Abstract
Invasive fractional flow reserve (FFR) is the gold standard for the determination of physiologic stenosis severity and the need for revascularization. FFR computed from standard acquired coronary computed tomographic angiography datasets (FFRCT) is an emerging technology which allows calculation of FFR using resting image data from coronary computed tomographic angiography (CCTA). However, the diagnostic accuracy of FFRCT in the evaluation of lesion-specific myocardial ischemia remains to be confirmed, especially in patients with intermediate coronary stenosis. We performed an integrated analysis of data from 3 prospective, international, and multicenter trials, which assessed the diagnostic performance of FFRCT using invasive FFR as a reference standard. Three studies evaluating 609 patients and 1050 vessels were included. The total calculated sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of FFRCT were 82.8%, 77.7%, 60.8%, 91.6%, and 79.2%, respectively, for the per-vessel analysis, and 89.4%, 70.5%, 69.7%, 89.7%, and 78.7%, respectively, for the per-patient analysis. Compared with CCTA alone, FFRCT demonstrated significantly improved accuracy (P < 0.001) in detecting lesion-specific ischemia. In patients with intermediate coronary stenosis, FFRCT remained both highly sensitive and specific with respect to the diagnosis of ischemia. In conclusion, FFRCT appears to be a reliable noninvasive alternative to invasive FFR, as it demonstrates high accuracy in the determination of anatomy and lesion-specific ischemia, which justifies the performance of additional randomized controlled trials to evaluate both the clinical benefits and the cost-effectiveness of FFRCT-guided coronary revascularization.
INTRODUCTION
Invasive coronary angiography (ICA) has served as the gold standard for the diagnosis of coronary artery disease (CAD).1 However, ICA provides only anatomic information and cannot assess physiological severity. Fractional flow reserve (FFR), an invasive index measured using a coronary pressure wire at the time of ICA, is commonly used in clinical practice to determine the hemodynamic significance of coronary stenosis.2,3 Compared with angiographic guidance, FFR-guided revascularization improves event-free survival and decreases medical costs.4–6 However, the routine use of ICA and FFR is not easy, nor is it without risk, as such usage increases case complexity and may also increase the risk of catheter-related complications, including bleeding, arrhythmia, stroke, coronary artery perforation, and dissection.7
Given its high sensitivity and negative predictive value (NPV), coronary computed tomographic angiography (CCTA) has become a useful noninvasive alternative to ICA and has been increasingly utilized in the clinic to diagnose and rule-out CAD.8 However, CCTA tends to overestimate the severity of coronary artery stenosis, as only a minority of lesions identified by CCTA have been found to cause cardiac ischemia. Moreover, the presence of motion artifacts, calcified plaque, stents, and limited spatial resolution may severely compromise anatomical evaluations performed using CCTA.9 The suboptimal specificity and positive predictive value (PPV) of CCTA in diagnosing CAD may encourage the unnecessary use of ICA and coronary revascularization. FFR computed from standard acquired CCTA datasets (FFRCT) is a novel noninvasive method of assessing lesion-specific ischemia, as it utilizes the computational fluid dynamics of CCTA and has enabled the calculation of FFR values without the use of additional medication, image acquisition techniques, or radiation exposure.10,11 The diagnostic accuracy of noninvasive FFRCT has been evaluated in recent 3 prospective, multicenter studies.12–14 However, the diagnostic performance of FFRCT in the identification or exclusion of functionally significant coronary stenosis using measured FFR as the reference standard remains controversial, especially in patients with intermediate coronary stenosis, wherein the clinical utility of FFRCT would be most commonly expected for use. The aim of this integrated analysis of the 3 studies was to further investigate the diagnostic efficacy of FFRCT, particularly on in subgroup with intermediate stenosis.
