Significance
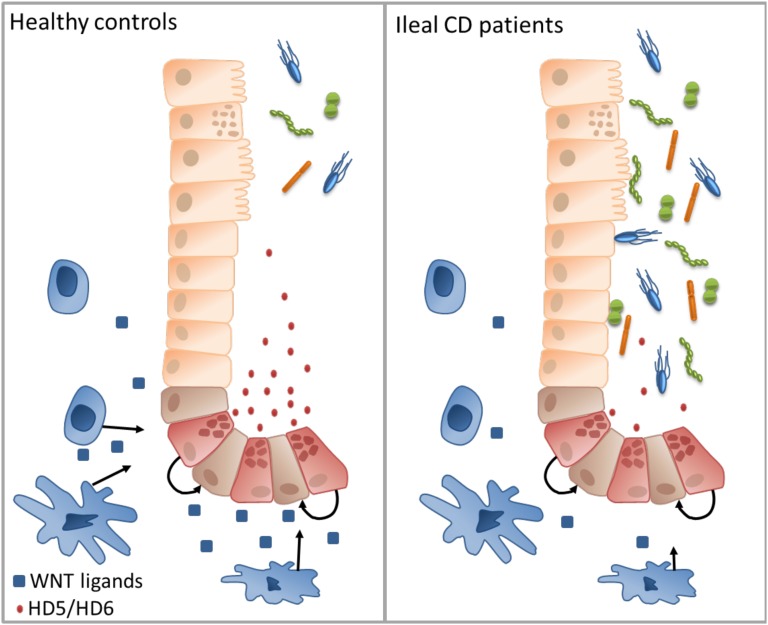
Paneth cell defensins (human α-defensins 5 and 6) are central players in the regulation of the human microbiome in the small intestine, but their regulation remains unclear. Here, we show that healthy monocytes can induce the expression of these defensins via Wnt ligands, especially in patients with Crohn’s disease (CD), who normally display reduced levels of human α-defensin 5 (HD5) and HD6, resulting in impaired host defense and, consequently, mucosal inflammation. However, monocytes from these patients are lacking this defensin-inducing capability, which seems to be based on compromised expression of Wnt ligands. This translational human study demonstrates defective cross-talk between monocytes and Paneth cells in CD with implications for gastrointestinal infections and bone marrow transplantation.
Keywords: α-defensins, Wnt ligands, Paneth cells, ileum, Crohn’s disease
Abstract
Crohn’s disease (CD) is associated with a multitude of genetic defects, many of which likely affect Paneth cell function. Paneth cells reside in the small intestine and produce antimicrobial peptides essential for the host barrier, principally human α-defensin 5 (HD5) and HD6. Patients with CD of the ileum are characterized by reduced constitutive expression of these peptides and, accordingly, compromised antimicrobial barrier function. Here, we present a previously unidentified regulatory mechanism of Paneth cell defensins. Using cultures of human ileal tissue, we showed that the secretome of peripheral blood mononuclear cells (PBMCs) from healthy controls restored the attenuated Paneth cell α-defensin expression characteristic of patients with ileal CD. Analysis of the Wnt pathway in both cultured biopsies and intestinal epithelial cells implicated Wnt ligands driving the PBMC effect, whereas various tested cytokines were ineffective. We further detected another defect in patients with ileal CD, because the PBMC secretomes derived from patients with CD were unable to restore the reduced HD5/HD6 expression. Accordingly, analysis of PBMC subtypes showed that monocytes of patients with CD express significantly lower levels of canonical Wnt ligands, including Wnt3, Wnt3a, Wnt1, and wntless Wnt ligand secretion mediator (Evi/Wls). These studies reveal an important cross-talk between bone marrow-derived cells and epithelial secretory Paneth cells. Defective Paneth cell-mediated innate immunity due to inadequate Wnt ligand stimulation by monocytes provides an additional mechanism in CD. Because defects of Paneth cell function stemming from various etiologies are overcome by Wnt ligands, this mechanism is a potential therapeutic target for this disease.
Crohn’s disease (CD) is characterized by intense gastrointestinal inflammation, including infiltration of immune cells, such as granulocytes and mononuclear cells. The pathogenesis is complex and not fully understood, although a combination of microbial and other environmental elements, as well as host genetics, is known to influence susceptibility (1, 2). Although CD may principally affect the whole gastrointestinal tract, predilection sites are the terminal ileum and/or colon, where the location remains stable during the course of disease, suggesting local rather than systemic immune-based susceptibility factors.
In patients who have CD with small intestinal involvement, different pathophysiological defects and genetic associations are described that focus on the Paneth cell (2). This cell type is normally located on the bottom of small intestinal crypts, where it is the main source for antimicrobial peptides, predominantly the human α-defensin 5 (HD5) and HD6. One main molecular characteristic of patients with ileal CD is reduced expression of these defensins, resulting in an impaired defense barrier through reduced antimicrobial killing (3). However, the impact of inflammation on Paneth cell function in the small intestine is so far poorly investigated. It also remains unclear whether the observed diminished defensin production is irreversible or a reversible regulatory defect.
The reduction of HD5 and HD6 in ileal CD in humans is also associated with mutations in the pattern recognition receptor nucleotide-binding oligomerization domain containing 2 (NOD2) (4), which also represents the strongest genetic link to ileal CD (5–7). In addition, our group and others showed alterations in Wnt pathway components in the epithelium of patients with CD (8–10). Furthermore, mutations in the Paneth cell granule exocytosis pathway factor ATG16L1 (11, 12) or in the endoplasmic reticulum stress response gene XBP1 (13, 14), with the latter resulting in increased Paneth cell apoptosis, are associated with this disease. Irrespective of genetics, other defects, including increased Paneth cell autophagy and a reduced number of secretory granules in patients with CD, were detected (15). Paneth cell deletion or dysfunction can ultimately result in inflammation (13, 16).
Although all these observations emphasize the central role of the Paneth cell in small intestinal CD, little is known about the regulation of these important defensins that were assumed to be constitutively expressed. However, the Wnt pathway known to control stem cell function and epithelial proliferation also affects the final maturation, as well as biological function, of Paneth cells by regulating the expression of HD5/HD6 (17, 18). For activating the canonical Wnt pathway, Wnt ligands bind to Frizzled/Lrp receptors, promoting the intracellular stabilization of β-catenin, which then translocates into the nucleus. There, it interacts with the transcription factors TCF/LEF and has further impacts on the transcription of its target genes, such as DEFA5 or DEFA6 (HD5/HD6) (19). Various Wnt components, including the transcription factors TCF4 (9) and TCF1 (20), the receptor LRP6 (8), and β-catenin/E-cadherin (10), are linked to CD with ileal involvement, likely through effects on defensin formation.
Studying Paneth cell defensins in humans is rather challenging, because there is no human Paneth cell line and colon cancer-derived cell lines exhibit mutations in Wnt pathway components. Moreover, to identify underlying defects of ileal CD, patients’ material is indispensable. Therefore, we established an ex vivo biopsy culture approach and used the secretome of peripheral blood mononuclear cells (PBMCs) as a tool to mimic an inflammatory setting. We found induction of α-defensin expression in ileal biopsies treated with the PBMC secretome ex vivo. In addition, we showed that this induction was mediated by Wnt factors rather than cytokines and, finally, that this stimulation was absent in mononuclear cells derived from patients with CD.
Results
Induction of Paneth Cell α-Defensin Expression by PBMC Conditioned Medium.
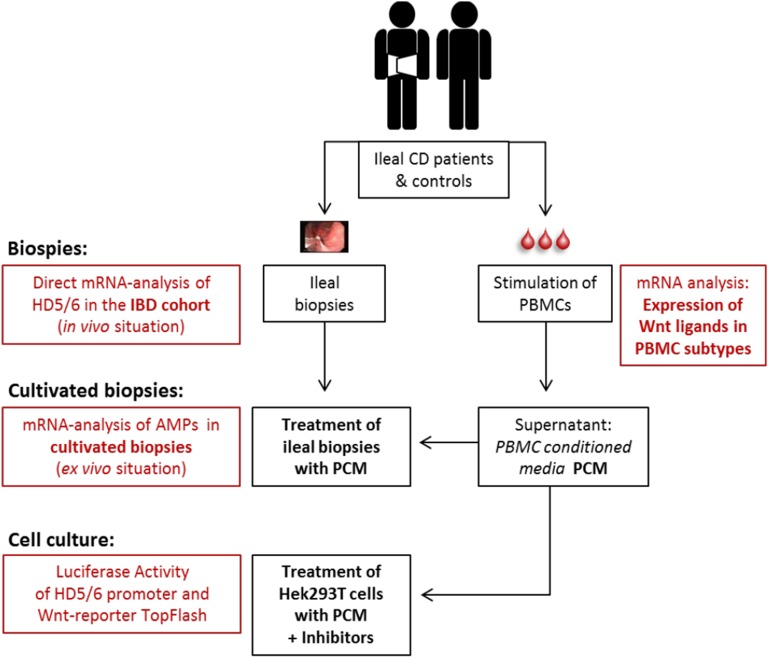
To get a broad picture of the cross-talk between inflammatory factors and Paneth cells, we applied several methods, including application of the PBMC secretome in cell and biopsy cultures and analysis of untreated biopsies (Fig. S1).
