Abstract
Introduction
With the development and improvement of laparoscopic surgery, procedures have become common. However, post-operative complications occur when patients are released from hospital. These complications increase patients’ morbidity and mortality. They also lead to re-hospitalization, an extended recovery period, and an increase in the cost of treatment.
Aim
To evaluate and determine the prognostic properties of C-reactive protein in the early diagnosis of postoperative complications after a laparoscopic colon resection.
Material and methods
The prospective study included patients who underwent laparoscopic colorectal surgery in 2010–2014. The patients were divided into two groups – uncomplicated ones and those with complications. C-reactive protein concentrations in their blood serum were measured on the 2nd, 4th and 6th day after surgery. Logistic regression analysis was used to evaluate the relation between C-reactive protein values measured on the 2nd, 4th and 6th postoperative day and related complications. Receiver operating characteristic curves were used to determine the sensitivity and specificity of each C-reactive protein value measured on the 2nd, 4th and 6th postoperative day.
Results
One hundred and six patients were included in the trial; 14 of them had complications. On the second day, a C-reactive protein cut-off value of 88.6 mmol/l provided the highest sensitivity and specificity for predicting evolving complications, being 71.4% and 84.8% respectively (p = 0.003). The significant predictive cut-off value decreases and becomes more sensitive and specific each post-operative day.
Conclusions
It is possible to detect developing post-operative complications early on by monitoring C-reactive protein concentration levels in the blood serum on the 2nd, 4th, and 6th post-operative days.
Keywords: C-reactive protein, colorectal, laparoscopic
Introduction
With the development and improvement of laparoscopic surgery, procedures have become common. However, post-operative complications occur when patients are released from hospital. These complications increase patients’ morbidity and mortality; they also lead to re-hospitalization, an extended recovery period, and an increase in the cost of treatment [1–4]. Research which was carried out shows the direct benefits of laparoscopic colorectal surgery compared to open colorectal surgery [5–8]. Complications develop immediately after laparoscopic surgery or within a certain period of time. Thus, these complications can be unnoticed and not diagnosed in time. Both open and laparoscopic colorectal resection surgery causes trauma to the body, provoking an immune response. However, the bodily response is weaker during laparoscopic surgery, and it allows for the identification of complications induced by changes in the immune system, which can go unnoticed during open surgery due to the active immune response [9–11]. Serum markers are sufficiently sensitive and allow for prediction of early developing complications. During surgery, when tissues are damaged, certain cytokines are released: tumor necrosis factor α (TNF-α), interleukin 6 (IL-6), IL-1β. The release of cytokines correlates with the extent of surgery [12–14]. The above-mentioned cytokines promote C-reactive protein (CRP) synthesis in the liver. Because of its short half-life, this protein is useful as a diagnostic indicator, predicting activity of diseases, the inflammatory response, and the post-operative course. In addition, the detection of this protein is inexpensive and readily available [15, 16]. C-reactive protein is considered to be an indicator of adverse post-operative course, which includes both surgical and non-surgical complications [17]. The aim of this research is to evaluate the sensitivity and specificity of CRP as well as its predictive properties in early diagnosis of developing complications after laparoscopic colorectal surgery. Timely diagnosis of these complications and early treatment will help to avoid life-threatening situations.
Aim
The aim of the study was to evaluate and determine the prognostic properties of CRP in the early diagnosis of postoperative complications after a laparoscopic colon resection.
Material and methods
One hundred and six patients who underwent an elective laparoscopic colorectal resection between 2010 and 2014 at Vilnius University Hospital Santariskiu Clinics 1st Abdominal Surgery Department were the subjects of the research. Complications were diagnosed by daily examination of patients during the post-operative period, and were graded according to the Clavien-Dindo surgical complication classification. We graded the following complications: infection, fistula/leakage, bleeding/haematoma, impaired gastrointestinal motility/nausea/vomiting, cardiopulmonary, liver failure, neurological, pain, allergy, pancreatitis and other complications. According to the complications mentioned above, all patients were divided into two groups: uncomplicated and with complications. C-reactive protein concentrations were measured by using an automated analytic system with a reference range of < 5 mmol/l. C-reactive protein reaction concentrations in the blood serum were measured on the 2nd, 4th and 6th postoperative days. We also analysed demographics, operative data, and diagnoses.
