Abstract
Background
Younger age and female sex are both associated with greater mental stress in the general population, but limited data exist on status of perceived stress in young and middle-aged patients presenting with acute myocardial infarction (AMI).
Methods and Results
We examined sex difference in stress, contributing factors to such difference, and whether this difference helps explain sex-based disparities in 1-month recovery using data from 3,572 AMI patients (2,397 women and 1,175 men) 18–55 years of age. The average score of 14-item Perceived Stress Scale (PSS-14) at baseline was 23.4 for men and 27.0 for women (p<0.001). Higher stress in women was largely explained by sex differences in comorbidities, physical and mental health status, intra-family conflict, care-giving demand, and financial hardship. After adjustment for demographic and clinical characteristics, women had worse recovery than men at 1-month post-AMI, with mean differences in improvement score ranging from −0.04 for Euro-Qol utility index to −3.96 for angina-related quality of life (p<0.05 for all). Further adjustment for baseline stress reduced these sex-based differences in recovery to −0.03 to −3.63, which however remained statistically significant (p<0.05 for all). High stress at baseline was associated with significantly worse recovery in angina-specific and overall quality of life, as well as mental health status. The effect of baseline stress on recovery did not vary between men and women.
Conclusions
Among young and middle-aged patients, higher stress at baseline is associated with worse recovery in multiple health outcomes after AMI. Women perceive greater psychological stress than men at baseline, which partially explains women’s worse recovery.
Keywords: Acute myocardial infarction, Sex difference, Perceived stress, Early recovery
Psychosocial factors have been increasingly recognized as risk factors for coronary events and poor cardiovascular outcomes after acute myocardial infarction (AMI).1–6 Mental stress, in particular, can induce myocardial ischemia and promote atherogenesis and is associated with behavioral factors that may adversely affect health outcomes such as treatment non-compliance.7, 8 Prior studies have linked several psychosocial stressors (e.g., job strain and financial hardship) to increased incidence of coronary heart disease and AMI.4, 5, 9 However, few studies have examined status of perceived stress in patients presenting with AMI.
Importantly, women tend to report greater stress and more stressful life events than men, potentially because of their different roles in family life and work, as compared with men.10–12 This differential level of stress between men and women may be an important reason for sex-based differences in post-AMI recovery that have been observed in previous studies.3, 13, 14 Psychological stress may be particularly pertinent to younger patients. Data from a 2009 national survey showed that self-perceived stress was inversely associated with advancing age, with the level of stress particularly high in people younger than 55 years of age.15 However, we know little about sex difference in stress in younger patients with AMI.
The purpose of this study was to characterize sex difference in perceived stress in young and middle-aged patients presenting with AMI and to evaluate which factors may contribute to the difference. We also examined the association of baseline stress with one-month recovery and whether sex difference in baseline stress helps explain differential post-AMI recovery between men and women. Findings from this study will enhance our understanding of psychosocial characteristics of young and middle-aged patients with AMI and their potential contribution to sex-based differences in health outcomes.
METHODS
Data Source
We used data from the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, the largest prospective observational study of young and middle-aged women and men with AMI. Details about the design of the VIRGO study are reported elsewhere.16 In brief, VIRGO was a prospective, observational study of AMI patients 18–55 years old from a large, diverse, network of 103 hospitals in the U.S., 24 in Spain, and 3 in Australia enrolled from August 2008 through January 2012. Younger women with AMI differ from men and older women with this condition in etiology and outcomes.16–18 However, low enrollment of young and middle-aged women in major registries and clinical trials remained an important barrier to our understanding of their risk-factor profiles and treatment patterns, as well as factors that may contribute to the poorer outcomes among women than men.16, 19 The VIRGO study was designed to address these research questions and hence targeted young and middle-aged patients with AMI and oversampled women than men (2:1 ratio). The Yale University Human Investigation Committee approved VIRGO study and all participants gave informed consent.
Eligible participants must have: 1) a rise of cardiac biomarkers (generally troponin) with at least one value above the 99th percentile of the upper reference limit within 24 hours of admission, and 2) evidence of acute myocardial ischemia including symptoms of ischemia, ECG changes indicative of new ischemia in the ECG (new ST-T changes), new or presumably new left bundle-branch block, development of pathological Q waves), or other evidence of myocardial necrosis (imaging, pathology). In addition, the participants must either present at or were transferred within the first 24 hours to an enrolling institution to ensure that the primary clinical decision-making was conducted at the enrolling site. Patients were excluded if any of the following was true: 1) previous enrollment in VIRGO, 2) neither English nor Spanish-speaking, 3) unable to provide informed consent, 4) unable to be contacted for follow-up (e.g., no access to phone, not planning on living in the country of enrollment), 5) AMI caused by physical trauma, or 6) currently a prisoner.
Baseline data were collected by site coordinators during the index hospitalization for AMI via patient interviews, medical record review, physical measurements, and analysis of blood specimens. Early recovery was assessed at one month after hospital discharge based on patient interviews. One-month interviews were administered by the Yale Follow-Up Center in the US, a dedicated contract research organization in Spain and site coordinators in Australia. All staff involved in the project received specific training to ensure consistency in data collection, abstraction and interview administration. Because one of our study aims was to characterize sex difference in perceived stress in patients presenting with AMI, our analytic sample included all patients available at baseline.
Perceived Stress at Baseline
We measured each patient’s self-perceived psychological stress at baseline using the 14-item Perceived Stress Scale (PSS-14).20 PSS-14 is a global measure of perceived stress, asking respondents about the degree to which their life situations during the last month were unpredictable, uncontrollable, and overloaded.21 For example, “In the last month, how often have you been upset because of something that happened unexpectedly?” Response to each item was scored as never (0), almost never (1), sometimes (2), fairly often (3), and very often (4). Negatively stated items primarily reflect perceived distress, while positively stated items mostly reflect coping ability.21, 22 The overall PSS-14 score was calculated by reversely coding positive items such that the total score ranged from 0 to 56 with a higher score indicating greater stress. In order to compare the stress level of young and middle-aged AMI patients with that of the general U.S. population, which was only available from a 2009 national survey based on PSS-10,15 we also calculated each patient’s PSS-10 score. PSS-10 was calculated similarly as PSS-14 except that only 10 of the items were included, resulting in a total PSS-10 score ranging from 0 to 40.