Fig. S1.
Study design. PBMCs from patients and controls were isolated and stimulated for 72 h. The supernatant includes the PBMC secretome and is termed PCM. RNA from suspension cells (lymphocytes) and adherent cells (monocytes) was analyzed separately. Biopsies were obtained from patients and controls during routine colonoscopy. Biopsies were either analyzed directly (in vivo situation) or cultivated for 6 h with PCM, control media, or other indicated reagents (ex vivo situation). Additionally, PCM was used to treat transfected Hek293T cells for 6 h. AMPs, antimicrobial peptides; IBD, inflammatory bowel disease.
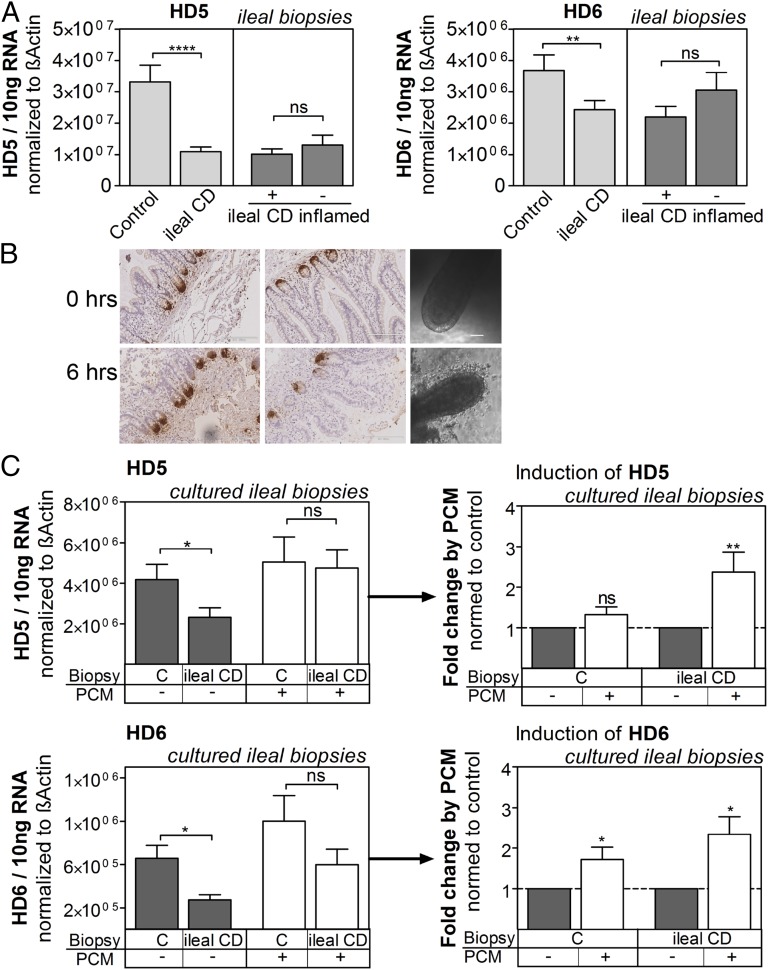
First, we studied the influence of tissue inflammation in patients on the expression of HD5 and HD6. In line with our previous data, we confirmed in a newly assembled cohort that expression of the main antimicrobials of the small intestine, HD5 and HD6, is diminished in patients with ileal CD (3, 4). In addition, HD5 and HD6 expression was comparable in inflamed tissue compared with uninflamed specimens from patients who had CD with ileal involvement (Fig. 1A).
Fig. 1.
PCM enhances α-defensin expression. (A) In untreated biopsies, the expression levels of HD5 and HD6 are diminished in patients with ileal CD and independent of inflammation. Shown are mRNA expression levels normalized to β-actin in inflamed and noninflamed tissue of patients with CD (n = 62, n = 45 inflamed) and controls (n = 25). HD5, P < 0.0001; HD6, P = 0.0038. (B) Cultured ileal biopsies. Anti-HD5 staining and microscopic pictures from ileal biopsies with or without cultivation (6 h). (C) PCM enhances HD5 and HD6 expression in cultured biopsies of patients with ileal CD. Ileal biopsies were treated either with PCM or control media (RPMI + PHA) for 6 h. Shown are the transcript levels normalized to β-actin (Left) or the fold change after PCM treatment normalized to respective control-treated biopsies (Right). In some cases, it was not possible to obtain data from both treatments because single biopsies did not pass quality control; therefore, the induction could not be calculated (n = 2). HD5, P = 0.0498; HD5 induction, P = 0.0039 (range: 1.2–5.3); HD6, P = 0.0114; HD6 induction, P = 0.0322; HD6 induction ileal CD, P = 0.0156 (range: 0.9–4.3) (n = 8–11). ns, not significant. *P < 0.05; **P < 0.01; ****P < 0.0001.
To study the effect of CD-independent inflammation on patient tissue mechanistically, we first designed a method to simulate inflammatory conditions ex vivo. Therefore, we generated a culture system where the secretome of activated PBMCs [PBMC conditioned medium (PCM)] was used to treat freshly isolated biopsies. After an incubation period of 6 h, the crypt-villus structures of the tissue remained intact and abundant HD5 protein was observed in Paneth cells (Fig. 1B). Consistent with the data from fresh biopsies, reduced expression of HD5 and HD6 persisted in ileal specimens of patients with CD after cultivation with control media, although the expression levels were generally even lower by a factor of 5–8 (Fig. 1C, Left). Interestingly, the difference between patients and controls was minimized after treatment with PCM, because the supernatant led to a significant 2.5-fold increase of HD5 mRNA expression in CD specimens, but not in controls. HD6, in contrast, was also enhanced in controls and slightly more in CD (Fig. 1C). We additionally tested a mix of killed bacteria in the biopsy culture approach. However, the tested bacteria were not able to influence HD5/HD6 (Fig. S2).
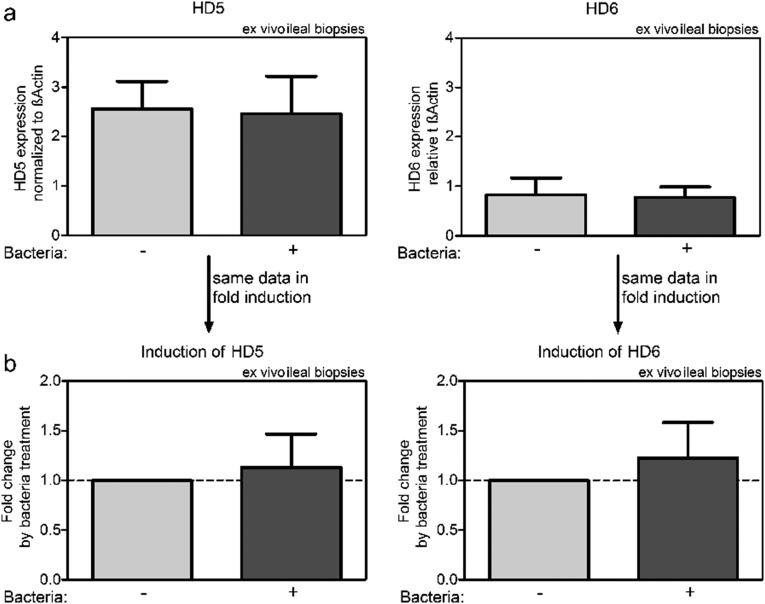
Fig. S2.
Tested bacteria show no influence on HD5/HD6 expression. Biopsies from controls were incubated with a mix of heat-inactivated bacteria or control media for 6 h. Displayed are the relative expression levels (A) and the fold changes (B) normalized to the respective media-control specimen (n = 6).
