Abstract
Background and Objectives:
Cholecystectomy performed during bariatric surgery is technically demanding. Herein is described a technique we term the Glissonian approach along with an evaluation of its effectiveness and safety.
Methods:
From April 1, 2009, through February 28, 2014, laparoscopic cholecystectomy was performed during laparoscopic Roux-en-Y gastric bypass (LRYGB) or laparoscopic sleeve gastrectomy (LSG) in 38 patients with proven cholecystopathy on diagnostic imaging. Perioperative outcomes were compared between the patients operated on with the Glissonian approach and those who underwent conventional laparoscopic cholecystectomy.
Results:
The Glissonian approach was adopted in 13 patients—11 during LRYGB and 2 during LSG—and the conventional operation was performed on 16 patients during LRYGB and 9 during LSG. Mean body mass indexes were 40.1 kg/m2 in the Glissonian-approach group and 37.6 kg/m2 in the conventional group. Laparoscopic cholecystectomy by the Glissonian approach saved a mean operative time of 7 minutes compared with the operative time of the conventional operation. No surgical complications related to cholecystectomy were noted in either group.
Conclusion:
This simple technique can be performed safely in morbidly obese patients, with low resultant morbidity and acceptable operation times.
Keywords: Cholecystectomy, Glissonian approach, Morbid obesity
INTRODUCTION
The prevalence of morbid obesity treated by bariatric surgery is increasing rapidly.1 Gallbladder disease is one of the most common comorbidities related to obesity, and obesity increases the prevalence of gallbladder disease, especially gallstones.2,3 Whether to perform prophylactic cholecystectomy during bariatric surgery is a subject of debate among bariatric surgeons.4 Three different approaches have been proposed: prophylactic cholecystectomy in all patients who receive gastric bypass5–7; a selective approach, in which cholecystectomy is performed only when gallstones are present8–10; and no screening—instead, cholecystectomy is delayed and performed only when symptoms develop.11–14
In theory, prophylactic cholecystectomy abolishes the risk of gallbladder disease and its related complications, as well as the risks associated with further surgery; it also avoids the danger presented by common bile duct stones, which can be particularly challenging to treat after a Roux-en-Y bypass. However, opponents argue that, despite the increased prevalence of gallstones after weight loss surgery, rates of cholecystectomy remain under 15% in most large studies.15–17 Furthermore, as laparoscopic bariatric surgery has gained popularity, the need for intraoperative cholecystectomy has been questioned because postoperative adhesions are expected to be minimal after laparoscopic surgery, so that subsequent cholecystectomy is much less difficult than cholecystectomy after open bariatric surgical procedures. Those with the opposing view argue that selective cholecystectomy for ultrasonography-diagnosed gallbladder disease can be performed safely and efficiently during bariatric surgery6,9,10 and that the duration of the hospital stay is not affected in laparoscopic cases.18
As investigators have argued in the past, performing a cholecystectomy during bariatric surgery is technically demanding.8,14 Therefore, we developed a procedure for simultaneous cholecystectomy and named it the Glissonian approach. This study was designed to evaluate the effectiveness and safety of this technique in morbidly obese patients with proven gallbladder disease.
METHODS
Patients
A database of patients who had undergone bariatric surgery was reviewed retrospectively. Thirty-eight patients who underwent simultaneous cholecystectomy during laparoscopic Roux-en-Y gastric bypass (LRYGB) or laparoscopic sleeve gastrectomy (LSG) at Soonchunhyang University Seoul Hospital from April 1, 2009, through August 31, 2013, and at Hanyang University Hospital from September 1, 2013, through February 28, 2014, were enrolled. All patients were evaluated before surgery by abdominal ultrasonography or computed tomography, and simultaneous cholecystectomy was planned in patients with proven gallbladder disease, such as gallstones or polyps. The clinical and surgical outcomes of the patients treated with the Glissonian approach were assessed and compared with those of patients who underwent conventional cholecystectomy with clips.
