Abstract
Centralized HIV program oversight and repeal of the Department of Defense policy “Don’t Ask Don’t Tell” permitted characterization of HIV transmission among soldiers assigned to a large US Army base continental United States from 2012 to 2013. An investigation of a greater than expected number of new HIV infections among soldiers was initiated to characterize transmission and identify opportunities to disrupt transmission and deliver services.
All soldiers who were assigned to the base at the time of their first positive HIV test and who had their first positive HIV test in 2012 or in the first 6 months of 2013 and who had a clinical genotype available for analysis were eligible for inclusion in the investigation.
All patients (n = 19) were men; most were black (52%) and less than 30 years old (64%). Fifteen of the 19 patients participated in in-depth interviews. Eighty percent were men who have sex with men who reported multiple sex partners having met through social and electronic networks. All were subtype B infections. Significant knowledge gaps and barriers to accessing testing and care in the military healthcare system were identified. Most (58%) belonged to transmission networks involving other soldiers.
This investigation represents an important step forward in on-going efforts to develop a comprehensive understanding of transmission networks in the Army that can inform delivery of best practices combination prevention services. The Army is developing plans to directly engage individuals in key affected populations most at risk for HIV infection to identify and address unmet needs and expand delivery and uptake of prevention services. Further investigation is underway and will determine whether these findings are generalizable to the Army.
INTRODUCTION
By regulation, all US soldiers are subject to periodic serologic screening for human immunodeficiency virus (HIV) every 2 years and soldiers who deploy to combat are also screened both before, and after returning from, deployments. HIV-infected soldiers are excluded from overseas missions.1,2 The prevalence of HIV infection among active duty US Army soldiers is approximately 0.02%3 and is lower than that of the general young adult US population.4 Identifiable risk factors for HIV infection among Army personnel include younger age, black race, and single marital status.1 Behavioral risk data and understanding of social sexual networks among US military personnel is limited because of regulations in place before 2011 that restricted the collection/disclosure of information regarding sexual orientation.5
In 2012, the US Army Public Health Command (USAPHC) centralized HIV program oversight and partnered with the Military HIV Research Program (MHRP) at the Walter Reed Army Institute of Research (WRAIR) to initiate a public health activity to comprehensively characterize all incident HIV infections. Objectives are to actively characterize the epidemic and generate actionable public health data intended to inform prevention policy and practices. This report describes the findings from an investigation that followed the observation of a greater than expected number of patients of new HIV infections among US Army soldiers at a large base in the continental United States.
METHODS
Program Description
This centralized USAPHC program is executed across the Army enterprise by MHRP/WRAIR and is supported by local HIV Program staff (including preventive medicine physicians and public health nurses) and other military healthcare providers. Program data include comprehensive health surveillance data in the Defense Medical Surveillance System (DMSS) routinely collected from Department of Defense (DoD) personnel2,6 and data generated through routine public health practice and clinical care.
At the time of the investigation, the US Army used an HIV diagnostic algorithm that included a third generation HIV-1/HIV-2 plus O enzyme immunoassay screen, type HIV-1/HIV-2 differentiation by rapid test, with confirmation by HIV-1 western blot. A qualitative HIV-1 ribonucleic acid assay was used to resolve infection status of negative or indeterminate western blot specimens and identify acute HIV infection.7
Study Population
This epidemiological investigation was initiated in 2012 and included in-depth public health interviews of patients who were assigned to the base at the time of their first positive HIV test and who had their first positive HIV test in 2012 or in the first 6 months of 2013 and who had a clinical genotype available for analysis.
Data Collection
Program staff complete a standardized public health HIV case report form for all soldiers identified with incident HIV-1 infections.2 Clinical data collected include HIV viral load and genotype determinations and cluster of differential counts, routinely performed for HIV care,8 and history of sexually transmitted infections. Data from the DMSS include demographics, complete HIV test history, deployment history, and medical encounters in the period at risk for HIV infection. Archived assignment and HIV screening data from the DMSS for all soldiers in the period 1996 to current were used to determine baseline/expected rates and patterns of infection.