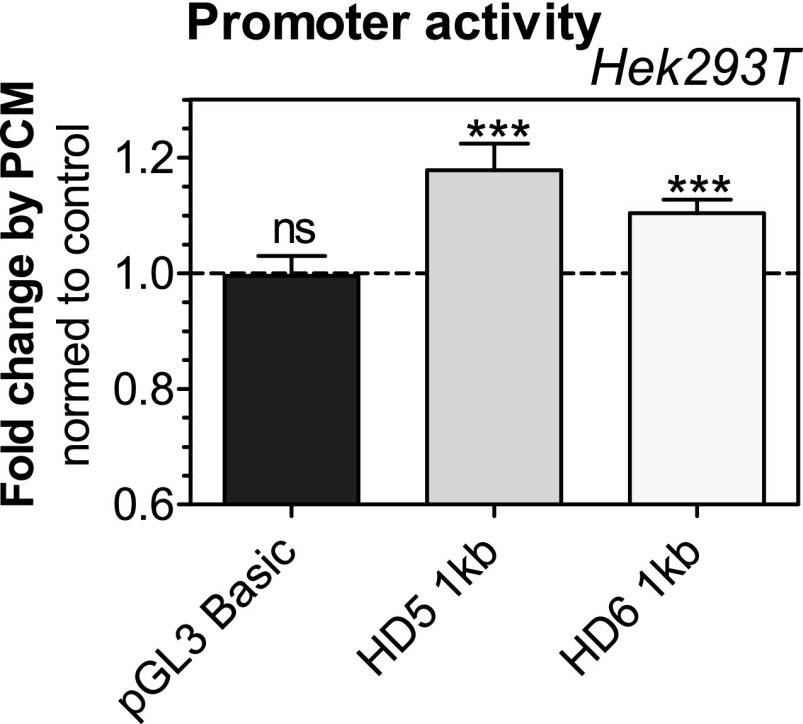
To confirm the stimulatory effect in another system, we used reporter gene assays in cell culture. Because most gastrointestinal cell lines have mutations in the Wnt pathway (21), we used the adenoviral established human embryonic kidney cell line Hek293T. Again, we detected a significant induction of the promoter activity of HD5 and HD6 by PCM treatment normalized to control media (Fig. S3). The observed effect in cell culture was comparably smaller; nonetheless, it confirmed our results obtained in the ex vivo biopsy approach.
Fig. S3.
PCM enhances HD5 and HD6 promoter activity also in vitro. Hek293T cells were transfected with reporter plasmids containing the promoter of HD5 or HD6 or the empty vector (pGL3 Basic) and stimulated with PCM or control media for 6 h. Renilla was used as an internal standard. Shown are fold changes normalized to basal treatment. HD5, P = 0.0001; HD6, P = 0.0006 (n = 16–28). ***P < 0.001. ns, not significant.
Differential Effect of PCM on Other Paneth Cell Antimicrobials.
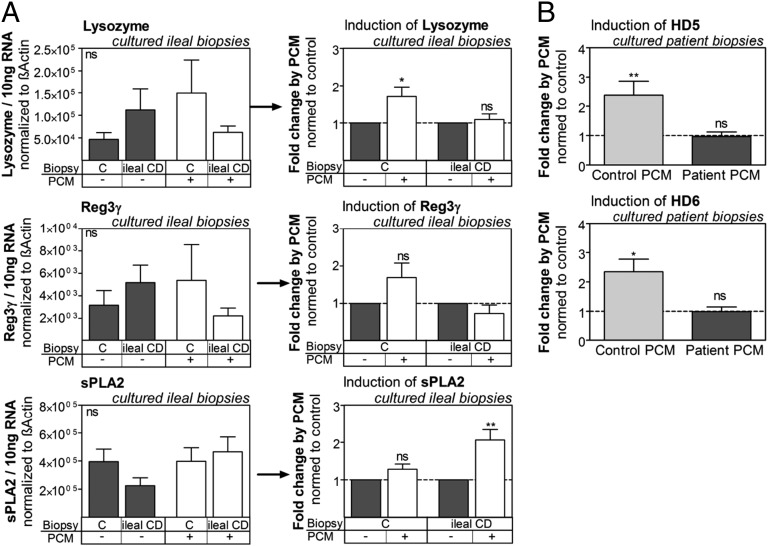
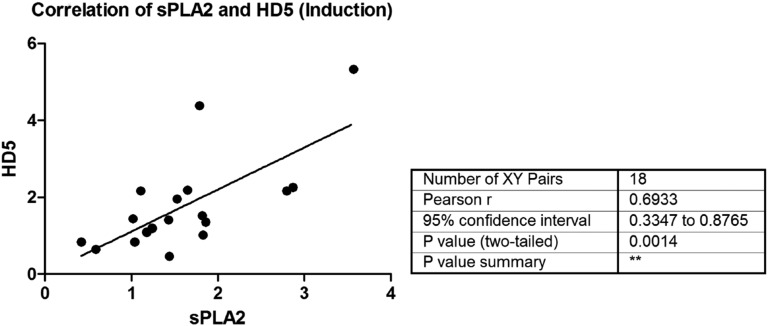
Paneth cells also produce several other antimicrobial peptides (22). Thus, we further checked for expression of lysozyme, phospholipase A2, group IIA (sPLA2), and regenerating islet-derived 3 (Reg3γ) in cultured biopsies with and without PCM treatment. There was no significant difference in the expression levels between patients and controls (Fig. 2A, Left), as has also been previously reported (3). In contrast to α-defensin expression, we observed an induction of lysozyme only in controls (Fig. 2A, Right). Furthermore, we observed no significant effect on Reg3γ expression. Although the mean expression pattern of this antimicrobial peptide appeared similar to lysozyme, no correlation between these factors was found, hinting at a different regulation. Only sPLA2, which can also be controlled by the Wnt pathway (23), exhibited a similar expression pattern to HD5 and HD6 and showed a significant correlation with HD5 (Fig. S4). The data therefore indicate that Paneth cell antimicrobials are differentially regulated.
Fig. 2.
Paneth cell antimicrobials are differentially regulated, and PCM from patients is functionally impaired. (A) Expression of other Paneth cell antimicrobials in cultivated biopsies. Small intestinal biopsies were treated with either PCM or control media (RPMI +PHA) for 6 h. Shown are transcript levels normalized to β-actin (Left) or fold changes of mRNA expression normalized to control treatment. Lysozyme, P = 0.0391; sPLA2, P = 0.0039 (n = 8–11). (B) Treatment of ileal CD patient biopsies with PCM from patients and controls shows functional differences. Freshly obtained biopsies were incubated with different PCMs for 6 h. Shown are fold changes by PCM treatment normalized to control media. HD5, P = 0.0039; HD6, P = 0.0156 (n = 8–9). *P < 0.05; **P < 0.01.
Fig. S4.
Correlation of HD5 and sPLA2 induction. Small intestinal biopsies were treated either with PCM or control media (RPMI + PHA) for 6 h. Shown is the correlation of HD5 and sPLA2 induction.
Defective Induction of HD5/HD6 by PBMCs from CD.
Because inflamed tissue of patients with ileal CD did not exhibit changed levels of HD5/HD6, whereas PCM treatment induced both defensins, we concluded that the secretome of controls contained a stimulating factor responsible for the induction. This mediator might be diminished in PBMCs from patients with CD, for which reason HD5/HD6 is not induced in inflamed tissue of these patients.
We consequently tested if PCM obtained from patient blood might differ in its capacity to induce HD5/HD6. Supporting our hypothesis, PCM stemming from patient blood essentially lacked the capability to induce these α-defensins (Fig. 2B), whereas PCM from controls exhibited normal induction. This observation demonstrated that immune cells from patients are functionally impaired in their ability to regulate Paneth cell defensins.
Regulatory Role of the Wnt Pathway but Not of Cytokines.
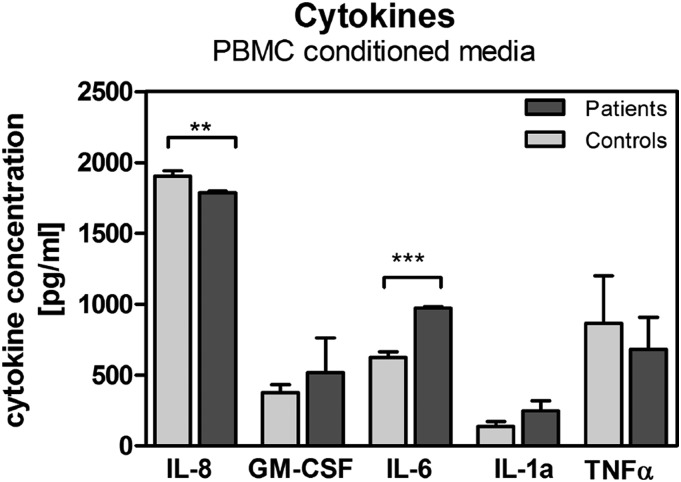
Next, we aimed at identifying the inducing factor in the PCM. Because the PBMC activation agent Phytohemagglutinin-L (PHA-L) is important for T-cell proliferation and further leads to the release of many cytokines (24, 25), we first looked into the effect of different cytokines on α-defensin expression. In the PCM, we tested the protein levels of selected cytokines (Fig. S5), which are released by activated PBMCs after PHA-L treatment (24). In line with the literature, we observed a decrease of IL-8 and increase of IL-6 levels in the PCM of patients (26, 27). For our stimulation experiments, we selected cytokines that were changed in the PCM of patients or known to be associated with CD (28).
