Abstract
Recent years have brought notable progress in the field of IgA nephropathy. Here, we highlight important new directions and latest developments, including successful discovery of several genetic susceptibility loci, formulation of the multi-hit pathogenesis model that integrates findings from studies of galactose-deficient IgA1, anti-glycan response and immune complex-induced kidney injury, introduction of the Oxford pathology scoring system, and formalization of the Kidney Disease Improving Global Outcomes (KDIGO) consensus treatment guidelines. We focus on the latest genetic findings that confirm a strong contribution of inherited factors and explain some of the geo-ethnic disparities in disease susceptibility. Most IgA nephropathy susceptibility loci discovered to date encode genes involved in the maintenance of the intestinal epithelial barrier and response to mucosal pathogens. The concerted pattern of inter-population allelic differentiation across all Genome Wide Association Studies (GWAS) loci parallels the disease prevalence and correlates with variation in local pathogens, suggesting that multi-locus adaptation might have shaped the present-day landscape of IgA nephropathy. Importantly, the “Intestinal Immune Network for IgA Production” emerged as one of the new targets for potential therapeutic intervention. We place these findings in the context of the multi-hit pathogenesis model and existing knowledge of IgA immunobiology. Lastly, we provide our perspective on the existing treatment options, discuss areas of clinical uncertainty, and outline ongoing clinical trials and translational studies.
Keywords: IgA nephropathy, O-glycosylation, GWAS, glomerulonephritis, adaptive immunity, innate immunity, complement system, treatment
Introduction
Since its description in 1968 1, IgA nephropathy (IgAN) has been recognized as the most common form of primary glomerulonephritis and an important cause of chronic kidney disease and end stage kidney failure. Recent years have brought remarkable progress in the field of IgAN, largely due to increased collaborative efforts that enabled execution of well-powered clinical and genetic studies. Landmark developments include the discovery of new genetic susceptibility loci, formulation of the multi-hit pathogenesis model based on the studies of IgA1 O-glycosylation and anti-glycan antibodies, introduction of the Oxford pathology scoring system, as well as formalization of IgAN treatment guidelines. In this review, we provide an update on these developments, give our perspective on the treatment guidelines, outline the remaining areas of uncertainty, and highlight important new directions in the field.
The Diagnosis of IgA Nephropathy
IgAN typically affects young adults, but can also occur in children and the elderly. The disease has a wide spectrum of clinical symptoms, ranging from asymptomatic microscopic hematuria to a more severe course characterized by sustained proteinuria and rapid deterioration of renal function. Definitive diagnosis of IgAN requires a kidney biopsy; the disease is defined immunohistologically by dominant or co-dominant glomerular deposits of IgA 2. According to recent consensus, the IgA should be at least 1+ in intensity 3 and in most cases is 2+ or more 4, and involves the glomeruli diffusely. Typically there is obvious dominant staining for IgA with weaker and more variable staining for IgG and/or IgM 4. The deposits consist predominantly of polymeric IgA of the IgA1 subclass 5. Among 2,249 cases of IgAN compiled from 13 published biopsy series, 100% of cases had positivity for IgA, 43% had positivity for IgG and 54% for IgM 6. The stronger staining for lambda light chain than kappa light chain observed in most cases reflects the predominance of IgA1-lambda in the circulation 7.
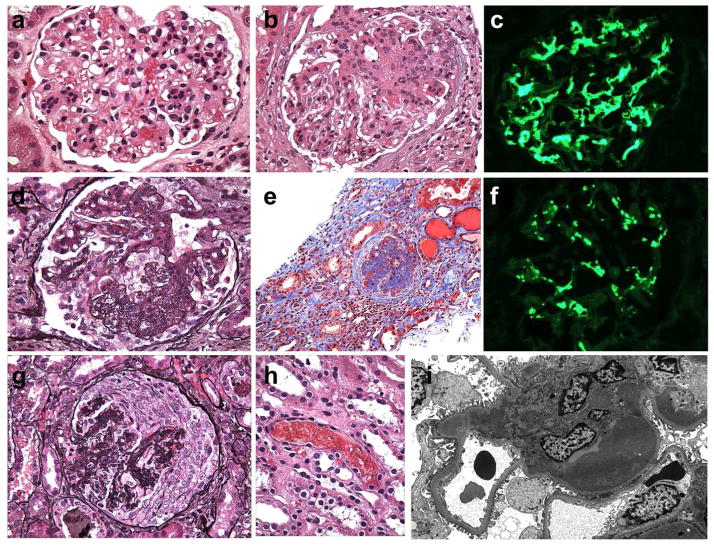
The histologic features of IgAN are diverse and span the gamut seen in most forms of immune complex-mediated proliferative glomerulonephritis (Figure 1). These include no or minimal abnormalities by light microscopy, mesangial hypercellularity (defined as 4 or more mesangial cells per mesangial area in a 3 μm-thick histologic section, Figure 1a), focal endocapillary proliferative (involving <50% glomeruli, Figure 1b), diffuse endocapillary proliferative (involving ≥50% glomeruli), necrotizing and crescentic lesions, and more rarely membranoproliferative patterns of injury 3,8. Red blood cell casts may be associated with acute tubular injury (Figure 1h). In the chronic stages, progression to focal or diffuse segmental and global glomerulosclerosis 9 with attendant tubular atrophy and interstitial fibrosis occurs (Figure 1d and e).
Figure 1. Pathologic features of IgA nephropathy by light microscopy, immunofluorescence and electron microscopy.
(a) The glomerulus has global mesangial proliferation with at least 4 cells per mesangial area. When >50% of glomeruli exhibit mesangial hypercellularity, the biopsy receives a score of M1 according to the Oxford/IgA MEST system (H&E, x600).
(b) Segmental endocapillary proliferation obliterates capillary lumina (score E1 when a biopsy contains one or more such lesions). The adjacent glomerular segments have mild mesangial hypercellularity (H&E, x600).
(c) The stain for IgA is intense and globally outlines the mesangial framework of the glomerulus (immunofluorecence, x600).
(d) Segmental glomerular scarring develops as postinflammatory sclerosis, mimicking the changes in focal segmental glomerulosclerosis. (score S1 when a biopsy contains one or more such lesions), (Jones methenamine silver, x600).
(e) A case with high chronicity contains globally sclerotic glomeruli and exhibits more than 50% tubular atrophy/interstitial fibrosis (score T2), (Masson trichrome, x200).
(f) The immunofluorescence staining for C3 is similar in distribution as the mesangial staining for IgA (shown from the same glomerulus as in 1C) but exhibits weaker intensity and a more punctate, granular texture (immunofluorescence, x600).
(g) A severe example has a cellular crescent that compresses the glomerular tuft. Global mesangial expansion is present (Jones methenamine silver, x400).
(h) One or more red blood cell casts are commonly encountered at biopsy and may be numerous, especially in cases with gross hematuria and acute tubular injury (H&E, x600).
(i) By electron microscopy, large mesangial deposits elevate the glomerular basement membrane reflection over the mesangium, bulging towards the urinary space. This deposit involves the entire mesangium but is most prominent in the paramesangial region, beneath the GBM reflection. The mesangial cellularity is increased but the capillary lumen is patent (electron micrograph, x5000).
By electron microscopy, the glomerular deposits in IgAN are primarily localized to the mesangium, with variable subendothelial and rare subepithelial deposits in the more severe forms. Mesangial deposits tend to cluster beneath the glomerular basement membrane reflection over the mesangium, a location referred to as paramesangial (Figure 1i). The glomerular basement membranes may manifest focal thinning, rupture and remodeling, which present sources for hematuria.
Henoch-Schönlein purpura nephritis (HSPN) is a systemic form of IgA vasculitis (IgAV) with renal manifestations that occurs predominantly in the pediatric age group 10. This disease typically manifests with a tetrad of palpable purpura, arthralgia, abdominal pain, and renal disease. Although HSPN is frequently self-limiting in children, persistent proteinuria and chronic or progressive renal dysfunction are often observed in adult cases 11. The renal disease has a similar histologic spectrum as IgA nephropathy, but with greater frequency of severe lesions such as glomerular necrosis and crescents (Figure 1g) 12. Correspondingly, HSPN has a higher frequency of glomerular staining for fibrin than IgAN, but with an otherwise similar immunofluorescence profile.
Heuristic classification systems applied to IgAN in the past, including those by Lee et al. 13 and Haas et al. 8, were based on the pattern and severity of the proliferative and sclerosing lesions, similar to the WHO classification of lupus nephritis. The Oxford IgAN classification, devised by a working group of over 40 nephrologists and pathologists representing the International IgA Nephropathy Network and the Renal Pathology Society, is unique as the first evidence-based schema 3,14. It sought to identify reproducible histologic features that predict progression in a large disease cohort with known outcomes, and thus represents a scoring system, not a comprehensive classification. The discovery cohort included 265 cases of IgAN from Europe, North America and Asia, of which 78% were adults. Because the study excluded cases with proteinuria of <0.5 g/day, initial eGFR of <30 mL/min per 1.73 m2 and progression to ESRD within 12 months of biopsy, patients with very mild disease, rapidly progressive glomerulonephritis, and advanced chronic disease were underrepresented 14. Three reproducible histologic features correlated independently with both the rate of renal functional decline and renal survival endpoints (defined as ≥ 50% reduction in eGFR or ESRD), namely diffuse mesangial hypercellularity (M), segmental glomerulosclerosis (S) and tubular atrophy/interstitial fibrosis involving >25% of the cortical area (T) 3. Tubular atrophy/interstitial fibrosis involving >50% (versus 26–50%) of the cortex was associated with even worse outcomes. Endocapillary hypercellularity (E) was associated with response to immunosuppressive therapy. The MEST score applies the designations M0 or M1 for mesangial hypercellularity involving ≤50% or >50% of glomeruli, respectively; E0 or E1 for endocapillary hypercellularity in 0 versus at least 1 glomerulus, S0 or S1 for segmental sclerosis in 0 versus at least 1 glomerulus, and T0, T1 and T2 for tubular atrophy/interstitial fibrosis involving ≤25%, 26–50%, and >50% of the cortical area, respectively 3. The major limitation of the Oxford system is that the study design constrained its ability to fully address the impact of crescents and specific immunofluorescence features, such as the presence of peripheral capillary wall deposits of IgA and co-deposits of IgG.
A number of studies have attempted to validate the predictive value of the MEST lesions in independent cohorts from North America 15,16, Europe 17–20 and Asia 21–29, including pediatric cases 30,31. These studies have generally confirmed the predictive value of various components by univariate and multivariate analyses, but with some differences 32,33. The largest meta-analysis based on 16 retrospective cohort studies and involving a total of 3,893 IgAN cases validated the predictive utility of the M, S, and T lesions, but did not confirm the prognostic value of the E score 33. While the E score exhibited some of the weakest and most heterogeneous associations with disease progression, the T score was consistently the most significant predictor of poor renal outcomes across all cohorts. In addition, five of 16 studies (4 Asian and 1 European with a total of 1,487 patients) examined the association of crescents with clinical outcomes; meta-analysis of these studies showed that the C score (defined as presence of any crescents) was strongly associated with progression to kidney failure 33. Lastly, the recently published VALIGA study of 1,147 patients from 13 European countries (not included in the above meta-analysis) provided an independent validation of the predictive value of the M, S and T lesions across a broader spectrum of the disease 31. The E score, again, was not associated with outcomes. However, the relationship between some variables, such as the E score, and clinical outcomes might have been confounded by immunosuppressive treatment exposure, since all of the published validation studies have been based on retrospective observational data.
In summary, the Oxford scoring system represents an important step toward improved prognostication and standardization of diagnosis, but further refinements of the score may be needed to enhance its prognostic utility. A more definitive assessment of the scoring system would require a sizable randomized controlled trial in which decisions regarding therapy are not made on the basis of pathology. The TESTING study (see below) may present a unique opportunity to validate and refine this scoring system while removing inherent therapeutic biases.
The Epidemiology of IgA Nephropathy
Because the diagnosis of IgAN requires a kidney biopsy, the exact disease prevalence remains difficult to establish. The prevalence of mesangial IgA deposits assessed in necropsy studies is surprisingly high, ranging from 4% to 16% depending on the population studied 34–36. Similarly, the frequency of IgA deposition in protocol biopsies of living or cadaveric donor kidneys is reported to be as high as 16% in Japan 37. These studies suggest that subclinical IgA deposition is common and may be more prevalent in East Asian populations.
Another commonly reported metric of IgAN occurrence is a relative frequency of IgAN among all cases of primary glomerulonephritis in a biopsy registry. Depending on the geographic region, this number tends to be highly variable, ranging from 5% in the Middle East38,39, 10–35% across Europe40–44 and up to 50% in Japan and China45,46. This metric, however, can be affected by disparities in local biopsy practices47 and local incidence of other glomerular diseases. An alternate approach to estimating the incidence of IgAN is to use data from national ESRD registries. These data still do not reflect true incidence as only the patients with progressive disease are captured. A subset of patients with “hypertension” as the cause of ESRD may also represent patients with IgAN who never underwent kidney biopsy. In the US, depending on the state of residence, the incidence of ESRD due to IgAN ranges from 18 to 264 cases per million population (USRDS 2009) 48. The high level of variability between states may be attributable to regional differences in racial/ethnic composition and accessibility to healthcare, but it may also reflect a general lack of consensus among clinicians on the utility of biopsy in specific clinical settings, resulting in high degree of regional disparities in biopsy practices even within the US.