The period at risk for HIV infection was defined by the interval from last known negative specimen to first positive specimen. Last negative specimen evaluations were conducted on residual serum reposed in the Department of Defense Serum Repository.9 Serum from the last HIV seronegative sample was evaluated for HIV-1 ribonucleic acid with nucleic acid-amplification testing assays.
Semistructured interviews were performed by a single infectious disease physician with prior military service and included collection of health, social, and military occupational history, relevant medical encounters, and potential exposures to HIV. The interviewing physician was not a member of the healthcare team at this base. The treating infectious diseases physicians facilitated the interview process by making their patients aware that they would be contacted as part of this investigation and invited to participate in an interview. Participation was voluntary and private, one on one interviews were conducted in the infectious diseases clinic during nonduty hours when the clinic was closed. The interviewing physician took written notes during the interviews. Following each interview, the interviewing physician was debriefed by 2 or 3 members of the investigative team during which time the interviewer referred to his written notes.
Analyses
Following identification of increased counts in HIV patients at this base, phylogenetic tree analysis of the protease-reverse transcriptase (pro-RT) gene sequences (2262–2549 and 2661–3290 base positions in HXB2) allowed for identification of potential network clusters. The initial HIV-1 genotype was determined using the HIV-1 genotyping tool.10 The HIV-1 sequences were aligned along with selected reference sequences downloaded from the HIV sequence database,11 and were analyzed using molecular evolutionary genetic analysis.12 Pairwise genetic distances of sequences were performed using the Kimura 2-parameter substitution model against all incident Army sequences acquired from this base in the period 2001 to 2013 (n = 29). To confirm networking in another region of the virus, the HIV-1 envelope sequences encompassing HXB2 5984–9063 were generated and analyzed using methods previously described13,14 for individuals who were networked (less than 2.0% divergence between sequences) in pro-RT sequence analysis.
Interview data were analyzed using thematic analysis. Two team members independently identified and coded key themes from the interviews. The most common and the most actionable themes were categorized. These key themes were stripped of identifiers and merged in to the analysis database; subsequent analysis was performed by unique anonymous study identification number to preserve anonymity. The investigators subsequently reached agreement on the themes that would be extracted and summarized. They then independently reviewed the in-depth interview debriefing notes a second time and quantified key and actionable theme categories.
Ethical Approval
Approval of this activity and the investigation was obtained from the Division of Human Subjects Protections and Institutional Review Board of the WRAIR (#1861) and the USAPHC Public Health Review Board.
RESULTS
There was an average of fewer than 2 new cases per year (range: 0–5) in the period 2001 to 2010 at this base. In 2011, there were 10 new cases observed among active duty personnel. There were 14 and 5 new cases among active duty soldiers in 2012 and the first 6 months of 2013, respectively. All 19 were included in the investigation.
Sociodemographic Characteristics
All patients (n = 19) were male soldiers and most were less than 30 years old (64%: median: 23). Most were black (52%) or Hispanic (26%) and most were single/never married (52%). Nine of 19 (47%) were either currently married (n = 6) or separated (n = 3). Nearly half (40%) were junior enlisted soldiers who were serving at their first duty assignment after initial entry training. The period at risk for HIV infection ranged from 105 to 765 days (median: 329 days). All had overlapping periods at risk with at least one other case.