METHODS
Search Strategy and Eligibility Criteria
A literature search was performed using the Cochrane Library, PubMed, OVID, and EMBASE to identify articles published through October 2014. Complex search strategies were formulated using the following MESH terms and text words: fractional flow reserve, FFR, computed tomography, CT, coronary computed tomographic angiography, CCTA, coronary CTA, CTA, noninvasive FFR and FFRCT. To identify any studies missed by the literature searches, we hand-searched reference lists of eligible studies and relevant review articles. We included studies where the following criteria were met: the study population included ≥10 patients with either suspected or known CAD; the diagnostic performance of FFRCT was evaluated using invasive FFR as the reference standard; and the study allowed for sensitivity, specificity, NPV, and PPV calculations. Trials were excluded if they did not conform to the above criteria, or if there were overlapping study subjects. Finally, The DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained via Noninvasive Fractional Flow Reserve), DeFACTO (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography), and NXT (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps) studies were included.12–14
Study Design
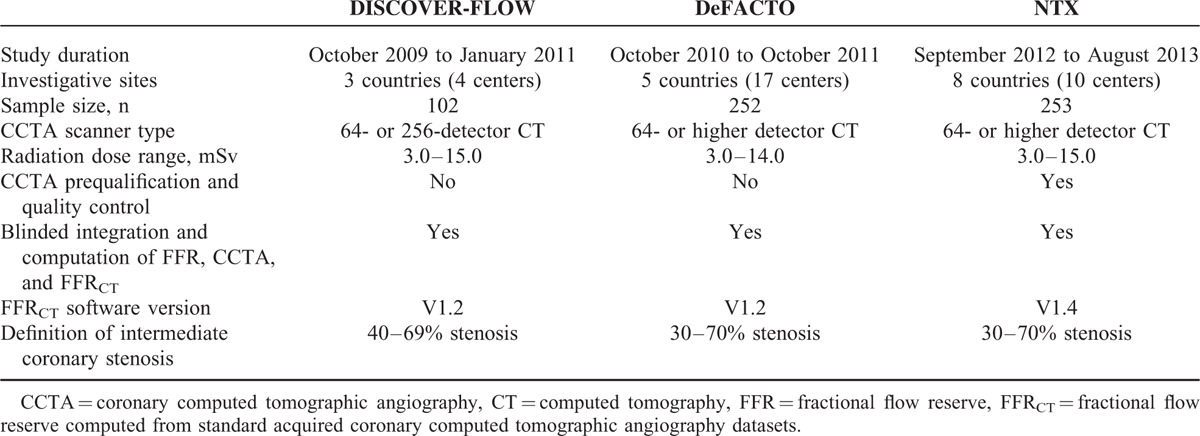
The DISCOVER-FLOW, DeFACTO, and NXT studies were prospective, international, multicenter trials designed to investigate the diagnostic accuracy of FFRCT for the discrimination of hemodynamically significant CAD, when compared to invasive FFR as the reference standard.12–14 These studies were registered with ClinicalTrials.gov (identifiers NCT01189331, NCT01233518, and NCT01757678). The methodological characteristics of the selected studies are shown in Table 1. The DISCOVER-FLOW was conducted at 4 centers in 3 countries (South Korea [2], Latvia [1], and the United States [1]). The DeFACTO was conducted at 17 centers in 5 countries (Belgium [n = 1], Canada [n = 1], Latvia [n = 1], South Korea [n = 2], and the United States [n = 12]). The NXT was conducted at 10 centers at 8 countries (Japan [3], Australia [1], England [1], Germany [1], South Korea [1], Scotland [1], Latvia [1], and Denmark [1]). The studies were approved by the institutional review board at each site and all patients provided written informed consent.
TABLE 1.
Characteristics of the Prospective Studies
FFRCT and FFR Measurement and Integration
In all of the 3 included trials, CCTA was performed by following guidelines with 64- or higher detector row scanners.15 CCTA images were transmitted to the central cores laboratory for further blinded analysis. Investigators evaluated evaluate luminal diameter stenosis in each segment of the coronary tree with an 18-segment coronary model. CCTA images were also transferred to the FFRCT core laboratory for the computation of FFRCT in blinded fashion. In NXT trials, a predefined image quality score was applied to select cases suitable for FFRCT analysis. Similarly, selective ICA was also performed according to guidelines or standard practice.16,17 FFR was measured during ICA. In DISCOVER-FLOW and DeFACTO studies, FFR procedure was performed as clinically indicated, and in NXT study measurement of FFR was performed for each stenosis ≥30% in a vessel segment with diameter ≥2 mm. Finally, the blinded integration core laboratory identified the location on CCTA that corresponded to the point where the FFR was measured.