Despite these limitations, some important prevalence patterns have clearly emerged 49. Most notably, there is a clear West-to-East prevalence gradient, with the disease being most common in East Asia (32–54% of primary GN in China 50 and Japan 51) compared to European countries (10–35% of primary GN) 41,42,44,52–63. Similar trends are observed when the incidence of ESRD due to IgAN is compared between ethnicities in the US. Asian-Americans have a 4-fold higher ESRD incidence due to IgAN compared to European-Americans, and a 7-fold higher incidence compared to African-Americans, further supporting a substantial role of genetic factors (USRDS data, 2009) 48. Additionally, a more subtle South-to-North prevalence gradient has also been described within Europe; Northern Europeans have up to 2.4-fold increased risk of ESRD due to IgAN compared to Southern Europeans 48. Lastly, IgAN occurrence has unequal gender distribution. In Europe and North America, the disease generally affects males more frequently than females, with male-to-female ratio as high as 3:1 in Europeans 64,65. In contrast, this ratio approximates 1:1 in East Asia 66–68, a pattern that may be shaped by differences in ancestry or local environments. These geographic differences also suggest that our existing definition of IgAN may encompass a number of distinct disease entities with differential distribution between Europe and Asia. Improved sub-classification of IgAN based on the underlying disease mechanism rather than descriptive pathology represents perhaps one of the greatest challenges for the IgAN research community. In this respect, some of the notable progress comes from genetic studies.
The Genetics of IgA Nephropathy
Multiple studies have recognized familial aggregation of IgAN 69–74. In most cases, the inheritance is suggestive of autosomal dominant pattern with variable penetrance; however, other more complex genetic models are also plausible. Although no large twin studies have been performed to formally estimate the heritability of IgAN, several cases of disease concordance in identical twins have been reported 75–77. The blood relatives of patients affected by IgAN also appear to be at a higher risk of urinary abnormalities 78 and have higher levels of galactose-deficient IgA1 79,80.
The first successful application of genome-wide linkage analysis to IgAN families identified the significant linkage peak on chromosome 6p22–23 under an autosomal dominant inheritance 81. Follow-up linkage studies reported additional suggestive peaks at several other loci, providing evidence for significant locus heterogeneity 73,82. Confirmation of these loci in the setting of heterogeneity represents a major challenge; if each family carries a unique molecular defect in a different gene, hundreds of families will not suffice to provide linkage replication. Newer approaches using next generation sequencing face the same limitation – considering significant genetic heterogeneity, finding an independent segregating mutation may require sequencing of thousands of probands. For this reason, the discovery of rare variants underlying familial IgAN has been challenging, and no causal mutations have been identified to date.
Genome-wide association studies (GWAS) represent an alternative approach to genetically complex traits, such as IgAN. In contrast to linkage studies, GWAS offer a powerful tool to identify susceptibility variants even in the setting of significant locus heterogeneity. The inherent limitations of GWAS include the ability to detect only common (frequency > 1–5%) variants, which typically exhibit relatively small effects; thus, GWAS tend to explain only a relatively small proportion of disease heritability 83. To date, GWAS has been successfully applied to IgAN in four large-scale studies that led to the identification of 15 distinct common risk variants at a genome wide significance (Table 1) 84–87. Cumulatively, the 15 new and replicated GWAS loci explain approximately 6–8% of the overall disease risk 87.
Table 1.
Summary of IgAN GWAS loci, their functions, pleiotropic effects, and potential role in the pathogenesis of IgAN.
| GWAS Candidate Genes | Structure, Function, and Gene Expression | Potential Relationship to the Multi-hit Pathogenesis Model | Pleiotropic Effects and Links to Other Immune- mediated Diseases |
|---|---|---|---|
| HLA-DQA1, HLA-DQB1, HLA-DRB1, |
|
|
|
| HLA-DP |
|
|
|
| TAP2, PSMB8, PSMB9 |
|
|
|
| CFHR1, CFHR3 |
|
|
|
| ITGAM, ITGAX |
|
|
|
| CARD9 |
|
|
|
| VAV3 |
|
|
|
| DEFA1, DEFA3, DEFA5, DEFA6 |
|
|
|
| TNFSF13 |
|
||
| LIF, OSM, HORMAD2, MTMR3 |
|
|
|
Although the overall disease risk explained by GWAS is relatively small, the hypothesis-free approach of GWAS provided novel and unbiased insights into human biology of IgAN. Most importantly, GWAS loci highlighted several pathogenic disease pathways and pointed to potential new therapeutic targets. The implicated pathways include antigen processing and presentation (MHC region), the complement system (CFHR1/3 and ITGAM-ITGAX loci), regulation of mucosal IgA production (TNFSF13 and LIF/OSM loci) and innate immunity against pathogens (DEFA, CARD9, ITGAM-ITGAX and VAV3 loci). The cumulative burden of GWAS risk alleles has a strong inverse relationship with the age at disease onset, with up to a 20-year difference between the cases with highest and lowest numbers of risk alleles 87. These observations may be clinically relevant and suggest that pediatric patients have a different disease pathogenesis compared to a late-onset adult disease, and thus may also differ in their responsiveness to specific treatments.
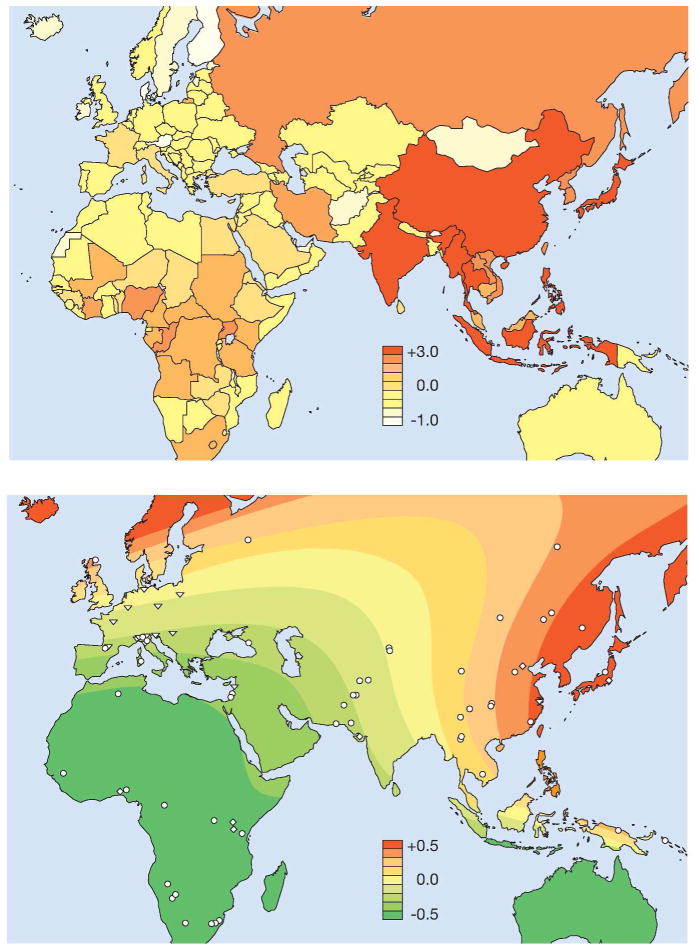
In the geospatial analysis of 6,319 individuals representative of 85 worldwide populations, the IgAN genetic risk increases sharply with eastward distance from Africa (Figure 2, top panel) 48. This model parallels the known West-to-East gradient in disease prevalence, suggesting that variation in frequency of GWAS risk alleles may partially explain the geo-epidemiology of IgAN (see URL for an online genetic risk calculator). Moreover, higher resolution geo-genetic analysis of the European continent revealed additional South-to-North risk gradient, which subsequently led to the discovery of a parallel trend in disease incidence. Similar to IgAN, higher latitude has been associated with increased risk of other immune diseases, such as multiple sclerosis, type I diabetes or inflammatory bowel disease, all of which share common susceptibility loci with IgAN 88–91. Complex selective pressures likely underlie these gradients.
Figure 2. Geospatial Pattern of Genetic Risk for IgA Nephropathy and Worldwide Map of Helminth Diversity.
Top Panel: Surface interpolation of the standardized genetic risk over Africa and Euroasia. Symbols represent the locations of sampled populations: Human Genome Diversity Panel (HGDP; 1,050 individuals representative of 52 worldwide populations), HapMap III (1,184 individuals representative of 11 populations), other population samples (4,547 individuals representative of 25 populations); from Kiryluk et al. PLoS Genetics 2012;8(6):e1002765.
Bottom Panel: Standardized values for the diversity of helminth species infecting humans per country; data from the Global Infectious Disease and Epidemiology Online Network (GIDEON), see URL.
The inter-population differences in genetic risk become even more pronounced for the latest set of GWAS loci. Interestingly, the risk alleles with largest effects tend to have the greatest population differentiation and contribute most to the observed geo-genetic patterns. For example, the ITGAM-ITGAX risk alleles demonstrate nearly complete fixation in East Asian populations. Taken together, these findings suggest that local selective pressures might have systematically increased the frequency of risk alleles in some populations through the process of multilocus adaptation. In the analysis of different ecological variables that could potentially provide a selective pressure that drives this adaptation, the diversity of endemic pathogens emerged as one of the strongest predictors of genetic risk. Among different pathogen classes, the strongest association was found for local helminth diversity (defined as a number of endemic helminthic species infecting humans in a given geographic area). Notably, worm infestations have been a major source of morbidity and mortality throughout human history, and even today helminthes infect nearly a quarter of the world population 92. The enhanced IgA response conferred by GWAS risk alleles is likely protective against these pathogens, but it can also explain the known association of mucosal infections as a common trigger for IgAN.
In aggregate, these findings gave rise to a novel hypothesis that higher genetic risk of IgAN in Asia represents an untoward consequence of protective adaptation to worm infections, the process that has likely occurred over thousands of years of human-parasite co-evolution. Despite recent amelioration of life conditions, availability of effective anti-helminthic therapies, and improvements in healthcare delivery, worm infections are far from being eradicated in these regions 92,93. Even in the most developed Asian countries, humans continue to be exposed to a high diversity of worm species (Figure 2, bottom panel). Moreover, the time scale of recent developments would not have been sufficiently long to reverse the effect of genetic adaptation. For example, Japan has some of the largest number of helminthic species infecting humans, despite the fact that the overall incidence of parasitic infections has declined recently. In parallel, Japanese carry the greatest load of IgAN risk alleles (Figure 2, top panel) and consistently have some of the highest metrics of IgAN prevalence worldwide. Further studies will be needed to test this intriguing new hypothesis.
The Multi-hit Pathogenesis Model
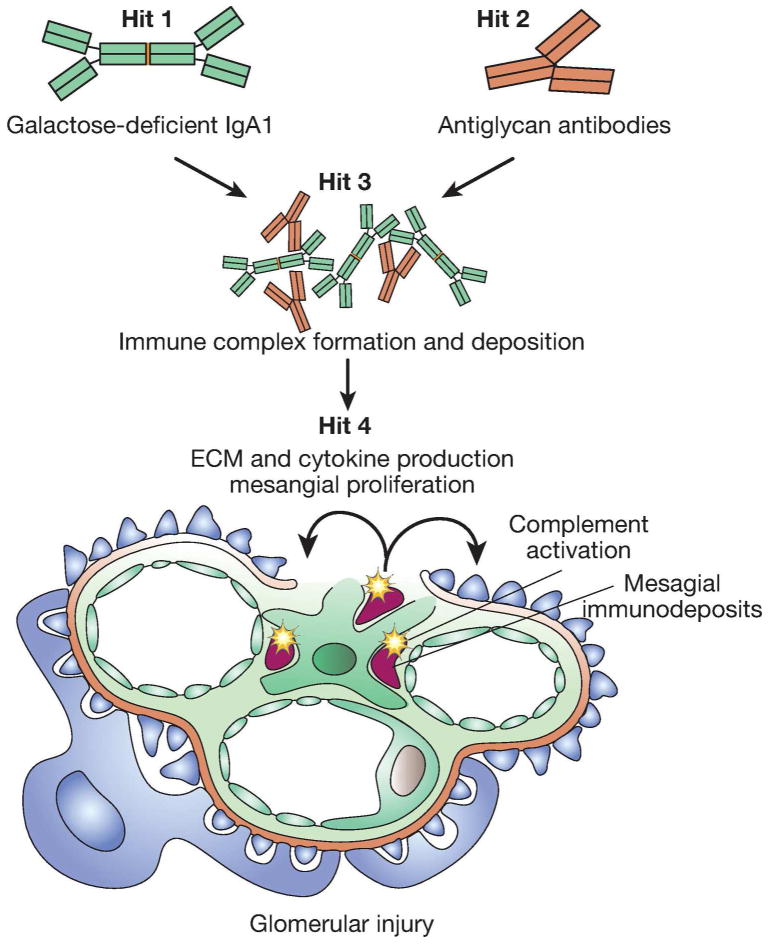
The originally proposed multi-hit pathogenesis model integrates findings from studies of galactose-deficient IgA1, anti-glycan response, formation and deposition of IgA1-containing immune complexes, and mechanisms of immune complex-mediated tissue injury 94 (Figure 3). Newer insights arising from GWAS contributed to the refinement of this model 95,96 and here we extend the model to incorporate the latest genetic data (Table 1). Abnormalities in the production of IgA1, leading to elevated levels of galactose-deficient IgA1 (Gd-IgA1), represent the first hit in the model. These IgA1 glycosylation defects have been shown to have high heritability 79,80. However, family-based studies also demonstrate that an elevated level of Gd-IgA1 alone is not sufficient to produce IgAN and additional co-factors are required to trigger the formation of immune complexes 79,80. More recent work suggests that elevated Gd-IgA1 elicits an autoimmune response, resulting in generation of anti-glycan antibodies that recognize N-acetylgalactosamine epitopes on Gd-IgA1 97. This anti-glycan response may represent a second hit in the model. The elevation of both Gd-IgA1 and anti-glycan antibodies leads to formation of immune complexes (Hit 3), which then deposit in the glomerular mesangium. This deposition activates the complement pathway, stimulates mesangial cells, and induces secretion of cytokines, chemokines, and extracellular matrix proteins resulting in inflammation and fibrosis (Hit 4). While this model likely oversimplifies the sequence of pathogenic events, it provides a conceptual framework for focused functional studies and testing of candidate genes.