Recovery Outcomes at One Month
We measured each patient’s recovery based on changes in their angina-specific and overall health status (symptoms, function and quality of life) between baseline and one month after AMI. Angina frequency, angina-related physical limitation, and angina-related quality of life were assessed using the Seattle Angina Questionnaire (SAQ).23 General health status was measured using the 12-item short-form health survey (SF-12) physical component summary (PCS) and mental component summary (MCS) scores.24 Health-related quality of life was assessed by the Euro-Qol (EQ-5D) utility index and visual analog scale.25 The EQ-5D utility index generates scores between 0 and 1, while all other scales are scored between 0 and 100. On all measures, higher value indicated better symptoms, function, or quality of life. We calculated change in each measure between baseline and one-month follow-up. A positive change score indicates improvements in symptoms, function, or quality of life, while a negative score indicates deterioration in symptoms, function, or quality of life.
Explanatory Variables
Our primary explanatory variable was sex (female versus male). We also measured patient sociodemographic and health characteristics at baseline, psychosocial stressors and support at baseline, AMI clinical characteristics indicative of disease severity at the time of index admission and treatment received during the index hospitalization, and country of residence. Baseline sociodemographic and health characteristics included age (18–34 years, 35–44 years, versus 45–55 years), race/ethnicity, education, marital status, smoking history, body mass index, comorbid conditions (e.g., diabetes mellitus, hypertension, depression), cardiac history (e.g., prior AMI, prior coronary artery bypass graft (CABG), prior percutaneous coronary intervention (PCI)). Measures of psychosocial stressors and support included adverse life events (based on individual items of the INTERHEART Stressful Life Events (SLE) scale, except for “other major stress” which represents a highly mixed group of events),5, 26 care-giving demand (number of children, grandchildren, and parents living in household), financial hardship (not having enough money to make ends meet, just enough to make ends meet, versus having some money left over at the end of the month), work-related strain (number of jobs; not working for pay, work part-time, work full-time with extended hours, versus work full-time without extended hours), and social support (assessed using the ENRICHD Social Support Inventory (ESSI)).27, 28 AMI clinical characteristics included ST-elevation myocardial infarction (STEMI) or non–ST-segment elevation myocardial infarction (NSTEMI), Killip Class at arrival, peak troponin, left ventricular ejection fraction, Global Registry of Acute Coronary Events (GRACE) risk score,29 hemodynamic instability, pre-hospital delay in presentation, receipt of PCI or CABG procedures, length of hospital stay, and quality of care received during index hospitalization. We assessed quality of care using the hospital AMI Core Measure Set endorsed by the Joint Commission and the Centers for Medicare & Medicaid Services,30 including aspirin at arrival, aspirin at discharge, ACE inhibitor or ARB for Left Ventricular Systolic Dysfunction (LVSD) at discharge, smoking cessation instructions, Beta Blocker at arrival, Beta Blocker at discharge, timely diagnostic cardiac catheterization, timely reperfusion for STEMI/LBBB, and Statin at discharge. Similar to prior research,7 we constructed a composite measure for the percentage of eligible AMI core measures each patient received.
Statistical Analysis
Descriptive statistics of patient characteristics were calculated. We compared total PSS-14 score, as well as sub-scales of positive and negative items, between men and women using Student’s t test. Bivariate analyses and multivariable linear regression analysis were conducted to identify factors that differed between men and women and might explain sex difference in baseline stress. The regression model used baseline PSS-14 score as the dependent variable, and patient demographic characteristics, baseline health status, baseline psychosocial stressors and support, and country of residence as explanatory variables.
We also conducted multivariable linear regression analyses to assess the relationship between sex, baseline perceived stress, and one-month recovery. Recovery outcomes (angina frequency, angina-related physical limitation, angina-related quality of life, SF-12 PCS score, SF-12 MCS scores, EQ-5D utility index, and EQ-5D visual analog scale) served as dependent variables in these models. Explanatory variables included patient sex and baseline stress, as well as other demographic characteristics, baseline health status and psychosocial stressors and support, AMI severity and treatment factors, and country of residence. As there were no established cutoffs for the PSS-14, we categorized a patient’s baseline stress level as low, moderate, or high based on tertiles of the total score (with 21 and 30 being the cut-offs). We estimated the models with and without adjustment for baseline stress to assess whether controlling for this factor reduced estimated sex differences in recovery. Statistical significance of interaction terms between sex and baseline stress levels were also examined in these models to test potential interaction effects. All data analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Sample Characteristics
There were 3,572 AMI patients in VIRGO (1,175 men and 2,397 women) (Table 1; Supplemental Table 1). Of them, 3,275 (91.7%) completed both baseline and one-month interviews, and 30 (0.8%) died before one-month follow-up. Median age of VIRGO participants was 48 years for both sexes. Sixty percent of men and 48.2% of women presented with STEMI (p<0.001). Clinical severity of AMI presentation was similar between men and women: 7.9% of men and 8.9% of women had a GRACE risk score greater than 99 (p=0.3), while 11.1% of men and 10.5% of women had an ejection fraction less than 40% (p=0.6). Women were more likely than men to present more than 6 hours after symptom onset (44.8% versus 36.3%, p<0.001). Median peak troponin was 9.6 ng/mL among men (interquartile range [IQR]: 2.0 – 37.5) versus 5.8 ng/mL among women (IQR: 1.4 – 23.1) (p<0.001).
Table 1.
