pt 1):315–22. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 6.Carroll CL, Sala KA. Pediatric status asthmaticus. Crit Care Clin. 2013;29:153–66. doi: 10.1016/j.ccc.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Werner HA. Status asthmaticus in children: A review. Chest. 2001;119:1913–29. doi: 10.1378/chest.119.6.1913. [DOI] [PubMed] [Google Scholar]
- 8.Eid NS. National Asthma Education and Prevention Program. Update on National Asthma Education and Prevention Program pediatric asthma treatment recommendations. Clin Pediatr (Phila) 2004;43:793–802. doi: 10.1177/000992280404300903. [DOI] [PubMed] [Google Scholar]
- 9.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 10.Elward KS, Pollart SM. Medical therapy for asthma: Updates from the NAEPP guidelines. Am Fam Physician. 2010;82:1242–51. [PubMed] [Google Scholar]
- 11.Jones BP, Paul A. Management of acute asthma in the pediatric patient: An evidence-based review. Pediatr Emerg Med Pract. 2013;10:1–23. [PubMed] [Google Scholar]
- 12.Wong JJ, Lee JH, Turner DA, Rehder KJ. A review of the use of adjunctive therapies in severe acute asthma exacerbation in critically ill children. Expert Rev Respir Med. 2014;8:423–41. doi: 10.1586/17476348.2014.915752. [DOI] [PubMed] [Google Scholar]
- 13.Abu-Ekteish FM, Zahraa JN, Al-Mobaireek KF, Nasir AA, Al-Frayh AS. The management of acute severe asthma in a pediatric intensive care unit. Saudi Med J. 2003;24:388–90. [PubMed] [Google Scholar]
- 14.Slater A, Shann F, Pearson G. Paediatric Index of Mortality (PIM) Study Group. PIM2: A revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29:278–85. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 15.Chalut DS, Ducharme FM, Davis GM. The Preschool Respiratory Assessment Measure (PRAM): A responsive index of acute asthma severity. J Pediatr. 2000;137:762–8. doi: 10.1067/mpd.2000.110121. [DOI] [PubMed] [Google Scholar]
- 16.Ducharme FM, Chalut D, Plotnick L, Savdie C, Kudirka D, Zhang X, et al. The Pediatric Respiratory Assessment Measure: A valid clinical score for assessing acute asthma severity from toddlers to teenagers. J Pediatr. 2008;152:476–80. doi: 10.1016/j.jpeds.2007.08.034. 480.e1. [DOI] [PubMed] [Google Scholar]
- 17.Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in admissions for pediatric status asthmaticus in New Jersey over a 15-year period. Pediatrics. 2010;126:e904–11. doi: 10.1542/peds.2009-3239. [DOI] [PubMed] [Google Scholar]
- 18.Chiang BL, Hsieh CT, Wang LC, Lee JH, Yu HH, Lin YT, et al. Clinical course and outcome of children with status asthmaticus treated in a pediatric intensive care unit: A 15-year review. J Microbiol Immunol Infect. 2009;42:488–93. [PubMed] [Google Scholar]
- 19.Sala KA, Carroll CL, Tang YS, Aglio T, Dressler AM, Schramm CM. Factors associated with the development of severe asthma exacerbations in children. J Asthma. 2011;48:558–64. doi: 10.3109/02770903.2011.585411. [DOI] [PubMed] [Google Scholar]
- 20.Sheikh S, Khan N, Ryan-Wenger NA, McCoy KS. Demographics, clinical course, and outcomes of children with status asthmaticus treated in a pediatric intensive care unit: 8-year review. J Asthma. 2013;50:364–9. doi: 10.3109/02770903.2012.757781. [DOI] [PubMed] [Google Scholar]
- 21.Pendergraft TB, Stanford RH, Beasley R, Stempel DA, McLaughlin T. Seasonal variation in asthma-related hospital and intensive care unit admissions. J Asthma. 2005;42:265–71. doi: 10.1081/jas-200057893. [DOI] [PubMed] [Google Scholar]
