Abstract
Women (N = 171), distressed from their partners’ untreated alcoholism, received either coping skills training (CST), 12-step facilitation (TSF), or delayed treatment (DTC). CST and TSF resulted in lower depression levels than DTC but did not differ from one another. Skill acquisition mediated the treatment effects of CST; Al-Anon attendance did not mediate the TSF effect. Lower depression levels were maintained at 12 months with no differences between groups. Partner drinking decreased from pretreatment to follow-up in the CST and TSF conditions. However, for partners with a history of relationship violence, drinking improved across follow-up in the CST condition but worsened in the TSF condition. Partner relationship violence was less in the CST condition. CST may be particularly useful for women experiencing physical violence from a partner with alcoholism.
Women who have a partner with alcoholism have been found to be at greater risk for depression, trauma, and other stress-related disorders and to make greater use of health care services than the general population (Roberts & Brent, 1982; Svenson, Forster, Woodhead, & Platt, 1995). The distress seen in this population most recently has been conceptualized from within a family stress and family interactional model (Hobfoll & Speilberger, 1992; Moos, Finney, & Cronkite, 1990; Orford, 1986; Rychtarik & McGillicuddy, 1997). This model proposes that stress brought on by the negative consequences of the partner’s drinking largely accounts for the negative affect experienced in this population. The woman’s negative affect, however, is also both directly and indirectly associated with her own coping skills. More effective coping is associated with lower negative affect generally, but it also is hypothesized to have an indirect effect through its negative influence on partner drinking and the buffering (moderating) of partner negative drinking consequences. In this interactive model, however, spouse negative affect is also thought to have a detrimental effect on coping skills (e.g., greater negative affect may interfere with effective coping) and to have a positive impact on the maintenance of the partner’s drinking (e.g., greater negative affect in the spouse may increase or help maintain negative affect and continued drinking in the partner).
The literature shows growing empirical support for several of the pathways proposed in this model. The depression and marital distress experienced by women with a partner with alcoholism appear directly related to stress, burden, or extent of problems brought on by their partner’s drinking (Moos et al., 1990; Rychtarik & McGillicuddy, 1997; Zweben, 1986). Moreover, in ways consistent with the model, the manner in which individuals cope with these problems appears to influence their own functioning (Moos et al., 1990; Moos, Finney, & Gamble, 1982; Rychtarik & McGillicuddy, 1997), their partner’s drinking (Orford et al., 1975; Rychtarik & McGillicuddy, 1997; Schaffer & Tyler, 1979), and their partner’s recognition of a drinking problem (Rychtarik & McGillicuddy, 1997; Sobell, Sobell, Toneatto, & Leo, 1993).
A direct implication of this stress and coping model is that individuals can be taught more effective skills in coping with problems brought on by their partners’ drinking. These new skills are hypothesized to result in improved functioning in the individual and to have a positive effect on the partners’ drinking problem. To date, empirical evaluations of skill-based interventions involving the spouse or intimate of persons with alcoholism have largely been limited to studies of conjoint marital therapy in treatment populations. The findings of these studies are consistent in demonstrating the effectiveness of marital therapy over nonmarital treatment alone in improving relationship satisfaction and the partner’s drinking (see Stanton & Shadish, 1997). Still, many persons with active alcoholism do not seek or are not currently involved in treatment (Substance Abuse & Mental Health Services Administration, 2003). A small but growing body of empirical research has emerged that evaluates coping skill-based interventions designed specifically for the spouse or intimate of this nontreatment population. Conceptually, these interventions can be grouped into two broad but overlapping categories depending on the primary pathways targeted in the stress and coping model: (a) those with the specific goal of teaching the spouse skills to motivate the partner to change his or her drinking and (b) those focused predominantly on improving the functioning of the spouse or intimate partner, regardless of the partner’s drinking. Often these interventions are compared with the self-help Group Al-Anon or variations of the Al-Anon, 12-Step approach. Al-Anon focuses on improving the well-being of participants by offering support and encouraging the individual to detach from the partner’s drinking, focusing instead on the individual’s own needs.
Interventions Targeting the Partner’s Drinking
Thomas, Yoshioka, Ager, and Adams (1990) reported that after 6 months 39% of participants in a unilateral family therapy condition (treatment including only the spouse but focused on training skills to engage the partner in treatment) indicated their partner had sought help for the drinking problem compared to 10.5% and 15.2% in delayed treatment and no treatment conditions, respectively. Even larger effects were noted at 12 months. Barber and Gilbertson (1996) randomly assigned 48 individuals with partners who have alcoholism to either an individualized skill-based pressures-to-change drinking program, a group pressures-to-change program, a wait list control, or participation in Al-Anon. At the end of treatment, the individual and group-based pressures-to-change conditions each had 33% of the partners seek treatment compared to none in either the wait list or Al-Anon conditions. However, no change in overall well-being of study participants in any condition was observed. Miller, Meyers, and Tonigan (1999) followed up on the earlier pilot work of Sisson and Azrin (1986) and randomly assigned 130 significant others (59% spouses or intimates) to either (a) a behavioral skills training intervention specifically designed to motivate the partner to seek help, (b) the Johnson & Johnson family intervention approach (Johnson, 1986) to motivate the partner to seek help, or (c) a structured 12-step oriented intervention designed to facilitate participation in Al-Anon. At a 12-month follow-up, significantly more participants in the behavioral skills training intervention reported that the person with alcoholism sought help (67%) than did participants in either the Johnson & Johnson intervention (35%) or the Al-Anon facilitation (20%) conditions. Collapsed across conditions, however, spouses, when compared to parents, were significantly less likely to engage the person with alcoholism in treatment. Notably, individuals participating in all conditions improved in their own psychological functioning regardless of whether the person with alcoholism sought treatment and without any differences between groups. In summary, interventions for the spouse or significant other with the stated goal of either motivating the person with alcoholism to seek help or to stop or decrease alcohol use appear to be more effective than no or alternate treatments in increasing treatment engagement, although they may be relatively less effective in engaging the partner when the significant other is a spouse. Their effect on the spouse or intimate’s functioning, however, has varied.
Interventions Targeting Negative Affect in the Spouse or Intimate
Fewer researchers have studied ways to improve the functioning of the spouse or intimate. Dittrich and Trapold (1984) randomly assigned 23 spouses of persons with alcoholism to either an 8-week experimental treatment provided in a group format or a wait list that received only literature on reducing enabling behaviors. The experimental treatment included education, identification of enabling behaviors, assertiveness training, setting of personal goals, and a buddy system for participants. No significant differences were observed between conditions in participant depression at the end of treatment, but researchers found between-group differences favoring the experimental treatment on measures of self-concept and anxiety. Collapsed across conditions, once the wait list condition received treatment, participants significantly improved across all measures from pretreatment to the end of treatment. In addition, by the end of a 12-month follow-up, 48% of partners were reported to have sought help.
Halford, Price, Kelly, Bouma, and Young (2001) randomly assigned 61 women with partners with alcoholism to one of three individually administered interventions to reduce the woman’s stress: supportive counseling, stress management, or stress management plus alcohol-focused couples therapy (if the partner subsequently engaged in treatment). All treatments showed a reduction in the woman’s stress, but there were no significant differences between conditions and no change in the partners’ drinking or partner relationship violence.
Critique and the Current Study
Several factors appear to limit the findings of research to date on interventions for the spouse or intimate of the person with alcoholism. Most notable is the exclusion of individuals with a history of partner physical violence. In fact, each of the two largest studies of interventions to motivate the person with alcoholism to seek help appear to have excluded individuals with a history of partner domestic violence (Miller et al., 1999; Thomas et al., 1990). Moreover, only Halford et al. (2001) have reported the effects of the interventions on partner violence. Spouses from physically violent relationships have been excluded out of concern that a change in the coping or interactional pattern of the spouse might precipitate a violent reaction in the partner (Thomas & Ager, 1993). Yet, the exclusion of those from violent-partner relationships raises the concern that results may not generalize to a potentially large percentage of individuals with a partner who has alcoholism—more than 50% by some reports (e.g., Gondolf & Foster, 1991). A related limitation is that studies to date have focused only on the main effects of treatment. No published study has examined what spouse factors (e.g., history of partner violence) might moderate treatment effects. Do some individuals benefit more from one treatment approach over another?
Another limitation is that comparisons with other treatments have been confounded by treatment goal. For example, Barber and Gilbertson (1996) and Miller et al. (1999) compared their respective drinking reduction and treatment engagement conditions with Al-Anon or an intervention designed to increase Al-Anon attendance. However, Al-Anon focuses almost exclusively on improving the functioning of the individual without alcoholism—encouraging the spouse to not actively intervene with the partner. Moreover, Al-Anon and similar 12-step interventions rely heavily on the support of the group, yet in Miller et al. the Al-Anon facilitation condition was individually based. Hence, it is not clear whether differences in treatments reflect true differences or simply differences in treatment goal–expectancy or format (or both). Finally, no study has systematically assessed the proximal outcomes of these skill-based treatments to determine whether improvements in skill actually occur, whether they are associated with outcome, and whether they mediate any treatment differences observed.