Figure 3.
The Multi-hit Pathogenesis Model of IgA Nephropathy.
Defect in the regulation of IgA1 production and glycosylation (Hit 1)
Human IgA molecules are composed of two subclasses: IgA1 and IgA2; IgA1 is the predominant form in the circulation of healthy individuals and this subclass is also found in circulating immune complexes and mesangial immune deposits of patients with IgAN 98,99. The IgA1 molecule has a unique hinge segment between the first and second constant-region domains of the heavy chains that is the site of attachment of O-linked glycan moieties.
Multiple studies have shown that IgAN patients have significantly higher levels of circulating IgA1 with galactose-deficient O-linked glycans in the hinge region (Gd-IgA1), and this defect represents a risk factor for nephritis 99–103 and more rapid progression of kidney disease 104. Moreover, serum levels of Gd-IgA1 are highly heritable among the relatives of adult patients with IgAN 79 as well as pediatric IgAN and HSP nephritis 80, and these findings are reproducible in different ethnicities 105. The enzymatic pathway responsible for the elongation of IgA1 glycan chains has been studied extensively: the key enzymes include N-acetyl-galactosaminyltransferases-2 and −14 (GalNAc-T2 and GalNAc-T14), which link N-acetylgalactosamine to Serine or Threonine residues of the hinge region, followed by core-1-β1,3-galactosyltransferase-1 (C1GalT1) and its chaperone Cosmc, which add galacotose to N-acetylgalactosamine, and a number of sialyltransferases 96,99. Interestingly, the pattern of O-glycosylation is normal for IgD in patients with IgAN, suggesting that these enzymes may be altered specifically in IgA1-producing cells secondary to their aberrant immunoregulation 106. Furthermore, IgA1-secreting cell lines from patients with IgAN demonstrated a decrease in C1GalT1 activity and an increase in α-N-acetylgalactosaminide-α-2,6-sialyltransferase 2 (ST6GalNAc-II) activity, which suggests that premature sialylation of N-acetylgalactosamine may be contributing to this defect 107.
The glycosylation defects involve predominantly polymeric IgA1, which is normally produced by mucosal IgA1-secreting cells 108. Presently, it is not clear how polymeric Gd-IgA1 finds its way to the circulation in patients with IgAN. An intriguing possibility is that mucosal IgA1-secreting cells may migrate to the bone marrow or other systemic sites and that this “mis-trafficking” may occur because of faulty expression of surface homing receptors 109–111. An alternative hypothesis is that upon antigenic stimulation of genetically-predisposed individuals, there is an enhanced mucosal IgA1 response that leads to a “spill-over” from mucosal sites, leading to increased circulating levels of polymeric Gd-IgA1. Clinical associations of macroscopic hematuria coinciding with mucosal infections (“synpharyngitic hematuria”) further suggest that enhanced mucosal IgA responsiveness to an antigenic challenge triggers IgAN. These hypotheses are not mutually exclusive; exaggerated mucosal IgA1 responsiveness may lead to a “spill-over” of polymeric Gd-IgA1 into the circulation, while overstimulation of IgA1-secreting cells may promote “mis-trafficking” of these cells.
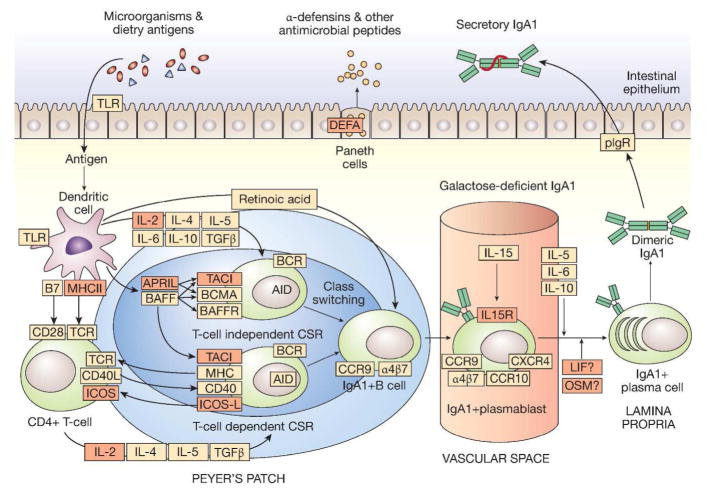
The interplay between mucosal pathogens and IgA immunity is central to the disease process; the inherited propensity for enhanced mucosal IgA production in response to microbial antigens represents a common pathway for most of the GWAS loci discovered to date (Figure 4, Table 1). For example, the TNFSF13 locus encodes a proliferation inducing ligand (APRIL) involved in T cell-independent generation of IgA-secreting plasma cells 112,113. The risk variant is associated with a higher serum IgA levels among IgAN cases 86,87. Inactivation of Tnfsf13 in mice produces reduced IgA antibody responses to mucosal immunization 114. Conversely, over-expression of B cell activating factor (BAFF), a related molecule with overlapping functions and receptors with APRIL, results in autoimmune disease with commensal flora-dependent mesangial IgA deposits in mice 115. Another GWAS locus on chromosome 22q12 encompasses several genes including the cytokine-encoding genes LIF and OSM 85. These cytokines are members of the IL-6 family, are expressed in mucosal tissues, and have immunoregulatory properties 116–118. The effects of LIF and OSM on mucosal production of IgA have not been well studied, but the IgAN risk allele at this locus has previously been associated with protection against Crohn’s disease, pointing to its involvement in the regulation of intestinal inflammation 119–121. Critically, the IgAN risk allele is also associated with higher serum IgA levels among IgAN patients 85,87.
Figure 4. Genetic Hits to the “Intestinal Immune Network for IgA Production”.
IgA is the most abundant antibody isotype in the body, with the majority of IgA found in mucosal secretions. Mucosal IgA production is induced by T cell-dependent and T cell-independent mechanisms. T cell-independent production of IgA is primarily stimulated by IL-6, IL-10, TGF-β, BAFF, and APRIL produced by intestinal epithelial, dendritic, and stromal cells. In this environment, intestinal B cells undergo class switching from IgM to IgA1. IgA-secreting plasma cells migrate to lamina propria, where they release dimeric IgA1. The dimers are formed through an interaction of two IgA1 molecules with a joining chain (J-chain), which is synthesized by plasma cells. IgA1 dimers can bind to the polymeric Ig receptor (pIgR) on the basolateral surface of the mucosal epithelium and undergo transcytosis to the apical surface, where they dissociate from pIgR and are secreted into the lumen carrying the secretory component of the receptor. The secretory component protects IgA molecules from proteolytic enzymes in the gut lumen. The bacteriostatic effects of secretory IgA1 are accompanied by antimicrobial peptides, such as defensins, secreted into the gut lumen by Paneth cells. The key molecules involved in the intestinal immune network for IgA production are indicated in orange; molecules implicated by GWAS are marked in red. The risk alleles generally lead to increased IgA1 responsiveness stimulating IgA1 production; increased levels of polymeric IgA1 in the circulation may represent a consequence of “spill-over” from mucosal sites and/or “mis-trafficking” of stimulated plasma cell to bone marrow sites.
Additional GWAS loci that are likely involved in the regulation of mucosal responses to pathogens include the DEFA locus (encoding alpha-defensin antimicrobial peptides) and CARD9 locus (encoding a pro-inflammatory adapter molecule implicated in the pathogenesis of inflammatory bowel disease and involved in the activation of NFk-B signaling), as well as ITGAM-ITGAX locus (encoding leukocyte-specific alpha-integrins involved in the process of phagocytosis and regulation of IgA production). There is also a large set of suggestive IgAN loci that is dramatically enriched for additional genes participating in the “Intestinal Immune Network for IgA Production”, one of the pathways curated by the Kyoto Encyclopedia of Genes and Genomes database (Figure 4). This includes the IL2RA-IL15RA locus (encoding receptor components for IL2 and IL15), the ICOS and ICOSLG loci (encoding inducible T-cell co-stimulatory molecules) and the TNFRSF13B locus (encoding TACI, a receptor for both BAFF and APRIL). Genetic perturbations to the “Intestinal Immune Network for IgA Production” may also have an effect on the composition of the commensal gut microbiome, as suggested by early studies showing dramatic differences in fecal microbiota between IgAN cases and healthy controls 122.
However, the hypothesis of intestinal IgA over-reactivity may not be so straightforward. For example, previous studies demonstrated a reduction in J-chain mRNA expression in duodenal IgA plasma cells in patients with IgAN 123 and lack of enhanced human IgA response to an immune challenge with mucosal tetanus toxoid immunization 124–126. Clearly, additional investigations of intestinal IgA responsiveness in IgAN are needed to clarify this issue. Follow-up studies are also needed to test if any of these candidate genes also affect the process of IgA1 O-glycosylation. Lastly, newer gene mapping approaches that utilize serum Gd-IgA1 levels as a quantitative endophenotype may offer further insights into the genetic architecture of this trait 127.
Anti-glycan antibodies (Hit 2)
The galactose-deficient hinge-region of IgA1 contains N-acetylgalactosamine (GalNac) residues with or without terminal sialic acid. Recent data suggest that exposed GalNac may represent an epitope recognized by specific anti-glycan antibodies, promoting formation of circulating immune complexes 97. Because some bacteria and viruses express GalNac on their surfaces, exposure to these pathogens could act as a trigger for the formation of cross-reacting antibodies. The presence of permissive MHC class II alleles may be required for this response. While very attractive, this “molecular mimicry” hypothesis will require experimental validation. The formation of immune complexes appears critical for the nephritogenic property of Gd-IgA1. In vitro studies of cultured human mesangial cells show activation with IgA1-IgG immune complexes, but absence of reactivity to isolated Gd-IgA1128. Recent clinical studies also suggest that using elevated levels of circulating anti-glycan antibodies as a disease biomarker outperforms serum Gd-IgA1 levels 129. Furthermore, the presence of anti-glycan antibodies correlates with proteinuria 97, more severe histopathologic injury 129, and faster progression of kidney disease 130. These promising findings now require prospective validation.
Immune complex formation and deposition (Hit 3)
A complex series of molecular interactions that remain poorly characterized lead to the formation of circulating immune complexes. Circulating polymeric IgA1-containing immune complexes induce cleavage of the extracellular domain of FcαR (CD89), forming an IgA1-CD89 complex; mice expressing both human IgA1 and CD89 develop mesangial deposition of IgA1 resembling human disease 131. These mice also overexpress transglutaminase-2 in the mesangium, while transglutaminase-2-deficient animals are protected from IgA1 deposition. Transglutaminase-2 is a multifunctional protein ubiquitously expressed in all tissues 132; the protein can be externalized, after which it cross-links with proteins of the extracellular matrix 133,134, but its role in human disease requires further study. Interestingly, one of the newly identified loci contains ITGAM, encoding integrin αM that is essential for interactions between CD89 and secretory IgA 135,136, but the dissection of its precise role also awaits additional studies. Several other molecules have been implicated in immune complex binding by mesangial cells 137, of which transferrin receptor (CD71) appears most promising 138–141.