Fig. S5.
Cytokine concentration in PCM from patients and controls. PBMCs from patients or controls were isolated and stimulated for 72 h. The supernatant (PCM) was analyzed by ELISAs (R&D Systems) (n = 7–14). **P < 0.01; ***P < 0.001.
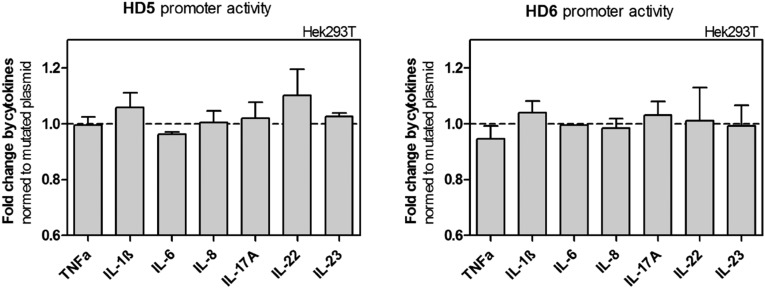
However, we could not detect a significant effect of any individually tested cytokine on Paneth cell defensin expression in vitro in our experiments (Fig. S6). Cytokines are the main effectors in regulating immune responses; however the tested candidates seem to be of no or only minor importance in enteric α-defensin regulation.
Fig. S6.
Single cytokines show no influence on HD5 or HD6 promoter activity. Different cytokines were individually used to treat transfected Hek293T cells for 6 h. Promoter activity was measured using a luciferase assay. Shown are fold changes normalized to mutated plasmid (n = 2–9).
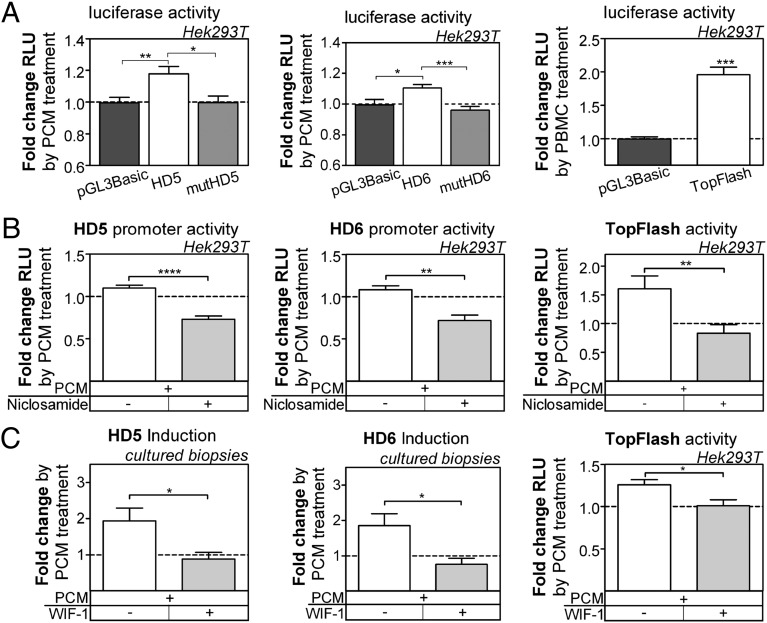
Because the Wnt pathway may play a role in regulating HD5 and HD6 in vitro and in vivo (8, 20, 29) and only Wnt-regulated Paneth antimicrobials were changed in our setting, we checked if this pathway is also involved in the PCM effect. To do so, we used HD5/HD6 promoter reporter gene constructs with and without mutations in the TCF-binding sites, as previously described (20). Mutated promoters exhibited diminished induction by PCM compared with the WT (Fig. 3A). Furthermore, we used the Wnt reporter plasmid TOPflash (kindly provided by Vladimir Korinek, Academy of Sciences of the Czech Republic, Prague), which contains several Wnt-binding sites (30) and observed an enhancing effect on TOPflash activity by PCM treatment (Fig. 3A).
Fig. 3.
PCM effect is mediated via Wnt. (A) PCM effect is impaired when Wnt-binding sites are mutated. HD5/HD6 constructs with mutated Wnt-binding sites or Wnt reporter TOPflash were transfected in Hek293T cells and treated with PCM for 6 h. Relative luciferase (RLU) values are normalized to untreated control: HD5 (n = 27) vs. pGL3 Basic (n = 16), P = 0.0069; HD5 vs. mutHD5 (n = 9), P = 0.031; HD6 (n = 28) vs. pGL3 Basic, P = 0.0246; HD6 vs. mutHD6 (n = 9), P = 0.0009; TOPflash (n = 19), P = 0.0001. (B) Frizzled receptor is essential for the PCM effect. Hek293T cells transfected with reporter gene plasmids were treated with PCM and ±5 μM niclosamide for 6 h. Relative luciferase values are normalized to untreated control. HD5 (n = 13), P < 0.0001; HD6 (n = 8), P = 0.007; TOPflash (n = 5), P = 0.0079. (C) Blocking Wnt ligands prevents PCM effect. Patient biopsies were treated with PCM and ±1 μg/mL WIF-1 for 6 h. Shown are fold changes by PCM treatment normalized to control media. HD5, P = 0.0285; HD6, P = 0.0281. PCM + WIF-1 (n = 10), PCM (n = 15). Transfected Hek293T cells were treated with PCM and ±1 μg/mL WIF-1 for 6 h. Relative luciferase values are normalized to untreated control. P = 0.015 (n = 7–8). *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001.
Several studies could show that inflammatory factors can have an impact on the Wnt pathway at different levels in the signaling cascade (31–33). To clarify at which level the PCM influences the Wnt pathway, we blocked the extracellular signaling events by inhibiting the Frizzled receptor. The small molecule inhibitor niclosamide is a known inhibitor of Frizzled1 and was shown to inhibit Wnt3A signaling (34, 35). Adding niclosamide to the cell culture system completely blocked the PCM effect (Fig. 3B) and even led to a decrease compared with the untreated setting. This effect might be due to the additional influence of niclosamide on other pathways (36), but it is also attributable to the fact that Wnt activity is generally needed for basal Paneth cell defensin expression. However, our results clearly demonstrated that external Wnt signals are involved in the induction observed after PCM treatment.
To pin down the effect on the Wnt pathway in the ex vivo situation, we used the protein Wnt inhibitory factor-1 (WIF-1), which binds to Wnt ligands and blocks their downstream effect (37, 38). Using PCM and WIF-1 simultaneously to treat patient biopsies, the enhancing effect was totally lost (Fig. 3C), which further underlines a clinical relevant Wnt deficiency in this disease. Additionally, using TOPflash as a read-out system in Hek293T cells, the same inhibition was achieved by WIF-1 (Fig. 3C, last graph). These data clearly demonstrate that Wnt ligands are the main effector molecules of PCM-mediated up-regulation of Paneth cell defensins.
Reduction of Wnt Ligands in CD Monocytes.
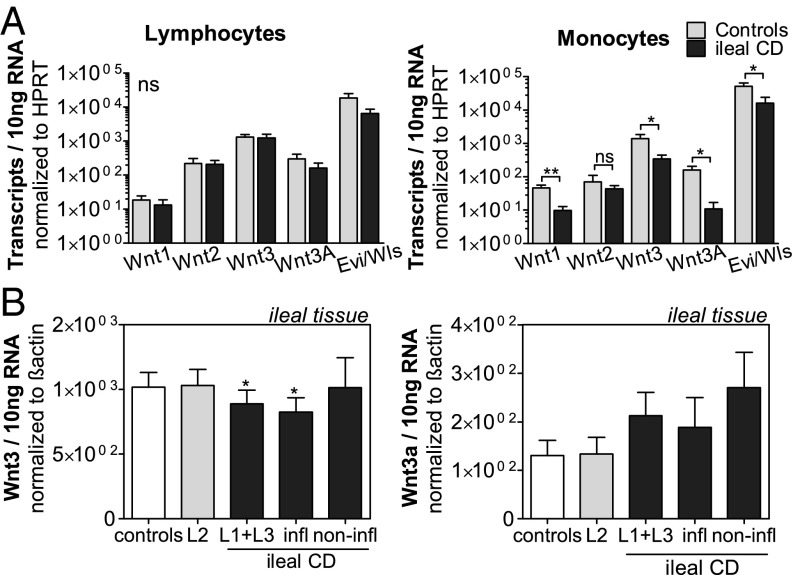
Because we demonstrated that Wnt ligands are responsible for the PCM-mediated effect and this influence is impaired in patients with ileal CD, we analyzed the expression of the main Wnt ligands in PBMC subtypes and in tissue of patients with ileal CD vs. healthy human controls. No expression differences were detected in lymphocytes (suspension cells) isolated from patients or controls (Fig. 4A, Left). In contrast, monocytes (adherent cells) originating from patient blood showed a significant reduction in Wnt1, Wnt3, and Wnt3A expression (Fig. 4A, Right). Additionally, a significant reduction of the Wnt ligand secretion mediator Evi/Wls in patient monocytes was seen, hinting at a potential additionally impaired export of Wnt ligands.