- 22.Sears MR. Epidemiology of asthma exacerbations. J Allergy Clin Immunol. 2008;122:662–8. doi: 10.1016/j.jaci.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Hon KL, Tang WS, Leung TF, Cheung KL, Ng PC. Outcome of children with life-threatening asthma necessitating pediatric intensive care. Ital J Pediatr. 2010;36:47. doi: 10.1186/1824-7288-36-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Narayanan S, Magruder T, Walley SC, Powers T, Wall TC. Relevance of chest radiography in pediatric inpatients with asthma. J Asthma. 2014;51:751–5. doi: 10.3109/02770903.2014.909459. [DOI] [PubMed] [Google Scholar]
- 25.Koninckx M, Buysse C, de Hoog M. Management of status asthmaticus in children. Paediatr Respir Rev. 2013;14:78–85. doi: 10.1016/j.prrv.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Keeney GE, Gray MP, Morrison AK, Levas MN, Kessler EA, Hill GD, et al. Dexamethasone for acute asthma exacerbations in children: A meta-analysis. Pediatrics. 2014;133:493–9. doi: 10.1542/peds.2013-2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Papo MC, Frank J, Thompson AE. A prospective, randomized study of continuous versus intermittent nebulized albuterol for severe status asthmaticus in children. Crit Care Med. 1993;21:1479–86. doi: 10.1097/00003246-199310000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Sarnaik SM, Saladino RA, Manole M, Pitetti RA, Arora G, Kuch BA, et al. Diastolic hypotension is an unrecognized risk factor for ß-agonist-associated myocardial injury in children with asthma. Pediatr Crit Care Med. 2013;14:e273–9. doi: 10.1097/PCC.0b013e31828a7677. [DOI] [PubMed] [Google Scholar]
- 29.Bates ML, Jacobson JE, Eldridge MW. Transient intrapulmonary shunting in a patient treated with ß2-adrenergic agonists for status asthmaticus. Pediatrics. 2014;133:e1087–91. doi: 10.1542/peds.2013-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Moamary MS, Al-Hajjaj MS, Idrees MM, Zeitouni MO, Alanezi MO, Al-Jahdali HH, et al. The Saudi initiative for asthma. Ann Thorac Med. 2009;4:216–33. doi: 10.4103/1817-1737.56001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wheeler DS, Jacobs BR, Kenreigh CA, Bean JA, Hutson TK, Brilli RJ. Theophylline versus terbutaline in treating critically ill children with status asthmaticus: A prospective, randomized, controlled trial. Pediatr Crit Care Med. 2005;6:142–7. doi: 10.1097/01.PCC.0000154943.24151.58. [DOI] [PubMed] [Google Scholar]
- 32.Travers AH, Jones AP, Camargo CA, Jr, Milan SJ, Rowe BH. Intravenous beta(2)-agonists versus intravenous aminophylline for acute asthma. Cochrane Database Syst Rev. 2012;12:CD010256. doi: 10.1002/14651858.CD010256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Albuali WH. The use of intravenous and inhaled magnesium sulphate in management of children with bronchial asthma. J Matern Fetal Neonatal Med. 2014;27:1809–15. doi: 10.3109/14767058.2013.876620. [DOI] [PubMed] [Google Scholar]
- 34.Doymaz S, Schneider J, Sagy M. Early administration of terbutaline in severe pediatric asthma may reduce incidence of acute respiratory failure. Ann Allergy Asthma Immunol. 2014;112:207–10. doi: 10.1016/j.anai.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Kantor DB, Phipatanakul W. Intravenous β agonists and severe pediatric asthma exacerbation: Time for a closer look at terbutaline? Ann Allergy Asthma Immunol. 2014;112:187. doi: 10.1016/j.anai.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Morris I, Lyttle MD, O'sullivan R, Sargant N, Doull IJ, Powell CV, et al. Which intravenous bronchodilators are being administered to children presenting with acute severe wheeze in the UK and Ireland? Thorax. 2015;70:88–91. doi: 10.1136/thoraxjnl-2014-206041. [DOI] [PubMed] [Google Scholar]
- 37.Singhi S, Grover S, Bansal A, Chopra K. Randomised comparison of intravenous magnesium sulphate, terbutaline and aminophylline for children with acute severe asthma. Acta Paediatr. 2014;103:1301–6. doi: 10.1111/apa.12780. [DOI] [PubMed] [Google Scholar]