Patient Interviews
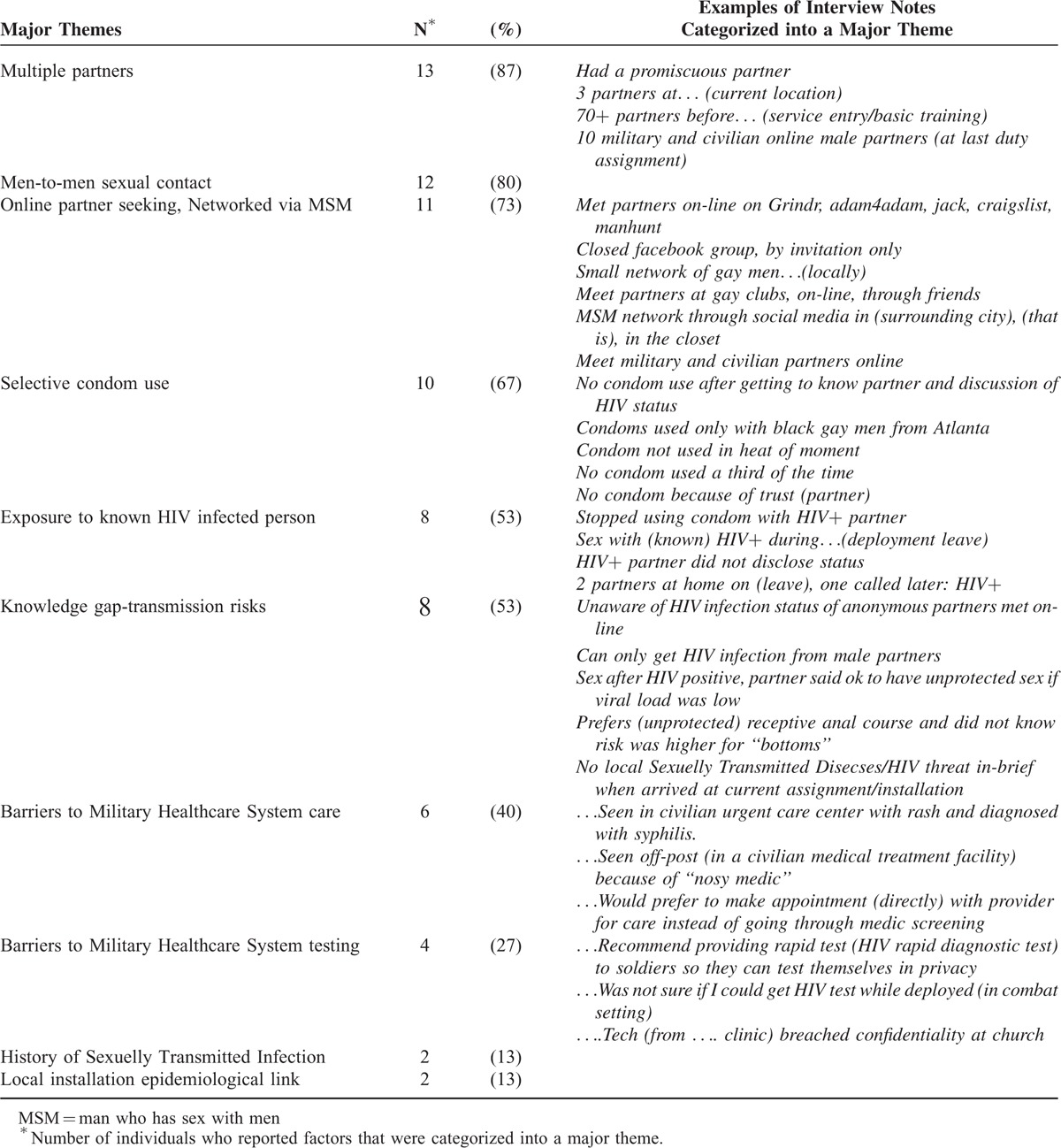
In depth interviews of 15 of the 19 patients were conducted. A number of common key theme categories were identified (Table 1). The most common themes were self-report of being a man who has sex with men (MSM), membership in MSM social sexual networks, having multiple sex partners, seeking sex partners through on-line social media sources, and selective condom use. Key themes also included HIV-specific knowledge gaps, confidentiality concerns, and perceived barriers to accessing services in the Military Healthcare System. Participants infrequently reported information that could be used to establish a direct epidemiological link to other HIV-infected soldiers at the same base (Table 1).
TABLE 1.