Diagnostic Efficacy Analysis
Diagnostic performance of FFRCT was evaluated on a per-vessel as well as per-patient basis. For FFR and FFRCT, hemodynamically significant coronary stenosis was defined as a value ≤0.80. Significant obstruction on CCTA was recorded with stenosis ≥50%. Diagnostic measures included accuracy, sensitivity, specificity, PPV, NPV, positive likelihood ratio, and negative likelihood ratio. Discrimination was quantified using the area under the receiver operating characteristic curve of FFRCT and CCTA.
Statistical Analysis
We pooled the diagnostic accuracy data of both FFRCT and CCTA from the 3 studies on both a per-vessel and a per-patient basis. In the per-patient analysis, vessels with the most adverse clinical status were selected to represent a given patient. The reported percentages were recalculated and confirmed according to the patient numbers provided in the original publication, using standard formulas.18 Potential heterogeneity, meaning variation between studies, was evaluated by calculating the I2 statistic, with a value of 50% or more indicating a substantial level inconsistency. Data with I2 ≥ 50% were pooled using the DerSimoniane–Laird model, whereas data with I2 < 50% were pooled using the Mantel Haenszel model. Comparison of the diagnostic performances of FFRCT and CCTA was completed using a chi-squared test. The results were considered statistically significant at P < 0.05. The integrated analyses were conducted using Stata, version 12 (Stata Corp, College Station, TX). The aggregate results from the studies were summarized as weighted means (95% confidence intervals [CI] reported in the tables and figures). A subgroup analysis was conducted involving patients with intermediate coronary stenosis. In the DISCOVER-FLOW study, intermediate stenosis was defined as a coronary lesion with diameter stenosis ranging from 40% to 69% as determined via CCTA,19 whereas the range was 30% to 70% in the DeFACTO and NXT studies.13,14
RESULTS
Study Population
A total of 609 subjects (mean age 63.3 ± 9.2 years, male 68%) who underwent CCTA, FFRCT, ICA, and FFR were involved across the 3 studies. The demographic and baseline characteristics of the patients are detailed in Table 2. In DeFACTO and NXT studies, approximately 78% of the patients had experienced angina within the past month. The mean interval between CCTA and ICA plus invasive FFR was 2.3 to 18.0 days. Coronary dissection requiring percutaneous coronary intervention occurred in 2 patients in DeFACTO trial and 1 patient in NXT trial during FFR measurement. Following FFR measurement, 1 patient in DeFACTO trial suffered from retroperitoneal bleeding, and 2 patients in NXT experienced transient cerebral ischemia. No serious adverse complications were observed during examination in DISCOVER-FLOW study.
