Preeclampsia is a hypertensive, multisystem disorder of pregnancy that occurs after 20 weeks of gestation and is the most common form of high blood pressure that complicates pregnancy. Preeclampsia is classically defined as new onset hypertension with proteinuria although some women present with hypertension and other multisystem symptoms indicative of preeclampsia, such as thrombocytopenia, impaired liver function, new development of renal insufficiency, or cerebral disturbances, without proteinuria.1 Preeclampsia affects 5% to 8% of pregnancies worldwide and is a major cause of maternal, fetal, and neonatal morbidity and mortality.2 Preeclampsia is thought to develop as a result of insufficient spiral artery remodeling due to shallow invasion of trophoblasts; this results in an ischemic placenta that secretes soluble factors into the maternal circulation, which leads to systemic endothelial and vascular dysfunction. However, the underlying pathophysiologic mechanisms leading to the development of preeclampsia remain elusive.2 The only effective treatment for the abatement of preeclampsia symptoms is delivery of the placenta. The lack of mechanistic understanding makes early diagnosis and prevention of preeclampsia nearly impossible. Therefore, the identification of biomarkers for early diagnosis is of great importance. Moreover, novel biomarkers may lead to the identification of new therapeutic targets that could result in the development of more effective treatment options for this devastating disease.
Yeung et al3 evaluated the potential use of copeptin as a predictive model of preeclampsia by examining the association between circulating copeptin and the development of preeclampsia or other pregnancy-associated disorders. There are currently only a handful of biomarkers suggested for potential predictive use for the development of preeclampsia. These biomarkers are grouped into 2 categories: angiogenic and immunologic.4 The potential angiogenic markers for preeclampsia are 2 serum proteins: proangiogenic placental growth factor and antiangiogenic soluble fms-like tyrosine kinase 1 (sFlt-1). Placental growth factor is a key player in the development of the placental vascular system and is found to be decreased in preeclampsia.2,4 Levels of sFlt-1 are found to be elevated as early as 5 weeks before the diagnosis of preeclampsia and directly correlate with disease severity. However, follow-up measurements of sFlt-1 suggest this measurement to be too unreliable for clinical use.4,5 An increased sFlt-1/placental growth factor ratio has been reported during midgestation in pregnancies that resulted in the development of preeclampsia and is proposed as a better predictive marker for preeclampsia than placental growth factor or sFlt-1 levels alone.4 The immunologic marker, placental protein 13, is proposed to function at the fetomaternal interface and in maternal vascular remodeling. Levels of placental protein 13 have been detected at abnormally low levels during the first trimester in women who eventually developed preeclampsia. However, first trimester serum levels, alone, are only suggested as an early diagnostic marker for mild preeclampsia but not for severe cases. Placental protein 13 serum levels coupled with uterine artery pulsatility index is suggested as a predictive model for severe preeclampsia.4 Pregnancy-associated plasma protein A is another immunologic marker that is shown to be decreased in plasma in the first trimester of women who subsequently developed preeclampsia. Measurement of pregnancy-associated plasma protein A, coupled with uterine Doppler studies, is suggested as a predictive model for preeclampsia. However measurement of plasma pregnancy-associated plasma protein A alone is more useful as a marker for intrauterine growth restriction. The identification of new potential biomarkers of preeclampsia before clinical diagnosis is of significant importance because of the limited number of biomarkers currently described.
