Abstract
Objective
This study investigated the role of a specialized physical therapy program for muscle tension dysphonia patients as an adjunct to standard of care voice therapy.
Study Design
Retrospective Cohort Study
Methods
Adult MTD patients seen between 2007 and 2012 were identified from the clinical database. They were prescribed voice therapy and, if concomitant neck pain, adjunctive physical therapy. In a pragmatic observational cohort design, patients underwent one of four potential treatment approaches: voice therapy alone (VT), voice therapy and physical therapy (VT+PT), physical therapy alone (PT), or incomplete/no treatment. Voice handicap outcomes were compared between treatment approaches.
Results
Of 153 patients meeting criteria (Median age 48 years, 68% female, and 30% had fibromyalgia, chronic pain, chronic fatigue, depression, and/or anxiety), there was a similar distribution of patients with moderate or severe pre-treatment VHI scores across treatment groups (VT 45.5%, VT+PT 43.8%, PT 50%, no treatment 59.1%; p=0.45). Patients treated with VT alone had significantly greater median improvement in VHI than those not treated: 10-point vs. 2-point (p=0.02). Interestingly, median VHI improvement in patients with baseline moderate-severe VHI scores was no different between VT (10), VT+PT (8) and PT alone (10; p=0.99).
Conclusions
Findings show voice therapy to be an effective approach to treating MTD. Importantly, other treatment modalities incorporating physical therapy had a similar, albeit not significant, improvement in VHI. This preliminary study suggests that physical therapy techniques may have a role in the treatment of a subset of MTD patients. Larger, comparative studies are needed to better characterize the role of physical therapy in this population.
1. 0 INTRODUCTION
Lifetime risk of developing a voice disorder is 30% with an estimated point prevalence of 3–9% in the U.S. population.1,2 Voice disorders negatively impact quality of life3, job performance, and job attendance3, costing approximately $2.67 billion dollars in lost wages, physicians’ visits, and treatment expenses.1,4 Muscle tension dysphonia (MTD) is a functional voice disorder that comprises approximately 10–40% of clinical caseloads in voice centers.5 It is characterized by increased laryngeal musculoskeletal tension with excessive muscular recruitment in the larynx and pharynx with concomitant disruption of efficient vibratory parameters.6 MTD is further classified as primary or secondary. Primary occurs in the absence of identifiable fixed laryngeal pathology (e.g. vocal fold lesions, paralysis), while secondary refers to MTD that occurs concomitantly with such pathologies. Clinically, both types present with variable symptomology including hoarseness, vocal fatigue, effortful voice production, change in habitual pitch, reduced vocal range, pain with voice use, muscular cramping and neck stiffness.
There is growing recognition that voice production requires whole-body muscular engagement. For example, posture related to the spine, shoulders, and hip position can impact voice.7,8,9 During speaking tasks, expiratory muscles and passive recoil of the thorax act to maintain adequate subglottic pressure for voicing. The sternocleidomastoid, scalene, and trapezius muscles are recruited to allow greater control of thoracic contraction during singing and complex speech tasks in which loudness and pitch are varied. This permits greater regulation of the subglottic pressures required to complete these demanding tasks10. Resonance also necessitates intricate coordination of muscles that alter tongue position, larynx height, and mouth opening.11 Therefore, muscle imbalances can disrupt any and all aspects of the mechanism – respiration, phonation, and articulation/resonance –and produce symptoms of MTD.
Treatment of MTD focuses on the rebalancing of subsystems involved in voice production, including respiration, phonation, and articulation, ultimately resulting in restoration of proper vibratory parameters and improved efficiency of voice production.11, 12 A systematic review from the Cochrane Collaboration found behavioral voice therapy – a combination of direct and indirect methods – to be an effective treatment for MTD.13 Indirect methods include vocal hygiene and voice conservation education. Direct methods use vocal exercises, facilitating vocal techniques, and often circumlaryngeal massage to increase efficiency of voice production and reduction of extra-laryngeal muscle tension. Manual circumlaryngeal massage is used to regulate and restore the balance of intrinsic and extrinsic laryngeal musculature during phonation.12 Some have attributed a portion of voice therapy failures to insufficient reduction of musculoskeletal tension,14 thereby underscoring the importance of manual treatment in this patient population.
Current treatment for MTD addresses extrinsic laryngeal area muscle tension, despite growing recognition implicating both laryngeal and “extralaryngeal musculature” as therapeutic targets.12,15 To treat the entire mechanism requires collaboration with practitioners adept at treating neck, back, shoulder, and diaphragmatic/abdominal muscular tension. In this study, we introduced a manual physical therapy treatment program as an adjunct to traditional voice therapy. The aim of this study was to determine patient perceived improvement in voice handicap using the Voice Handicap Index (VHI)16 when treated with 1) voice therapy alone, 2) combined voice and physical therapy, 3) physical therapy alone, or 4) incomplete or no treatment.