Baseline sample characteristics
| Sample Characteristics | Men (N=1,175) | Women (N=2,397) | P-value |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age, median (IQR) (range) | 48 (IQR: 43 – 52) (range: 23 – 55) | 48 (IQR: 44 – 52) (range: 18 – 55) | 0.221 |
| Age, % | 0.041 | ||
| 18–34 years | 42 (3.6%) | 123 (5.1%) | |
| 35–44 years | 314 (26.7%) | 578 (24.1%) | |
| 45–55 years | 819 (69.7%) | 1696 (70.8%) | |
| Race | <.001 | ||
| White | 980 (83.5%) | 1820 (76.1%) | |
| Black | 114 (9.7%) | 440 (18.4%) | |
| Other | 79 (6.7%) | 133 (5.6%) | |
| Education | 0.085 | ||
| Less than high school | 47 (4.1%) | 138 (5.9%) | |
| High school | 489 (42.6%) | 970 (41.2%) | |
| More than high school | 612 (53.3%) | 1248 (53.0%) | |
| Married/living with a partner as if married | 754 (64.6%) | 1315 (55.0%) | <.001 |
| Baseline health status | |||
| Diabetes mellitus | 317 (27.0%) | 929 (38.8%) | <.001 |
| Hypertension | 730 (62.1%) | 1530 (63.8%) | 0.322 |
| Hypercholesterolemia | 1080 (91.9%) | 1982 (82.7%) | <.001 |
| Chronic lung disease | 65 (5.5%) | 298 (12.4%) | <.001 |
| Chronic renal dysfunction | 91 (7.8%) | 276 (11.6%) | 0.001 |
| Depression | 245 (21.6%) | 886 (38.7%) | <.001 |
| History of cancer | 23 (2.0%) | 96 (4.0%) | 0.001 |
| History of cardiovascular condition | |||
| Prior acute myocardial infarction (AMI) | 200 (17.0%) | 353 (14.7%) | 0.075 |
| Prior coronary artery bypass graft | 39 (3.3%) | 81 (3.4%) | 0.938 |
| Prior percutaneous coronary intervention | 195 (16.7%) | 321 (13.4%) | 0.010 |
| Prior peripheral artery disease | 23 (2.0%) | 57 (2.4%) | 0.427 |
| Prior angina pectoris | 307 (26.2%) | 659 (27.5%) | 0.400 |
| History of congestive heart failure | 24 (2.0%) | 117 (4.9%) | <.001 |
| Prior stroke | 27 (2.3%) | 120 (5.0%) | 0.001 |
| Prior valve surgery | 4 (0.3%) | 19 (0.8%) | 0.112 |
| SF-12 physical component summary (PCS) score, median (IQR) | 49.1 (39.0 – 55.1) | 44.0 (33.4 – 53.1) | <.001 |
| SF-12 mental component summary (MCS) score, median (IQR) | 50.8 (41.1 – 57.3) | 45.3 (34.7 – 54.3) | <.001 |
| History of smoking | 0.002 | ||
| Never smoked | 244 (20.9%) | 574 (24.0%) | |
| Current smoker | 657 (56.2%) | 1377 (57.5%) | |
| Past smoker (>1month and <1year) | 51 (4.4%) | 112 (4.7%) | |
| Past smoker (>1year) | 217 (18.6%) | 333 (13.9%) | |
| Body mass index, median (IQR) | 29.4 (26.5 – 33.1) | 30.1 (25.5 – 35.7) | 0.017 |
| Baseline psychosocial stressors and support | |||
| Stressful life events during past year | |||
| Marital separation/Divorce/Break-up of long-term relationship | 125 (10.8%) | 291 (12.3%) | 0.191 |
| Loss of job (fired)/Forced retirement | 211 (18.2%) | 409 (17.2%) | 0.467 |
| Loss of crop/Business failure | 86 (7.4%) | 82 (3.5%) | <.001 |
| Violence/Victim of a crime | 62 (5.3%) | 131 (5.5%) | 0.807 |
| Major intra-family conflict | 242 (20.8%) | 784 (33.1%) | <.001 |
| Major personal injury or illness (other than your heart problem) | 193 (16.6%) | 532 (22.4%) | <.001 |
| Death/Major illness of a close family member | 323 (27.8%) | 866 (36.6%) | <.001 |
| Death of a spouse | 6 (0.5%) | 24 (1.0%) | 0.131 |
| Number of children living in household | 0.014 | ||
| 0 | 567 (48.6%) | 1051 (44.0%) | |
| 1–2 | 479 (41.0%) | 1102 (46.2%) | |
| ≥ 3 | 121 (10.4%) | 233 (9.8%) | |
| Number of grandchildren living in household | <.001 | ||
| 0 | 1138 (97.7%) | 2196 (92.5%) | |
| ≥ 1 | 27 (2.3%) | 177 (7.5%) | |
| Number of parents living in household | 0.744 | ||
| 0 | 1078 (92.5%) | 2203 (92.8%) | |
| 1–2 | 87 (7.5%) | 170 (7.2%) | |
| Finance at the end of the month | <.001 | ||
| Some money left over | 442 (38.1%) | 623 (26.4%) | |
| Just enough to make ends meet | 433 (37.4%) | 884 (37.4%) | |
| Not enough to make ends meet | 284 (24.5%) | 856 (36.2%) | |
| Number of jobs | 0.215 | ||
| 0–1 | 1080 (93.2%) | 2244 (94.2%) | |
| ≥2 | 79 (6.8%) | 137 (5.8%) | |
| Employment status | <.001 | ||
| Not working for pay | 309 (27.3%) | 1038 (43.9%) | |
| Working part-time (<35 hours/week) | 104 (9.2%) | 366 (15.5%) | |
| Working full-time (35–55 hours/week) | 564 (49.8%) | 872 (36.9%) | |
| Working full-time with extended hours (>55 hours/week) | 156 (13.8%) | 90 (3.8%) | |
| Low social support | 158 (13.8%) | 326 (13.9%) | 0.915 |
| AMI presentation | |||
| STEMI | 705 (60.0%) | 1155 (48.2%) | <.001 |
| Cardiogenic shock upon hospital admission | 5 (0.4%) | 16 (0.7%) | 0.374 |
| Peak troponin during index hospital stay | 9.6 (2.0 – 37.5) | 5.8 (1.4 – 23.1) | <.001 |
| Ejection fraction <40% | 127 (11.1%) | 243 (10.5%) | 0.568 |
| GRACE risk score >99 | 91 (7.9%) | 208 (8.9%) | 0.305 |
| Hemodynamic instability | 97 (8.3%) | 212 (8.8%) | 0.556 |
| Length of hospital stay, median (range) | 3 (0 – 42) | 3 (0 – 61) | 0.006 |
| First heart rate measured, median (IQR) | 80.0 (68.0 – 92.5) | 82.0 (70.0 – 95.0) | 0.001 |
| First systolic blood pressure, median (IQR) | 143.0 (125.0 – 161.0) | 141.0 (122.0 – 161.0) | 0.012 |
| Present more than 6 hours after symptom onset | 425 (36.3%) | 1070 (44.8%) | <.001 |
| Country | 0.817 | ||
| US | 976 (83.1%) | 2009 (83.8%) | |
| Spain | 176 (15.0%) | 340 (14.2%) | |
| Australia | 23 (2.0%) | 48 (2.0%) | |
Statistics are reported as n (%) unless otherwise specified. GRACE = Global Registry of Acute Coronary Events; IQR = interquartile range; STEMI = ST-elevation myocardial infarction.