In the current study we compared the immediate and long-term efficacy of an empirically based coping skills training (CST) program and a theoretically distinct professionally administered 12-step, Al-Anon facilitation condition for women whose partners’ have alcoholism. The sample included women from both nonviolent and violent relationships. Both treatments were group-based and shared the common goal of improving the spouse or intimate’s own functioning—in this case depressive symptoms. We also evaluated the presumed indirect effects of the treatments (through their effects on the woman) on partner drinking, and we examined the mediating role of skill acquisition and Al-Anon attendance in each respective treatment on primary participant and partner outcomes. Furthermore, although not primary foci of the treatments, we assessed the secondary outcomes of partner help-seeking and partner physical violence as secondary outcome measures. We then tested three a priori hypothesized Client Attribute × Treatment interactions. Specifically, we hypothesized that, because of the higher spiritual emphasis of Al-Anon, higher levels of meaning seeking (spirituality) would be associated with better outcomes in 12-step facilitation (TSF) than in the coping skills training condition. We also hypothesized that women from more cohesive relationships would benefit more from skills training than 12-step because the partner in a high cohesive relationship would be more responsive to the woman’s change in skill than in a relationship with low cohesion. Our third a priori hypothesis was that women with higher levels of interpersonal dependency would benefit more from 12-step than skill training, whereas the opposite was hypothesized for those low in interpersonal dependency. We hypothesized that women with higher levels of dependency would identify more with the 12-step program, which aims to switch dependency from the partner to dependency on the Al-Anon group. Finally, given concerns over the involvement of spouses from violent relationships in skill training programs such as that studied here, we explored whether a history of partner relationship violence moderates treatment effects.
Method
Participants
Participants were recruited over a 2-year period through media advertisements offering a program for women experiencing stress as a result of their partner’s drinking. Individuals were eligible if they were (a) living with their partner; (b) married or cohabiting for at least 1 year; (c) free of a substance use disorder of their own by scoring less than 9 on the Alcohol Use Disorders Identification Test (AUDIT; Babor, De la Fuente, Saunders, & Grant, 1989) and less than 4 on the Drug Abuse Screening Test (DAST; Skinner, 1982); (d) inactive in Al-Anon or another treatment program related to their partner’s drinking in the last 3 months; and (e) willing to participate. In addition, based on the woman’s report, the partner had to obtain a score of 9 or more on the AUDIT, have been actively drinking in the last 3 months, and not have attended Alcoholics Anonymous (AA) or formal treatment for substance abuse in that period. Participants also were asked to provide the name of an individual familiar with both the participant’s and the partner’s drinking and other functioning, who could serve as a corroborating source. Of 221 individuals attending an in-person screening interview, 171 (77%) met eligibility criteria, consented to participation, and attended a separate pretreatment assessment. The remaining 23% either did not meet eligibility criteria, met eligibility criteria but declined participation, did not complete additional pretreatment assessment requirements, or were judged to be in immediate danger and in need of other services (i.e., a domestic violence shelter; n = 1). The final sample was 42.60 (SD = 9.79) years of age, had 13.44 (SD = 2.09) years of education, was predominantly white (84%), employed full or part time (85%), and married (87%). They scored an average of 13.50 (SD = 8.51) on the Beck Depression Inventory—Version I, Amended (BDI-IA; Beck & Steer, 1993); 47% reported experiencing partner physical violence during the previous year. As reported by the women, partners averaged 23.48 (6.19) on the AUDIT and averaged 19.02 (SD = 10.72) years of problem drinking. More detailed characteristics of the final sample are presented in Table 1. Treatment conditions differed significantly only on participant employment stability (i.e., months employed over the past 3 years), F(2, 33) = 5.92, p < .01.
Table 1.
Participant Pretreatment Characteristics by Treatment Condition
| Characteristic | Coping skills training (n = 55) | 12-Step facilitation (n = 58) | Delayed Treatment Control (n = 58) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| % | M | SD | % | M | SD | % | M | SD | |
| Age (years) | 42.78 | 10.35 | 42.62 | 9.69 | 42.41 | 9.50 | |||
| Racial-ethnic status | |||||||||
| White | 76 | 86 | 90 | ||||||
| Black | 18 | 12 | 7 | ||||||
| Hispanic | 2 | 2 | 2 | ||||||
| Native American | 4 | 0 | 2 | ||||||
| Full/part-time employment (%) | 41 | 54 | 50 | ||||||
| Months employed (past 3 years)** | 14.96a | 16.08 | 26.60b | 13.47 | 20.50 | 16.40 | |||
| Year of educations | 13.13 | 2.26 | 13.75 | 2.20 | 13.41 | 1.78 | |||
| Married (%) | 85 | 79 | 97 | ||||||
| Years living with partner | 17.33 | 11.93 | 15.80 | 14.63 | 15.86 | 10.03 | |||
| Occupational statusa | 4.62 | 1.95 | 5.30 | 1.65 | 4.93 | 1.74 | |||
| Spiritualityb | −29.24 | 32.60 | −31.45 | 31.65 | −30.69 | 34.11 | |||
| Dyadic adjustmentc | 68.77 | 24.48 | 72.09 | 21.53 | 74.88 | 21.98 | |||
| Dyadic Cohesiond | 9.30 | 4.48 | 9.64 | 4.43 | 10.01 | 4.65 | |||
| Interpersonal dependencye | 46.38 | 15.22 | 44.50 | 14.43 | 45.11 | 13.10 | |||
| SSI coping skill levelf | 3.01 | 0.29 | 3.03 | 0.28 | 2.98 | 0.29 | |||
| SSI Problem Similarity Scoreg | 2.20 | .52 | 2.18 | .60 | 2.26 | .62 | |||
| Participant depressionh | 13.80 | 7.85 | 13.48 | 9.37 | 13.22 | 8.34 | |||
| Partner AUDITi | 25.11 | 5.91 | 22.99 | 5.85 | 22.43 | 6.57 | |||
| Partner readiness-to-change | 3.36 | 2.73 | 4.21 | 2.68 | 3.31 | 2.54 | |||
| Partner violencek | |||||||||
| Prevalence | 55 | 45 | 41 | ||||||
| Intensity | 7.45 | 18.69 | 10.45 | 26.21 | 4.07 | 10.35 | |||
| Partner length of problem (years) | 19.73 | 10.48 | 18.58 | 10.46 | 18.78 | 11.34 | |||
| Partner abstinent days (%)l | 25 | 28 | 24 | 29 | 27 | 33 | |||
| Partner drinks per drinking dayl | 11.92 | 10.71 | 9.99 | 8.91 | 10.13 | 6.51 | |||
| Partner prior substance abuse treatment | 51 | 38 | 47 | ||||||
Note: Values with subscripts are significantly different from one another.
Hollingshead and Redlich (1958) coded 1 (low status) to 9 (high status).
Meaning seeking as measured by the Purpose in Life Test and Seeking of Noetic Goals Scale.
Total adjustement score of the Dyadic Adjustment Scale.
Dyadic Adjustment Scale, Cohesion subscale.
Interpersonal Dependency Inventory.
Mean situation skillfulness score (1 = Least Skillful, 6 = Most Skillful) on the Spouse Situation Inventory (SSI).
Mean situation similarity score (1 = Not Similar at All, 5 = Extremely Similar) on the SSI.
Beck Depression Inventory.
Alcohol Use Disorders Identification Test (AUDIT).
From the University of Rhode Island Change Assessment Scale.
Conflict Tactics Scale, Physical Violence subscale.
90 days pretreatment.
p < .01.
Design and Procedure
A 3 group (CST, TSF, or delayed treatment control [DTC]) longitudinal design was used.1 Each consecutive set of four to six eligible participants formed a cohort or therapy group. After completing all pretreatment assessments, a cohort was randomly assigned to one of the three treatment conditions.
Assignment was random with the provision that an equal number of cohorts be assigned to each condition.2 An assigned cohort then participated in 8 weeks of either CST, TSF, or no treatment. Overall, 36 cohorts were randomized (12 in each condition). On completion of the 8-week period, participants engaged in a posttreatment assessment. Cohorts whose treatment had been delayed then were randomly assigned to either CST or TSF. On completion of their treatment, these participants were again assessed. All participants received telephone assessments at 3 and 9 months following treatment completion; in-person interviews were conducted at 6 and 12 months. All assessments were conducted by research assistants who were blind to treatment assignment.
Treatment Conditions
CST
Participants in the CST condition learned to conceptualize their distress from within a family stress and coping perspective. According to this view, the participant’s depression and other distress resulted from cumulative problems brought on by the partner’s drinking and the inability of the participant’s usual ways of coping to deal with them. The group was initially introduced to (a) the stress and coping model; (b) an explanation of the relationship between thoughts, feelings, behavior, and how the consequences of behavior influenced how they felt and acted and how their partner reacted; and (c) an introduction to a problem-solving approach adapted from D’Zurilla and Goldfried (1971). Each session’s content then focused on applying this approach to certain types of problematic drinking-related situations experienced by women with partners with alcoholism (e.g., partner physical violence, effects of drinking on the family; relationship and sexual functioning problems). The situations and empirically derived scoring criteria of the Spouse Situation Inventory (SSI; Rychtarik & McGillicuddy, 1997) served as program content (see the section Proximal outcomes). For each SSI situation, the therapist led the group in problem solving and provided situation-specific skill hints. Skill hints were compiled from the components of responses judged as highly effective during SSI scale development. The therapist then modeled the recommended response, group members role-played the situation, and the therapist and group provided feedback. Participants kept a diary of personal problematic situations encountered for subsequent discussion in the group. Al-Anon attendance was not discouraged but was viewed as a problem-solving option.