2.0 MATERIALS AND METHODS
This retrospective cohort study was performed in accordance with the Declaration of Helsinki, Good Clinical Practice, and was approved by the Institutional Review Board (IRB #131767).
2.1 Patient Database
Patients who presented to our voice clinic had demographic information and selected clinical data collected and entered into a secure Research Electronic Database Capture System (REDCap) database. 17 Patients completed survey materials at their initial clinic visit, follow-up visits, and any unique visits for voice therapy or manual physical therapy. Specific components included patient characteristics (e.g. age, gender), type of voice disorder (e.g. MTD, nodules), and treatments (e.g. voice therapy, physical therapy, and number/dates of visits) and Voice Handicap Index (VHI) scores.16
2.2 Inclusion criteria
For study inclusion, patients must have 1) been diagnosed with MTD by the treating laryngologist between 2007 and 2012; 2) had no laryngeal lesions (e.g. polyps, nodules, cancer) or neurological voice disorders (e.g. spasmodic dysphonia, tremor, vocal fold paresis/paralysis); 3) were ≥18 years of age; and 4) had ≥2 completed VHI scores with an initial VHI greater than 10; and 5) had no treatment lapses >90 days. A cut-off of 10 on the VHI was considered a conservative “normal” voice score based on a normative study that reported a mean VHI of 6.86 (SD 9.88).18 Patients with breaks in treatment >90 days were excluded because of the potential need for clinical re-evaluation and/or re-establishment of treatment goals. Such a lapse may also imply a cessation of treatment by the patient against clinician recommendation. A separate chart review was completed on all patients meeting inclusion criteria to validate database integrity and to ensure that all inclusion criteria had been met. Psychosomatic and related comorbidities were also collected during chart review; specific diagnoses included were fibromyalgia, chronic pain, chronic fatigue, anxiety, and depression. These were captured because they often coexist with MTD and can be treatment effect modifiers.19,20,21,22
2.3 Treatment Groups
The treating laryngologist recommended voice therapy for patients diagnosed with primary MTD.13 Primary MTD was defined as dysphonia in the absence of laryngeal pathology (e.g. laryngeal lesions, neurological laryngeal disorders).6 Adjuvant physical therapy was also recommended for MTD patients who were identified to have concomitant increased tenderness or tension in the thyrohyoid space, anterior neck, shoulders, and upper back identified by digital palpation. Patients’ variably complied with recommendations and self-selected into 4 pragmatic treatment groups: 1) voice therapy alone (VT), 2) combined voice therapy + physical therapy (VT+PT), 3) physical therapy alone (PT), 4) and incomplete or no treatment (None).
2.3.1 Voice Therapy
VT was defined as participation in at least 2 sessions of voice therapy within a 90-day window. Two visits included an initial voice evaluation consisting of baseline measurements and some facilitators and a second treatment session (Table 1). Patients continued after the second voice therapy session if still symptomatic or were discharged from voice therapy if the patient had achieved treatment goals developed at the time of evaluation. Voice therapy was provided by certified and licensed speech-language pathologists who exclusively treat voice disorders. Treatment approaches were selected based on clinician judgment. Voice therapy techniques had foundations with approaches consistent with motivational interviewing23, vocal hygiene, Lessac-Madsen Resonant Voice Therapy24, semi-occluded vocal tract25, and circumlaryngeal manipulation.12 Home exercise programs were developed with the patient and often audio and/or video recorded to promote adherence to recommendations.26 Treatment approaches were employed independent of one another or in combinations depending on the needs and learning approach of the individual patient, and thus had inherent variability. The retrospective nature of this study coupled with individualization of treatment approach prevented standardization within the voice therapy sessions. Minor overlap of approaches occurred during voice therapy and physical therapy (e.g. circumlaryngeal manipulation).
Table 1.