Surgical Techniques
A standard LRYGB, indicated by body mass index (BMI), was performed with a 50-cm biliopancreatic and 100-cm antecolic antegastric alimentary limb, or the patient underwent a standard LSG. Six trocars were used, and, when necessary, an additional 5-mm trocar was inserted into the right subcostal area, to proceed with conventional cholecystectomy. In contrast, no additional trocar was needed during the Glissonian approach. For conventional cholecystectomy, once the critical view of safety was convincingly achieved, the cystic duct and the artery were separately ligated with medium-sized clips, using a 5-mm clip applier inserted through the right-hand working port located in the epigastrium, before dividing them between the clips, and then the gallbladder was dissected completely from its fossa. In the Glissonian approach, the gallbladder was first dissected from its fossa, and then the cystic duct and the artery were ligated together with an endoloop (Ethicon Endosurgery, Cincinnati, Ohio) without separation (Figure 1). A drain was routinely inserted in the right subhepatic space, regardless of whether a cholecystectomy was performed.
Figure 1.
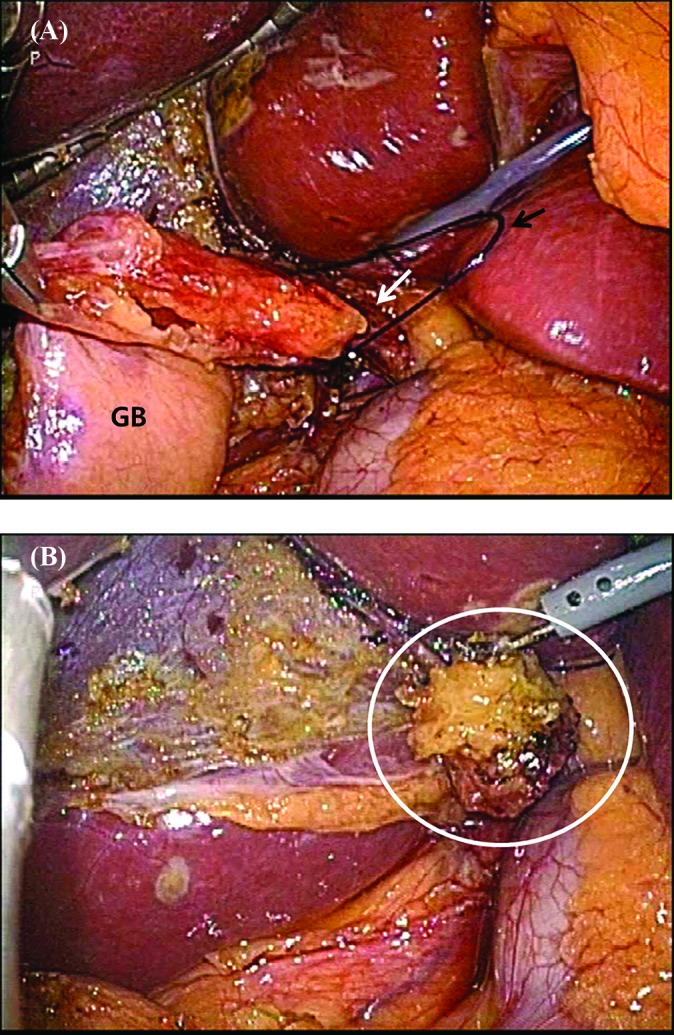
(A) Before pedicle ligation. Simultaneous ligation of the pedicle composed of the cystic duct and artery (white arrow) with an endoloop (black arrow). GB, gallbladder. (B) After transection of pedicle. White circle: transected pedicle.
Statistical Analysis
Statistical analysis was performed with SPSS version 18.0 (IBM Inc., Armonk, New York). Continuous data are reported as the mean ± SD. The χ2 test, Fisher's exact test, and independent Student's t test were used for comparisons between groups. P < .05 was considered statistically significant.