Fig. 4.
Wnt ligands are diminished in patient monocytes and partly in patient tissue. (A) mRNA expression of Wnt ligands from suspension cells (lymphocytes, n = 14–17) and adherent cells (monocytes, n = 9–10). PBMCs were isolated from whole blood and stimulated with PHA-L for 72 h. RNA from suspension and adherent cells was separately isolated. Shown is the mRNA expression of Wnt ligands and wntless Wnt ligand secretion mediator (Evi/Wls) normalized to hypoxanthine phosphoribosyltransferase (HPRT). Wnt1, P = 0.0017; Wnt3, P = 0.035; Wnt3A, P = 0.0345; Evi/Wls, P = 0.022. (B) In untreated ileal biopsies, the expression levels of Wnt3 are diminished in patients with ileal CD during inflammation. Shown are mRNA expression levels normalized to β-actin in inflamed and noninflamed tissue of patients with CD. Controls (n = 26), L2 (n = 21), L1 + L3 (n = 63), P = 0.0225; inflamed (n = 42), P = 0.0247; noninflamed (n = 21). *P < 0.05.
Keeping in mind that Wnt3A alone can activate TOPflash in Hek cells (38) leads to the conclusion that patients cannot provide enough Wnt ligands in inflammatory conditions to up-regulate HD5/HD6. Moreover, the analysis of Wnt ligands in the tissue is more inconclusive. Wnt3A was widely unchanged or rather increased in this setting (Fig. 4B), which might be due to a mixture of immune and epithelial cells in the studied tissue biopsies. However, we observed a reduction of the most abundant Wnt ligand, Wnt3, in ileal tissue of patients’ biopsies. This observation hints to a more prominent role for Wnt3 in the regulation of Paneth cell defensins.
Discussion
The present data show that, despite all described Paneth cell defects (2), the epithelium of patients with ileal CD is capable of producing a sufficient amount of enteric α-defensins in response to activated immune cells. However, infiltrating monocytes of these patients are impaired in producing important Wnt ligands acting as stimulants.
One main characteristic of the ileal type of CD is reduced expression of the main Paneth cell products HD5 and HD6, as reported by our group in 2004 (3, 4). Importantly, suggesting a primary role, this defect was independent of concurrent tissue inflammation. It therefore seemed that inflammatory cells have no role in the regulation of Paneth cell function, but the current data suggest the opposite: Normal monocyte supernatants apparently induce defensin formation in both control and CD Paneth cells. However, CD monocytes apparently exhibit an important deficit in this mechanism (summarized in Fig. S7). This impairment is consistent with our original observation of a low defensin synthesis also during active inflammation and disproves the findings of another report (39). In contrast, in CD-independent inflammatory situations in the ileum, such as infections, released immune cell factors like Wnt ligands may stimulate Paneth cell function to coordinate defense. Influences on HD5/HD6 expression were not observed when treating biopsies with certain cytokines or bacteria mixes, however, which emphasizes the specificity of these ligands in the PBMC secretome to regulate these defensins.
Fig. S7.
Schematic model for suggested hypothesis. In patients with ileal CD, monocytes are impaired in producing a sufficient amount of Wnt ligands, which leads to lower expression of Paneth cell defensins and, ultimately, to prolonged inflammation and reduced defense.
Since our original observation, a multitude of mostly genetic mechanisms have been found to be associated with the Paneth cells in ileal CD (2). As discussed above, the Paneth cell in CD is compromised by genetically defective NOD2 (6) and ATG16L1 (11), as well as endosomal stress (14), which, in combination, leads to ileal inflammation in the experimental animal (13). In addition, altered granules have been described in CD Paneth cells irrespective of genetics (15), which may add to the functional defects. It is therefore quite surprising that these defects may apparently be overcome and defensin expression may be normalized to control levels by an inflammatory cell supernatant. Our findings may also be relevant in the context that the majority of individuals with homozygous NOD2 mutations do not develop CD (40). These individuals may be protected by normal monocyte induction that could override other potential genetic Paneth cell defects. However, the rare occurrence of these SNPs would require stratification in a much larger cohort of patients than available for these ex vivo studies.
To define the monocyte mediators, we first tested cytokines as likely candidates. However, none of the tested cytokines exhibited a significant influence on the expression of α-defensins, despite their abundance in the PCM. However, previous studies could show a relationship between several cytokines, such as IFN-γ and TNF-α, and the Wnt pathway (41, 42), but these connections seem to depend strongly on the cell type or cross-talk with other cytokines or pathways (43). Other Paneth cell antimicrobials have also been reported to be influenced by cytokines, such as lysozyme, which is reduced after TNF-α treatment (44). Because our stimulation experiments using different single cytokines did not show any Paneth cell defensin induction, we concluded that these inflammatory factors are likely not responsible for the PCM-mediated effect on α-defensins.
Several hints led us finally to suspect a relevance of the Wnt pathway in the PCM stimulation setting. In former studies, we and others demonstrated that HD5 and HD6 are regulated by the Wnt pathway (29). It is known that Wnt factors are indeed found in macrophages (45–47) but are also expressed by intestinal tissue and by Paneth cells themselves (48, 49). However, a recent study in mice showed that epithelially derived Wnt ligands are not exclusively essential for proper epithelial homeostasis, hinting that another cell type is involved in Wnt ligand secretion (50). In our study, several lines of evidence suggest that the Wnt pathway is the key in regulation of Paneth cells by inflammatory cells. In cultured cells, the effect of the supernatant was abolished in the case of mutated HD5 and blocked by niclosamide. Potentially, several Wnt ligands could be involved in PCM induction; therefore, we used WIF-1 to block Wnt ligands globally rather than a multitude of Wnt ligand antibodies. The addition of WIF-1 to the PCM abolished the induction in cell culture and, most importantly, also in cultured ileal biopsies. This experiment clearly indicates that Wnt ligands are the inducing agent in the PCM.
Interestingly, the PBMC secretome derived from CD patients did not enhance enteric α-defensin expression, explaining why their levels are not normalized in the presence of inflammation in vivo. This deficit shows a primary functional impairment in peripheral immune cells of patients with ileal CD.
Additionally, in our setting, we observed differences between patients and controls in Wnt ligand expression in monocytes, but not in lymphocytes. Here, we showed, for the first time to our knowledge, that monocytes of patients with ileal CD express lower levels of important canonical Wnt ligands. It is already known that M2 macrophages, which are important for tissue regeneration, display differences regarding the expression of Wnt ligands in patients with ulcerative colitis (45). Because we isolated the monocytes by a basic sedimentation method (51), we could not further differentiate between monocytic subsets; nevertheless, we could clearly show that monocytes as a whole exhibit lower expression of important Wnt ligands in ileal CD. Future studies should include testing and analysis of different macrophage subsets to further clarify the functional Wnt ligand defect in patient PBMCs further. In addition, analyzing Wnt expression in tissue macrophages would be of great interest, because these cells are directly affecting Paneth cells in vivo.
These impairments in monocytes of patients with ileal CD could not only contribute to the diminished innate immune barrier based on lower HD5 and HD6 levels but could also have implications regarding tissue repair and healing. Fishbein et al. (52) and Lough et al. (53) also reported that HD5 expression decreases in intestinal allografts after transplantation into a NOD2-mutated recipient. These data underline the importance of myeloid cells for proper Paneth cell function, indicating the general importance of this interaction.
However, the origin of the differences in monocyte Wnt ligand expression remains unknown. Because some of the patients were on antiinflammatory drugs, such as steroids and azathioprine, we first washed the cells rigorously and cultivated the cells for 72 h to minimize drug effects. Because we only saw diminished expression of Wnt ligands in monocytes, but not in lymphocytes, we concluded that medications were an unlikely explanation of the differences observed between control and patient monocytes. It is clear that further mechanistic studies will be needed to elucidate underlying processes involved in the regulation of Wnt ligand expression in inflammatory cells. Furthermore, we cannot exclude the possibility that only one Wnt ligand is responsible for the observed effect. However, testing single Wnt ligands is currently technically impossible due to the limited availability of active Wnt proteins.