Program of Voice Therapy Interventions by Session.
| Topics | Major Content and Activities | Muscle group |
|---|---|---|
| Session 1: Evaluation | Program purpose Establish home exercise program Relaxation techniques Circumlaryngeal massage Cervical stretches Ergonomics Posture |
|
| Session 2 | Review home exercise program Supplemental techniques Ergonomics Posture |
Sternocleidomastoid m. Scalene m. |
| Session 3 | Neck and chest extensions Shoulder rotations Trunk Rotations |
Suprahyoid m. Infrahyoid m. |
| Session 4 | Review home exercise program Supplemental techniques Pectoralis stretches |
Chest m. |
| Session 5 | Self-releases Independent Exercises |
Posterior cervical m. |
| Session 6 | Tongue stretches Temporomandibular joint stretches |
Temporomandibular joint Masseter m. |
| Session 7 | Muscle imbalances in scapula and core | Suprahyoid m. .Infrahyoid m. |
| Session 8 | Stress management education | Psoas m. |
| Session 9 | Review home exercise program Discharge planning Additional referrals |
Thyroid releases Hyoid releases |
| Session 10 | Scar management Lower extremity stretching |
Thyroid releases Hyoid Releases Scar tissue releases (PRN) |
| Sessions 11 – 18 | Review home exercise program Additional individualized exercises |
Cervical traction Occipital traction Temporomandibular joint techniques |
2.3.2 Physical Therapy
Physical therapy was defined as having had least 8 sessions within a 90-day window. Eight sessions were deemed necessary to provide at least one treatment session focused on all targeted muscle areas (Table 2). Physical therapy was provided by physical therapists that had completed a training course in manual treatment specific to voice disorders by one of the authors. Physical therapy consisted of a systematic approach of manual therapy, education, and therapeutic exercises to address posture, muscle imbalances of the anterior neck, cervical range of motion, and symptoms of stress. Manual physical therapy techniques consist of a combination of joint mobilizations, passive range of motion, contract-relax stretches and myofascial release. It is speculated that muscular restrictions occur when connective tissue remodels in response to tension and stress. Thus, the therapeutic goal of this program was to decrease such restrictions within muscle groups and surrounding structures to improve function.
Table 2.
Program of Physical Therapy Interventions by Session
| VT | VT + PT | PT | Incomplete/None | p-value | |
|---|---|---|---|---|---|
| Age, Median (IQR) | 55 (44–59) | 44 (30–58.5) | 45.5 (39.5–59.5) | 47 (39.5–58.5) | 0.07 |
| Female | 82% | 63% | 50% | 67% | 0.14 |
| Tobacco Use | – | 6.3% | 6.3% | 4.6% | 0.60 |
| Treatment Duration, Days (IQR) | 74 (43–119) | 100 (61–139.5) | 67 (38.5–114) | 65 (27–90) | 0.27 |
| Fibromyalgia | 9.1% | 6.3% | 31.3% | 3.4% | 0.002* |
| Depression | 12.1% | 18.8% | 6.3% | 12.5% | 0.76 |
| Chronic Pain | 3.0% | – | 12.5% | 6.8% | 0.41 |
| Anxiety | 21.2% | 18.8% | 18.8% | 9.1% | 0.28 |
| Chronic Fatigue | – | – | 12.5% | – | 0.001* |
| Moderate/Severe VHI Score | 45.5% | 43.8% | 50.0% | 59.1% | 0.45 |
2.3.3 Other Treatment Groups
Patients treated with combined VT + PT were required to complete both within a 90-day window. Patients that did not participate in voice therapy or physical therapy, or had incomplete therapy defined as <2 voice therapy sessions within a 90-day window and/or <8 physical therapy sessions were categorized as “incomplete or no treatment” (None).
2.4 Statistical Analysis
VHI total score was the primary outcome measure used to compare treatment response between groups. Severity of voice disorder was judged based on initial VHI score, with 10–39 considered “mild”, 40–59 “moderate” and 60–120 “severe”.16 For analysis, severity was dichotomized into “mild” (i.e. VHI 10 – 39) and “moderate/severe” (i.e. VHI 40 – 120), as patients with a mild VHI score may not reach a clinically significant change given low baseline score. Median change in VHI score was selected as the primary outcome measure. Median was chosen to measure central tendency since it is more stable than mean in small samples with potential outliers. Change in VHI scores was used to measure the magnitude of voice handicap improvement or decrement. Statistical analyses were performed using chi-square and Kruskal-Wallis tests where appropriate. A secondary analysis evaluated the effect of having a psychosomatic comorbidity on treatment outcomes. All statistical analyses were performed in STATA MP version 12 (StataCorp, College Station, TX).
3.0 RESULTS
The categorization of patients included and excluded from this study is shown in Figure 1. In total, the 153 patients who met inclusion criteria had a median age of 48 years [Interquartile Range (IQR) 40–59] and 68% were female. Approximately 30% of patients had pre-existing psychosomatic or psychological comorbidities including anxiety (13.7%), depression (12.4%), fibromyalgia (8%), chronic pain (5.9%), and/or chronic fatigue (1.3%), as documented in their medical record.
Figure 1.