Perceived Stress at Baseline
At baseline, young and middle-aged patients presenting with AMI had an average PSS-14 score of 25.8 (standard deviation [SD] = 9.7). When evaluated using PSS-10, the mean score was 18.5 (SD=8.1) for the overall sample; and 20.1, 18.9, and 18.3 for patients age 18–34, 35–44, and 45–55 years, respectively. For reference and based on prior literature, the PSS-10 is 16.4 and 16.9, respectively, for individuals age 35–44 and 45–54 years old in the general U.S. population.15
Sex Difference in Perceived Stress at Baseline
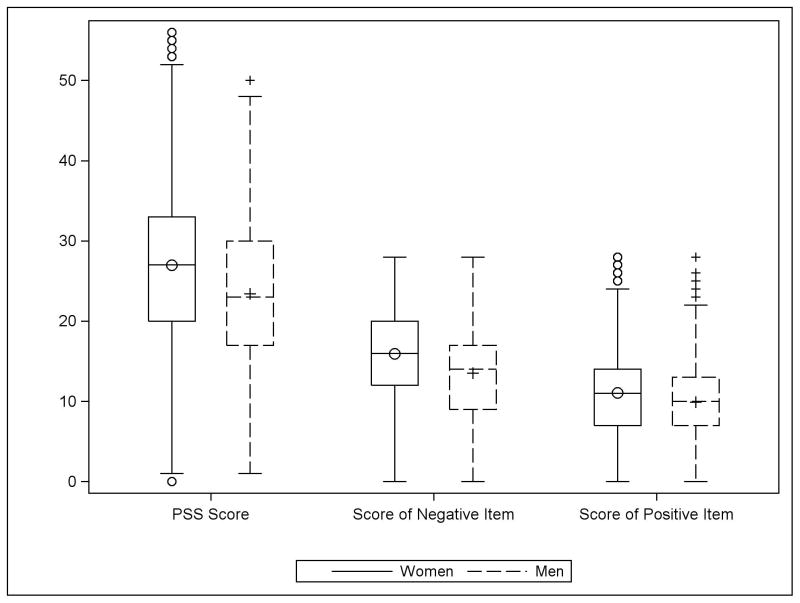
The overall PSS-14 score averaged 23.4 for men (SD=9.0), compared with 27.0 for women (SD=9.9) (p<0.001, Figure 1; Supplemental Table 2). In general, women perceived greater stress across all 14 items (Supplemental Table 3). They perceived negatively stated items (primarily reflecting perceived distress) more often than men and positively stated items (primarily reflecting coping ability) less often than men.21, 22
Figure 1.
Sex differences in perceived stress scale (PSS-14). Overall PSS-14 score, score of negative items (primarily reflecting perceived distress), and score of positive items (primarily reflecting coping ability) were all statistically different between men and women (all p values <0.001).
Women differed from men in many important characteristics. Compared with men, women had significantly higher rates of diabetes, chronic lung disease, chronic renal dysfunction, depression, and cancer, as well as previous PCI, congestive heart failure, and stroke (p<0.01 for all) (Table 1). They also had worse PCS (median=44.0 for women versus 49.1 for men, p<0.001) and MCS scores (median=45.3 for women versus 50.8 for men, p<0.001). With respect to psychosocial stressors, women were more likely than men to report stressful life events during the past year, such as major intra-family conflict (33.1% versus 20.8%, p<0.001), major personal injury or illness (22.4% versus 16.6%, p<0.001), and death/major illness of a close family member (36.6% versus 27.8%, p<0.001). In contrast, a higher proportion of men reported loss of crop/business failure (7.4% versus 3.5%, p<0.001). Women were also more likely than men to have children or grandchildren living in their household, while experiencing greater financial strain (Table 1). In terms of work-related strain, women were more likely than men to not work for pay (43.9% versus 27.3%) or work part-time (15.5% versus 9.2%) (p<0.001 for overall comparison of employment status).
Adjustment for patient sociodemographic, health, and psychosocial characteristics in multivariable linear regression model substantially reduced sex difference in baseline PSS-14 score from 3.29 (95% confidence interval [CI]: 2.54 to 4.04) to 0.72 (95% CI: 0.13 to 1.30), but it remained statistically significant (p=0.02) (Table 2; Supplemental Table 4). In particular, younger age, higher education, baseline depression, worse PCS and MCS scores, low social support, marital separation/divorce/break-up of long-term relationship, major intra-family conflict, greater child care responsibility, financial hardship, and working full-time were all associated with a significantly higher PSS-14 score at baseline.
Table 2.