- 38.Ohn M, Jacobe S. Magnesium should be given to all children presenting to hospital with acute severe asthma. Paediatr Respir Rev. 2014;15:319–21. doi: 10.1016/j.prrv.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 39.Shedd GC, Noe SM. Intravenous magnesium sulfate reduces rates of mechanical ventilation in pediatric asthma. Adv Emerg Nurs J. 2014;36:3–8. doi: 10.1097/TME.0000000000000009. [DOI] [PubMed] [Google Scholar]
- 40.Louie S, Morrissey BM, Kenyon NJ, Albertson TE, Avdalovic M. The critically ill asthmatic - From ICU to discharge. Clin Rev Allergy Immunol. 2012;43:30–44. doi: 10.1007/s12016-011-8274-y. [DOI] [PubMed] [Google Scholar]
- 41.Dalabih A, Harris ZL, Bondi SA, Arnold DH. Contemporary aminophylline use for status asthmaticus in pediatric ICUs. Chest. 2012;141:1122–3. doi: 10.1378/chest.11-2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dalabih AR, Bondi SA, Harris ZL, Saville BR, Wang W, Arnold DH. Aminophylline infusion for status asthmaticus in the pediatric critical care unit setting is independently associated with increased length of stay and time for symptom improvement. Pulm Pharmacol Ther. 2014;27:57–61. doi: 10.1016/j.pupt.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen ZC, Ding JJ, Qian HY, Lin XH, Feng KQ, Wang J. Clinical efficacies of inhaled corticosteroids plus theophylline in the treatment of bronchial asthma. Zhonghua Yi Xue Za Zhi. 2013;93:1076–9. [PubMed] [Google Scholar]
- 44.Nievas IF, Anand KJ. Severe acute asthma exacerbation in children: A stepwise approach for escalating therapy in a pediatric intensive care unit. J Pediatr Pharmacol Ther. 2013;18:88–104. doi: 10.5863/1551-6776-18.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wallis LA, Stander M. Asthma guidelines: Why aminophylline? S Afr Med J. 2013;103:274. doi: 10.7196/samj.6929. [DOI] [PubMed] [Google Scholar]
- 46.Yokoba M, Ichikawa T, Takakura A, Ishii N, Kurosaki Y, Yamada Y, et al. Aminophylline increases respiratory muscle activity during hypercapnia in humans. Pulm Pharmacol Ther. 2015;30:96–101. doi: 10.1016/j.pupt.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 47.Basnet S, Mander G, Andoh J, Klaska H, Verhulst S, Koirala J. Safety, efficacy, and tolerability of early initiation of noninvasive positive pressure ventilation in pediatric patients admitted with status asthmaticus: a pilot study. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2012;13:393–8. doi: 10.1097/PCC.0b013e318238b07a. Epub 2011/11/10. doi: 10.1097/PCC.0b013e318238b07a. PubMed PMID: 22067982. [DOI] [PubMed] [Google Scholar]
- 48.Rampa S, Allareddy V, Asad R, Nalliah RP, Allareddy V, Rotta AT. Outcomes of invasive mechanical ventilation in children and adolescents hospitalized due to status asthmaticus in United States: A population based study. J Asthma. 2015;52:423–30. doi: 10.3109/02770903.2014.971969. [DOI] [PubMed] [Google Scholar]
- 49.Bratton SL, Odetola FO, McCollegan J, Cabana MD, Levy FH, Keenan HT. Regional variation in ICU care for pediatric patients with asthma.The Journal of pediatrics. 2005;147:355–61. doi: 10.1016/j.jpeds.2005.05.008. Epub 2005/09/27. doi: 10.1016/j.jpeds.2005.05.008. PubMed PMID: 16182675. [DOI] [PubMed] [Google Scholar]
- 50.Carroll CL, Zucker AR. The increased cost of complications in children with status asthmaticus.Pediatr Pulmonol. 2007;42:914–9. doi: 10.1002/ppul.20682. Epub 2007/08/30. doi: 10.1002/ppul.20682. PubMed PMID: 17726707. [DOI] [PubMed] [Google Scholar]
- 51.Stow PJ, Pilcher D, Wilson J, George C, Bailey M, Higlett T, et al. Improved outcomes from acute severe asthma in Australian intensive care units (1996 2003) Thorax. 2007;62:842–7. doi: 10.1136/thx.2006.075317. [DOI] [PMC free article] [PubMed] [Google Scholar]