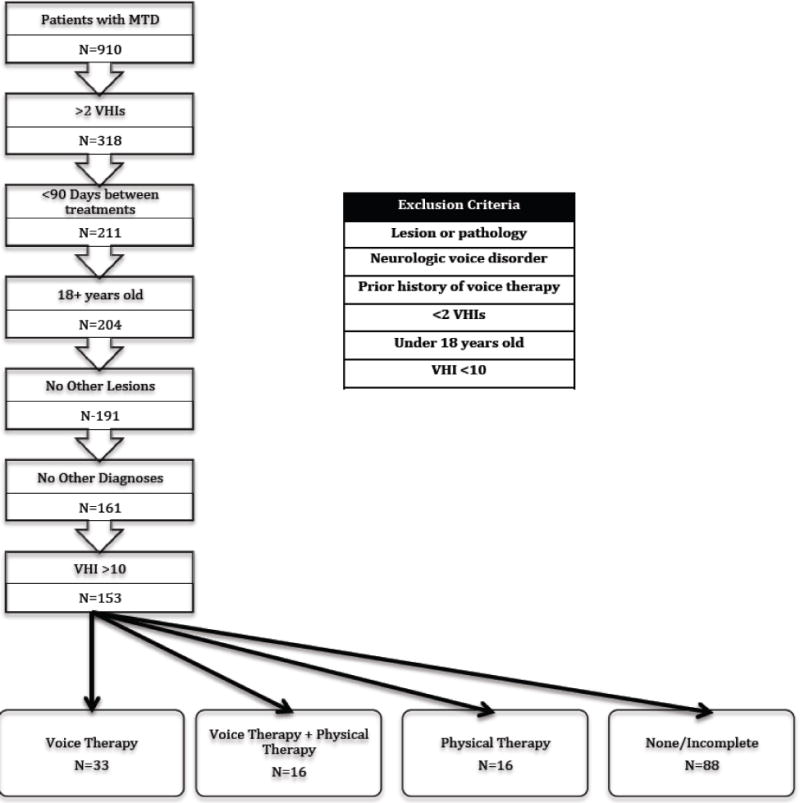
Inclusion/Exclusion Criteria
Patients with MTD treated with the four different approaches were similar in relation to age, gender, tobacco use, incidence of depression, chronic pain, and anxiety, treatment duration, and the proportion of individuals with “moderate and severe” baseline VHI scores (Table 3). The median number of visits differed significantly by treatment approach (VT 3 [IQR 2 – 4], VT + PT 16.5 [IQR 13.5 – 18.5], PT 13.5 [IQR 11.5 – 15], and none 0 [IQR 0 – 0]; Chi2=109.5, p=0.0001).
Table 3.
Comparison of Patient Characteristics by Treatment Group
| VT | VT + PT | PT | Incomplete/None | p-value | |
|---|---|---|---|---|---|
| Age, Median (IQR) | 55 (44–59) | 44 (30–58.5) | 45.5 (39.5–59.5) | 47 (39.5–58.5) | 0.07 |
| Female | 82% | 63% | 50% | 67% | 0.14 |
| Tobacco Use | – | 6.3% | 6.3% | 4.6% | 0.60 |
| Treatment Duration, Days (IQR) | 74 (43–119) | 100 (61–139.5) | 67 (38.5–114) | 65 (27–90) | 0.27 |
| Fibromyalgia | 9.1% | 6.3% | 31.3% | 3.4% | 0.002* |
| Depression | 12.1% | 18.8% | 6.3% | 12.5% | 0.76 |
| Chronic Pain | 3.0% | – | 12.5% | 6.8% | 0.41 |
| Anxiety | 21.2% | 18.8% | 18.8% | 9.1% | 0.28 |
| Chronic Fatigue | – | – | 12.5% | – | 0.001* |
| Moderate/Severe VHI Score | 45.5% | 43.8% | 50.0% | 59.1% | 0.45 |
| Number of treatment sessions | 3 | 16.5 | 13.5 | 0 | 0.0001* |
3.1 VHI Outcomes
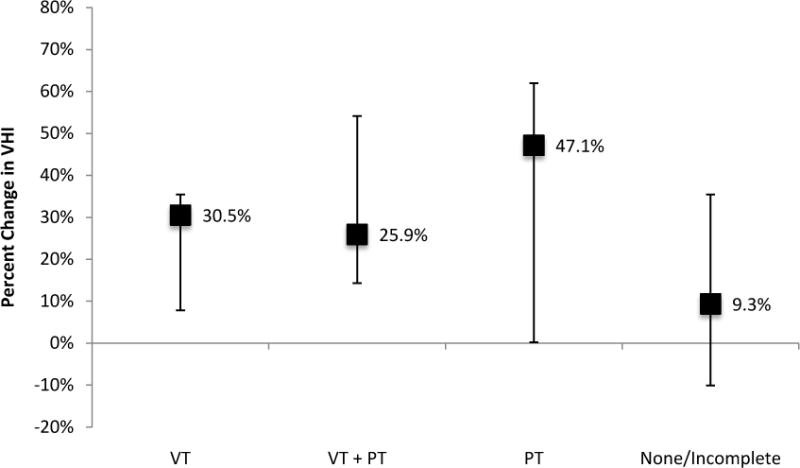
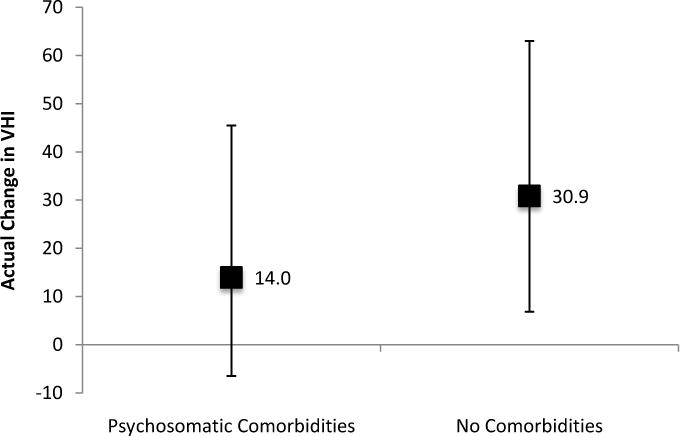
Overall, there was median 5-point (IQR 4 – 18) improvement of VHI regardless of treatment approach. When stratified, median VHI improvements were 10 (IQR 2 – 18), 8 (IQR −3.5 – 23.5), 10 (IQR −2.5 – 24), and 2 (IQR −7.5 – 13) for VT, VT+PT, PT, and none, respectively (Figure 2). However, only those treated with VT had significantly greater improvement than those with no treatment (Chi2=5.50, p=0.02). Patients presenting with mild dysphonia had 2-point VHI improvement (IQR −6 – 10) compared to 9- (IQR −2 – 25) among those with moderate to severe dysphonia (Chi2=10.6, p=0.001) (Figure 3).