Patient characteristics associated with baseline perceived stress scale (PSS-14) score
| Baseline characteristics | Unadjusted | Adjusted* | ||
|---|---|---|---|---|
|
| ||||
| Coefficient | 95% CI | Coefficient | 95% CI | |
| Women (versus men) | 3.29 | (2.54, 4.04) | 0.72 | (0.13, 1.30) |
| Age | ||||
| 18–34 years | 2.14 | (0.91, 3.37) | ||
| 35–44 years | 0.67 | (0.06, 1.27) | ||
| 45–55 years | Reference category | |||
| Education | ||||
| Less than high school | Reference category | |||
| High school | 1.57 | (0.31, 2.84) | ||
| More than high school | 1.61 | (0.33, 2.89) | ||
| Not married (versus Married/living with a partner as if married) | −1.07 | (−1.64, −0.50) | ||
| Depression | 3.98 | (3.31, 4.66) | ||
| SF-12 physical component summary (PCS) score | −0.08 | (−0.11, −0.06) | ||
| SF-12 mental component summary (MCS) score | −0.36 | (−0.39, −0.34) | ||
| Low social support | 1.80 | (1.03, 2.57) | ||
| Stressful life events during past year | ||||
| Marital separation/Divorce/Break-up of long-term relationship | 1.09 | (0.27, 1.91) | ||
| Loss of job (fired)/Forced retirement | 0.12 | (−0.58, 0.82) | ||
| Loss of crop/Business failure | 1.19 | (−0.04, 2.41) | ||
| Violence/Victim of a crime | −0.01 | (−1.17, 1.15) | ||
| Major intra-family conflict | 1.92 | (1.33, 2.51) | ||
| Major personal injury or illness (other than your heart problem) | 0.04 | (−0.63, 0.71) | ||
| Death/Major illness of a close family member | 0.09 | (−0.45, 0.63) | ||
| Death of a spouse | 0.18 | (−2.37, 2.72) | ||
| Number of children living in household | ||||
| 0 | Reference category | |||
| 1–2 | 0.89 | (0.33, 1.44) | ||
| ≥ 3 | 1.16 | (0.26, 2.05) | ||
| Finance at the end of the month | ||||
| Some money left over | Reference category | |||
| Just enough to make ends meet | 1.56 | (0.92, 2.19) | ||
| Not enough to make ends meet | 3.25 | (2.50, 4.00) | ||
| Employment status | ||||
| Not working for pay | −1.25 | (−1.93, −0.57) | ||
| Working part-time (<35 hours/week) | −0.49 | (−1.29, 0.31) | ||
| Working full-time (35–55 hours/week) | Reference category | |||
| Working full-time with extended hours (>55 hours/week) | 0.91 | (−0.12, 1.94) | ||
CI = confidence interval.
Table only reports patient characteristics that were statistically significant in the regression model. Model also adjusted for race/ethnicity, smoking status, body mass index, other baseline conditions, number of grandchildren living in household, number of parents living in household, number of jobs, and country of residence.
Further analyses suggested significant interaction effect of sex with financial hardship. Not having enough to make ends meet was associated with a higher PSS-14 score for men than for women. Coefficient estimate on interaction term between “not enough to make ends meet” and female sex was −1.96 (95% CI: −3.36 to −0.57, p=0.006).
Sex, Perceived Stress and One-Month Recovery
At one-month post-AMI, patients’ general and angina-specific health status improved on average (except for SF-12 PCS) (Table 3). However, multivariable linear regression analyses showed significant difference in recovery between men and women after adjustment for sociodemographic and clinical characteristics (Table 3; Supplemental Tables 5–11). Table 3 presents the adjusted mean difference between women and men in improvement scores, which indicated statistically significant worse recovery for women on nearly all outcome measures. Sex difference in improvement scores ranged from −0.04 (95% CI: −0.05 to −0.02) for EQ-5D utility index to −3.96 (95% CI: −5.97 to −1.96) for angina-related quality of life (p<0.05 for all except for angina frequency). As shown in Table 3, these differences are large when compared with sample mean improvement scores over this time.
Table 3.
Adjusted mean difference in one-month recovery associated with sex and baseline perceived stress
| Recovery outcome (measured by improvement between baseline and one- month follow-up)* | Sample average recovery†
|
Before adjustment for baseline perceived stress‡
|
After adjustment for baseline perceived stress‡
|
||
|---|---|---|---|---|---|
| Female | Female | Perceived stress
|
|||
| Mean (SD) | (versus Male) | (versus Male) | Moderate (versus Low) | High (versus Low) | |
| Angina frequency | 4.8 (24.0) | −1.14 (−2.66, 0.37) | −1.00 (−2.52, 0.52) | −1.83 (−3.47, −0.18) | −1.60 (−3.57, 0.37) |
| Angina-related physical limitation | 8.2 (27.4) | −1.88 (−3.52, −0.23) | −1.71 (−3.37, −0.06) | −1.28 (−3.08, 0.51) | −2.06 (−4.20, 0.09) |
| Angina-related quality of life | 11.3 (28.2) | −3.96 (−5.97, −1.96) | −3.63 (−5.64, −1.62) | −3.50 (−5.68, −1.33) | −4.09 (−6.71, −1.46) |
| SF-12 PCS score | −2.1 (11.6) | −2.25 (−3.16, −1.34) | −2.18 (−3.09, −1.26) | −0.40 (−1.39, 0.58) | −0.93 (−2.11, 0.25) |
| SF-12 MCS score | 3.9 (12.5) | −2.88 (−3.78, −1.99) | −2.72 (−3.61, −1.83) | −1.96 (−2.96, −0.96) | −3.66 (−4.93, −2.38) |
| EQ-5D utility index score | 0.1 (0.2) | −0.04 (−0.05, −0.02) | −0.03 (−0.05, −0.02) | −0.005(−0.02, 0.01) | −0.02 (−0.04, −0.01) |
| EQ-5D visual analog scale | 6.3 (22.9) | −2.24 (−3.87, −0.60) | −1.79 (−3.43, −0.15) | −2.70 (−4.48, −0.93) | −5.39 (−7.54, −3.24) |
SD = standard deviation; PCS = physical component summary; MCS = mental component summary; EQ-5D = Euro-Qol.