Local activation of inflammatory pathways and the complement system (Hit 4)
Once deposited, IgA1-containing immune complexes stimulate mesangial proliferation and local production of cytokines, such as IL-6 and TGF-β142,143. These molecules promote inflammatory responses by recruiting leukocytes and promote glomerular and tubulointerstitial fibrosis. Furthermore, glomerular inflammation is enhanced by the complement system; C3 glomerular staining (Figure 1f) is present in over 90–95% of IgAN biopsies 2,4,12. In general, C3 staining tends to be less intense and more granular than the staining for IgA. C1q is generally negative (in 90% of cases) with less then 10% of cases exhibiting scant C1q staining of low (<1+) mean intensity 4,12. Such positivity for C3 with negativity for C1q is consistent with activation of either the lectin or the alternative pathway. Lectin pathway activation is further suggested by glomerular staining for C4d in the absence of C1q in approximately 40% of IgAN biopsies 144. Moreover, mesangial deposition of mannose-binding lectin (MBL) is reported in 25% of IgAN biopsies 145. All MBL-positive cases show glomerular co-deposition of L-ficolin, MBL-associated serine proteases and C4d, and these patients exhibit greater mesangial and extracapillary proliferation, glomerular sclerosis, interstitial infiltration, and proteinuria.
Support for alternative pathway activation in IgAN comes from GWAS. Inheritance of a common deletion in factor H-related genes 1 and 3 (CFHR3,1-del) provides additive protection from IgAN 48,85,87. CFHR1 and CFHR3 encode regulatory proteins that promote activation of the alternative pathway, likely through a competitive inhibition of factor H (FH) 146,147. Recent data suggests that CFHR3,1-del is associated with higher levels of circulating FH and lower levels of complement activation split products in IgAN. Higher FH levels are also positively associated with circulating C3 and negatively correlated with mesangial C3 deposition 148. Interestingly, a similar protective effect of CFHR3,1-del has been described for age-related macular degeneration, a common cause of retinal disease characterized by increased local overactivity of the alternative pathway 149. In contrast, CFHR3,1-del has been associated with increased risk of systemic lupus eryhtematosus and atypical hemolytic uremic syndrome 150,151. The mechanisms underlying these opposed pleiotropic effects of the deletion are presently not well understood.
The Treatment and Prognosis of IgA Nephropathy
The new Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines for glomerulonephritis provide an evidence-based review and appraisal of the literature on treating IgAN (Table 2). Because these guidelines have been published recently, we refer interested readers to the original publication for detailed discussion of supporting evidence 152. Here, we provide a brief synthesis of the recommended treatment plan and highlight specific areas of ongoing controversy.
Table 2.
Summary of the KDIGO treatment recommendations for IgAN.
| Intervention | Recommendation | Grade | Comments and areas of uncertainty |
|---|---|---|---|
| Blood pressure control and use of ACE inhibitors or ARBs | Long-term use of ACE inhibitors or ARBs is recommended for patients with proteinuria > 1g/day, with up-titration of the drug depending on blood pressure to achieve proteinuria <1g/day. | 1B | It is not clear at what level of proteinuria one should start ACE inhibitors or ARBs. Combined ACE inhibition and ARB use is generally not advised given potential risks of side effects of hyperkalemia and hypertension, especially in elderly. |
| A target blood pressure of <130/80 mm Hg is recommended for patients with proteinuria <1 g daily, and <125/75 for patients with proteinuria >1 g daily. | Not graded | ||
| Corticosteroids | A 6-month trial of corticosteroids is recommended in patients with persistent proteinuria of >1g/day despite 3–6 months of optimal supportive care and GFR > 50 ml/min per 1.73m2 | 2C | Presently, it is unclear at what level of reduced GFR this therapy becomes futile (i.e. “the point of no return”), and whether patients with lower levels of proteinuria should also be treated. |
| Other immunosuppressive agents | Patients with crescentic IgAN involving over 50% of glomeruli and rapidly progressive course should be treated with steroids and cyclophosphamide. | 2D | The definition of crescentic IgAN remains controversial. Rituximab has not yet been used in a significant enough number of patients to be recommended, however, data from studies on other crescentic diseases suggest a potential benefit. |
| Not treating with corticosteroids combined with cyclophosphamide or azathioprine (unless crescentic forms with rapidly progressive course). | 2D | There is no convincing evidence for the use of combined immunosuppression in IgAN, except for crescentic forms. | |
| Not using immunosuppressive therapy in patients with GFR < 30 ml/min per 1.73 m2 (unless crescentic forms with rapidly progressive course). | 2C | There is no convincing evidence for the use of immunosuppressive treatments in advanced stages of CKD due to IgAN. | |
| Not using MMF | 2C | The data for MMF in IgAN is generally of poor quality | |
| Fish oils | Fish oils may be potentially useful in patients with persistent proteinuria ≥ 1g/d, despite 3–6-months of optimized supportive care. | 2D | RCTs give equivocal results on the benefit of fish oils. Given low side effect profile and over-the-counter availability, the use of fish oils can probably be left to the choice of individual patients. However, this treatment should not replace corticosteroids, for which the evidence is stronger. |
| Tonsillectomy | Not recommended | 2C | No convincing evidence of benefit. Generally not recommended, unless specifically indicated by recurrent episodes of tonsillitis with synpharyngitic disease flares. |
Recommendation grading: Level 1 = “Recommended”, Level 2 = “Suggested”. Quality of evidence grading: A = “High”, B = “Moderate”, C = “Low”, D = “Very Low”.
The only KDIGO recommendation in IgAN based on unequivocal evidence is for blood pressure control and the use of ACE inhibitors or ARBs 152. A target of <130/80 mm Hg is recommended for patients with proteinuria <1 g daily, and <125/75 is recommended for patients with proteinuria >1 g daily. Additionally, it is recommended that medication be up-titrated to achieve <1 g of proteinuria daily. A number of randomized controlled trials (RCTs) document reduction of proteinuria and delay of GFR deterioration with this treatment 153,154,155,156. However, it remains unclear at what level of proteinuria this therapy should be initiated. Moreover, although several small studies suggest a benefit in proteinuria reduction with combined ACE inhibition and ARB use 157, there are no data showing decreased rate of renal failure or mortality. Given the potential risks of such combinations, specifically in older and high-risk cardiovascular populations, the combination is generally not advised.
The KDIGO guidelines suggest the use of a 6-month trial of corticosteroids in patients with persistent proteinuria of >1g/day despite 3–6 months of optimal supportive care. This recommendation is based on three RCTs performed in patients with generally preserved renal function 158–161 and a meta-analysis, concluding that steroids reduce kidney disease progression in this setting 162. Presently, it is unclear at what level of reduced renal function this therapy becomes futile (i.e. “the point of no return”) and whether patients with lower levels of proteinuria should also be treated 163.
For patients with crescents involving over 50% of glomeruli, the outcome is likely to be unfavorable 164,165. Most nephrologists treat such patients aggressively with pulse solumedrol followed by oral corticosteroids and IV cyclophosphamide 166. Rituximab has not yet been used in a significant enough number of patients to be recommended, however, data from studies on other crescentic diseases suggest a potential benefit 167,168. Of note, the exact definition of crescentic IgAN remains somewhat controversial.
Except for crescentic forms, KDIGO does not recommend a routine use of cyclophosphamide in addition to corticosteroids. Similarly, the use of MMF and azathioprine are generally not recommended; the data for MMF are inadequate, while azathioprine offered no additional benefit in a recent well-designed RCT 169. The benefits of other interventions, such as tonsillectomy or oral fish oils, also do not appear convincing 152. Overall, the evidence supporting these recommendations is of relatively poor quality.
The publication of KDIGO guidelines made it clear that the effectiveness of the existing therapies is limited and targeted treatments, more specific to the pathogenic process in IgAN, are still lacking. Despite the recommended treatment approach, IgAN remains a progressive disease in up to 50% of individuals 170. Overall, it is estimated that 20–40% of IgAN cases develop end stage renal disease (ESRD) within 20 years from the time of diagnosis 171,172. In the recent VALIGA cohort of 1,147 European patients, the annual rate of eGFR decline was 1.8±7.5 ml/min and ESRD developed in 12% of the patients that were followed for an average period of 4.7 years from the time of diagnosis 173. A number of retrospective studies pointed to several clinical risk factors for kidney disease progression, such as depressed baseline eGFR, low serum albumin and hemoglobin levels, severity of proteinuria, and elevated blood pressure at the time of biopsy 172,174–177. New online clinical decision support tools are also being developed based on these data (see URL for the IgAN Progression Calculator). However, most of the progression studies are based on single-center cohorts and rely on retrospective data; well-powered prospective cohort studies are needed to validate these findings.
In summary, the prognosis of IgAN is quite variable and the outcome remains difficult to predict in individual patients 178. The high level of inter-individual differences in disease course and inconsistent response to immunosuppressive therapies provide additional support for the hypothesis that our existing diagnostic criteria for IgAN likely encompass a more diverse set of disease entities. Further disease sub-classification, perhaps based on genetic and biomarker profiles specific to the underlying pathogenic process, is urgently needed to improve our treatment strategies.
Future Directions
There is a number of new important studies underway to address some of the most critical clinical questions outlined above. The CureGN Study (see URL) is a large prospective multicenter study of 2,400 patients with common forms of glomerular disease, including 600 patients with IgAN. This cohort will generate data on the natural history of IgAN, and provide means for a well-powered prospective validation of novel serum, urine, and tissue biomarkers for diagnosis, prognosis, and for tailoring treatments. Additionally, new clinical trials will soon clarify the role of immunosuppressive regimens in IgAN. The STOP IgAN Study (see URL) is a multicenter RCT of nearly 150 IgAN patients with persistent proteinuria of >0.75 g daily despite RAS inhibition and supportive therapy; the patients with a GFR of >60 cc/min are randomized to alternate day steroid treatment plus solumedrol pulses versus placebo, while those with a GFR of 30–60 cc/min are randomized to a regimen of cyclophosphamide for 3 months followed by azathioprine versus placebo. Lastly, the newly launched TESTING study will randomize >1,000 patients (proteinuria of >1.0 gm/day and an eGFR of >20 cc/min) to corticosteroids or placebo and is likely to provide definitive data on the utility of systemic glucocorticoids.
Moreover, GWAS findings have already stimulated investigations of promising treatment approaches that target the newly implicated pathways. Budesonide, a glucocorticoid locally released in the ileocecal region near the Peyer’s patches, is being studied in a larger controlled trial after proving successful in a small pilot trial 179. Other promising agents include Bortezomib (proteosome inhibitor), Fostamatinib (Syk inhibitor), Blisibimod (BAFF inhibitor), and Atacicept (humanized recombinant TACI-IgGFc fusion protein with anti-APRIL and anti-BAFF activity). In addition, the discovery of the protective effect of CFHR1,3-del suggests that pharmacologic suppression of the alternative complement pathway may be of potential benefit in IgAN.
Nevertheless, GWAS loci discovered to date explain less then 8% of the disease risk, suggesting contributions of additional, yet unidentified, genetic and environmental factors. Similar to other autoimmune diseases, IgAN is likely to have a highly complex genetic architecture with a large number of contributing risk alleles. For example, recent GWAS for inflammatory bowel disease (IBD) defined 193 independent risk loci, explaining over 25% of familial risk 121. Similarly, 110 GWAS risk alleles have been identified for multiple sclerosis (MS), explaining nearly 30% of sibling recurrence 180. New biology arising from these studies allowed for identification of previously unrecognized pathways that are shared between different autoimmune disorders, shedding light on the common underlying mechanisms that could now be targeted pharmaceutically 181. This is highly relevant to IgAN, since many of the IgAN risk alleles have shared effects on the risk of IBD, MS, and other autoimmune traits. However, the sample size of the aforementioned IBD or MS studies is over 4-fold greater compared to the largest IgAN study. Thus, one could reasonably expect to discover more IgAN risk alleles with increased GWAS sample size. In addition, fine mapping or re-sequencing of risk loci can identify causal alleles and potentially explain a larger proportion of disease risk. Moreover, post-GWAS functional studies of the molecular mechanisms underlying the observed genetic effects are needed to effectively translate the GWAS findings into clinical applications.
The discovery of rare variants with large effect that underlie familial forms of IgAN would also be valuable, because such variants readily demonstrate the consequence of severe gain or loss of function, and can inform the therapeutic potential of encoded gene products. Moreover, studies of pediatric patients may be especially worthwhile, since early onset of disease is correlated with genetic risk. In this regard, the newly established GIGA-kids Study (Genomics of IgA-related disorders in kids Study, see URL) aims to enroll >1,000 children for genetic, genomic, and biomarker discovery studies in IgAN and HSPN. Lastly, the ongoing studies aimed at refining the multi-hit model are likely to define new biomarkers and potential therapeutic targets. Integration of this model with additional genetic discoveries may finally lead to improved disease classification and novel personalized treatment strategies.
Acknowledgments
The authors are supported by the Center for Glomerular Disease at Columbia University. Krzysztof Kiryluk is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NIDDK) grants K23-DK090207 and R03-DK099654, and Carl W. Gottschalk Research Scholar Grant from the American Society of Nephrology (ASN) Foundation for Kidney Research.