Summary of Themes from Expanded Interviews of 15 HIV-Infected Soldiers, 2012 to 2013
Molecular Epidemiology
All patients had HIV-1 subtype B infections. Molecular clustering was observed among 11/19 (58%) of patients (Figure 1A). There were 3 groups observed in the pro-RT analysis which included 6, 3, and 2 individuals, respectively. Mean genetic distance were 1.1% (range: 0.0%–2.7%), 0.0%, and 1.4% (range: 0.7%–1.8%) for groups 1, 2, and 3, respectively. In the largest group, 1 sequence (case: 02) was more divergent than the other members of this group. It, however, clustered more closely with the group than with any other sequence and this relationship was present and significant in both the pro-RT and env analyses. Env sequencing results confirmed all of these findings and sequence relationships; mean genetic distances were 4.6%, 0.04%, and 4.6% for groups 1, 2, and 3, respectively (Figure 1B). In addition, 2 groups of 2 clustered sequences and 1 nonsubtype B (CRF02_AG) infection were observed among the pro-RT sequences obtained in the period before this investigation (Figure 1C). Among the 11 patients from whom sequences were observed to cluster, 8 participated in in-depth interviews. Interview data was not available for 3 individuals who were members of pairs that most closely clustered within groups 1 to 3 because they did not participate in the investigation (Figure 1A).
FIGURE 1.
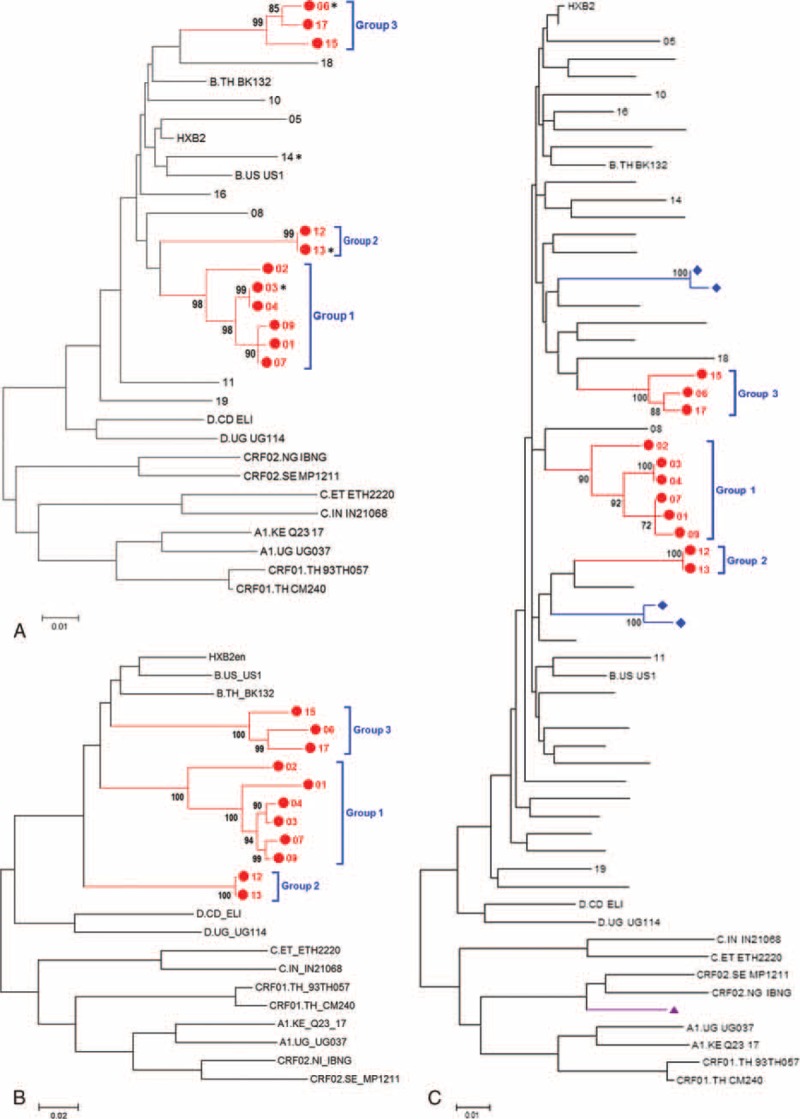
Maximum-likelihood trees of protease/reverse transcriptase) and envelope sequences of HIV-1. Bootstrap values (as percentages) are indicated at the nodes. Branch reproducibility was assessed at 1000 replicates. A, ML tree of pro-RT sequences (n = 19) from individuals included in this investigation with reference strains. ∗In-depth interviews not performed. B, ML tree of envelope sequences (n = 11) for subset of sequences that clustered in pro-RT with reference strains. C, ML tree of pro-RT sequences (n = 48) from all incident Army sequences acquired from this base in the period 2001 to 2013 with reference strains; (diamond/blue) indicate 2 pairs of sequences that cluster from individuals infected before this investigation. (triangle/purple) indicates subtype CRF02_AG sequence from individual infected before this investigation. ML, Maximum-likelihood; pro-RT, protease-reverse transcriptase.