TABLE 2.
Baseline Demographics and Clinical Characteristics

Diagnostic Accuracy of FFRCT for Detecting Ischemia
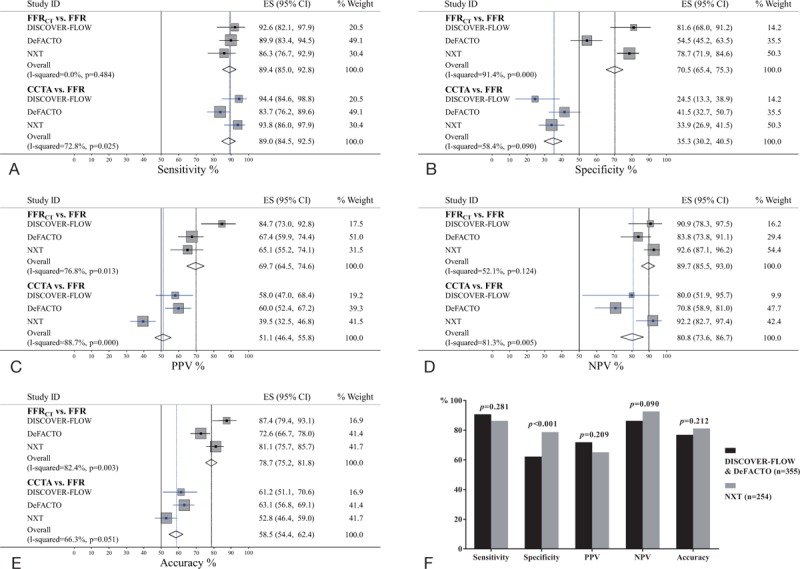
A total of 421 vessels and 337 patients were found to have functionally significant coronary stenosis as determined via FFR, or prevalence of 40.1% and 55.3%. Heterogeneities for relative statistics were evaluated in Tables 3 and 4. The per-vessel performances of FFRCT and CCTA are included in Table 3. FFRCT and CCTA demonstrated similar sensitivities (82.8% vs 86.1%, P = 0.369) and NPVs (91.6% vs 92.5%, P = 0.645). However, there were significant improvements in specificity (77.7% vs 55.7%, P < 0.001), PPV (60.8% vs 38.7%, P < 0.001), and accuracy (79.2% vs 63.1%, P < 0.001) with the utilization of FFRCT. On a patient-specific basis, the total calculated sensitivities, specificities, PPVs, NPVs, and accuracies for FFRCT and CCTA are included in Table 4. Additional between-group analyses demonstrated that FFRCT exhibited a high per-patient sensitivity compared with CCTA (P = 0.888) but also demonstrated significantly increased diagnostic specificity (P < 0.001), PPV (P < 0.001), NPV (P = 0.010), and accuracy (P < 0.001) (Fig. 1A–E).
TABLE 3.
Diagnostic Performance of FFRCT and CCTA for Detection of Lesion-Specific Ischemia on Per-Vessel Basis
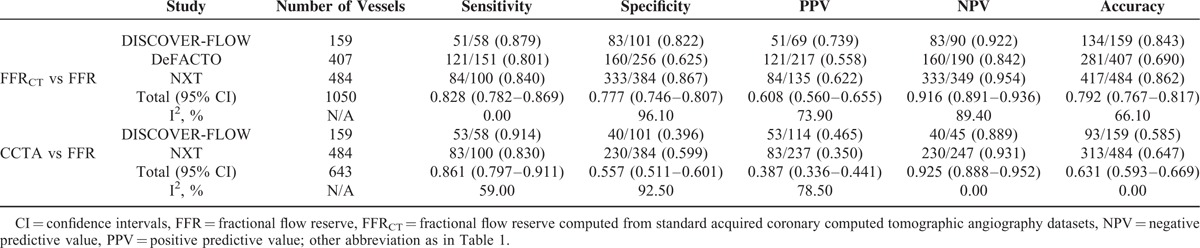
TABLE 4.
Diagnostic Performance of FFRCT and CCTA for Detection of Lesion-Specific Ischemia on Per-Patient Basis
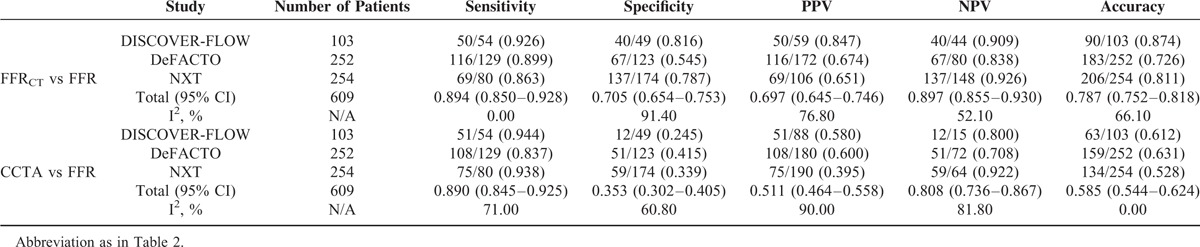
FIGURE 1.

Diagnostic accuracies of fractional flow reserve computed from standard acquired coronary computed tomographic angiography datasets (FFRCT) and coronary computed tomography angiography (CCTA) in the detection of hemodynamically significant coronary stenosis using a patient-based analysis and invasive FFR as a reference standard. (A–E) Forest plots of the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy of FFRCT, and CCTA. (F) A comparison between the integrated diagnostic values of the DISCOVER-FLOW and DeFACTO trials and the data from the NXT trial. FFR = fractional flow reserve.