Figure 2.

Overall Median Improvement in Voice Handicap Index Score by Treatment Group (VT=Voice therapy; VT+PT=Voice therapy and physical therapy; PT=Physical Therapy)
Figure 3.
Overall Median Improvement in Voice Handicap Index Score by Baseline Severity Voice Handicap Index Score
Moreover, those with mild dysphonia showed no statistical difference in post-treatment VHI improvement regardless of treatment approach (VT 3.5 [IQR −2 – 17]; VT+PT −3 [IQR −5 – 9]; PT 6.5 [IQR −15.5 –15.5]; None 0.5 [IQR −9 – 6.5]; Chi2=3.13, p=0.37) (Figure 4). Patients with moderate to severe dysphonia treated with VT, VT+PT, PT, and none had 10- (IQR 2 – 18), 8- (IQR −3.5 – 23.5), 10- (IQR −2.5 – 24), and 2-point (IQR −7.5 – 13) post-treatment improvement in VHI. There was significant improvement in VHI between patients treated with VT compared to no treatment (median 10 vs. 2; Chi2=5.50, p=0.02; Figure 5). No difference in voice handicap was observed between those treated with VT, VT+PT, and PT (Chi2=0.012, p=0.99). Greater, but non-significant improvement existed for moderate to severely dysphonic patient treated with all approaches compared to none [VT 17 vs. none 5 (p=0.07); VT+PT 22 vs. 5 (p=0.06); PT 24 vs. 5 (p=0.06)]. In secondary analysis, median presenting VHI scores were similar whether or not patients had psychosomatic or psychological comorbidities (absent 25 [IQR 18 – 32] vs. present 25.5 (IQR 22 – 30); p=0.93). Moreover, presence of these comorbidities did not have a differential affect on VHI improvement (absent 4 [IQR −5 – 17] vs. present 7 [IQR −4 – 22]; p=0.39).
Figure 4.
Median Voice Handicap Index Improvement with Mild Baseline (VT= Voice therapy; VT+PT=Voice therapy and physical therapy; PT=Physical Therapy)
Figure 5.