TSF
Participants in the TSF condition learned to view their problem as one of codependence; the 12 steps of Al-Anon then served as a blueprint to facilitate codependence recovery. Codependence was defined as preoccupation with and extreme social, emotional, and possibly physical dependence on another person (in this case the partner with alcoholism; Wegscheider-Cruse, 1989). Participants learned the symptoms of codependency (i.e., denial, self-delusion), its consequences (e.g., low self-worth), and the 12 steps of Al-Anon. Sessions focused on Al-Anon Steps 1–5, enabling behaviors and detachment, codependency relapse, and briefly on Al-Anon Steps 6–12. To control for exposure to the SSI situations, participants in TSF were presented the same situations and in the same order as participants in CST. In TSF, however, situations were used to demonstrate and discuss issues of codependency and application of the 12 steps. Other than discussion of enabling behaviors, the therapist avoided specific instruction in effective behaviors and took the approach advocated in Al-Anon that, whereas it is helpful to share similar experiences, it can be harmful to advise another what she should do because she is the one who has to live with the results of the decision. Instead, the therapist helped participants to recognize what was manageable and unmanageable in the situations and used general advice such as “look to your Higher Power for guidance” or “focus on yourself and what you can change in the situation.” Participants were to attend Al-Anon weekly and were assigned Al-Anon reading material.
DTC
After completion of the 8-week wait period, participant cohorts were randomly assigned to receive either CST or TSF treatment identical to that above.
Therapists and Therapist Compliance
Four female, masters-level certified alcoholism or rehabilitation counselors provided the treatments. Therapists were open to both treatment approaches and received extensive instruction in each. Therapists were randomly assigned to treatment group (one per cohort) with the provision that each therapist conduct approximately equal numbers of CST and TSF groups. There was no significant difference between therapists in the proportion of clients in each treatment for whom they were responsible, χ2(3, N = 171) = 2.95, ns. To ensure fidelity of treatment administration and to avoid therapist drift, treatments were manualized, and therapists used a session checklist and materials (e.g., demonstration posters) specific to the treatment assigned. All sessions were videotaped and monitored for adherence by a clinical supervisor; weekly therapist supervision was provided. In addition, a second rater, not associated with the treatment, independently rated a random 25% sample of supervisor-scored tapes using a checklist of primary session content for each session. Supervisor-rater absolute agreement, intraclass correlation coefficients (ICCs) on percentage of primary session content items completed were .96 and .84 for CST and TSF, respectively. On average, 88% and 93% of primary session content were completed in the two respective treatment conditions. A review indicated that noncompliance typically occurred when heavier than usual discussion of client personal issues prevented the therapist from completing all material planned for a session.
Measures
The primary participant outcome measure was depression (Beck & Steer, 1993; BDI-IA range = 0–63). The BDI-IA was administered at pretreatment, posttreatment, and 6 and 12 months posttreatment. The primary partner outcome measures were percentage of days abstinent and number of standard drinks per drinking day in each follow-up month. Partner drinking data were obtained from the participant and a secondary corroborating source using the timeline-followback method (Sobell & Sobell, 1992) administered at pretreatment, posttreatment, postdelay, and at each 90-day follow-up point.3 Missing follow-up interviews were conducted, when possible, at the next interview. Abstinent days were coded as zero drinks per drinking day. To reduce skew, a square root transformation was used for participant follow-up depression and partner drinks per drinking day; an arcsine transformation was used for percentage of abstinent days.4
Secondary follow-up outcome measures of participant-reported partner functioning included incidence (0 = No; 1 = Yes) of partner help seeking (through AA or formal treatment) during the treatment, treatment-delay, and 90-day follow-up periods; and the incidence (0 = No; 1 = Yes) and frequency (inverse transformed) of physical violence in the year pretreatment and in each 6-month follow-up period, as measured by the physical violence subscale of the Conflict Tactics Scale (CTS; Straus, 1979). The total physical violence score was used because factor analytic work has found that the partner’s physical violence as reported by the female spouse loads on a single CTS violence factor, irrespective of severity (Pan, Neidig, & O’Leary, 1994).
A priori hypotheses measures
Meaning seeking was measured with a composite index of the 20-item Purpose in Life Test (PIL; Crumbaugh & Maholick, 1976) and the 20-item Seeking of Noetic Goals Scale (SONG; Crumbaugh,1977). The PIL measures the extent to which an individual has found purpose and meaning in life. The SONG is a complementary scale that measures the extent to which an individual seeks to obtain meaning and life purpose. Items on each are scored on a 1–7 scale and summed. The difference score between the SONG and the PIL (i.e., SONG – PIL) was used to define readiness for spiritual growth (Tonigan, Miller, & Connors, 2001; range = −120 to 120). High scores on this measure represent individuals who are strongly seeking meaning in life when their life is not meaningful to them. Low scores are indicative of individuals who have found meaning in life and are not actively looking for it. The measure has shown acceptable reliability and construct validity (Crumbaugh, 1977). Relationship cohesion was measured with the Dyadic Adjustment Scale’s (DAS; Spanier, 1989) Dyadic Cohesion subscale (range = 0–22). Items assess the extent to which the couple engages in outside interests together, have a stimulating exchange of ideas, work together on a project, and so forth. The Interpersonal Dependency Inventory (IDI; Hirschfeld et al. (1977) measured dependency. A total dependency score (range = −22–122) was derived from the sum of the Emotional Reliance on Another Person and Lack of Self-Confidence subscales minus the Assertion of Autonomy subscale (Bornstein, 1994; Bornstein, Rossner, & Hill, 1994).
Treatment expectancies and treatment received
Participants completed a 6-item Feelings About Your Scheduled Treatment Scale (coefficient α = .91) at the end of Session 1. On this scale, the participant rated the treatment along a 10-point scale (1 = Not at all; 10 = Extremely) with respect to its reasonableness, their confidence that it would be helpful, whether they would recommend it to others, how similar it was to that expected, the expected ease of participating, and their overall satisfaction with the treatment as scheduled. Expectancies were high, overall, but CST participants had slightly higher mean item expectancy scores (M = 8.02, SD = 1.28) than those in TSF (7.31, SD = 2.00), F(1, 34) = 4.33, p < .05, proportion of variance accounted for (PV) = .03. However, no significant effect of treatment, F(1, 32) = .23, ns, PV = .00; delayed treatment status, F(1, 32) = .09, ns, PV = .00; or Treatment × Delayed Status interaction, F(1, 32) = 2.26, ns, PV = .01, was found on percentage of sessions attended. Collapsed across delayed status condition, 77% attended 6 or more sessions; 32% attended all eight sessions.
Follow-up rates
At the end of the 8-week treatment or treatment-delay period, data were available from 96% of participants (95% CST, 93% TSF, and 100% DTC). Ninety-eight percent of DTC participants also were followed at the end of their treatment (97% CST; 100% TSF). At least one in-person follow-up assessment was conducted with 87% of participants in each treatment condition; 73% completed all posttreatment and follow-up in-person assessments. For partner drinking variables, data from at least one monthly follow-up point was available from 95% of the sample (in each treatment condition); complete follow-up partner drinking data were available from 81%. Data from the secondary, corroborating source for at least one follow-up point were available from 78% and 71% of the sample for partner percentage of days abstinent and drinks per drinking day, respectively. Among these secondary sources, 33% were friends of the participant and partner; 33% were a parent or sibling; 28% were grown children or other relatives; and 5% were other. Participant-corroborator ICCs were .64 (SD = .05) and .54 (SD = .10), for the two respective partner drinking measures.
Proximal outcomes: Skill acquisition and Al-Anon attendance
Skill acquisition during treatment was measured using the SSI (Rychtarik & McGillicuddy, 1997) administered at pretreatment and, with the alternate SSI form (to which participants had not been exposed during treatment), at the end of the treatment or treatment delay. Each SSI form consists of 24 representative alcohol-related problem-situation vignettes commonly experienced by women with partners with alcoholism (e.g., dealing with partner drunkenness, violence, and dereliction of duties). The role-played response to each situation is videotaped and scored for effectiveness on a 6-point scale (1 = Not effective at all; 6 = Extremely effective). The mean SSI situation score served as the measure of coping skillfulness. The SSI shows good levels of generalizability, alternate form reliability, and is associated negatively with partner drinking and positively with partner recognition of a problem. A rater blind to treatment condition scored all SSI responses. A second rater independently scored SSI responses from pretreatment, posttreatment, postdelay, or postdelayed treatment administrations on a random 20% sample of participants (i.e., only one administration was rated per participant). The interrater ICC for this sample combined was .92. At the end of the treatment or delay period CST participants were significantly more skillful than those in either TSF or DTC (see Table 2). The skill difference between TSF and DTC only approached the Bonferroni adjusted significance criterion (p < .10).
Table 2.