Compared with both the DISCOVER-FLOW and the DeFACTO trials, the FFRCT technology used in the NXT trial was refined.20 Therefore, additional analyses were conducted to determine whether the improvements in FFRCT technology influenced its diagnostic performance. Although there were no significant differences noted in per-patient sensitivity (90.7% vs 86.3%, P = 0.281), PPV (71.9% vs 65.1%, P = 0.209), NPV (86.3% vs 92.6%, P = 0.090), or accuracy (76.9% vs 81.1%, P = 0.212) between the integrated results from the DISCOVER-FLOW and the DeFACTO trials compared with the data from the NXT trial, there was a significant increase noted in specificity (62.2% vs 78.7%, P < 0.001) with the use of the upgraded FFRCT technology (Fig. 1F).
Diagnostic Accuracy of FFRCT for Patients With Intermediate Coronary Stenosis
Of the 609 patients enrolled in the 3 included studies, 378 patients (62.1%) were found to have intermediate coronary stenosis by CCTA. In the DISCOVER-FLOW study, only the per-lesion diagnostic performances of FFRCT and CCTA were reported for the patients with intermediate stenosis. In light of the similar numbers of patients (n = 60) and lesions (n = 66) with intermediate stenosis in the DISCOVER-FLOW trial, we used the per-lesion diagnostic value instead of the per-patient value for the integrated analysis. When the patient-based analysis was restricted to patients with intermediate stenosis, the combined sensitivity, specificity, PPV, NPV, and accuracy for FFRCT were 85.3% (95% CI: 78.0–90.9), 76.5% (95% CI: 70.8–81.5), 64.7% (95% CI: 57.0–71.9), 91.1% (95% CI: 86.5–94.6), and 79.4% (95% CI: 75.0–83.4), respectively. Consistent with the findings in the general patient population, per-patient diagnostic specificity (P < 0.001), PPV (P < 0.001), NPV (P = 0.003), and accuracy (P < 0.001) were each significantly higher for FFRCT than for CT, with similar sensitivities (P = 0.321) among the patients with intermediate coronary stenosis (Fig. 2A–E). However, there was no significant difference between the combined results from the DISCOVER-FLOW and the DeFACTO trials compared with the data from the NXT trial (Fig. 2F).
FIGURE 2.
Diagnostic accuracy of FFRCT and CCTA in the detection of hemodynamically significant coronary stenosis, using a patient-based analysis and invasive FFR as a reference standard, among patients with intermediate coronary stenosis. (A–E) Forest plots of the sensitivity, specificity, PPV, NPV, and diagnostic accuracy of FFRCT and CCTA. (F) A comparison between the integrated diagnostic values from the DISCOVER-FLOW and DeFACTO trials and the data from the NXT trial. The abbreviations are the same as those used in Fig. 1.
DISCUSSION
This integrated analysis of 3 prospective, multicenter trials involving 609 patients with either suspected or known CAD was characterized by the high diagnostic accuracy of FFRCT in the detection of hemodynamically significant coronary stenosis, using invasive FFR as standard reference. We observed that FFRCT exhibited comparable sensitivity to CCTA but was superior with respect to all other evaluated parameters compared with CCTA among patients with CAD, both on a per-vessel and a per-patient basis, which was also consistent with a recent review about FFRCT.21 Importantly, we confirmed that FFRCT maintained a high sensitivity and specificity for the diagnosis of ischemia in patients with intermediate coronary stenosis, who are particularly challenging for clinicians to manage due to the poor relationship between angiographic severity and ischemia.22 Compared with CCTA, the number of false-positive findings was significantly lower for FFRCT. These results are germane, particularly for individuals whose coronary stenosis fall below conventional definitions of angiographically severe, yet confer hemodynamic importance that may explain symptoms of angina. Diffuse mild luminal narrowing has been demonstrated to be associated with decreased stress-induced myocardial blood flow and abnormal epicardial coronary artery resistance even before a high-grade segmental stenosis is apparent.23