Because we performed an ex vivo study with human material, the findings can be easily applied to the human situation. This study highlights the importance of the Wnt pathway in the regulation of Paneth defensins and features an involvement of hematopoietic inflammatory cells in the pathogenesis of ileal CD. Most importantly, it shows that the defensin deficiency in ileal CD may be reversible, which opens up new avenues for the development of effective therapeutic possibilities. Other than only administering defensins to increase antimicrobial defense, there might be possibilities to stimulate the epithelium to produce a sufficient amount of these antimicrobial peptides. GM-CSF, which is known to stimulate macrophage activation and proliferation, was shown to be protective against dextran sulfate sodium (DSS)-induced colitis in mouse models (54) and some patient cohorts (55), but failed in a larger phase III study in the overall analysis (56). This failure might be explained by already impaired monocytes in these patients.
This mechanism described herein provides an additional rationale for bone marrow transplantation as a treatment option in severe cases (57). Other possible therapeutic interventions, such as activating the Wnt pathway, can have serious side effects like cancer, because this pathway has several other roles in cell proliferation. So far, not enough is known about the regulation of Wnt ligands, and further research regarding this aspect might be important for developing innovative therapeutic strategies.
Materials and Methods
Patient Material.
All patients and controls included in this study gave their written and informed consent after they were informed about the study purpose, sample procedure, and potential adjunctive risks. The study protocol was previously approved by the Ethical Committee of the University Hospital, Tuebingen, Germany. Biopsies from the terminal ileum were sampled during routine colonoscopy, and blood samples were obtained additionally for standard blood tests, both at the Robert Bosch Hospital, Stuttgart, Germany.
PCM and PBMC Subtype Separation.
PBMCs were isolated from EDTA-Blood using the Ficoll Histopaque (Biochrome) gradient centrifugation method, stimulated with PHA-L and incubated for 72 h. The supernatant was then centrifuged, resulting in the PCM. RNA was isolated from the resulting pellet (suspension cells = lymphocytes) (51) using an RNeasy Mini Kit (QIAGEN). To obtain RNA from monocytes (adherent cells), cells attached to the flask bottom were collected and centrifuged for 10 min at 400 × g, and the pellet was used for RNA isolation.
Biopsy Culture and Real-Time PCR.
Freshly obtained biopsies were washed several times with ice-cold PBS, immediately set into 1 mL of PCM or control media (RPMI+PHA), and incubated at 37 °C with 5% CO2 for 6 h. Denaturing agarose gels and lactate dehydrogenase (LDH)-cytotoxicity detection kit were used to check the quality of each sample. Samples with degraded RNA or high LDH values were excluded from the analysis. Absolute mRNA quantification was measured using a LightCycler 480 (Roche). The absolute copy numbers were calculated from the crossing point (Cp) values according to a standard plasmid. Primer sequences are listed in Table S1. Formalin fixed paraffin embedded tissue was stained with anti-DEFA5 antibody (Sigma–Aldrich) for immunohistochemistry.
Table S1.
Primers used in quantitative real-time PCR assays
| Gene product | Forward primer (5′→3′) | Reverse primer (5′→3′) |
| DEFA5 | GCC ATC CTT GCT GCC ATT C | AGA TTT CAC ACA CCC CGG AGA |
| DEFA6 | CCT CAC CAT CCT CAC TGC TGT TC | CCA TGA CAG TGC AGG TCC CAT A |
| HPRT | CCT GGC GTC GTG ATT AGT GA | CGA GCA AGA CGT TCA GTC CT |
| Lysozyme | GCT ACA GGG GAA TCA GCC TA | TGC TTC TGT CTC CAG CAT TG |
| REG3γ | CCT GCC TCA TTC TCC TGT GT | GAC AGC TGA TCC GTG GAG AG |
| sPLA2 | GCA GGA GCC CTT CTA TAC CC | GTT GAG GTG GAG GAG AGC AG |
| WNT1 | CCG ATG GTG GGG TAT TGT GAA | TCC CCG GAT TTT GGC GTA TC |
| WNT2 | TAG TCG GGA ATC TGC CTT TG | AAA TGC CTT TGC TGT CCT TG |
| WNT3 | ATG CCA CTG CAT CTT CCA CT | GTG CCC TAC TTG CAG GGT GT |
| WNT3A | TTG TCC ACG CCA TTG CCT CA | AGA CAC CAT CCC ACC AAA CTC G |
| β-ACTIN | GCC AAC CGC GAG AAG ATG A | CAT CAC GAT GCC AGT GGT A |
HPRT, hypoxanthine phosphoribosyltransferase.
Cell Culture and Transfection.
Hek293T cells were transfected with 500 ng of DNA using Turbofect (Fermentas). Plasmids used in these experiments were described previously (17, 20, 30). Twenty-four hours posttransfection, treatment with indicated media or agents was started. After 6 h of treatment, cells were lysed for measuring luciferase activity with the Dual Luciferase Reporter Assay (Promega).
A detailed description of all methods can be found in SI Materials and Methods.
SI Materials and Methods
Patient Material.
Freshly obtained biopsies were immediately stored in liquid nitrogen for analysis of uncultivated biopsies from patients (n = 90, mean age: 40 ± 1.4 y, 48% males, n = 48 inflamed) and controls (n = 27, mean age: 49 ± 4 y, 41% males) or put into ice-cold PBS for further cultivation experiments (patients: n = 21, median age: 40 ± 3.8 y, 70% males; controls: n = 20, median age: 48 ± 3.6 y, 50% males). The diagnosis was performed according to standard criteria using clinical, radiological, endoscopic, and histopathological results. Patients with CD were grouped after standard Vienna classifications with L1 as CD with ileal involvement, L2 as CD with colonic involvement, and L3 as CD with ileocolonic involvement. The genetic status of LRP6 and NOD2 was checked as described (8) but had no influence on the results. The detailed numbers of patient biopsies used for different experiments are specified in all figure legends.
PCM and PBMC Subtype Separation.
PBMCs were isolated from 18 mL of EDTA-blood from patients or controls (patients: n = 17, median age = 39 y, 53% males; controls: n = 14, median age = 43 y, 36% males) using the Ficoll Histopaque (Biochrome) gradient centrifugation method according to standard protocols. Cells (1 × 106 cells per milliliter) were seeded in RPMI-1640 media (Biochrome) containing 10% FCS, 1% penicillin/streptomycin, 1% l-glutamine, 1% sodium pyruvate, 1% Hepes buffer (1 M), 1% β-mercaptoethanol, 0.6% nonessential amino acids, and 0.2% Asn; stimulated with 2.5 μg/mL PHA-L (Roche); and incubated for 72 h. The supernatant was then centrifuged, resulting in the PCM. RNA was isolated from the resulting pellet (suspension cells = lymphocytes) (50) using an RNeasy Mini Kit (QIAGEN). To receive RNA from monocytes (adherent cells), cells attached to the flask bottom were washed rigorously with PBS, incubated with trypsin, and collected by scrapping. Cells were centrifuged for 10 min at 400 × g. RNA isolation was performed using the RNeasy Mini Kit.
Biopsy Culture.
Freshly obtained biopsies were washed several times with ice-cold PBS, immediately set into 1 mL of designated media, and incubated at 37 °C with 5% CO2 for 6 h. Thereafter, biopsies were put into RNAlater (Qiagen), and the supernatant was collected for subsequent quality control. The integrity of total RNA was analyzed using denaturing agarose gels. The viability of the samples was tested in the media using LDH-cytotoxicity detection kit (Roche) according to the manufacturer’s protocol. Samples with degraded RNA or high LDH values were excluded from the analysis.
Treatment of Ileal Biopsies with Inactivated Bacteria.
Bacteria (Lactobacillus fermentum, Lactobacillus acidophilus, Streptococcus salivarius, Enterococcus faecalis, Bacteroides vulgatus, Escherichia coli, and Bifidobacterium breve) were separately cultivated and heat-inactivated at 65 °C for 45 min. An amount of 3 × 108 bacteria per milliliter was dissolved in DMEM used to treat ileal biopsies for 6 h as described above.
Cell Culture and Transfection.