Raw Outcome Means at the End of the 8-Week Treatment or Delay Period Across Treatment Conditions
| Measure | Treatment condition
|
Overall | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CST (n = 55) | TSF (n = 58) | DTC (n = 58) | Individual comparisons
|
|||||||||||
| t(33) | t(33) | t(33) | ||||||||||||
|
| ||||||||||||||
| M | SD | M | SD | M | SD | F (2, 33) | PV | CST-TSF | PV | CST-DTC | PV | TSF-DTC | PV | |
| Coping skillfulnessa | 3.42 | .39 | 3.26 | .31 | 3.09 | .30 | 13.83**** | .15 | 2.90† | .08 | 5.26†††† | .21 | 2.23 | .05 |
| Al-Anon (days) b | .07 | .54 | 3.02 | 3.46 | .12 | .93 | 50.03**** | .80 | −8.96†††† | .74 | .38 | .00 | 9.57†††† | .75 |
| Depressionc | 9.69 | 7.13 | 7.07 | 6.20 | 12.60 | 8.33 | 7.93*** | .09 | .87 | .00 | −2.82† | .07 | −3.77†† | .12 |
| Partner PDA (%)d | 33 | 37 | 28 | 36 | 37 | 41 | .72 | .00 | ||||||
| Partner DDDe | 10.61 | 8.57 | 7.93 | 5.55 | 10.25 | 8.94 | .64 | .00 | ||||||
Note. All analyses controlled for the pretreatment value of the dependent variable and were conducted in a two-level, mixed effects model with treatment cohorts (treatment groups) nested within treatment condition. PV = proportion of variance; CST = coping skills training; TSF = 12-step facilitation; DTC = delayed treatment control; PDA = partner days abstinent; DDD = drinks per drinking day.
Skillfulness Score on the Spouse Situation Inventory (n = 52, 54, and 58 for CST, TSF, and DTC, respectively).
Days attended an Al- Anon meeting in the 50-day treatment period (n=54, 57, and 57 for CST, TSF, and DTC, respectively).
Participant Beck Depression Inventory score (n = 52, 54, and 58 for CST, TSF, and DTC, respectively). Depression scores were square root transformed for analyses.
PDA during the 50-day treatment period (n = 51, 56, and 54 for CST, TSF, and DTC, respectively). PDA data were arcsine transformed for analyses.
Partner DDD during the 50-day treatment period (n = 50, 54, and 54 for CST, TSF, and DTC, respectively). DDD data were square root transformed for analyses.
p < .001.
p < .0001.
Bonferroni-corrected p < .05.
Bonferroni-corrected p < .01.
Bonferroni-corrected p < .0001.
Self-reported Al-Anon attendance in days (inverse transformed to reduce skew) was recorded for the year pretreatment, the 8-week treatment period, and for each 90-day follow-up interval. As expected, during treatment, participants in TSF had significantly more Al-Anon days than either CST or DTC; the latter not differing from one another (see Table 2). Collapsed across delay condition, 71% attended at least one Al-Anon meeting in TSF; only 2% attended Al-Anon in CST. The low Al-Anon attendance did not change across follow-up in CST, t(158) = −.37, ns, PV = .00. However, a significant decline occurred in TSF, t(158) = −5.37, p < .0001, PV = .15. CST participants had significantly less Al-Anon attendance (M = .55, SD = 2.40) than TSF (M = 3.39, SD = 4.94), in months 1–3, t(34) = −6.33, p < .0001, PV = .22; but a smaller, yet still significant difference, between CST (M = .41, SD = 1.93) and TSF (M = 1.18, SD = 2.93) existed at months 9–12, t(34) = −2.24, p < .05, PV = .04.
Data Analysis Plan
End-of-treatment or treatment-delay comparisons
Differences between conditions at the end of the treatment or delay period were examined in a two-level mixed effects model with treatment condition as a fixed effect, cohort as a random effect (nested within treatment condition), and person as a random effect (nested within cohort and treatment). The pretreatment value of the dependent variable served as a covariate. Participant employment stability also was covaried in these analyses because of pretreatment differences between conditions on this variable. Significant treatment condition effects were probed with two-tailed, pairwise multiple comparison t tests on adjusted least square means using the Bonferroni correction for the three contrasts (i.e., p < .05/3). Pretreatment to posttreatment change patterns in participant and partner primary outcome variables were examined using three-level mixed effects models with time period as a random effect nested within participant, participant as a random effect nested within cohort, and cohort as a random effect nested within treatment. All CST-TSF comparisons were repeated in DTC once treated. Results of the latter analyses mirrored CST-TSF findings among those without a treatment delay and are not reported here. To test whether differences in skill level and Al-Anon attendance mediated observed treatment effects, we first tested the association of each with the primary outcome measures on which significant treatment effects occurred. If significant, outcome analyses were repeated controlling for pretreatment and end-of-treatment or delay skill level and Al-Anon attendance, respectively. Mediation was considered present if, in these models, the treatment effect was reduced or no longer significant and the proximal outcome measure continued to predict outcome (Judd & Kenny, 1981).
Follow-up analyses
Preliminary analyses included treatment delay status (0 = Not delayed; 1 = Delayed) as a variable in the model with cohorts then nested within delayed status and treatment condition. In no case was inclusion of this variable found to influence the results. Thus, follow-up analyses collapsed across treatment delay status.5 Analyses of main effects for treatment, follow-up period (time), and the Treatment × Time interaction used a three-level, mixed effects model that assumed a random intercept and random linear time effects. Time was treated as a continuous variable centered at the midpoint of the follow-up period. Unless noted otherwise, analyses of participant functioning and partner violence measures used two time periods (i.e., 6-month, and 12-month follow-ups); analyses of partner drinking variables, for which monthly data were available, included 12 monthly follow-up periods. Pretreatment-to-follow-up change analyses and follow-up a priori and exploratory Attribute × Treatment Interaction effects also were examined in three-level mixed effects models. The latter models included the baseline dependent variable, the standardized client attribute (e.g., interpersonal dependence), treatment, time, and the Attribute × Treatment, Attribute × Time, Treatment × Time, and Attribute × Treatment × Time interactions. Significant interactions were probed by testing the slope of the moderating attribute-dependent measure relationship within each treatment condition using two-tailed, multiple comparison t tests, Bonferroni-corrected for the number of slopes or slope contrasts tested. All results reported are from final reduced models in which variance components accounting for 0% of the variance and nonsignificant, higher order interaction terms are eliminated. Study analyses were conducted using SAS PROC MIXED and, for point prevalence data, the PROC MIXED GLIMMIX macro (Littell, Milliken, Stroup, & Wolfinger, 1996). The Kenward and Rodgers (1997) method was used to provide estimated standard errors and associated F and t values. The denominator degrees of freedom (ddfs) used to obtain p values were calculated directly on the basis of the final reduced model used.6 Effect sizes are presented in the form of PV. For continuous measures, PV values were calculated using procedures outlined by Snijders and Bosker (1999).7 To obtain PV for effects within individual treatment condition, simple effects modeling was used. At the end of the treatment or delay period, effect sizes of mean differences between treatment condition pairs were calculated by computing the standard deviation from the standard error estimates: SD = SE X (sqrt[n]), computing the number of standard deviation units between estimated least square means and converting this to PV according to Cohen (1988). For point prevalence measures, effect sizes are computed from differences between estimated proportions in the GLIMMIX models using methods outlined by Cohen and then converted to the PV scale. PVs of .01, .06, and .14 are comparable to small, medium, and large effects, respectively, as defined by Cohen. All analyses used the intent-to-treat sample.
Results
What Were the Effects of Treatment on Participant Depression?
At the end of the treatment or delay period, depression was significantly less in CST and TSF relative to DTC; CST and TSF did not differ from one another (see Table 2). Analyses of change from pretreatment-to-end of treatment or delay indicated a significant Treatment × Time interaction, F(1, 34) = 14.03, p < .001, PV = .14, with a large decline in depressive symptoms among those treated, t(34) = −7.20, p < .0001, PV = .24, but no significant change in those yet to be treated, t(34) = −0.63, ns, PV = .00. Following treatment, participants in DTC also showed a large and significant improvement in depressive symptoms, F(1, 11) = 11.34, p < .01, PV = .23.
During follow-up, CST and TSF also did not differ significantly in depressive symptomatology (see Table 3). Nevertheless, depression at the 12 month follow-up continued to be significantly lower than at pretreatment, F(1, 35) = 74.37, p < .0001, PV = .28. Mean pretreatment and 12-month follow-up depression levels for participants with complete follow-up data were 13.19 (SD = 8.14) and 7.88 (SD = 7.98), respectively. This change appeared to be clinically significant. At pretreatment, 38%, 27%, 32%, and 3% of the sample fell, respectively, within minimal (0–9), mild (10–16), moderate (17–29), and severe (30–63) BDI-IA diagnostic levels (score ranges). At the end of the follow-up period, 68%, 20%, 8%, and 4% were so classified, respectively.
Table 3.