RESULTS
Demographics
Of 575 patients who underwent primary laparoscopic bariatric surgery (226 LSG and 349 LRYGB), simultaneous laparoscopic cholecystectomy was performed in 38 (6.6%) (Table 1). None of the patients had a history of gallbladder-related symptoms. The Glissonian approach was performed in 13 patients (11 during LRYGB and 2 during LSG) and the conventional procedure in 25 patients (16 during LRYGB and 9 during LSG). The patients who underwent the Glissonian approach included 1 man and 12 women, with a mean age of 39.8 ± 13.8 years (range, 19–59) and a mean BMI of 40.1 ± 6.6 kg/m2 (range, 32.7–56.5). The patients who underwent conventional cholecystectomy included 1 man and 24 women, with a mean age of 41.0 ± 10.2 years (range, 25–60) and a mean BMI of 37.6 ± 5.2 kg/m2 (range, 30.8–51.6). Of the 13 patients who underwent the Glissonian approach, 4 (30.8%) had 1 or more comorbidities, whereas in the conventional-approach group, 15 (60.0%) had 1 or more. There was a significant difference between the 2 study groups with respect to ASA score (P = .029), but the surgical risks of all patients were confined to ASA scores of 1 or 2. Simultaneous cholecystectomy was conducted in most of the patients because of gallstones, with or without chronic inflammation. Only one patient in each group underwent simultaneous cholecystectomy because of gallbladder polyps.
Table 1.
Demographics
| Characteristics | Conventional Clipping (n = 25) |
Glissonian Approach (n = 13) |
P |
|---|---|---|---|
| n (%) | n (%) | ||
| Age (years ± SD)a | 41 ± 10.2 | 39.8 ± 13.8 | 0.757 |
| Gender ratio (male/female) | 1:24 | 1:12 | 1.000* |
| Type of operation | 0.268* | ||
| LSG | 9 (36.0) | 2 (15.4) | |
| LRYGB | 16 (64.0) | 11 (84.6) | |
| BMI (kg/m2)a | 37.6 ± 5.2 | 40.1 ± 6.6 | 0.22 |
| ASA score | 0.029 | ||
| 1 | 8 (32.0) | 9 (69.2) | |
| 2 | 17 (68.0) | 4 (30.8) | |
| Comorbidities | 15 (60.0) | 4 (30.8) | 0.17 |
| Hypertension | 7 (28.0) | 2 (15.4) | 0.456* |
| Diabetic mellitus | 7 (28.0) | 2 (15.4) | 0.456* |
| Hyperlipidemia | 5 (20.0) | 0 (0) | 0.144* |
| Sleep apnea | 2 (8.0) | 4 (30.8) | 0.154* |
| Pathological diagnosis | 0.212* | ||
| Acute calculous cholecystitis | 0 (0) | 0 (0) | |
| Chronic calculous cholecystitis | 19 (76.0) | 12 (92.3) | |
| GB stone | 5 (20.0) | 0 (0) | |
| GB polyp | 1 (4.0) | 1 (7.7) |
Data are expressed as n (%), unless otherwise specified. GB, gallbladder.
Mean ± SD.
Pearson's χ2 test.
Surgical Outcomes
No significant differences were observed in operation time, amount of blood loss, and hospital stay between the 2 groups (Table 2). However, operating time in the conventional-approach group was slightly longer than in the Glissonian-approach group (154.8 ± 35.5 minutes [range, 90–220] vs 148.1 ± 36.9 minutes [range, 105–210]; P = .588). Operative time was also longer in the conventional-approach group than in the Glissonian-approach group when the comparison was performed according to type of bariatric surgery, although the effect was not statistically significant (LRYGB: 165.0 ± 36.1 minutes vs 153.2 ± 37.4 minutes, P = .418; LSG: 136.7 ± 27.6 minutes vs 120.0 ± 21.2 minutes, P = .450). There were no intraoperative deaths with either approach. In the conventional-clipping group, 2 patients had complications caused by postoperative bleeding, and 1 underwent operative bleeding control. In the Glissonian-approach group, 1 patient experienced postoperative bleeding that was controlled by conservative management with transfusion. No surgical complication related to the cholecystectomy occurred in either group, and preoperative and postoperative bilirubin and liver enzymes did not differ between the groups.
Table 2.