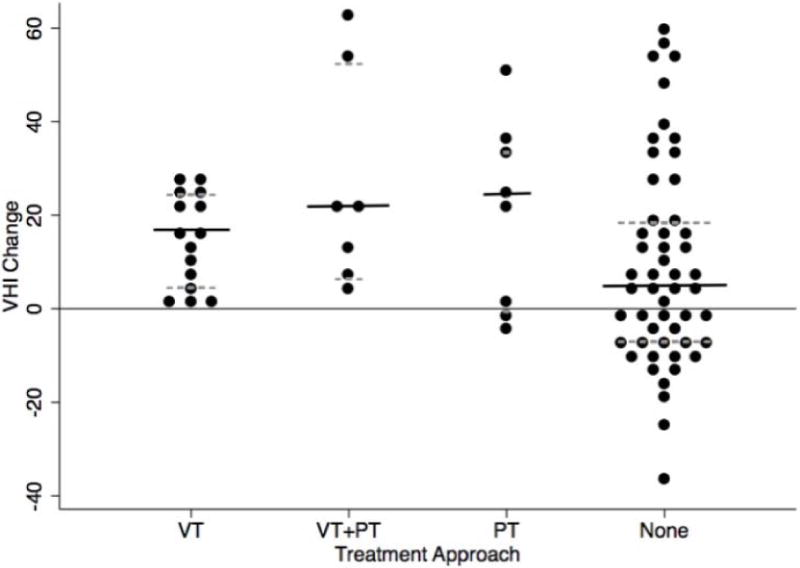
Median Voice Handicap Index Improvement with Moderate-Severe Baseline (VT= Voice therapy; VT+PT=Voice therapy and physical therapy; PT=Physical Therapy)
4.0 DISCUSSION
This study found that patients with muscle tension dysphonia (MTD) treated with voice therapy, combined voice and physical therapy, or physical therapy alone had similar magnitude improvement in VHI score. However, only those treated with voice therapy showed statistically greater improvement when compared to no treatment. While this finding was largely anticipated based on prior studies,27,28 less expected was the strong trend toward VHI improvement among patients treated with the physical therapy regimen alone.
The decision to add adjunctive physical therapy to standard of care voice therapy was made for MTD patients with concomitant thyrohyoid space tenderness, strap muscle recruitment, base of tongue tightness, and/or neck tightness or tenderness. Physical therapy was not recommended as a monolithic treatment approach during the period studied. Instead, some patients who had combined voice and physical therapy recommended opted for physical therapy alone for varying reasons (e.g. insurance, time commitment). Clearly, treating MTD with physical therapy alone is unconventional, but the retrospective pragmatic study design allowed us to compare it to standard-of-care voice therapy and to combined voice and physical therapy, and no treatment. Somewhat surprisingly, physical therapy alone showed VHI improvement on par with voice therapy. Lack of a demonstrable statistical difference from no treatment is likely the byproduct of the small sample size and insufficient power. Nonetheless, this finding provides impetus for further evaluation of physical therapy as a potential adjunct in the MTD treatment armamentarium.
Several plausible explanations for the apparent effect of physical therapy exist, but perhaps the most probable is that some patients have dysphonia arising from muscle tension that extends beyond the intrinsic and extrinsic laryngeal musculature. Previously, it has been proposed that a proportion of voice therapy failures in MTD patients relate to inadequate reduction of muscle tension.14 This is speculative since identifying the role and degree that muscle tension contributes to dysphonia in difficult to objectively measure. Several studies propose that extra-laryngeal muscle tension is an unlikely contributor to dysphonia if patients are nonresponsive to circumlaryngeal massage.5,12 In this regard, circumlaryngeal massage is being used as a diagnostic tool as well as a therapeutic approach. However, based on our preliminary data, abandonment of manual therapy in the clinical setting if circumlaryngeal massage is not immediately effective may be premature especially if extra-laryngeal components of the voicing mechanism (e.g. neck, back, shoulders, diaphragm musculature) are contributing to vocal dysfunction. In essence, determining the etiology of dysphonia and contribution of muscle tension based on circumlaryngeal massage may be too simplistic. Importantly, circumlaryngeal massage and manual therapy practiced by physical therapists (and others) have similar foundational underpinnings, but the latter addresses muscular areas that may be overlooked or completely treated and can confound voice therapy results. The treating clinician (e.g. physician or speech language pathologist) should consider all extra-laryngeal components of the voicing mechanism and take care not to prematurely abandon strategies that reduce musculoskeletal tension.
It remains uncertain whether MTD promotes or is the consequence of extra-laryngeal muscle tension. A window into this relationship is the finding that a high percentage of our patients (30%) had concomitant fibromyalgia, chronic pain, chronic fatigue, anxiety and/or depression. These conditions have been posited to mitigate therapy effectiveness. This assertion is supported by prior studies that have found dysphonia in this population to be refractory to standard of care voice therapy19,20,21. In our cohort, patients with fibromyalgia, chronic pain, anxiety and/or depression had similar baseline VHI scores and demonstrated no difference in post-treatment VHI improvement when compared to patients who do not carry these diagnoses. Interestingly, a disproportionate number of these patients participated in physical therapy alone (Table 3), highlighting the need for further studies investigating treatment efficacy in complex patient populations.