Primary and Seconday Participant and Partner Follow-Up Outcomes and Summary Mulitlevel Analysis Results
| Outcome measure | n | Coping skills training | 12-step facilitation | Treatment | Time | Treatment X Time | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| M | SD | M | SD | F(dfs) | PV | F(dfs) | PV | F (dfs) | PV | ||
| Primary | |||||||||||
| Depressiona | 149 | 8.01 | 8 | 8.51 | 7.35 | .04 (1, 34) | .00 | .63 (1, 34) | .00 | 2.20 (1, 34) | .01 |
| Partner PDAb | 162 | 38 | 37 | 35 | 35 | .04 (1, 34) | .00 | 5.04 (1, 123) * | .01 | .96 (1, 123) | .00 |
| Partner DDDb | 160 | 7.15 | 6.11 | 6.70 | 4.97 | .00 (1, 155) | .00 | 2.41 (1, 155) | .00 | 3.81 (1, 155)† | .01 |
| Secondary | |||||||||||
| Partner treatment status (%)c | 162 | 14.73 | 1.42 | 11.44 | 2.31 | .92 (1, 159) | .00 | .19 (1, 158) | .00 | .42 (1, 157) | .00 |
| Partner violence(%)d | 149 | 21.19 | 0.88 | 31.16 | 2.17 | 4.83 (1, 146)* | .03 | .00 (1,34) | .00 | .84 (1, 34) | .01 |
| Partner violence intensitye | 162 | 4.47 | 20.14 | 2.22 | 6.26 | 2.19 (1, 146) | .01 | .28 (1, 145) | .00 | .85 (1, 144) | .00 |
Note. Means are untransformed and represent the average of (a) two 6-month intervals for depression, and violence meesaures; (b) twelve monthly intervals for percentage of partner days abstinent (PDA) and drinks per drinking day (DDD); and (c) four 90-day intervals for treatment status. Unless otherwise noted, F tests are results of reduced three-level mixed effect models: cohorts nested witin treatment; participants nested within cohort and treatment, and time; and assumed random intercept and linear time slopes. In cases where variance accounted for by both intercept and time at the cohort level was zero, the analysis used a two-level model (collapsed across cohort). Three-level models are denoted by denominator ddf = 34 for the treatment effect and, when variance accounted for by time at the cohort level was greater than zero, the time and Treatment X Time interaction effects. A backward elimination procedure was used (i.e., sequential elimination of nonsignificant Treatment X Time and time terms, respectively). F tests reported for treatment and time effects are those obtained after prior nonsignificant effects are eliminated from the model. All analyses controlled for the pretreatment value of the dependent variable and, except for prevalence measures, used transformed variables. PV = proportion of variance.
Participant Beck Depression Inventory.
From the timeline follow-back method.
Percentage of partners receiving either formal treatment, attending self-help groups, or both.
Percentage reporting partner physical violence on the the Conflict Tactics Scale. This analysis assumed a fixed time effect at the individual level; inclusion of a random time effect did not converge.
Conflict Tactics Scale Physical Violence subscale score.
p < .05.
p < .10.
What Were the Effects of the Treatments on Partner Drinking?
No differences between treatment conditions in partner drinking were observed during the treatment or delay period (see Table 2). When conditions were combined (after DTC participants had received treatment), only a relatively small respective increase and decrease in percentage of days abstinent, F(1, 35) = 3.73, p = .061, PV = .02, and drinks per drinking day, F(1, 35) = 11.32, p < .01, PV = .02, occurred from the 8 weeks before treatment to the 8-week treatment period.
During follow-up, no significant effects of treatment were observed on partner drinking (See Table 3). A Treatment × Time interaction on partner drinks per drinking day approached significance (p = .0527). This interaction suggested that drinks per drinking day declined across follow-up to a relatively small but significant degree in CST, t(155) = −2.46, p < .05, PV = .03, but not in TSF, t(155) = 0.28, ns, PV = .00. Despite the lack of treatment differences, participants reported a moderate significant increase in partner percentage of days abstinent from pretreatment (raw M = 26, SD = 30) to the end of the 12-month follow-up (raw M = 41, SD = 41), F(1, 35) = 19.22, p < .0001, PV = .07. Similarly, participants reported a large significant decrease in partner drinks per drinking day from the year pretreatment (raw M = 10.02, SD = 6.88) to the last month of the follow-up period (raw M = 6.63, SD = 6.90), F(1, 35) = 32.01, p < .0001, PV = .21.
Did Changes in Proximal Skill Level and Al-Anon Attendance Account for Treatment Effects Observed on Participant Depression and Partner Drinking?
Both posttreatment skill level, t(124) = −3.23, p < .01, PV = .05, and within treatment Al-Anon attendance, t(124) = −2.84, p < .05, PV = .05, alone had significant negative associations with end-of-treatment depression. Controlling for treatment condition differences in skill, the prior difference in depression observed between CST and DTC was no longer significant, t(34) = −1.60, ns, PV = .00, but skill level continued to contribute significantly to the model F (1,125) = 5.74, p < .05—indicative of a mediation effect. TSF and DTC, however, still differed significantly, t(33) = −3.14, p < .01, PV = .09; CST and TSF were still not different from one another, t(33) = 1.34, ns, PV = .01. Controlling for Al-Anon attendance differences, the prior difference in depression between TSF and DTC only approached the corrected significance level, t(33) = −2.32, p = .072, PV = .06, but Al-Anon also did not contribute significantly to the full model, F (1, 125) = .51, ns, suggesting little or no mediation effect. CST and DTC were still significantly different from one another, t(33) = −2.81, p < .05, PV = .07; the CST-TSF difference remained nonsignificant, t(33) = 0.22, ns, PV = .00. Overall, relative to DTC, differences in skill level appeared to mediate end-of-treatment improvement in depression in CST; differences in Al-Anon attendance did not appear to mediate improvement in TSF.
In follow-up, end of treatment skill level continued to have a significant negative association with participant depression, F(1, 123) = 4.29, p < .05, PV = .03, but did not vary with treatment, time, or Treatment × Time. For partner drinking variables, skill level had no main or interactive effect with time on percentage of days abstinent. A significant Treatment × Skill Level interaction did emerge for drinks per drinking day, F(1, 149) = 7.06, p < .01, PV = .03. Skill level had a negative association with drinks per drinking day in CST, which approached the Bonferonni-corrected significance level, t(151) = −2.07, p < .07, PV = .03, but not in TSF, t(151) = 1.54, ns, PV = .01. Al-Anon attendance within treatment was not associated with any primary outcome measure during follow-up. Furthermore, follow-up Al-Anon attendance in TSF was not associated with follow-up depression, F(1, 72) = .00, ns, PV = .00, partner percentage of days abstinent, F(1, 79) = 1.32, ns, PV = .01, or partner drinks per drinking day, F(1, 77) = .14, ns, PV = .00, and these effects did not vary with time.
What Were Treatment Effects on Partner Help Seeking and Physical Violence?
The percentage of partners seeking help during any one 6-month follow-up period did not differ between treatments (see Table 3), nor did the percentage of partners seeking help at any time during the 12-month follow-up differ between CST (34%) and TSF (27%), F(1, 34) = .99, ns, PV = .00. With respect to violence, CST participants reported a significantly lower incidence of partner physical violence per 6-month follow-up period (see Table 3).8 Similarly, among those with full follow-up data, analysis of pretreatment-to-follow-up change in the prevalence of violence found a Treatment × Time interaction, F(1, 34) = 9.14, p < .01. CST declined significantly from 50% to 37%, t(124) = −2.74, p < .05, PV = .14; but TSF showed a nonsignificant increase from 44% to 51%, t(124) = 1.50, ns, PV = .05. Notably, among those experiencing violence at pretreatment, 63% experienced violence during follow-up in CST, whereas 85% of those in TSF did.
Did Meaning Seeking, Couple Cohesion, Interpersonal Dependency, or History of Partner Physical Violence Moderate Treatment Effects on Participant Depression and Partner Drinking?
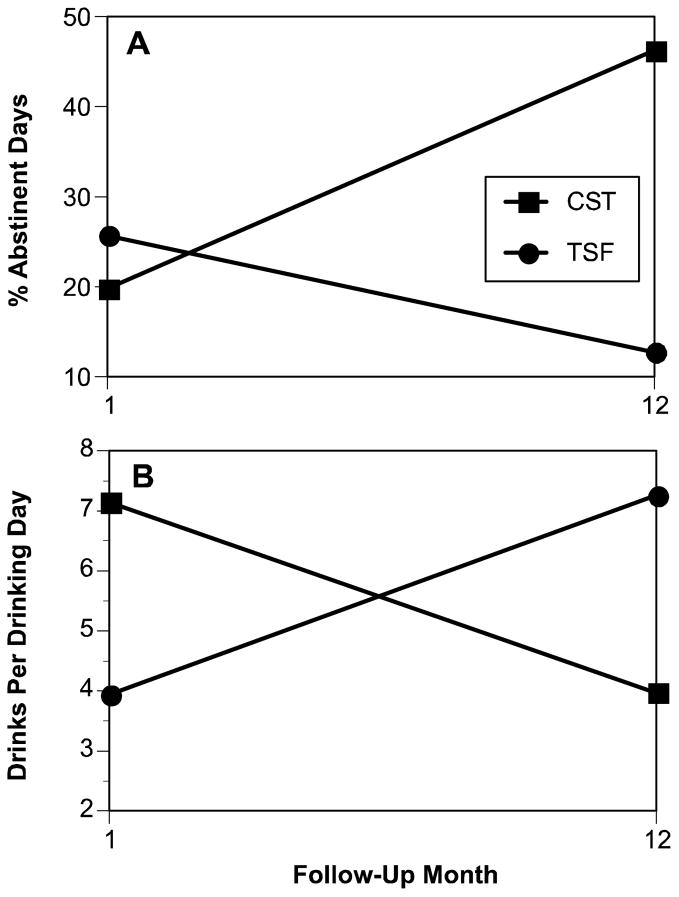
Results of Attribute × Treatment interaction analyses are presented in Table 4. No support was found for any a priori hypothesis. With respect to relationship violence, the incidence of partner violence in the pretreatment year did not moderate the effects of treatments on depression. However, a significant Violence History × Treatment × Time interaction was found for both percentage of abstinent days and drinks per drinking day. Specifically, a significant Treatment × Time interaction occurred in the violent but not the nonviolent group for each drinking measure. In the violent group, a significant increase in abstinent days from the beginning to the end of the 12-month follow-up occurred in CST, whereas no significant time slope was observed in TSF (see Figure 1). Probing indicated no significant treatment difference at the first follow-up month, t(153) = −0.06, ns, but by Month 12, there was a significant difference between conditions, t(153) = 3.09, p < .01, with CST reporting a higher percentage of days abstinent than TSF. For drinks per drinking day, a negative association between time and drinks per drinking day occurred in CST, whereas a significant positive association occurred in TSF. Mean treatment differences at follow-up Month 1 were significant, t(153) = 2.35, p < .05, with greater drinking intensity in CST than TSF. By Month 12 of the follow-up, the pattern is reversed with CST having less drinking intensity than TSF, t(153) = −2.20, p < .05. Treatment expectancies, attendance, posttreatment SSI skillfulness, days separated, Al-Anon attendance, and partner help seeking were not differentially associated with partner violence history in the two treatments and could not account for the interaction effects observed.