Perioperative Outcomes
| Parameter | Conventional Clipping |
Glissonian Approach |
P |
|---|---|---|---|
| (n = 25) | (n = 13) | ||
| Operative time (min ± SD) | 154.8 ± 35.5 | 148.1 ± 36.9 | 0.588 |
| LRYGB | 165.0 ± 36.1 | 153.2 ± 37.4 | 0.418 |
| LSG | 136.7 ± 27.6 | 120.0 ± 21.2 | 0.450 |
| Operative blood loss (mL) | 155.6 ±133.6 | 119.2 ± 48.0 | 0.351 |
| Hospital stay (days) | 2.8 ± 3.3 | 2.9 ± 1.7 | 0.933 |
| Morbidity, n (%) | 0.372* | ||
| No | 23 (92.0) | 11 (92.3) | |
| Postoperative bleeding | 2 (8.0) | 1 (7.7) | |
| Reoperation, n (%) | 1 (4.0) | 0 (0.0) | 1.000* |
| Mortality | 0 | 0 | 1.000* |
| Preoperative LFT | |||
| Total bilirubin (mg/dL) | 0.5 ± 0.1 | 0.5 ± 0.2 | 0.227 |
| AST (U/L) | 32.4 ± 24.9 | 28.6 ± 11.0 | 0.7 |
| ALT (U/L) | 40.2 ± 33.2 | 41.7 ± 33.7 | 0.894 |
| Postoperative LFT | |||
| Total bilirubin (mg/dL) | 0.9 ± 0.2 | 0.7 ± 0.1 | 0.196 |
| AST (U/L) | 55.6 ± 33.1 | 57.4 ± 53.9 | 0.9 |
| ALT (U/L) | 57.9 ± 35.7 | 65.1 ± 45.7 | 0.599 |
Data are expressed as the mean ± SD, unless otherwise specified. LFT, liver function test.
Pearson's χ2 test.
DISCUSSION
The best management option for the gallbladder during bariatric surgery is still a matter of debate. Opponents of concomitant cholecystectomy claim that it is associated with prolonged hospital stay, longer operation time, and higher complication rates.8,11–14 Therefore, we developed a technique called the Glissonian approach to simplify the simultaneous cholecystectomy procedure. This method consists of separating the gallbladder from its fossa and simultaneously ligating the cystic duct and artery with an endoloop. The procedure was straightforward, even in obese patients, and saved operation time compared with the conventional-clipping procedure. In addition, our technique was safe, with no conversions and a low complication rate without significant differences from conventional cholecystectomy.
In the past decade, there has been a shift away from routine prophylactic cholecystectomy. Worni et al14 reported a markedly decreased rate of simultaneous cholecystectomy (from 26.3% in 2001 to 3.7% in 2008). The decrease was most likely caused by the growing evidence that cholecystectomy after LRYGB could be performed with a minimally invasive approach with fewer complications. Actually, Warschkow et al12 in a recent meta-analysis, showed that the surgical complication rate related to subsequent cholecystectomy was as low as 1.8%, and they therefore suggested that prophylactic cholecystectomy during LRYGB should not be performed in patients with no evidence of gallstones. However, the question that remains to be answered is how to proceed with patients with asymptomatic cholelithiasis. Some authors favor, as we do, selective cholecystectomy after preoperative confirmation of gallstones.9,10 Thus, Tucker et al9 reported that about 20% of patients with gallstones and 30% of those with sludge underwent cholecystectomy when they had not undergone selective cholecystectomy during LRYGB, and more than half of those showed complicated disease or had a bile duct stone requiring additional procedures. However, the available evidence is not sufficient to answer the question. Further studies should evaluate how to treat patients with asymptomatic cholelithiasis.
The critical-view cholecystectomy technique was first described in 1995 by Strasberg et al19 and is considered the standard procedure for laparoscopic cholecystectomy. Its safety has been validated by many investigators.20–22 There are 3 requirements for the procedure. First, the tissue surrounding Calot's triangle must be completely removed. Second, the nonperitonealized lowest part of the gallbladder must be separated from the liver bed. Third, the cystic duct and artery connecting with the gallbladder must be identified. The procedure can fail in difficult cases, such as those involving patients with severe inflammation, or obese patients in whom exposure and dissection of Calot's triangle are difficult. Some surgeons have recommended fundus-first cholecystectomy as another way to prevent bile duct injuries. This procedure is mainly used in open surgery.23–25 Our Glissonian approach may be considered a modified version of fundus-first cholecystectomy, as performed by hepatic surgeons in open and laparoscopic anatomic hepatic resection.26–28 After the gallbladder was dissected from its fossa, the pedicle, including the cystic duct and artery enveloped by the Glissonian sheath, were ligated with an endoloop without further dissection, similar to the Glissonian pedicle approach used for anatomic partial hepatectomy. We performed this technique safely and easily in obese patients during bariatric surgery, with a low risk of postoperative complications. In addition, we completed all procedures without the use of additional ports.