In this issue of Hypertension, Yeung et al3 describe copeptin as a new, emerging predictive biomarker specific for preeclampsia. Copeptin is a glycopeptide that makes up the C-terminal portion of prepro-arginine vassopressin (prepro-AVP), which is the precursor protein of vasopressin (AVP), a vasoactive neuropituitary hormone.6 Copeptin acts as a carrier protein for vasopressin in conjunction with neurophysin II. The 2 carrier proteins are separated from AVP during transport to the pituitary gland and are secreted with AVP6 Vasopressin has a role in blood pressure regulation but primarily functions in water regulation and homeostasis of electrolytes.6,7 It has also been suggested that AVP is involved in the pathophysiology of preeclampsia.7 However, the short half-life and instability of AVP make reliable measurement of this protein improbable. Copeptin is produced in a 1:1 ratio to AVP, has a longer half-life, is more stable in serum and in plasma-isolated samples than AVP, and has no known physiological function. Therefore, copeptin levels are used as a surrogate measurement for vasopressin secretion. Moreover, copeptin has also previously been studied as a potential diagnostic and prognostic biomarker for various other diseases.6
The current study by Yeung et al3 examined the association between circulating copeptin and development of preeclampsia, gestational hypertension, gestational diabetes mellitus, and preterm birth in 136 normal pregnant women, 71 preterm preeclampsia, 88 gestational diabetes mellitus, 86 preterm birth, 78 gestational hypertension, and 89 term preeclampsia cases. Copeptin was measured in patient serum samples using a sandwich immunoluminometric assay. The authors report that baseline levels of copeptin taken at or ≈16-weeks gestation were significantly and positively correlated with the risk of preeclampsia before diagnosis. When adjusted for covariates, copeptin was no longer associated with term preeclampsia risk but remained associated with risk of preterm preeclampsia. In addition, increased copeptin levels were more strongly associated with severe than mild preeclampsia. Copeptin levels were associated with increased risk of preterm birth but not after being adjusted for race and were also found not to be associated with gestational hypertension or gestational diabetes mellitus. These data suggest that abnormally high levels of copeptin are specifically associated with increased risk of preeclampsia and not with other pregnancy-associated morbidities.3 A significant limitation of this study is that the findings are purely associative and provide no mechanistic link between copeptin levels, or vasopressin secretion, and the development of preeclampsia.
A few other studies have measured copeptin in regard to its association with preeclampsia. Zulfikaroglu et al8 first measured serum levels of copeptin in 32 normotensive, 32 mild preeclamptic, and 32 severe preeclamptic women during the third trimester of pregnancy. They found that copeptin levels to be significantly higher in preeclamptic women when compared with that in normotensive pregnant women. Moreover, women with severe preeclampsia had higher serum copeptin levels than those with mild preeclamptics. Copeptin was found to be significantly increased in preeclamptic women with abnormal Doppler velocimetry when compared with preeclamptic women with normal Doppler velocimetry.8 In a different study aimed at examining the effects of vaginal delivery versus cesarean delivery on copeptin levels in different groups of pregnant women, preeclamptic women were found to have greater copeptin when compared with normotensive women.9 Wellman et al10 examined the ability of several cardiovascular biomarkers to predict preeclampsia in pregnant women presenting in triage and found that all cardiovascular biomarkers tested, including copeptin, were increased in patients with preeclampsia. A more recent study measured maternal plasma levels of copeptin throughout pregnancy in 54 control pregnant, 50 preeclamptic pregnant, and 33 nonpregnant women.5 Copeptin was assessed and found to be significantly higher, in all 3 trimesters, in pregnant women who subsequently developed preeclampsia when compared with women who remained normotensive throughout pregnancy. Receiver operating characteristic curves of the data also revealed that maternal plasma levels of copeptin in all 3 trimesters, even as early as 6 weeks, were predictive of the development of preeclampsia, even when controlling for clinical covariates.5 In addition, copeptin can now easily be measured using commercially available ELISAs. Collectively, this suggests that copeptin may be a good candidate biomarker for efficient first-trimester prediction of imminent preeclampsia. To be of clinical use, studies are needed to determine the range of increased copeptin that is predictive of preeclampsia. In addition, methods are needed for rapid measurement of copeptin in clinical/hospital laboratories or for point-of-care testing.
The study by Yeung et al3 is much larger than any previous study in which copeptin levels were found to be associated with preeclampsia.3 Moreover, the authors demonstrated that increased copeptin is specifically predictive to the development of preeclampsia and not with other pregnancy-related cardiovascular and renal complications. Although these studies show an association between copeptin levels, and thus vasopressin secretion, with development of preeclampsia, a role for vasopressin in the pathophysiology of preeclampsia has not been elucidated. In a previously mentioned study, Santillan et al5 demonstrated that chronic infusion of AVP before conception and throughout gestation led to the development of preeclampsia-like symptoms, including hypertension, proteinuria, and intrauterine growth restriction, in a mouse model. This suggests that abnormally high AVP secretion during pregnancy may be directly involved in the development of preeclampsia. Additional studies to elucidate a mechanistic link between AVP secretion and development of preeclampsia are necessary. The specific pathways, mechanisms, and specific AVP receptors activated to elicit the effects of AVP in pregnancy are needed to increase our understanding of the role of vasopressin in the pathophysiology of preeclampsia (Figure). Studies to investigate the cause of AVP over secretion should also be undertaken. In addition, the effect of AVP receptor antagonists on pathophysiology of preeclampsia is a pharmacological angle that should be explored. This study by Yeung et al3 will contribute to the identification of therapeutic targets and the development of effective prevention and treatment strategies for this disease and may open new areas of research in preeclampsia.