Recovery was assessed as change in each measure between baseline and one-month follow-up. A positive change score indicates improvement in symptoms, function, or quality of life, while a negative score indicates deterioration in symptoms, function, or quality of life.
Sample average recovery reflects the mean (SD) of the change score in each measure between baseline and one-month follow-up for all participants in the sample.
Model also adjusted for patient sociodemographic characteristics (age, race/ethnicity, education, marital status), smoking status, social support, baseline health condition, severity of acute myocardial infarction, pre-hospital delay in presentation, procedure and quailty of care received during index hospitalization, country, and the corresponding baseline value of the outcome variable. Results are reported as coefficient estimate (95% confidence interval).
Further adjustment for baseline psychological stress attenuated these sex differences, but they remained statistically significant (Table 3). Compared with patients with low stress, those with moderate or high stress had significantly worse recovery in angina frequency, angina-related quality of life, SF-12 MCS score, EQ-5D utility index, and EQ-5D visual analog scale (Table 3). Interaction terms between sex and baseline stress (high, moderate, versus low) were not statistically significant in any of the models for one-month recovery, indicating that the effect of baseline stress did not vary between men and women.
DISCUSSION
Among young and middle-aged AMI patients, higher stress at baseline was associated with worse recovery in multiple health outcomes after AMI. Women perceived greater psychological stress than men at baseline, which partially explained their worse recovery. However, the effect of baseline stress on recovery did not vary between men and women. Higher stress in women was largely explained by sex differences in comorbidities, physical and mental health status, intra-family conflict, care-giving demand, and financial hardship.
This study extends prior literature in three important ways. First, it demonstrates a negative association between baseline psychological stress and AMI recovery among patients 18–55 years old. As self-perceived stress is inversely associated with advancing age, it is particularly important to understand the role of stress in influencing AMI-recovery in younger patients. Arnold and colleagues7 recently showed that moderate and high perceived stress at baseline is linked to an increased 2-year mortality rate and poorer 1-year outcomes in older AMI patients. However, the study examined the broad AMI patient population with a mean age of 59 years. How mental stress is associated with AMI recovery in younger patients remained a major gap in literature. Our results corroborate findings from Arnold et al.,7 and suggest that stress is significantly associated one-month recovery among younger patients as well. Helping patients develop positive attitudes and coping skills for stressful situations may not only improve their psychological well-being, but also help recovery after AMI. Pilot studies testing stress reduction interventions as a hypothesized secondary prevention strategy will be informative and further research assessing the independent (versus mediating) role of stress in influencing outcomes would inform the design of such interventions. In addition, given our finding that physical, mental, and psychosocial factors were all associated with a patient’s stress level, stress management interventions may need to take interdisciplinary approaches (e.g., targeting physical functioning, mental health, and social support).
Second, our study suggests that difference in baseline mental stress between men and women partially explains sex disparities in recovery after AMI. Earlier studies in older patients documented worse post-AMI outcomes in angina, physical functioning, quality of life, rehospitalization, and mortality in women than in men.3, 13 Here we found significant sex differences in improvement in physical functioning, mental health status, and quality of life at one-month post-AMI in young and middle-aged patients. This gap was partially attenuated after we adjusted for differential levels of baseline stress between men and women. While mental stress is not likely a dominant cause for sex disparities in recovery, our findings offer another opportunity for narrowing this gap and enhancing care for women with AMI. If the relationship between mental stress and one-month recovery is causal, stress management interventions may help decrease sex-based differences in outcomes. Even if the association does not involve a causal relationship, the strong linkage suggests that baseline stress may be a useful prognostic marker for predicting health outcomes in young and middle-aged AMI patients. As psychological stress can influence both extrinsic (autonomic tone, hypothalamic-pituitary-adrenal axis function and platelet reactivity) and intrinsic (atherosclerotic plaque, endothelial function, inflammation and vasomotor tone) vascular processes,8, 31 further mechanistic studies of the exact pathophysiological pathways responsible for the post-AMI recovery outcomes and potential sex differences may help identify novel therapeutic interventions.8
Third, our findings show that male and female patients are burdened by different stressors and that some stressors exert different effect on men versus women. For instance, compared with men, women had worse physical and mental health status and were more likely to report major intra-family conflict or have children living in their household. In contrast, men were more likely than women to work full-time or over time and report loss of crop/business failure, and financial hardship was more distressing for men versus women. This is consistent with the traditional role expectations of “men as breadwinner” and “women as caregiver.” Moreover, changes in social context, such as increased labor force participation among women and higher rates of divorce and single parenthood, significantly influence social roles of women in the younger generation, which can become important stressors.32 Hence, stress management interventions that recognize and address different sources of stress for men and women would be beneficial.