DISCUSSION
This investigation characterized installation local level transmission of HIV infection in an identifiable, highly networked population consisting primarily of MSM and identified opportunities to disrupt transmission, enhance delivery of preventive interventions, and improve public health. The Army at the time of this writing is evaluating the generalizability of these findings and is developing plans to directly engage individuals in key affected populations most at risk for HIV infection to identify unmet needs and address barriers to testing, care and treatment, and uptake of prevention services.
The degree of clustering among soldiers in these networks was higher than that present at the same base before this investigation and is similar to or higher than that observed in other epidemics among MSM in the United States, United Kingdom, and Europe.15–17 Understanding of transmission dynamics and the complexities of key social sexual networks is critically important in responding to changes in the epidemic. It is unclear, however, whether this degree of networking is generalizable to the Army. Additional, retrospective analysis of existing Army-wide data and prospectively collected data are required. These findings do suggest, however, the possibility that targeted interventions aimed at disrupting transmission networks involving soldiers could result in a significant decrease in the number of new infections both in the Army and in the civilian communities where social sexual networks intersect.
This investigation occurred after repeal of Don’t Ask Don’t Tell and was executed in an environment free of regulatory limitations restricting collection and disclosure of same sex behaviors. These findings add to emerging data that suggest the HIV epidemic in the military is consistent with the civilian epidemic in the United States and is largely concentrated among MSM.1,4,18–20 The transmission dynamics reported here also appear to be consistent with reports among MSM in the United States, United Kingdom, and Europe.17,21–23
This investigation identified a number of key risk exposures that are potentially modifiable to reduce individual risk for HIV infection and that can further inform delivery of preventive interventions. These findings present opportunities to provide risk reduction counseling and education to close knowledge gaps.
Important themes regarding stigma and barriers to accessing treatment and care were identified. This is not surprising given the relatively recent repeal of policies in the military that prohibited same sex behavior and disclosure. Stigma and barriers to care will likely present significant on-going challenges in the engagement of these key affected populations. Uptake and effectiveness of services could be markedly limited by reluctance to seek care, unwillingness to disclose important data to healthcare providers, and/or lack of awareness by healthcare providers to consider and obtain relevant information necessary to address some of the unique needs of MSM in the areas of mental and social health and substance abuse.24–26 The findings of a recent survey of military primary care providers suggest there may be significant gaps that must be addressed in knowledge and training among military providers in the culturally competent delivery of primary care for lesbian, gay, bisexual, and transgender patients.27 This investigation identified a number of epidemiologic links to the social sexual networks among soldiers and their contacts in the community but the majority of interviews did not result in soldiers naming other soldiers as their contacts. This is not surprising because of nonparticipation in the investigation by a number of individuals with HIV sequences most closely related to other members of transmission clusters and the potential for nondisclosure because of stigma, fear of breaches in confidentiality, and/or unfavorable interviewer response. It is also possible that there were other non-soldier intermediary members of transmission networks among those cases with less closely clustered sequences. And, because anonymous partner seeking was frequent, it is possible that soldiers may not have known or could not identify other soldiers among their sex partners.
Given the small number of individuals involved in this investigation and the fact that it occurred on a single base, it is likely that these findings are not generalizable to the Army epidemic. Since this investigation, annual counts of new cases have been lower, with 7, 6, and 6 new cases occurring in 2013, 2014, and 2015, respectively and molecular clustering among new cases has been similar to the period before investigation. Given the similarities observed to the civilian HIV epidemic, some of the key findings may be generalizable. Additional, study is warranted.