Figure.
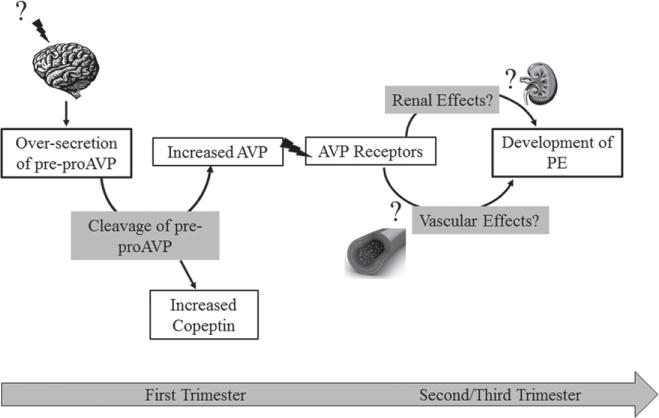
Hypothetical relationship of copeptin to preeclampsia (PE). Early in pregnancy an unknown factor(s) triggers the release of prepro–arginine vassopressin (prepro-AVP) from the brain. On cleavage of this precursor protein, AVP and measureable copeptin levels are increased in the circulation. In normal pregnancy, copeptin levels increase throughout gestation. However, an oversecretion of prepro-AVP leads to significantly increased AVP and copeptin levels. Increased AVP triggers overactivation of AVP receptors, which have currently unknown renal and vascular effects that lead to the development of PE in the second or third trimester of pregnancy.
Footnotes
Disclosures
None.
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.American College of Obstetricians and Gynecologists. Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–1131. doi: 10.1097/01.AOG.0000437382.03963.88. [DOI] [PubMed] [Google Scholar]
- 2.George EM, Granger JP. Recent insights into the pathophysiology of preeclampsia. Expert Rev Obstet Gynecol. 2010;5:557–566. doi: 10.1586/eog.10.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yeung EH, Liu A, Mills JL, Zhang C, Mannisto Y, Lu Z, Tsai MY, Mendola P. Increased levels of copeptin before clinical diagnosis of preeclampsia. Hypertension. 2014;64:xxx–xxx. doi: 10.1161/HYPERTENSIONAHA.114.03762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kar M. Role of biomarkers in early detection of preeclampsia. J Clin Diagn Res. 2014;8:BE01–BE04. doi: 10.7860/JCDR/2014/7969.4261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santillan MK, Santillan DA, Scroggins SM, Min JY, Sandgren JA, Pearson NA, Leslie KK, Hunter SK, Zamba GK, Gibson-Corley KN, Grobe JL. Vasopressin in preeclampsia: a novel very early human pregnancy biomarker and clinically relevant mouse model. Hypertension. 2014;64:xxx–xxx. doi: 10.1161/HYPERTENSIONAHA.114.03848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobsa L, Edozien KC. Copeptin and its potential role in diagnosis and prognosis of various diseases. Biochem Med (Zagreb) 2013;23:172–190. doi: 10.11613/BM.2013.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krege JH, Katz VL. A proposed relationship between vasopressinase altered vasopressin and preeclampsia. Med Hypotheses. 1990;31:283–287. doi: 10.1016/0306-9877(90)90020-f. [DOI] [PubMed] [Google Scholar]
- 8.Zulfikaroglu E, Islimye M, Tonguc EA, Payasli A, Isman F, Var T, Danisman N. Circulating levels of copeptin, a novel biomarker in preeclampsia. J Obstet Gynaecol Res. 2011;37:1198–1202. doi: 10.1111/j.1447-0756.2010.01498.x. [DOI] [PubMed] [Google Scholar]
- 9.Foda AA, Abdel Aal IA. Maternal and neonatal copeptin levels at cesarean section and vaginal delivery. Eur J Obstet Gynecol Reprod Biol. 2012;165:215–218. doi: 10.1016/j.ejogrb.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Wellmann S, Benzing J, Fleischlin S, Morgenthaler N, Fouzas S, Buhrer CA, Szinnai G, Burkhardt T, Lapaire O. Cardiovascular biomarkers in preeclampsia at triage. Fetal Diagn Ther. doi: 10.1159/000361016. [published online ahead of print May 17, 2014] http://www.karger.com/Article/FullText/361016. Accessed August 4, 2014. [DOI] [PubMed]