Our study has some limitations. First, the patient sample was too small to draw significant conclusions. Second, we were unable to analyze the operative time for the cholecystectomy alone, because it had not been recorded separately from the time for the LRYGB or LSG.
In conclusion, our technique for simultaneous selective cholecystectomy during LRYGB or LSG was comparable to conventional cholecystectomy in postoperative outcomes. In addition, the increase in operative time was less than in conventional cholecystectomy with clips. The procedure may be applied safely to difficult cases, although the conventional critical-view cholecystectomy is the standard. A prospective study is needed to establish whether this method can be applied universally.
Contributor Information
Ju-Hee Lee, Department of Surgery, Hanyang University College of Medicine, Seoul, Korea.
Guru Han, Department of Surgery, Soonchunhyang University College of Medicine, Seoul, Korea.
Yong Jin Kim, Department of Surgery, Soonchunhyang University College of Medicine, Seoul, Korea.
Min-Sung Jung, Department of Surgery, Hanyang University College of Medicine, Seoul, Korea.
Dongho Choi, Department of Surgery, Hanyang University College of Medicine, Seoul, Korea.
References:
- 1. Kohn GP, Galanko JA, Overby DW, Farrell TM. Recent trends in bariatric surgery case volume in the United States. Surgery. 2009;146:375–380. [DOI] [PubMed] [Google Scholar]
- 2. Shiffman ML, Sugerman HJ, Kellum JH, Brewer WH, Moore EW. Gallstones in patients with morbid obesity: relationship to body weight, weight loss and gallbladder bile cholesterol solubility. Int J Obes Relat Metab Disord. 1993;17:153–158. [PubMed] [Google Scholar]
- 3. Dittrick GW, Thompson JS, Campos D, Bremers D, Sudan D. Gallbladder pathology in morbid obesity. Obes Surg. 2005;15:238–242. [DOI] [PubMed] [Google Scholar]
- 4. Mason EE, Renquist KE. Gallbladder management in obesity surgery. Obes Surg. 2002;12:222–229. [DOI] [PubMed] [Google Scholar]
- 5. Liem RK, Niloff PH. Prophylactic cholecystectomy with open gastric bypass operation. Obes Surg 2004;14:763–765. [DOI] [PubMed] [Google Scholar]
- 6. Kim JJ, Schirmer B. Safety and efficacy of simultaneous cholecystectomy at Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5:48–53. [DOI] [PubMed] [Google Scholar]
- 7. Tarantino I, Warschkow R, Steffen T, Bisang P, Schultes B, Thurnheer M. Is routine cholecystectomy justified in severely obese patients undergoing a laparoscopic Roux-en-Y gastric bypass procedure? A comparative cohort study. Obes Surg. 2011;21:1870–1878. [DOI] [PubMed] [Google Scholar]
- 8. Hamad GG, Ikramuddin S, Gourash WF, Schauer PR. Elective cholecystectomy during laparoscopic Roux-en-Y gastric bypass: is it worth the wait? Obes Surg. 2003;13:76–81. [DOI] [PubMed] [Google Scholar]
- 9. Tucker ON, Fajnwaks P, Szomstein S, Rosenthal RJ. Is concomitant cholecystectomy necessary in obese patients undergoing laparoscopic gastric bypass surgery? Surg Endosc. 2008;22:2450–2454. [DOI] [PubMed] [Google Scholar]
- 10. Escalona A, Boza C, Muñoz R, et al. Routine preoperative ultrasonography and selective cholecystectomy in laparoscopic Roux-en-Y gastric bypass. Why not? Obes Surg. 2008;18:47–51. [DOI] [PubMed] [Google Scholar]