Hek293T cells were transfected with 500 ng of DNA using Turbofect (Fermentas) according to the manufacturer’s protocol. Plasmids used in these experiments (TOPflash, HD6, HD5, mutHD6, and mutHD5) were described previously (17, 20, 30). Twenty-four hours posttransfection, treatment with indicated media or agents was started. Used media were the above-described PCM or control media (RPMI + PHA). Agents used for stimulation or inhibition were TNF-α (Sigma), IL-6, IL-22 (ImmunoTools), IL-1β (PeproTech), IL-8, IL-17A, IL-23, niclosamide (Sigma), and WIF-1 (R&D Systems). After 6 h of treatment, cells were lysed for measuring luciferase activity with the Dual Luciferase Reporter Assay (Promega) using an Enspire PlateReader (PerkinElmer). Firefly luciferase signals were normalized to Renilla activities, with the latter representing the transfection efficiency. Each transfection was performed in triplicate in three or more independent experiments. The toxicity of the agents was tested, and therefore excluded by MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide] Tetrazolium assays.
RNA Preparation and Real-Time PCR.
RNA from tissue was isolated using TRIzol Reagent (Life Technologies). RNA from blood cells was isolated with the RNeasy Mini Kit, both according to each manufacturer’s protocol. RNA was quantified with a NanoDrop (Thermo Scientific) and transcribed into cDNA using the reverse transcription system (Promega) with oligo(dT)15-primer. The amount of cDNA according to 10 ng of RNA was applied in all assays. The absolute mRNA quantification was done using SYBR Green I (Roche) and measured in a Roche LightCycler 480. Used primers are listed in Table S1. The absolute copy numbers were calculated from the crossing point (Cp) values according to the respective standard plasmid.
Immunohistochemistry.
Formalin fixed paraffin embedded (FFPE) tissue slides from cultivated or fresh biopsies were used for staining procedures with anti-DEFA5 antibody (1:5,000; Sigma–Aldrich) using an EnVision Kit (Dako) according to standard protocols. Target retrieval solution at pH 6 (S1699, 1:10 ratio) and endogenous peroxidase blocking solution (S2023), both from Dako, were used. Hematoxylin counterstaining was performed to visualize the cell nuclei.
Statistical Analysis.
Expression differences between groups were analyzed using t tests. Fold changes, normalized to control treatment, were analyzed by Wilcoxon signed rank tests. All results are displayed by mean values ± SEM. Values of P < 0.05 were considered as statistically significant. Data were analyzed using GraphPad Prism 5.
Acknowledgments
We thank Jutta Bader, Kathleen Siegel, Katharina Höger, and Marion Strauss for the excellent technical assistance and Charles Bevins for data discussion. This work was supported by Deutsche Forschungsgemeinschaft (DFG) Project SPP1656 “Intestinal Microbiota” and by the Heisenberg Program (DFG), Robert Bosch Foundation, and European Research Council (Defensinactivity).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1510084112/-/DCSupplemental.
References
- 1.Rosenstiel P, Sina C, Franke A, Schreiber S. Towards a molecular risk map--recent advances on the etiology of inflammatory bowel disease. Semin Immunol. 2009;21(6):334–345. doi: 10.1016/j.smim.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Wehkamp J, Stange EF. Paneth’s disease. J Crohn’s Colitis. 2010;4(5):523–531. doi: 10.1016/j.crohns.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Wehkamp J, et al. Reduced Paneth cell alpha-defensins in ileal Crohn’s disease. Proc Natl Acad Sci USA. 2005;102(50):18129–18134. doi: 10.1073/pnas.0505256102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wehkamp J, et al. NOD2 (CARD15) mutations in Crohn’s disease are associated with diminished mucosal alpha-defensin expression. Gut. 2004;53(11):1658–1664. doi: 10.1136/gut.2003.032805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Economou M, Trikalinos TA, Loizou KT, Tsianos EV, Ioannidis JPA. Differential effects of NOD2 variants on Crohn’s disease risk and phenotype in diverse populations: A metaanalysis. Am J Gastroenterol. 2004;99(12):2393–2404. doi: 10.1111/j.1572-0241.2004.40304.x. [DOI] [PubMed] [Google Scholar]
- 6.Hugot JP, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411(6837):599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- 7.Ogura Y, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411(6837):603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- 8.Koslowski MJ, et al. Association of a functional variant in the Wnt co-receptor LRP6 with early onset ileal Crohn’s disease. PLoS Genet. 2012;8(2):e1002523. doi: 10.1371/journal.pgen.1002523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koslowski MJ, et al. Genetic variants of Wnt transcription factor TCF-4 (TCF7L2) putative promoter region are associated with small intestinal Crohn’s disease. PLoS One. 2009;4(2):e4496. doi: 10.1371/journal.pone.0004496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muise AM, et al. Polymorphisms in E-cadherin (CDH1) result in a mis-localised cytoplasmic protein that is associated with Crohn’s disease. Gut. 2009;58(8):1121–1127. doi: 10.1136/gut.2008.175117. [DOI] [PubMed] [Google Scholar]
- 11.Cadwell K, et al. A key role for autophagy and the autophagy gene Atg16l1 in mouse and human intestinal Paneth cells. Nature. 2008;456(7219):259–263. doi: 10.1038/nature07416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hampe J, et al. A genome-wide association scan of nonsynonymous SNPs identifies a susceptibility variant for Crohn disease in ATG16L1. Nat Genet. 2007;39(2):207–211. doi: 10.1038/ng1954. [DOI] [PubMed] [Google Scholar]
- 13.Adolph TE, et al. Paneth cells as a site of origin for intestinal inflammation. Nature. 2013;503(7475):272–276. doi: 10.1038/nature12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaser A, et al. XBP1 links ER stress to intestinal inflammation and confers genetic risk for human inflammatory bowel disease. Cell. 2008;134(5):743–756. doi: 10.1016/j.cell.2008.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thachil E, et al. Abnormal activation of autophagy-induced crinophagy in Paneth cells from patients with Crohn’s disease. Gastroenterology. 2012;142(5):1097–1099.e4. doi: 10.1053/j.gastro.2012.01.031. [DOI] [PubMed] [Google Scholar]
- 16.Kaser A, Blumberg RS. Paneth cells and inflammation dance together in Crohn’s disease. Cell Res. 2008;18(12):1160–1162. doi: 10.1038/cr.2008.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andreu P, et al. Crypt-restricted proliferation and commitment to the Paneth cell lineage following Apc loss in the mouse intestine. Development. 2005;132(6):1443–1451. doi: 10.1242/dev.01700. [DOI] [PubMed] [Google Scholar]
- 18.van Es JH, et al. Wnt signalling induces maturation of Paneth cells in intestinal crypts. Nat Cell Biol. 2005;7(4):381–386. doi: 10.1038/ncb1240. [DOI] [PubMed] [Google Scholar]
- 19.Logan CY, Nusse R. The Wnt signaling pathway in development and disease. Annu Rev Cell Dev Biol. 2004;20(1):781–810. doi: 10.1146/annurev.cellbio.20.010403.113126. [DOI] [PubMed] [Google Scholar]
- 20.Beisner J, et al. TCF-1-mediated Wnt signaling regulates Paneth cell innate immune defense effectors HD-5 and -6: Implications for Crohn’s disease. Am J Physiol Gastrointest Liver Physiol. 2014;307(5):G487–G498. doi: 10.1152/ajpgi.00347.2013. [DOI] [PubMed] [Google Scholar]
- 21.Ikenoue T, et al. Analysis of the β-catenin/T cell factor signaling pathway in 36 gastrointestinal and liver cancer cells. Jpn J Cancer Res. 2002;93(11):1213–1220. doi: 10.1111/j.1349-7006.2002.tb01226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bevins CL, Salzman NH. Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat Rev Microbiol. 2011;9(5):356–368. doi: 10.1038/nrmicro2546. [DOI] [PubMed] [Google Scholar]
- 23.Ganesan K, et al. Inhibition of gastric cancer invasion and metastasis by PLA2G2A, a novel beta-catenin/TCF target gene. Cancer Res. 2008;68(11):4277–4286. doi: 10.1158/0008-5472.CAN-07-6517. [DOI] [PubMed] [Google Scholar]