Table 4.
Summary of Tests of a Priori and Exploratory Attribute X Treatment Interactions for Primary Dependent Measures
| Attribute | n | F | t | df(s) | PV |
|---|---|---|---|---|---|
| A priori | |||||
| Meaning seekinga | |||||
| Depression | |||||
| Attribute X Treatment | 148 | 0.98 | 1, 108 | .01 | |
| Attribute X Treatment X Time | 148 | 0.01 | 1, 105 | .00 | |
| Partner PDA | |||||
| Attribute X Treatment | 161 | 0.02 | 1, 121 | .00 | |
| Attribute X Treatment X Time | 161 | 1.46 | 1, 118 | .00 | |
| Partner DDD | |||||
| Attribute X Treatment | 159 | 1.19 | 1, 153 | .01 | |
| Attribute X Treatment X Time | 159 | 0.14 | 1, 150 | .01 | |
| Couple cohesionb | |||||
| Depression | |||||
| Attribute X Treatment | 147 | 0.19 | 1, 107 | .00 | |
| Attribute X Treatment X Time | 147 | 0.03 | 1, 104 | .00 | |
| Partner PDA | |||||
| Attribute X Treatment | 160 | 0.01 | 1, 120 | .00 | |
| Attribute X Treatment X Time | 160 | 1.77 | 1, 117 | .00 | |
| Partner DDD | |||||
| Attribute X Treatment | 158 | 0.69 | 1, 150 | .01 | |
| Attribute X Treatment X Time | 158 | 0.84 | 1, 149 | .01 | |
| Dependencyc | |||||
| Depression | |||||
| Attribute X Treatment | 148 | 0.50 | 1, 108 | .00 | |
| Attribute X Treatment X Time | 148 | 1.30 | 1, 105 | .00 | |
| Partner PDA | |||||
| Attribute X Treatment | 161 | 0.31 | 1, 121 | .00 | |
| Attribute X Treatment X Time | 161 | 0.98 | 1, 118 | .00 | |
| Partner DDD | |||||
| Attribute X Treatment | 159 | 2.45 | 1, 151 | .02 | |
| Attribute X Treatment X Time | 159 | 0.72 | 1, 150 | .01 | |
|
| |||||
| Exploratory | |||||
| Partner violenced | |||||
| Depression | |||||
| Attribute X Treatment | 149 | 0.76 | 1, 109 | .00 | |
| Attribute X Treatment X Time | 1.23 | 1, 106 | .00 | ||
| Partner PDA | |||||
| Attribute X Treatment | 162 | 2.78 | 1, 119 | -- | |
| Attribute X Treatment X Time | 11.28** | 1, 119 | .02 | ||
| Treatment X Time (nonviolent)e | −1.56 | 119 | .00 | ||
| Treatment X Time (violent) e | 3.15** | 119 | .02 | ||
| Time slope (CST) f | 3.04** | 119 | .06 | ||
| Time slope (TSF) f | −1.43 | 119 | .01 | ||
| Partner DDD | |||||
| Attribute X Treatment | 160 | 0.05 | 1, 151 | -- | |
| Attribute X Treatment X Time | 10.54** | 1, 151 | .01 | ||
| Treatment X Time (nonviolent)e | .69 | 151 | .00 | ||
| Treatment X Time (violent) e | −3.81** | 151 | .06 | ||
| Time slope (CST) f | −2.58* | 151 | .07 | ||
| Time slope (TSF) f | 2.81* | 151 | .06 | ||
Note. F and t values have been calculated using the Kenward-Rodgers method. Degrees of freedom have been calculated manually on the basis of the model. PV = proportion of variance, PDA = percentage of days abstinent. DDD = drinks per drinking day. CST = coping skills training; TSF = 12-step facilitation.
Measure derived from subtracting the Purpose in Life Scale from the Seeking of Noetic Goals Scale.
Cohesion subscale from the Dyadic Adjustment Scale.
Total Interpersonal Dependency score of the Interpersonal Dependency Inventory.
Incidence of pretreatment partner physical violence toward the participant as measured by the Conflict Tactics Scale.
Multiple comparison t test of the Treatment X Time interaction at the indicated attribute level; comparison used a Bonferroni-corrected .05 level of significant of p < .025.
Multiple comparison t test of the treatment condition’s time slopes within each treatment at the attribute level in which the Treatment X Time interaction was significant; comparison used a Bonferroni-corrected .05 level of significance of p < .025.
p < .05.
P < .01.
Figure 1.
Interaction between treatment condition and time on partner (A) percentage of days abstinent and (B) drinks per drinking day in women experiencing pretreatment partner physical violence. Data points are predicted adjusted arcsine least square means (for percentage of abstinent days) and square root least square means (for drinks per drinking day), which have been transformed back to percentage and standard drink units, respectively. CST = coping skills training; TSF = 12-step facilitation.
Having identified differences between treatments in the incidence of violence during follow-up and, in the violent group, the rate of change in abstinent days and drinking intensity across follow-up, we explored the proximal relationship and change in relationship between drinking and violence in the follow-up year. These analyses were driven by converging evidence that alcohol use appears to facilitate relationship violence, at least in certain marital relationships (Fals-Stewart, 2003), and questions about whether this drinking-violence relationship had been affected differentially by treatment condition in the present study. For these analyses, average monthly percentage of days abstinent and drinks per drinking day in each of the two 6-month periods of follow-up (for which violence data were available) were included (along with all possible interactions) as a time-varying parameter in respective models of follow-up partner violence prevalence. Consistent with the literature, the percentage of days abstinent was negatively related to the incidence of violence during follow-up, F(1, 141) = 17.01, p < .001, PV = .16, and did not vary by treatment, violence group, or time. For drinks per drinking day, however, a significant Treatment × Drinks Per Drinking Day interaction emerged, F(1, 133) = 5.23, p < .05. Probing indicated that, whereas the incidence of violence was low at low levels of drinking for both conditions, as drinking intensity increased there was a significant increase in the incidence of violence in TSF, t(133) = 3.29, p < .01, PV = .58., but not CST, t(133) = 0.51, ns, PV = .02. Participation in CST appeared to buffer the effects of drinking intensity on the incidence of violence during follow-up, whereas TSF did not.
Discussion
The stress and coping model of functioning in spouses of persons with alcoholism posits that more effective skills in coping with problems arising from the partner’s drinking will result in better functioning in the spouse and, indirectly, in the partner with alcoholism. We found support for this notion in that higher skill level was associated with less depression and, at least in CST (where posttreatment skill level was higher), a tendency for less drinking intensity in the partner. Moreover, CST’s effect relative to no treatment was mediated by skill differences across conditions. Still, skill level differences between CST and TSF did not translate into main differences between these treatments in either participant depression or partner drinking, even though moderate to large reductions in both outcome measures occurred from pretreatment to follow-up. The results suggest that, although coping skill level may be an important pathway to improving spouse functioning, as defined here it is not the only avenue to change. Al-Anon attendance, at least during treatment, did not appear to mediate differences in participant depression between TSF and DTC. Other factors, not measured, may be active in initiating and maintaining change in TSF. In fact, Al-Anon itself can be conceptualized as training certain cognitive coping skills such as recognizing that one cannot control the partner’s drinking, relying on a higher power, and so forth. These skills, not measured in the current study, may have been avenues for change observed in TSF. Furthermore, the effects of coping skillfulness were modest at best, suggesting that other mediating factors may be present in CST as well. Future research may benefit from assessing and, in the case of CST, evaluating whether cognitive changes in both 12-step and coping skill interventions mediate the maintenance of change in depressive symptoms.
A notable finding was that CST reduced the incidence of partner relationship violence; TSF did not. Instead of being excluded from skill training interventions, women who experience partner violence may particularly benefit from them. Not only was the incidence of partner physical violence reduced in CST, but violent partners’ drinking was reduced over time as well. Moreover, CST appeared to, at least partially, break the proximal association between drinking and violence, whereas TSF did not. The mechanisms accounting for these treatment differences are not clear. Reflecting differences in the two general approaches, CST incorporated some specific training in dealing with partner violence, whereas TSF did not. Moreover, CST participants were trained to avoid engaging in violent behaviors (e.g., slapping, hitting partner) as a coping mechanism. Unfortunately, we only collected violence data on the partner, but in response to a single question at pretreatment, 59% of participants indicated that they themselves had been violent toward their partner. It may be that a reduction in the woman’s own violence toward the partner itself contributed to a reduction in the incidence of partner violence. Integrating negative affect and self-regulation models of abusive drinking (e.g., Sher, Trull, Bartholow, & Vieth, 1999) and marital discord (e.g., Bradbury, Cohan, & Karney, 1998), we speculate that the greater reduction in the incidence of violence in CST relative to TSF may (over time) reduce the level of tension and negative affect in the violent relationship and in the partner himself. A greater reduction in the partner’s negative affect in CST relative to TSF may then account for the reduction in the frequency and intensity of his drinking. Additional research exploring the nature of these complex relationships is needed.