These and other recent findings are promising because the epidemic appears to be concentrated among a now identifiable population with whom public health and clinical providers can partner to assess unmet needs and deliver current best practices combination preventive interventions.18,20,28 These findings are also challenging because the Army is likely to face disease control challenges that are similar to those in nonmilitary settings. These include challenges associated with factors that include complex networks, multiple partners, biologic risks that increase risk for HIV infection, and social/structural factors that contribute to an increased risk for HIV transmission.29,30 These challenges must be addressed while also considering military unique exposures such as frequent geographic and cultural isolation, combat, and exposure to the battlefield emergency blood supply.1,31 This investigation represents an important step forward in on-going efforts to develop a comprehensive understanding of transmission networks in the Army that can inform delivery of best practices combination prevention services. Additional, investigation is underway and will determine whether these findings are generalizable to the Army. Best use of these data will require creative solutions to identify and partner with key affected populations to develop, deliver, and evaluate optimal interventions services. The Army is developing plans to directly engage individuals in key affected populations most at risk for HIV infection to identify and address unmet needs and expand delivery and uptake of prevention services.
Acknowledgments
We gratefully acknowledge the MHRP/WRAIR LMVP sequencing team for their technical assistance, Major Aatif Hayat and Paul Pietrusiak for contribution of critical data, and Francine McCutchan for providing molecular consultative services.
Footnotes
Abbreviations: DMSS = Defense Medical Surveillance System, DoD = Department of Defense, env = HIV-1 envelope, HIV = human immunodeficiency virus, MHRP = Military HIV Research Program, MSM = man who has sex with men, pro-RT = protease-reverse transcriptase, RNA = ribonucleic acid, USAPHC = US Army Public Health Command, WRAIR = Walter Reed Army Institute of Research.
Department of Defense Disclaimer: “The views expressed are those of the authors and should not be construed to represent the positions of the US Department of Defense.”
This work was supported by OCONUS Contingency Operations funds from the United States Department of Defense.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Singer DE, Bautista CT, O’Connell RJ, et al. HIV infection among U.S. Army and Air Force military personnel: sociodemographic and genotyping analysis. AIDS Res Hum Retroviruses 2010; 26:889–894. [DOI] [PubMed] [Google Scholar]
- 2.Department of the Army. Identification, surveillance, and administration of personnel infected with human immunodeficiency virus (HIV). Washington, DC: AR 600-110 22; 2014. [Google Scholar]
- 3.Armed Forces Health Surveillance Branch.. Update: routine screening for antibodies to human immunodeficiency virus, Civilian Applicants for U.S. Military Service and U.S. Armed Forces, Active and Reserve Components, January 2009–June, 2014. MSMR 2014; 21:16–22. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. HIV Surveillance Report, 2012; vol. 24. http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2014 Accessed [February 10,2015]. [Google Scholar]
- 5.Undersecretary of Defense Clifford L. Stanley. Department of Defense, Personnel and Readiness. Memorandum. Repeal of ‘Don’t Ask Don’t Tell’. September 20, 2011. [Google Scholar]
- 6.Department of Defense Directive 6490.02E, “Comprehensive Health Surveillance,” October 3, 2013. [Google Scholar]
- 7.Hakre S, Paris RM, Brian JE, et al. Enhanced U. S. Army HIV diagnostic algorithm used to diagnose acute HIV infection in a deployed soldier. Mil Med 2012; 177:609–613. [DOI] [PubMed] [Google Scholar]
- 8.Panel on antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. Available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf Accessed [February 9, 2015] [Google Scholar]