- 24.De Groote D, et al. Direct stimulation of cytokines (IL-1β, TNF-α, IL-6, IL-2, IFN-γ and GM-CSF) in whole blood. I. Comparison with isolated PBMC stimulation. Cytokine. 1992;4(3):239–248. doi: 10.1016/1043-4666(92)90062-v. [DOI] [PubMed] [Google Scholar]
- 25.Greaves M, Janossy G, Doenhoff M. Selective triggering of human T and B lymphocytes in vitro by polyclonal mitogens. J Exp Med. 1974;140(1):1–18. doi: 10.1084/jem.140.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gijsbers K, et al. CXCR1-binding chemokines in inflammatory bowel diseases: Down-regulated IL-8/CXCL8 production by leukocytes in Crohn’s disease and selective GCP-2/CXCL6 expression in inflamed intestinal tissue. Eur J Immunol. 2004;34(7):1992–2000. doi: 10.1002/eji.200324807. [DOI] [PubMed] [Google Scholar]
- 27.Jyonouchi H, Geng L, Cushing-Ruby A, Monteiro IM. Aberrant responses to TLR agonists in pediatric IBD patients; the possible association with increased production of Th1/Th17 cytokines in response to candida, a luminal antigen. Pediatr Allergy Immunol. 2010;21(4 Pt 2):e747–e755. doi: 10.1111/j.1399-3038.2009.00923.x. [DOI] [PubMed] [Google Scholar]
- 28.Neurath MF. Cytokines in inflammatory bowel disease. Nat Rev Immunol. 2014;14(5):329–342. doi: 10.1038/nri3661. [DOI] [PubMed] [Google Scholar]
- 29.Wehkamp J, et al. The Paneth cell alpha-defensin deficiency of ileal Crohn’s disease is linked to Wnt/Tcf-4. J Immunol. 2007;179(5):3109–3118. doi: 10.4049/jimmunol.179.5.3109. [DOI] [PubMed] [Google Scholar]
- 30.Korinek V, et al. Constitutive transcriptional activation by a beta-catenin-Tcf complex in APC-/- colon carcinoma. Science. 1997;275(5307):1784–1787. doi: 10.1126/science.275.5307.1784. [DOI] [PubMed] [Google Scholar]
- 31.Gustafson B, Smith U. Cytokines promote Wnt signaling and inflammation and impair the normal differentiation and lipid accumulation in 3T3-L1 preadipocytes. J Biol Chem. 2006;281(14):9507–9516. doi: 10.1074/jbc.M512077200. [DOI] [PubMed] [Google Scholar]
- 32.Kaler P, Godasi BN, Augenlicht L, Klampfer L. The NF-κB/AKT-dependent Induction of Wnt Signaling in Colon Cancer Cells by Macrophages and IL-1β. Cancer Microenviron. 2009;2(1):69–80. doi: 10.1007/s12307-009-0030-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwitalla S, et al. Intestinal tumorigenesis initiated by dedifferentiation and acquisition of stem-cell-like properties. Cell. 2013;152(1-2):25–38. doi: 10.1016/j.cell.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 34.Chen M, et al. The anti-helminthic niclosamide inhibits Wnt/Frizzled1 signaling. Biochemistry. 2009;48(43):10267–10274. doi: 10.1021/bi9009677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osada T, et al. Antihelminth compound niclosamide downregulates Wnt signaling and elicits antitumor responses in tumors with activating APC mutations. Cancer Res. 2011;71(12):4172–4182. doi: 10.1158/0008-5472.CAN-10-3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Y, et al. Multi-targeted therapy of cancer by niclosamide: A new application for an old drug. Cancer Lett. 2014;349(1):8–14. doi: 10.1016/j.canlet.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsieh JC, et al. A new secreted protein that binds to Wnt proteins and inhibits their activities. Nature. 1999;398(6726):431–436. doi: 10.1038/18899. [DOI] [PubMed] [Google Scholar]
- 38.Surmann-Schmitt C, et al. Wif-1 is expressed at cartilage-mesenchyme interfaces and impedes Wnt3a-mediated inhibition of chondrogenesis. J Cell Sci. 2009;122(Pt 20):3627–3637. doi: 10.1242/jcs.048926. [DOI] [PubMed] [Google Scholar]
- 39.Simms LA, et al. Reduced alpha-defensin expression is associated with inflammation and not NOD2 mutation status in ileal Crohn’s disease. Gut. 2008;57(7):903–910. doi: 10.1136/gut.2007.142588. [DOI] [PubMed] [Google Scholar]
- 40.Caruso R, Warner N, Inohara N, Núñez G. NOD1 and NOD2: Signaling, host defense, and inflammatory disease. Immunity. 2014;41(6):898–908. doi: 10.1016/j.immuni.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leppkes M, Roulis M, Neurath MF, Kollias G, Becker C. Pleiotropic functions of TNF-α in the regulation of the intestinal epithelial response to inflammation. Int Immunol. 2014;26(9):509–515. doi: 10.1093/intimm/dxu051. [DOI] [PubMed] [Google Scholar]
- 42.Nava P, et al. Interferon-gamma regulates intestinal epithelial homeostasis through converging beta-catenin signaling pathways. Immunity. 2010;32(3):392–402. doi: 10.1016/j.immuni.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Silva-García O, Valdez-Alarcón JJ, Baizabal-Aguirre VM. The Wnt/β-catenin signaling pathway controls the inflammatory response in infections caused by pathogenic bacteria. Mediators Inflamm. 2014;2014:310183. doi: 10.1155/2014/310183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Günther C, et al. Caspase-8 regulates TNF-α-induced epithelial necroptosis and terminal ileitis. Nature. 2011;477(7364):335–339. doi: 10.1038/nature10400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cosín-Roger J, et al. M2 macrophages activate WNT signaling pathway in epithelial cells: Relevance in ulcerative colitis. PLoS One. 2013;8(10):e78128. doi: 10.1371/journal.pone.0078128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pereira CP, Bachli EB, Schoedon G. The wnt pathway: A macrophage effector molecule that triggers inflammation. Curr Atheroscler Rep. 2009;11(3):236–242. doi: 10.1007/s11883-009-0036-4. [DOI] [PubMed] [Google Scholar]
- 47.Smith K, et al. Up-regulation of macrophage wnt gene expression in adenoma-carcinoma progression of human colorectal cancer. Br J Cancer. 1999;81(3):496–502. doi: 10.1038/sj.bjc.6690721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farin HF, Van Es JH, Clevers H. Redundant sources of Wnt regulate intestinal stem cells and promote formation of Paneth cells. Gastroenterology. 2012;143(6):1518–1529.e7. doi: 10.1053/j.gastro.2012.08.031. [DOI] [PubMed] [Google Scholar]
- 49.Gregorieff A, et al. Expression pattern of Wnt signaling components in the adult intestine. Gastroenterology. 2005;129(2):626–638. doi: 10.1016/j.gastro.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 50.San Roman AK, Jayewickreme CD, Murtaugh LC, Shivdasani RA. Wnt secretion from epithelial cells and subepithelial myofibroblasts is not required in the mouse intestinal stem cell niche in vivo. Stem Cell Rep. 2014;2(2):127–134. doi: 10.1016/j.stemcr.2013.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wahl LM, Wahl SM, Smythies LE, Smith PD. Isolation of human monocyte populations. Curr Protoc Immunol. 2006 doi: 10.1002/0471142735.im0706as70. Chapter 7:Unit 6A. [DOI] [PubMed] [Google Scholar]
- 52.Fishbein T, et al. NOD2-expressing bone marrow-derived cells appear to regulate epithelial innate immunity of the transplanted human small intestine. Gut. 2008;57(3):323–330. doi: 10.1136/gut.2007.133322. [DOI] [PubMed] [Google Scholar]
- 53.Lough D, et al. Abnormal CX3CR1+ lamina propria myeloid cells from intestinal transplant recipients with NOD2 mutations. Am J Transplant. 2012;12(4):992–1003. doi: 10.1111/j.1600-6143.2011.03897.x. [DOI] [PubMed] [Google Scholar]
- 54.Sainathan SK, et al. Granulocyte macrophage colony-stimulating factor ameliorates DSS-induced experimental colitis. Inflamm Bowel Dis. 2008;14(1):88–99. doi: 10.1002/ibd.20279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Korzenik JR, Dieckgraefe BK, Valentine JF, Hausman DF, Gilbert MJ. Sargramostim in Crohn’s Disease Study Group Sargramostim for active Crohn’s disease. N Engl J Med. 2005;352(21):2193–2201. doi: 10.1056/NEJMoa041109. [DOI] [PubMed] [Google Scholar]
- 56.Roth L, MacDonald JK, McDonald JWD, Chande N. Sargramostim (GM-CSF) for induction of remission in Crohn’s disease: A cochrane inflammatory bowel disease and functional bowel disorders systematic review of randomized trials. Inflamm Bowel Dis. 2012;18(7):1333–1339. doi: 10.1002/ibd.22973. [DOI] [PubMed] [Google Scholar]
- 57.Burt RK, et al. Autologous nonmyeloablative hematopoietic stem cell transplantation in patients with severe anti-TNF refractory Crohn disease: Long-term follow-up. Blood. 2010;116(26):6123–6132. doi: 10.1182/blood-2010-06-292391. [DOI] [PubMed] [Google Scholar]