On a cautionary note, whereas drinking intensity was greater in TSF than CST among violent partners by the end of the follow-up period, the reverse was true early in follow-up. It may be that, when drinking, partners of those in CST drank heavier initially, relative to those in the TSF condition, in response to the change in contingencies placed on their drinking behavior (as in a classical extinction paradigm). We further caution that these findings with respect to partner violence may not be applicable to all violent relationships affected by alcohol nor to all types of violent partners with alcoholism. Future research is needed in this area.
To ensure safety, privacy, and recruitment of a representative sample, participants were not required to tell or involve their partner. In fact, many, if not most, participants chose not to tell the partner of their participation, and follow-up assessments were conducted discretely. In the absence of drinking reports directly from the partner, we relied on the woman’s report as a surrogate. Research has generally found fair-to-good correspondence between the drinking reports of significant others and the reports of persons with alcoholism (Connors & Maisto, 2003), with better correspondence occurring when the significant other is a spouse or live-in intimate partner (Sobell, Agrawal, & Sobell, 1997). Babor, Steinberg, Anton, and Del Boca (2000) found that drinking outcome results of analyses using significant other reports corresponded well to those using reports of the persons with alcoholism. Such research, however, has focused on treatment populations or populations in which the report of the person with alcoholism also is available. Little is known about the validity of spouse or intimate reports when the person with alcoholism is not in treatment and not available. In the current study, to place more confidence in the woman’s report, we obtained independent corroboration from a second surrogate. Agreement between participants and these second surrogates was moderate-to-good. Still, little is known about such secondary surrogate reports, and agreement between surrogates does not necessarily mean that the reports are valid. Further research is needed on factors affecting surrogate drinking measures, and in adjusting for potential measurement error in mixed effects models when surrogate reports are used. We also relied on participant reports of their partner’s relationship violence, but we consider reports of partner physical violence to be based on dyadic behavior about which the spouse has direct knowledge.
We also should note that TSF was a structured, professionally administered 12-step treatment that encouraged Al-Anon engagement; our findings cannot extend to Al-Anon participation alone. Similarly, for methodological reasons focused on the evaluation of the skill training program, TSF presented the 12-steps and related concepts within the context of the SSI situations. Expert 12-step consultants who reviewed the TSF manual prior to the study viewed this situational approach as a strength. Yet it is different from typical 12-step approaches and may limit generalizations. Our findings also may not extend to the smaller population of individuals with female or same-gender partners with alcoholism. Moreover, we found the treatments to be administered as planned, but we did not formally assess whether the treatments were actually differentiable in their defining characteristics and implementation (see Carroll et al., 1998). Still, proximal treatment outcomes were treatment specific and provide strong treatment discriminability support. We also relied here on depressive symptoms as the sole measure of participant distress, in large part because of the high degree of overlap between depression and other negative affect measures (e.g., anxiety). Recent advances in the measurement of negative affect, however, appear to more clearly discriminate between depression, anxiety, and general stress (Lovibond & Lovibond, 1995) and may be most applicable for future research with this population. Methodologically, our use of the treatment group as the unit of randomization may also have reduced statistical power—particularly in the more complex exploratory analyses.
Finally, we did not find treatment differences in partner help seeking, as has been reported elsewhere (e.g., Miller et al., 1999). However, study differences (e.g., in treatment focus [spouse functioning vs. partner treatment engagement], populations, treatment length [8 weeks vs. 6 months], and modality [group vs. individual]) make comparisons difficult.
To summarize, CST and TSF were equally effective in reducing depressive symptomatology in women whose partner has alcoholism. Drinking in the partner also was significantly reduced from pretreatment to follow-up. The results suggest that potentially important health benefits resulted for both the woman and the partner with alcoholism. However, CST may be particularly useful for those with physically violent partners both with respect to reducing the incidence of partner relationship violence and partner drinking. The behaviors targeted by each treatment appear to be independent of one another and, in the case of CST, important in the initiation of change, at least with respect to the woman’s depression. Researchers should replicate these findings, extend assessment of coping skills to the cognitive arena, assess other negative affect outcomes, conduct detailed analyses of relationship violence, study combined CST and TSF approaches, and evaluate their relative efficacy in other populations of individuals experiencing distress from a partner’s substance abuse.
Acknowledgments
This research was funded by National Institute on Alcohol Abuse and Alcoholism Grant AA07712. We appreciate the helpful advice we received from George Milliken and George Papandonatos regarding the analytic plan and the data analyses, and we thank Joan Duquette for her assistance drafting the coping skills training and 12-step facilitation treatment manuals and the staff of Hazelden Foundation, especially to Patricia Owen, who reviewed and provided helpful feedback regarding the 12-step facilitation manual. We also thank the talented therapists and research staff who worked on this project.
Footnotes
A second design factor, Spouse Situation Inventory (SSI) form (Rychtarik & McGillicuddy, 1997; see the Proximal outcome section) to which cohorts were randomized and on which they were initially assessed and exposed during treatment, also was included in the design. However, preliminary analyses found no significant SSI form or SSI Form × Treatment interaction in any analyses. Thus, to simplify analyses and reporting, the current report collapses across the SSI form factor.
The procedure worked as follows. Within the SSI form factor (see Footnote 1), the first cohort in each consecutive set of three cohorts was randomly assigned to one of the three treatment conditions. The second cohort in the set was randomly assigned to one of the two treatment conditions not yet assigned. The third cohort in the set was assigned to the remaining treatment condition. This process then was repeated within each consecutive set of three cohort pairs. Randomization of a cohort to treatment condition only occurred when the cohort was full and all participants had completed the pretreatment assessment. This randomization procedure controlled for potential confounding because of seasonal differences in treatment populations, treatment condition sequence, and staff changes. The design also allowed for treatment to occur within a controlled, closed group format. The design had the limitation that once treatment assignments had been made in the first two cohorts, the assignment of treatment condition in the third cohort of the set was known. However, treatment and research staff were kept blind to the randomization plan. Moreover, after a series of cohorts had been assigned, staff lost track of the sequencing of treatments and essentially remained blind to the next treatment condition.
We also collected participant and corroborating timeline reports of the participant’s drinking but, because screening procedures eliminated participants with a drinking problem, these data showed low levels of drinking and are not reported here.
Three participants reported pretreatment or follow-up levels of monthly partner drinks per drinking day that, although clinically feasible, were determined to be distribution outliers using the Generalized Extreme Studentized Deviate Many-Outlier Procedure discussed in Iglewicz and Hoaglin (1993). To further reduce distributional skew and the potential influence of these outliers on study findings, we used the procedure discussed in Tabachnik and Fidell (2001) whereby the lowest outlier raw score was assigned a level one unit larger than the next most extreme (but nonoutlier) raw score in the distribution, the next highest outlier was assigned a score two units larger, and the highest outlier was assigned a score three units larger. This procedure further improved skew on these measures, but the primary results of analyses with these accommodations did not vary from those conducted either without the accommodations or without the outliers.
The pooling of data across delay status condition eliminated pretreatment differences on employment stability.
The Kenward-Rodgers (KR) method for computing standard errors of estimators and ddfs has been found to reduce Type I error rates relative to other procedures (Schaalje, McBride, & Fellingham, 2001). However, in complex covariance structures the KR method may still produce inflated Type I error rates and estimates of ddfs may not accurately portray those in the model. Hence, to further reduce Type I error, we manually calculated ddfs on the basis of the nested model used and as recommended by Murray and Wolfinger (1994). We subsequently used these ddfs to obtain significance values of F and t statistics produced by the KR method. The nested design yields ddfs of 33 and 34 at the cohort level in within treatment and follow-up analyses, respectively (i.e., p [q−1], where p equals the number of treatment conditions and q equals the number of cohorts per condition). At the individual level, ddfs are computed with the following formula: N − [p (q−1)] −r −1 where N equals the total sample size in the analysis and r equals the number of terms in the model.
For analyses involving random time slopes, variances in outcome can vary somewhat over time. To simplify the reporting of effect sizes here, we report the highest effect size occurring among the follow-up points. Effect sizes are not reported for lower order effects in models where a higher order interaction involving the effect is significant.
Analyses of the prevalence of partner physical violence did not converge when a random linear time effect was included at the individual subject level (possibly because we had only two time points). As a result, all analyses of partner violence prevalence assumed a fixed time effect at the individual (but not the cohort) level.