This study has several limitations. First, because VIRGO was composed of patients who voluntarily enrolled in the study and survived the initial hospitalization, our sample may not be representative of the overall young and middle-aged AMI patient population in the three study countries. However, many key clinical characteristics (e.g., STEMI versus NSTEMI, prior AMI, history of heart failure, systolic blood pressure, heart rate, and smoking status) of American and Spanish patients in our sample were comparable to those reported in other studies of young and middle-aged adults hospitalized for AMI in the U.S.18, 33, 34 and Span.35 We recognize that our sample size for Australia is relatively small, which may limit generalizability of our data to the broader Australian patient population. Second, baseline stress was measured during the AMI hospitalization. Although the PSS instrument assessed patients’ experience over the past month, their responses might be disproportionately influenced by the AMI event and thus the PSS scores should be interpreted as reflecting patient experience surrounding AMI event, rather than prior to AMI. Third, due to longitudinal nature of the study, some patients were lost to follow-up at one-month after AMI. If they were less healthy than the remaining patients and were disproportionately distributed between men and women, our estimated sex difference in recovery may be biased. However, our data suggest that rates of lost to follow-up were comparable between men (8.3%) and women (8.3%), and baseline sociodemographic and clinical attributes were generally similar between those who were lost to follow-up and those remained in the sample. Fourth, our measure of work-related strain was crude and did not reflect detailed job nature such as psychological demand and decision latitude at work as hypothesize in the job demand-control model.36 Nonetheless, this would only affect our ability to identify factors contributing to perceived stress, and should not affect our estimated sex difference in perceived stress (which was measured by PSS-14) and its relationship with one-month recovery. Finally, our study was limited to recoveries during the first month after AMI. Further research analyzing longer-term outcomes will provide additional insights regarding the role of mental stress in influencing recovery in young and middle-aged AMI patients. However, examining early recovery at one-month post-AMI still provides important data expanding our understanding of sex differences in recovery as the association between sex and outcomes may vary during the course of recovery.37
Although 35,000 women under 65 years of age experience myocardial infarction each year in the U.S.,38 there is very limited data on baseline psychosocial characteristics and recovery outcomes of young and middle-aged women with AMI. 16 In this study, we demonstrated a significantly higher level of mental stress in women 18–55 years old with AMI, compared to their male counterparts. Baseline stress was an important risk factor for poor recovery in young and middle-aged AMI patients and adjustment for baseline mental stress partially attenuated the observed sex gap in early recovery. However, the effect of baseline stress on recovery did not vary between men and women and significant sex differences in recovery remained even after adjustment for baseline perceived stress. Continued effort is needed to understand the physiological pathways underlying the relationships among sex, perceived stress and post-AMI recovery and to identify additional risk factors that may account for the excess adverse outcomes in women and determine reasons for their disproportionate burden of mental stress.
Supplementary Material
Acknowledgments
We thank Rachel P. Dreyer, BSc(Hons), PhD, for her work in leading/coordinating data collection for VIRGO in Australia and for her administrative support in implementing this study.
Funding Sources: This research project is supported by R01 HL081153-01A1K from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services. IMJOVEN (VIRGO in Spain) was supported by PI 081614 from the Fondo de Investigaciones Sanitarias del Instituto Carlos III, Ministry of Science and Technology, and additional funds from the Centro Nacional de Investigaciones Cardiovasculares (CNIC). VIRGO Australia was in part supported by the Hospital Research Foundation Program Grant for the Vascular Disease Therapeutic Research Group. Drs. Xu and Krumholz were supported by grant U01 HL105270-04 (Center for Cardiovascular Outcomes Research at Yale University). Dr. Bueno was supported in part by grant BA08/90010 from the Fondo de Investigación Sanitaria del Instituto de Salud Carlos III, Spain.
Footnotes
Disclosures: Dr. Krumholz reports that he is the recipient of a research grant from Medtronic, Inc. through Yale University, to develop methods of clinical trial data sharing and is chair of a cardiac scientific advisory board for UnitedHealth. Dr. Bueno has received advisory/consulting fees from AstraZeneca, Bayer, BMS, Daichii-Sankyo, Eli-Lilly, Menarini, Novartis, Sanofi, and Servier, and research grants from AstraZeneca.
References
- 1.Grewal K, Gravely-Witte S, Stewart DE, Grace SL. A simultaneous test of the relationship between identified psychosocial risk factors and recurrent events in coronary artery disease patients. Anxiety Stress Coping. 2011;24:463–475. doi: 10.1080/10615806.2010.546838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leifheit-Limson EC, Reid KJ, Kasl SV, Lin H, Jones PG, Buchanan DM, Parashar S, Peterson PN, Spertus JA, Lichtman JH. The role of social support in health status and depressive symptoms after acute myocardial infarction: Evidence for a stronger relationship among women. Circ Cardiovasc Qual Outcomes. 2010;3:143–150. doi: 10.1161/CIRCOUTCOMES.109.899815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parashar S, Rumsfeld JS, Reid KJ, Buchanan D, Dawood N, Khizer S, Lichtman J, Vaccarino V. Impact of depression on sex differences in outcome after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:33–40. doi: 10.1161/CIRCOUTCOMES.108.818500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peter R, Siegrist J, Hallqvist J, Reuterwall C, Theorell T. Psychosocial work environment and myocardial infarction: Improving risk estimation by combining two complementary job stress models in the sheep study. J Epidemiol Community Health. 2002;56:294–300. doi: 10.1136/jech.56.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-amorn C, Sato H, Yusuf S. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the interheart study): Case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 6.von Kanel R, Hari R, Schmid JP, Saner H, Begre S. Distress related to myocardial infarction and cardiovascular outcome: A retrospective observational study. BMC Psychiatry. 2011;11:98. doi: 10.1186/1471-244X-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnold SV, Smolderen KG, Buchanan DM, Li Y, Spertus JA. Perceived stress in myocardial infarction: Long-term mortality and health status outcomes. J Am Coll Cardiol. 2012;60:1756–1763. doi: 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 9.Kivimaki M, Nyberg ST, Batty GD, Fransson EI, Heikkila K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, Clays E, De Bacquer D, Dragano N, Ferrie JE, Geuskens GA, Goldberg M, Hamer M, Hooftman WE, Houtman IL, Joensuu M, Jokela M, Kittel F, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Kumari M, Madsen IE, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Rugulies R, Salo P, Siegrist J, Singh-Manoux A, Suominen SB, Vaananen A, Vahtera J, Virtanen M, Westerholm PJ, Westerlund H, Zins M, Steptoe A, Theorell T. Job strain as a risk factor for coronary heart disease: A collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491–1497. doi: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen SJ. Construction and preliminary validation of a dictionary for cognitive rigidity: Linguistic markers of overconfidence and overgeneralization and their concomitant psychological distress. J Psycholinguist Res. 2012;41:347–370. doi: 10.1007/s10936-011-9196-9. [DOI] [PubMed] [Google Scholar]