The DISCOVER-FLOW trial was the first study to compare the diagnostic performances of CCTA and FFRCT with invasive FFR. Although the DISCOVER-FLOW study confirmed that FFRCT correlated well with invasive FFR, the study was not powered on a per-patient level. Therefore, the DeFACTO trial was subsequently conducted to evaluate the diagnostic accuracy of FFRCT; invasive FFR served as a reference standard in the diagnosis of per-patient ischemia; the primary analysis was performed to determine whether the per-patient diagnostic accuracy of FFRCT exceeded 70% using a 1-sided test at the 0.05 level of significance, with a power calculation based on the DISCOVER-FLOW findings.24 FFRCT demonstrated improved diagnostic accuracy compared with CCTA alone in the DeFACTO trial. However, the study did not achieve its prespecified primary end point regarding the diagnostic accuracy of FFRCT compared with FFR. Actually, the DISCOVER-FLOW and DeFACTO trials had almost identical study designs. When we combined the results of these 2 trials, we observed that the integrated per-patient diagnostic accuracy was 76.9% (95% CI: 72.2–81.2), with a lower 95% CI border >70%, which indicated that an insufficient number of study subjects may have been one of the reasons why the DeFACTO trial failed to meet the prospective primary endpoint. The recently published NXT trial, which used a refined version of the FFRCT technology that exhibited an improved ability to identify luminal boundaries and improvements in physiological models of microcirculatory resistance, demonstrated improved results compared with both the DISCOVER-FLOW and the DeFACTO trials, particularly regarding specificity. In addition to refinements in FFRCT technology, more stringent CT image quality control in the NXT trial may also have contributed to the improvements noted in diagnostic specificity.25 In contrast, FFRCT demonstrated both a high sensitivity and a high NPV in the diagnosis of ischemia, or 89.4% (with a lower 95% CI of 85.0%) and 89.7% (with a lower 95% CI of 85.5%) in the detection of hemodynamically significant coronary stenosis. However, missing a diagnosis of ischemia producing lesions in 1 to 2 patients out of 10 is unacceptable, as such an error may have serious consequences. Therefore, additional effort is necessary to improve the diagnostic performance of FFRCT.
Several landmark trials have demonstrated that the clinical benefits of coronary revascularization are primarily limited to ischemia-producing lesions. It has been reported that coronary revascularization in patients with intermediate stenosis without objective proof of ischemia neither reduce adverse cardiac events nor lead to a better functional angina class compared with medical treatment.26 Invasive FFR is now the gold standard for the determination of lesion-specific ischemia. However, this method is associated with complications related to coronary vessel instrumentation. In the 3 trials studied, 3 patients and 1 patient suffered from coronary dissection and retroperitoneal bleeding, respectively. FFRCT allows for the determination of anatomy and lesion-specific ischemia via noninvasive testing. Moreover, a recent published pilot research study suggested that virtual coronary stenting based on FFRCT results is feasible.27 Furthermore, 2 studies used the clinical data from the DISCOVER-FLOW and the NXT trials to evaluate the cost-effectiveness of FFRCT and determined that treatment planning using FFRCT to guide the selection of patients for ICA and virtual coronary stenting may reduce costs and improve clinical outcomes in patients with suspected CAD.28,29
Although FFRCT represents a promising means of noninvasively assessing the functional significance of coronary stenosis, several major points must be addressed. First, numerous CT-related artifacts and patient-related factors, including misalignment, motion, beam hardening from coronary calcification, and increased image noise, may adversely affect the image quality and subsequent diagnostic performance of FFRCT.30 Proper adherence to imaging protocols to ensure optimal image quality and enable the quantitative interpretation of lumen boundaries and nitroglycerin pretreatment before CCTA acquisition to ensure that the coronary arteries are dilated may improve the diagnostic accuracy of FFRCT.31 Second, the calculation of FFRCT costs several hours per examination due to both segmentation and computational processing.32 FFRCT is based on computational fluid dynamics. The computational technology underlying FFRCT incorporates multiple numerical methods and algorithms to solve the governing equations of fluid dynamics, which are founded in the balanced relationship between the conservations of mass and momentum.33 The equations are known as the Navier–Stokes equations and have been known for almost 2 centuries. However, the solving of these equations requires significant computational power which only became possible with the development of modern supercomputers and numerical methods. At present, this computational power is greater than can be made available onsite, thereby requiring said data to be transferred off-site for any subsequent calculations and analysis. Improvements in both the segmentation and the computational processing may allow for both on-site and timely integration.