Footnotes
URLs:
Genomics of IgA-related disorders in kids (GIGA-kids) Study: www.gigakids.org
Cure Glomerulonephropathy (CureGN) Study: www.curegn.org
STOP-IgAN Study: www.stop-igan-study.rwth-aachen.de
IgAN Progression Calculator: www.columbiamedicine.org/divisions/gharavi/calc_progression.php
IgAN Genetic Risk Calculator: www.columbiamedicine.org/divisions/gharavi/calc_genetic.php
Global Infectious Disease and Epidemiology Online Network (GIDEON): www.gideononline.com
References
- 1.Berger J, Hinglais N. Intercapillary deposits of IgA-IgG. Journal d’urologie et de nephrologie. 1968;74:694–5. [PubMed] [Google Scholar]
- 2.Roberts IS. Pathology of IgA nephropathy. Nature reviews Nephrology. 2014;10:445–54. doi: 10.1038/nrneph.2014.92. [DOI] [PubMed] [Google Scholar]
- 3.Working Group of the International Ig ANN, the Renal Pathology S. Roberts IS, et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney international. 2009;76:546–56. doi: 10.1038/ki.2009.168. [DOI] [PubMed] [Google Scholar]
- 4.Jennette JC. The immunohistology of IgA nephropathy. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1988;12:348–52. doi: 10.1016/s0272-6386(88)80022-2. [DOI] [PubMed] [Google Scholar]
- 5.Valentijn RM, Radl J, Haaijman JJ, et al. Circulating and mesangial secretory component-binding IgA-1 in primary IgA nephropathy. Kidney international. 1984;26:760–6. doi: 10.1038/ki.1984.213. [DOI] [PubMed] [Google Scholar]
- 6.Haas M. IgA Nephropathy and Henoch-Schonlein Purpura Nephritis. In: Jennette JCDAVD, Olson JL, Silva FG, editors. Heptinstall’s Pathology of the Kidney. 7. Philadelphia: Lippincott Williams & Wilkins; 2015. [Google Scholar]
- 7.Chui SH, Lam CW, Lewis WH, Lai KN. Light-chain ratio of serum IgA1 in IgA nephropathy. Journal of clinical immunology. 1991;11:219–23. doi: 10.1007/BF00917428. [DOI] [PubMed] [Google Scholar]
- 8.Haas M. Histologic subclassification of IgA nephropathy: a clinicopathologic study of 244 cases. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1997;29:829–42. doi: 10.1016/s0272-6386(97)90456-x. [DOI] [PubMed] [Google Scholar]
- 9.Hill GS, Karoui KE, Karras A, et al. Focal segmental glomerulosclerosis plays a major role in the progression of IgA nephropathy. I. Immunohistochemical studies. Kidney international. 2011;79:635–42. doi: 10.1038/ki.2010.466. [DOI] [PubMed] [Google Scholar]
- 10.Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis and rheumatism. 2013;65:1–11. doi: 10.1002/art.37715. [DOI] [PubMed] [Google Scholar]
- 11.Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D. Henoch-Schonlein Purpura in adults: outcome and prognostic factors. J Am Soc Nephrol. 2002;13:1271–8. doi: 10.1097/01.asn.0000013883.99976.22. [DOI] [PubMed] [Google Scholar]
- 12.Haas M. IgA Nephropathy and IgA vasculitis (Henoch-Schonlein Purpura Nephritis) 2015. [Google Scholar]
- 13.Lee SM, Rao VM, Franklin WA, et al. IgA nephropathy: morphologic predictors of progressive renal disease. Human pathology. 1982;13:314–22. doi: 10.1016/s0046-8177(82)80221-9. [DOI] [PubMed] [Google Scholar]
- 14.Working Group of the International Ig ANN, the Renal Pathology S. Cattran DC, et al. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney international. 2009;76:534–45. doi: 10.1038/ki.2009.243. [DOI] [PubMed] [Google Scholar]
- 15.Herzenberg AM, Fogo AB, Reich HN, et al. Validation of the Oxford classification of IgA nephropathy. Kidney international. 2011;80:310–7. doi: 10.1038/ki.2011.126. [DOI] [PubMed] [Google Scholar]
- 16.Yau T, Korbet SM, Schwartz MM, Cimbaluk DJ. The Oxford classification of IgA nephropathy: a retrospective analysis. American journal of nephrology. 2011;34:435–44. doi: 10.1159/000332223. [DOI] [PubMed] [Google Scholar]
- 17.Alamartine E, Sauron C, Laurent B, Sury A, Seffert A, Mariat C. The use of the Oxford classification of IgA nephropathy to predict renal survival. Clinical journal of the American Society of Nephrology: CJASN. 2011;6:2384–8. doi: 10.2215/CJN.01170211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edstrom Halling S, Soderberg MP, Berg UB. Predictors of outcome in paediatric IgA nephropathy with regard to clinical and histopathological variables (Oxford classification) Nephrol Dial Transplant. 2012;27:715–22. doi: 10.1093/ndt/gfr339. [DOI] [PubMed] [Google Scholar]
- 19.El Karoui K, Hill GS, Karras A, et al. Focal segmental glomerulosclerosis plays a major role in the progression of IgA nephropathy. II. Light microscopic and clinical studies. Kidney Int. 2011;79:643–54. doi: 10.1038/ki.2010.460. [DOI] [PubMed] [Google Scholar]
- 20.Gutierrez E, Zamora I, Ballarin JA, et al. Long-term outcomes of IgA nephropathy presenting with minimal or no proteinuria. J Am Soc Nephrol. 2012;23:1753–60. doi: 10.1681/ASN.2012010063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeng CH, Le W, Ni Z, et al. A multicenter application and evaluation of the oxford classification of IgA nephropathy in adult chinese patients. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2012;60:812–20. doi: 10.1053/j.ajkd.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 22.Katafuchi R, Ninomiya T, Nagata M, Mitsuiki K, Hirakata H. Validation study of oxford classification of IgA nephropathy: the significance of extracapillary proliferation. Clinical journal of the American Society of Nephrology: CJASN. 2011;6:2806–13. doi: 10.2215/CJN.02890311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang SH, Choi SR, Park HS, et al. The Oxford classification as a predictor of prognosis in patients with IgA nephropathy. Nephrol Dial Transplant. 2012;27:252–8. doi: 10.1093/ndt/gfr295. [DOI] [PubMed] [Google Scholar]
- 24.Shi SF, Wang SX, Jiang L, et al. Pathologic predictors of renal outcome and therapeutic efficacy in IgA nephropathy: validation of the oxford classification. Clinical journal of the American Society of Nephrology: CJASN. 2011;6:2175–84. doi: 10.2215/CJN.11521210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shima Y, Nakanishi K, Hama T, et al. Validity of the Oxford classification of IgA nephropathy in children. Pediatric nephrology. 2012;27:783–92. doi: 10.1007/s00467-011-2061-0. [DOI] [PubMed] [Google Scholar]
- 26.Kataoka H, Ohara M, Shibui K, et al. Overweight and obesity accelerate the progression of IgA nephropathy: prognostic utility of a combination of BMI and histopathological parameters. Clinical and experimental nephrology. 2012;16:706–12. doi: 10.1007/s10157-012-0613-7. [DOI] [PubMed] [Google Scholar]
- 27.Moriyama T, Nakayama K, Iwasaki C, et al. Severity of nephrotic IgA nephropathy according to the Oxford classification. International urology and nephrology. 2012;44:1177–84. doi: 10.1007/s11255-011-0109-5. [DOI] [PubMed] [Google Scholar]
- 28.Lee H, Yi SH, Seo MS, et al. Validation of the Oxford classification of IgA nephropathy: a single-center study in Korean adults. The Korean journal of internal medicine. 2012;27:293–300. doi: 10.3904/kjim.2012.27.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le W, Zeng CH, Liu Z, et al. Validation of the Oxford classification of IgA nephropathy for pediatric patients from China. BMC nephrology. 2012;13:158. doi: 10.1186/1471-2369-13-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Working Group of the International Ig ANN, the Renal Pathology S. Coppo R, et al. The Oxford IgA nephropathy clinicopathological classification is valid for children as well as adults. Kidney international. 2010;77:921–7. doi: 10.1038/ki.2010.43. [DOI] [PubMed] [Google Scholar]
- 31.Coppo R, Troyanov S, Bellur S, et al. Validation of the Oxford classification of IgA nephropathy in cohorts with different presentations and treatments. Kidney international. 2014;86:828–36. doi: 10.1038/ki.2014.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haas M, Rastaldi MP, Fervenza FC. Histologic classification of glomerular diseases: clinicopathologic correlations, limitations exposed by validation studies, and suggestions for modification. Kidney international. 2014;85:779–93. doi: 10.1038/ki.2013.375. [DOI] [PubMed] [Google Scholar]
- 33.Lv J, Shi S, Xu D, et al. Evaluation of the Oxford Classification of IgA nephropathy: a systematic review and meta-analysis. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2013;62:891–9. doi: 10.1053/j.ajkd.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Sinniah R. Occurrence of mesangial IgA and IgM deposits in a control necropsy population. Journal of clinical pathology. 1983;36:276–9. doi: 10.1136/jcp.36.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waldherr R, Rambausek M, Duncker WD, Ritz E. Frequency of mesangial IgA deposits in a non-selected autopsy series. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 1989;4:943–6. doi: 10.1093/ndt/4.11.943. [DOI] [PubMed] [Google Scholar]
- 36.Varis J, Rantala I, Pasternack A. Immunofluorescence of immunoglobulins and complement in kidneys taken at necropsy. Journal of clinical pathology. 1989;42:1211–4. doi: 10.1136/jcp.42.11.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suzuki K, Honda K, Tanabe K, Toma H, Nihei H, Yamaguchi Y. Incidence of latent mesangial IgA deposition in renal allograft donors in Japan. Kidney international. 2003;63:2286–94. doi: 10.1046/j.1523-1755.63.6s.2.x. [DOI] [PubMed] [Google Scholar]
- 38.Demircin G, Delibas A, Bek K, et al. A one-center experience with pediatric percutaneous renal biopsy and histopathology in Ankara, Turkey. International urology and nephrology. 2009;41:933–9. doi: 10.1007/s11255-008-9433-9. [DOI] [PubMed] [Google Scholar]
- 39.Monfared A, Khosravi M, Lebadi M, et al. Distribution of renal histopathology in Guilan: a single-center report. Iranian journal of kidney diseases. 2012;6:173–7. [PubMed] [Google Scholar]
- 40.Berthoux F. Annual incidence of glomerulonephritis in the extended Rhone-Alpes region in 1987–1988. Presse medicale. 1990;19:1417. [PubMed] [Google Scholar]
- 41.Gesualdo L, Di Palma AM, Morrone LF, Strippoli GF, Schena FP Italian Immunopathology Group ISoN. The Italian experience of the national registry of renal biopsies. Kidney Int. 2004;66:890–4. doi: 10.1111/j.1523-1755.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- 42.Hanko JB, Mullan RN, O’Rourke DM, McNamee PT, Maxwell AP, Courtney AE. The changing pattern of adult primary glomerular disease. Nephrol Dial Transplant. 2009;24:3050–4. doi: 10.1093/ndt/gfp254. [DOI] [PubMed] [Google Scholar]
- 43.Schena FP. Survey of the Italian Registry of Renal Biopsies. Frequency of the renal diseases for 7 consecutive years. The Italian Group of Renal Immunopathology. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 1997;12:418–26. doi: 10.1093/ndt/12.3.418. [DOI] [PubMed] [Google Scholar]
- 44.Kurnatowska I, Jedrzejka D, Malyska A, Wagrowska-Danilewicz M, Danilewicz M, Nowicki M. Trends in the incidence of biopsy-proven glomerular diseases in the adult population in central Poland in the years 1990–2010. Kidney & blood pressure research. 2012;35:254–8. doi: 10.1159/000334418. [DOI] [PubMed] [Google Scholar]
- 45.Sugiyama H, Yokoyama H, Sato H, et al. Japan Renal Biopsy Registry: the first nationwide, web-based, and prospective registry system of renal biopsies in Japan. Clinical and experimental nephrology. 2011;15:493–503. doi: 10.1007/s10157-011-0430-4. [DOI] [PubMed] [Google Scholar]
- 46.Zhou FD, Zhao MH, Zou WZ, Liu G, Wang H. The changing spectrum of primary glomerular diseases within 15 years: a survey of 3331 patients in a single Chinese centre. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2009;24:870–6. doi: 10.1093/ndt/gfn554. [DOI] [PubMed] [Google Scholar]
- 47.McQuarrie EP, Mackinnon B, Young B, et al. Centre variation in incidence, indication and diagnosis of adult native renal biopsy in Scotland. Nephrol Dial Transplant. 2009;24:1524–8. doi: 10.1093/ndt/gfn677. [DOI] [PubMed] [Google Scholar]
- 48.Kiryluk K, Li Y, Sanna-Cherchi S, et al. Geographic differences in genetic susceptibility to IgA nephropathy: GWAS replication study and geospatial risk analysis. PLoS genetics. 2012;8:e1002765. doi: 10.1371/journal.pgen.1002765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Okpechi I, Swanepoel C, Duffield M, et al. Patterns of renal disease in Cape Town South Africa: a 10-year review of a single-centre renal biopsy database. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2011;26:1853–61. doi: 10.1093/ndt/gfq655. [DOI] [PubMed] [Google Scholar]