Statistical analysis
Statistical analysis was carried out using IBM SPSS Statistics 21 software. Categorical data were reported as a number (percentage) of patients. To define the distribution, continuous variables were explored for skewness and kurtosis. Normally distributed continuous variables were reported as the mean with a standard deviation and non-normally distributed continuous variables were reported as the median with a range of minimum and maximum values. Logistic regression analysis was used to evaluate the relation between CRP values measured on the 2nd, 4th and 6th day after the resection and the presence of post-operative complications. Odds ratios and confidence intervals were determined. Receiver operating characteristic curves were used to determine sensitivity and specificity of each CRP value measured on the 2nd, 4th and 6th postoperative day. Cut-off values with the highest sensitivity and specificity were determined for each day by using the Youden index. The level of statistical significance was defined by p ≤ 0.05.
Results
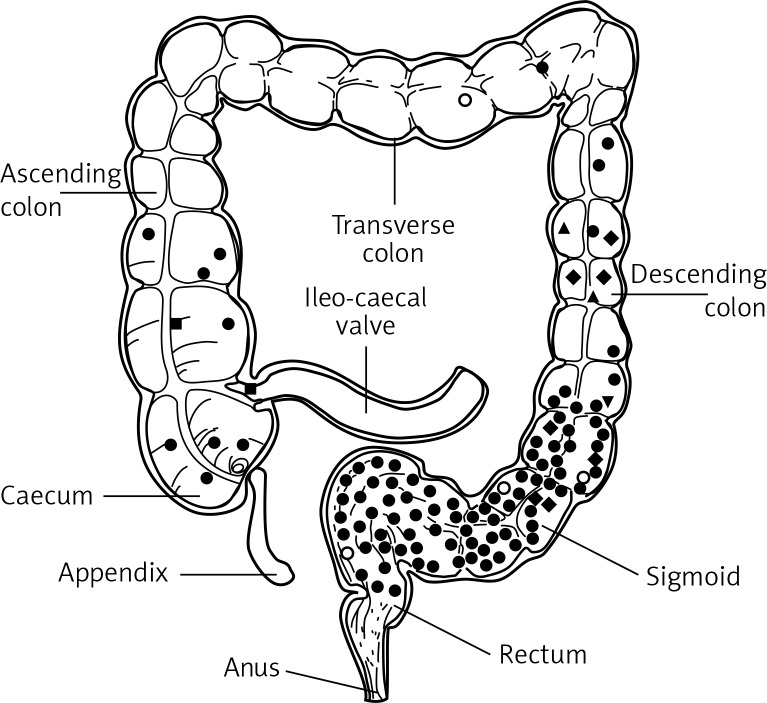
The study included 106 patients who underwent laparoscopic colorectal resection. Complications developed in 14 (13.2%) patients. The remaining 92 patients did not develop any complications (86.8%). The average age in the group without complications (64.9 ±11.6) was slightly higher than in the group with complications (60.2 ±10.4) (Table I). 64.2% of subjects were women, while 35.8% were men. The main reasons for resection were adenocarcinoma (85.8%), diverticulosis (5.7%), and adenoma (3.8%). According to the location it was a disease of the sigma (48.1%), rectum (35.8%), and ascending colon (5.7%) (Figure 1). The most common complications were 6 surgical site infections (5.7%) and 4 anastomotic leakages (3.8%).
Table I.
Demographics, operative data
| Parameter | Total | Uncomplicated | Complications |
|---|---|---|---|
| N | 106 | 92 | 14 |
| Age [years] | 64.3 ±11.5 | 64.9 ±11.6 | 60.2 ±10.4 |
| Male: female | 38: 68 | 31: 61 | 7: 7 |
| Length of stay [days] | 9 (5–34) | 8 (5–17) | 15.5 (10–34) |
| Operation time [min] | 160 (100–380) | 171.3 ±43.6* | 155 (100–380) |
| Estimated blood loss [ml] | 50 (0–500) | 50 (0–500) | 75 (10–300) |
| Resection length [cm] | 30 (12–80) | 30 (12–80) | 30 (20–70) |
All data are presented as n, except for length of stay, operation time, estimated blood loss and operation time, which is presented as median with range. Age is presented as mean with standard deviation.