References
- Babor TF, de la Fuente WB, JR, Saunders J, Grant M. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1989. [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Barber JG, Gilbertson R. An experimental study of brief unilateral intervention for the partners of heavy drinkers. Research on Social Work Practice. 1996;6:325–336. [Google Scholar]
- Beck AT, Steer RA. BDI: Beck Depression Inventory Manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Bornstein RF. Construct validity of the Interpersonal Dependency Inventory: 1977–1992. Journal of Personality Disorders. 1994;1:64–76. [Google Scholar]
- Bornstein RF, Rossner SC, Hill EL. Retest reliability of scores on objective and projective measures of dependency: Relationship to life events and intertest interval. Journal of Personality Assessment. 1994;62:398–415. doi: 10.1207/s15327752jpa6203_2. [DOI] [PubMed] [Google Scholar]
- Bradbury TN, Cohan CL, Karney BR. Optimizing longitudinal research for understanding the preventing marital dysfunction. In: Bradbury TN, editor. The developmental course of marital dysfunction. Cambridge, United Kingdom: Cambridge University Press; 1998. pp. 279–311. [Google Scholar]
- Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Kadden RR, Longabaugh RL, Rounsaville BJ, Wirtz PW, Zweben A. Internal validity of Project MATCH treatments: Discriminability and integrity. Journal of Consulting and Clinical Psychology. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Connors GJ, Maisto SA. Drinking reports from collateral individuals. Addiction. 2003;98(Suppl 2):21–29. doi: 10.1046/j.1359-6357.2003.00585.x. [DOI] [PubMed] [Google Scholar]
- Crumbaugh JC. The Seeking of Noetic Goals Test (SONG): A complementary scale to the Purpose In Life Test (PIL) Journal of Clinical Psychology. 1977;33:900–907. doi: 10.1002/1097-4679(197707)33:3<900::aid-jclp2270330362>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Crumbaugh J, Maholick L. Purpose In Life Test. Murfreesboro, TN: Psychological Affiliates; 1976. [Google Scholar]
- Dittrich JE, Trapold MA. A treatment program for wives of alcoholics: An evaluation. Bulletin of the Society of Psychologists in Addictive Behaviors. 1984;3:91–102. [Google Scholar]
- D’Zurilla TJ, Goldfried MR. Problem solving and behavior modification. Journal of Abnormal Psychology. 1971;78:107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart WS. The occurrence of partner physical aggression on days of alcohol consumption: A longitudinal diary study. Journal of Consulting and Clinical Psychology. 2003;71:41–52. doi: 10.1037//0022-006x.71.1.41. [DOI] [PubMed] [Google Scholar]
- Gondolf EW, Foster RA. Wife assault among VA alcohol rehabilitation patients. Hospital and Community Psychiatry. 1991;42:74–79. doi: 10.1176/ps.42.1.74. [DOI] [PubMed] [Google Scholar]
- Halford WK, Price J, Kelly AB, Bouma R, Young RM. Helping the female partners of men abusing alcohol: A comparison of three treatments. Addiction. 2001;96:1497–1508. doi: 10.1046/j.1360-0443.2001.9610149713.x. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Klerman GL, Gouch HG, Barre J, Korchin SJ, Chordoff P. A measure of interpersonal dependency. Journal of Personality Assessment. 1977;41:610–618. doi: 10.1207/s15327752jpa4106_6. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Speilberger CD. Family stress: Integrating theory and measurement. Journal of Family Psychology. 1992;6:99–112. [Google Scholar]
- Hollingshead AB, Redlich FC. Social class and mental illness: A community study. New York: Wiley; 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglewicz B, Hoaglin DG. How to detect and handle outliers. Milwaukee, WI: Quality Press; 1993. [Google Scholar]
- Johnson VE. Intervention: How to help those who don’t want help. Minneapolis, MN: Johnson Institute; 1986. [Google Scholar]
- Judd CM, Kenny DA. Process analysis: Estimating mediation in treatment evaluations. Evaluation Review. 1981;5:602–619. [Google Scholar]
- Kenward MG, Rodgers JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation of Australia; 1995. [Google Scholar]
- Miller WR, Meyers RJ, Tonigan JS. Engaging the unmotivated in treatment for alcohol problems: A comparison of three strategies for intervention through family members. Journal of Consulting and Clinical Psychology. 1999;67:688–697. doi: 10.1037//0022-006x.67.5.688. [DOI] [PubMed] [Google Scholar]
- Moos RH, Finney JW, Cronkite RC. Alcoholism treatment: Context, process, and outcome. New York: Oxford University Press; 1990. [Google Scholar]
- Moos RH, Finney JW, Gamble W. The process of recovery from alcoholism: II. Comparing spouses of alcoholic patients and matched community controls. Journal of Studies on Alcohol. 1982;43:888–909. doi: 10.15288/jsa.1982.43.888. [DOI] [PubMed] [Google Scholar]
- Murray DM, Wolfinger RD. Analysis issues in the evaluation of community trials: Progress toward solutions in SAS/STAT MIXED [Special issue] Journal of Community Psychology. 1994:140–154. [Google Scholar]
- Orford J. Coping with disorder in the family. London: Croom Helm; 1986. [Google Scholar]
- Orford J, Guthrie S, Nicholls P, Oppenheimer E, Egert S, Hensman C. Self-reported coping behavior of wives of alcoholics and its associations with drinking outcome. Journal of Studies on Alcohol. 1975;36:1254–1267. doi: 10.15288/jsa.1975.36.1254. [DOI] [PubMed] [Google Scholar]
- Pan HS, Neidig PH, O’Leary KD. Male-female and aggressor-victim differences in the factor structure of the modified Conflict Tactics Scales. Journal of Interpersonal Violence. 1994;9:366–382. [Google Scholar]
- Roberts KS, Brent EE. Physician utilization and illness patterns in families of alcoholics. Journal of Studies on Alcohol. 1982;43:119–128. doi: 10.15288/jsa.1982.43.119. [DOI] [PubMed] [Google Scholar]
- Rychtarik RG, McGillicuddy NB. The Spouse Situation Inventory: A role-play measure of coping skills in women with alcoholic partners. Journal of Family Psychology. 1997;11:289–300. doi: 10.1037/0893-3200.11.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaalje GB, McBride JB, Fellingham GW. Approximations to distributions of test statistics in complex mixed linear models using SAS Proc MIXED. Paper presented at the annual meeting of the SAS User Group International; Long Beach, CA. 2001. Apr, [Google Scholar]
- Schaffer JB, Tyler JD. Degree of sobriety in male alcoholics and coping styles used by their wives. British Journal of Psychiatry. 1979;135:431–437. doi: 10.1192/bjp.135.5.431. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Trull TJ, Bartholow BD, Vieth A. Personality and alcoholism: Issues, methods, and etiological processes. In: Leonard KE, Blane HT, editors. Psychological theories of drinking and alcoholism. 2. New York: Guilford Press; 1999. pp. 54–105. [Google Scholar]
- Sisson RW, Azrin NH. Family-member involvement to initiate and promote treatment of problem drinkers. Journal of Behavior Therapy and Experimental Psychiatry. 1986;17:15–21. doi: 10.1016/0005-7916(86)90005-4. [DOI] [PubMed] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Sobell LC, Agrawal S, Sobell MB. Factors affecting agreement between alcohol abusers’ and their collaterals’ reports. Journal of Studies on Alcohol. 1997;58:405–413. doi: 10.15288/jsa.1997.58.405. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB, Toneatto T, Leo GI. What triggers the resolution of alcohol problems without treatment? Alcoholism: Clinical and Experimental Research. 1993;17:217–224. doi: 10.1111/j.1530-0277.1993.tb00752.x. [DOI] [PubMed] [Google Scholar]
- Spanier G. Dyadic Adjustment Scale. North Tonawanda, NY: Multi-Health Systems; 1989. [Google Scholar]
- Stanton MD, Shadish WR. Outcome, attrition, and family-couples treatment for drug abuse. A meta-analysis and review of the controlled, comparative studies. Psychological Bulletin. 1997;122:170–191. doi: 10.1037/0033-2909.122.2.170. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The conflict tactic (CT) scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Overview of findings from the 2002 National Survey on Drug Use and Health. Rockville, MD: Author; 2003. Office of Applied Studies, NHSDA Series H-21, DHHS Publication No. SMA 03–3774. [PubMed] [Google Scholar]
- Svenson LW, Forster D, Woodhead SE, Platt GH. Individuals with a chemical-dependent family member—Does their health-care use increase? Canadian Family Physician. 1995;41:1488–1493. [PMC free article] [PubMed] [Google Scholar]
- Tabachnik BG, Fidell LS. Using mulitvariate statistics. 4. Needham Heights, MA: Allyn & Bacon; 2001. [Google Scholar]
- Thomas EJ, Ager RD. Unilateral family therapy with the spouses of uncooperative alcohol abusers. In: O’Farrell TJ, editor. Treating alcohol problems: Marital and family interventions. New York: Guilford Press; 1993. pp. 3–33. [Google Scholar]
- Thomas EJ, Yoshioka MR, Ager R, Adams KB. Reaching the uncooperative alcohol abuser through a cooperative spouse. Paper presented at the Fifth Congress of the International Society for Bio-Medical Research on Alcoholism; Toronto, CA. 1990. Jun, [Google Scholar]
- Tonigan JS, Miller WR, Connors GJ. The search for meaning in life as a predictor of alcoholism treatment outcome. In: Longabaugh R, Wirtz PW, editors. Project MATCH hypotheses: Results and causal chain analyses. Vol. 8. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 154–165. [Google Scholar]
- Wegscheider-Cruse S. Another chance: Hope and health for the alcoholic family. 2. Palo Alto, CA: Science and Behavior Books; 1989. [Google Scholar]
- Zweben A. Problem drinking and marital adjustment. Journal of Studies on Alcohol. 1986;47:167–172. doi: 10.15288/jsa.1986.47.167. [DOI] [PubMed] [Google Scholar]