Study Limitations
There were several limitations to this integrated analysis. First, all 3 of the included trials were supported by funding from HeartFlow, which also supplied the proprietary software. Second, the results of our study were limited to patients with stable (suspected) CAD. Patients with acute coronary syndromes and a history of either prior coronary intervention or bypass graft surgery were excluded from all 3 studies. Patients with cardiac arrhythmias were also excluded. Third, although each of the trials had similar study designs, there was some heterogeneity regarding CCTA prequalification, quality control, and the FFRCT evaluation. Unlike the 2 prior trials, the NXT trial optimized CCTA data acquisition and utilized improved FFRCT technology. Finally, in the subgroup analysis, the definition of intermediate coronary stenosis was not identical among the trials, which may have resulted in selection bias.
CONCLUSIONS
In this integrated analysis, FFRCT demonstrated high accuracy in the detection of lesion-specific ischemia using invasive FFR as a reference standard. Notably, the high sensitivity and NPV suggest the ability of FFRCT to effectively rule out intermediate lesions that cause ischemia. However, in light of the serious health consequences of a missed diagnosis of hemodynamically significant coronary stenosis, efforts should be undertaken to improve the diagnostic efficacy of FFRCT. Additionally, randomized controlled trials evaluating both the clinical benefits and the cost-effectiveness of FFRCT guided coronary revascularization are warranted.
Footnotes
Abbreviations: CAD = coronary artery disease, CCTA = coronary computed tomographic angiography, CI = confidence interval, FFR = fractional flow reserve, FFRCT = fractional flow reserve computed from standard acquired coronary computed tomographic angiography dataset, ICA = invasive coronary angiography, NPV = negative predictive value, PPV = positive predictive value.
XR and LC have contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Lucas FL, Siewers AE, Malenka DJ, et al. Diagnostic-therapeutic cascade revisited: coronary angiography, coronary artery bypass graft surgery, and percutaneous coronary intervention in the modern era. Circulation 2008; 118:2797–2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122. [DOI] [PubMed] [Google Scholar]
- 3.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35:2541–2619. [DOI] [PubMed] [Google Scholar]
- 4.Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009; 360:213–224. [DOI] [PubMed] [Google Scholar]
- 5.De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001. [DOI] [PubMed] [Google Scholar]
- 6.Li J, Elrashidi MY, Flammer AJ, et al. Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice. Eur Heart J 2013; 34:1375–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tobis J, Azarbal B, Slavin L. Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol 2007; 49:839–848. [DOI] [PubMed] [Google Scholar]
- 8.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 2010; 56:1864–1894. [DOI] [PubMed] [Google Scholar]
- 9.Tashakkor AY, Nicolaou S, Leipsic J, et al. The emerging role of cardiac computed tomography for the assessment of coronary perfusion: a systematic review and meta-analysis. Can J Cardiol 2012; 28:413–422. [DOI] [PubMed] [Google Scholar]
- 10.Kim HJ, Jansen KE, Taylor CA. Incorporating autoregulatory mechanisms of the cardiovascular system in three-dimensional finite element models of arterial blood flow. Ann Biomed Eng 2010; 38:2314–2330. [DOI] [PubMed] [Google Scholar]
- 11.Kim HJ, Vignon-Clementel IE, Coogan JS, et al. Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann Biomed Eng 2010; 38:3195–3209. [DOI] [PubMed] [Google Scholar]
- 12.Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011; 58:1989–1997. [DOI] [PubMed] [Google Scholar]
- 13.Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. J Am Med Assoc 2012; 308:1237–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014; 63:1145–1155. [DOI] [PubMed] [Google Scholar]