Operation time for uncomplicated group is presented as mean with standard deviation.
Figure 1.
Location map of the colon disease
Full circle – adenocarcinoma; empty circle – adenoma; lozenge – diverticulosis; square – neuroendocrine tumour; pyramid – obstipation; inverted pyramid – endometriosis.
A statistically significant difference of CRP levels between the uncomplicated group and the group with complications was identified during all days of analysis. The biggest difference was on the 4th post-operative day (44.3 ±36.4 vs. 147.6 ±91.3; p < 0.001). C-reactive protein levels become significant in predicting complications from the second post-operative day (OR = 1.007; 95% CI: 0.979–1.036; p < 0.001) (Table II). On the second day, a CRP cut-off value of 88.6 mmol/l provided the highest sensitivity and specificity for predicting evolving complications, being 71.4% and 84.8% respectively (p = 0.003). The significant predictive cut-off value decreases and becomes more sensitive and specific during each post-operative day (Table III).
Table II.
Predicting complications by routinely measuring CRP level
| POD | CRP [mmol/l] | ||
|---|---|---|---|
| Odds ratio | 95% Confidence interval | Value of p* | |
| 2 | 1.007 | 0.979–1.036 | < 0.001 |
| 4 | 0.982 | 0.953–1.011 | < 0.001 |
| 6 | 1.071 | 1.021–1.123 | < 0.001 |
POD – Postoperative day, CRP – C-reactive protein
p – values are based on logistic regression analysis.
Table III.
Sensitivity and specificity of significant CRP cut-off values for identifying complications after elective laparoscopic colorectal surgery
| POD | Cut-off | Sensitivity (%) | Specificity (%) | J | AUC | Value of p |
|---|---|---|---|---|---|---|
| 2 | 88.6 | 71.4 | 84.8 | 0.562 | 0.745 | 0.003 |
| 4 | 66.2 | 78.6 | 78.3 | 0.569 | 0.846 | < 0.001 |
| 6 | 59.9 | 85.7 | 95.7 | 0.814 | 0.918 | < 0.001 |
POD – Postoperative day, CRP – C-reactive protein, J – Youden index, AUC – area under the curve.
Discussion
The research that was undertaken and the collected data prove that long-term results after laparoscopic colorectal resection are the same as those after an open colorectal resection. However, having assessed short-term results, it has been noted that results are better after laparoscopic colorectal surgery than after open surgery [18, 19]. With the development of laparoscopic surgery, the recovery of patients has accelerated and the duration of hospitalization has decreased. However, when discharging patients earlier, developing complications may go unnoticed. It is the main task to diagnose the complications which are mentioned above early so as to reduce their consequences, but in everyday practice the diagnosis is often delayed. It is particularly important to detect a developing anastomotic leakage in time. This is a serious complication, which must be diagnosed as soon as possible in order to avoid its associated morbidity and mortality [20, 21]. A rapid and reliable diagnostic method is needed, which allows the early detection of developing complications, so that patients can be safely discharged from hospital and prevented from having the complications mentioned above.
Serum markers can provide information about the developing inflammatory processes in the body. C-reactive protein was examined as a potential indicator of developing septic complications after open colorectal surgery [17, 22–25]. According to the study of Buunen et al., CRP levels > 145 mg/l on the 4th postoperative day after rectum or colon surgery have the highest specificity and sensitivity for developing septic complications [17]. Based on the study by Korner et al. [23], CRP levels with the highest sensitivity and specificity are claimed to be on the third post-operative day when the concentration of the protein was > 190 mg/l. According to the study by Ortega-Deballon et al. [26], patients with CRP levels on the third postoperative day > 125 mg/l should not be released from hospital. The sensitivity of CRP on the third post-operative day was 81.2% and the negative prognostic value was 95.8%. The above-mentioned studies evaluated CRP concentrations only in open colorectal resection surgery. A study published in 2014, which was carried out by Adamina et al. [27], analysed patients after laparoscopic colorectal surgery. It proved that the mean value of CRP with the highest sensitivity and specificity for development of infectious complications was 56 mg/l on the 6th post-operative day. The sensitivity was 100% (95% CI: 0.8–1), specificity was 46% (95% CI: 0.4–0.6), and diagnostic accuracy was 78% (95% CI: 0.7–0.9). We can compare the above-mentioned study to this study, because it also included patients only after elective laparoscopic colorectal surgery.