That the voice improvement in MTD patients treated with physical therapy alone or in combination with voice therapy is of similar magnitude as those treated with standard of care voice therapy is intriguing, but were not significantly better than no treatment. While these results are necessarily preliminary, there is an apparent effect and it is suggested that the treatment of muscle tension outside the narrow focus on the intrinsic and extrinsic laryngeal musculature deserves further study.
Use of retrospective data has inherent limitations. Specific treatment recommendations and physician decision-making impose a selection bias, as patients with concomitant neck pain were disproportionately referred for physical therapy. Patient self-selection of treatment may also contribute bias. For example, patients with fibromyalgia may opt for manual therapy because they have somatic complaints. Sample size limitations obviated the ability to meaningfully analyze this subpopulation. Finally, we were only able to analyze those patients who had adequate available VHI data captured in the database. In fact, lack of follow-up VHI data was the primary reason for exclusion from the study as demonstrated in Figure 1. This does not necessarily mean that these patients did not follow-up, but rather that they did not complete the VHI survey at their visit. Generalizability could be reduced if patients who completed the surveys were systematically different from those who did not. While possible, this seems unlikely. Despite recognized limitations, ours is among the first studies to show that a manual physical therapy treatment regimen encompassing a full-body approach may prove to be effective adjunctive to or, in select circumstances, a stand alone treatment for muscle tension dysphonia.
5. 0 CONCLUSION
Muscle tension dysphonia is arguably the most common voice disorder seen at tertiary voice centers and its treatment, to date, has largely focused on direct and indirect behavioral voice therapy treatment. Voice therapy is an efficacious treatment for this disease entity and has been strengthened with inclusion of circumlaryngeal massage. The focus on massage has spurned consideration for a more holistic manual therapy approach to the entire voicing mechanism including the neck, back, shoulders, diaphragm and abdomen. We provide preliminary data, albeit not statistically significant, that suggest manual physical therapy techniques may have a role in a subset of patients with MTD and that it should be considered in treatment planning as part of the voice clinician’s armamentarium. Future comparative effectiveness studies are needed to prove effectiveness and to better refine indications for its use.
Acknowledgments
Dr. Francis is supported by K23 DC013559/DC/NIDCD NIH HHS/United States
Footnotes
Level of Evidence: Retrospective Cohort Study; 2b
Conflict of interest: The Physical Therapy intervention is a copyrighted program.
This data was presented as an oral presentation at the British Laryngological Association Annual Meeting, London, United Kingdom on June 26th, 2014.
6.0 REFERENCES
- 1.Roy N, Merrill RM, Gray SD, Smith EM. Voice disorders in the general population: prevalence risk factors and occupational impact. The Laryngoscope. 2005;115(11):1988–1995. doi: 10.1097/01.mlg.0000179174.32345.41. 2005. [DOI] [PubMed] [Google Scholar]
- 2.Verdolini K, Ramig LO. Review: occupational risks for voice problems. Logopedics Phonatrics Vocology. 2001;26(1):37–46. [PubMed] [Google Scholar]
- 3.Cohen SM, Dupont WD, Courey MS. Quality-of-life impact of non-neoplastic voice disorders: a meta-analysis. Annals of Otology, Rhinology and Laryngology. 2006;115(2):128. doi: 10.1177/000348940611500209. 2006. [DOI] [PubMed] [Google Scholar]
- 4.American Speech-Language-Hearing Association. The use of voice therapy in the treatment of dysphonia [Technical Report] 2005 Available from www.asha.org/policy. – See more at: http://www.asha.org/policy/TR2005-00158.htm#sthash.jDjYqN2l.dpuf.