- 9.Rubertone MV, Brundage JF. The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health 2002; 92:1900–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rozanov M, Plikat U, Chappey C, et al. A web-based genotyping resource for viral sequences. Nucleic Acids Res 2004; 32:W654–W659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HIV Sequence Compendium 2013. Foley B, Leitner T, Apetrei C, Hahn B, Mizrachi I, Mullins J, Rambaut A, Wolinsky S, and Korber B, Eds. Published by Theoretical Biology and Biophysics Group, Los Alamos National Laboratory, NM, LA-UR 13-26007. [Google Scholar]
- 12.Tamura K, Peterson D, Peterson N, et al. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol 2011; 28:2731–2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heipertz RA, Jr, Sanders-Buell E, Kijak G, et al. Molecular epidemiology of early and acute HIV type 1 infections in the United States Navy and Marine Corps, 2005–2010. AIDS Res Hum Retroviruses 2013; 29:1310–1320. [DOI] [PubMed] [Google Scholar]
- 14.Rolland M, Tovanabutra S, deCamp AC, et al. Genetic impact of vaccination on breakthrough HIV-1 sequences from the STEP trial. Nat Med 2011; 17:366–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aldous JL, Pond SK, Poon A, et al. Characterizing HIV transmission networks across the United States. Clin Infect Dis 2012; 55:1135–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith DM, May SJ, Tweeten S, et al. A public health model for the molecular surveillance of HIV transmission in San Diego, California. AIDS 2009; 23:225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leigh Brown AJ, Lycett SJ, Weinert L, et al. Transmission network parameters estimated from HIV sequences for a nationwide epidemic. J Infect Dis 2011; 204:1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hakre S, Armstrong AW, O’Connell RJ, et al. A pilot online survey assessing risk factors for HIV acquisition in the Navy and Marine Corps, 2005–2010. J Acquir Immune Defic Syndr 2012; 61:125–130. [DOI] [PubMed] [Google Scholar]
- 19.Brett-Major DM, Hakre S, Naito NA, et al. Epidemiology of contemporary seroincident HIV infection in the Navy and Marine corps. Mil Med 2012; 177:1328–1334. [DOI] [PubMed] [Google Scholar]
- 20.Hakre S, Scoville S, Pacha L, et al. Sexual risk behaviors of HIV seroconverters in the U.S. Army, 2012–2014. J Acquir Immune Defic Sydr 2015; In Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oster AM, Pieniazek D, Zhang X, et al. Demographic but not geographic insularity in HIV transmission among young black MSM. AIDS 2011; 25:2157–2165. [DOI] [PubMed] [Google Scholar]
- 22.Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS 2011; 25:1103–1112. [DOI] [PubMed] [Google Scholar]
- 23.Yebra G, Holguin A, Pillay D, et al. Phylogenetic and demographic characterization of HIV-1 transmission in Madrid, Spain. Infect Genet Evol 2013; 14:232–239. [DOI] [PubMed] [Google Scholar]
- 24.Lewis NM. Mental health in sexual minorities: recent indicators, trends, and their relationships to place in North America and Europe. Health Place 2009; 15:1029–1045. [DOI] [PubMed] [Google Scholar]
- 25.Bostwick WB, Boyd CJ, Hughes TL, et al. Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. Am J Public Health 2010; 100:468–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beyrer C, Sullivan PS, Sanchez J, et al. A call to action for comprehensive HIV services for men who have sex with men. Lancet 2012; 380:424–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tong RL, Lane J, McCleskey P, et al. A pilot study describing knowledge and practices in the health care of men who have sex with men by U.S. Air Force primary care providers. Mil Med 2013; 178:e248–e254. [DOI] [PubMed] [Google Scholar]
- 28.CDC- Gay and Bisexual Men's Health-homepage. http://www/cdc.gov/msmhealth/msm-programs February 10, 2014. [Google Scholar]
- 29.Beyrer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS 2013; 27:2665–2678. [DOI] [PubMed] [Google Scholar]
- 30.Mayer KH, Wang L, Koblin B, et al. Concomitant socioeconomic, behavioral, and biological factors associated with the disproportionate HIV infection burden among Black men who have sex with men in 6 U.S. cities. PLoS One 2014; 9:e87298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spinella PC, Dunne J, Beilman GJ, et al. Constant challenges and evolution of US military transfusion medicine and blood operations in combat. Transfusion 2012; 52:1146–1153. [DOI] [PubMed] [Google Scholar]