- 50.Li L. Pathological classification and clinical characteristics of primary glomerulonephritis in China: bioptic study of 1001 cases. Zhonghua yi xue za zhi. 1989;69:20–3. 4. [PubMed] [Google Scholar]
- 51.Tojo S, Hatano M, Honda N, et al. Natural history of IgA nephropathy in Japan. Seminars in nephrology. 1987;7:386–8. [PubMed] [Google Scholar]
- 52.Abdulmassih Z, Makdassi R, Bove N, et al. Epidemiology of primary glomerulonephritis in Picardie. Annales de medecine interne. 1990;141:129–33. [PubMed] [Google Scholar]
- 53.Braun N, Schweisfurth A, Lohofener C, et al. Epidemiology of glomerulonephritis in Northern Germany. International urology and nephrology. 2011;43:1117–26. doi: 10.1007/s11255-011-9955-4. [DOI] [PubMed] [Google Scholar]
- 54.Browne O, Doyle GD, Campbell E. An immunohistological study of IgA nephropathy and a report of its incidence in Ireland. Irish journal of medical science. 1985;154:461–5. doi: 10.1007/BF02937198. [DOI] [PubMed] [Google Scholar]
- 55.Carvalho E, do Sameiro Faria M, Nunes JP, Sampaio S, Valbuena C. Renal diseases: a 27-year renal biopsy study. Journal of nephrology. 2006;19:500–7. [PubMed] [Google Scholar]
- 56.Fisi V, Mazak I, Degrell P, et al. Histological diagnosis determines complications of percutaneous renal biopsy: a single-center experience in 353 patients. Kidney & blood pressure research. 2012;35:26–34. doi: 10.1159/000329939. [DOI] [PubMed] [Google Scholar]
- 57.Heaf J, Lokkegaard H, Larsen S. The epidemiology and prognosis of glomerulonephritis in Denmark 1985–1997. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 1999;14:1889–97. doi: 10.1093/ndt/14.8.1889. [DOI] [PubMed] [Google Scholar]
- 58.Mesquita M, Fosso C, Bakoto Sol E, et al. Renal biopsy findings in Belgium: a retrospective single center analysis. Acta clinica Belgica. 2011;66:104–9. doi: 10.2143/ACB.66.2.2062527. [DOI] [PubMed] [Google Scholar]
- 59.Mustonen J, Pasternack A, Helin H, et al. Circulating immune complexes, the concentration of serum IgA and the distribution of HLA antigens in IgA nephropathy. Nephron. 1981;29:170–5. doi: 10.1159/000182350. [DOI] [PubMed] [Google Scholar]
- 60.Riispere Z, Ots-Rosenberg M. Occurrence of kidney diseases and patterns of glomerular disease based on a 10-year kidney biopsy material: a retrospective single-centre analysis in Estonia. Scandinavian journal of urology and nephrology. 2012;46:389–94. doi: 10.3109/00365599.2012.693133. [DOI] [PubMed] [Google Scholar]
- 61.Rivera F, Lopez-Gomez JM, Perez-Garcia R Spanish Registry of G. Clinicopathologic correlations of renal pathology in Spain. Kidney international. 2004;66:898–904. doi: 10.1111/j.1523-1755.2004.00833.x. [DOI] [PubMed] [Google Scholar]
- 62.Schmekel B, Svalander C, Bucht H, Westberg NG. Mesangial IgA glomerulonephritis in adults. Clinical and histopathological observations. Acta medica Scandinavica. 1981;210:363–72. doi: 10.1111/j.0954-6820.1981.tb09832.x. [DOI] [PubMed] [Google Scholar]
- 63.Tiebosch AT, Wolters J, Frederik PF, van der Wiel TW, Zeppenfeldt E, van Breda Vriesman PJ. Epidemiology of idiopathic glomerular disease: a prospective study. Kidney international. 1987;32:112–6. doi: 10.1038/ki.1987.179. [DOI] [PubMed] [Google Scholar]
- 64.Radford MG, Jr, Donadio JV, Jr, Bergstralh EJ, Grande JP. Predicting renal outcome in IgA nephropathy. Journal of the American Society of Nephrology: JASN. 1997;8:199–207. doi: 10.1681/ASN.V82199. [DOI] [PubMed] [Google Scholar]
- 65.Knoop T, Vikse BE, Svarstad E, Leh S, Reisaeter AV, Bjorneklett R. Mortality in patients with IgA nephropathy. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2013;62:883–90. doi: 10.1053/j.ajkd.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 66.Feehally J, Cameron JS. IgA nephropathy: progress before and since Berger. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2011;58:310–9. doi: 10.1053/j.ajkd.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 67.Lee H, Hwang JH, Paik JH, et al. Long-term prognosis of clinically early IgA nephropathy is not always favorable. BMC nephrology. 2014;15:94. doi: 10.1186/1471-2369-15-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chandrika BK. IgA nephropathy in Kerala, India: a retrospective study. Indian journal of pathology & microbiology. 2009;52:14–6. doi: 10.4103/0377-4929.44954. [DOI] [PubMed] [Google Scholar]
- 69.O’Connell PJ, Ibels LS, Thomas MA, Harris M, Eckstein RP. Familial IgA nephropathy: a study of renal disease in an Australian aboriginal family. Australian and New Zealand journal of medicine. 1987;17:27–33. doi: 10.1111/j.1445-5994.1987.tb05045.x. [DOI] [PubMed] [Google Scholar]
- 70.Levy M. Familial cases of Berger’s disease and anaphylactoid purpura: more frequent than previously thought. The American journal of medicine. 1989;87:246–8. doi: 10.1016/s0002-9343(89)80720-x. [DOI] [PubMed] [Google Scholar]
- 71.Julian BA, Quiggins PA, Thompson JS, Woodford SY, Gleason K, Wyatt RJ. Familial IgA nephropathy. Evidence of an inherited mechanism of disease. The New England journal of medicine. 1985;312:202–8. doi: 10.1056/NEJM198501243120403. [DOI] [PubMed] [Google Scholar]
- 72.Scolari F, Amoroso A, Savoldi S, et al. Familial clustering of IgA nephropathy: further evidence in an Italian population. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1999;33:857–65. doi: 10.1016/s0272-6386(99)70417-8. [DOI] [PubMed] [Google Scholar]
- 73.Paterson AD, Liu XQ, Wang K, et al. Genome-wide linkage scan of a large family with IgA nephropathy localizes a novel susceptibility locus to chromosome 2q36. Journal of the American Society of Nephrology: JASN. 2007;18:2408–15. doi: 10.1681/ASN.2007020241. [DOI] [PubMed] [Google Scholar]
- 74.Karnib HH, Sanna-Cherchi S, Zalloua PA, et al. Characterization of a large Lebanese family segregating IgA nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2007;22:772–7. doi: 10.1093/ndt/gfl677. [DOI] [PubMed] [Google Scholar]
- 75.Masuda J, Shiiki H, Fujii Y, Dohi K, Harada A. Identical twin sisters with IgA nephropathy. Nihon Jinzo Gakkai shi. 1996;38:52–6. [PubMed] [Google Scholar]
- 76.Tsuboi N, Kawamura T, Okonogi H, Ishii T, Utsunomiya Y, Hosoya T. Discordant clinicopathological features in monozygotic twins with IgA nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2011;26:4146–8. doi: 10.1093/ndt/gfr519. [DOI] [PubMed] [Google Scholar]
- 77.Ahlmen J, Hedman I, Svalander C. Recurrent IgA-nephropathy in an identical twin transplant. Clinical transplants. 1989:297. [PubMed] [Google Scholar]
- 78.Schena FP, Scivittaro V, Ranieri E, et al. Abnormalities of the IgA immune system in members of unrelated pedigrees from patients with IgA nephropathy. Clinical and experimental immunology. 1993;92:139–44. doi: 10.1111/j.1365-2249.1993.tb05960.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gharavi AG, Moldoveanu Z, Wyatt RJ, et al. Aberrant IgA1 glycosylation is inherited in familial and sporadic IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2008;19:1008–14. doi: 10.1681/ASN.2007091052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kiryluk K, Moldoveanu Z, Sanders JT, et al. Aberrant glycosylation of IgA1 is inherited in both pediatric IgA nephropathy and Henoch-Schonlein purpura nephritis. Kidney international. 2011;80:79–87. doi: 10.1038/ki.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gharavi AG, Yan Y, Scolari F, et al. IgA nephropathy, the most common cause of glomerulonephritis, is linked to 6q22–23. Nature genetics. 2000;26:354–7. doi: 10.1038/81677. [DOI] [PubMed] [Google Scholar]
- 82.Bisceglia L, Cerullo G, Forabosco P, et al. Genetic heterogeneity in Italian families with IgA nephropathy: suggestive linkage for two novel IgA nephropathy loci. American journal of human genetics. 2006;79:1130–4. doi: 10.1086/510135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Maher B. Personal genomes: The case of the missing heritability. Nature. 2008;456:18–21. doi: 10.1038/456018a. [DOI] [PubMed] [Google Scholar]
- 84.Feehally J, Farrall M, Boland A, et al. HLA has strongest association with IgA nephropathy in genome-wide analysis. Journal of the American Society of Nephrology: JASN. 2010;21:1791–7. doi: 10.1681/ASN.2010010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gharavi AG, Kiryluk K, Choi M, et al. Genome-wide association study identifies susceptibility loci for IgA nephropathy. Nature genetics. 2011;43:321–7. doi: 10.1038/ng.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yu XQ, Li M, Zhang H, et al. A genome-wide association study in Han Chinese identifies multiple susceptibility loci for IgA nephropathy. Nature genetics. 2012;44:178–82. doi: 10.1038/ng.1047. [DOI] [PubMed] [Google Scholar]
- 87.Kiryluk K, Li Y, Scolari F, et al. Discovery of new risk loci for IgA nephropathy implicates genes involved in immunity against intestinal pathogens. Nature genetics. 2014 doi: 10.1038/ng.3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shapira Y, Agmon-Levin N, Shoenfeld Y. Defining and analyzing geoepidemiology and human autoimmunity. J Autoimmun. 2010;34:J168–77. doi: 10.1016/j.jaut.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 89.Borchers AT, Uibo R, Gershwin ME. The geoepidemiology of type 1 diabetes. Autoimmun Rev. 2010;9:A355–65. doi: 10.1016/j.autrev.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 90.Milo R, Kahana E. Multiple sclerosis: geoepidemiology, genetics and the environment. Autoimmun Rev. 2010;9:A387–94. doi: 10.1016/j.autrev.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 91.Handel AE, Handunnetthi L, Giovannoni G, Ebers GC, Ramagopalan SV. Genetic and environmental factors and the distribution of multiple sclerosis in Europe. Eur J Neurol. 2010;17:1210–4. doi: 10.1111/j.1468-1331.2010.03003.x. [DOI] [PubMed] [Google Scholar]
- 92.Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasites & vectors. 2014;7:37. doi: 10.1186/1756-3305-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Barry MA, Simon GG, Mistry N, Hotez PJ. Global trends in neglected tropical disease control and elimination: impact on child health. Archives of disease in childhood. 2013;98:635–41. doi: 10.1136/archdischild-2012-302338. [DOI] [PubMed] [Google Scholar]
- 94.Suzuki H, Kiryluk K, Novak J, et al. The pathophysiology of IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2011;22:1795–803. doi: 10.1681/ASN.2011050464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kiryluk K, Novak J, Gharavi AG. Pathogenesis of immunoglobulin A nephropathy: recent insight from genetic studies. Annu Rev Med. 2013;64:339–56. doi: 10.1146/annurev-med-041811-142014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kiryluk K, Novak J. The genetics and immunobiology of IgA nephropathy. The Journal of clinical investigation. 2014;124:2325–32. doi: 10.1172/JCI74475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Suzuki H, Fan R, Zhang Z, et al. Aberrantly glycosylated IgA1 in IgA nephropathy patients is recognized by IgG antibodies with restricted heterogeneity. The Journal of clinical investigation. 2009;119:1668–77. doi: 10.1172/JCI38468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pabst O. New concepts in the generation and functions of IgA. Nature reviews Immunology. 2012;12:821–32. doi: 10.1038/nri3322. [DOI] [PubMed] [Google Scholar]
- 99.Mestecky J, Raska M, Julian BA, et al. IgA nephropathy: molecular mechanisms of the disease. Annual review of pathology. 2013;8:217–40. doi: 10.1146/annurev-pathol-011110-130216. [DOI] [PubMed] [Google Scholar]
- 100.Allen AC, Harper SJ, Feehally J. Galactosylation of N- and O-linked carbohydrate moieties of IgA1 and IgG in IgA nephropathy. Clinical and experimental immunology. 1995;100:470–4. doi: 10.1111/j.1365-2249.1995.tb03724.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Novak J, Julian BA, Tomana M, Mestecky J. IgA glycosylation and IgA immune complexes in the pathogenesis of IgA nephropathy. Seminars in nephrology. 2008;28:78–87. doi: 10.1016/j.semnephrol.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hiki Y, Horii A, Iwase H, et al. O-linked oligosaccharide on IgA1 hinge region in IgA nephropathy. Fundamental study for precise structure and possible role. Contributions to nephrology. 1995;111:73–84. [PubMed] [Google Scholar]