C-reactive protein belongs to the group of acute phase proteins, which are synthesized in the liver. The production of this protein is provoked by cytokines. It is important to mention that levels of CRP in the serum begin to rise 4–12 h after the beginning of pathophysiological processes in the body. In order to use CRP to identify developing septic complications, we need to determine the diagnostic value of this protein in the blood serum. In the above-mentioned articles, the protein values range from 56 to 190 mg/l. In the current study, the obtained CRP values are much lower, because it only included laparoscopic colorectal resection surgery. On the 2nd post-operative day, a CRP value of 88.6 mg/l had the highest sensitivity (71.4%) and specificity (84.8%). On the fourth post-operative day the protein value of 66.2 mg/l had the highest sensitivity (78.6%) and specificity (78.3%). On the sixth post-operative day, the CRP value of 59.9 mg/l had a 85.7% sensitivity and 95.7% specificity. Thus, with each day we can predict more accurately whether the complications are developing. However, a presumption about the developing complications cannot be based only on the concentration of CRP. The protein concentration may increase in response to the mechanical tissue damage. Its levels also rise with other various diseases (oncology, connective tissue diseases, rheumatism, tuberculosis, pathological obesity) [17, 18]. Increased levels of protein after laparoscopic colorectal resection surgery will indicate the need to conduct a more detailed follow-up examination of the patient (ultrasound, endoscopy, MRI and others). Then, it will help to avoid the potential negative consequences of post-operative complications.
Conclusions
Developing post-operative complications can be detected early on by monitoring CRP concentration levels in the blood serum on the 2nd, 4th, and 6th post-operative days, which is very important for safe and early discharge after laparoscopic colorectal surgery.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Alves A, Panis Y, Mathieu P, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery. Arch Surg. 2005;140:278–83. doi: 10.1001/archsurg.140.3.278. [DOI] [PubMed] [Google Scholar]
- 2.Branagan G, Finnis D. Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum. 2005;48:1021–6. doi: 10.1007/s10350-004-0869-4. [DOI] [PubMed] [Google Scholar]
- 3.Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004;91:1111–24. doi: 10.1002/bjs.4640. [DOI] [PubMed] [Google Scholar]
- 4.Liang JT, Shieh MJ, Chen CN, et al. Prospective evaluation of laparoscopy-assisted colectomy versus laparotomy with resection for management of complex polyps of the sigmoid colon. World J Surg. 2002;26:377–83. doi: 10.1007/s00268-001-0235-9. [DOI] [PubMed] [Google Scholar]
- 5.Monson JR, Darzi A, Carey PD, et al. Prospective evaluation of laparoscopic-assisted colectomy in an unselected group of patiens. Lancet. 1992;340:831–3. doi: 10.1016/0140-6736(92)92694-b. [DOI] [PubMed] [Google Scholar]
- 6.Zucker KA, Pitcher DE, Martin DT, et al. Laparoscopic-assisted colon resection. Surg Endosc. 1994;8:12–7. doi: 10.1007/BF02909486. [DOI] [PubMed] [Google Scholar]
- 7.Braga M, Vignali A, Gianotti L, et al. Laparoscopic versus open colorectal surgery a randomized trial on short-term outcome. Ann Surg. 2002;236:759–67. doi: 10.1097/01.SLA.0000036269.60340.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lacy AM, García-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–9. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 9.Vittimberga FJ, Foley DP, Meyers WC, et al. Laparoscopic surgery and the systemic immune response. Ann Surg. 1998;227:326–34. doi: 10.1097/00000658-199803000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ordemann J, Jacobi CA, Schwenk W, et al. Cellular and humoral inflammatory response after laparoscopic and conventional colorectal resections. Surg Endosc. 2001;15:600–8. doi: 10.1007/s004640090032. [DOI] [PubMed] [Google Scholar]