- 11. Papasavas PK, Gagné DJ, Ceppa FA, Caushaj PF. Routine gallbladder screening not necessary in patients undergoing laparoscopic Roux en-Y gastric bypass. Surg Obes Relat Dis. 2006;2:41–46. [DOI] [PubMed] [Google Scholar]
- 12. Warschkow R, Tarantino I, Ukegjini K, et al. Concomitant cholecystectomy during laparoscopic Roux-en-Y gastric bypass in obese patients is not justified: a meta-analysis. Obes Surg. 2013;23:397–407. [DOI] [PubMed] [Google Scholar]
- 13. Tsirline VB, Keilani ZM, El Djouzi S, et al. How frequently and when do patients undergo cholecystectomy after bariatric surgery? Surg Obes Relat Dis. 2014;10:313–321. [DOI] [PubMed] [Google Scholar]
- 14. Worni M, Guller U, Shah A, et al. Cholecystectomy concomitant with laparoscopic gastric bypass: a trend analysis of the nationwide in patient sample from 2001 to 2008. 2012;22:220–229. [DOI] [PubMed] [Google Scholar]
- 15. Villegas L, Schneider B, Provost D, et al. Is routine cholecystectomy required during laparoscopic gastric bypass? Obes Surg. 2004;14:60–66. [DOI] [PubMed] [Google Scholar]
- 16. Ellner SJ, Myers TT, Piorkowski JR, Mavanur AA, Barba CA. Routine cholecystectomy is not mandatory during morbid obesity surgery. Surg Obes Relat Dis. 2007;3:456–460. [DOI] [PubMed] [Google Scholar]
- 17. Swartz DE, Felix EL. Elective cholecystectomy after Roux-en-Y gastric bypass: why should asymptomatic gallstones be treated differently in morbidly obese patients? Surg Obes Relat Dis. 2005;1:555–560. [DOI] [PubMed] [Google Scholar]
- 18. Ahmed AR, O'Malley W, Johnson J, Boss T. Cholecystectomy during laparoscopic gastric bypass has no effect on duration of hospital stay. Obes Surg. 2007;17:1075–1079. [DOI] [PubMed] [Google Scholar]
- 19. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 20. Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. 2008;74:985–987. [PubMed] [Google Scholar]
- 21. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. 2009;13:498–503. [DOI] [PubMed] [Google Scholar]
- 22. Vettoretto N, Saronni C, Harbi A, Balestra L, Taglietti L, Giovanetti M. Critical view of safety during laparoscopic cholecystectomy. JSLS. 2011;15:322–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cengiz Y, Janes A, Grehn A, Israelson LA. Randomized clinical trial of traditional dissection with electrocautery versus ultrasonic fundus-first dissection in laparoscopic cholecystectomy. Br J Surg. 2005;92:810–813. [DOI] [PubMed] [Google Scholar]
- 24. Wang YC, Yang HR, Chung PK, Jeng LB, Chen RJ. Role of fundus-first cholecystectomy in the management of acute cholecystitis in elderly patients. J Laparoendosc Adv Surg Tech A. 2006;16:124–127. [DOI] [PubMed] [Google Scholar]
- 25. Neri V, Ambrosi A, Fersini A, Tartaglia N, Valentino TP. Antegrade dissection in laparoscopic cholecystectomy. JSLS. 2007;11:225–228. [PMC free article] [PubMed] [Google Scholar]
- 26. Machado MA, Herman P, Machado MC. Intrahepatic Glissonian approach for pedicle control during anatomic mesohepatectomy. Surgery. 2007;141:533–537. [DOI] [PubMed] [Google Scholar]
- 27. Machado MA, Kalil AN. Glissonian approach for laparoscopic mesohepatectomy. Surg Endosc. 2011;25:2020–2022. [DOI] [PubMed] [Google Scholar]
- 28. Machado MA, Surjan RC, Makdissi FF. Video: intrahepatic Glissonian approach for pure laparoscopic right hemihepatectomy. Surg Endosc. 2011;25:3930–3933. [DOI] [PubMed] [Google Scholar]