- 103.Moldoveanu Z, Wyatt RJ, Lee JY, et al. Patients with IgA nephropathy have increased serum galactose-deficient IgA1 levels. Kidney international. 2007;71:1148–54. doi: 10.1038/sj.ki.5002185. [DOI] [PubMed] [Google Scholar]
- 104.Zhao N, Hou P, Lv J, et al. The level of galactose-deficient IgA1 in the sera of patients with IgA nephropathy is associated with disease progression. Kidney international. 2012;82:790–6. doi: 10.1038/ki.2012.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hastings MC, Moldoveanu Z, Julian BA, et al. Galactose-deficient IgA1 in African Americans with IgA nephropathy: serum levels and heritability. Clinical journal of the American Society of Nephrology: CJASN. 2010;5:2069–74. doi: 10.2215/CJN.03270410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Smith AC, de Wolff JF, Molyneux K, Feehally J, Barratt J. O-glycosylation of serum IgD in IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2006;17:1192–9. doi: 10.1681/ASN.2005101115. [DOI] [PubMed] [Google Scholar]
- 107.Suzuki H, Moldoveanu Z, Hall S, et al. IgA1-secreting cell lines from patients with IgA nephropathy produce aberrantly glycosylated IgA1. The Journal of clinical investigation. 2008;118:629–39. doi: 10.1172/JCI33189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Boyd JK, Cheung CK, Molyneux K, Feehally J, Barratt J. An update on the pathogenesis and treatment of IgA nephropathy. Kidney international. 2012;81:833–43. doi: 10.1038/ki.2011.501. [DOI] [PubMed] [Google Scholar]
- 109.Buren M, Yamashita M, Suzuki Y, Tomino Y, Emancipator SN. Altered expression of lymphocyte homing chemokines in the pathogenesis of IgA nephropathy. Contributions to nephrology. 2007;157:50–5. doi: 10.1159/000102304. [DOI] [PubMed] [Google Scholar]
- 110.Batra A, Smith AC, Feehally J, Barratt J. T-cell homing receptor expression in IgA nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2007;22:2540–8. doi: 10.1093/ndt/gfm228. [DOI] [PubMed] [Google Scholar]
- 111.Kennel-De March A, Bene MC, Hurault de Ligny B, Kessler M, Faure GC. Enhanced expression of CD31 and CD54 on tonsillar high endothelial venules in IgA nephropathy. Clinical immunology and immunopathology. 1997;84:158–65. doi: 10.1006/clin.1997.4389. [DOI] [PubMed] [Google Scholar]
- 112.Stein JV, Lopez-Fraga M, Elustondo FA, et al. APRIL modulates B and T cell immunity. The Journal of clinical investigation. 2002;109:1587–98. doi: 10.1172/JCI15034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.He B, Xu W, Santini PA, et al. Intestinal bacteria trigger T cell-independent immunoglobulin A(2) class switching by inducing epithelial-cell secretion of the cytokine APRIL. Immunity. 2007;26:812–26. doi: 10.1016/j.immuni.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 114.Castigli E, Scott S, Dedeoglu F, et al. Impaired IgA class switching in APRIL-deficient mice. Proc Natl Acad Sci U S A. 2004;101:3903–8. doi: 10.1073/pnas.0307348101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.McCarthy DD, Kujawa J, Wilson C, et al. Mice overexpressing BAFF develop a commensal flora-dependent, IgA-associated nephropathy. The Journal of clinical investigation. 2011;121:3991–4002. doi: 10.1172/JCI45563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rockman SP, Demmler K, Roczo N, et al. Expression of interleukin-6, leukemia inhibitory factor and their receptors by colonic epithelium and pericryptal fibroblasts. Journal of gastroenterology and hepatology. 2001;16:991–1000. doi: 10.1046/j.1440-1746.2001.02588.x. [DOI] [PubMed] [Google Scholar]
- 117.Guimbaud R, Abitbol V, Bertrand V, et al. Leukemia inhibitory factor involvement in human ulcerative colitis and its potential role in malignant course. European cytokine network. 1998;9:607–12. [PubMed] [Google Scholar]
- 118.Esashi E, Ito H, Minehata K, Saito S, Morikawa Y, Miyajima A. Oncostatin M deficiency leads to thymic hypoplasia, accumulation of apoptotic thymocytes and glomerulonephritis. European journal of immunology. 2009;39:1664–70. doi: 10.1002/eji.200839149. [DOI] [PubMed] [Google Scholar]
- 119.Imielinski M, Baldassano RN, Griffiths A, et al. Common variants at five new loci associated with early-onset inflammatory bowel disease. Nature genetics. 2009;41:1335–40. doi: 10.1038/ng.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Franke A, McGovern DP, Barrett JC, et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nature genetics. 2010;42:1118–25. doi: 10.1038/ng.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–24. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.De Angelis M, Montemurno E, Piccolo M, et al. Microbiota and metabolome associated with immunoglobulin A nephropathy (IgAN) PloS one. 2014;9:e99006. doi: 10.1371/journal.pone.0099006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Harper SJ, Pringle JH, Wicks AC, et al. Expression of J chain mRNA in duodenal IgA plasma cells in IgA nephropathy. Kidney Int. 1994;45:836–44. doi: 10.1038/ki.1994.110. [DOI] [PubMed] [Google Scholar]
- 124.Waldo FB. Systemic immune response after mucosal immunization in patients with IgA nephropathy. Journal of clinical immunology. 1992;12:21–6. doi: 10.1007/BF00918269. [DOI] [PubMed] [Google Scholar]
- 125.Layward L, Allen AC, Hattersley JM, Harper SJ, Feehally J. Response to mucosal antigen challenge in IgA nephropathy. Experimental nephrology. 1995;3:300–7. [PubMed] [Google Scholar]
- 126.Roodnat JI, de Fijter JW, van Kooten C, Daha MR, van Es LA. Decreased IgA1 response after primary oral immunization with live typhoid vaccine in primary IgA nephropathy. Nephrol Dial Transplant. 1999;14:353–9. doi: 10.1093/ndt/14.2.353. [DOI] [PubMed] [Google Scholar]
- 127.Kiryluk K, Julian BA, Wyatt RJ, et al. Genetic studies of IgA nephropathy: past, present, and future. Pediatric nephrology. 2010;25:2257–68. doi: 10.1007/s00467-010-1500-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yanagihara T, Brown R, Hall S, et al. generated immune complexes containing galactose-deficient IgA1 stimulate proliferation of mesangial cells. Results in immunology. 2012;2:166–72. doi: 10.1016/j.rinim.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yanagawa H, Suzuki H, Suzuki Y, et al. A panel of serum biomarkers differentiates IgA nephropathy from other renal diseases. PloS one. 2014;9:e98081. doi: 10.1371/journal.pone.0098081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Berthoux F, Suzuki H, Thibaudin L, et al. Autoantibodies targeting galactose-deficient IgA1 associate with progression of IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2012;23:1579–87. doi: 10.1681/ASN.2012010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Berthelot L, Papista C, Maciel TT, et al. Transglutaminase is essential for IgA nephropathy development acting through IgA receptors. The Journal of experimental medicine. 2012;209:793–806. doi: 10.1084/jem.20112005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lorand L, Graham RM. Transglutaminases: crosslinking enzymes with pleiotropic functions. Nature reviews Molecular cell biology. 2003;4:140–56. doi: 10.1038/nrm1014. [DOI] [PubMed] [Google Scholar]
- 133.Shweke N, Boulos N, Jouanneau C, et al. Tissue transglutaminase contributes to interstitial renal fibrosis by favoring accumulation of fibrillar collagen through TGF-beta activation and cell infiltration. The American journal of pathology. 2008;173:631–42. doi: 10.2353/ajpath.2008.080025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fesus L, Piacentini M. Transglutaminase 2: an enigmatic enzyme with diverse functions. Trends in biochemical sciences. 2002;27:534–9. doi: 10.1016/s0968-0004(02)02182-5. [DOI] [PubMed] [Google Scholar]
- 135.van Egmond M, van Vuuren AJ, Morton HC, et al. Human immunoglobulin A receptor (FcalphaRI, CD89) function in transgenic mice requires both FcR gamma chain and CR3 (CD11b/CD18) Blood. 1999;93:4387–94. [PubMed] [Google Scholar]
- 136.Van Spriel AB, Leusen JH, Vile H, Van De Winkel JG. Mac-1 (CD11b/CD18) as accessory molecule for Fc alpha R (CD89) binding of IgA. Journal of immunology. 2002;169:3831–6. doi: 10.4049/jimmunol.169.7.3831. [DOI] [PubMed] [Google Scholar]
- 137.Floege J, Moura IC, Daha MR. New insights into the pathogenesis of IgA nephropathy. Seminars in immunopathology. 2014;36:431–42. doi: 10.1007/s00281-013-0411-7. [DOI] [PubMed] [Google Scholar]
- 138.Matysiak-Budnik T, Moura IC, Arcos-Fajardo M, et al. Secretory IgA mediates retrotranscytosis of intact gliadin peptides via the transferrin receptor in celiac disease. The Journal of experimental medicine. 2008;205:143–54. doi: 10.1084/jem.20071204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Moura IC, Arcos-Fajardo M, Gdoura A, et al. Engagement of transferrin receptor by polymeric IgA1: evidence for a positive feedback loop involving increased receptor expression and mesangial cell proliferation in IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2005;16:2667–76. doi: 10.1681/ASN.2004111006. [DOI] [PubMed] [Google Scholar]
- 140.Moura IC, Arcos-Fajardo M, Sadaka C, et al. Glycosylation and size of IgA1 are essential for interaction with mesangial transferrin receptor in IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2004;15:622–34. doi: 10.1097/01.asn.0000115401.07980.0c. [DOI] [PubMed] [Google Scholar]
- 141.Moura IC, Centelles MN, Arcos-Fajardo M, et al. Identification of the transferrin receptor as a novel immunoglobulin (Ig)A1 receptor and its enhanced expression on mesangial cells in IgA nephropathy. The Journal of experimental medicine. 2001;194:417–25. doi: 10.1084/jem.194.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Novak J, Julian BA, Mestecky J, Renfrow MB. Glycosylation of IgA1 and pathogenesis of IgA nephropathy. Seminars in immunopathology. 2012;34:365–82. doi: 10.1007/s00281-012-0306-z. [DOI] [PubMed] [Google Scholar]
- 143.Lai KN. Pathogenesis of IgA nephropathy. Nature reviews Nephrology. 2012;8:275–83. doi: 10.1038/nrneph.2012.58. [DOI] [PubMed] [Google Scholar]
- 144.Espinosa M, Ortega R, Sanchez M, et al. Association of C4d deposition with clinical outcomes in IgA nephropathy. Clinical journal of the American Society of Nephrology: CJASN. 2014;9:897–904. doi: 10.2215/CJN.09710913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Roos A, Rastaldi MP, Calvaresi N, et al. Glomerular activation of the lectin pathway of complement in IgA nephropathy is associated with more severe renal disease. Journal of the American Society of Nephrology: JASN. 2006;17:1724–34. doi: 10.1681/ASN.2005090923. [DOI] [PubMed] [Google Scholar]
- 146.Goicoechea de Jorge E, Caesar JJ, Malik TH, et al. Dimerization of complement factor H-related proteins modulates complement activation in vivo. Proc Natl Acad Sci U S A. 2013;110:4685–90. doi: 10.1073/pnas.1219260110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Tortajada A, Yebenes H, Abarrategui-Garrido C, et al. C3 glomerulopathy-associated CFHR1 mutation alters FHR oligomerization and complement regulation. The Journal of clinical investigation. 2013;123:2434–46. doi: 10.1172/JCI68280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhu L, Zhai YL, Wang FM, et al. Variants in Complement Factor H and Complement Factor H-Related Protein Genes, CFHR3 and CFHR1, Affect Complement Activation in IgA Nephropathy. Journal of the American Society of Nephrology: JASN. 2014 doi: 10.1681/ASN.2014010096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hughes AE, Orr N, Esfandiary H, Diaz-Torres M, Goodship T, Chakravarthy U. A common CFH haplotype, with deletion of CFHR1 and CFHR3, is associated with lower risk of age-related macular degeneration. Nature genetics. 2006;38:1173–7. doi: 10.1038/ng1890. [DOI] [PubMed] [Google Scholar]
- 150.Zhao J, Wu H, Khosravi M, et al. Association of genetic variants in complement factor H and factor H-related genes with systemic lupus erythematosus susceptibility. PLoS genetics. 2011;7:e1002079. doi: 10.1371/journal.pgen.1002079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zipfel PF, Edey M, Heinen S, et al. Deletion of complement factor H-related genes CFHR1 and CFHR3 is associated with atypical hemolytic uremic syndrome. PLoS genetics. 2007;3:e41. doi: 10.1371/journal.pgen.0030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney inter, Suppl. 2012;2:139–274. [Google Scholar]