- 11.Whelan RL, Franklin , Holubar M, et al. Postoperative cell mediated immune response is better preserved after laparoscopic vs open colorectal resection in humans. Surg Endosc. 2003;17:972–8. doi: 10.1007/s00464-001-8263-y. [DOI] [PubMed] [Google Scholar]
- 12.Cruickshank AM, Fraser WD, Burns HJ, et al. Response of serum interleukin-6 in patients undergoing elective surgery of varying severity. Clin Sci (Lond) 1990;79:161–5. doi: 10.1042/cs0790161. [DOI] [PubMed] [Google Scholar]
- 13.Kragsbjerg P, Holmberg H, Vikerfors T. Serum concentrations of interleukin-6, tumor necrosis factor-alpha and C-reactive protein in patients undergoing major operations. Eur J Surg. 1995;161:17–22. [PubMed] [Google Scholar]
- 14.Robert A, Mustard J, John M, et al. C-reactive protein levels predict postoperative septic complications. Arch Surg. 1987;122:69–73. doi: 10.1001/archsurg.1987.01400130075011. [DOI] [PubMed] [Google Scholar]
- 15.Hart WR, Deodhar SD. C-reactive protein: the best laboratory indicator available for monitoring disease activity. Cleve Clin J Med. 1989;56:126–30. doi: 10.3949/ccjm.56.2.126. [DOI] [PubMed] [Google Scholar]
- 16.Welsch T, Müller SA, Ulrich A, et al. C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int J Colorectal Dis. 2007;22:1499–507. doi: 10.1007/s00384-007-0354-3. [DOI] [PubMed] [Google Scholar]
- 17.Buunen M, Veldkamp R, Kuhry E, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44–52. doi: 10.1016/S1470-2045(08)70310-3. [DOI] [PubMed] [Google Scholar]
- 18.Guillou PJ, Quirke P, Thorpe H, et al. Short-term of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–26. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 19.Dulk M, Noter SL, Hendriks ER, et al. Improved diagnosis and treatment of anastomotic leakage after colorectal surgery. Eur J Surg Oncol. 2009;35:420–6. doi: 10.1016/j.ejso.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Nesbakken A, Nygaard K, Lunde OC. Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer. Br J Surg. 2001;88:400–4. doi: 10.1046/j.1365-2168.2001.01719.x. [DOI] [PubMed] [Google Scholar]
- 21.MacKay GJ, Molloy RG, O'Dwyer PJ. C-reactive protein as a predictor of postoperative infective complications following elective colorectal resection. Colorectal Dis. 2011;13:583–7. doi: 10.1111/j.1463-1318.2010.02236.x. [DOI] [PubMed] [Google Scholar]
- 22.Platt JJ, Ramanathan ML, Crosbie RA, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19:4168–77. doi: 10.1245/s10434-012-2498-9. [DOI] [PubMed] [Google Scholar]
- 23.Korner H, Nielsen HJ, Soreide JA, et al. Diagnostic accuracy of C-reactive protein for intraabdominal infections after colorectal resections. J Gastrointest Surg. 2009;13:1599–606. doi: 10.1007/s11605-009-0928-1. [DOI] [PubMed] [Google Scholar]
- 24.Schwenk W, Jacobi C, Mansmann U, et al. Inflammatory response after laparoscopic and conventional colorectal resections – results of a prospective randomized trial. Langenbecks Arch Surg. 2000;385:2–9. doi: 10.1007/s004230050002. [DOI] [PubMed] [Google Scholar]
- 25.Mickevicius A, Sufi P, Heath D. Factors predicting the occurence of a gastrojejunal anastomosis leak following gastric bypass. Videosurgery Miniinv. 2014;9:436–440. doi: 10.5114/wiitm.2014.44142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ortega-Deballon P, Radais F, Facy O, et al. C-reactive protein is an early predictor of septic complications after elective colorectal surgery. World J Surg. 2010;34:808–14. doi: 10.1007/s00268-009-0367-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adamina M, Warschkow R, Naf F, et al. Monitoring C-reactive protein after laparoscopic colorectal surgery excludes infectious complications and allows for safe and early discharge. Surg Endosc. 2014;28:2939–48. doi: 10.1007/s00464-014-3556-0. [DOI] [PubMed] [Google Scholar]