- 15.Abbara S, Arbab-Zadeh A, Callister TQ, et al. SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009; 3:190–204. [DOI] [PubMed] [Google Scholar]
- 16.Naidu SS, Rao SV, Blankenship J, et al. Clinical expert consensus statement on best practices in the cardiac catheterization laboratory: Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 2012; 80:456–464. [DOI] [PubMed] [Google Scholar]
- 17.Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol 1999; 33:1756–1824. [DOI] [PubMed] [Google Scholar]
- 18.Altman DG, Bland JM. Diagnostic tests 1 sensitivity and specificity. BMJ 1994; 308:1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Min JK, Koo BK, Erglis A, et al. Usefulness of noninvasive fractional flow reserve computed from coronary computed tomographic angiograms for intermediate stenoses confirmed by quantitative coronary angiography. Am J Cardiol 2012; 110:971–976. [DOI] [PubMed] [Google Scholar]
- 20.Gaur S, Achenbach S, Leipsic J, et al. Rationale and design of the HeartFlowNXT (HeartFlow analysis of coronary blood flow using CT angiography: NeXt sTeps) study. J Cardiovasc Comput Tomogr 2013; 7:279–288. [DOI] [PubMed] [Google Scholar]
- 21.Li S, Tang X, Peng L, et al. The diagnostic performance of CT-derived fractional flow reserve for evaluation of myocardial ischaemia confirmed by invasive fractional flow reserve: a meta-analysis. Clin Radiol 2015; 70:476–486. [DOI] [PubMed] [Google Scholar]
- 22.Fearon WF, Takagi A, Jeremias A, et al. Use of fractional myocardial flow reserve to assess the functional significance of intermediate coronary stenoses. Am J Cardiol 2000; 86:1013–1014.A1010. [DOI] [PubMed] [Google Scholar]
- 23.De Bruyne B, Hersbach F, Pijls NH, et al. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “Normal” coronary angiography. Circulation 2001; 104:2401–2406. [DOI] [PubMed] [Google Scholar]
- 24.Min JK, Berman DS, Budoff MJ, et al. Rationale and design of the DeFACTO (Determination of Fractional Flow Reserve by Anatomic Computed Tomographic AngiOgraphy) study. J Cardiovasc Comput Tomogr 2011; 5:301–309. [DOI] [PubMed] [Google Scholar]
- 25.Min JK, Koo BK, Erglis A, et al. Effect of image quality on diagnostic accuracy of noninvasive fractional flow reserve: results from the prospective multicenter international DISCOVER-FLOW study. J Cardiovasc Comput Tomogr 2012; 6:191–199. [DOI] [PubMed] [Google Scholar]
- 26.Bech GJ, De Bruyne B, Pijls NH, et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 2001; 103:2928–2934. [DOI] [PubMed] [Google Scholar]
- 27.Kim KH, Doh JH, Koo BK, et al. A novel noninvasive technology for treatment planning using virtual coronary stenting and computed tomography-derived computed fractional flow reserve. JACC Cardiovasc Interv 2014; 7:72–78. [DOI] [PubMed] [Google Scholar]
- 28.Kimura T, Shiomi H, Kuribayashi S, et al. Cost analysis of non-invasive fractional flow reserve derived from coronary computed tomographic angiography in Japan. Cardiovasc Interv Ther 2015; 30:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hlatky MA, Saxena A, Koo BK, et al. Projected costs and consequences of computed tomography-determined fractional flow reserve. Clin Cardiol 2013; 36:743–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Hassan D, Leipsic J. Noninvasive fractional flow reserve derived from coronary computed tomography angiography: integrated anatomical and functional assessment. Future Cardiol 2013; 9:243–251. [DOI] [PubMed] [Google Scholar]
- 31.Leipsic J, Yang TH, Thompson A, et al. CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve: results from the Determination of Fractional Flow Reserve by Anatomic CTA (DeFACTO) study. AJR Am J Roentgenol 2014; 202:989–994. [DOI] [PubMed] [Google Scholar]
- 32.Yoon YE, Koo BK. Non-invasive functional assessment using computed tomography: when will they be ready for clinical use? Cardiovasc Diagn Ther 2012; 2:106–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meijs MF, Cramer MJ, El Aidi H, et al. CT fractional flow reserve: the next level in non-invasive cardiac imaging. Neth Heart J 2012; 20:410–418. [DOI] [PMC free article] [PubMed] [Google Scholar]