- 153.Coppo R, Peruzzi L, Amore A, et al. IgACE: a placebo-controlled, randomized trial of angiotensin-converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. Journal of the American Society of Nephrology: JASN. 2007;18:1880–8. doi: 10.1681/ASN.2006040347. [DOI] [PubMed] [Google Scholar]
- 154.Li PK-T, Leung CB, Chow KM, et al. Hong Kong Study Using Valsartan in IgA Nephropathy (HKVIN): A Double-Blind, Randomized, Placebo-Controlled Study. American Journal of Kidney Diseases. 2006;47:751–60. doi: 10.1053/j.ajkd.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 155.Praga M, Gutierrez E, Gonzalez E, Morales E, Hernandez E. Treatment of IgA nephropathy with ACE inhibitors: a randomized and controlled trial. Journal of the American Society of Nephrology: JASN. 2003;14:1578–83. doi: 10.1097/01.asn.0000068460.37369.dc. [DOI] [PubMed] [Google Scholar]
- 156.Horita Y, Tadokoro M, Taura K, et al. Prednisolone co-administered with losartan confers renoprotection in patients with IgA nephropathy. Renal failure. 2007;29:441–6. doi: 10.1080/08860220701260511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Russo D, Pisani A, Balletta MM, et al. Additive antiproteinuric effect of converting enzyme inhibitor and losartan in normotensive patients with IgA nephropathy. American Journal of Kidney Diseases. 33:851–6. doi: 10.1016/s0272-6386(99)70416-6. [DOI] [PubMed] [Google Scholar]
- 158.CP, PGB, GBF, et al. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999 doi: 10.1016/s0140-6736(98)03563-6. [DOI] [PubMed] [Google Scholar]
- 159.Pozzi C, Andrulli S, Del Vecchio L, et al. Corticosteroid effectiveness in IgA nephropathy: long-term results of a randomized, controlled trial. Journal of the American Society of Nephrology: JASN. 2004;15:157–63. doi: 10.1097/01.asn.0000103869.08096.4f. [DOI] [PubMed] [Google Scholar]
- 160.Manno C, Torres DD, Rossini M, Pesce F, Schena FP. Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2009;24:3694–701. doi: 10.1093/ndt/gfp356. [DOI] [PubMed] [Google Scholar]
- 161.Lv J, Xu D, Perkovic V, et al. Corticosteroid therapy in IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2012;23:1108–16. doi: 10.1681/ASN.2011111112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Strippoli GF, Maione A, Schena FP, Tognoni G, Craig JC. IgA nephropathy: a disease in search of a large-scale clinical trial to reliably inform practice. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2009;53:5–8. doi: 10.1053/j.ajkd.2008.10.035. [DOI] [PubMed] [Google Scholar]
- 163.Komatsu H, Fujimoto S, Sato Y, et al. “Point of no return (PNR)” in progressive IgA nephropathy: significance of blood pressure and proteinuria management up to PNR. Journal of nephrology. 2005;18:690–5. [PubMed] [Google Scholar]
- 164.Tang Z, Wu Y, Wang QW, et al. Idiopathic IgA nephropathy with diffuse crescent formation. American journal of nephrology. 2002;22:480–6. doi: 10.1159/000065281. [DOI] [PubMed] [Google Scholar]
- 165.Abe T, Kida H, Yoshimura M, et al. Participation of extracapillary lesions (ECL) in progression of IgA nephropathy. Clinical nephrology. 1986;25:37–41. [PubMed] [Google Scholar]
- 166.Tumlin JA, Lohavichan V, Hennigar R. Crescentic, proliferative IgA nephropathy: clinical and histological response to methylprednisolone and intravenous cyclophosphamide. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2003;18:1321–9. doi: 10.1093/ndt/gfg081. [DOI] [PubMed] [Google Scholar]
- 167.Stone JH, Merkel PA, Spiera R, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. The New England journal of medicine. 2010;363:221–32. doi: 10.1056/NEJMoa0909905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Specks U, Merkel PA, Seo P, et al. Efficacy of remission-induction regimens for ANCA-associated vasculitis. The New England journal of medicine. 2013;369:417–27. doi: 10.1056/NEJMoa1213277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Pozzi C, Andrulli S, Pani A, et al. Addition of azathioprine to corticosteroids does not benefit patients with IgA nephropathy. Journal of the American Society of Nephrology: JASN. 2010;21:1783–90. doi: 10.1681/ASN.2010010117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Alamartine E, Sabatier JC, Berthoux FC. Comparison of pathological lesions on repeated renal biopsies in 73 patients with primary IgA glomerulonephritis: value of quantitative scoring and approach to final prognosis. Clinical nephrology. 1990;34:45–51. [PubMed] [Google Scholar]
- 171.Schena FP. A retrospective analysis of the natural history of primary IgA nephropathy worldwide. The American journal of medicine. 1990;89:209–15. doi: 10.1016/0002-9343(90)90300-3. [DOI] [PubMed] [Google Scholar]
- 172.Xie J, Kiryluk K, Wang W, et al. Predicting progression of IgA nephropathy: new clinical progression risk score. PloS one. 2012;7:e38904. doi: 10.1371/journal.pone.0038904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Coppo R, Troyanov S, Bellur S, et al. Validation of the Oxford classification of IgA nephropathy in cohorts with different presentations and treatments. Kidney Int. 2014 doi: 10.1038/ki.2014.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Magistroni R, Furci L, Leonelli M, et al. A validated model of disease progression in IgA nephropathy. Journal of nephrology. 2006;19:32–40. [PubMed] [Google Scholar]
- 175.Koyama A, Igarashi M, Kobayashi M. Natural history and risk factors for immunoglobulin A nephropathy in Japan. Research Group on Progressive Renal Diseases. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1997;29:526–32. doi: 10.1016/s0272-6386(97)90333-4. [DOI] [PubMed] [Google Scholar]
- 176.Katafuchi R, Oh Y, Hori K, et al. An important role of glomerular segmental lesions on progression of IgA nephropathy: a multivariate analysis. Clinical nephrology. 1994;41:191–8. [PubMed] [Google Scholar]
- 177.Okada H, Suzuki H, Konishi K, Sakaguchi H, Saruta T. Histological alterations in renal specimens as indicators of prognosis of IgA nephropathy. Clinical nephrology. 1992;37:235–8. [PubMed] [Google Scholar]
- 178.D’Amico G. Natural history of idiopathic IgA nephropathy: role of clinical and histological prognostic factors. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2000;36:227–37. doi: 10.1053/ajkd.2000.8966. [DOI] [PubMed] [Google Scholar]
- 179.Smerud HK, Barany P, Lindstrom K, et al. New treatment for IgA nephropathy: enteric budesonide targeted to the ileocecal region ameliorates proteinuria. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2011;26:3237–42. doi: 10.1093/ndt/gfr052. [DOI] [PubMed] [Google Scholar]
- 180.International Multiple Sclerosis Genetics C. Beecham AH, Patsopoulos NA, et al. Analysis of immune-related loci identifies 48 new susceptibility variants for multiple sclerosis. Nat Genet. 2013;45:1353–60. doi: 10.1038/ng.2770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Visscher PM, Brown MA, McCarthy MI, Yang J. Five years of GWAS discovery. American journal of human genetics. 2012;90:7–24. doi: 10.1016/j.ajhg.2011.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Visekruna A, Joeris T, Seidel D, et al. Proteasome-mediated degradation of IkappaBalpha and processing of p105 in Crohn disease and ulcerative colitis. The Journal of clinical investigation. 2006;116:3195–203. doi: 10.1172/JCI28804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Wu F, Dassopoulos T, Cope L, et al. Genome-wide gene expression differences in Crohn’s disease and ulcerative colitis from endoscopic pinch biopsies: insights into distinctive pathogenesis. Inflammatory bowel diseases. 2007;13:807–21. doi: 10.1002/ibd.20110. [DOI] [PubMed] [Google Scholar]
- 184.Schmidt N, Gonzalez E, Visekruna A, et al. Targeting the proteasome: partial inhibition of the proteasome by bortezomib or deletion of the immunosubunit LMP7 attenuates experimental colitis. Gut. 2010;59:896–906. doi: 10.1136/gut.2009.203554. [DOI] [PubMed] [Google Scholar]
- 185.Fujimoto K, Karuppuchamy T, Takemura N, et al. A new subset of CD103+CD8alpha+ dendritic cells in the small intestine expresses TLR3, TLR7, and TLR9 and induces Th1 response and CTL activity. Journal of immunology. 2011;186:6287–95. doi: 10.4049/jimmunol.1004036. [DOI] [PubMed] [Google Scholar]
- 186.Uematsu S, Fujimoto K, Jang MH, et al. Regulation of humoral and cellular gut immunity by lamina propria dendritic cells expressing Toll-like receptor 5. Nature immunology. 2008;9:769–76. doi: 10.1038/ni.1622. [DOI] [PubMed] [Google Scholar]
- 187.Hom G, Graham RR, Modrek B, et al. Association of systemic lupus erythematosus with C8orf13-BLK and ITGAM-ITGAX. The New England journal of medicine. 2008;358:900–9. doi: 10.1056/NEJMoa0707865. [DOI] [PubMed] [Google Scholar]
- 188.Bertin J, Guo Y, Wang L, et al. CARD9 is a novel caspase recruitment domain-containing protein that interacts with BCL10/CLAP and activates NF-kappa B. The Journal of biological chemistry. 2000;275:41082–6. doi: 10.1074/jbc.C000726200. [DOI] [PubMed] [Google Scholar]
- 189.Sokol H, Conway KL, Zhang M, et al. Card9 mediates intestinal epithelial cell restitution, T-helper 17 responses, and control of bacterial infection in mice. Gastroenterology. 2013;145:591–601. e3. doi: 10.1053/j.gastro.2013.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Beaudoin M, Goyette P, Boucher G, et al. Deep resequencing of GWAS loci identifies rare variants in CARD9, IL23R and RNF186 that are associated with ulcerative colitis. PLoS genetics. 2013;9:e1003723. doi: 10.1371/journal.pgen.1003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Rivas MA, Beaudoin M, Gardet A, et al. Deep resequencing of GWAS loci identifies independent rare variants associated with inflammatory bowel disease. Nature genetics. 2011;43:1066–73. doi: 10.1038/ng.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Lanternier F, Pathan S, Vincent QB, et al. Deep dermatophytosis and inherited CARD9 deficiency. The New England journal of medicine. 2013;369:1704–14. doi: 10.1056/NEJMoa1208487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Vigorito E, Gambardella L, Colucci F, McAdam S, Turner M. Vav proteins regulate peripheral B-cell survival. Blood. 2005;106:2391–8. doi: 10.1182/blood-2004-12-4894. [DOI] [PubMed] [Google Scholar]
- 194.Liu JY, Seno H, Miletic AV, Mills JC, Swat W, Stappenbeck TS. Vav proteins are necessary for correct differentiation of mouse cecal and colonic enterocytes. Journal of cell science. 2009;122:324–34. doi: 10.1242/jcs.033720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Levison SE, Fisher P, Hankinson J, et al. Genetic analysis of the Trichuris muris-induced model of colitis reveals QTL overlap and a novel gene cluster for establishing colonic inflammation. BMC genomics. 2013;14:127. doi: 10.1186/1471-2164-14-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Eriksson N, Tung JY, Kiefer AK, et al. Novel associations for hypothyroidism include known autoimmune risk loci. PloS one. 2012;7:e34442. doi: 10.1371/journal.pone.0034442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Litinskiy MB, Nardelli B, Hilbert DM, et al. DCs induce CD40-independent immunoglobulin class switching through BLyS and APRIL. Nature immunology. 2002;3:822–9. doi: 10.1038/ni829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Osman W, Okada Y, Kamatani Y, Kubo M, Matsuda K, Nakamura Y. Association of common variants in TNFRSF13B, TNFSF13, and ANXA3 with serum levels of non-albumin protein and immunoglobulin isotypes in Japanese. PloS one. 2012;7:e32683. doi: 10.1371/journal.pone.0032683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Castigli E, Wilson SA, Garibyan L, et al. TACI is mutant in common variable immunodeficiency and IgA deficiency. Nature genetics. 2005;37:829–34. doi: 10.1038/ng1601. [DOI] [PubMed] [Google Scholar]
- 200.Kalabis J, Patterson MJ, Enders GH, et al. Stimulation of human colonic epithelial cells by leukemia inhibitory factor is dependent on collagen-embedded fibroblasts in organotypic culture. FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2003;17:1115–7. doi: 10.1096/fj.02-0852fje. [DOI] [PubMed] [Google Scholar]
- 201.Ernst M, Inglese M, Waring P, et al. Defective gp130-mediated signal transducer and activator of transcription (STAT) signaling results in degenerative joint disease, gastrointestinal ulceration, and failure of uterine implantation. The Journal of experimental medicine. 2001;194:189–203. doi: 10.1084/jem.194.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]