- 5.Van Houtte E, Van Lierde K, Claeys S. Pathophysiology and treatment of muscle tension dysphonia: a review of the current knowledge. Journal of Voice. 2001;25(2):202–207. doi: 10.1016/j.jvoice.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Morrison MD, Rammage LA. Muscle misuse voice disorders: description and classification. Acta oto-laryngologica. 1993;113(3):428–434. doi: 10.3109/00016489309135839. [DOI] [PubMed] [Google Scholar]
- 7.Gilman M. Learning to See: The role of posture in vocal rehabilitation. ASHA Convention. 2010 Nov 19, 2010. [Google Scholar]
- 8.Kooijman PGC, De Jong FICRS, Oudes MJ, Huinck W, Van Acht H, Graamans K. Muscular tension and body posture in relation to voice handicap and voice quality in teachers with persistent voice complaints. Folia phoniatrica et logopaedica. 2005;57(3):134–147. doi: 10.1159/000084134. [DOI] [PubMed] [Google Scholar]
- 9.Schneider CM, Dennehy CA, Saxon KG. Exercise Physiology Principles Applied to Vocal Performance: The Improvement of Postureal Alignment. Journal of Voice. 1997;11(3):332–337. doi: 10.1016/s0892-1997(97)80012-4. [DOI] [PubMed] [Google Scholar]
- 10.Pettersen V, Bjorkoy K, Torp H, Westgaard R. Neck and shoulder muscle activity and thorax movement in singing and speaking tasks with variation in vocal loudness and pitch. Journal of Voice. 2005;19(4):623–634. doi: 10.1016/j.jvoice.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Roy N, Nissen SL, Dromey C, Sapir S. Articulator changes in muscle tension dysphonia: Evidence of vowel space expansion following manual circumlaryngeal therapy. Journal of Communication Disorders. 2009;42(2):124–135. doi: 10.1016/j.jcomdis.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Roy N, Bless D. Manual circumlaryngeal techniques in the assessment and treatment of voice disorders. Current Opinion in Otolaryngology & Head and Neck Surgery. 1998;6:151–155. [Google Scholar]
- 13.Ruotsalainen Jani H, et al. Interventions for preventing voice disorders in adults. Cochrane Database of Systematic Reviews. 2007;17:4. doi: 10.1002/14651858.CD006372.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aronson AE. Clinical Voice Disorders: An Interdisciplinary Approach. 3. New York: Thieme; 1990. [Google Scholar]
- 15.Boone DR, McFarlane SC, Von Berg SL, Zraick RI. The voice and voice therapy. 8th. Allyn & Bacon; 2010. [Google Scholar]
- 16.Jacobson B, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger M, Newman C. The Voice Handicap Index (VHI): Development and Validation. Am J Speech Lang Pathol. 1997;6:66–70. [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arffa RE, Krishna P, Gartner-Schmidt J, Rosen CA. Normative values for the voice handicap index-10. Journal of Voice. 2012;26(4):462–465. doi: 10.1016/j.jvoice.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Thieme K, Rose U, Pinkpank T, Spies C, Turk DC, Flor H. Psychophysiological responses in patients with fibromyalgia syndrome. Journal of psychosomatic research. 2006;61(5):671–679. doi: 10.1016/j.jpsychores.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 20.Gurbuzler L, Inanir A, Yelken K, Koc S, Eyibilen A, Uysal IO. Voice disorder in patients with Fibromyalgia. Auris Nasus Larynx. 2013;40(6):554–557. doi: 10.1016/j.anl.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 21.Elert J, Kendall SA, Larsson B, Månsson B, Gerdle B. Chronic pain and difficulty in relaxing postural muscles in patients with fibromyalgia and chronic whiplash associated disorders. The Journal of rheumatology. 2001;28(6):1361–1368. [PubMed] [Google Scholar]
- 22.Willinger U, Völkl-Kernstock S, Aschauer HN. Marked depression and anxiety in patients with functional dysphonia. Psychiatry research. 2005;134(1):85–91. doi: 10.1016/j.psychres.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 23.Behrman Alison. Facilitating behavioral change in voice therapy: the relevance of motivational interviewing. American Journal of Speech-Language Pathology. 2006;15(3):215–225. doi: 10.1044/1058-0360(2006/020). [DOI] [PubMed] [Google Scholar]
- 24.KV Abbott. Lessac-Madsen Resonant Voice Therapy: Clinician Manual. Plural Publishing. 2008 [Google Scholar]
- 25.Titze Ingo R. Voice training therapy with a semi-occluded vocal tract: rationale and scientific underpinnings. Journal of Speech, Language, and Hearing Research. 2006;49(2):448–459. doi: 10.1044/1092-4388(2006/035). [DOI] [PubMed] [Google Scholar]
- 26.van Leer E, Connor NP. Use of portable digital media players increases patient motivation and practice in voice therapy. Journal of Voice. 2012;26(4):447–453. doi: 10.1016/j.jvoice.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carding Paul N, Horsley Irmgarde A, Docherty Gerard J. A study of the effectiveness of voice therapy in the treatment of 45 patients with nonorganic dysphonia. Journal of Voice. 1999;13(1):72–104. doi: 10.1016/s0892-1997(99)80063-0. [DOI] [PubMed] [Google Scholar]
- 28.MacKenzie Kenneth, et al. Is voice therapy an effective treatment for dysphonia? A randomised controlled trial. BMJ. 3232001:7314. 658. doi: 10.1136/bmj.323.7314.658. [DOI] [PMC free article] [PubMed] [Google Scholar]