- 11.Orth-Gomer K. Psychosocial and behavioral aspects of cardiovascular disease prevention in men and women. Curr Opin Psychiatry. 2007;20:147–151. doi: 10.1097/YCO.0b013e32802b705e. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, McLeod JD, Wethington E. The costs of caring: A perspective on the relationship between sex and psychological distress. In: Sarason IG, Sarason BR, editors. Social support: Theory, research, and applications. Boston, MA: Martinus Nijhoff; 1985. pp. 491–507. [Google Scholar]
- 13.Garavalia LS, Decker C, Reid KJ, Lichtman JH, Parashar S, Vaccarino V, Krumholz HM, Spertus JA. Does health status differ between men and women in early recovery after myocardial infarction? J Womens Health (Larchmt) 2007;16:93–101. doi: 10.1089/jwh.2006.M073. [DOI] [PubMed] [Google Scholar]
- 14.Steiner C, Barrett M, Weiss A. Hcup projections: Cardiovascular/cerebrovascular conditions and procedures 2011 to 2012. HCUP Methods Series. 2012 [Google Scholar]
- 15.Cohen S, Janicki-Deverts D. Who’s stressed? Distributions of psychological stress in the united states in probability samples from 1983, 2006, and 2009. J Appl Soc Psych. 2012;42:1320–1334. [Google Scholar]
- 16.Lichtman JH, Lorenze NP, D’Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM, Krumholz HM. Variation in recovery: Role of gender on outcomes of young ami patients (virgo) study design. Circ Cardiovasc Qual Outcomes. 2010;3:684–693. doi: 10.1161/CIRCOUTCOMES.109.928713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bellasi A, Raggi P, Merz CN, Shaw LJ. New insights into ischemic heart disease in women. Cleveland Clin J Med. 2007;74:585–594. doi: 10.3949/ccjm.74.8.585. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Fang J, Gillespie C, Wang G, Hong Y, Yoon PW. Age-specific gender differences in in-hospital mortality by type of acute myocardial infarction. Am J Cardiol. 2012;109:1097–1103. doi: 10.1016/j.amjcard.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Kim ES, Menon V. Status of women in cardiovascular clinical trials. Arterioscler Thromb Vasc Biol. 2009;29:279–283. doi: 10.1161/ATVBAHA.108.179796. [DOI] [PubMed] [Google Scholar]
- 20.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 21.Cohen S, Williamson G. Psychological stress in a probability sample of the united states. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont symposium on applied social psychology. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- 22.Hewitt PL, Flett GL, Mosher SW. The perceived stress scale: Factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess. 1992;14:247–257. [Google Scholar]
- 23.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the seattle angina questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 24.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 25.EuroQol Group. Euroqol - a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 26.Enhancing recovery in coronary heart disease patients (enrichd): Study design and methods. The enrichd investigators. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 27.Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, Froelicher ES, Czajkowski S, Youngblood M, Huber M, Berkman LF. A short social support measure for patients recovering from myocardial infarction: The enrichd social support inventory. J Cardiopulm Rehabil. 2003;23:398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Vaglio J, Jr, Conard M, Poston WS, O’Keefe J, Haddock CK, House J, Spertus JA. Testing the performance of the enrichd social support instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. doi: 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore JM, Budaj A, Avezum A, Flather MD, Fox KA, Investigators G. A validated prediction model for all forms of acute coronary syndrome: Estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004;291:2727–2733. doi: 10.1001/jama.291.22.2727. [DOI] [PubMed] [Google Scholar]
- 30.The Joint Commission. Acute myocardial infarction. 2013 [Google Scholar]
- 31.Kershaw KN, Brenes GA, Charles LE, Coday M, Daviglus ML, Denburg NL, Kroenke CH, Safford MM, Savla T, Tindle HA, Tinker LF, Van Horn L. Associations of stressful life events and social strain with incident cardiovascular disease in the women’s health initiative. J Am Heart Assoc. 2014;3:e000687. doi: 10.1161/JAHA.113.000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams K, Kurina LM. The social structure, stress, and women’s health. Clin Obstet Gynecol. 2002;45:1099–1118. doi: 10.1097/00003081-200212000-00018. [DOI] [PubMed] [Google Scholar]
- 33.Awad HH, McManus DD, Anderson FA, Jr, Gore JM, Goldberg RJ. Young patients hospitalized with an acute coronary syndrome. Coron Artery Dis. 2013;24:54–60. doi: 10.1097/MCA.0b013e32835b0bf7. [DOI] [PubMed] [Google Scholar]
- 34.Tisminetzky M, McManus DD, Gore JM, Yarzebski J, Coles A, Lessard D, Goldberg RJ. 30-year trends in patient characteristics, treatment practices, and long-term outcomes of adults aged 35 to 54 years hospitalized with acute myocardial infarction. Am J Cardiol. 2014;113:1137–1141. doi: 10.1016/j.amjcard.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morillas P, Bertomeu V, Pabon P, Ancillo P, Bermejo J, Fernandez C, Aros F PRIAMHO II Investigators. Characteristics and outcome of acute myocardial infarction in young patients. The PRIAMHO II study. Cardiology. 2007;107:217–225. doi: 10.1159/000095421. [DOI] [PubMed] [Google Scholar]
- 36.Karasek R. Demand/control model: A social, emotional, and physiological approach to stress risk and active behaviour. In: Hurrell J, Joseph J, Levi, Lennart, Murphy, Lawrence R, Sauter, Steven L, editors. Theories of job stress. Geneva: International Labor Organizatio; 2011. [Google Scholar]
- 37.Bonarjee VV, Rosengren A, Snapinn SM, James MK, Dickstein K group Os. Sex-based short- and long-term survival in patients following complicated myocardial infarction. Eur Heart J. 2006;27:2177–2183. doi: 10.1093/eurheartj/ehl160. [DOI] [PubMed] [Google Scholar]
- 38.Women’s Heart Foundation. Women and heart disease facts. West Trenton, NJ: [Accessed August 21, 2013]. Available at: http://www.womensheart.org/content/heartdisease/heart_disease_facts.asp. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.